Abstract
Insulin modulates glucose disposal in muscle and adipose tissue by regulating the cellular redistribution of the GLUT4 glucose transporter. Protein kinase Akt/PKB is a central mediator of insulin-regulated translocation of GLUT4; however, the GLUT4 trafficking step(s) regulated by Akt is not known. Here, we use acute pharmacological Akt inhibition to show that Akt is required for insulin-stimulated exocytosis of GLUT4 to the plasma membrane. Our data also suggest that the AS160 Rab GAP is not the only Akt target required for insulin-stimulated GLUT4 translocation. Using a total internal reflection microscopy assay, we show that Akt activity is specifically required for an insulin-mediated prefusion step involving the recruitment and/or docking of GLUT4 vesicles to within 250 nm of the plasma membrane. Moreover, the insulin-stimulated fusion of GLUT4 vesicles with the plasma membrane can occur independently of Akt activity, although based on inhibition by wortmannin, it is dependent on phosphatidylinositol 3′ kinase activity. Hence, to achieve full redistribution of GLUT4 into the plasma membrane, insulin signaling bifurcates to independently regulate both fusion and a prefusion step(s).
INTRODUCTION
Insulin regulates glucose uptake into muscle and fat cells by inducing the reversible redistribution of the GLUT4 glucose transporter from intracellular storage sites to the plasma membrane (PM) (Ishiki et al., 2005; Watson and Pessin, 2006). In unstimulated adipocytes, GLUT4 is excluded from the PM by a dynamic process involving slow exocytosis and rapid endocytosis. Insulin induces a net redistribution of GLUT4 to the PM by accelerating GLUT4 exocytosis and inhibiting its endocytosis (Govers et al., 2004; Karylowski et al., 2004; Martin et al., 2006). The exocytic steps regulated by insulin are not known and potentially include stimulation of the formation of GLUT4 transport vesicles (Xu and Kandror, 2002), mobilization of a pool of GLUT4 vesicles (Bogan et al., 2003), increased movement of GLUT4 vesicles (Bose et al., 2002; Semiz et al., 2003), increased docking at the PM of GLUT4 vesicles, and/or increased fusion of GLUT4 vesicles with the PM (Koumanov et al., 2005; Lizunov et al., 2005; van Dam et al., 2005).
Substantial evidence supports the serine/threonine protein kinase Akt/PKB as a crucial regulator of insulin-mediated GLUT4 redistribution (for review, see Watson and Pessin [2006]). Overexpression of a constitutively active mutant of Akt leads to the translocation of GLUT4 to the PM (Kohn et al., 1996), and inhibition of Akt by interfering antibodies, substrate peptides, or overexpression of a dominant-negative Akt construct partially blocks insulin-induced GLUT4 translocation (Hill et al., 1999; Wang et al., 1999). Of the three mammalian Akt isoforms, Akt2 is strongly correlated with the regulation of glucose homeostasis. Targeted disruption of Akt2, but not Akt1 or Akt3, resulted in impaired insulin-regulated glucose uptake (Cho et al., 2001; Bae et al., 2003).
Despite advances in our understanding of GLUT4 intracellular trafficking and strong evidence of Akt being a crucial regulator of insulin-induced GLUT4 redistribution, the specific input of Akt signaling to GLUT4 trafficking is not known. Recently, an allosteric Akt1 and Akt2 inhibitor, Akti-1/2, has been developed. This compound has been shown to inhibit Akt activation but not affect other AGC kinase family members (DeFeo-Jones et al., 2005; Zhao et al., 2005). Given the broad range of metabolic actions of Akt signaling, acute inhibition of insulin-induced Akt activation represents a useful tool to address the specific role of Akt signaling on GLUT4 trafficking. In this study, we use acute pharmacological inhibition and short hairpin RNA (shRNA)-mediated Akt knockdown to identify the steps in GLUT4 trafficking modulated by Akt signaling. We found that Akt is a crucial regulator of insulin-induced GLUT4 exocytosis, whereas insulin-regulated GLUT4 endocytosis is independent of Akt activation. Using total internal reflection fluorescence (TIRF) microscopy and a novel fusion assay, we show that along the exocytic pathway Akt regulates the insulin-mediated prefusion recruitment and/or docking of GLUT4 vesicles to the PM. In contrast, insulin-regulation of GLUT4 vesicle fusion with the PM is dependent on phosphatidylinositol 3′ kinase (PI3-kinase) activity but independent of Akt activity.
MATERIALS AND METHODS
Ligands and Chemicals
Fluorescent secondary antibodies were purchased form Jackson ImmunoResearch Laboratories (West Grove, PA). Antibodies against phospho-Akt (Ser473), Akt, Akt2, phospho-Akt substrate (PAS), phosho-glycogen synthase kinase (GSK)3β (Ser9), and extracellular signal-regulated kinase (ERK)1/2 were from Cell Signaling Technology (Beverly, MA). Antibodies against Akt1, cEBPα, and peroxisome proliferator-activated receptor (PPAR)γ were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). The GLUT4 antibody was a gift from Sam Cushman (National Institutes of Health, Bethesda, MD). The insulin-regulated aminopeptidase (IRAP) antibody was a gift from Susanna Keller (University of Virginia, Charlottesville, VA). Anti-AS160 antibody was a gift from Gustav Lienhard (Dartmouth Medical School, Hanover, NH). The isozyme selective Akt inhibitor AI1/2 (Akti-1/2) and the PI3-kinase inhibitor wortmannin were purchased from Calbiochem (San Diego, CA). Mouse anti-hemagglutinin (HA) epitope monoclonal antibody was purified from ascites (Covance, Berkley, CA) by using a protein G affinity column (GE Healthcare, Little Chalfont, Buckinghamshire, United Kingdom). The concentration of HA.11 required to saturate the HA epitope of HA-GLUT4-green fluorescent protein (GFP) was determined for each preparation of antibody as described previously (Karylowski et al., 2004).
Cell Culture and Electroporation
3T3-L1 fibroblast were cultured, differentiated into adipocytes, and electroporated as described previously (Zeigerer et al., 2002). The HA-GLUT4-GFP, IRAP-transferrin receptor (TR), and TR constructs have been described previously (Lampson et al., 2000; Subtil et al., 2000). Stable expression of HA-GLUT4 was achieved using the retroviral expression vector pBABE-Puro (Shewan et al., 2000; Karylowski et al., 2004). Cells were maintained at 37°C in 5% CO2, air during growth and differentiation and for all incubations in kinetic experiments. All experiments were conducted on day 6 after differentiation.
Drug Treatment, Cell Lysates, and Immunoblots
Cells were serum starved for 2 h in serum-free DMEM with 20 mM sodium bicarbonate, 20 mM HEPES, pH 7.2 (SF-DMEM) at 37°C in 5%CO2, air before all experiments. AI1/2 and wortmannin were dissolved in dimethyl sulfoxide and stored at −20°C.
For immunoblots, cells were washed with 150 mM NaCl, 20 mM HEPES, 1 mM CaCl2, 5 mM KCl, 1 mM MgCl2, pH 7.2 (media 1) and lysed in Laemmli buffer. Cells were harvested by scraping, and the lysates were sheared through a Q26G5/8 syringe. Proteins were resolved in SDS-PAGE, transferred to nitrocellulose membranes, and probed with antibodies by using protocols provided by the suppliers.
shRNA Retroviral Constructs
The pSIREN RetroQ system from Clontech (Mountain View, CA) was used according to manufacturer's instructions. The targeting sequences used for Akt1 and Akt2 were Akt1, 5′-AGAACCGTGTCCTGCAGAA-3′ and Akt2, 5′-CCATGAATGACTTCGATTA-3′, the nonspecific sequence used as negative control for shRNA activity and the targeting sequence used for AS160 have been described previously (Eguez et al., 2005). Hairpins were cloned into the pSIREN RetroQ vector, and AmphoPak-293 cells (Clontech) were transfected with the retroviral constructs. Media from the packaging cells were harvested and used to infect 3T3-L1 fibroblast. Infected cells were selected for growth in puromycin (Eguez et al., 2005).
