Abstract
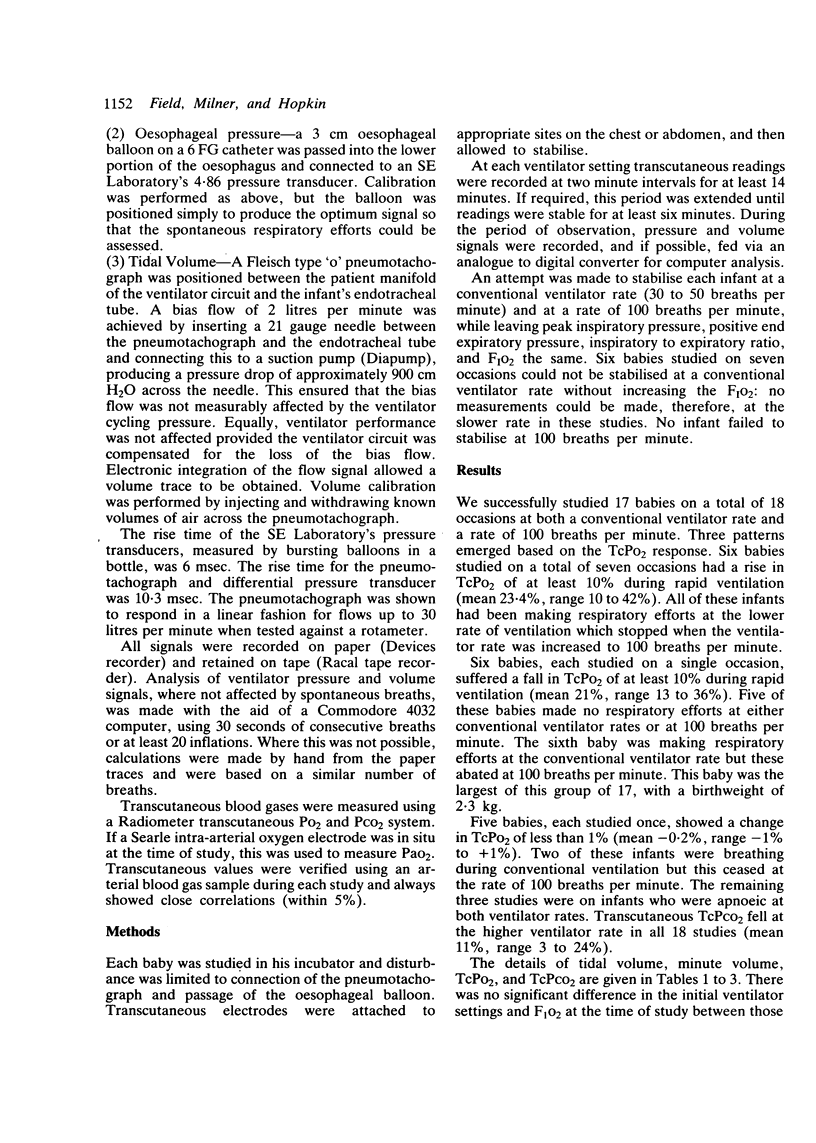
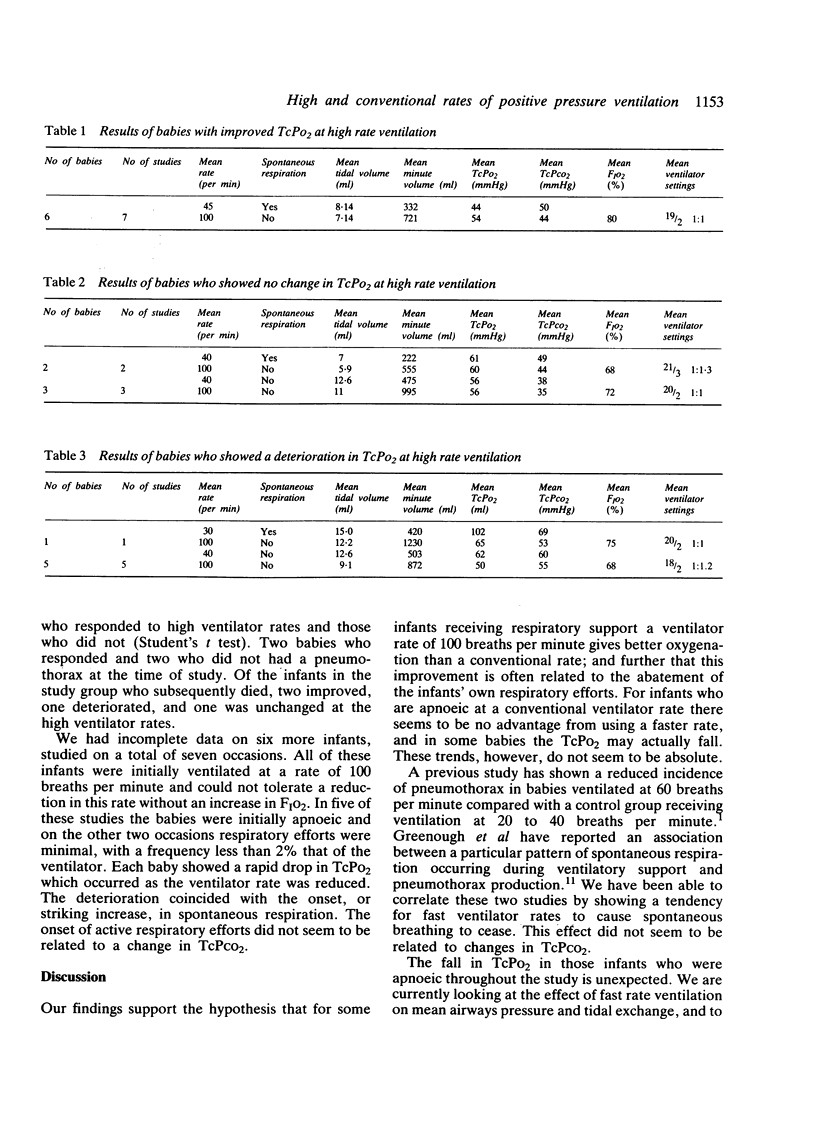
We compared high frequency positive pressure ventilation with conventional rate ventilation in 23 preterm infants with the idiopathic respiratory distress syndrome. Nine infants (10 studies) were making spontaneous respiratory efforts during conventional ventilation that abated at 100 breaths per minute. Six of these showed an increase in TcPo2 of at least 10% at the higher rate (mean 18.5%). Two babies showed no change during high frequency positive pressure ventilation, and in one baby (the largest) the TcPo2 fell. Eight infants were apnoeic at both ventilator rates: five suffered a fall in TcPo2 of at least 10% at 100 breaths per minute (mean 19%) and three were unchanged. A further six infants (seven studies) would not tolerate a reduction in rate from 100 breaths per minute without an increase in FIO2. Failure to tolerate a conventional ventilator rate in these circumstances seemed related to the onset or a noticeable increase in spontaneous respiratory efforts.
Full text
PDF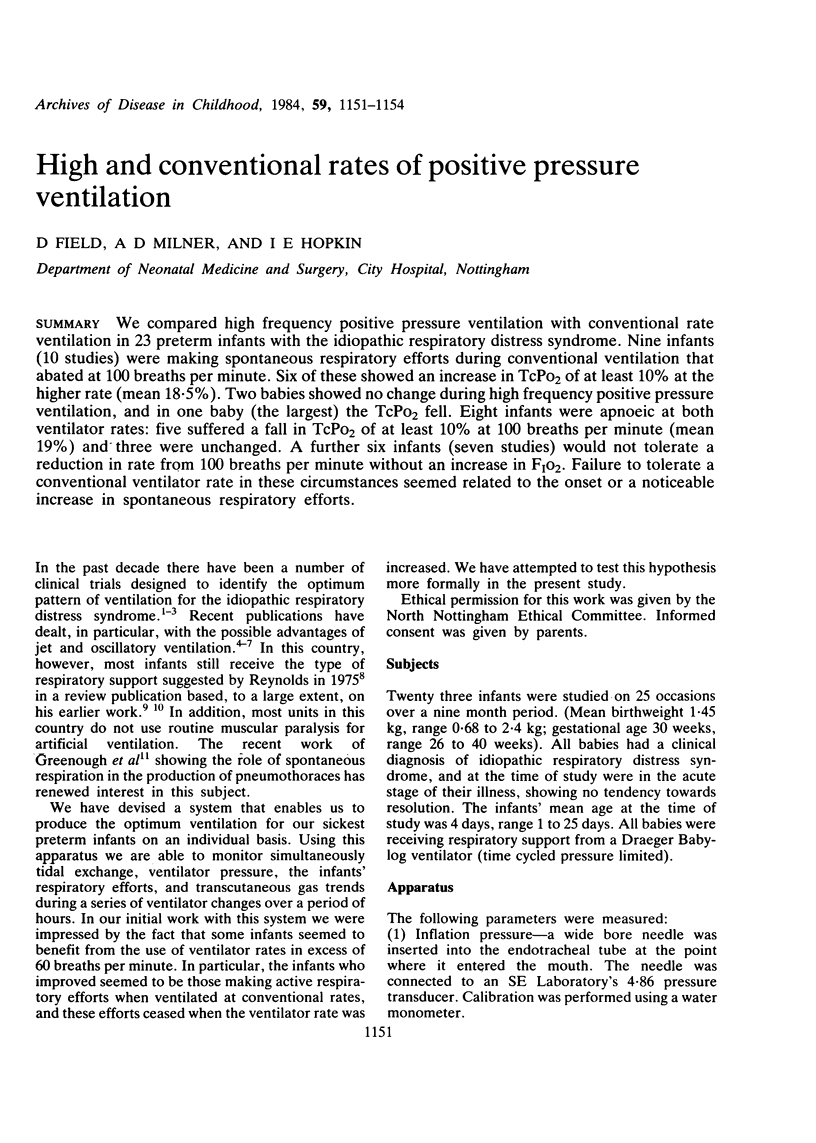

