Abstract
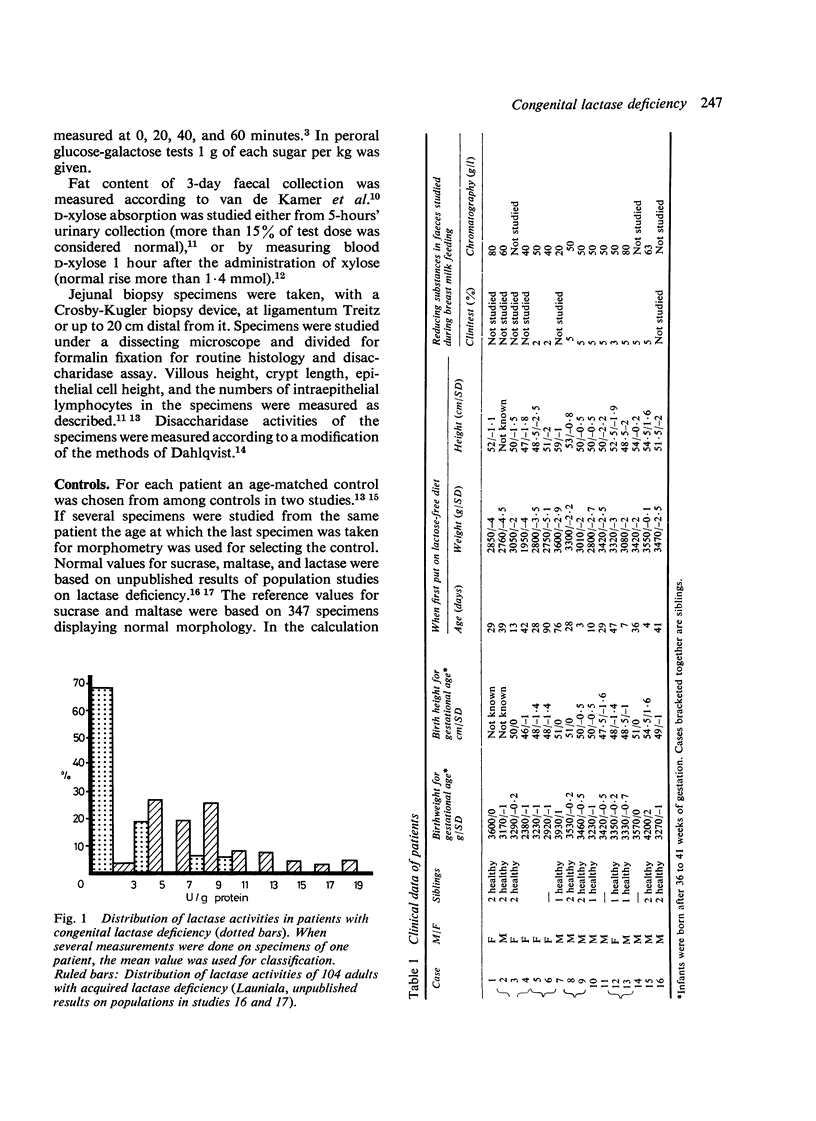
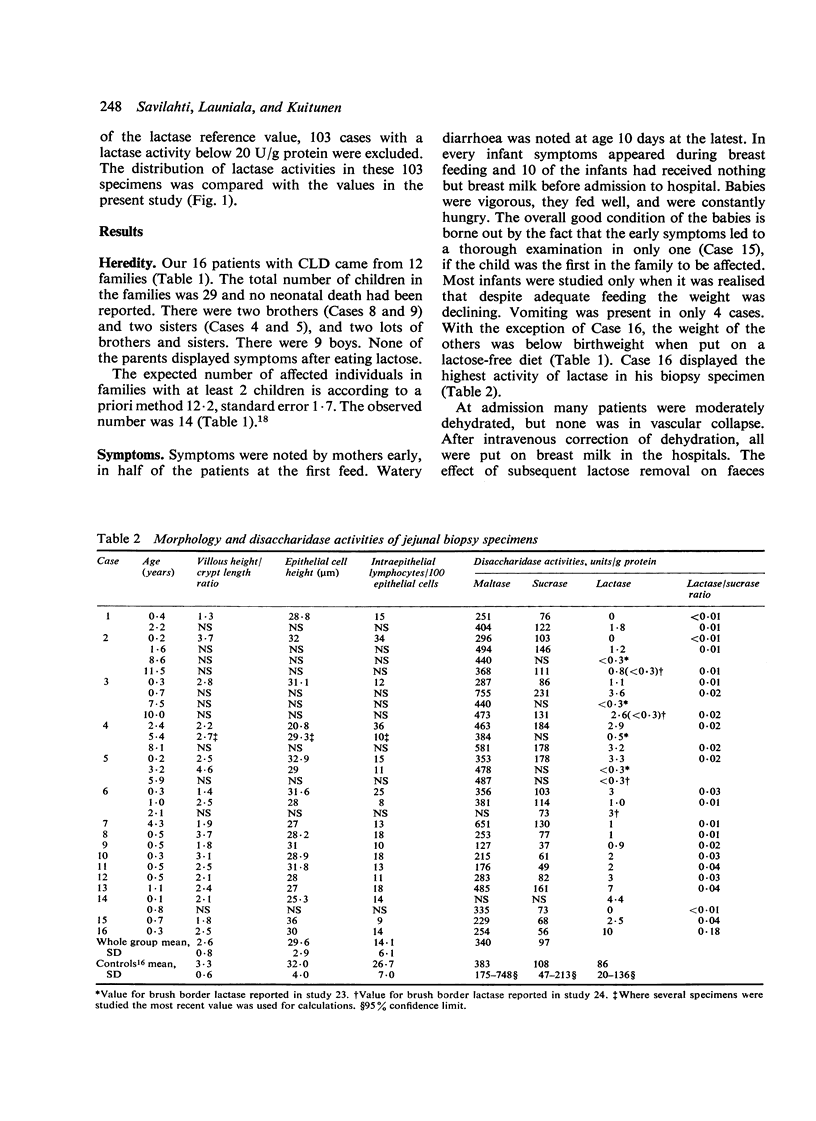
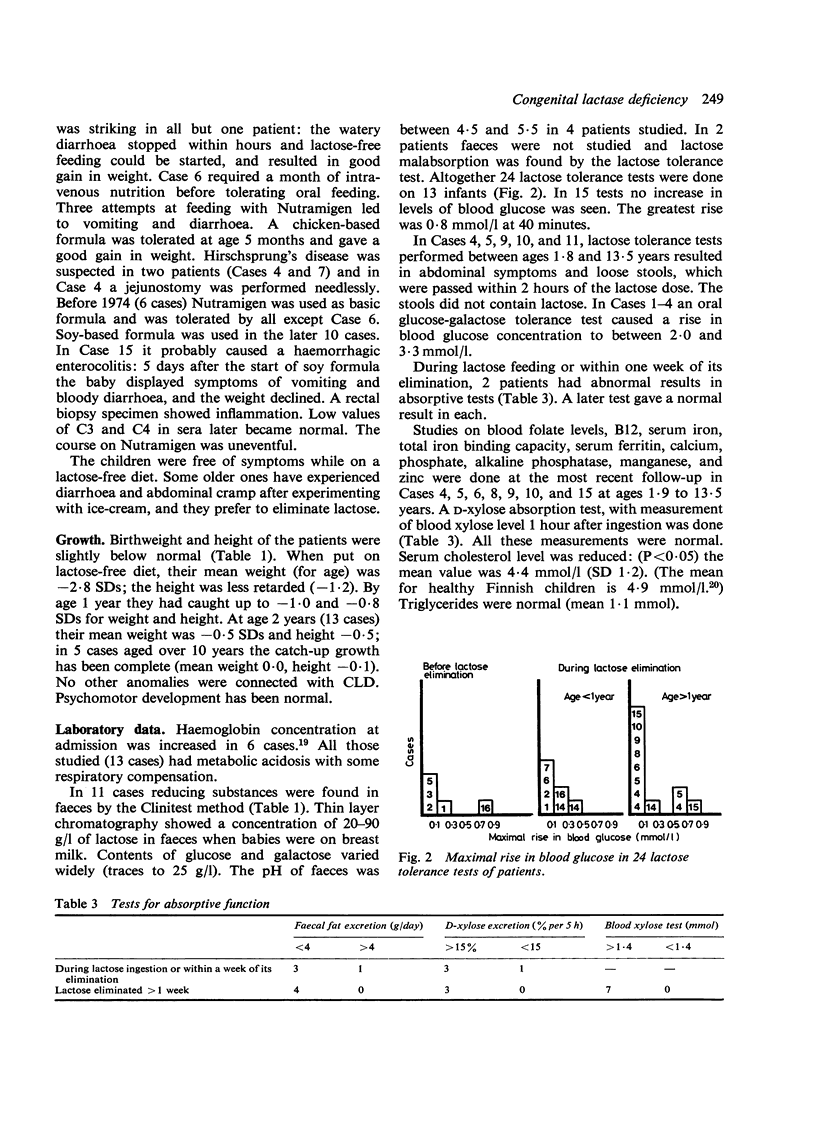
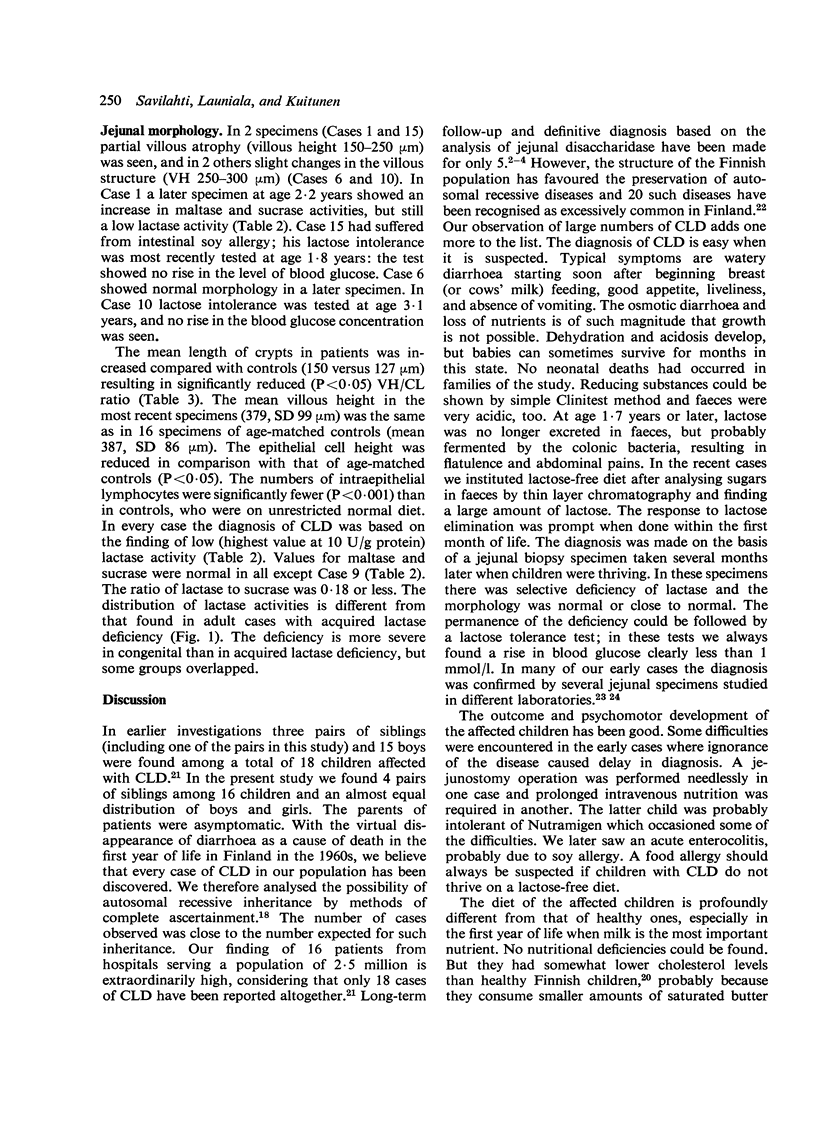
There are at least 20 rare autosomal recessive disorders that are excessively common in Finland of which congenital lactase deficiency is one. During the last 17 years we have found 16 cases. In each case the mother noted watery diarrhoea, generally after the first feed of breast milk, and at the latest, by age 10 days. The lactose malabsorption was verified at a mean age of 36 (range 3-90) days, by which time the infants were dehydrated and 15 of them weighed less than at birth (mean weight for age was -2.8 SDs). On a lactose-free elimination diet (a group of 6 on Nutramigen and a group of 10 on soy-based formula) the children caught up in growth. One infant in each group showed allergic symptoms. While the infants were being breast fed their faeces contained 20 to 80 g/l lactose. In 24 peroral lactose tolerance tests, the greatest rise in blood glucose concentration was 0.8 mmol/l. Only 2 patients showed abnormal absorption when tested within a week of lactose elimination, and in each absorption tests became normal during the elimination period. Slight to partial villous atrophy of the jejunum was present in 4 early specimens, but in later ones the mean villous height was normal. The mean height of the epithelial cells was reduced and there were fewer intraepithelial lymphocytes in patients. The lactase activities in jejunal biopsy specimens were lower than in most patients with acquired lactase deficiency, with some overlap. The maltase and sucrase activities were normal.