There is little agreement among doctors and midwives about the optimal time to clamp the umbilical cord after birth. The most important points of difference relate to maternal and infant safety. Many healthcare workers worldwide tend to clamp the cord and pass the baby off as quickly as possible. Infants in resource poor settings are the main victims of immediate clamping, as this prevents a cost-free means of boosting their small iron stores.
Infant anaemia is common in poor communities, especially where malaria is endemic. In sub-Saharan Africa more than 75% of infants are anaemic before 6 months of age.w1-w3 Infant anaemia is associated with increased mortalityw4 w5 and with impaired mental and motor development.w6 Its prevention is of critical importance, and delaying clamping of the umbilical cord could be an effective strategy to reduce anaemia and improve child survival.
We propose a practice guideline on cord clamping for resource poor countries for singleton vaginal deliveries, based on published systematic reviews, randomised controlled trials, and biological evidence. Taking account of the safety of mothers and infants, we provide evidence about inclusion and exclusion criteria for delayed cord clamping, optimal timing of clamping, infant position during placental-fetal transfusion, and potential side effects. We present the evidence as a series of structured clinical questions, which identify the population concerned (mothers and infants from resource poor countries), the options being compared (mostly delayed versus immediate cord clamping), and the outcome measures used to measure effectiveness and safety of delayed cord clamping. We also present a practical and simple flow chart for quick reference.
Clinical questions
Is delayed cord clamping associated with improved haematological status in infancy?
Four randomised controlled trials, all from developing countries, evaluated haemoglobin concentrations in term infants 2-4 months after birth.2-5 Meta-analysis showed that haemoglobin concentrations were significantly higher after delayed cord clamping (317 infants, weighted mean difference 4.9 g/l (95% confidence interval 2.6 to 7.2 g/l)). The proportion of infants with anaemia was lower with delayed cord clamping (three trials, 127 infants, relative risk 0.53 (95% confidence interval 0.40 to 0.69)).2,3,5 A large randomised controlled trial from Mexico showed a beneficial effect of delayed cord clamping on infant iron status could be measured six months after birth, although haemoglobin levels were no longer different.6
Summary points
There is little agreement about the optimal time to clamp the umbilical cord after birth
Delaying clamping of the umbilical cord is a cheap and effective strategy to reduce infant anaemia and improve child survival in resource poor settings
This practice guideline for singleton vaginal deliveries takes into account the safety of both mothers and infants
Delayed cord clamping should be considered in every infant born in a resource poor setting, regardless of gestational age
It should be combined with the administration of oxytocin immediately after delivery to reduce maternal blood loss in the third stage of labour
Cord clamping should be delayed for at least three minutes for optimal placental transfusion, regardless of fetal weight
When the state of the infant does not allow a clamping delay of three minutes, aim for a delay of at least 60 seconds with the infant placed between the mother's legs
The haematological effects of delayed cord clamping in preterm infants were studied in four randomised controlled trials from industrialised countries.7-10 The observation period lasted four to six weeks and comprised the time the infants were admitted to the neonatal intensive care unit. Many of these infants born before 30 weeks of gestation would not have survived in resource poor countries. After delayed cord clamping, fewer of these infants required blood transfusion in the first six weeks after birth (183 infants, relative risk 0.64 (0.46 to 0.88)).
Is delayed cord clamping associated with side effects that require treatment?
Four controlled trials and one randomised controlled trial, all from industrialised countries,11-16 and two randomised controlled trials from resource poor countries5,17 evaluated the incidence of hyperbilirubinaemia and hyperviscosity in term neonates. Packed cell volume was significantly higher after delayed cord clamping, but infants showed no evidence of hyperviscosity syndrome and partial exchange transfusion was never needed. Although peak bilirubin concentrations tended to be higher after delayed cord clamping, the phototherapy threshold was never exceeded and none required exchange transfusion. Meta-analysis showed that delayed cord clamping in healthy term infants caused no side effects requiring treatment (seven trials, 583 infants, relative risk 0.20 (0.01 to 3.97)).