Kinetic Studies
All live cell incubations were performed in SF-DMEM. Adipocytes were incubated in SF-DMEM for 2 h before insulin stimulation. Cells were preincubated with the Akt inhibitor 1 μM AI1/2 or vehicle for 1 h before insulin stimulation. For indirect immunofluorescence, cells were fixed with 3.7% formaldehyde, incubated with primary antibody in phosphate-buffered saline (PBS) and 5% calf serum for 30 min at 37°C, washed, and incubated with fluorescent secondary antibody in PBS, 5% calf serum. PBS with 5% calf serum and 250 μg/ml saponin was used for indirect immunofluorescence of permeabilized cells. The methods to measure translocation and kinetics have been described previously (Lampson et al., 2001; Zeigerer et al., 2002, 2004; Karylowski et al., 2004; Martin et al., 2006).
Fluorescence Quantification
Fluorescence microscopy was performed using a DMIRB inverted microscope (Leica Microsystems, Deerfield, IL) with a cooled charge-coupled device camera (Princeton Instruments, Trenton, NJ). Images were collected with a 40 × 1.25 numerical aperture oil immersion objective. MetaMorph software (Molecular Devices, Sunnyvale, CA) was used for image processing and quantification as described previously (Lampson et al., 2001; Zeigerer et al., 2002; Karylowski et al., 2004).
TIRF Microscopy
To measure GLUT4 translocation adipocytes were incubated in SF-DMEM medium for 3 h at 37°C in 5% CO2, air. Some cells were incubated with Akt inhibitor 1 μM AI1/2 during the last hour of this incubation or with the PI3-kinase inhibitor 100 nM wortmannin for 30 min before stimulation with 1 nM insulin for 30 min. Cells were fixed in 3.7% formaldehyde, and the insulin-induced GFP redistribution was determined using a total internal reflection fluorescence microscope. The TIRF microscope has been described previously (Moskowitz et al., 2003). A 60 × 1.45 numerical aperture oil immersion objective (Olympus America, Melville, NY) was used to perform “prism-less” TIRF. The evanescent field decay length was ∼250 nm with this objective, with a pixel size of 112 × 112 nm2 in the acquired images. Cells expressing HA-GLUT4-GFP were identified by GFP in epifluorescence mode of the microscope. Both epifluorescence and TIRF images of cells were acquired. The GFP fluorescence in the TIRF mode was divided by the GFP epifluorescence intensity, normalizing the TIRF fluorescence for the total HA-GLUT4-GFP expressed per cell. All images were corrected for background fluorescence measured in cells that did not express HA-GLUT4-GFP.
To measure insulin-induced HA-GLUT4 fusion, adipocytes stably expressing HA-GLUT4 were used. Two samples were prepared per experimental condition and cells were fixed and stained with anti-HA antibody followed by Cy3-labeled secondary antibody in the presence or absence of saponin. Epifluorescence and TIRF images were acquired. All images were corrected for background fluorescence measured in cells stained with Cy3-labeled secondary antibody. Fluorescence in TIRF mode in permeabilized cells was divided by total fluorescence in the epifluorescence mode to measure insulin-induced recruitment and docking of HA-GLUT4. Fluorescence in the TIRF mode in intact nonpermeabilized cells was divided by fluorescence in TIRF mode in permeabilized cells to measure insulin-induced HA-GLUT4 vesicle fusion. For each condition in each experiment, images of 10–15 fields were acquired (6–10 cells/field). The TIRF signal was between two and eightfold the background TIRF signal depending on the experimental conditions. The variance of total fluorescence in both epifluorescence and TIRF mode for the different fields in each experiment was <20% of the mean fluorescence value.
For live cell TIRF microscopy studies, cells were serum starved for 2 h in SF-DMEM at 37°C in 5% CO2, and incubated for 1 h in 1 μM AI1/2 or vehicle. Cells were allowed to equilibrate in the TIRF microscope equipped with a temperature-controlled objective at 37°C for 30 min. Videos were acquired at a rate of two frames per minute with a cooled charge-coupled device camera. Insulin was added to the samples after recording five frames. To quantify the insulin-induced recruitment of GLUT4 to the vicinity of the PM, TIR fluorescence in each frame was quantified, background was subtracted, and values were normalized to TIRF at time 0 and plotted as a function of time.
Hexose Transport
Hexose transport activity in 3T3-L1 adipocytes was measured by the uptake of [3H]2-deoxy-glucose as described previously (Gibbs et al., 1988).
RESULTS
Akt Inhibition Impairs Insulin-induced GLUT4 Translocation and Glucose Uptake in Adipocytes
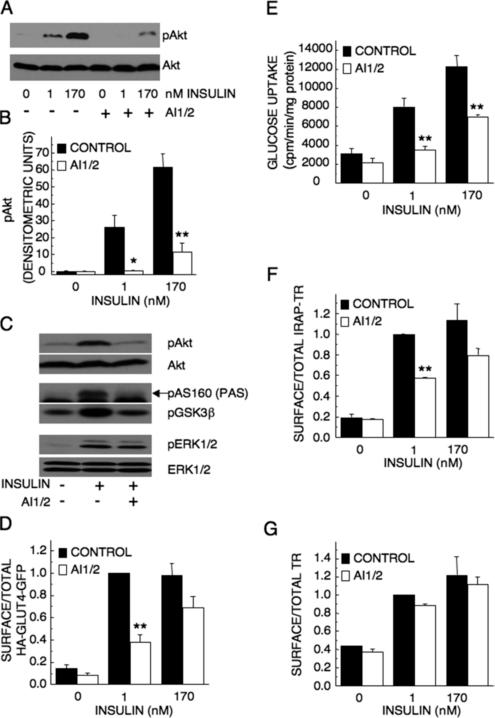
The effect of acute pharmacological inhibition of Akt activity on insulin-regulated GLUT4 trafficking and glucose transport has not been explored previously. Although overexpression of Akt mutants and down-regulation or knockout of Akt isoforms have all proved the importance of Akt activity on insulin-regulated GLUT4 redistribution, when studying the acute effect of insulin on GLUT4 redistribution, prolonged Akt inhibition could render confounding effects, considering the signaling potential of this kinase. We used the recently developed allosteric Akt1 and Akt2 inhibitor AI1/2 (Akti-1/2) to explore the role of insulin-induced Akt activation on GLUT4 redistribution and glucose uptake in 3T3-L1 adipocytes. Pretreatment of adipocytes for 1 h with 1 μM AI1/2 completely blocked the phosphorylation of Akt at Ser473 promoted by 1 nM insulin and partially inhibited Akt phosphorylation in cells stimulated with 170 nM insulin (Figure 1, A and B). AI1/2 (1 μM) was used in this study, because it was the lowest concentration of AI1/2 required to completely inhibit Akt phosphorylation induced by 1 nM insulin (our unpublished data). Insulin-induced phosphorylation of GSK3β and AS160, two targets of Akt action, was reduced by AI1/2, demonstrating that AI1/2 inhibited Akt activation. Insulin-stimulated phosphorylation of the mitogen-activated protein kinases ERK1/2, which is independent of Akt activation, was not affected by AI1/2, documenting that AI1/2 inhibited Akt signaling without having general inhibitory effects on signaling downstream of the insulin receptor.
Figure 1.
Inhibition of Akt impairs GLUT4 translocation and glucose uptake in 3T3-L1 adipocytes. (A) 3T3-L1 adipocytes were treated with 1 μM AI1/2 or vehicle for 1 h before insulin stimulation for 15 min. Cell lysates were analyzed in immunoblots by using noted antibodies. (B) Densitometric analyses from pooled immunoblot data. The means ± SE of three independent experiments are shown. (C) Immunoblot analyses of adipocytes stimulated with 1 nM insulin for 15 min. As noted, some samples were treated with 1 μM AI1/2 for 1 h before insulin stimulation. Phosphorylated AS160 (arrow) was detected with the PAS antibody. (D) Surface-to-total distribution of HA-GLUT4-GFP. Each bar is the mean ± SE of three independent experiments. The surface-to-total HA-GLUT4-GFP distribution was normalized to the distribution in cells stimulated with 1 nM insulin for 30 min. As noted, some samples were treated with 1 μM AI1/2 for 1 h before 30-min insulin stimulation. (E) Glucose uptake in adipocytes. Cells were treated with vehicle or 1 μM AI1/2 for 1 h before 30-min insulin stimulation. Each bar is the mean ± SE of four independent experiments. (F and G) Surface-to-total distribution of IRAP-TR chimera (F) and TR (G) in adipocytes. Cells were treated with vehicle or 1 μM AI1/2 for 1 h before 30-min incubation in insulin. Each bar is the mean ± SE of two independent experiments. The surface-to-total distributions were normalized to the distribution in control cells stimulated with 1 nM insulin. *p < 0.05, **p < 0.01 versus cells that were not treated with AI1/2 (analysis of variance [ANOVA]).
