Abstract
These recommendations are the result of a national, multidisciplinary, year-long process to discuss whether and how to proceed with organ donation after cardiocirculatory death (DCD) in Canada. A national forum was held in February 2005 to discuss and develop recommendations on the principles, procedures and practice related to DCD, including ethical and legal considerations. At the forum's conclusion, a strong majority of participants supported proceeding with DCD programs in Canada. The forum also recognized the need to formulate and emphasize core values to guide the development of programs and protocols based on the medical, ethical and legal framework established at this meeting.
Although end-of-life care should routinely include the opportunity to donate organs and tissues, the duty of care toward dying patients and their families remains the dominant priority of health care teams. The complexity and profound implications of death are recognized and should be respected, along with differing personal, ethnocultural and religious perspectives on death and donation. Decisions around withdrawal of life-sustaining therapies, management of the dying process and the determination of death by cardiocirculatory criteria should be separate from and independent of donation and transplant processes.
The recommendations in this report are intended to guide individual programs, regional health authorities and jurisdictions in the development of DCD protocols. Programs will develop based on local leadership and advance planning that includes education and engagement of stakeholders, mechanisms to assure safety and quality and public information. We recommend that programs begin with controlled DCD within the intensive care unit where (after a consensual decision to withdraw life-sustaining therapy) death is anticipated, but has not yet occurred, and unhurried consent discussions can be held. Uncontrolled donation (where death has occurred after unanticipated cardiac arrest) should only be considered after a controlled DCD program is well established. Although we recommend that programs commence with kidney donation, regional transplant expertise may guide the inclusion of other organs. The impact of DCD, including pre-and post-mortem interventions, on donor family experiences, organ availability, graft function and recipient survival should be carefully documented and studied.
There are 2 fundamental but not mutually exclusive perspectives on organ donation. As an important part of end-of-life care, patients who die should be provided the opportunity to donate organs and tissues. Potential transplant recipients, who would otherwise die or be substantially compromised, can benefit from initiatives that address the current shortage of organs for transplantation. Current Canadian practice supports organ donation after death determined by neurologic criteria and tissue donation after death determined by cardiocirculatory criteria. However, contrary to international practice and the practice in Canada before the establishment of brain death criteria, organ donation after cardiocirculatory death (DCD) has not been offered to dying patients and is not available to families who request it. Reflecting these perspectives, the Canadian transplant and donation communities have called for the establishment of this form of donation.1
The Canadian Critical Care Society, representing intensive care unit (ICU) physicians caring for critically ill patients, strongly supports collaborative initiatives to develop, implement and evaluate processes to increase organ and tissue donation within a sound legal and ethical framework.2 At the same time, they have cautioned against proceeding with DCD — sometimes described as non-heart-beating (NHB) donation — without a comprehensive national discussion. In Quebec, a recent consultative report by the Commission de l'éthique de la science et de la technologie addressed a number of the ethical issues inherent in this form of donation.3
The purpose of the Canadian Council for Donation and Transplantation (CCDT) is to strengthen Canada's donation and transplant system through recommendations to the Conference of Deputy Ministers of Health. The strategy of the CCDT Donation Committee is to develop a framework for action at local, provincial, territorial and national levels that will develop and incorporate best practices for organ and tissue donation as a routine part of end-of-life care. This framework is based on best evidence provided through a review of existing practices, policies and guidelines, both national and international; a review of scientific data and literature; and expert consensus.
To date, the CCDT Donation Committee has hosted 2 forums to consult with health professionals and other key stakeholders on best practices: Severe Brain Injury to Neurological Determination of Death, held in April 2003, focused on development of a national agreement on the processes of care, commencing with severe brain injury and culminating with neurologic determination of death;4 Medical Management to Maximize Donor Organ Potential, held in February 2004, developed guidelines and standards that will enable Canadian health professionals to improve organ donor management and the use of organs from consenting donors.5
As the next step in this strategy, on Feb. 17–20, 2005, the CCDT Donation Committee convened a third Canadian forum, Donation after Cardiocirculatory Death. The focus of this forum was to initiate a national multistakeholder discussion to inform and guide health care professionals involved in developing programs for DCD. For the purposes of this forum, the concept of organ and tissue donation after death was accepted, as it is a reflection of current practice. Discussion at the forum was restricted to optimal and safe practice in the field as it pertains to DCD. The recommendations in this report promote patient-care-based principles for providing the option of donation within a sound ethical framework and provide guidance to individual programs in developing parameters for safe practice in this field.
Background and objectives
The purpose of this initiative was to discuss and develop recommendations on the principles, procedures and practice related to DCD within a sound ethical and legal framework in the context of protecting and serving the public. The main question that the forum expected to answer was: can we offer DCD while maintaining the fundamental principles that preserve patient and family interests and professional standards? For the purposes of this document and forum recommendations, “family” is broadly defined to include those people identified by the patient or client as providing familial support, regardless of whether they are biologically related.
The objectives of the forum included:
• Establish Canadian medical criteria for defining eligibility for organ donation after cardiocirculatory death.
• Discuss conditions under which cardiocirculatory death, once anticipated or established, can activate organ donation procedures.
• Explore the ethical implications of DCD including:
a) Defining death independent of the needs of organ donation and transplantation
b) Interventions on patients before expressed or granted consent
c) Interventions after consent
d) Potential conflicts of interest
e) Protecting and serving the public.
• Address consent issues (e.g., related to timing and accountability for decision-making).
• Define the technical procedures and preservation techniques for organ donation and procurement.
• Define reasonable time limits for solid organ donation to be successful, including discussion of evolving techniques to maximize the opportunity.
The forum focused on the interval from the anticipation or determination of cardiocirculatory death to organ recovery. The following issues were not included in the scope of this forum.
• Ethical considerations related to existing medical practice did not include the ethical framework for:
a) Withdrawal of life-sustaining therapy (WLST) in the ICU: the medical decision to withdraw life support is within the domain of critical care practice. Discussion of these processes was limited to the manner in which they influence organ donation practice and organ viability.
b) Not initiating or terminating cardiopulmonary resuscitation (CPR).
• Ethnocultural and religious considerations regarding the cardiocirculatory determination of death from the perspectives of various communities were not addressed.
• Details of ex situ organ preservation were not included.
• Issues related to organ allocation were not included.
Process
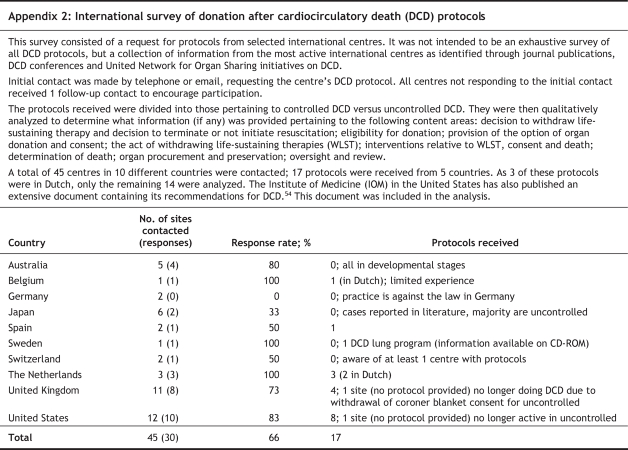
In advance of the forum, the Steering Committee provided substantive background documents, including comprehensive literature reviews (on current and historical clinical practices, death review, ethics, legal, allograft outcomes) and related practice surveys (international survey of practice [Appendix 2], expert clinical speaker survey of practice). Given the complexity of the social, medical, ethical and legal challenges related to DCD, a substantial part of the forum agenda was dedicated to presentations from family, patient and medical perspectives to enable participant learning and understanding (Appendix3). During the forum, each topic area was addressed using the following process:
1. Presentations by experts from international jurisdictions where DCD is currently practised were followed by open plenary discussions. Participants then worked in small groups guided by worksheets that provided:
• A summary of existing scientific evidence
• A summary of bioethical and legal implications
• A comparative summary of international DCD management guidelines
• Forum principles
• Key considerations
• A list of references.
2. Small-group discussions focused on specific questions related to the processes of care. They explored
• Death and minimum criteria to proceed with organ donation (controlled and uncontrolled DCD)
• Processes and procedures for WLST as they pertain to DCD (controlled DCD)
• Options for organ donation and consent processes (controlled and uncontrolled DCD)
• Interventions related to phases of care (controlled DCD)
• Post-mortem care and interventions (uncontrolled DCD)
• Limits of organ viability (controlled and uncontrolled DCD)
• Preservation techniques: organ specific (controlled and uncontrolled DCD).
3. The Forum Recommendations Group (FRG) reviewed the results of small group and plenary discussions and developed consensus recommendations that were returned to a plenary session for further clarification and discussion.
4. Participants' suggestions for relevant research questions were gathered and summarized.
5. The Management and Administrative Focus Group considered issues related to logistics and implementation that were identified during the forum (Appendix 4).
Forum participants represented a broad range of disciplines, ensuring that discussions were inclusive and involved multiple perspectives. Forum deliberations were thoughtful, dynamic and collegial as participants focused on building agreement on key challenge questions. Members of the FRG panel came to unanimous agreement on recommendations to inform current and future practice. Potential research areas were also identified (Appendix 5) as well as logistic and knowledge transfer issues.
Recommendations related to DCD
Forum discussions about fundamental principles and ethics led to the expression of concern and related discussions about the need to formulate and emphasize core values to guide the development of program protocols and new procedures related to DCD.
Core values and ethics
The following core values provide a framework to guide deliberations of local programs with respect to the ethical implementation of recommendations in this report.
Respect for the life and dignity of all individuals — All human life, regardless of its actual or perceived quality or its stage in the dying process, deserves respect. Although it is generally seen as appropriate to use the human body as a source of tissues and organs to serve the well-being of other human beings, the donor's body should always be treated with great care and respect. Decisions about a human being must be guided by that individual's values and beliefs with respect to a meaningful life and death. The care of the dying patient must never be compromised by the desire to protect organs for donation or expedite death to allow timely organ retrieval.
Optimal end-of-life care that respects the holistic well-being of the dying patient — The first responsibility of health care providers, regardless of the potential for donation, is to advance the well-being of the dying patient. This includes psychologic, emotional and spiritual well-being in addition to physical well-being.
Respect for patient autonomy — Decisions about care at the end of life should be based on the known values and beliefs of the patient. These decisions should be consistent with what each patient understands to be a meaningful life and death. A meaningful death for patients may or may not include the ability or desire to provide organs to others.
Support for the grieving family and loved ones — It is important to provide support for those about to be bereaved, regardless of whether organ donation occurs. Memories of a loved one's death remain with those left behind. Support for families and loved ones should continue through all phases of dying: before, during and after WLST.