Methods
Search strategy
We identified systematic reviews from the Cochrane Library (issue 2, 2006). We identified randomised controlled trials from the Cochrane Library, PubMed (1966 to June 2006), and EMBASE (1988 to June 2006) using the terms “umbilical cord” and “clamp*.” We examined related articles and reference lists of published trials, and hand searched major journals on perinatal and tropical medicine. Any new evidence was used to update existing meta-analyses. When a systematic review or meta-analysis did not exist, we completed our own following published methods.w7
Criteria for considering trials for meta-analysis
We included randomised and quasi-randomised trials comparing immediate cord clamping (within 20 seconds of birth) with delayed clamping in infants born vaginally at 30-42 weeks' gestation and with birth weight > 1000 g. We excluded infants born before 30 completed weeks' gestation or with birth weights < 1000 g because their mortality is high in resource poor countries.w8-w10
Quality assessment
To minimise bias and to aid interpretation of the guidelines, we used the systematic approach to grading the strength of recommendations developed by the GRADE working group1:
-
Levels of evidence
High—Further research is unlikely to change our confidence in the estimate of effect
Moderate—Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate
Low—Further research is highly likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate
Very low—Any estimate of effect is very uncertain
-
Grades of recommendations
The strength of a recommendation indicates the extent to which one can be confident that adherence to the recommendation will do more good than harm
Strong—Do it
Weak—Probably do it
Three randomised trials and one quasi-randomised controlled trial in preterm neonates, all from industrialised countries, measured peak bilirubin and found significantly higher concentrations after delayed cord clamping (259 infants, weighted mean difference 25 μmol/l (14 to 36 μmol/l)).8-10,15 Two of these four trials reported the incidence of hyperbilirubinaemia necessitating treatment and found no difference between delayed cord clamping and immediate clamping (138 infants, relative risk 1.09 (0.66 to 1.81)).10,15 It is unclear whether these results can be extrapolated to resource poor countries, where low birth weight babies are predominantly growth retarded. About a third of the preterm infants in the study by Rabe et al10 were growth retarded and equally distributed between delayed cord clamping and immediate clamping. Necrotising enterocolitis was examined in two trials, and the incidence did not differ between delayed and immediate clamping (111 infants, relative risk 0.76 (0.37 to 1.58)).9,10
Body temperature on admission to the neonatal intensive care unit was studied in only one trial, which found no difference between delayed and immediate clamping (39 infants, weighted mean difference 0.20°C (-0.03 to 0.43)).10 This should be studied further and advice is required about keeping the baby wrapped and warm.
Recommendation
• Delayed cord clamping should be considered in every infant born in a resource poor setting, regardless of gestational age
Grade of recommendation: Strong
Is delayed cord clamping associated with increased maternal blood loss?
Two randomised controlled trials (one from a resource poor country5) evaluated the effect of cord clamping on maternal blood loss.5,16 Major limitations of these trials were the differences in the method of measuring blood loss (visual estimation versus measuring jar), the mode of delivery (100% vaginal versus > 25% caesarean section), and the definition of delayed cord clamping. The risk of postpartum haemorrhage, defined as blood loss of > 500 ml, was not different after delayed cord clamping or immediate clamping (363 participants, relative risk 0.89 (0.58 to 1.36)). A Mexican trial did not quantitatively measure maternal blood loss but classified the bleeding as normal, high, or severe, and found no differences between delayed cord clamping and immediate clamping.6
How does delayed cord clamping affect obstetric management of the third stage of labour?