We used a HA-GLUT4-GFP reporter construct to characterize the role of Akt signaling in insulin-induced GLUT4 translocation. This construct contains an exofacial HA epitope and GFP fused to the carboxy-cytoplasmic domain (Lampson et al., 2000). The increase of HA-GLUT4-GFP in the PM is measured by an increase in HA epitope in the PM. Stimulation of adipocytes with insulin induced the redistribution of HA-GLUT4-GFP to the PM. Despite the significant difference in Akt phosphorylation induced by 1 and 170 nM insulin (Figure 1A), both insulin concentrations promoted a similar GLUT4 translocation to the PM, suggesting that Akt activation induced by 1 nM insulin, a physiological concentration of insulin, is sufficient to promote maximum effects on GLUT4 translocation in 3T3-L1 adipocytes (Figure 1D).
Insulin-induced redistribution of HA-GLUT4-GFP was significantly inhibited by 1 μM AI1/2 (Figure 1D). GLUT4 translocation stimulated by 1 nM insulin was reduced by 65 ± 6%, and translocation induced by 170 nM insulin was reduced by 30 ± 10%, establishing that acute inhibition of Akt activity by AI1/2 blunts insulin-stimulated GLUT4 translocation to the PM. Importantly, although AI1/2 treatment abolished 1 nM insulin-induced Akt phosphorylation (Figure 1A), it did not completely block GLUT4 translocation (Figure 1D), suggesting that signaling pathways other than Akt contribute to the full effect of insulin on GLUT4 redistribution to the PM.
AI1/2 inhibited insulin-stimulated 2-deoxy-glucose uptake, demonstrating that Akt activity is required for insulin-regulated glucose transport (Figure 1E). Thus, both the translocation data and the hexose uptake data support a prominent role for Akt signaling in insulin-regulation of GLUT4 trafficking in adipocytes. However, a comparison of GLUT4 translocation and insulin-stimulated 2-deoxy-glucose uptake at 1 nM insulin revealed an uncoupling of hexose transport from GLUT4 redistribution, because 1 nM insulin is sufficient for maximal translocation yet not for maximal hexose uptake (Figure 1, D and E). Because the GLUT1 transporter also contributes to insulin-stimulated glucose uptake in 3T3-L1 adipocytes, hexose uptake is not a direct measure of GLUT4 translocation. The discordance in GLUT4 in the PM and hexose uptake may reflect differences in insulin signaling to GLUT4 and GLUT1 (Yeh et al., 1995; Liao et al., 2006).
GLUT4/IRAP Trafficking but Not TR Trafficking Is Regulated by Akt Signaling
The only other protein known to traffic by the GLUT4 pathway is the aminopeptidase IRAP (Ross et al., 1997; Garza and Birnbaum, 2000). To explore whether Akt signaling is specifically required for insulin-induced GLUT4 redistribution or regulates the IRAP/GLUT4 pathway, we next determined the effect of AI1/2 inhibition of Akt on the behavior of IRAP. For these studies, we used an IRAP-transferrin receptor chimera (IRAP-TR) previously shown to traffic like IRAP in adipocytes (Subtil et al., 2000). Inhibition of Akt significantly impaired insulin-induced IRAP-TR translocation to the PM, consistent with the effects of AI1/2 on GLUT4 translocation (Figure 1F). Thus, AI1/2 inhibition of Akt activation affects insulin regulation of the GLUT4/IRAP trafficking pathway rather than specially alerting the behavior of GLUT4.
Insulin promotes a twofold increase of TR in the PM, documenting that insulin has effects on general membrane trafficking, albeit minor in magnitude compared with the effect on GLUT4 and IRAP. AI1/2 inhibition of Akt signaling did not have a significant effect on insulin-stimulated redistribution of the TR to the PM, establishing that although Akt signaling is involved in the regulation of the GLUT4/IRAP trafficking pathway, it is not required for the effect of insulin on general endocytic trafficking (Figure 1G). Thus, the insulin signaling pathway that affects general membrane recycling does not completely overlap with the signaling mechanism that regulates GLUT4/IRAP translocation.
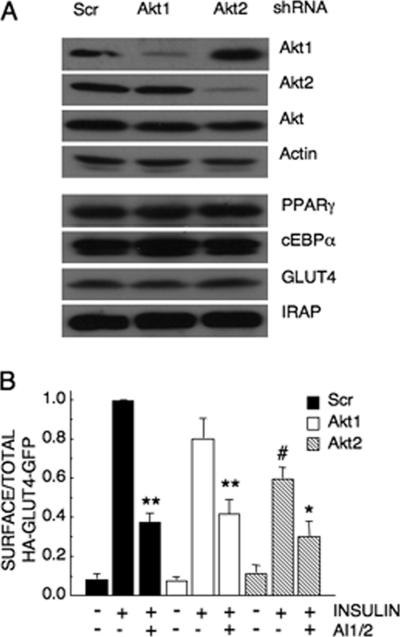
Akt2 Knockdown Impairs Insulin-induced GLUT4 Translocation
To further explore the role of Akt in insulin-regulated GLUT4 translocation, we individually knocked down Akt1 and Akt2 by using retroviral-delivered shRNA. Akt1 and Akt2 expression was significantly reduced by the isoform-specific shRNA (Figure 2A). Down-regulation of Akt1 or Akt2 did not reproducibly alter the expression level of the other isoform, nor did it alter differentiation into adipocytes, as determined by the expression of the differentiation markers PPARγ, cEBPα, GLUT4, and IRAP (Figure 2A).
Figure 2.
shRNA-mediated Akt knockdown impairs insulin-induced GLUT4 translocation. (A) Immunoblot analyses of extracts from adipocytes expressing scrambled, Akt1- or Akt2-specific shRNA. (B) Surface-to-total distribution of HA-GLUT4-GFP in control, Akt1, and Akt2 knockdown adipocytes. Insulin (1 nM) and 1 μM AI1/2 were used. Each bar is the mean ± SE of three independent experiments. In each experiment, the surface-to-total HA-GLUT4-GFP distribution was normalized to the distribution in control insulin-stimulated cells. *p < 0.05, **p < 0.01 versus cells that were not treated with AI1/2; #p < 0.01 versus insulin-stimulated control cells (ANOVA).
In Akt2 knockdown adipocytes, insulin-induced GLUT4 translocation was inhibited by 40 ± 6% (Figure 2B). The effect of Akt1 knockdown on GLUT4 translocation was not statistically significant, although the data trended toward a reduction in translocation (Figure 2B). These results show that Akt2 is the principal Akt isoform regulating GLUT4 trafficking, in agreement with previous studies (Bae et al., 2003; Jiang et al., 2003). Inhibition of Akt activity with AI1/2 further reduced GLUT4 translocation in Akt2 knockdown adipocytes, suggesting that the Akt in these cells, either Akt1 or residual Akt2, contributes to the effect of insulin on GLUT4 distribution. However, even in AI1/2-treated Akt2 knockdown adipocytes, insulin still promoted an approximately threefold redistribution of GLUT4 to the PM (Figure 2B). These data provide strong support for the hypothesis that insulin signals to GLUT4 by both Akt-dependent and -independent pathways.