Public trust and avoidance of actual and perceived conflicts of interest — It is important to recognize and minimize possibilities for conflicts of interest that might occur in the setting of DCD. Conflicts of interest occur when those involved in providing health care have relationships with people or organizations outside the healing relationship that may influence their actions, regardless of whether they believe these relationships actually affect their judgement. Conflict of interest should be differentiated from dual commitments or the congruence of interests that naturally arises when health care teams provide the opportunity to donate for those who may wish to do so.
Conflicts of interest may have a negligible or considerable effect on judgement. They may influence care at any stage in the process of organ and tissue donation and, therefore, should be identified. Failure to identify and disclose such conflicts may undermine the integrity of a program and jeopardize public and professional trust.
Respect for professional integrity — Those involved with end-of-life care, donation and transplantation are guided by their own values and beliefs and by the professional values and standards of practice as articulated by their professional organizations. Decisions in the context of DCD must not be influenced by considerations of professional loyalties, prestige, personal gain or any actions that are in conflict with the pursuit of excellence in end-of-life care for the potential or actual organ donor.
Overarching considerations
• This forum and participating organizations support efforts to incorporate donation into end-of-life care and to optimize organ and tissue donation in Canada. Individuals should be given the option of organ donation after death, and health care systems should establish the processes and procedures to provide this option.
• Donation services should be offered in the context of maintaining respect for the beliefs and values of the individuals involved. It is recognized that based on societal, cultural, religious and other personal beliefs, some individuals within families and within the health care team may have different views on the meaning and permissibility of organ and tissue donation after death as determined by neurologic or cardiocirculatory criteria. If patients and families decline the opportunity to donate, their decision should be fully supported. Health care team members who do not support organ donation should seek the involvement of an alternate colleague in appropriate circumstances.
• The current law related to donation is subject to interpretation in the context of DCD. Current consent to treatment legislation has not addressed issues specific to this form of donation. Forum participants discussed the need for further legal review to address this issue (currently in the planning phase at CCDT).
Based on these overarching considerations, the forum made the following recommendations.
1. Terminology and patient conditions
We recommend that:
a) The term “donation after cardiocirculatory death (DCD)” be adopted to refer to this form of donation in Canada.
b) “Controlled DCD” refer to circumstances where donation may initially be considered when death is anticipated, but has not yet occurred. This may take place in an ICU or special care unit after a consensual decision to withdraw life-sustaining therapy. Before considering donation, the patient should be judged to have:
• A non-recoverable injury or illness
• Dependence on life-sustaining therapy
• Intention to withdraw life-sustaining therapy, and
• Anticipation of imminent death after withdrawal of life-sustaining therapy.
c) “Uncontrolled DCD” refer to circumstances where donation is initially considered after death has occurred, but was not anticipated. This may occur in the emergency department, hospital ward, ICU, special care unit or pre-hospital locations. The deceased will have had a witnessed cardiocirculatory arrest of known duration, and there should already be an established decision to terminate or not to initiate cardiopulmonary resuscitation (CPR).
d) Donor suitability be determined by many factors including age of the donor, comorbid disease states, specific tests of organ function and terminal donor events. Demographic and organ function criteria should be the same as for donors after neurologic determination of death (NDD) and should be determined by individual transplant programs.
e) Potential DCD donors should be considered regardless of age, but it is recognized that many existing DCD programs have a greater restriction on age criteria than for donors after NDD. Strict age criteria should be determined by individual programs.
Key considerations
• A “consensual decision to withdraw life-sustaining therapies” is defined as a decision that has been agreed to by the patient, family and the treating health care team.
• DCD replaces but is synonymous with other terms such as NHB donation, donation after cardiocirculatory determination of death or donation after cardiac death.
• This forum has used the terms “uncontrolled” (regardless of location, cardiac arrest is unanticipated) and “controlled” (cardiac arrest is anticipated). These terms replace existing categorizations that include the Maastricht criteria.6
• The terms “controlled” and “uncontrolled” should not be misunderstood to imply a reflection on professional behaviour or the organization of clinical services. The degree of control refers to the temporal constraints and the opportunity for consent discussions in relation to death.
• For uncontrolled DCD, management is complicated by the fact that death is sudden or unanticipated and may not have occurred within the medical setting. Although donation interventions should be initiated as soon as possible, the surrogate decision-makers or advance directives may not be immediately available to provide consent.
• For controlled DCD, life-sustaining therapy can be defined as ventilatory support, artificial airway support, hemodynamic support or a combination of these provided in the ICU or special care unit. Patient conditions may include, but are not limited to, severe brain injury of diverse etiology, end-stage neuromuscular failure, high cervical spinal cord injury and end-stage organ failure.
• For completeness, the forum addressed both forms of DCD. However, in its conclusion, the forum has recommended that programs initiate and establish controlled DCD before advancing with uncontrolled DCD (recommendation 9.2).
Summaries of evidence
Controlled versus uncontrolled donors
For the purposes of the forum and from a practical clinical perspective, it is useful to classify DCD into 2 subgroups (Fig. 1):
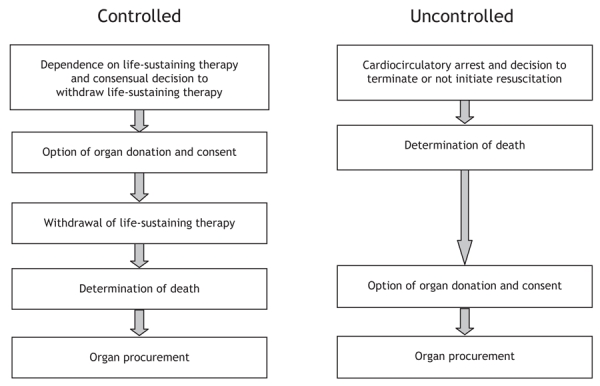
Fig. 1: Sequence of care in controlled and uncontrolled donation after cardiocirculatory death.
Uncontrolled: The patient presents with an unanticipated cardiac arrest, regardless of location. Precise information on the time of cardiac arrest is required to estimate warm ischemic time, which directly affects organ viability. It includes:
1. Dead on arrival to the emergency department (Maastricht category I)
2. Unsuccessful resuscitation in patients with cardiac arrest, which may occur in the emergency department, ICU, special care units or hospital wards (Maastricht category II)
3. Cardiac arrest following NDD in the ICU (Maastricht category IV).
Most uncontrolled NHB donors worldwide are category I and II and account for the bulk of patients considered eligible for NHB donation in continental Europe and Japan.
Controlled: Cardiac arrest is anticipated and, characteristically, these patients are
1. Already being treated in the ICU or special care unit environment
2. Do not fulfill neurologic criteria for death
3. Require ventilatory, artificial airway or hemodynamic support
4. Continuing medical care may be considered futile or treatment burden exceeds benefit
5. Death is anticipated to occur imminently on withdrawal of life-sustaining therapies.
Patient conditions may include, but are not limited to, catastrophic brain injury of diverse etiology, cervical spinal cord injury and end-stage neuromuscular diseases (Table 1). These patients (Maastricht category III) constitute the majority of identifiable DCD in the United States.
Table 1
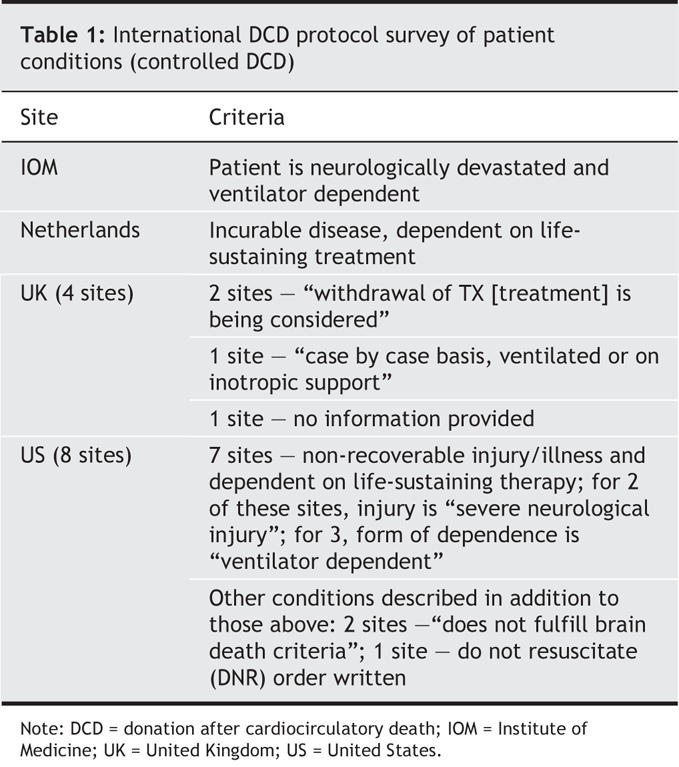
Eligibility criteria for DCD
As a general rule, eligibility criteria are similar to those for organ donation after NDD and should be based on demographic, age and organ-function criteria detailed in the previous CCDT forum.5 Patients with a history of intravenous drug abuse, sepsis or serious systemic infection, or active malignancies and high-grade brain tumours are excluded. Bacteremic patients are not necessarily excluded.7 Patients with non-melanoma skin malignancies and some primary non-metastatic brain tumours may be eligible.8–10 Organs contaminated with hepatitis B, C or HIV may be transplanted into recipients already infected with these same viruses. Infections with human T-cell leukemia-lymphoma virus, systemic viral infection (e.g., measles, rabies, adenovirus), prion-related disease and herpetic meningoencephalitis are contraindications for organ donation.
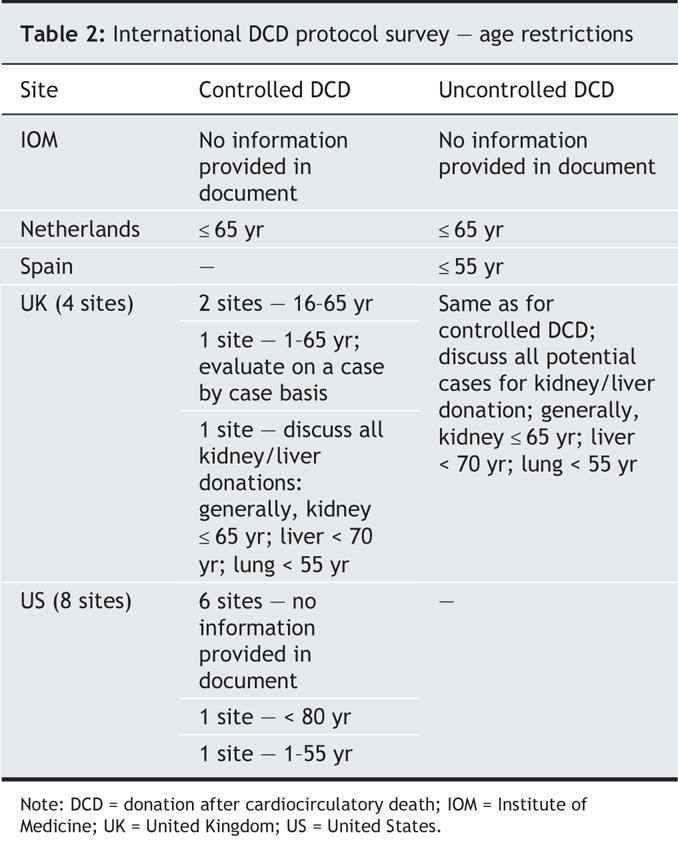
Donor age
There has been no consensus as to age limits for donors after brain death or cardiac death. In most series comparing DCD donors with donors after brain death, the mean age of the DCD donors tends to be lower than that of the brain death cohort (Table 2). In a multicentre Japanese series of 706 kidney transplants from DCD donors, donor age > 55 years had the largest negative impact on long-term allograft survival.11 There is a strong relation between donor age and delayed graft functioning (DGF) rates. Given that DCD donors have increased DGF rates, the combination of older age and DCD donors may result in the highest DGF rates, although this has not been well documented.