The third stage of labour is defined as the period from expulsion of the fetus to the expulsion of the placenta. In active management the aim is to keep this period as short as possible to reduce maternal blood loss, but the time frame is not exactly specified. In expectant management the aim is to deliver the placenta within one hour without medical interference. A Cochrane review compared active management with expectant management and included five randomised controlled trials from industrialised countries.18 Active management involves clamping the cord as soon as possible, as well as routinely using prophylactic uterotonic drugs and controlled cord traction. Expectant management is a “hands off” policy, in which signs of placental separation are awaited and spontaneous delivery of the placenta is allowed. Active management was associated with a reduction in clinically estimated maternal blood loss (two trials, 2941 participants, weighted mean difference -79 ml (-94 to -64))w11 w12 and a reduced risk of postpartum haemorrhage (four trials, 6284 participants, relative risk 0.38 (0.32 to 0.46)).w11-w14
The administration of uterotonic drugs immediately after delivery of the baby, which forms the main-stay of active management, would hasten the transfer of blood into the baby and increase the infant's red cell mass.w15 w16 Immediately after placental transfusion is completed, after about three minutes, the cord can be clamped and cut, and delivery of the placenta by controlled cord traction can commence.
The authors of the Cochrane review concluded that routine “active management is superior to expectant management” in terms of maternal complications but considered that research was needed in the developing world, with its higher incidence of maternal and infant mortality. Whether all the components of full active management are useful should also be investigated.w17 The International Confederation of Midwives and the International Federation of Gynaecologists and Obstetricians have not waited for these studies before acting and have removed immediate cord clamping from their recommendations.w18 Oxytocin is the uterotonic drug of choice, but there are problems with its universal availability and storage conditions.
Recommendation
• Delayed cord clamping should be combined with the administration of oxytocin immediately after delivery of the infant to reduce maternal blood loss in the third stage of labour
Grade of recommendation: Strong
Is delayed cord clamping in growth retarded infants associated with more adverse effects?
A systematic review has established the safety of delayed cord clamping in normal birthweight babies,19 but there is little information about growth retarded babies.20 Those born in industrialised countries often have an increased incidence of polycythaemia due to chronic hypoxaemia in utero and increased fetal erythropoiesis. In the presence of sufficient iron this leads to increased packed cell volume, although half of growth retarded newborn babies have ferritin concentrations below the fifth centile.w19 Most polycythaemic infants remain asymptomatic, although growth retarded babies may be at greater risk of symptoms and the clinical consequences of altered blood viscosity.w20
The baseline risk for polycythaemia and hyperviscosity in growth retarded babies in resource poor countries should be low because many infants have low cord haemoglobin concentration in areas where malaria and maternal iron deficiency anaemia are common.w21-w23 In these areas up to 30% of babies have fetal anaemia, defined as cord haemoglobin concentration below 125 g/l.w21
What is the optimal delay for cord clamping in infants in relation to their position during placental transfusion?
Vaginally born, normal birthweight infants
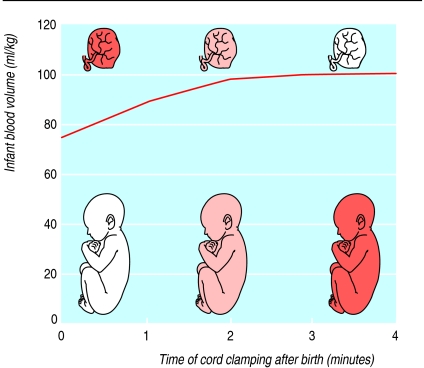
The total fetoplacental blood volume is about 120 ml/kg of fetal weight.w24-w27 At birth, the distribution of blood between fetus and placenta is roughly in a ratio of 2:1, and this distribution remains unchanged if the cord is clamped immediately. Figure 1 shows that allowing placental transfusion to occur for at least three minutes results in a larger infant blood volume (ratio 5:1).w24 w25 The rate of placental transfusion is markedly influenced by the position of the delivered infant. An infant held 50-60 cm above the placenta will not receive any blood from the placenta. From 10 cm above to 10 cm below the level of the placenta, infants receive the maximum possible amount after at least three minutes of birth. Keeping the infant 40 cm below the placenta hastens placental transfusion to near completion within one minute.w24 w28
Fig 1.
Distribution of blood between infant and placenta depending on time of cord clamping after birth (adapted from Linderkampw24 and Yaoetalw25). The term infants are at the level of the introitus, about 10 cm below the placenta
The randomised and quasi-randomised controlled trials that studied delayed cord clamping in vaginally born, healthy, term infants differed in clamping time and infant position before clamping (see table). All the trials showed that placental transfusion occurred after delayed cord clamping by showing higher packed cell volume or haemoglobin concentration in the first 24 hours after birth compared with immediate clamping.2-6,11-16,21,22
Table 1.