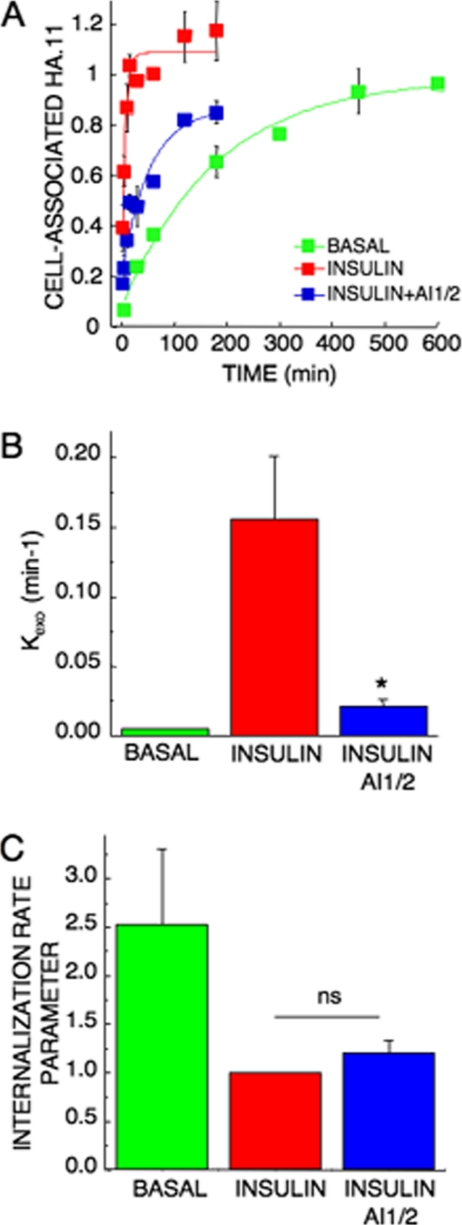
Akt Regulates Insulin-induced HA-GLUT4-GFP Exocytosis
We next determined whether Akt activation is required for insulin stimulation of HA-GLUT4-GFP exocytosis. Adipocytes expressing HA-GLUT4-GFP were stimulated with insulin for 30 min ± AI1/2, followed by incubation in medium containing anti-HA epitope antibody HA.11, insulin ± AI1/2. During the incubation, HA-GLUT4-GFP that appears on the PM binds HA.11 antibody in the medium; therefore, the rate at which cell-associated fluorescence increases over time of incubation is a measure of the exocytosis of HA-GLUT4-GFP (Figure 3A) (Karylowski et al., 2004). Because the appearance of the HA epitope on the cell surface, which is ultimately dependent on vesicle fusion, is monitored in this exocytosis assay, this assay does not distinguish between regulation of prefusion processes (e.g., docking) from regulation of vesicle fusion. AI1/2 treatment slowed insulin-stimulated GLUT4 exocytosis (appearance on the PM) by approximately sevenfold (Figure 3, A and B). In addition to slowing GLUT4 exocytosis, AI1/2 also reduced the plateau level reached in insulin-stimulated cells, indicating that a portion of intracellular GLUT4 did not cycle to the PM during the time frame of these experiments (Figure 3A).
Figure 3.
Akt regulates insulin-induced GLUT4 exocytosis but not insulin inhibition of GLUT4 internalization. (A) Steady-state basal and insulin-stimulated GLUT4 exocytosis kinetics in 3T3-L1 adipocytes. The data are the mean ± SE of three independent experiments for the insulin-stimulated state and two experiments for the basal state. Insulin (1 nM) and 1 μM AI1/2 were used. The lines are a fit of the data to (Cy3/GFP)t = (HA-GLUT4-GFP)plateau − [(HA-GLUT4-GFP)intracellular × (e−kexo*t)]; where Kexo is the exocytosis rate constant, t is the time of incubation, Cy3/GFP is cell-associated HA.11 at time t, (HA-GLUT4-GFP)plateau is the Cy3-to-GFP plateau level, and (HA-GLUT4-GFP)intracellular is the amount of HA-GLUT4-GFP intracellular at time 0. (B) Basal and insulin-stimulated GLUT4 Kexo in the presence or absence of AI1/2. Each bar is the mean ± SE of two or three independent experiments. *p < 0.05 compared with insulin-stimulated state in the absence of the Akt inhibitor (ANOVA). (C) Basal and insulin-stimulated GLUT4 internalization rate parameter in the presence or absence of AI1/2. Each bar is the mean ± SE of two to four independent experiments. The data are normalized to the internalization rate parameter measured for control cells in the insulin-stimulated state. The internalization rate parameter is proportional to the internalization rate constant but is not the rate constant, because different fluorophores are used to measure surface and internal HA-GLUT4-GFP.
AI1/2 inhibition of Akt did not completely abrogate the insulin stimulatory effects on GLUT4 exocytosis. In insulin-stimulated AI1/2-treated adipocytes, GLUT4 was exocytosed ∼3 times as fast as in basal adipocytes (Figure 3, A and B). These results demonstrate that although Akt signaling is required for insulin regulation of GLUT4 exocytosis, inhibition of Akt signaling is not sufficient to completely block the effects of insulin on GLUT4 exocytosis, and they are consistent with the conclusions of translocation experiments in Figures 1D and 2B.
Akt Activity Is Not Required for Insulin Regulation of GLUT4 Internalization
Insulin-mediated regulation of GLUT4 redistribution to the plasma membrane occurs mainly by accelerating the exocytosis rate of GLUT4, but insulin also has an inhibitory effect on GLUT4 internalization (Jhun et al., 1992; Czech and Buxton, 1993; Zeigerer et al., 2004). We measured the effect of Akt inhibition on insulin regulation of GLUT4 internalization. 3T3-L1 adipocytes expressing HA-GLUT4-GFP were stimulated with insulin ± AI1/2 and incubated with a saturating concentration of HA.11 antibody. The ratio between the amounts of HA.11 internalized versus HA.11 on the cell surface at different times gives us a measure of the endocytosis rate of GLUT4. We observed that the internalization rate of HA-GLUT4-GFP in insulin-stimulated cells was ∼2–3 times slower than in basal adipocytes (Figure 3C). Inhibition of Akt signaling did not significantly perturb the internalization rate of insulin-stimulated adipocytes, demonstrating that Akt activity is not required for insulin-regulation of GLUT4 internalization.
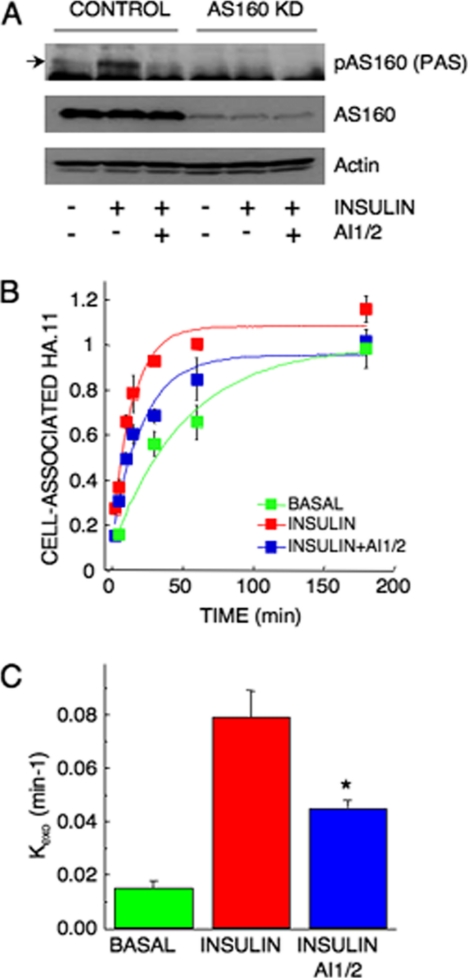
Akt Signaling to GLUT4 Exocytosis Involves Several Akt Targets
The Akt substrate AS160 is a Rab GTPase-activating protein (GAP) required for basal GLUT4 intracellular retention as well as for insulin-induced GLUT4 redistribution to the PM (Sano et al., 2003; Zeigerer et al., 2004; Eguez et al., 2005). AS160 is proposed to function as a negative regulator of basal GLUT4 exocytosis by maintaining an unknown rab protein in the GDP-bound, inactive state. Akt phosphorylation of AS160 turns off the GAP activity, allowing the rab protein to switch to the GTP-bound, active state. Consistent with this model, knockdown of AS160 results in an increase in basal GLUT4 exocytosis (Eguez et al., 2005).
If AS160 is the sole Akt substrate required for Akt-dependent effects on GLUT4 translocation, then inhibition of Akt in AS160 knockdown cells should not have a further effect on insulin-stimulated GLUT4 translocation to the PM. To address this question, we examined the effect of AI1/2 on AS160 knockdown adipocytes (Eguez et al., 2005). AS160 was efficiently down-regulated by the shRNA, and we did not detect any insulin-induced AS160 phosphorylation in the knockdown cells (Figure 4A). AI1/2 inhibited insulin-stimulated exocytosis of GLUT4 in AS160 knockdown adipocytes by approximately twofold, reducing the rate constant from ∼0.08 to ∼0.05 min−1 (Figure 4, B and C). Thus, inhibition of Akt impairs GLUT4 exocytosis in AS160-knockdown adipocytes, suggesting that Akt substrates other than AS160 are involved in insulin regulation of GLUT4 exocytosis. Furthermore, the observation that insulin promotes an acceleration of GLUT4 exocytosis in AI1/2-treated AS160-knockdown adipocytes provides additional evidence for non-Akt–mediated regulation of GLUT4 exocytosis.
Figure 4.