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boros S. J., Campbell K. A comparison of the effects of high frequency--low tidal volume and low frequency--high tidal volume mechanical ventilation. J Pediatr. 1980 Jul;97(1):108–112. doi: 10.1016/s0022-3476(80)80146-6. [DOI] [PubMed] [Google Scholar]
- Carlo W. A., Chatburn R. L., Martin R. J., Lough M. D., Shivpuri C. R., Anderson J. V., Fanaroff A. A. Decrease in airway pressure during high-frequency jet ventilation in infants with respiratory distress syndrome. J Pediatr. 1984 Jan;104(1):101–107. doi: 10.1016/s0022-3476(84)80604-6. [DOI] [PubMed] [Google Scholar]
- Greenough A., Wood S., Morley C. J., Davis J. A. Pancuronium prevents pneumothoraces in ventilated premature babies who actively expire against positive pressure inflation. Lancet. 1984 Jan 7;1(8367):1–3. doi: 10.1016/s0140-6736(84)90177-6. [DOI] [PubMed] [Google Scholar]
- Heicher D. A., Kasting D. S., Harrod J. R. Prospective clinical comparison of two methods for mechanical ventilation of neonates: rapid rate and short inspiratory time versus slow rate and long inspiratory time. J Pediatr. 1981 Jun;98(6):957–961. doi: 10.1016/s0022-3476(81)80604-x. [DOI] [PubMed] [Google Scholar]
