Abstract
Medicaid conversion from fee for service to managed care raised numerous questions about outcomes for substance abuse treatment clients. For example, managed care criticisms include concerns that clients will be undertreated (with too short and/or insufficiently intense services). Also of interest are potential variations in outcome for clients served by organizations with assorted financial arrangements such as for-profit status versus not-for-profit status. In addition, little information is available about the impact of state Medicaid managed care policies (including client eligibility) on treatment outcomes. Subjects of this project were Medicaid clients aged 18–64 years enrolled in the Oregon Health Plan during 1994 (before substance abuse treatment managed care, N = 1751) or 1996–1997 (after managed care, N = 14,813), who were admitted to outpatient non-methadone chemical dependency treatment services. Outcome measures were retention in treatment for 90 days or more, completion of a treatment program, abstinence at discharge, and readmission to treatment. With the exception of readmission, there were no notable differences in outcomes between the fee for service era clients versus those in capitated chemical dependency treatment. There were at most minor differences among various managed care systems (such as for-profit vs not-for-profit). However, duration of Medicaid eligibility was a powerful predictor of positive outcomes. Medicaid managed care does not appear to have had an adverse impact on outcomes for clients with substance abuse problems. On the other hand, state policies influencing Medicaid enrollment may have substantial impact on chemical dependency treatment outcomes.
Introduction
People with substance abuse problems depend heavily on the public sector for treatment.1–3 In particular, Medicaid is a substantial and growing payer for chemical dependency services.1 Medicaid behavioral healthcare systems have undergone marked change in the last decade2 as programs shifted away from fee for service and toward managed care approaches, such as case rates or capitation.3–5 Concerns have been expressed about the impact of these changes on access to services and the outcomes thereof.6
Mechanic pointed out that providers operating under managed care arrangements have “a disincentive to offer a level of comprehensiveness and quality of care that will attract particularly needy and expensive clients.”7 Critics of managed care have also suggested that clients may be given services that are less intense or of shorter duration than clinically indicated.8 The concerns are that managed care programs such as capitation may motivate providers to ignore more severely impaired clients, decrease intensity of services, and/or reduce the duration of treatment. The implication here is that client outcomes will be worse under managed care than under fee for service.
These concerns are especially important for Medicaid clients. Several authors have noted that state Medicaid agencies have increasingly embraced managed care approaches such as health maintenance organizations and/or financial risk sharing even as the private sector has moved away from these programs.9–11 With regard to substance abuse treatment, Alexander et al found that over the last few years public sector managed care arrangements have increased whereas those in the private sector have decreased.12
Since Medicaid managed behavioral healthcare is evidently “here to stay,” decision makers in state substance abuse and Medicaid agencies need information about the impact of the various managed care arrangements on services and outcomes. Moreover, given the importance of Medicaid to the funding of substance abuse treatment,1 attention should also be paid to relationships between state Medicaid policies (such as enrollment criteria) and treatment outcomes.
As it happens, projects in Oregon,13 Iowa,14,15 and Maryland16 have examined the impact of Medicaid managed care on use of substance abuse treatment services. In general, these studies showed that overall access to services apparently increased following the shift to managed care.13,14 However, Ettner et al pointed out that capitation may provide incentives for health plans to focus on less severely impaired patients16 (sometimes referred to as “cream-skimming”). Interestingly enough, the severity of patients entering publicly funded substance abuse treatment programs was about the same before and after Medicaid managed care in Oregon17 and even increased in Iowa.16
Service provision for Medicaid clients with substance abuse disorders has been another area of considerable concern. Whereas the fee for service system rewards treatment delivery, managed care financing mechanisms such as capitation may motivate providers to reduce services.4,18,19 Ettner et al noted that capitated programs in particular may be tempted to minimize service provision16 (which might be called “short-changing”). Indeed, Etheridge et al found a significant reduction nationwide over time in the number and range of services that substance abuse clients received.20 Studies in Iowa15 and Maryland16 showed a shift from inpatient and residential to outpatient programs following introduction of Medicaid managed care. While it is conceivable that such changes in service provision might lead to poor treatment outcomes, no adverse impact was found in Maryland.16 On the other hand, little information is available from states (such as Oregon) that have traditionally emphasized outpatient services (rather than inpatient or residential care) for people with substance abuse problems.
Especially worrisome is the (potential) impact of managed care and/or state Medicaid enrollment policies on treatment duration for public sector chemical dependency clients. This topic is of interest to policymakers since a large body of literature suggests that there is a minimum duration of treatment for people with substance abuse problems.21,22 Indeed, the National Institute on Drug Abuse in its Thirteen Principles of Effective Drug Addiction Treatment states that “remaining in treatment for an adequate period of time is critical for treatment effectiveness.”23 While this statement is not entirely without controversy,24 the National Institute on Drug Abuse has also suggested that “the threshold of significant improvement is reached at about 3 months in treatment.”23 Work from Maryland suggests that the implementation of managed care led, if anything, to increased treatment duration for Medicaid clients with substance abuse problems.16 However, this finding has yet to be replicated elsewhere.
Naturally, there is also considerable interest in outcomes of substance abuse treatment before versus after Medicaid managed care. A Colorado study found that youth with alcohol problems had reduced contact with juvenile justice authorities after the change from fee for service to capitated Medicaid behavioral healthcare.25 The Maryland Medicaid study showed that substance abuse treatment outcomes were either no different or improved following implementation of managed care.16 Again, it remains to be seen if other states will have similar experiences.
As was mentioned, it is unlikely that Medicaid programs will return to fee for service anytime soon. Indeed, the majority of Medicaid clients are enrolled in managed care systems of one sort or another.10 Of more interest to state decision makers, then, is the relative performance of different types of managed care programs. For example, one can wonder if clients enrolled in for-profit systems have different outcomes than their counterparts in not-for-profit programs. Outcomes of interest include completion of treatment goals, abstinence at discharge, and readmission.16 Of course, readmission is not unexpected given the recurring nature of substance abuse.
Oregon’s experience with Medicaid managed care over the last decade provides opportunities to address these issues. The purpose of this study was to examine (a) the change (if any) in treatment outcomes from before to after Medicaid managed care for substance abuse services, (b) the impact (if any) of various organization and financing arrangements (such as for-profit versus not-for-profit providers) on outcomes, and (c) the relationship between length of Medicaid enrollment and treatment outcomes in the fee for service and managed care eras, respectively. This project adds to the understanding of these issues by examining several different types of Medicaid managed behavioral healthcare organizations and by investigating relationships between state Medicaid characteristics (such as enrollment duration) and treatment outcomes.