Akt regulates GLUT4 exocytosis by AS160-dependent and -independent mechanisms. (A) Immunoblot analyses of cell extracts from adipocytes expressing scrambled or AS160 shRNA. Phosphorylated AS160 (arrow) was detected with the PAS antibody. (B) Steady-state basal and insulin-stimulated GLUT4 exocytosis kinetics in AS160 knockdown 3T3-L1 adipocytes. The data are the mean ± SE of three independent experiments in the insulin-stimulated state and two independent experiments in the basal state. Insulin (1 nM) and 1 μM AI1/2 were used. (C) Basal and insulin-stimulated GLUT4 Kexo in the presence or absence of AI1/2 in AS160 knockdown adipocytes. Each data point is the mean ± SE of two to three independent experiments. *p < 0.05 compared with insulin-stimulated state in the absence of the Akt inhibitor (ANOVA).
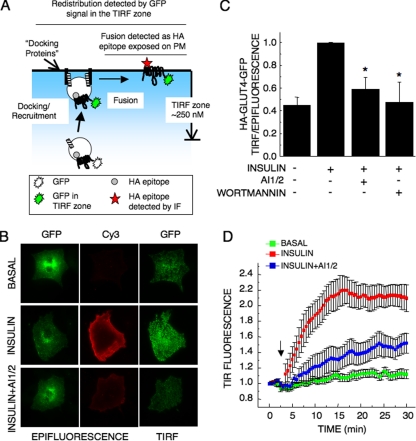
Akt Signaling Regulates Insulin-induced Recruitment/Docking of GLUT4 Vesicles to the PM
Insulin regulation of GLUT4 exocytosis might occur at several steps, including the recruitment, docking, and/or the fusion of GLUT4 vesicles with the PM. To further explore the role of Akt signaling in regulation of GLUT4 exocytosis, we used TIRF microscopy and a fixed time-point assay to measure insulin-induced redistribution of HA-GLUT4-GFP (Zeigerer et al., 2004). In this assay, the effect of insulin on GLUT4 distribution is measured as an increase in GLUT4-containing vesicles within ∼250 nm of the dorsal PM (Figure 5A). Quantification of these data revealed a two- to threefold redistribution of HA-GLUT4-GFP to the TIRF zone (Figure 5, B and C). The fold redistribution measured in the TIRF assay is smaller than in the epitope exposure assay, because in the TIRF assay the basal value reflects GLUT4 within 250 nm of the PM, whereas in the epitope exposure assay only GLUT4 that is in the PM is detected (Figure 5A). Inhibition of PI3-kinase with 100 nM wortmannin blocked insulin-induced redistribution of GLUT4 in the TIRF assay, demonstrating that in these conditions GLUT4 vesicles were not trapped within 250 nm of the dorsal PM, as would be the case if GLUT4 vesicles had docked but had not fused to the PM (Figure 5C). AI1/2 also inhibited recruitment of GLUT4 in the TIRF microscopy assay (Figure 5, B and C), demonstrating that Akt activity is required for GLUT4 vesicle recruitment and/or docking to the PM and suggesting Akt is the downstream effector of the PI3-kinase required for insulin regulation of recruitment and/or docking.
Figure 5.
Akt signaling is required for insulin-induced recruitment/docking of GLUT4 vesicles to the plasma membrane. (A) TIRF translocation assay. HA-GLUT4-GFP fluorescence in basal or insulin-stimulated cells was measured in the epifluorescence mode and in the TIRF mode. In the epifluorescence mode, translocation is measured as the exposure of the HA-epitope of HA-GLUT4-GFP on the surface of intact adipocytes, which is measured by IF. The HA fluorescence is normalized to GFP in cells also detected by epifluorescence (Lampson et al., 2000). In the TIRF assay, redistribution of HA-GLUT4-GFP to within 250 nm of the membrane is measured by GFP fluorescence. The TIRF GFP signal is normalized to the total amount of HA-GLUT4-GFP per cell measured in the epifluorescence mode of the microscope. The TIRF assay measures redistribution to within 250 nm of the PM independently of whether the GLUT4 is inserted into the PM (that is, independently of vesicle fusion). (B) Representative images of HA-GLUT4-GFP in the basal state and after 1 nM insulin stimulation for 30 min ± 1 μM AI1/2. Total HA-GLUT4-GFP was determined by GFP fluorescence in the epifluorescence mode, HA-GLUT4-GFP inserted in the PM was determined by indirect immunofluorescence of the HA epitope, and HA-GLUT4-GFP in the TIRF zone was determined by GFP fluorescence in the TIRF mode. (C) Quantification of GLUT4 redistribution measured using TIRF microscopy. For each experiment, the data are normalized to the insulin stimulated state. The values shown are the means ± SE of three independent experiments. AI1/2 (1 μM), 100 nM wortmannin, and 1 nM insulin were used. *p < 0.05 versus the insulin-stimulated state (ANOVA). (D) Quantification of time-lapsed TIRF microscopy of HA-GLUT4-GFP in the TIRF zone. Images were acquired every 30 s for 30 min. Insulin (1 nM) or vehicle (mock) was added after the fifth frame (noted by the arrow). AI1/2 (1 μM) was added 1 h before recording. Data shown are the mean ± SE from six to nine cells per condition, derived from three independent experiments.
We further analyzed the effect of Akt inhibition on insulin-induced GLUT4 redistribution by using time-lapse TIRF microscopy. It has been shown previously that GLUT4 vesicles are mobile within the TIRF zone in basal rat primary adipocytes (Lizunov et al., 2005). We also found that GLUT4-containing vesicles in basal 3T3-L1 adipocytes are highly mobile within the TIRF zone (our unpublished data). Insulin stimulation triggers the recruitment of HA-GLUT4-GFP–containing vesicles to the TIRF zone, reaching a plateau within 15 min of insulin addition (Figure 5D). On insulin stimulation, the GFP fluorescence in the TIRF zone increases, and the fluorescence becomes less punctate and more diffuse, consistent with HA-GLUT4-GFP having fused into the membrane. GLUT4 vesicles in insulin-stimulated AI1/2 pretreated cells were also highly motile in the TIRF zone; however, HA-GLUT4-GFP accumulation within the TIRF zone was dramatically reduced compared with insulin-treated control adipocytes (Figure 5D). GLUT4 within the TIRF zone of AI1/2-treated, insulin-stimulated adipocytes plateaued at ∼30% of the control level, consistent with the translocation studies in Figures 1 and 2. Although we did not extend the live cell imaging beyond 30 min, we found in fixed cell experiments that the amount of GLUT4 in the PM of AI1/2-treated adipocytes did not increase when incubation with insulin was increased from 30 to 60 min, indicating that the reduced amount of GLUT4 in the PM of AI1/2-treated cells at 30 min reflects a new steady-state distribution of GLUT4 between the PM and interior of cells (our unpublished data). Live cell analysis also revealed a 1- to 2-min lag in the recruitment of GLUT4 to the TIRF zone in AI1/2-treated cells compared with control adipocytes as well as a reduction in the rate of accumulation of GLUT4 in the TIRF zone. These data demonstrate that Akt signaling is essential for insulin-induced accumulation of GLUT4 vesicles within ∼250 nm of the PM and thereby suggest that Akt regulates recruitment and/or docking of these vesicles to the PM.
PI3-Kinase but Not Akt Signaling Regulates Insulin-induced Fusion of GLUT4 Vesicles to the PM
We developed a TIRF microscopy fusion assay to determine whether Akt signaling was required for insulin stimulation of GLUT4 vesicle fusion with the PM. For these studies, we used adipocytes stably expressing HA-GLUT4 (Govers et al., 2004; Martin et al., 2006). First, we developed a TIRF assay to measure redistribution of HA-GLUT4 to within 250 nm of the PM by adapting the assay described in Figure 5. Indirect immunofluorescence (IF) of HA-epitope in permeabilized cells by using the TIRF microscopy mode was performed to measure HA-GLUT4 within 250 nm of the PM (Figure 6A). The total amount of HA-GLUT4 in cells was measured in epifluorescence microscopy of the same cells (Figure 6B). The ratio of the TIRF fluorescence to epifluorescence is a measure of the redistribution of HA-GLUT4 to within 250 nm of the PM, independent of fusion of HA-GLUT4 into the PM. As was the case in the TIRF translocation assay using HA-GLUT4-GFP (Figure 5C), insulin induced an approximately twofold increase in HA-GLUT4 in the TIRF zone, and both wortmannin and AI1/2 inhibited this redistribution (Figure 6D). These data provide additional support for the hypothesis that Akt and PI3-kinase activity is required for the recruitment and/or docking of GLUT4 vesicles to the PM.