Position of infant in relation to timing of cord clamping in trials that studied vaginally born, healthy, term infants
|
Position of infant in relation to placenta
|
Time to cord clamping (minutes)
|
|||
|---|---|---|---|---|
| 1-2 | 3 | 5 | >5 | |
| >10 cm above | Ceriani Cernadas et al16 | Nelle et al12-14; Ceriani Cernadas et al16 | — | — |
| 0-10 cm below | Chaparro et al6 | Linderkamp et al11 | Grajeda et al2; van Rheenen et al5; Pao-Chen et al22 | Gupta et al3; Lanzkowsky et al4; Geethanath et al21 |
| 30 cm below | Saigal et al15 | — | Saigal et al15 | — |
Recommendation
• Cord clamping should be delayed for at least three minutes for the optimal volume of placental transfusion, regardless of fetal weight
Grade of recommendation: Weak
Vaginally born, low birthweight infants
Most of the low birthweight infants in the cord clamping trials were born by caesarean section. Six trials had a sufficient number of vaginally born preterm infants.7-9,15,23-25 There was considerable heterogeneity in clamping time and infant position before clamping. In five trials the cord was clamped after a delay of 30-60 seconds,7-9,23,25 and all but one compensated for the relatively short delay by lowering the infant as much as cord length permitted to ensure placental transfusion. The trial in which infants were not lowered failed to show placental transfusion.8 In the trial with a clamping delay of 1-2 minutes the infants were also not lowered, but the longer delay was sufficient for placental transfusion.24
What is the optimal time of clamping when neonatal resuscitation is required?
The vast majority of newborn infants do not require resuscitation—immediate drying and keeping them warm is all that is required. Less than 10% of newborns require help to start breathing at birth (stimulation, positioning, clearing the airway), and about 1% require extensive resuscitation. When respiratory efforts are absent or inadequate despite initial stabilisation, positive pressure ventilation with a self inflating bag is the priority.w29 The earliest time to assess whether ventilation is successful is about 60 seconds after delivery.
All these steps can be done while the umbilical cord is intact. When resuscitation is required the preferred position for the infant should be between the mother's legs, as bag-mask ventilation is not feasible if the infant is placed on the mother's abdomen. Immediate cord clamping to enable resuscitation away from the mother could deprive the infant of much needed extra blood volume, and the resulting hypovolaemia might adversely affect tissue perfusion. Furthermore, as long as the uterus is not contracting and the placenta has not been detached, the infant may still receive oxygen via the intact placental-fetal circulation.
Recommendation
• When the state of the infant does not allow a clamping delay of three minutes, aim for a delay of at least 60 seconds with the infant placed between the mother's legs
Grade of recommendation: Weak
Conclusions
The evidence we reviewed can be summarised as follows:
-
Delayed cord clamping in term infants is safe and, compared with immediate clamping, is associated with higher haemoglobin concentrations and lower incidence of anaemia in the first 4 months of life, and higher iron stores up to at least 6 months
Level of evidence: Moderate
-
Although delayed cord clamping in preterm infants is associated with higher peak bilirubin concentrations, the need to give treatment for hyperbilirubinaemia was not different after immediate clamping. Delayed cord clamping is safe in preterm infants and is associated with fewer blood transfusions in the first 6 weeks of life compared with immediate clamping
Level of evidence: Moderate
-
Delayed cord clamping in combination with administration of oxytocin immediately after delivery of the baby is safe for mothers
Level of evidence: Moderate
-
There is little information on delayed cord clamping in growth retarded babies, but the presumed baseline risk for polycythaemia in these infants is probably lower in resource poor countries than in industrialised countries
Level of evidence: Low
-
In normal birthweight babies, for the maximum possible volume of placental transfusion cord clamping should be delayed for at least three minutes, provided that the position of the baby before clamping is on the mother's abdomen or lower
Level of evidence: Moderate
-
In low birthweight babies delaying clamping for 30-60 seconds without lowering the baby is probably not effective
Level of evidence: Moderate
When immediate neonatal resuscitation is required, place the child between the legs of the mother, start positive pressure ventilation with the umbilical cord intact and delay clamping for at least 60 seconds
Level of evidence: Very low
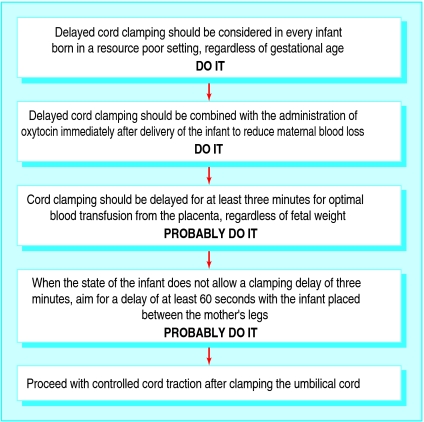
We also provide a flow chart of our guidelines on cord clamping in resource poor settings for quick reference (fig 2).