- Herman S., Reynolds E. O. Methods for improving oxygenation in infants mechanically ventilated for severe hyaline membrane disease. Arch Dis Child. 1973 Aug;48(8):612–617. doi: 10.1136/adc.48.8.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchak B. E., Thompson W. K., Duffty P., Miyaki T., Bryan M. H., Bryan A. C., Froese A. B. Treatment of RDS by high-frequency oscillatory ventilation: a preliminary report. J Pediatr. 1981 Aug;99(2):287–292. doi: 10.1016/s0022-3476(81)80480-5. [DOI] [PubMed] [Google Scholar]
- Reynolds E. O. Effect of alterations in mechanical ventilator settings on pulmonary gas exchange in hyaline membrane disease. Arch Dis Child. 1971 Apr;46(246):152–159. doi: 10.1136/adc.46.246.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds E. O. Management of hyaline membrane disease. Br Med Bull. 1975 Jan;31(1):18–24. doi: 10.1093/oxfordjournals.bmb.a071235. [DOI] [PubMed] [Google Scholar]
- Spahr R. C., Klein A. M., Brown D. R., MacDonald H. M., Holzman I. R. Hyaline membrane disease. A controlled study of inspiratory to expiratory ratio in its management by ventilator. Am J Dis Child. 1980 Apr;134(4):373–376. doi: 10.1001/archpedi.1980.04490010031011. [DOI] [PubMed] [Google Scholar]


