Iron availability is a critical factor in the growth of Mucorales (5). Here we report the novel use of deferasirox (Exjade; Novartis), an iron chelator recently approved by the U.S. Food and Drug Administration for the treatment of transfusion-related iron overload (3), as salvage therapy for a patient with progressive rhinocerebral mucormycosis.
A 40-year-old man presented to an outside hospital with diabetic ketoacidosis, left retrobulbar pain, and a left cranial nerve VI palsy. The patient developed complete left ophthalmoplegia, blindness, and worsening proptosis. He received amphotericin B lipid complex, but no surgery was performed.
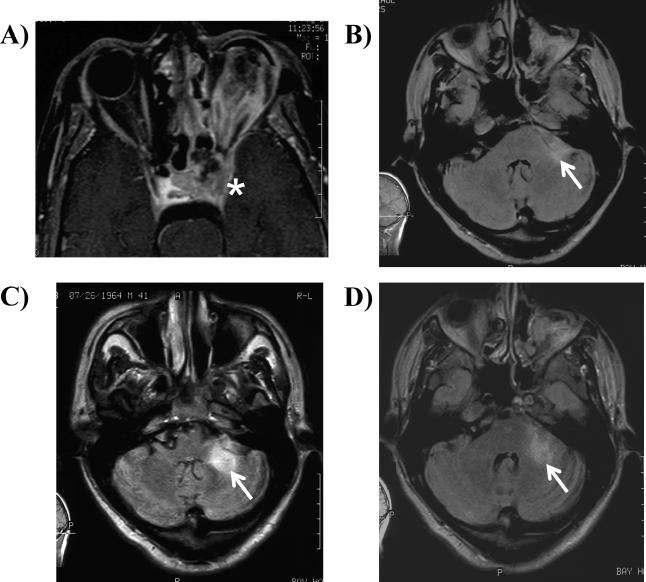
The patient was transferred to our institution on day 14 and underwent immediate left orbital exenteration, revealing an ischemic globe with extensive necrosis of the extraocular muscles. Frozen sections revealed broad, aseptate hyphae branching at 90°, typical of Mucorales; fungal cultures were negative. The patient was started on liposomal amphotericin B (LAmB) at 15 mg/kg of body weight/day and caspofungin at 70 mg/day (based on mouse data demonstrating polyene-echinocandin synergy) (6). Postoperatively, a magnetic resonance imaging (MRI) scan confirmed the presence of left cavernous sinus thrombosis (Fig. 1A).
FIG. 1.
(A) T1-weighted fat-saturated postgadolinium MRI obtained after left orbital exenteration. This is an axial image through the orbits and cavernous sinus, demonstrating abnormal enhancement in the left orbit, absence of normal flow void in the left carotid artery, and abnormal signal within the left cavernous sinus (asterisk). (B) MRI with fluid attenuated inversion recovery (FLAIR), 5 months after diagnosis, showing a small focus of abnormal signal (arrow) in the anterior aspect of the left cerebellar hemisphere. (C) MRI with FLAIR showing the interval development of a large area of abnormal signal (arrow) in the anterior aspect of the left cerebellar hemisphere after 8 months of treatment with liposomal amphotericin B. (D) MRI with FLAIR showing significant reduction in the amount of abnormal signal (arrow) 1 week after treatment with deferasirox.
Over the next several months, MRIs revealed new enhancement of cranial nerve V and a new lesion in the pons and left cerebellum (Fig. 1B). Because of worsening renal insufficiency (serum creatinine of >4.5 mg/dl versus a baseline of 0.8 mg/dl), the dose of LAmB was eventually titrated down to once weekly (∼day 210). A subsequent MRI (∼day 240) showed significant increase in size and enhancement of the left cerebellar signal consistent with progressive mucormycosis (Fig. 1C). A 7-day course of salvage deferasirox was administered orally at a dose of 1,000 mg (∼15 mg/kg) daily. Repeat MRI of the brain 1 week after conclusion of deferasirox treatment demonstrated significant improvement in cerebellar disease (Fig. 1D). LAmB was discontinued. Four months after the end of all antifungal therapy (∼day 400), the patient has remained asymptomatic, neurologically intact, and without radiographic changes on serial MRIs of the brain.
The potential therapeutic role of iron chelation therapy for mucormycosis was initially obscured by the paradoxically increased risk of developing mucormycosis during treatment with deferoxamine (1). However, Mucorales fungi are able to specifically bind to deferoxamine-iron complexes, strip the iron from the chelator through a reductive process, and facilitate iron uptake (1). Animal models have shown that other iron chelators do not act as iron siderophores for Mucorales. Specifically, treatment of mucor-infected mice (4) or guinea pigs (2) with deferiprone markedly improved survival. These data suggested that iron chelation might be useful in the treatment of refractory mucormycosis.
In summary, we describe a patient with advanced brainstem and cavernous sinus mucormycosis, who had significant progression radiographically despite months of polyene treatment but had a successful outcome after salvage deferasirox was added. The precise effect of the deferasirox treatment is confounded by concurrent polyene therapy. Nevertheless, given the encouraging results in this case, additional study of iron chelation in treatment of mucormycosis is warranted.
(This case was reported in part at the 16th Congress of the International Society for Human and Animal Mycology [ISHAM] meeting in Paris, France, June 2006.)
Acknowledgments
This work was supported by Public Health Service grants R01 AI063503-01A2 and R21 AI064716-01A2 and a research and educational grant from Gilead Sciences, Inc., to A.S.I. B.S. is supported by Public Health Service grant K08 AI060641 and AHA grant 012435. J.E.E. is supported by R01 AI19990 and AI063382 and an unrestricted Freedom to Discover Grant for Infectious Disease from Bristol Myers Squibb. A.S.I. is also supported by a Burroughs Wellcome New Investigator Award in Molecular Pathogenic Mycology.
There are no conflicts of interest for the authors of this letter.
Footnotes
Published ahead of print on 25 September 2006.
REFERENCES
- 1.Boelaert, J. R., M. de Locht, J. Van Cutsem, V. Kerrels, B. Cantinieaux, A. Verdonck, H. W. Van Landuyt, and Y. J. Schneider. 1993. Mucormycosis during deferoxamine therapy is a siderophore-mediated infection. In vitro and in vivo animal studies. J. Clin. Investig. 91:1979-1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boelaert, J. R., J. Van Cutsem, M. de Locht, Y. J. Schneider, and R. R. Crichton. 1994. Deferoxamine augments growth and pathogenicity of Rhizopus, while hydroxypyridinone chelators have no effect. Kidney Int. 45:667-671. [DOI] [PubMed] [Google Scholar]
- 3.Cappellini, M. D. 2005. Iron-chelating therapy with the new oral agent ICL670 (Exjade). Best Pract. Res. Clin. Haematol. 18:289-298. [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim, A. S., J. E. Edwards, Jr., Y. Fu, and B. J. Spellberg. 23 August 2006, posting date. Deferiprone iron chelation as a novel therapy for experimental mucormycosis. J. Antimicrob. Chemother. [Online.] doi: 10.1039/jac/dk1350. [DOI] [PubMed]
- 5.Spellberg, B., J. Edwards, Jr., and A. Ibrahim. 2005. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin. Microbiol. Rev. 18:556-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spellberg, B., Y. Fu, J. E. Edwards, Jr., and A. S. Ibrahim. 2005. Combination therapy with amphotericin B lipid complex and caspofungin acetate of disseminated zygomycosis in diabetic ketoacidotic mice. Antimicrob. Agents Chemother. 49:830-832. [DOI] [PMC free article] [PubMed] [Google Scholar]