Table 2
2. Death and the minimum criteria to proceed with organ donation
a) Determination of fact of death — By law, for the purposes of a post-mortem transplant and as it applies to DCD, the fact of death shall be determined by 2 physicians in accordance with “accepted medical practice.” Physicians must be physically present to determine death.
b) Conflict of interest — No physician who has had any association with a proposed transplant recipient that might influence their judgement shall take any part in the determination of death of the donor.
c) Prohibition on participation in transplant — No physician who took any part in the determination of the fact of death of the donor shall participate in any way in transplant procedures.
d) Determination of cardiocirculatory death — This forum only defined accepted medical practice for the determination of death for the purposes of organ donation in the context of DCD. For the purposes of DCD, we recommend that the following criteria be met before organ procurement:
• Beginning with the onset of circulatory arrest, there must be a 5-minute period during which the absence of palpable pulses, blood pressure and respiration are continuously observed by at least 1 physician and
• Death is determined by 2 physicians by documenting the absence of palpable pulses, blood pressure and respiration on completion of this 5-minute period.
The physician present during the 5-minute period of continuous observation and who makes 1 of the determinations of death must be a staff physician with the requisite skill and training.
Monitoring to establish the fact of death is the priority during this period of observation. There must be no interventions to facilitate donation during this period.
Key considerations
• For the purposes of DCD, 1 of the physicians determining death must be a staff physician with full and current licensure for independent medical practice in the relevant Canadian jurisdiction. Physicians on an educational register (residents, fellows) may carry out the second determination.
• The legal time of death is the determination after a 5-minute observation period.
• The purpose of the 5-minute observation period is to confirm the irreversibility of cardiocirculatory arrest before organ procurement.
• Blood pressure is defined as an arterial pressure that generates anterograde circulation. The preferred method to confirm the absence of blood pressure is by arterial line monitoring.
Summaries of evidence
Legal criteria for the determination of death
There is no federal statutory definition of death in Canada and, therefore, no standard legal definition of death that applies across the country. As health care comes under provincial and territorial jurisdictions, each province and territory has a statute that governs organ and tissue donation. With the exception of Quebec, New Brunswick, the Northwest Territories and Nunavut, all provinces have legislation that includes provision for the determination of death for the purposes of post-mortem transplantation, which can be paraphrased as follows:
1. Determination of death must be made by at least 2 physicians in accordance with “accepted medical practice.”
2. The physicians making the determination of death
a. must not have any association with the proposed transplant recipient that might influence their judgement and
b. cannot participate in the transplant proceedings.
The United States Uniform Determination of Death Act12 (UDDA) specifies that death may be established by the irreversible loss of all brain function (brain death/determination of death by neurologic criteria) or by the irreversible cessation of cardiorespiratory function.
Medical criteria for the determination of death
Provincial and territorial legislation does not outline what is meant by “accepted medical practice” or the tests or mechanisms that should be employed to determine death. The strict medical procedures for death determined by neurologic criteria were established by a previous CCDT-sponsored forum.5 The UDDA specifies 3 criteria for death by cardiorespiratory criteria: unresponsiveness; apnea; and permanent cessation of circulation. However, the UDDA has never provided criteria for the determination; death should be declared based on current standards established by the medical community.
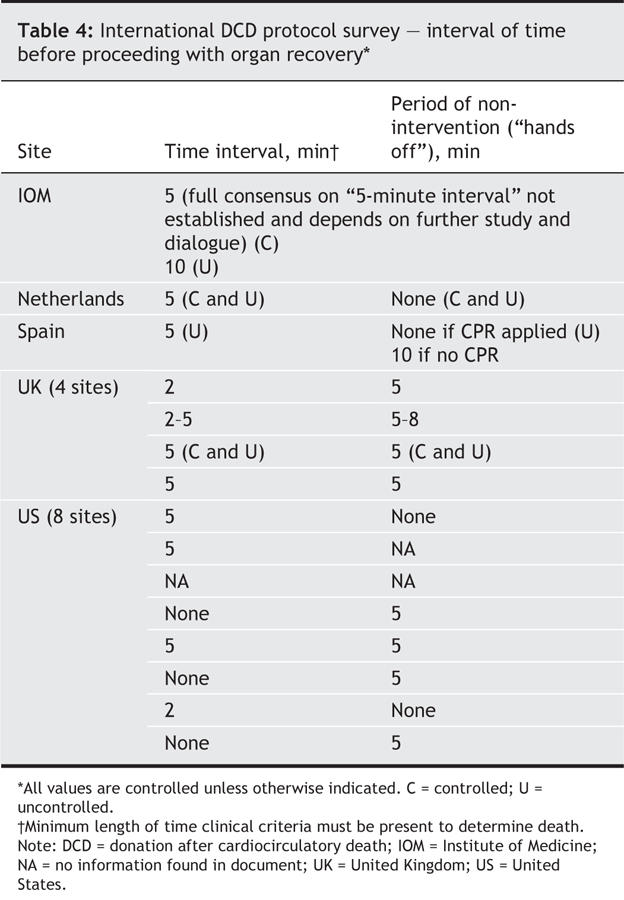
Outside of review articles on DCD, the cardiorespiratory criteria for death are rarely mentioned in the literature. A literature review did not reveal any studies examining the various methods of monitoring for cardiocirculatory function at or near the time of death (Table 3, Table 4).
Table 3
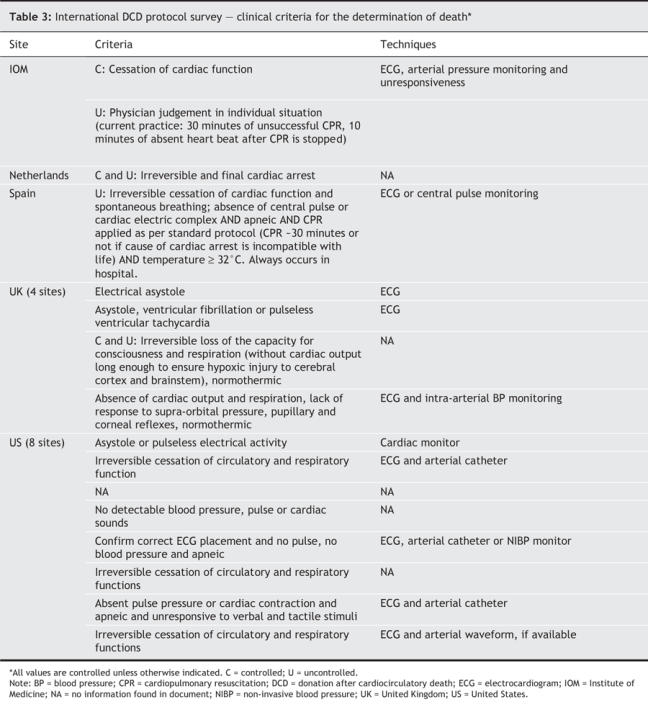
Table 4
Irreversibility of death
Until recently, there has been little need for the medical community to concern itself with the timing of a patient's death and the literature pertaining to this issue is scarce. In Canada, death is declared by physicians (or their delegates) and coroners or medical examiners. Less frequently, nurses with advanced specialization may declare death, particularly in remote service areas. The timing of this declaration following cardiopulmonary arrest has been largely irrelevant and remains unspecified. The vast majority of deaths in Canada occur in circumstances where organ donation is not a consideration.
However, when contemplating DCD, the duration of cardiocirculatory arrest becomes relevant as the organs will deteriorate rapidly following cessation of oxygenation and perfusion. Organ procurement must not precede the clinical declaration of death by either neurologic or cardiocirculatory criteria. The “dead donor rule”13 is upheld to avoid causing death by removing an individual's organs.
In the context of end-of-life care with potential DCD, a decision has been made to withdraw, terminate or not initiate resuscitative measures. Of concern is the meaning of “irreversible,” particularly when a decision to withhold or discontinue CPR has been made. Death requires irreversible stoppage, yet it is unclear whether that means the heart could not be started or merely will not be.14 The Institute of Medicine (IOM) argues that irreversibility is defined by the absence of spontaneous recovery of cardiorespiratory function. Although controversial, there has been speculation that a phenomenon known as autoresuscitation may exist (spontaneous, transient resumption of cardiac function following cardiopulmonary arrest),15 but has not been reported to occur beyond 2 minutes.16
Addressing the ambiguity surrounding the term “irreversible” in its position paper on NHB organ donation, the ethics committee of the American College of Critical Care Medicine (ACCCM) distinguishes between stronger and weaker interpretations of “irreversible.”16 In the stronger interpretation, the heart cannot be restarted no matter what intervention is done, including CPR. In the weaker interpretation, circulation cannot be restored because CPR efforts have been refused by the patient (as a DNR order in an advance directive), by a surrogate decision-maker or by the medical team because it is not medically indicated. The ACCCM group has recommended the weaker interpretation, with a reasonable observation time of between 2 minutes from cessation of cardiocirculatory functions with no spontaneous restoration of circulation (as recommended by the Pittsburgh Protocol) and 5 minutes (as recommended by the IOM).
The ACCCM argues that no less than 2 minutes is acceptable and no more than 5 minutes is necessary when determining death for potential DCD. Menikoff17 argues that irreversibility of cardiopulmonary functioning may not be guaranteed following a 5-minute period of arrest and that portions of the dying person's brain may not have completely ceased functioning at this point. Based on animal studies and isolated human case reports, electrical function of the brain ceases within 20 s after circulatory arrest.18–21 The forum literature review could not identify any evidence base for either Menikoff's arguments or the IOM position.