Figure 6.
PI3-kinase but not Akt signaling regulates insulin-induced GLUT4 vesicle fusion to the PM. (A) HA-GLUT4 redistribution to within 250 nm of the dorsal PM was measured by IF of permeabilized cells using TIRF microscopy. Although all the anti-HA antibodies in the cells are bound by fluorescently labeled secondary antibody, only the fluorescent secondary antibody bound to anti-HA-epitope antibodies within the TIRF zone are excited (red stars). (B) The total amount of HA-GLUT4 in permeabilized cells was determined by epifluorescence microscopy. The ratio of the TIRF to epifluorescence is a measure of the redistribution of HA-GLUT4 to within 250 nm of the dorsal PM (see D). (C) HA-GLUT4 inserted into the PM was determined IF of intact (nonpermeabilized cells) by TIRF microscopy. The ratio of the TIRF fluorescence in intact cells to TIRF fluorescence on permeabilized cells (see A) is proportional to the efficiency of HA-GLUT4 vesicle fusion with the PM, because it reflects the fraction of HA-GLUT4 within 250 nm of the membrane that is inserted in the PM. (D) Measurement of insulin-induced GLUT4 vesicle recruitment/docking in 3T3-L1 adipocytes stably expressing HA-GLUT4. The data are the ratio of the HA-GLUT4 within 250 nm of the PM of permeabilized cells, as determined by IF (anti-HA) in TIRF mode (see A), divided by the total HA-GLUT4 in cells determined in epifluorescence mode of the same samples (see B). The data are normalized to the insulin-stimulated state of control cells. The data are the means ± SE of three to six independent experiments. Insulin (1 nM), 100 nM wortmannin, and 1 μM AI1/2 were used. (E) Efficiency of GLUT4 vesicle fusion with PM. The data are the ratio of the HA-GLUT4 in the PM, as determined by IF in TIRF mode of intact cells (see C) divided by the HA-GLUT4 within the TIRF zone, as determined in TIRF mode of permeabilized cells (see A). The means ± SE of three to six independent experiments are shown. Insulin (1 nM), 100 nM wortmannin, and 1 μM AI1/2 were used. The difference between insulin-stimulated AI1/2-treated cells and insulin-stimulated control cells was not statistically different. *p < 0.001 versus the insulin-stimulated control cells; #p < 0.05 versus AI1/2, insulin-stimulated cells (ANOVA).
Next, we developed an assay to measure insulin regulation of the fusion of HA-GLUT4 vesicles with the dorsal PM, independent of insulin's effects on recruitment/docking. HA-GLUT4 in the dorsal PM (vesicle fusion) was measured by IF of HA epitopes in intact cells using TIRF microscopy (Figure 6C). Only HA-GLUT4 fused into the dorsal PM is detected in the absence of detergent. In parallel samples, we measured, using TIRF microscopy, HA-GLUT4 within 250 nm of the dorsal membrane by IF of detergent-permeabilized cells, which is a measure of the total HA-GLUT4 within the TIRF zone (Figure 6A). The efficiency of HA-GLUT4 fusion with the PM was measured as the ratio of the amount inserted into the PM to the total amount in the TIRF zone. In the insulin-stimulated state ∼60% of GLUT4 recruited to the TIRF zone is fused with the PM versus ∼25% in the basal state (Figure 6E). These data demonstrate that insulin stimulates a twofold increase in the efficiency of the fusion of HA-GLUT4-containing vesicles with the PM as well as increasing the accumulation of GLUT4 vesicles near the plasma membrane, as shown in Figure 5C.
Inhibition of Akt with AI1/2 did not significantly reduce insulin-stimulation of the efficiency of GLUT4 vesicle fusion with the PM (Figure 6E), even though Akt inhibition reduced GLUT4 recruitment to the TIRF zone (Figure 6D). These data indicate that Akt activity is required for a prefusion step involving the recruitment/docking of GLUT4-containing vesicles to the PM but not for efficient fusion of GLUT4 vesicles with the PM, because insulin stimulation of GLUT4 vesicle fusion is not significantly affected by inhibition of Akt, whereas insulin-stimulated recruitment/docking of GLUT4 vesicles is affected by Akt inhibition. By contrast, inhibition of PI3-kinase with 100 nM wortmannin reduced the efficiency of GLUT4 vesicle fusion to the PM, demonstrating a requirement for PI3-kinase activity in insulin-stimulated fusion of GLUT4 vesicles (Figure 6E). These results suggest that insulin regulates GLUT4 exocytosis by increasing both the recruitment/docking and the fusion of GLUT4 vesicles with the PM. Both these processes are dependent on PI3-kinase signaling. However, only the recruitment and/or docking of GLUT4 vesicles is dependent on Akt activation.
DISCUSSION
In this study, we have used acute inhibition of Akt activity to dissect the role of Akt signaling on insulin-regulated GLUT4 trafficking. We show that Akt signaling is required for insulin-stimulated GLUT4 exocytosis but not for insulin regulation of GLUT4 internalization. Along the exocytic pathway, Akt activity is specifically required for the recruitment/docking of GLUT4 vesicles that precedes insulin-stimulated fusion of these vesicles with the PM. Although the fusion of the vesicles with the PM requires PI3-kinase signaling, it is independent of Akt activity. Thus, our data are consistent with insulin signaling to GLUT4 exocytosis by both Akt-dependent and Akt-independent mechanisms. Although Akt activation is specifically required for insulin regulation of the GLUT4/IRAP trafficking pathway, the effects of insulin on TR trafficking do not require Akt activity. Therefore, our data indicate that insulin signaling to GLUT4 trafficking diverges from signaling to the general endocytic pathway (that is, TR trafficking). The effect of insulin on TR behavior may be the Akt-independent arm of signaling to GLUT4. Studies to determine the overlap between insulin signaling to TR and GLUT4 will be the subject of future work.
Protein kinase Akt has been established as a crucial regulator of insulin-induced GLUT4 translocation; however, a number of observations support the hypothesis that insulin signals to GLUT4 by both Akt-dependent and -independent mechanisms. For example, knockdown of both Akt1 and Akt2 in 3T3-L1 adipocytes did not completely inhibit GLUT4 translocation (Jiang et al., 2003), although residual Akt in the knockdown cells could account for the effect of insulin in that study. Here, we show that acute inhibition of Akt with 1 μM AI1/2, which completely blocked phosphorylation of Akt-Ser473 induced by 1 nM insulin (the concentration used for functional studies) significantly reduced but did not completely block insulin-stimulated GLUT4 translocation in control adipocytes as well as adipocytes in which Akt2 was knocked down. These data reinforce the idea that insulin signals to GLUT4 by Akt-dependent and -independent mechanisms and that full GLUT4 translocation to the PM requires both signaling pathways.
What other effectors of insulin action are required for redistribution of GLUT4 to the PM? There is evidence that insulin activation of atypical protein kinase C (PKC) is required for insulin-stimulated glucose uptake (Kotani et al., 1998; Standaert et al., 1999; Sajan et al., 2006). In addition, insulin activation of the small GTPase TC10, by a mechanism independent of PI3-kinase, has a role in GLUT4 redistribution to the PM (Chiang et al., 2001; Inoue et al., 2003; Saltiel and Pessin, 2003). Additional studies are required to determine the relative contributions of these pathways and their individual roles in the redistribution of GLUT4. As a first step toward this goal, in this report we have mapped the role of Akt activation on GLUT4 translocation to the PM.
GLUT4 Exocytosis Is a Multistep-regulated Process: An Akt-dependent, Prefusion Vesicle Recruitment/Docking Step
Here, we use a TIRF microscopy assay in intact cells to show that insulin enhances both the recruitment/docking of GLUT4 vesicles and the fusion of GLUT4 vesicles with the PM. The recruitment/docking step is measured as a change in GLUT4 in the TIRF excitation zone (∼250 nm of the dorsal PM) and is independent of whether the GLUT4 vesicles have fused to the PM. Inhibition of Akt blocked insulin-stimulated GLUT4 accumulation within 250 nm of the PM (Figure 5). The TIRF zone is approximately three GLUT4 vesicle diameters in depth; therefore, it should encompass vesicles docked to the PM. Hence, these data suggest that Akt signaling is required for the GLUT4 vesicle recruitment/docking, because if vesicles were arrested at a docked state, GFP in the TIRF zone would have been increased by insulin. Inhibition of PI3-kinase activation, which is required for activation of Akt, also inhibited insulin-stimulated accumulation of GLUT4 within the TIRF zone.