Oregon Health Plan
In the early 1990s, the Oregon legislature initiated a demonstration project to expand Medicaid coverage while controlling the rising public cost of healthcare through a series of bills that became known as the Oregon Health Plan. This initiative incorporated important innovations such as expanded eligibility and integration of chemical dependency services with physical healthcare.26–31 The (then) Health Care Financing Administration granted Oregon a 5-year Medicaid waiver, which enabled the state to expand coverage to all adults and their dependents whose income fell below the federal poverty limit.31 This section 1115 waiver took effect in February 1994, more than doubling the Medicaid-eligible population. These newly entitled individuals came to be known as the “expansion” eligibility category (in contradistinction to traditional Medicaid categories such as clients of the Aid to Families with Dependent Children/Temporary Assistance to Needy Families [AFDC/TANF] program). The state increased the cigarette tax to help finance this new program.
All Medicaid clients were required to enroll in one of the state-approved prepaid health plans with a contract to serve the county in which they resided. The state’s intent was to use capitated financing as a mechanism to predict and control Medicaid expenditures. By the third quarter of 1994, more than 80% of the Medicaid-eligible population had enrolled in prepaid health plans.
In May 1995, the state added a capitated chemical dependency benefit to improve the integration of substance abuse treatment with physical healthcare. This benefit covered outpatient treatment services, including regular outpatient, intensive outpatient, and methadone maintenance. The new program placed responsibility for Medicaid chemical dependency treatment services on prepaid health plans and replaced the previous fee for service and block grant system.32 The health plans received increased capitation rates to provide substance abuse treatment for their Medicaid enrollees. This development markedly altered the organization and financing of these services.33 Previously, little or no connection existed between the public sector substance abuse treatment system and the larger medical-surgical healthcare sector.34
There was considerable variation in the organizational and financial arrangements governing the health plans.13,34 For example, some plans were for-profit whereas others were not-for-profit. Some plans were integrated systems that offered both medical-surgical and behavioral health services while other organizations employed “carve-out” arrangements to deliver mental health and/or substance abuse treatments.
The health plans themselves adopted assorted organizational and financial arrangements for the provision of chemical dependency treatment to their Medicaid enrollees.13,34 For example, some health plans reimbursed providers on a modified fee for service basis whereas others employed subcapitation or case rate payment methodologies. Still other plans relied on preexisting salaried chemical dependency treatment clinicians who were integrated into the overall healthcare system.
Detailed descriptions of the health plans have been provided elsewhere.13 Briefly, this project focused on the 6 prepaid health plans (ranging in size from roughly 8000 to about 50,000 Medicaid clients) that enrolled the majority of Medicaid clients. One plan was for-profit and the others were not-for-profit. Two plans had fully integrated substance abuse treatment services whereas the others had carve-out arrangements. Provider reimbursement mechanisms included modified fee for service (3 plans), subcapitation (1 plan), and case-rate systems (2 plans). Three plans required prior authorization and reauthorization whereas the others did not. All plans offered Medicaid clients the same “package” of substance abuse treatment services including assessment, detoxification, outpatient, intensive outpatient, and methadone maintenance. Residential treatment (rarely used in Oregon) was a separate benefit funded by the state substance abuse agency.
Medicaid member characteristics of the health plans have been described previously.13 There were variations across the plans in demographics of Medicaid enrollees and in characteristics of Medicaid clients seeking substance abuse treatment services.13 For example, one plan had high representation of minority group Medicaid members (about 33% vs 16% overall). Similarly, this plan also had high representation of minorities in its Medicaid substance abuse treatment program. These demographic and clinical differences among health plans are addressed in the data analysis.
These variations in organizational and financing arrangements provided opportunities for before (1994) versus after (subsequent to 1995) comparison. Individuals in the “before” condition were eligible for capitated medical-surgical care from their health plans while chemical dependency treatment remained fee for service. Conversely, people in the “after” (managed care) condition were entitled to both medical-surgical care and substance abuse treatment under capitated arrangements.
Given this “natural experiment,” the present project compares treatment outcomes for Medicaid outpatients before versus after this substantial change in organization and financing of services. The project also contrasts outcomes for Medicaid clients enrolled in for-profit systems with those in not-for-profit health plans. In addition, the study compares treatment outcomes for Medicaid clients in health plans that “carved out” drug abuse treatment with those in programs that integrated chemical dependency services with physical healthcare. Importantly, the project also examines the impact of state Medicaid policies affecting coverage duration on treatment outcomes. As noted, this study provides useful information for state decision makers since these topics have had little (if any) coverage in the current literature.
Methods
This project focused on Medicaid clients who entered regular or intensive outpatient drug-free (non-methadone) chemical dependency treatment during the study period. These individuals comprised the vast majority of Medicaid substance abuse treatment patients during those years. In accordance with state requirements, treatment programs emphasized abstinence as a goal. Therefore, dependent variables of interest included retention in treatment for at least 90 days,23 completion of treatment goals, abstinence at discharge, and readmission. Of course, given the chronic, relapsing nature of chemical dependency, readmission is not unexpected. Conceptually, treatment retention and completion can be regarded as “quality of care” measures, abstinence is an outcome indicator, and readmission reflects both treatment outcomes and access to care.
Data
Information was obtained from the Oregon Client Process Monitoring System (CPMS), which records admissions to, and discharges from, all publicly funded chemical dependency treatment programs in the State of Oregon. The system provides detailed demographic and clinical information at intake. CPMS records were merged with Medicaid eligibility and enrollment files from Oregon’s Office of Medical Assistance Programs to determine eligibility category and enrollment in a prepaid health plan. Only records for adults aged 18–64 years, enrolled in a prepaid health plan, provided outpatient (or intensive outpatient) treatment, and with complete data for all the potential predictors and at least 1 of the 4 dependent measures (defined below) were used to predict substance abuse treatment outcomes.
Outcome measures
The outcomes included in this study were dichotomous variables describing the status of the patient after receiving treatment: retention, completion, abstinence at discharge, or readmission to treatment. A patient was defined to be retained if the individual remained in the index treatment episode for at least 90 days. A patient completed treatment if the drug abuse counselor indicated that the person achieved at least two thirds of the goals in the treatment plan. A patient abstained if the individual reported no use of the primary drug of choice in the month preceding discharge. A patient was readmitted to treatment if the person reentered treatment during the 12 months following discharge from the index episode, not counting any transfers within the first 21 days following discharge from the index episode.
Independent measures
Continuous variables used as possible predictors of substance abuse treatment outcomes were age, proportion of the year following intake the patient was Medicaid eligible, and a severity index described in the next section. Several dichotomous variables (coded 0 or 1) were also used as predictors. For these dichotomous variables, the subjects in the group coded as “0” were defined to be the “reference” category. Dichotomous predictors included gender (with female as the reference category); ethnicity (with nonwhite as the reference category); participation in publicly funded treatment during the 24 months prior to intake (with no as the reference category); and before versus after (with treatment before managed care went into effect as the reference category). Category of Medicaid eligibility was also represented as a dichotomous variable with the AFDC/TANF as the reference group. The AFDC/TANF population and the expansion population were the only groups considered since other categories either were small or were not enrolled in prepaid plans until after 1994. Community type was represented by 2 dichotomous variables: urban and town, both referenced to rural. Health plans were represented by 6 indicator variables (1 for each of the largest plans) with the reference group all the remaining plans combined.