3. Process and procedures for withdrawal of life-sustaining therapy (WLST) in controlled DCD
3.1 Process and procedures for WLST
Decision-making process for WLST
a) The medical and ethical framework for WLST in the ICU falls within the domain of critical care and neurocritical care practice and must not be influenced by donation potential. It is the responsibility of the critical care and neurocritical care communities to ensure optimal and safe practice in this field.
b) Health care professionals responsible for the decision and procedure to withdraw life-sustaining therapies should
• Have the requisite skill and knowledge in the area
• Not have any association with the proposed transplant recipient that might influence judgement
• Be independent of transplant proceedings and
• Act in accordance with current end-of-life practice in the local ICU or special care unit.
c) The decision to withdraw life-sustaining therapies should be made before any discussion of organ and tissue donation that is initiated by health care providers. The organ donation/procurement/transplant team must not be involved in the decision to withdraw life-sustaining therapies.
Procedures for WLST
a) The management of the dying process, including procedures for WLST and sedation, analgesia and comfort care, should proceed according to existing ICU practice in the best interests of the dying patient and should not be influenced by donation potential.
b) Consideration for the dignity of the dying process should be guided by patient interests and the family's needs and desires.
c) The family should be provided with a clear explanation of their option to remain with the patient during WLST, at the time of death and beyond, and there should be a full discussion of the variables that may affect organ viability for successful donation.
d) The ICU patient care team is responsible for all aspects of management during this interval of care leading to death. The organ donation/procurement/transplant team must not be involved in WLST procedures or in the management of the dying process.
e) WLST is an accepted part of end-of-life care in most hospitals in Canada and proceeds in accordance with accepted medical and ICU practice. We recommend that ICUs establish policies and procedures that
• Are consistent with current practices and
• Apply to all patients where WLST is considered.
These policies and procedures should be locally determined and may include a bioethics consultation or opinion by a second physician.
Key considerations
• The quality of the decision-making process must not be influenced by the potential for DCD.
• When WLST is proposed and DCD may be considered, the decision to proceed with WLST should be inclusive, consultative, contemplative and appropriately timed.
• As it applies to palliative care, the principle of double effect supports the administration of treatments with the intent to support patient comfort and alleviate suffering, even if there is a risk (foreseen but not intended) of hastening death.22
3.2 WLST requirements and safeguards
For the purposes of DCD, we recommend that the following additional requirements or safeguards be in place regarding the WLST decision-making process and procedures:
• Established ICU or hospital policies and guidelines related to WLST, including bioethics input
• Review of DCD case management and a periodic quality assurance process
• Planned staff debriefing on a regular basis.
Key considerations
• Quality of patient care and decision-making should be the same irrespective of whether donation is considered. Policies and procedures for WLST should be in place for both donation and non-donation cases.
• Support for health care professionals should be provided as required.
3.3 Donor and recipient care
In the ICUs of hospitals that perform transplants, there may be unavoidable times when a potential controlled DCD donor (before death) is cared for in the same unit as an end-stage organ failure patient who is a potential transplant recipient. Under these circumstances, we recommend that attending hospital staff caring for the recipient should be different from staff caring for the donor.
Key considerations
• “Attending staff” is defined as the attending staff physician and bedside nursing staff.
• It is recognized that local realities regarding logistics, staffing and practicalities may make it difficult to follow this recommendation. However, hospitals or jurisdictions implementing DCD programs should be responsible for providing the support necessary to develop this capacity.
3.4 Maximum time limit from WLST to death
We recommend that there be a maximum time limit from WLST to death beyond which organs will not be offered or procured; that is, if death does not occur within this period, organs will not be procured and ICU end-of-life care will continue.
This time limit should be 1 to 2 h, but should be guided by individual organ-specific programs and individual donor factors.
Key considerations
• Time limits are related to family factors and ICU and operating room logistics.
• Setting time limits helps clarify expectations for families and staff.
• Time limits are congruent with organ viability limits in section 7 of these recommendations.
3.5 Estimation of time to death after WLST
We recommend that following consent specific to this procedure, a formal estimation of the time to death after WLST be made using tools such as, but not restricted to, the Wisconsin evaluation tool.23 The tool may be used to:
• Determine eligibility to donate
• Provide input to family discussions about likelihood for successful donation
• Guide the preferred location for WLST.
Key considerations
• Tools to estimate time of death after WLST are not currently used as a standard practice in the ICU. They should be considered as a donor-based intervention and appropriate consent should be sought.
• The safety of the procedure should be considered before its application.
• The reliability of predictive tools depends on patient conditions and the specific ICU actions and tempo of procedures during WLST.
• These tools are in evolution and should be adjusted based on continuing research.
• Some clinical conditions, such as patients on extracorporeal life support, including artificial heart technology, or previous documentation of apnea (for other indications), do not require predictive testing.
3.6 Location of WLST
We recommend that WLST should occur in the ICU or in the operating room, with flexibility based on family preferences, institutional logistics, resources and facilities.
Key considerations
• The family should be given information about the impact of the location of WLST on the potential for successful donation.
• Psychosocial, spiritual and bereavement support should continue to be provided to families regardless of the location of WLST.
3.7 Transfer of patients before WLST
We recommend that a patient who fulfills eligibility criteria for controlled donation, at a hospital where DCD is not practised or available, may be transferred before WLST to a hospital that performs controlled DCD. This should only occur with the full informed consent of the patient or family and with full consultation with and the agreement of the receiving hospital.
Key considerations
• This recommendation is based on the principle of referring a patient to a hospital that provides a service not available at the source hospital and is specific to donation/procurement hospitals that provide DCD.
• Logistics and funding to support this activity should be provided by individual jurisdictions.
• Costs associated with transfers should not impose an economic burden on the family.
• The family should be aware that imminent death following WLST and organ donation may not occur despite the transfer.
Summaries of evidence
Role of the ICU team
Mortality rates of ICU patients in Canada are 10%–20% in adults and 3%–5% in children. Death in the ICU will usually occur in 1 of 4 ways:
1. Patients receiving full treatment suffer a cardiac arrest and an attempt at CPR is made but is unsuccessful.
2. Patients receiving full treatment suffer a cardiac arrest, but no attempt at CPR is made (DNR orders in place).
3. Some or all treatment is withheld or withdrawn, the patient suffers a cardiac arrest and no attempt at CPR is initiated.
4. Death is determined based on neurologic criteria (NDD or brain death).
Most deaths in neonatal, pediatric and adult intensive care are related to irrecoverable illness and are preceded by withdrawal or withholding of life-sustaining treatment. This is accepted ICU practice throughout the world, although there is considerable geographic variation. Where the burden of continued treatment far exceeds benefit, WLST takes place after discussion and consent or assent by the patient or the patient's surrogate. Reported WLST rates in single-centre Canadian ICUs range from 65%24 to 79%.25
There is evidence for practice variation in the provision of end-of-life care in the ICU related to patient factors, such as disease acuity, presence or absence of advance directives, attitudes and ethnocultural beliefs. Variance can also be explained by physician factors, such as age and experience, religious background, subspecialty or place of work (academic v. community centre or open v. closed ICU).26–28
WLST methods are influenced by patient condition, but may vary among individual physicians and ICU centres. Different approaches to withdrawal of mechanical ventilation have been cited.29 WLST methods may include, but are not limited to, 1 or more of the following:
1. Terminal extubation (removal of mechanical ventilation and the artificial airway)
2. Rapid discontinuation of mechanical ventilatory support
3. Terminal weaning (gradual decrease in mechanical ventilatory support with or without removal of the artificial airway)
4. Gradual weaning of hemodynamic supports
5. Rapid discontinuation of hemodynamic supports.
There are no standardized procedures for WLST, nor is there any intrinsically “correct” way to proceed or optimal duration of the process. Patient care during this phase must be directed toward maintaining patient comfort and alleviating suffering. The principle of double effect supports the administration of treatments consistent with this intent, even if there is a risk (foreseen but not intended) of hastening death. The use of comfort medications may vary in type (analgesics, sedatives), dose and strategy (proactive prevention of pain v. reactive treatment of pain).25,30 Regardless of underlying disease, variation in WLST method and the use of comfort medication may result in variation in the time from WLST to death.
It is widely agreed that patient care issues must be completely differentiated from those related to organ procurement. The decision to withdraw life-sustaining therapy must be made independent of any decision to donate organs for transplantation. Detailed discussions regarding organ donation and procurement should not to be held until the decision to withdraw medical therapy has been made.31 Physicians involved in the initial patient care and WLST as the patient dies must not be involved in the procurement and transplantation processes. This prevents both real and perceived conflicts of interest for ICU staff between their therapeutic duty to the critically ill patient and their non-therapeutic relation with potential organ transplant recipients.16,32 In circumstances where the ICU may concurrently care for end-stage organ failure patients who are potential transplant recipients, physicians and caregivers who may be in conflict should voluntarily withdraw from the care of a potential donor.
Once a decision to withdraw life-sustaining therapy has been made by the treating team and the family, approaching families about donation is ethically appropriate and consistent with a process that would enable patients or their substitute decision-makers to realize the patient's desire and intent to donate organs after death. Some families might perceive the request for donation as implying that the principal concern of the medical team is the patient's organs rather than the patient. It may be appropriate to delegate these discussions to representatives from an organ procurement organization or a program representative from the health care organization itself.
Predicting death
WLST does not necessarily lead to imminent death. ICU practitioners are cognizant of the difficulty of reliably predicting if and when a patient will die after WLST. Although no formal testing generally occurs (outside of DCD), influencing variables include patient condition (e.g., level of consciousness, degree of airway obstruction, ventilatory drive, oxygenation impairment, hemodynamic instability) and WLST methods (i.e., procedures and comfort medications).
After the family consents to controlled DCD, there are still steps in the process which may preclude donation. For example, the duration of the dying process might exceed the upper limit for organ viability in the context of transplantation. During the interval of time from WLST to death, patients who experience a slow progressive demise (hypotension and hypoxemia) may become unsuitable candidates for DCD as organs will be irreparably damaged by warm ischemic injury during the dying process.31 In addition, there are time constraints related to logistic preparations. For example, the surgical procurement team, anesthetist and other operating room staff must be alerted and kept on hold until death and minimum criteria to donate are established.
A clinical tool developed by the University of Wisconsin program has predicted, with 90% accuracy, patients who will expire within 2 h following WLST.23 The testing protocol requires the collection of information that includes patient age, airway status, vasopressor and inotrope therapy, and the respiratory status following 10 minutes of disconnect from the ventilator (respiratory rate, tidal volume, negative inspiratory force, blood pressure, pulse and oxygen saturation). Selection of candidates for organ donation is based on the respiratory drive assessment and the use of this predictive tool before WLST. In the Wisconsin experience, about 10% of identified potential DCD donors were returned to the unit or hospital floor for palliative care.33
The role of the operating room
WLST traditionally occurs within the ICU environment. Access to a surgical suite is typically required for organ procurement in controlled DCD, often necessitating transfer of the patient to the operating room before WLST to allow for rapid surgical intervention for organ preservation and procurement after death. Concerns have been cited about involvement of third-party anesthesiologists during WLST, particularly if they have not been previously involved with the care and WLST discussions specific to that patient.34,35 In most cases, it will be in the best interests of the patient and family for the ICU team to continue to assume responsibility for the dying process regardless of the location of WLST.