Fig 2.
Guidelines for cord clamping in resource poor settings
Supplementary Material
 References w1-w29 are on bmj.com
References w1-w29 are on bmj.com
We thank the following for their critical review of the manuscript: R Broadhead, College of Medicine, University of Malawi, Blantyre, Malawi; J Bunn, Department of Paediatrics, College of Medicine, Blantyre, Malawi; C Chintu, Department of Paediatrics and Child Health, University Teaching Hospital, Lusaka, Zambia; R Cooke, Neonatal Unit, Liverpool Women's Hospital, Liverpool; P Kazembe, Department of Paediatrics, Kamuzo Central Hospital, Lilongwe, Malawi; E Molyneux, Paediatric Department, Queen Elizabeth Central Hospital, College of Medicine, Blantyre, Malawi; JJM van Roosmalen, Department of Obstetrics, Leiden University Medical Centre, Leiden, Netherlands; DAA Verkuyl, Department of Gynaecology and Obstetrics, Bethesda Hospital, Hoogeveen, Netherlands. Contributors: PFvR and BJB were responsible for the study idea and design. Both authors contributed to interpreting the data and revising the text. PFvR is guarantor and drafted the manuscript.
Funding: None.
Competing interests: None declared.
References
- 1.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328: 1490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grajeda R, Perez-Escamilla R, Dewey KG. Delayed clamping of the umbilical cord improves hematologic status of Guatemalan infants at 2 mo of age. Am J Clin Nutr 1997;65: 425-31. [DOI] [PubMed] [Google Scholar]
- 3.Gupta R, Ramji S. Effect of delayed cord clamping on iron stores in infants born to anemic mothers: a randomized controlled trial. Indian Pediatr 2002;39: 130-5. [PubMed] [Google Scholar]
- 4.Lanzkowsky P. Effects of early and late clamping of umbilical cord on infant's haemoglobin level. BMJ 1960;ii: 1777-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Rheenen PF, de Moor LTT, Eschbach S, de Grooth H, Brabin BJ. Delayed cord clamping and haemoglobin levels in infancy: a randomised controlled trial in term babies. Unpublished study. [DOI] [PubMed]
- 6.Chaparro CM, Neufeld LM, Tena AG, Eguia-Liz CR, Dewey KG. Effect of timing of umbilical cord clamping on iron status in Mexican infants: a randomised controlled trial. Lancet 2006;367: 1997-2004. [DOI] [PubMed] [Google Scholar]
- 7.Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA. Umbilical cord clamping and preterm infants: a randomised trial. BMJ 1993;306: 172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonnell M, Henderson-Smart DJ. Delayed umbilical cord clamping in preterm infants: a feasibility study. J Paediatr Child Health 1997;33: 308-10. [DOI] [PubMed] [Google Scholar]
- 9.Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W. Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late onset sepsis: a randomized controlled trial. Pediatrics 2006;117: 1235-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rabe H, Wacker A, Hulskamp G, Hornig-Franz I, Schulze-Everding A, Harms E, et al. A randomised controlled trial of delayed cord clamping in very low birth weight preterm infants. Eur J Pediatr 2000;159: 775-7. [DOI] [PubMed] [Google Scholar]