Severity index
The study team developed a severity index, using the American Society for Addiction Medicine (ASAM) Patient Placement Criteria35 to guide the choice of candidate variables from the CPMS database. The composite measure included frequency of alcohol use at intake, number of years of alcohol use, frequency of illicit drug use at intake, number of years of illicit drug use, use of particularly addictive drugs (eg, heroin or cocaine), intravenous drug use, employment status, inability to work because of physical or psychological reasons, lack of an income source, and referral from another treatment agency. The index was validated against Addition Severity Index (ASI)36 composite scores (generated by research interviewers) and ASAM Patient Placement Criteria clinical recommendations (from treatment staff) for a sample of 499 adult Medicaid clients seeking services in publicly funded substance abuse treatment programs in Oregon or Washington state during the late 1990s.37 The Pearson correlation between the severity index and the ASAM Patient Placement Criteria recommendation was 0.395. Correlations between the severity index and the Addiction Severity Index measures were also significant: ASI total composite (0.574), ASI alcohol composite (0.135), ASI drug composite (0.397), ASI psychiatric composite (0.338), ASI medical composite (0.315), ASI legal composite (0.181), and ASI employment composite (0.322). This methodology is very similar to the work reported by Caspi et al.38 The severity index was used to adjust for case mix differences such as preferred drug of abuse and polysubstance use.
Regression analyses
Several methods were employed in the analyses. Bivariate analyses, such as chi-square tests, were used to compare the before versus after (managed care) subjects. Simple logistic regression was used to adjust the dependent measures for case mix differences in the before versus after (managed care) eras. Simple logistic regression was performed with the full sample sizes (14,285 to 16,102) to identify variables predicting outcomes. The simple logistic regression analyses used forward stepwise (loading) to examine all the independent measures as well as interaction terms.
Recognizing that subjects were not assigned at random to the before versus after (managed care) eras, propensity score methods39,40 were employed in an attempt to match fee for service with managed care patients on pertinent characteristics. The propensity score approach divided the total sample into strata on the basis of factors that distinguished before versus after (managed care) subjects. The stratification served as a matching mechanism.
The propensity score was computed for each subject using logistic regression to estimate the probability of being in the before group.39 Age, gender, ethnicity, proportion of the year following intake a patient was Medicaid eligible, severity index, prior treatment, Medicaid eligibility category, location in a town, and location in an urban area were included. The probability of being in the before group was then calculated from a logistic regression model that included only significant predictors. The predicted probabilities for the before patients were divided into deciles. Each decile contained about 175 subjects. The after (managed care) group was also divided into deciles on the basis of the (counterfactual) predicted probability of being a fee for service subject. Then 350 after (managed care) patients were selected at random from each decile. It should be noted that this procedure was, in effect, probability matching. Actual matching on many client characteristics would have yielded too few cases to be representative. Therefore, though imperfect at best, matching probabilities was a viable alternative.
This process yielded a sample of 5251 patients. The stratified sample was then analyzed using (a) simple logistic regression (with the strata entered as dummy variables and the first stratum as the reference group) as well as (b) approaches designed for stratified logistic regression.41 All independent measures were included as possible predictors in analyses using the stratified sample. This approach is very similar to analyses used in the Maryland Medicaid project.16
An important consideration in the analysis is possible dependency between subjects (ie, lack of independence). In this project, there may have been dependency between patients enrolled in the same health plan.16 Methodology developed originally by DerSimmonian and Laird addresses this lack of independence.42,43 The technique (often employed in meta-analysis) involves use of fixed effects and random effects models that focus attention on the aggregation unit (here, the health plan). The methodology allows one to examine possible heterogeneity among health plans while recognizing that treatment outcomes for patients (nested within health plans) may not be statistically independent. Before the outcome measures were compared via the fixed effects and random effects models, residuals were computed so that patient characteristics (ie, case mix differences) were taken into account. To compute residuals, a logistic regression equation was estimated for each outcome measure. Predictors considered for the logistic models were all the independent measures (except for before vs after status) plus indicators for the several health plans. The best fitting logistic regression model (for each outcome measure) was then used to compute for each subject the estimated probability of success (on that outcome measure). This estimated success probability was then subtracted from the observed value of the outcome measure to form a residual. In turn, the residuals were entered into the fixed effects and random effects models.43 Heterogeneity of treatment outcomes among health plans (taking into account nesting of patients within health plans) was measured with the Q statistic.42 This approach is similar to methods used in the Maryland Medicaid project.16
Multiple statistical tests
Since numerous statistical tests were performed, consideration was given to protecting against chance associations by, for example, the Bonferoni method. However, a major hypothesis addressed in this project is that managed care may be detrimental to Medicaid clients with substance abuse problems. In this study, detrimental impact would be shown by a negative coefficient pertaining to the after managed care indicator in the regression models. To avoid inappropriately overlooking such a finding, the results present regression coefficients that are statistically significant at the P < .05 level.
Results
Table 1 shows patient demographic and clinical measures. In the before group, there were more women than men but there were even numbers of men and women in the after (managed care) group. Patients in the managed care group were slightly older than fee for service clients. Subjects in fee for service were more likely to be from urban areas than were the managed care patients. Subjects in the managed care group were Medicaid eligible for less time than fee for service clients. As expected, there were substantially more expansion clients in the managed care group.
Table 1.
Demographics and outcomes*
| 1994 (before managed care) | 1996–1997 (after managed care) | Significance test | |
|---|---|---|---|
| N | 1751 | 14813 | |
| Female | 59.6% | 49.6% | 0.000 |
| Age | 32.3 (7.9) | 33.2 (0.84) | 0.000 |
| White | 80.1% | 83.4% | 0.000 |
| Location | |||
| Rural | 5.8% | 9.3% | 0.000 |
| Town | 20.3% | 28.9% | 0.000 |
| Urban | 73.9% | 61.9% | |
| Proportion of year after intake Medicaid eligible | 0.835 (0.241) | 0.760 (0.278) | 0.000 |
| Medicaid eligibility group | |||
| AFDC/TANF | 43.1% | 27.1% | 0.000 |
| Expansion | 56.9% | 72.9% | |
| Severity index | 0.404 (0.166) | 0.385 (0.170) | 0.000 |
| Prior treatment | 46.0% | 49.5% | 0.005 |
| Primary drug | 0.005 | ||
| Alcohol | 49.6% | 47.8% | |
| Amphetamine | 22.1% | 23.9% | |
| Marijuana | 10.7% | 13.0% | |
| Cocaine | 10.2% | 7.2% | |
| Opiates | 6.4% | 7.5% | |
| Other | 1.0% | 0.6% | |
| Polysubstance use | 67.0% | 66.0% | 0.112 |
| % Retained | 41.9% (718/1714) | 40.4% (5724/14158) | 0.245 |
| % Completed | 27.4% (474/1731) | 31.6% (4545/14371) | 0.000 |
| % Abstain | 42.1% (704/1673) | 47.1% (6694/14218) | 0.000 |
| % Readmitted | 34.1% (562/1646) | 37.9% (4793/12639) | 0.003 |
AFDC indicates Aid to Families with Dependent Children; TANF, Temporary Assistance to Needy Families.