4. The option of donation in controlled DCD
4.1 Option of organ and tissue donation
We recommend that:
a) The option of organ and tissue donation should be routinely provided to all potential donors and families. Distinct from common practice after NDD, it is necessary to present the option of donation before the fact of death in controlled DCD.
b) In centres that develop DCD programs, the option of organ and tissue donation should be presented to patients and families after the consensual decision to withdraw life-sustaining therapies but before the act of withdrawing life-sustaining therapies. A discussion of donation options may occur at any time if initiated by a patient or family request for information.
c) The person or group who is best trained and most experienced should hold the consent discussions, based on local organizational or institutional practice.
Key considerations
• A “consensual decision to withdraw life-sustaining therapies” is defined as a decision that has been agreed to by the patient or family and the treating health care team.
• The initial discussion about the possibility of donation should be distinguished from the discussion to obtain informed consent for donation.
4.2 Notification of coordinators
For controlled DCD where the patient fulfills eligibility criteria for donation, it is necessary to involve a separate coordinator before death. We recommend that coordinators be routinely notified by the ICU team after the consensual decision to withdraw life-sustaining therapies but before the act of WLST.
Key consideration
This recommendation should be considered in the context of provincial legislation.
Summaries of evidence
In controlled DCD, a competent patient or his or her surrogate has consented to the withdrawal of ventilation or other life-sustaining therapy. Consent implies that the patient or substitute decision-maker has been informed of the nature and purpose of the treatment withdrawal and understands what this action entails. Consent to organ procurement for transplantation is given by a patient or surrogate independently of consent to withdraw life support and presumes that procurement will take place only after death has been declared. Life support can justifiably be withdrawn and organ procurement commenced after a clinical declaration of death.36 Withdrawal of life support and subsequent organ procurement are permissible provided that the patient has been deemed imminently and irreversibly dying and has consented separately to the withdrawal of life support and to organ procurement for transplantation.37
5. Interventions relative to phases of care: controlled and uncontrolled DCD
From the bioethical and legal perspectives, the relevant intervals of care are before death and after death. Based on forum plenary discussions, the FRG concluded that it is premature to be prescriptive in the details for each donor-based medical intervention. The timing and type of interventions may vary by region and with the introduction of new therapies over time. The forum recommends the following parameters for safe practice in consideration of the risk–benefit ratio.
5.1 Donation-based interventions
We recommend the following:
a) Before death (as defined in recommendation 2a), and as it applies to controlled DCD, the care of the patient is under the direction of the patient care team. Interventions to facilitate donation require the specific and informed consent of the patient or family for each intervention. Their purpose should be understood in terms of how they might improve successful donation after death. These interventions should not be intended to hasten death or otherwise harm the patient and should pose no more than minimal risk. Interventions should only be undertaken with consideration of risks and benefits.
b) After death (as defined in recommendation 2a), and as it applies to controlled and uncontrolled DCD, interventions require only general consent to donation.
c) Surgical interventions related to cannulation and perfusion should be carried out only by the organ retrieval or transplant team.
d) Thrombolytic agents should not be administered before the fact of death.
e) Heparin should not be administered before death in cases of established or ongoing bleeding.
f) Vasodilators should not be administered before death in patients who are receiving vasopressor support.
g) Interventions that may re-institute cerebral perfusion and oxygenation after the fact of death should not be performed.
Key considerations
• Benefit to the patient is interpreted as both therapeutic benefit to the patient and realization of the donor's interests and wishes based on the desire and intent to donate.
• Where the medical team seeks consent for pre-or post-mortem interventions, the team must ensure that the proxy has appropriate (legal) authority to grant such consent. Consideration should be given to the legal authority granted by consent to treatment legislation, tissue and organ donation legislation, and case law.
• DCD has not been directly addressed in existing law. The consent regime as it applies to DCD, especially related to pre-mortem interventions, must be examined on a jurisdiction-by-jurisdiction basis to identify gaps or ambiguities.
• When the patient is capable, informed patient consent is to be obtained.
5.2 Responsibility for pharmacologic interventions before death
We recommend that the ICU team or the anesthesiologist caring for the potential donor in the operating room be permitted to administer pharmacologic donor-based interventions before death.
Key considerations
• Organ donation or transplant coordinators who are not part of the patient care team should not administer donor-based pharmacologic interventions.
• ICU team members should use their professional discretion in carrying out such treatments. This recommendation does not obligate ICU team members to carry out treatments they consider against the best interests of the patient.
Summaries of evidence
The doctrine of double effect,22 which acknowledges that the same act can have both good and bad effects, consists of 4 conditions:
1. The action must be intrinsically good, independent of its consequences.
2. Although the bad effect of the action can be foreseen, the agent must directly intend only the good effect.
3. The bad effect must not be a means to the good effect.
4. The good effect must be proportional to, compensate for or outweigh the bad effect.
In many DCD programs, it is permissible to perform interventions on the patient to preserve the option of donation for the family, maximize the potential for useable organs or improve the function of organs once transplanted. If the intention is not to hasten the death of the donor but to preserve the organs to provide benefit to the recipient, then the doctrine of double effect can potentially apply.14
These interventions may include:
• Blood testing and relevant investigations for donor eligibility (ABO type, HLA-typing, virology screen, organ function evaluations)
• Preparation for vessel cannulation
• Isolation or exposure of vessels for cannulation
• Vessel cannulation for in-situ perfusion
• Administration of anticoagulants (heparin)
• Administration of vasodilators (phentolamine)
• Administration of thrombolytic agents (streptokinase)
• Extracorporeal oxygenation and circulation
• In-situ perfusion with cold preservation solution.
In controlled DCD (depending on the intervention), these interventions may occur:
• Before WLST
• After WLST, but before death
• In the interval between the onset of cardiocirculatory arrest and the formal determination of death
• After the determination of death.
When discussing whether these interventions are permissible, it is important to consider:
• Evaluation of benefit, i.e., does it contribute to successful donation?
• Evaluation of foreseeable harm or risk:
- Interventions that do not involve greater than minimal harm or risk and thus do not require detailed consent
- Interventions that involve a minor increase over minimal harm or risk and thus require detailed consent
- Interventions that involve a significant increase over minimal harm or risk and thus should not be offered.
Pharmacotherapy: anticoagulants, vasodilators, thrombolytics
Heparin is administered as an anticoagulant to prevent thrombotic obstruction of blood vessels, which can occur after the arrest of circulation. Heparin may be associated with bleeding risk and is contraindicated in the presence of active bleeding. Phentolamine is a vasodilator (blood vessel relaxant) intended to enhance organ blood flow. It may be associated with a transient decrease in blood pressure. Streptokinase is a thrombolytic agent that dissolves existing clots that may interfere with organ perfusion and is associated with a higher risk of bleeding than heparin.
For these drugs to be effective, intact circulation (before death) is required for their systemic distribution, although some centres administer them after death in the preservation solution. Ethical concerns arise over therapies that have no direct benefit to the patient and where there is a theoretical but small risk. Practice is not uniform and no trials have been done to evaluate dosage, timing of administration (pre-mortem v. post-mortem) or impact on transplantable organ function. Although not proven, pre-morbid heparin administration may lower the primary non-function and delayed graft functioning rates. IOM recommends full disclosure in consent discussions.
Ethical concerns have been addressed in the United States, and in all DCD programs heparin is administered before death and often before WLST. Phentolamine use is less common and the use of streptokinase is not well established. Many, but not all, European countries have followed the Maastricht policy precluding the use of medication that is not beneficial to the patient until after death.38,39
Re-establishment of circulation following death
Following declaration of death, some centres may also choose to re-introduce cardiopulmonary support in an effort to provide some degree of perfusion of targeted organs and oxygenation of the lungs. These measures may include re-intubation and cardiac compression (manual or machine) or extracorporeal membrane oxygenation. Although primarily applied to uncontrolled DCD, some centres are in the early phase of using extracorporeal membrane oxygenation in controlled DCD. We could not find any evidence base for any of these interventions. Medical and ethical concerns are related to re-establishing cerebral blood flow after cardiac arrest. Mechanical reperfusion and oxygenation of the brain after circulatory arrest and determination of death has the theoretical but unproven possibility of reanimating residual neurologic function.
Access for in-situ preservation
Vascular access, which is required for administration of cold preservation solution to maintain organ viability after death, may be secured by femoral vessel cannulation or directly by sternolaparotomy. Staged preparation for in-situ preservation may include
• Sterile preparation and draping of the surgical field
• Isolation of femoral vessels by surgical cutdown
• Cannulation of vessels.
6. Post-mortem care and interventions: uncontrolled DCD
6.1 Consent process
We recommend that:
a) The option of organ and tissue donation should be routinely provided after death in uncontrolled DCD to the families of potential donors.
b) The consent process (which should include acknowledgement of expressed donor intent, the identification of appropriate legal surrogate or the consent or refusal of donation) should be dictated by provincial legislation and current medical and ethical practice.
c) Expressed donor intent is legally sufficient to proceed with donation in the absence of proxy consent. However, it is recognized that the psychosocial, emotional and spiritual meaning of the act of donation will influence the decision-making process with families, even in the presence of a signed donor card or other indication of intent to donate.
d) In the absence of expressed donor intent and family consent, interventions and procedures for donation should not proceed.
e) Given its complexity, the consent process should be led by the most experienced person who can obtain the requisite informed consent and who is not part of the transplant team.
Key consideration
Expressed donor intent is considered legally to be a valid form of consent and is defined as a signed donor card or donor registry in the absence of any reason to believe the consent has been withdrawn. It is acknowledged that ethical or moral considerations may override the authority that the legal regime bestows.