- 11.Linderkamp O, Nelle M, Kraus M, Zilow EP. The effect of early and late cord-clamping on blood viscosity and other hemorheological parameters in full-term neonates. Acta Paediatr 1992;81: 745-50. [DOI] [PubMed] [Google Scholar]
- 12.Nelle M, Zilow EP, Kraus M, Bastert G, Linderkamp O. The effect of Leboyer delivery on blood viscosity and other hemorheologic parameters in term neonates. Am J Obstet Gynecol 1993;169: 189-93. [DOI] [PubMed] [Google Scholar]
- 13.Nelle M, Zilow EP, Bastert G, Linderkamp O. Effect of Leboyer childbirth on cardiac output, cerebral and gastrointestinal blood flow velocities in full-term neonates. Am J Perinatol 1995;12: 212-6. [DOI] [PubMed] [Google Scholar]
- 14.Nelle M, Kraus M, Bastert G, Linderkamp O. Effects of Leboyer childbirth on left- and right systolic time intervals in healthy term neonates. J Perinat Med 1996;24: 513-20. [DOI] [PubMed] [Google Scholar]
- 15.Saigal S, O'Neill A, Surainder Y, Chua LB, Usher R. Placental transfusion and hyperbilirubinemia in the premature. Pediatrics 1972;49: 406-19. [PubMed] [Google Scholar]
- 16.Ceriani Cernadas JM, Carroli G, Pellegrini L, Otano L, Ferreira M, Ricci C, et al. The effect of timing of cord clamping on neonatal venous hematocrit values and clinical outcome at term: a randomized controlled trial. Pediatrics 2006;117: e779-86. [DOI] [PubMed] [Google Scholar]
- 17.Emhamed M, van Rheenen P, Brabin BJ. The early effects of delayed cord clamping in term infants born to Libyan mothers. Tropical Doctor 2004;34: 218-22. [DOI] [PubMed] [Google Scholar]
- 18.Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev 2000;(3):CD000007. [DOI] [PubMed]
- 19.Van Rheenen P, Brabin BJ. Late umbilical cord clamping as an intervention for reducing iron deficiency anaemia in term infants in developing and industrialised countries: a systematic review. Ann Trop Paediatr 2004;24: 3-16. [DOI] [PubMed] [Google Scholar]
- 20.Van Rheenen P, Gruschke S, Brabin BJ. Delayed umbilical cord clamping for reducing anaemia in LBW infants - implications for developing countries. Ann Trop Paediatr 2006;26: 157-67. [DOI] [PubMed] [Google Scholar]
- 21.Geethanath RM, Ramji S, Thirupuram S, Rao YN. Effect of timing of cord clamping on the iron status of infants at 3 months. Indian Pediatr 1997;34: 103-6. [PubMed] [Google Scholar]
- 22.Pao-Chen W, Tsu-Shan K. Early clamping of the umbilical cord. A study of its effect on the infant. Chin Med J 1960;80: 351-5. [PubMed] [Google Scholar]
- 23.Aladangady N, McHugh S, Aitchison TC, Wardrop CA, Holland BM. Infants' blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics 2006;117: 93-8. [DOI] [PubMed] [Google Scholar]
- 24.Hofmeyr GJ, Gobetz L, Bex PJ, Van der GM, Nikodem C, Skapinker R, et al. Periventricular/intraventricular hemorrhage following early and delayed umbilical cord clamping. A randomized controlled trial. Online J Curr Clin Trials 1993;110: 2002. [PubMed] [Google Scholar]
- 25.Mercer JS, McGrath MM, Hensman A, Silver H, Oh W. Immediate and delayed cord clamping in infants born between 24 and 32 weeks: a pilot randomized controlled trial. J Perinatol 2003;23: 466-72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.