Clinically, alcohol was the most popular drug of first choice in fee for service and managed care groups with amphetamines being the second most popular for both groups. Some two thirds of both groups were described as polysubstance abusers by their counselors. Managed care clients had lower (less severe) severity index scores than fee for service patients. On the other hand, the after (managed care) subjects were more likely (49.5% vs 46.0%) to have had prior treatment than the fee for service patients. Given the large sample sizes, almost all of these results are highly statistically significant. However, the magnitudes of many differences (eg, in the severity measure) are small and unlikely to be detected clinically.
Table 1 also describes the (unadjusted) outcomes. There was no difference in the percentage of patients retained in treatment for 90 days from before to after managed care. More patients completed treatment goals in the after (managed care) group. More subjects abstained from drug use in the 30 days prior to discharge in the managed care group than did the fee for service patients. More patients were readmitted to treatment in the managed care era than in the fee for service period.
These outcome measures were then analyzed at length. Here the overall regression results are described briefly focusing on policy-relevant predictors such as before versus after managed care and duration of Medicaid eligibility. Detailed descriptions of results from the regression analyses are in an appendix (available upon request).
Table 2 summarizes results from the several regression analyses. Here the simple logistic regression analyses (on the left-hand side of the table) not only are the most straight-forward but also make the fewest adjustments for differences between the before and after groups. Conversely, the stratified logistic regression analyses (on the right-hand side of the table) use the most conservative regression approaches to address differences between groups. The middle columns show simple logistic regression results for the stratified samples and represent a middle of the road approach to adjusting for baseline differences between groups. Consequently, there are more predictors shown to be statistically significant (at P < .05) in the left-hand columns of the table than in the middle columns while the right-hand columns display the fewest statistically significant predictors.
Table 2.
Regression analyses
|
Simple logistic regressions predicting substance abuse
treatment outcomes |
Simple logistic regressions predicting substance abuse
treatment outcomes using a stratified sample |
Stratified logistic regressions predicting substance abuse
treatment outcomes using a stratified sample |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | Lower CI | Upper CI | Odds ratio | Lower CI | Upper CI | Odds ratio | Lower CI | Upper CI | |
| Retain—Client remained in treatment for at least 90 days | |||||||||
| Age | 1.012 | 1.008 | 1.016 | 1.012 | 1.005 | 1.019 | 1.007 | 1.001 | 1.012 |
| Expansion | 1.287 | 1.193 | 1.388 | 1.195 | 1.054 | 1.354 | |||
| Town | 1.194 | 1.111 | 1.283 | ||||||
| Urban | 0.810 | 0.710 | 0.924 | ||||||
| Months Medicaid eligible following intake | 3.832 | 2.480 | 5.921 | 2.981 | 2.301 | 3.862 | 2.151 | 1.698 | 2.726 |
| Severity index | 0.125 | 0.103 | 0.153 | 0.213 | 0.149 | 0.304 | 0.426 | 0.321 | 0.565 |
| After | 1.356 | 0.912 | 2.017 | ||||||
| After × Months Medicaid eligible following intake | 0.619 | 0.394 | 0.974 | ||||||
| Complete—Counselor indicated client completed treatment plan | |||||||||
| Age | 1.018 | 1.013 | 1.022 | 1.021 | 1.014 | 1.029 | 1.012 | 1.005 | 1.019 |
| White | 1.238 | 1.124 | 1.363 | 1.403 | 1.186 | 1.661 | 1.247 | 1.075 | 1.448 |
| Expansion | 1.066 | 0.854 | 1.332 | ||||||
| Urban | 0.871 | 0.810 | 0.935 | ||||||
| Months Medicaid eligible following intake | 3.596 | 2.162 | 5.979 | 2.144 | 1.631 | 2.819 | 1.950 | 1.488 | 2.554 |
| Severity index | 0.095 | 0.077 | 0.117 | 0.158 | 0.108 | 0.232 | 0.305 | 0.219 | 0.425 |
| After | 1.767 | 1.065 | 2.932 | 1.165 | 1.021 | 1.330 | 1.118 | 1.002 | 1.248 |
| Health Plan 1 | 0.842 | 0.755 | 0.941 | 0.797 | 0.660 | 0.962 | 0.857 | 0.730 | 1.007 |
| Health Plan 2 | 1.113 | 1.002 | 1.236 | ||||||
| After × Expansion | 1.335 | 1.053 | 1.693 | ||||||
| After × Months Medicaid eligible following intake | 0.484 | 0.286 | 0.819 | ||||||
| Stratum 2 | 0.747 | 0.600 | 0.930 | ||||||
| Abstain—Abstain from primary drug in the month preceding discharge | |||||||||
| Age | 1.006 | 1.002 | 1.010 | 1.006 | 1.002 | 1.010 | |||
| White | 1.253 | 1.151 | 1.365 | 1.274 | 1.099 | 1.477 | 1.137 | 1.013 | 1.276 |
| Urban | 0.867 | 0.812 | 0.926 | 0.827 | 0.726 | 0.942 | |||
| Expansion | 1.252 | 1.163 | 1.347 | 1.274 | 1.132 | 1.433 | |||
| Months Medicaid eligible following intake | 2.536 | 1.652 | 3.895 | 1.678 | 1.312 | 2.145 | 1.496 | 1.209 | 1.851 |
| Severity index | 0.369 | 0.306 | 0.446 | 0.475 | 0.336 | 0.672 | 0.708 | 0.543 | 0.923 |
| After | 2.302 | 1.552 | 3.414 | 1.200 | 1.065 | 1.352 | 1.107 | 1.012 | 1.210 |
| Health Plan 3 | 1.116 | 0.902 | 1.380 | 1.116 | 0.902 | 1.380 | |||
| After × Months Medicaid eligible following intake | 0.493 | 0.316 | 0.770 | 0.493 | 0.316 | 0.770 | |||
| After × Health Plan 3 | 0.752 | 0.602 | 0.941 | 0.752 | 0.602 | 0.941 | |||
| Readmit—client readmitted during 12 months following discharge | |||||||||
| Age | 0.991 | 0.986 | 0.995 | 0.991 | 0.983 | 0.999 | |||
| White | 0.815 | 0.698 | 0.952 | ||||||
| Town | 0.813 | 0.604 | 1.094 | ||||||
| Urban | 1.191 | 1.047 | 1.356 | ||||||
| Expansion | 1.233 | 1.076 | 1.414 | 1.294 | 1.092 | 1.534 | |||
| Months Medicaid eligible following intake | 3.254 | 2.842 | 3.725 | 2.817 | 2.124 | 3.735 | 1.615 | 1.227 | 2.126 |
| Prior treatment | 1.674 | 1.558 | 1.799 | 1.664 | 1.469 | 1.885 | 1.434 | 1.289 | 1.596 |
| Severity index | 5.101 | 4.110 | 6.330 | 5.243 | 3.555 | 7.733 | 2.204 | 1.570 | 3.093 |
| After | 1.282 | 1.128 | 1.457 | 1.282 | 1.123 | 1.456 | 1.142 | 1.033 | 1.262 |
| Health Plan 6 | 1.922 | 1.164 | 3.175 | ||||||
| After × Town | 1.395 | 1.050 | 1.854 | ||||||
| After × Health Plan 6 | 0.472 | 0.279 | 0.798 | ||||||
| Stratum 9 | 0.687 | 0.549 | 0.860 | ||||||
Not surprisingly, the severity index was a powerful (negative) predictor of all outcomes in all the regression approaches. As expected, prior treatment predicted readmission in all statistical models. Demographics such as age and race predicted some outcomes in certain analyses as did location (urban, town, or rural). Medicaid eligibility category also predicted a few outcomes in some of the regression models. Some of the health plan indicator variables (or the interactions of health plan indicators with other measures) were statistically significant predictors in some regressions.