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asp N. G., Dahlqvist A., Kuitunen P., Launiala K., Visakorpi J. K. Complete deficiency of brush-border lactase in congenital lactose malabsorption. Lancet. 1973 Aug 11;2(7824):329–330. doi: 10.1016/s0140-6736(73)90841-6. [DOI] [PubMed] [Google Scholar]
- Buts J. P., Morin C. L., Roy C. C., Weber A., Bonin A. One-hour blood xylose test: a reliable index of small bowel function. J Pediatr. 1978 May;92(5):729–733. doi: 10.1016/s0022-3476(78)80138-3. [DOI] [PubMed] [Google Scholar]
- Bäckström L., Kantero R. L. Studies on growth of Finnish children from birth to 10 years. II. Cross-sectional studies of height and weight in Finnish children aged from birth to 20 years. Acta Paediatr Scand Suppl. 1971;220:9–12. doi: 10.1111/j.1651-2227.1971.tb14988.x. [DOI] [PubMed] [Google Scholar]
- DAHLQVIST A. METHOD FOR ASSAY OF INTESTINAL DISACCHARIDASES. Anal Biochem. 1964 Jan;7:18–25. doi: 10.1016/0003-2697(64)90115-0. [DOI] [PubMed] [Google Scholar]
- Freiburghaus A. U., Schmitz J., Schindler M., Rotthauwe H. W., Kuitunen P., Launiala K., Hadorn B. Protein patterns of brush-border fragments in congenital lactose malabsorption and in specific hypolactasia of the adult. N Engl J Med. 1976 May 6;294(19):1030–1032. doi: 10.1056/NEJM197605062941903. [DOI] [PubMed] [Google Scholar]