Summaries of evidence
For uncontrolled DCD, the deceased has had a witnessed cardiocirculatory arrest of known duration and there should already be an established decision to terminate or not to initiate CPR. Management of uncontrolled DCD is complicated in that death is unanticipated and medical teams are unprepared for commencement of in-situ preservation. When death is sudden or unexpected, the relatives of the deceased or surrogate decision-makers are often not present and advance directives may not be immediately available. In North America, ideally informed consent before donation-based interventions should be sought. However, the wishes of the deceased may or may not be known and next of kin may be absent. Some jurisdictions, including some American states, have adopted laws that allow for in-situ preservation without consent (District of Columbia DC ST 2002; Florida Statutes 2002; Virginia State Code 2002). There are time constraints on these interventions, and it is possible that consent may not be available in a time frame that allows organ procurement. Despite legalization of these interventions, serious ethical questions regarding the appropriate conduct of physicians at the time of death remain an issue. Possible interventions include:
• Blood testing for donor eligibility (tissue typing, cross match, virology screen)
• Vessel cannulation
• In-situ perfusion
• Administration of anticoagulants
• Administration of vasodilators (phentolamine)
• Administration of thrombolytic agents (streptokinase)
• Re-institution of chest compression, mechanical ventilation
• Extracorporeal circulation and oxygenation
There are 2 schools of thought on the issue of in-situ preservation without prior consent. Minimization of warm ischemic time (WIT) preserves post-transplant organ function and provides the family with an opportunity to consider the merits of organ donation in a less hurried and somewhat less stressful environment. Given more time to consider the option, family support for DCD has been shown to dramatically increase if cannula insertion occurs before, rather than after, family consent.40 Nonetheless, ethical questions may arise when medical interventions are performed in the absence of prior informed consent from the deceased or the family. Public surveys in the United States have shown that 74% of respondents opposed allowing physicians to proceed with intravascular cannulation without prior consent.41 Many authors do not support these interventions, arguing that dignity of the dead is undermined by the unilateral decision of medical caregivers to proceed with these interventions.
In some uncontrolled DCD programs, it is permissible to perform interventions on the deceased to preserve the option of donation for the family, to maximize the availability of useable organs and improve the function of transplanted organs. To achieve these goals, the interventions may need to be started before family consent is given.
When discussing whether these interventions are permissible, it is important to consider the ethical justifications for intervening with a dead body to preserve options of the family for donation, respect for the body, principles of consent and the legal implications.
Re-establishment of circulation following death
Following declaration of death, some centres may also choose to re-introduce cardiopulmonary support to provide some degree of perfusion of targeted organs and oxygenation of the lungs. These measures may include re-intubation and cardiac compression (manual or machine) or extracorporeal membrane oxygenation. These interventions are primarily applied in cases of uncontrolled DCD in Spain. We could not find any evidence base for any of these interventions. As with controlled DCD, medical and ethical concerns are related re-establishing cerebral blood flow after cardiac arrest.
Legal
Under organ and tissue donation legislation, there is no legal reason for the family or proxy to be asked for consent when there is:
• A valid consent from the deceased donor and
• No reason to believe the consent has been withdrawn.
Many physicians are unaware that a signed donor card or other documentation of intent to donate is sufficient legal authority to allow them to retrieve organs after death. This applies in the absence of available family consent or in the face of family opposition. The proxy has no legal authority to give or refuse consent in the face of valid donor consent. However, in actual clinical practice, ethical, moral and family-based considerations may override the authority that the legal regime bestows.
There are potential legal consequences of donation-based interventions after death in uncontrolled DCD in the absence of preceding patient or family consent. Under the criminal code, criminal liability may apply when there is an offence of interference with a dead body (“improperly or indecently interferes with or offers any indignity to a dead human body or human remains, whether buried or not”).
7. Limits of organ viability: controlled and uncontrolled DCD
Ischemic organ injury during normothermia, as a result of hypotension and hypoxemia before death and circulatory arrest after death, has a direct impact on organ viability for transplantation and is a limiting factor in organ recovery in DCD. Even after the patient or family consents to controlled DCD, steps in the process may preclude donation. For example, the duration of the dying process might exceed the upper limits of organ viability in the context of transplantation. During the interval from WLST to death, patients who experience a slow progressive demise (hypotension and hypoxemia) may become unsuitable candidates for donation as organs can be irreparably damaged by warm ischemic injury during the dying process. In addition, there are time constraints related to logistic preparations. For example, the surgical procurement team, anesthetist and other operating room staff must be alerted and kept on hold until death is established.
7.1 Warm ischemic time (WIT)
We recommend that WIT be defined as:
• Initiation of WLST to cold perfusion in controlled DCD
• Cardiac arrest to cold perfusion in uncontrolled DCD.
Independent of definition and limits of WIT, we recommend that the following data and times be recorded for transplant purposes:
Controlled DCD
• The first action in WLST (e.g., weaning inspired oxygen)
• The final action in WLST (e.g., extubation)
• Urine output during WLST
• First fall in systolic blood pressure below 50% of baseline
• First fall in oxygen saturation below 80%
• Onset of circulatory arrest
• The 5-minute interval
• Determination of death (physician 1 and physician 2)
• Initiation of cannulation (femoral or sternolaparotomy)
• Initiation of cold perfusion of organs
Uncontrolled DCD
• Time from cardiac arrest to initiation of CPR
• Duration of CPR before death determination
• Determination of death (physician 1 and physician 2)
• Initiation of cold perfusion of organs
Key considerations
• The process of WLST varies among hospitals and ICU practitioners; the terminal events in the process of dying also vary among individual patients.
• Documentation of physiologic events during WLST is important when organs may be used for transplantation.
7.2 Maximum time for offering organs
We recommend that the maximum time beyond which organs should not be offered for controlled or uncontrolled DCD be determined by local transplant program protocol and experience.
Key considerations
• According to current practice, the maximum time for offering organs is approximately 2 h (2 h for kidneys, 1 h for pancreas and lungs, 30 minutes for liver).
• Other variables important in the time limit include (but are not limited to) age and comorbidity of the donor and agonal events during WLST.
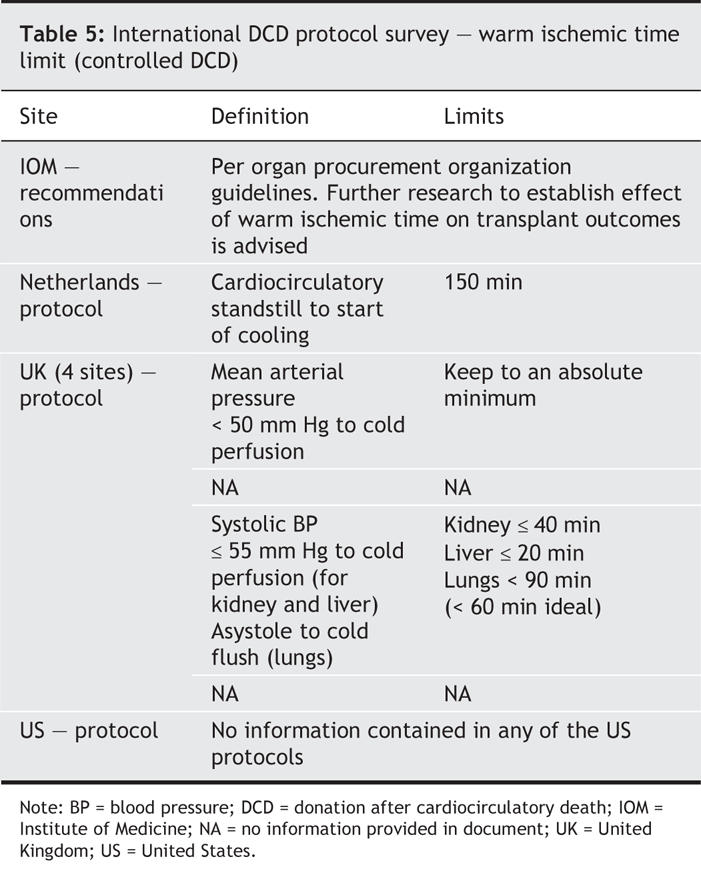
Summaries of evidence
Ischemic organ injury has a direct impact on organ viability for transplantation and is a limiting factor in organ recovery for DCD. This organ injury can be delayed by the use of hypothermia and preservation solutions. Definitions of WIT in controlled DCD vary in the literature (Table 5); WIT has been defined as:
Table 5
• The time from cardiocirculatory arrest to cold perfusion of the organs
• The time until a fall in physiologic parameters (blood pressure and oxygenation) below a predetermined level to cold perfusion of the organs or
• The time from WLST to cold perfusion.
Although there is general agreement that WIT should be minimized, various allowable time limits for WIT related to kidney transplantation have been recommended, most ranging from 30 to 45 minutes.42–44 However, longer WITs have resulted in satisfactory functional graft recovery in animal models for NHB kidney transplantation.45 This suggests that setting an absolute threshold for WIT is difficult. In clinical practice, other parameters such as the age and general health of a prospective NHB donor and the temporal progression of organ ischemia during the dying process are relevant.
Not all transplant teams share the opinion that WIT is of primary importance. Alonso and colleagues46 argued that a still-to-be-defined allowable period of warm ischemia does not alter outcomes in NHB renal grafting. Although they reported significantly increased rates of delayed graft functioning in their NHB donor kidneys where WIT > 2 h, 3-month recovery rates were no different. It seems inherently logical that the duration of warm ischemia is directly related to long-term transplant viability, but no evidence for this supposition could be identified during our review.
Among organs that may be transplanted, the lung is unique in its ability to withstand warm ischemia. Because of its histologic structure, consisting primarily of elastic tissue, the lung has minimal metabolic requirements. Furthermore, the alveolocapillary membrane of the lung can meet its requirements for oxygen through direct diffusion. Potential controlled NHB lung donors would be intubated and typically ventilated with oxygen, thereby maintaining the saturation of intrapulmonary blood. Furthermore, the pulmonary endothelium is also capable of functioning for several hours following circulatory arrest. For reasons not described in the reviewed literature, this continued functioning prevents clot formation following cardiac death. Although systemic heparin was administered to the donor patient described in the report by Steen and co-workers,47 many centres performing NHB lung transplantation no longer routinely administer heparin to the donor. In addition to traditional eligibility requirements for NHB organ donation, Steen and co-workers' only other mandatory requirement was that cooling should be initiated within 60 minutes of witnessed arrest or failed resuscitation.
8. Preservation techniques: controlled and uncontrolled DCD
8.1 In-situ techniques for preservation
We recommend that the preferred in-situ technique for preservation in both controlled and uncontrolled DCD be determined by local transplant program protocols and experience.
Key consideration
This recommendation depends on pre-mortem interventions (e.g., cannulation), surgical preferences (e.g., femoral cannulation v. sternolaparotomy) and logistics.
8.2 Ex situ kidney storage
We recommend that machine pulsatile perfusion be available at institutions offering DCD programs where kidneys must be stored ex situ.
Key consideration
Although no prospective studies have compared storage techniques, limited evidence suggests that machine pulsatile perfusion (MPP) is the preferred organ preservation technique as it may permit viability testing and may enhance organ viability.
Summaries of evidence
There are 2 primary means by which the kidney may be preserved following explantation: cold static storage and MPP. MPP was developed before the 1970s and became prevalent thereafter. The technique suffers from several disadvantages, including the cost of the device and consumables, the risk of machine failure and the requirements for an operating technician. MPP was subsequently largely abandoned when no evidence could be found for improved long-term outcome with MPP v. cold storage alone.48
Following a period of enthusiasm for cold storage alone, attention shifted back to the use of MPP in the belief that it might dimish rates of delayed graft function. There was evidence to suggest that delayed graft function contributed substantially to the cost of post-transplant care, increasing requirements for dialysis and lengthening hospital stays. Later reports suggested that it might also contribute to poorer long-term outcomes.49 All of these factors created renewed interest in MPP. Wight and colleagues50 undertook a meta-analysis to determine the effectiveness of MPP relative to cold storage. Although they found that high-quality studies were lacking, they concluded that MPP results in a 20% reduction in delayed graft function in both NHB and heart-beating kidney donation with diminished cost requirements for the care of the transplant recipient when compared with those for patients when cold storage was used.