The after managed care indicator was a statistically significant (P < .05) predictor of treatment completion, abstinence at discharge, and readmission (in all regression models). After managed care status per se did not predict retention in care but there was a statistically significant interaction between the after indicator and duration of Medicaid eligibility as will be described shortly.
Medicaid eligibility was a powerful (positive) predictor of all outcomes in all regression models. For example, each month of Medicaid eligibility increased the client’s chances of retention by 7%, completion by 6%, abstinence at discharge by 3%, and readmission by 4%. In some of the less conservative regression models, there was a negative interaction between the before versus after managed care indicator and the months of Medicaid eligibility predictor. The implication here is that Medicaid eligibility duration was not quite so significant in the managed care era as in the fee for service system. Figure 1 illustrates this point with regard to retention in treatment. The figure shows that one’s chances of retention in treatment (for 90 days) increased with the duration of Medicaid enrollment. The fitted lines show that the slopes of the graphs connecting treatment retention with Medicaid enrollment were different in fee for service versus managed care. Namely, the slope during the fee for service era was steeper (implying more impact of Medicaid duration) than under the managed care system.
Figure 1.
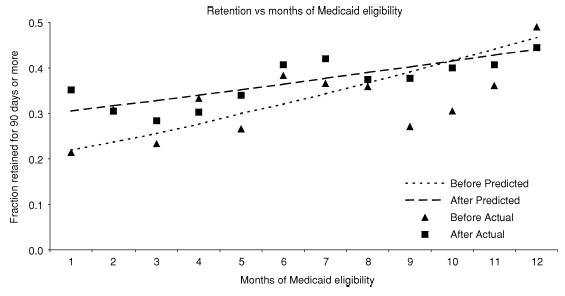
Fraction retained in treatment (for at least 90 days) versus months of Medicaid eligibility.
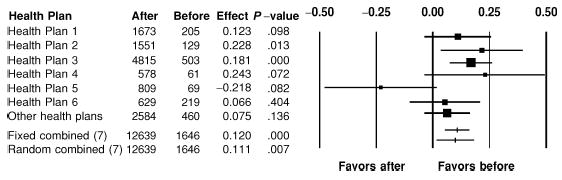
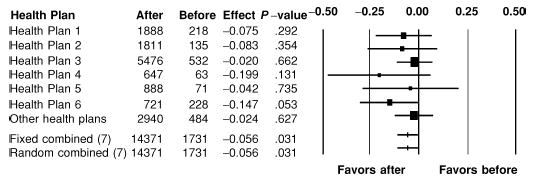
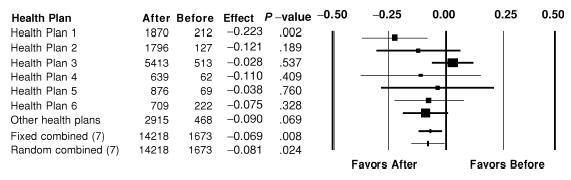
The regression analyses provide an important insight into factors that apparently had impact on the outcome measures. However, as noted, there may be statistical dependency among clients enrolled in a given health plan. Consequently, fixed effects and random effects models were also constructed for each outcome measure as shown in Figures 2 through 5. These analyses showed that the before versus after managed care indicator was not statistically significant for prediction of treatment retention nor was there heterogeneity among health plans with regard to retention (Fig 2). Treatment completion was higher in the after managed care group although the statistical significance was marginal (P = .03). Again, there was no evidence for heterogeneity among health plans with respect to treatment completion (Fig 3). Regarding abstinence at discharge, Figure 4 shows that there was evidence for improvement under managed care (at P = .02) and there was a trend toward heterogeneity among the health plans on this measure (P = .16). The heterogeneity appears due chiefly to Health Plan 3 (a large, not-for-profit, carve-out system). Finally, Figure 5 suggests that there was heterogeneity among health plans with regard to readmission (P = .05) most likely due to Health Plan 5 (not-for-profit). The random effects model depicted in Figure 5 shows that the chances of readmission increased markedly in the after managed care era (P = .007) except for Health Plan 5 in which readmission rates apparently declined.
Figure 2.
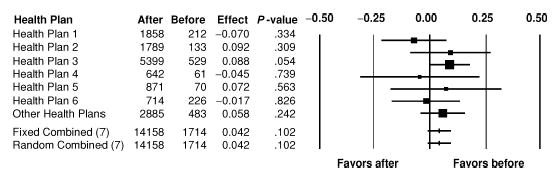
Treatment retention (for at least 90 days). Shown are the effect sizes (and 95% confidence intervals) for the before minus after differences in treatment retention (based on residuals reflecting adjustments for subjects’ demographic and clinical characteristics as well as health plan main effects). Marker size reflects numbers of health plan patients.
Figure 5.
Readmission to substance abuse treatment within 12 months of discharge from index episode. Shown are the effect sizes (and 95% confidence intervals) for the after minus before differences in readmission (based on residuals reflecting adjustments for subjects’ demographic and clinical characteristics as well as health plan main effects). Marker size reflects numbers of health plan patients.
Figure 3.
Completion of treatment goals. Shown are the effect sizes (and 95% confidence intervals) for the before minus after differences in completion of at least two thirds of treatment goals (based on residuals reflecting adjustments for subjects’ demographic and clinical characteristics as well as health plan main effects). Marker size reflects numbers of health plan patients.
Figure 4.
Abstinence at discharge. Shown are the effect sizes (and 95% confidence intervals) for the before minus after differences in counselor reports of abstinence at discharge (based on residuals reflecting adjustments for subjects’ demographic and clinical characteristics as well as health plan main effects). Marker size reflects numbers of health plan patients.