The TIRF microscopy assay cannot distinguish between active recruitment of GLUT4 vesicles to within 250 nm of the PM and regulated docking to the PM. There is some controversy in the literature whether insulin actively recruits GLUT4 vesicles to the PM. For example, a recent live cell TIRF analysis of GLUT4 trafficking in primary rat fat cells concluded that GLUT4 vesicle movement to the PM is not accelerated by insulin, but rather that the docking of these vesicles to the PM is regulated by insulin (Lizunov et al., 2005). Based on those observations, and the results of our studies, we favor the model that Akt is required for the regulated docking of GLUT4 vesicles with the PM. Using live cell TIRF microscopy, we observed that Akt inhibition reduced the insulin-stimulated net accumulation of GLUT4 at the PM, slowed the rate of GLUT4 accumulation within the TIRF zone, and induced a lag in the increase of GLUT4 in the TIRF zone after insulin stimulation (Figure 5D). These observations are all consistent with an inefficient docking of GLUT4 vesicles at the PM when Akt activation is blocked. However, once these vesicles are properly docked, albeit an inefficient process when Akt is inhibited, fusion with the PM is properly stimulated by insulin. Thus, the steady-state level of GLUT4 in the PM of insulin-stimulated, AI1/2-treated adipocytes is reduced compared with control cells, because the recruitment and/or docking is inefficient. However, GLUT4 in the PM of insulin-stimulated, AI1/2-treated adipocytes is increased relative to basal cells because fusion (and other steps of GLUT4 movement) are regulated by an Akt-independent process(es). Recently, Holman and coworkers have developed an vitro system to measure insulin-induced GLUT4 vesicle fusion (Koumanov et al., 2005). The results of that study argue that insulin regulation of GLUT4 vesicle fusion is a key step in GLUT4 translocation to the plasma membrane and that fusion is dependent on the recruitment of active Akt to the plasma membrane. However, the in vitro studies do not directly address differences between vesicle docking and fusion. Vesicle docking precedes fusion and therefore unstimulated (or inefficient) docking would be scored as poor fusion in the in vitro assay. Thus, their in vitro data are compatible with our proposal that Akt regulates a prefusion step. Our results in intact cells extend their proposal that insulin action on GLUT4 occurs, in part, at the plasma membrane, by showing that principally a prefusion step (recruitment and/or docking), and not the fusion, is the Akt-regulated step.
The best-characterized downstream effector of Akt required for GLUT4 translocation is the rab GAP AS160. Past studies have shown that a dominant-interfering AS160 mutant that cannot be phosphorylated by Akt, blocked insulin-stimulated redistribution of GLUT4 to within 250 nm of the PM (Zeigerer et al., 2004), and we have also observed that AS160 knockdown impairs insulin-induced recruitment of GLUT4 vesicles to the TIRF zone (Supplemental Figure 1). Those results support the model that Akt regulates docking of GLUT4 to the PM, and they suggest that Akt regulates docking at least in part by targeting AS160. Rab proteins are known to regulate docking and fusion of vesicles, and it is tempting to speculate that the rab target of AS160 GAP activity has a role in the regulation of docking. At this time, the rab target of AS160 is not known.
It is important to note, however, that although we favor the model that the prefusion step regulated by Akt activity is vesicle docking and not active recruitment of GLUT4 vesicles to the PM, the results of several studies support the hypothesis that insulin signals to regulate GLUT4 vesicle movement along microtubules (Bose et al., 2002; Semiz et al., 2003) and/or the actin cytoskeleton (Tong et al., 2001). Thus, these effects of insulin could have a role in the ”active“ recruitment of GLUT4 vesicles to within 250 nm of the PM. Regardless of whether insulin actively recruits GLUT4 from intracellular sites and/or promotes docking of vesicles, our data show that PI3-kinase and Akt signaling are necessary for a prefusion step resulting in the accumulation of GLUT4 vesicles within ∼250 nm of the PM.
Previous studies have shown that inhibition of PI3-kinase (Bose et al., 2004) or a temperature block of Akt activity (van Dam et al., 2005) promoted the accumulation of GLUT4 vesicles adjacent to the PM, as would be the case if the vesicles were docked but not fused. An interpretation of these data is that insulin regulates docking independently of PI3-kinase and Akt inactivation. We do not, however, observe this effect in the TIRF assay. One possible explanation for this discrepancy is that we measured GLUT4 near the PM with TIRF microscopy and the other studies used confocal microscopy. If the GLUT4 vesicles accumulate beyond 250 nm of the membrane when PI3-kinase or Akt are inhibited, they would not be detected in TIRF assay, but they would occur as a plasma membrane ring in confocal analysis. Thus, those previous studies may have uncovered a regulated tethering (beyond 250 nm) of the PM that is stimulated by insulin in a PI3-kinase/Akt–independent process, but according to our data might not have measured insulin-regulated GLUT4 vesicle docking at the PM.
GLUT4 Exocytosis Is a Multistep-regulated Process: GLUT4 Vesicle Fusion, a PI3-Kinase–dependent, Akt-independent Process
Although insulin-stimulated recruitment/docking of GLUT4 vesicles to the TIRF zone is reduced when Akt is inhibited, insulin-stimulated fusion of GLUT4 vesicles that are within 250 nm of the PM is not significantly affected by Akt inhibition, indicating that Akt activity does not regulate fusion. In contrast, in cells in which PI3-kinase is inhibited, insulin-induced fusion of GLUT4 vesicles is blocked. Therefore, our data document a divergence in insulin signaling to GLUT4 vesicles, with vesicle recruitment/docking requiring Akt activation and fusion requiring PI3-kinase activity but not Akt activation.
Previous studies support insulin-regulation of GLUT4 vesicle fusion (Kanda et al., 2005; Koumanov et al., 2005; van Dam et al., 2005). One possible candidate to regulate GLUT4 vesicle fusion is Munc18c, a syntaxin 4-interacting protein (Thurmond et al., 2000; Kanda et al., 2005). Studies of adipocytes derived from Munc18c null mice support the hypothesis that Munc18c is a negative regulator of GLUT4 fusion at the PM and a downstream target of PI3-kinase activation, consistent with our findings that fusion requires PI3-kinase activity (Kanda et al., 2005). It has been proposed that insulin signaling, through PKCζ/λ, promotes disassociation of Munc18c from syntaxin 4, allowing for the assembly of the soluble N-ethylmaleimide-sensitive factor attachment protein receptor fusion complex (Thurmond et al., 2000; Hodgkinson et al., 2005). Those results suggest that PKCζ/λ may be the PI3-kinase effector regulating the fusion. Alternatively, insulin-mediated recruitment of the exocyst complex to the PM has been proposed to regulate GLUT4 translocation, potentially by regulating docking (Inoue et al., 2003). Future studies are required to determine how and whether these pathways converge to regulate GLUT4 vesicle docking and fusion.
Insulin regulation of GLUT4 trafficking is a complex process that requires the integration of several signaling pathways downstream of the insulin receptor. Our data support a model in which insulin signals to GLUT4 exocytosis, regulating the recruitment/docking and fusion of GLUT4 vesicles to the PM. Dissecting the specific input of insulin signaling mediators on GLUT4 movement is a requisite if we are to understand how insulin regulates glucose transport in fat and muscles and how this process is disrupted in insulin-resistant states.
Supplementary Material
ACKNOWLEDGMENTS
We thank members of the McGraw laboratory, Gus Lienhard, and Markus Schober for helpful discussions and suggestions and Daniel Chung for expert technical assistance. This work was supported by National Institutes of Health Grant DK52852 (to T.E.M.) and an American Heart Association Heritage Affiliate Award (to E.G.).
Footnotes
 The online version of this article contains supplemental material at MBC Online (http://www.molbiolcell.org).
The online version of this article contains supplemental material at MBC Online (http://www.molbiolcell.org).
This article was published online ahead of print in MBC in Press (http://www.molbiolcell.org/cgi/doi/10.1091/mbc.E06-07-0585) on August 16, 2006.