- HOLZEL A., SCHWARZ V., SUTCLIFFE K. W. Defective lactose absorption causing malnutrition in infancy. Lancet. 1959 May 30;1(7083):1126–1128. doi: 10.1016/s0140-6736(59)90710-x. [DOI] [PubMed] [Google Scholar]
- Harrison M., Kilby A., Walker-Smith J. A., France N. E., Wood C. B. Cows' milk protein intolerance: a possible association with gastroenteritis, lactose intolerance, and IgA deficiency. Br Med J. 1976 Jun 19;1(6024):1501–1504. doi: 10.1136/bmj.1.6024.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel A. Sugar malabsorption due to deficiencies of disaccharidase activities and of monosaccharide transport. Arch Dis Child. 1967 Aug;42(224):341–352. doi: 10.1136/adc.42.224.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jussila J., Launiala K., Gorbatow O. Lactase deficiency and a lactose-free diet in patients with "unspecific abdominal complaints". Acta Med Scand. 1969 Sep;186(3):217–222. doi: 10.1111/j.0954-6820.1969.tb01466.x. [DOI] [PubMed] [Google Scholar]
- Jussila J. Milk intolerance and lactose malabsorption in hospital patients and young servicemen in Finland. Ann Clin Res. 1969 Nov;1(3):199–207. [PubMed] [Google Scholar]
- KERRY K. R., ANDERSON C. M. A WARD TEST FOR SUGAR IN FAECES. Lancet. 1964 May 2;1(7340):981–981. doi: 10.1016/s0140-6736(64)91777-5. [DOI] [PubMed] [Google Scholar]
- Kuitunen P. Duodenal-jejunal histology in malabsorption syndrome in infants. Ann Paediatr Fenn. 1966;12(2):101–132. [PubMed] [Google Scholar]