Discussion
Results from this study need to be interpreted in light of its limitations. Of course, the project was not a randomized trial. There may well have been many (both measured and unmeasured) differences between subjects in the fee for service era and their counterparts in managed care. Consequently, the project involved numerous analytic strategies intended to adjust for subject characteristics.
As in other Medicaid projects,14–16 patients were not interviewed and data were obtained only from automated record systems. Moreover, measures of drug use (or abstinence) were based on self-report. On the other hand, the present findings are consistent with results from a Medicaid substance abuse patient interview project37 that compared outcomes in Oregon (managed care) versus those in Washington state (which remained fee for service). Importantly, the present results are also consistent with findings from a patient interview study examining Oregon Medicaid substance abuse treatment services in the fee for service and managed care eras.44
Another limitation is that there may well have been secular trends in addition to the conversion of Oregon Medicaid chemical dependency treatment from fee for service to managed care. The Maryland Medicaid project16 addressed this issue by also comparing non-Medicaid subjects in the 2 eras and found no impact on the conclusions. Similarly, the Oregon client interview project also involved non-Medicaid substance abuse treatment patients.44
Also, this project examined only 1 state and caution should be exercised before generalizing outside of Oregon. However, it is noteworthy that the Oregon system has many similarities to the Maryland Medicaid program.16 Moreover, these and earlier13 findings from Oregon are similar to results reported from other states.14–16
It should be noted too that this study focused on client outcomes. Financial issues were not addressed in this project but are being examined in other studies.
Given these limitations, it is noteworthy that this study found no evidence for detrimental impact of managed care on treatment outcomes for Medicaid clients with substance abuse problems. Retention in treatment (which can be considered a “quality of care” measure) was unchanged from before to after the implementation of managed care. In other words, there was no evidence of “short-changing.” Again, this finding is very similar to results from Maryland’s Medicaid substance abuse treatment system.16
Similarly, treatment completion (which can also be regarded as a “quality of care” indicator) was, if anything, more likely after managed care than under fee for service. Indeed, the most conservative data analysis (the random effects models) suggested that treatment completion rates might have improved slightly under managed care. However, it has been pointed out45,46 that confidence intervals generated by the usual random effects models42,43 may be too small. Therefore, a conservative interpretation is to say there is no evidence for decline in treatment completion rates following conversion to Medicaid managed care.
For both treatment retention and treatment completion, there was no variation among health plans. The implication here is that organizational and financing arrangements (such as the health plans’ for-profit versus not-for-profit status) had little or no impact on quality of care.
On average, abstinence rates at discharge were not different (and might have been a bit more favorable) following the change from fee for service to capitation. However, the random effects modeling suggested that there was very slight health plan variation in that abstinent rates appeared to have deteriorated in a large, not-for-profit program after managed care. On the other hand, health plan variation was not detected in the stratified logistic regression analysis.
Readmission rates did increase following the implementation of Medicaid managed care for substance abuse treatment (although readmission declined notably for 1 not-for-profit health plan). Interpretation of readmission data is challenging since this measure involves both access to treatment and outcomes thereof.47 Presumably, readmission reflects relapse to use, which is not unexpected for people with substance abuse problems. However, readmission also reflects access to services. That is, in the absence of funding for services, readmission rates would presumably be low. As it happens, earlier work in Oregon13 showed that access to substance abuse treatment services for Medicaid clients increased markedly when fee for service was replaced by capitation. This increase in access presumably applied to previously treated individuals as well as to persons entering their first episode of chemical dependency care. Of course, readmission also suggests that the index treatment episode was less than successful. However, Humphreys and Weingardt suggest that (at least for veterans hospital programs) there is little correlation between readmission rates and other measures of client outcome.47 In any event, it is worth examining the contribution of both these factors to the change in readmission rates from before to after managed care.
Overall (unadjusted) readmission rates in this study rose by roughly 10%. However, the (adjusted) odds ratio for readmission suggested that the rates rose by about 30%. These estimates of readmission rate increases should be compared with the 30% rise in access to substance abuse treatment found in previous studies of Oregon’s Medicaid population.13 The implication here is that increased access may explain at least some of the apparent rise in readmission rates following the conversion to managed care. While readmission rates rose in several health plans from before to after managed care, 1 not-for-profit program in Oregon had a notable decrease. In the Maryland Medicaid study, there was no change in readmission rates from before to after managed care.16
In contrast to previous Oregon research that showed clear relationships between health plan characteristics and changes in rates of access to substance abuse treatment,13 there were no obvious connections between organizational and financing indicators and changes in outcome measures. Specifically, it was not evident that the for-profit versus not-for-profit distinction had a connection with outcomes nor did the integrated versus carve-out measure. Qualitative work (including interviews with payers and providers) suggested that health plans participating in the Oregon program were chiefly interested in quality assurance and less concerned about utilization management. Moreover, nearly all the participating health plans developed specialized behavioral health management programs (carve-out systems) designed to facilitate provision of chemical dependency treatment services to their Medicaid enrollees.34 In addition, the most common mechanism for reimbursement from health plans to providers was modified fee for service,13 which was not a dramatic change from the previous financing arrangements. It is conceivable that these factors may have minimized impact of capitation on frontline clinicians.
An important finding of the present project was the strong relationship between Medicaid eligibility duration and treatment outcomes. Months of eligibility for Medicaid powerfully predicted all the outcome measures in all the statistical models. For example, each month of Medicaid eligibility increased a client’s chances of abstinence at discharge by 3%. These results are consistent with recent work on Oregon’s methadone program for Medicaid clients.48 Studies on Utah Medicaid clients with schizophrenia showed a powerful connection between continuity of Medicaid eligibility and use of inpatient psychiatric services.49 Interestingly, in some cases in the present study, there was an interaction between months of Medicaid eligibility and before versus after managed care. These interactions suggested that short duration of Medicaid enrollment was more detrimental to treatment outcomes in the fee for service era than after managed care had been implemented.
Implications for Behavioral Health
In summary, there was little or no change in outcomes for substance abuse treatment patients following Oregon’s conversion of its Medicaid program from fee for service to managed care nor were there differences in outcomes for enrollees in various types of managed care programs. This finding is important since capitated Medicaid behavioral healthcare has numerous administrative advantages for state agencies not the least of which is improved budgetary predictability.30 Therefore, state substance abuse and Medicaid agencies would be well advised to shift attention away from the details of managed care organizational and financial arrangements and to focus instead on ways to improve quality of care.