For donors after brain death, a retrospective United Network for Organ Sharing analysis of 60 827 cadaveric kidneys transplanted between 1988 and 1995 in the United States showed that MPP exhibited a highly significant impact on the need for first-week dialysis and the benefit was increased in high-risk groups (age > 55 years, cold ischemic time > 24 h).51
The benefits of MPP may be related to:
• The continuous delivery of fresh solution to the allograft
• The ability to measure renal resistive indices52
• The ability to measure metabolites such as glutathione S transferase in the perfusate, which are correlated with the extent of renal tubular injury.53
9. DCD programs — Overarching recommendations for jurisdictions
9.1 Initiating a DCD program
We recommend the following before initiating a DCD program:
a) Formal institutional approval within the existing hospital reporting structure
b) An integrated, collaborative approach involving
• Consultation and involvement of hospital stakeholders (e.g., emergency department, ICU, operating room, risk management, pastoral care, bioethics)
• Communication, information and education of staff (e.g., emergency department, ICU, operating room, risk management, pastoral care, bioethics).
• Communication, information and education of the public.
c) Established quality assurance procedures in organ and tissue programs after NDD and tissue donation after cardiocirculatory death
d) Formal support of and collaboration with the regional organ donation organization
e) A risk management plan for DCD centres and partners.
We recommend that the following be in place to start an institutional DCD program:
a) Full-time emergency department (for uncontrolled DCD) and ICU (for controlled DCD) facilities
b) Established end-of-life care protocols
c) An established and effective program in organ donation after NDD
d) Availability of a procurement team
e) Structured support from regional organ procurement organizations.
Measures should be taken to ensure that concerns (real and perceived) for the safety of patients and the public, protection of health care workers and preservation of the integrity of the donation system are safeguarded. These measures may include:
• Auditing by an independent organization (analogous to a data safety monitoring board or research ethics board) or an internal health region or hospital based multidisciplinary group, or both.
• Approval of programs by the regional coroners or medical examiners.
9.2 Initial focus of a DCD program
We recommend that:
a) Centres initiating a DCD program start with kidney donation and expand to include other organs as experience and expertise develop.
b) In their initiation phase, centres proceed only with controlled DCD. Uncontrolled DCD should not be initiated until controlled DCD programs are well established with demonstrated quality assurance.
Key considerations
• Site visits to centres with established programs are advisable.
• Expansion depends on local physician expertise and the development of related programs.
• Centres must have adequate quality controls.
• Some centres may prefer to focus on any organs that may reasonably be used.
Conclusion
A principal objective of this forum was to discuss how to provide the opportunity and establish processes for implementing DCD without compromising patient interests and family support. At the conclusion of the forum, a strong majority of participants supported Canadian donation and transplantation programs proceeding with DCD under the medical, bioethical and legal framework articulated and enabled by these recommendations. It is understood that these are recommendations for minimum standards. Individual regions or programs may adopt, adapt or consider additional standards as they apply to their health care environments.
Acknowledgments
We gratefully acknowledge the collaboration of the Canadian Critical Care Society, the Canadian Association of Transplantation and the Canadian Society of Transplantation and the process consultation provided by Strachan-Tomlinson and Associates. We cannot overstate the contribution from our international clinical experts including Drs. Anthony D'Allessandro, Michael DeVita, Gauke Kootstra, Paolo Muiesan, José Nuñez Peña and Richard Hasz. We would like to thank Dr. Christopher Doig, in his role as co-chair, for his contribution to the planning of the forum and advice to the Forum Recommendations Group. We thank the following people who provided advice to the Steering and Planning Committees and the Forum Recommendations Group: Bill Barrable and Penny Clarke-Richardson (British Columbia Transplant Society), Dr. Cameron Guest and Clare Payne (Trillium Gift of Life Network), Karen Hornby (Montreal Children's Hospital), Dr. Peter Horton (Royal Victoria Hospital), Bashir Jiwani (Bioethics), Dr. Ronald Moore (University of Alberta Hospitals), Kathy O'Brien (Cassells Brock). We would like to acknowledge the contributions of Karen Hornby, Dr. Jeff Zaltzman, Dr. Len Baron and Kathy O'Brien in providing substantive topic reviews for the planning and steering committees.
APPENDIX
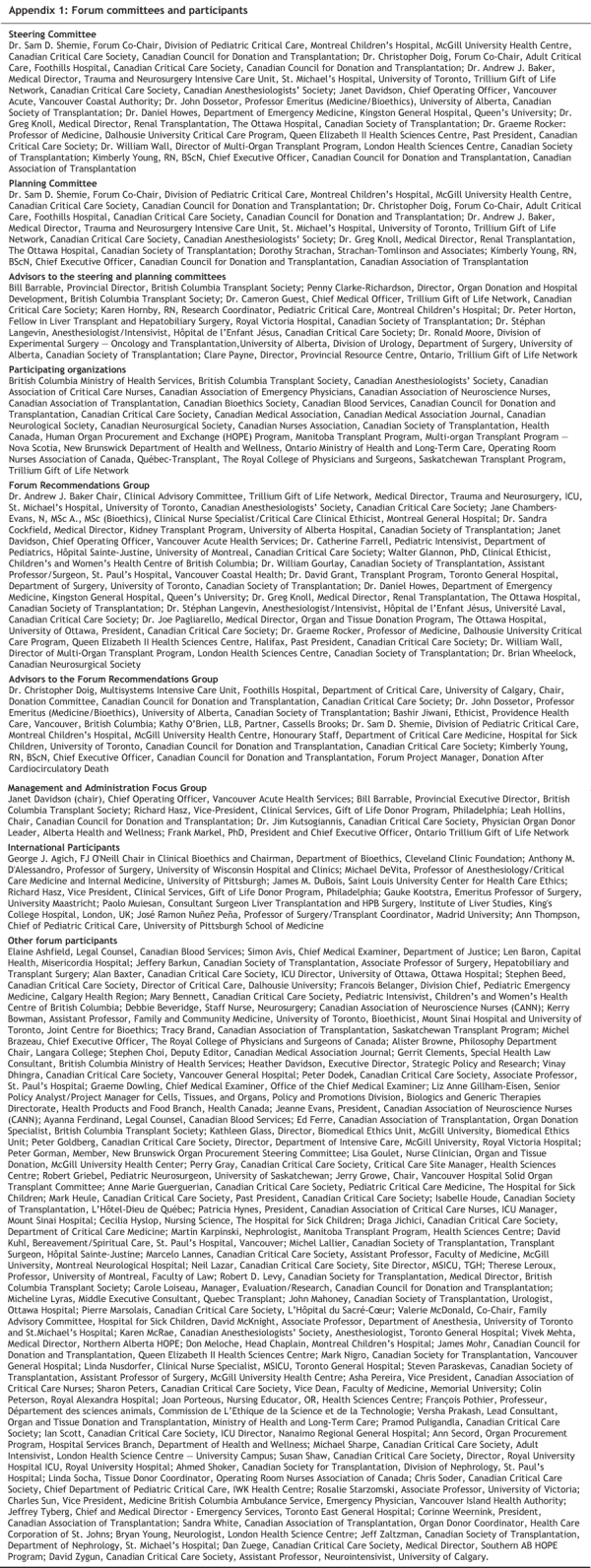
Appendix 1.
APPENDIX
Appendix 2.
APPENDIX
Appendix 3.
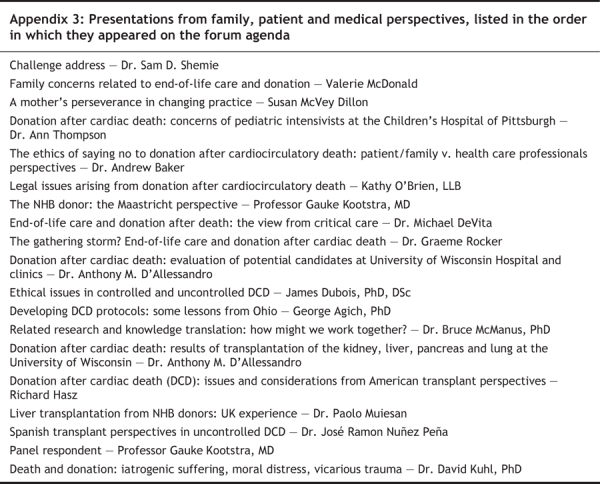
APPENDIX
Appendix 4.
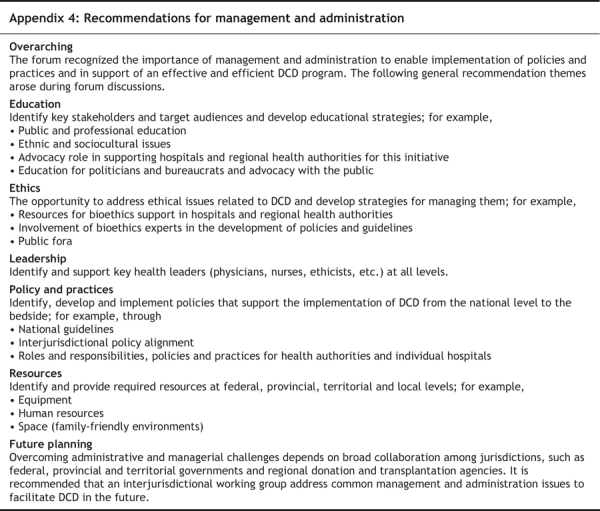
APPENDIX
Appendix 5.
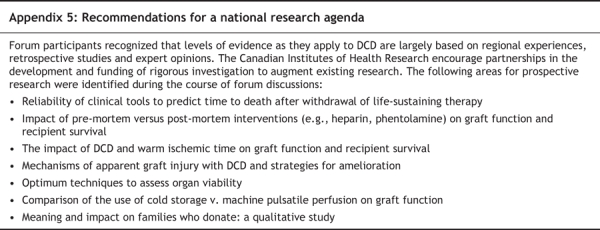
Footnotes
This article was reviewed through the consensus process of the Canadian forum “Donation after Cardiocirculatory Death,” which was convened by the Donation Committee of the Canadian Council for Donation and Transplantation. The final decisions were made by the Forum Recommendations Group.
This work was funded by the Canadian Council for Donation and Transplantation. Production of this report was made possible through a financial contribution from Health Canada. The views expressed herein do not necessarily represent the views of the federal, provincial or territorial governments.