- Kuitunen P., Kosnai I., Savilahti E. Morphometric study of the jejunal mucosa in various childhood enteropathies with special reference to intraepithelial lymphocytes. J Pediatr Gastroenterol Nutr. 1982;1(4):525–531. doi: 10.1097/00005176-198212000-00012. [DOI] [PubMed] [Google Scholar]
- LAUNIALA K., PERHEENTUPA J., VISAKORPI J., HALLMAN N. DISACCHARIDASES OF INTESTINAL MUCOSA IN A PATIENT WITH SUCROSE INTOLERANCE. Pediatrics. 1964 Nov;34:615–620. [PubMed] [Google Scholar]
- Launiala K., Kuitunen P., Visakorpi J. K. Disaccharidases and histology of duodenal mucosa in congenital lactose malabsorption. Acta Paediatr Scand. 1966 May;55(3):257–263. doi: 10.1111/j.1651-2227.1966.tb17652.x. [DOI] [PubMed] [Google Scholar]
- Levin B., Abraham J. M., Burgess E. A., Wallis P. G. Congenital lactose malabsorption. Arch Dis Child. 1970 Apr;45(240):173–177. doi: 10.1136/adc.45.240.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifshitz F. Congenital lactase deficiency. J Pediatr. 1966 Aug;69(2):229–237. doi: 10.1016/s0022-3476(66)80325-6. [DOI] [PubMed] [Google Scholar]
- McCalla R., Savilahti E., Perkkiö M., Kuitunen P., Backman A. Morphology of the jejunum in children with eczema due to food allergy. Allergy. 1980 Oct;35(7):563–571. doi: 10.1111/j.1398-9995.1980.tb01806.x. [DOI] [PubMed] [Google Scholar]
- Saarinen U. M., Siimes M. A. Developmental changes in red blood cell counts and indices of infants after exclusion of iron deficiency by laboratory criteria and continuous iron supplementation. J Pediatr. 1978 Mar;92(3):412–416. doi: 10.1016/s0022-3476(78)80429-6. [DOI] [PubMed] [Google Scholar]