In particular, duration of Medicaid eligibility was strongly related to successful treatment. Of course, it could be that relapse to (or worsening of) substance abuse precipitated loss of Medicaid coverage. On the other hand, it is also possible that abstinence led to increased wages and consequent loss of Medicaid eligibility. In addition, burdensome state requirements for recertifying Medicaid eligibility could have shortened duration of clients’ healthcare coverage. These issues are topics for ongoing research. In any event, the present results have important implications as states struggle with rising numbers of Medicaid clients and declining revenues.50 States that attempt to deal with these concerns by making it more difficult for Medicaid clients to maintain eligibility may well find that outcomes worsen for substance abuse treatment patients.
Supplementary Material
Acknowledgments
This research was supported in part by National Institute on Drug Abuse research grant R01 DA11970 (Dr McFarland), Substance Abuse and Mental Health Services Administration Cooperative Agreement 1 UR7 TI 1129401 (Dr Gabriel), and National Institute on Alcohol Abuse and Alcoholism grant K02 AA00281 (Dr McFarland).
Contributor Information
Bentson H. McFarland, Departments of Psychiatry and Public Health & Preventive Medicine, Oregon Health & Science University, Portland, Ore..
Dennis D. Deck, RMC Research Corporation, Portland, Ore..
Lynn E. McCamant, Department of Psychiatry, Oregon Health & Science University, Portland, Ore..
Roy M. Gabriel, RMC Research Corporation, Portland, Ore..
Douglas A. Bigelow, Departments of Psychiatry and Public Health & Preventive Medicine, Oregon Health & Science University, Portland, Ore..
References
- 1.Coffey R, Mark T, King E, et al. Rockville, Md: Substance Abuse & Mental Health Services Administration; 2000. National Estimates of Expenditures for Mental Health and Substance Abuse Treatment, 1997. DHHS Publication No. SMA 00-3499. [Google Scholar]
- 2.McKusick D, Mark TL, King E, et al. Spending for mental health and substance abuse, 1996. Health Affairs (Millwood) 1998;17:147–157. doi: 10.1377/hlthaff.17.5.147. [DOI] [PubMed] [Google Scholar]
- 3.Mark TL, Buck JA, Dilonardo JD, Coffey RM, Chalk M. Medicaid expenditures on behavioral health care. Psychiatric Services. 2003;54:188–194. doi: 10.1176/appi.ps.54.2.188. [DOI] [PubMed] [Google Scholar]
- 4.McFarland B. Overview of Medicaid managed behavioral health care. What the Oregon Health Plan Can Teach Us About Managed Mental Health Care. New Directions for Mental Health Services. In: Goetz R, McFarland B, Ross K, editors. Vol. 85. San Francisco: Jossey-Bass; 2000. pp. 17–22. [DOI] [PubMed] [Google Scholar]
- 5.McCarty D, Dilonardo J, Argerious M. State substance abuse and mental health managed care evaluation program. Journal of Behavioral Health Services and Research. 2003;30:7–17. doi: 10.1007/BF02287809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang CF, Kiser LJ, Bailey LE, et al. Tennessee’s failed managed care program for mental health and substance abuse services. JAMA. 1998;279:864–869. doi: 10.1001/jama.279.11.864. [DOI] [PubMed] [Google Scholar]
- 7.Mechanic D. 4th ed. Boston, Mass: Allyn & Bacon; 1999. Mental Health and Social Policy: The Emergence of Managed Care; p. 165. [Google Scholar]
- 8.Galanter M, Keller DS, Dermatis H, et al. The impact of managed care on substance abuse treatment: a problem in need of solution. A report of the American Society of Addiction Medicine. Recent Developments in Alcoholism. 2001;15:419–436. [PubMed] [Google Scholar]
- 9.Draper DA, Gold MR. Provider risk sharing in Medicaid managed care plans. Health Affairs. 2003;22(3):159–167. doi: 10.1377/hlthaff.22.3.159. [DOI] [PubMed] [Google Scholar]
- 10.Hurley RE, Somers SA. Medicaid and managed care: a lasting relationship? Health Affairs. 2003;22(1):77–88. doi: 10.1377/hlthaff.22.1.77. [DOI] [PubMed] [Google Scholar]
- 11.Draper DA, Hurley RE, Short AC. Medicaid managed care: the last bastion of the HMO? Health Affairs. 2004;23(2):155–167. doi: 10.1377/hlthaff.23.2.155. [DOI] [PubMed] [Google Scholar]
- 12.Alexander JA, Harris-Lemak C, Campbell CI, et al. Changes in managed care activity in outpatient substance abuse treatment organizations, 1995–2000. Journal of Behavioral Health Services & Research. 2003;30:369–381. doi: 10.1007/BF02287425. [DOI] [PubMed] [Google Scholar]
- 13.Deck DD, McFarland BH, Titus JM, Laws KE, Gabriel RM. Access to substance abuse treatment services under the Oregon Health Plan. JAMA. 2000;284:2093–2099. doi: 10.1001/jama.284.16.2093. [DOI] [PubMed] [Google Scholar]
- 14.McCarty D, Argeriou M. The Iowa managed substance abuse care plan: access, utilization, and expenditures for Medicaid recipients. Journal of Behavioral Health Services and Research. 2003;30:18–25. doi: 10.1007/BF02287810. [DOI] [PubMed] [Google Scholar]
- 15.Ettner SL, Argeriou M, McCarty D, et al. How did the introduction of managed care for the uninsured in Iowa affect the use of substance abuse services. Journal of Behavioral Health Services and Research. 2003;30:26–40. doi: 10.1007/BF02287811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ettner SL, Denmead G, Dilonardo J, et al. The impact of managed care on the substance abuse treatment patterns and outcomes of Medicaid beneficiaries: Maryland’s HealthChoice program. Journal of Behavioral Health Services and Research. 2003;30:41–62. doi: 10.1007/BF02287812. [DOI] [PubMed] [Google Scholar]
- 17.Deck DD, McFarland BH. Medicaid managed care and substance abuse treatment. Psychiatric Services. 2002;53:802. doi: 10.1176/appi.ps.53.7.802. [DOI] [PubMed] [Google Scholar]
- 18.Sosin M, D’Aunno T. The organization of substance abuse managed care. Recent Developments in Alcoholism. 2001;15:27–49. doi: 10.1007/978-0-306-47193-3_3. [DOI] [PubMed] [Google Scholar]
- 19.Steenrod S, Brisson A, McCarty D, et al. Effects of managed care on programs and practices for the treatment of alcohol and drug dependence. Recent Developments in Alcoholism. 2001;15:51–71. doi: 10.1007/978-0-306-47193-3_4. [DOI] [PubMed] [Google Scholar]
- 20.Etheridge RM, Craddock SG, Duteman GH, et al. Treatment services in two national studies of community based drug abuse treatment programs. Journal of Substance Abuse. 1995;7:9–26. doi: 10.1016/0899-3289(95)90303-8. [DOI] [PubMed] [Google Scholar]