Competing interests: None declared.
Correspondence to: Dr. Sam D. Shemie, Division of Pediatric Critical Care, Montreal Children's Hospital, McGill University Health Centre, Montréal QC H3H 1P3; sam.shemie@muhc.mcgill.ca
Reprint requests to: Communications Department, Canadian Council for Donation and Transplantation, 1702–8215 112 Street, Edmonton AB T6G 2C8; il:info@ccdt.ca
REFERENCES
- 1.Knoll GA, Mahoney JE. Non-heart-beating organ donation in Canada: Time to proceed? CMAJ 2003;169(4):302–3. [PMC free article] [PubMed]
- 2.Rocker G. Organ and tissue donation in the intensive care unit. CMAJ 2002; 167(11): 1248–9. [PMC free article] [PubMed]
- 3.Gouvernement du Québec. Rapport de consultation sur les enjeux éthiques du don et de la transplantation d'organes : resultats des entrevues de groupes et du mini-sondage réalisé dans le cadre de l'Enquête Statmédia du printemps 2004. Sainte-Foy, Québec: Commission de l'éthique de la science et de la technologie; 2004.
- 4.Shemie SD, Doig C, Dickens B, et al. Severe brain injury to neurological determination of death: Canadian forum recommendations. CMAJ 2006;174(6):S1–12. [DOI] [PMC free article] [PubMed]
- 5.Shemie SD, Ross H, Pagliarello J, et al. Organ donor management in Canada: recommendations of the forum on Medical Management to Optimize Donor Organ Potential. CMAJ 2006;174(6):S13–32. [DOI] [PMC free article] [PubMed]
- 6.Kootstra G, Daemen JH, Oomen AP. Categories of non-heart-beating donors. Transplant Proc 1995;27(5):2893–4. [PubMed]
- 7.Freeman R, Giatras I, Falagas ME, et al. Outcome of transplantation of organs procured from bacteremic donors. Transplantation 1999;68(8):1107–11. [DOI] [PubMed]
- 8.Heineman E, Daemen JH, Koostra G. Non-heart-beating donors: methods and techniques. Transplant Proc 1995;27(5):2895–7. [PubMed]
- 9.Brook NR, Waller JR, Nicholson ML. Non-heart-beating kidney donation: current practice and future developments. Kidney Int 2003;63(4):1516–29. [DOI] [PubMed]
- 10.Wood KE, Becker BN, McCartney JG, et al. Care of the potential organ donor. N Engl J Med 2004;351(26):2730–9. [DOI] [PubMed]
- 11.Hattori R, Ono Y, Yoshimura N, et al. Long-term outcome of kidney transplant using non-heart-beating donor: multicenter analysis of factors affecting graft survival. Clin Transplant 2003;17(6):518–21. [DOI] [PubMed]
- 12.Guidelines for the determination of death. Report of the medical consultants on the diagnosis of death to the President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. JAMA 1981; 246(19): 2184–6. [PubMed]
- 13.Robertson JA. The dead donor rule. Hasting Cent Rep 1999;29(6):6–14. [PubMed]
- 14.Veatch R. Transplantation ethics. Washington: Georgetown University Press; 2000.
- 15.Institute of Medicine, Herdman R, Potts J. Non-heart-beating organ transplantation: medical and ethical issues in procurement. Washington: National Academy Press; 1997. [PubMed]
- 16.Ethics Committee, American College of Critical Care Medicine, Society of Critical Care Medicine. Recommendations for nonheartbeating organ donation: a position paper by the Ethics Committee, American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 2001;29(9):1826–31. [DOI] [PubMed]
- 17.Menikoff J. The importance of being dead: non-heart-beating organ donation. Issues Law Med 2002;18(1):3–20. [PubMed]
- 18.Baker JD, Gluecklich B, Watson CW, et al. An evaluation of electroencephalographic monitoring for carotid study. Surgery 1975;78(6):787–94. [PubMed]
- 19.Hossmann KA, Kleihues P. Reversibility of ischemic brain damage. Arch Neurol 1973; 29(6):375–84. [DOI] [PubMed]
- 20.Moss J, Rockoff M. EEG monitoring during cardiac arrest and resuscitation. JAMA 1980; 244(24):2750–1. [PubMed]
- 21.Losasso TJ, Muzzi DA, Meyer FB, et al. Electroencephalographic monitoring of cerebral function during asystole and successful cardiopulmonary resuscitation. Anesth Analg 1992;75(6):1021–4. [DOI] [PubMed]
- 22.McIntyre A. Doctrine of double effect. In: Zalta EN, editor. The Stanford encyclopedia of philosophy. Fall 2004 edition. Available: http://plato.stanford.edu/archives/fall2004/entries/double-effect/ (accessed 10 Jul 2006).
- 23.Lewis J, Peltier J, Nelson H, et al. Development of the University of Wisconsin donation after dardiac death evaluation tool. Prog Transplant 2003;13(4):265–73. [DOI] [PubMed]
- 24.Wood GG, Martin E. Withholding and withdrawing life-sustaining therapy in a Canadian intensive care unit. Can J Anaesth 1995;42(3):186–91. [DOI] [PubMed]
- 25.Hall RI, Rocker GM, Murray D. Simple changes can improve conduct of end-of-life care in the intensive care unit. Can J Anaesth 2004;51(6):631–6. [DOI] [PubMed]
- 26.Keenan SP, Busche KD, Chen LM, et al. Withdrawal and withholding of life support in the intensive care unit: a comparison of teaching and community hospitals. Crit Care Med 1998;26(2):245–51. [DOI] [PubMed]
- 27.Asch DA, Faber-Langendoen K, Shea JA, et al. The sequence of withdrawing life-sustaining treatment from patients. Am J Med 1999;107(2):153–6. [DOI] [PubMed]
- 28.Cook DJ, Giacomini M, Johnson N, et al. Life support in the intensive care unit: a qualitative investigation of technological purposes. CMAJ 1999;161(9):1109–13. [PMC free article] [PubMed]
- 29.Rocker GM, Heyland DK, Cook DJ, et al. Most critically ill patients are perceived to die in comfort during withdrawal of life support: a Canadian multicentre study. Can J Anaesth 2004;51(6):623–30. [DOI] [PubMed]
- 30.Hall RI, Rocker GM. End-of-life care in the ICU: treatments provided when life support was or was not withdrawn. Chest 2000;118(5):1424–30. [DOI] [PubMed]
- 31.Zawistowski CA, DeVita MA. Non-heartbeating organ donation: a review. J Intensive Care Med 2003;18(4):189–97. [DOI] [PubMed]
- 32.Snell GI, Levvey BJ, Williams TJ. Non-heart-beating organ donation. Intern Med J 2004; 34(8):501–3. [DOI] [PubMed]
- 33.Cooper JT, Chin LT, Krieger NR, et al. Donation after cardiac death: the University of Wisconsin experience with renal transplantation. Am J Transplant 2004; 4(9): 1490–4. [DOI] [PubMed]
- 34.Van Norman GA. Another matter of life and death: what every anesthesiologist should know about the ethical, legal, and policy implications of the non-heart-beating cadaver organ donor. Anaesthesiology 2003;98(3):763–73. [DOI] [PubMed]
- 35.Truog RD. Organ donation after cardiac death: What role for anesthesiologists? Anaesthesiology 2003;98(3):599–600. [DOI] [PubMed]
- 36.Youngner SJ, Arnold RM, DeVita MA. When is death? Hastings Cent Rep 1999;29(6):14–21. [PubMed]
- 37.Truog R. Is it time to abandon brain death? Hastings Cent Rep 1997;27(2):29–37. [PubMed]
- 38.Sudhindran S, Pettigrew GJ, Drain A, et al. Outcome of transplantation using kidneys from controlled (Maastricht category 3) non-heart-beating donors. Clin Transplant 2003;17(2):93–100. [DOI] [PubMed]
- 39.Koffman G, Gambaro G. Renal transplantation from non-heart-beating donors: a review of the European experience. J Nephrol 2003;16(3):334–41. [PubMed]
- 40.DeVita MA, Snyder JV, Grenvik A. History of organ donation by patients with cardiac death. Kennedy Inst Ethics J 1993;3(2):113–29. [DOI] [PubMed]
- 41.Seltzer DL, Arnold RM, Siminoff LA. Are non-heart-beating cadaver donors acceptable to the public? J Clin Ethics 2000;11(4):347–57. [PubMed]
- 42.Light JA, Kowalski AE, Ritchie WO, et al. New profile of cadaveric donors: What are the kidney donor limits? Transplant Proc 1996;28(1):17–20. [PubMed]
- 43.Haisch C, Green E, Brasile L. Predictors of graft outcome in warm ischemically damaged organs. Transplant Proc 1997;29(8):3424–5. [DOI] [PubMed]
- 44.Orloff MS, Reed AI, Erturk E, et al. Nonheartbeating cadaveric organ donation. Ann Surg 1994;220(4):578–83. [DOI] [PMC free article] [PubMed]
- 45.Matsuno N, Kozaki K, Degawa H, et al. Importance of machine perfusion flow in kidney preservation. Transplant Proc 1999;31(5):2004–5. [DOI] [PubMed]
- 46.Alonso A, Buitron J, Gomez M, et al. Short-and long-term results with kidneys from non-heart-beating donors. Transplant Proc 1997;29(1–2):1378–80. [DOI] [PubMed]
- 47.Steen S, Sjoberg T, Pierre L, et al. Transplantation of lungs from a non-heart-beating donor. Lancet 2001;357(9259):825–9. [DOI] [PubMed]
- 48.Opelz G, Terasaki PI. Advantage of cold storage over machine perfusion for preservation of cadaver kidneys. Transplantation 1982;33(1):64–8. [DOI] [PubMed]
- 49.Cecka JM, Terasaki PI. The UNOS scientific renal transplant registry. United Network for Organ Sharing. Clin Transpl 1995;5:1–18. [PubMed]
- 50.Wight J, Chilcott J, Holmes M, et al. The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors. Health Technol Assess 2003;7(25):1–94. [DOI] [PubMed]
- 51.Burdick JF, Rosendale JD, McBride MA, et al. National impact of pulsatile perfusion on cadaveric kidney transplantation. Transplantation 1997;64(12):1730–3. [DOI] [PubMed]
- 52.Kootstra G, Kievit J, Nederstigt A. Organ donors: heartbeating and non-heartbeating. World J Surg 2002;26(2):181–4. [DOI] [PubMed]
- 53.Daemen J, Oomen A, Janssen M, et al. Glutathione S-transferase as predictor of functional outcome in transplantation of machine-preserved non-heart-beating donor kidneys. Transplantation 1997;63(1):89–93. [DOI] [PubMed]
- 54.Institute of Medicine. Non-heart-beating organ transplantation: practice and protocols. Washington: National Academy Press; 2000. [PubMed]