- 21.Simpson DD, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcomes Study (DATOS) Psychology of Addictive Behaviors. 1997;11:294–307. [Google Scholar]
- 22.Finney JW, Moos RH. Psychosocial treatments for alcohol use disorders. In: Nathan PE, Gorman JM, editors. A Guide to Treatments That Work. 2nd ed. New York: Oxford University Press; 2002. pp. 157–168. [Google Scholar]
- 23.National Institute on Drug Abuse. Rockville, Md: US Department of Health & Human Services; 1999. Principles of Drug Addiction Treatment: A Research-based Guide. [Google Scholar]
- 24.Manski CF, Pepper JV, Petrie CV. Washington, DC: National Academy Press; 2001. Informing America’s Policy on Illegal Drugs. What We Don’t Know Keeps Hurting Us. [Google Scholar]
- 25.Scott MA, Snowden LR, Libbey AM. Alcohol and juvenile justice contacts: a comparison of fee for service and capitated Medicaid mental health services. Journal of Studies on Alcohol. 2002;63:44–48. [PubMed] [Google Scholar]
- 26.McFarland B, Winthrop K, Cutler D. Integrating mental health into the Oregon Health Plan. Psychiatric Services. 1997;48:191–193. doi: 10.1176/ps.48.2.191. [DOI] [PubMed] [Google Scholar]
- 27.Cutler D, McFarland B, Winthrop K. Mental health in the Oregon Health Plan: integration or fragmentation? Administration and Policy in Mental Health. 1998;25:361–386. doi: 10.1023/a:1022249606959. [DOI] [PubMed] [Google Scholar]
- 28.Barron N, Thurston C, Rumptz M, et al. The Portland Target Cities Project: emerging patterns of service in a managed care environment. Journal of Psychoactive Drugs. 1999;31:241–248. doi: 10.1080/02791072.1999.10471753. [DOI] [PubMed] [Google Scholar]
- 29.Goetz R, McFarland B, Ross K. Editors’ notes. In: Goetz R, McFarland B, Ross K, editors. What the Oregon Health Plan Can Teach Us About Managed Mental Health Care. New Directions for Mental Health Services. Vol. 85. San Francisco: Jossey-Bass; 2000. pp. 1–3. [Google Scholar]
- 30.Goetz R, McFarland B, Ross K. Lessons learned. In: Goetz R, McFarland B, Ross K, editors. What the Oregon Health Plan Can Teach Us About Managed Mental Health Care. New Directions for Mental Health Services. Vol. 85. San Francisco: Jossey-Bass; 2000. pp. 7–16. [Google Scholar]
- 31.Penner N, McFarland B. Background on the Oregon Health Plan. In: Goetz R, McFarland B, Ross K, editors. What the Oregon Health Plan Can Teach Us About Managed Mental Health Care. New Directions for Mental Health Services. Vol. 85. San Francisco: Jossey-Bass; 2000. pp. 23–32. [DOI] [PubMed] [Google Scholar]
- 32.Cutler DL, Bigelow D, McFarland B. The cost of fragmented mental health financing: is it worth it? Community Mental Health Journal. 1992;28:121–133. doi: 10.1007/BF00754279. [DOI] [PubMed] [Google Scholar]
- 33.Ross K, McFarland B. The mental health organizations. In: Goetz R, McFarland B, Ross K, editors. What the Oregon Health Plan Can Teach Us About Managed Mental Health Care. New Directions for Mental Health Services. Vol. 85. San Francisco: Jossey-Bass; 2000. pp. 57–64. [Google Scholar]
- 34.Laws K, Gabriel R, McFarland B. Integration and its discontents: substance abuse treatment in the Oregon Health Plan. Health Affairs. 2002;21(4):284–289. doi: 10.1377/hlthaff.21.4.284. [DOI] [PubMed] [Google Scholar]
- 35.Mee-Lee D, Shulman GD, Fishman J, et al. 2nd ed, rev. Chevy Chase, Md: American Society of Addiction Medicine Inc; 2001. ASAM Patient Placement Criteria for the Treatment of Substance-related Disorders. [Google Scholar]
- 36.McLellan AT, Cacciola J, Kushner J, et al. The fifth edition of the Addiction Severity Index: cautions, additions, and normative data. Journal of Substance Abuse Treatment. 1992;9:192–199. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 37.Carlson M, Gabriel R. Patient satisfaction, use of services, and one-year outcomes in publicly funded substance abuse treatment. Psychiatric Services. 2001;52:1230–1236. doi: 10.1176/appi.ps.52.9.1230. [DOI] [PubMed] [Google Scholar]
- 38.Caspi Y, Turner WM, Panas L, et al. The severity index: an indicator of alcohol and drug dependence using administrative data. Alcoholism Treatment Quarterly. 2001;19:49–64. [Google Scholar]
- 39.Rosenbaum PR. Observational Studies. New York: Springer-Verlag; 1995. [Google Scholar]
- 40.Mojtabai R, Zivin JG. Effectiveness and cost-effectiveness of four treatment modalities for substance disorders: a propensity score analysis. Health Services Research. 2003;38:233–259. doi: 10.1111/1475-6773.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.SPSS Inc. Survival Analysis Procedures (Cox Regression) in SPSS Advanced Models, Version 12.0. Chicago, Ill: SPSS Inc; 2003. [Google Scholar]
- 42.DerSimonian R, Laird NM. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 43.Borenstein M, Rothstein H. Comprehensive Meta-analysis, a Computer Program for Research Synthesis. Englewood, NJ: Biostat; 1999. [Google Scholar]
- 44.McFarland BH, McCamant LE, Barron NM. Outcomes for clients of public substance abuse treatment programs before and after Medicaid managed care. Journal of Substance Abuse Treatment. 2005;28:149–157. doi: 10.1016/j.jsat.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 45.Brockwell SE, Gordon IR. A comparison of statistical methods for meta-analysis. Statistics in Medicine. 2001;20:825–840. doi: 10.1002/sim.650. [DOI] [PubMed] [Google Scholar]
- 46.Sidik K, Jonkman JN. A simple confidence interval for meta-analysis. Statistics in Medicine. 2002;21:3153–3159. doi: 10.1002/sim.1262. [DOI] [PubMed] [Google Scholar]
- 47.Humphreys K, Weingardt KR. Assessing readmission to substance abuse treatment as an indicator of outcome and program performance. Psychiatric Services. 2000;51:1568–1569. doi: 10.1176/appi.ps.51.12.1568. [DOI] [PubMed] [Google Scholar]
- 48.Deck DD, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two western states. Journal of Behavioral Health Services and Research. 2004;32:43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- 49.Harman JS, Manning WG, Lurie N, et al. Association between interruptions in Medicaid coverage and use of inpatient psychiatric services. Psychiatric Services. 2003;54:999–1005. doi: 10.1176/appi.ps.54.7.999. [DOI] [PubMed] [Google Scholar]
- 50.Smith V, Gifford K, Ramesh R, et al. Medicaid Spending Growth: a 50-state Update for Fiscal Year 2003. Washington, DC: Kaiser Commission on Medicaid & the Uninsured; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