REFERENCES
- Bae S. S., Cho H., Mu J., Birnbaum M. J. Isoform-specific regulation of insulin-dependent glucose uptake by Akt/protein kinase B. J. Biol. Chem. 2003;278:49530–49536. doi: 10.1074/jbc.M306782200. [DOI] [PubMed] [Google Scholar]
- Bogan J. S., Hendon N., McKee A. E., Tsao T. S., Lodish H. F. Functional cloning of TUG as a regulator of GLUT4 glucose transporter trafficking. Nature. 2003;425:727–733. doi: 10.1038/nature01989. [DOI] [PubMed] [Google Scholar]
- Bose A., Guilherme A., Robida S. I., Nicoloro S. M., Zhou Q. L., Jiang Z. Y., Pomerleau D. P., Czech M. P. Glucose transporter recycling in response to insulin is facilitated by myosin Myo1c. Nature. 2002;420:821–824. doi: 10.1038/nature01246. [DOI] [PubMed] [Google Scholar]
- Bose A., Robida S., Furcinitti P. S., Chawla A., Fogarty K., Corvera S., Czech M. P. Unconventional myosin Myo1c promotes membrane fusion in a regulated exocytic pathway. Mol. Cell. Biol. 2004;24:5447–5458. doi: 10.1128/MCB.24.12.5447-5458.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang S., Baumann C., Kanzaki M., Thurmond D., Watson R., Neudauer C., Macara I., Pessin J., Saltiel A. Insulin-stimulated GLUT4 translocation requires the CAP-dependent activation of TC10. Nature. 2001;410:944–948. doi: 10.1038/35073608. [DOI] [PubMed] [Google Scholar]
- Cho H., Mu J., Kim J. K., Thorvaldsen J. L., Chu Q., Crenshaw E. B., 3rd, Kaestner K. H., Bartolomei M. S., Shulman G. I., Birnbaum M. J. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB beta) Science. 2001;292:1728–1731. doi: 10.1126/science.292.5522.1728. [DOI] [PubMed] [Google Scholar]
- Czech M. P., Buxton J. M. Insulin action on the internalization of the GLUT4 glucose transporter in isolated rat adipocytes. J. Biol. Chem. 1993;268:9187–9190. [PubMed] [Google Scholar]
- DeFeo-Jones D., et al. Tumor cell sensitization to apoptotic stimuli by selective inhibition of specific Akt/PKB family members. Mol. Cancer Ther. 2005;4:271–279. [PubMed] [Google Scholar]
- Eguez L., Lee A., Chavez J. A., Miinea C. P., Kane S., Lienhard G. E., McGraw T. E. Full intracellular retention of GLUT4 requires AS160 Rab GTPase activating protein. Cell Metab. 2005;2:263–272. doi: 10.1016/j.cmet.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Garza L., Birnbaum M. Insulin-responsive aminopeptidase trafficking in 3T3–L1 adipocytes. J. Biol. Chem. 2000;275:2560–2567. doi: 10.1074/jbc.275.4.2560. [DOI] [PubMed] [Google Scholar]
- Gibbs E. M., Lienhard G. E., Gould G. W. Insulin-induced translocation of glucose transporters to the plasma membrane precedes full stimulation of hexose transport. Biochemistry. 1988;27:6681–6685. doi: 10.1021/bi00418a006. [DOI] [PubMed] [Google Scholar]
- Govers R., Coster A. C., James D. E. Insulin increases cell surface GLUT4 levels by dose dependently discharging GLUT4 into a cell surface recycling pathway. Mol. Cell. Biol. 2004;24:6456–6466. doi: 10.1128/MCB.24.14.6456-6466.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill M. M., Clark S. F., Tucker D. F., Birnbaum M. J., James D. E., Macaulay S. L. A role for protein kinase Bbeta/Akt2 in insulin-stimulated GLUT4 translocation in adipocytes. Mol. Cell. Biol. 1999;19:7771–7781. doi: 10.1128/mcb.19.11.7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson C. P., Mander A., Sale G. J. Protein kinase-zeta interacts with munc18c: role in GLUT4 trafficking. Diabetologia. 2005;48:1627–1636. doi: 10.1007/s00125-005-1819-y. [DOI] [PubMed] [Google Scholar]
- Inoue M., Chang L., Hwang J., Chiang S. H., Saltiel A. R. The exocyst complex is required for targeting of Glut4 to the plasma membrane by insulin. Nature. 2003;422:629–633. doi: 10.1038/nature01533. [DOI] [PubMed] [Google Scholar]
- Ishiki M., Randhawa V. K., Poon V., Jebailey L., Klip A. Insulin regulates the membrane arrival, fusion, and C-terminal unmasking of glucose transporter-4 via distinct phosphoinositides. J. Biol. Chem. 2005;280:28792–28802. doi: 10.1074/jbc.M500501200. [DOI] [PubMed] [Google Scholar]
- Jhun B. H., Rampal A. L., Liu H., Lachaal M., Jung C. Y. Effects of insulin on steady state kinetics of GLUT4 subcellular distribution in rat adipocytes. Evidence of constitutive GLUT4 recycling. J. Biol. Chem. 1992;267:17710–17715. [PubMed] [Google Scholar]
- Jiang Z. Y., Zhou Q. L., Coleman K. A., Chouinard M., Boese Q., Czech M. P. Insulin signaling through Akt/protein kinase B analyzed by small interfering RNA-mediated gene silencing. Proc. Natl. Acad. Sci. USA. 2003;100:7569–7574. doi: 10.1073/pnas.1332633100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanda H., Tamori Y., Shinoda H., Yoshikawa M., Sakaue M., Udagawa J., Otani H., Tashiro F., Miyazaki J., Kasuga M. Adipocytes from Munc18c-null mice show increased sensitivity to insulin-stimulated GLUT4 externalization. J. Clin. Investig. 2005;115:291–301. doi: 10.1172/JCI22681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karylowski O., Zeigerer A., Cohen A., McGraw T. E. GLUT4 is retained by an intracellular cycle of vesicle formation and fusion with endosomes. Mol. Biol. Cell. 2004;15:870–882. doi: 10.1091/mbc.E03-07-0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn A. D., Summers S. A., Birnbaum M. J., Roth R. A. Expression of a constitutively active Akt Ser/Thr kinase in 3T3–L1 adipocytes stimulates glucose uptake and glucose transporter 4 translocation. J. Biol. Chem. 1996;271:31372–31378. doi: 10.1074/jbc.271.49.31372. [DOI] [PubMed] [Google Scholar]
- Kotani K., et al. Requirement of atypical protein kinase Clambda for insulin stimulation of glucose uptake but not for Akt activation in 3T3–L1 adipocytes. Mol. Cell. Biol. 1998;18:6971–6982. doi: 10.1128/mcb.18.12.6971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koumanov F., Jin B., Yang J., Holman G. D. Insulin signaling meets vesicle traffic of GLUT4 at a plasma-membrane-activated fusion step. Cell Metab. 2005;2:179–189. doi: 10.1016/j.cmet.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Lampson M. A., Racz A., Cushman S. W., McGraw T. E. Demonstration of insulin-responsive trafficking of GLUT4 and vpTR in fibroblasts. J. Cell Sci. 2000;113:4065–4076. doi: 10.1242/jcs.113.22.4065. [DOI] [PubMed] [Google Scholar]
- Lampson M. A., Schmoranzer J., Zeigerer A., Simon S. M., McGraw T. E. Insulin-regulated release from the endosomal recycling compartment is regulated by budding of specialized vesicles. Mol. Biol. Cell. 2001;12:3489–3501. doi: 10.1091/mbc.12.11.3489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao W., Nguyen M. T., Imamura T., Singer O., Verma I. M., Olefsky J. M. Lentiviral short hairpin ribonucleic acid-mediated knockdown of GLUT4 in 3T3–L1 adipocytes. Endocrinology. 2006;147:2245–2252. doi: 10.1210/en.2005-1638. [DOI] [PubMed] [Google Scholar]
- Lizunov V. A., Matsumoto H., Zimmerberg J., Cushman S. W., Frolov V. A. Insulin stimulates the halting, tethering, and fusion of mobile GLUT4 vesicles in rat adipose cells. J. Cell Biol. 2005;169:481–489. doi: 10.1083/jcb.200412069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin O. J., Lee A., McGraw T. E. GLUT4 distribution between the plasma membrane and the intracellular compartments is maintained by an insulin-modulated bipartite dynamic mechanism. J. Biol. Chem. 2006;281:484–490. doi: 10.1074/jbc.M505944200. [DOI] [PubMed] [Google Scholar]
- Moskowitz H. S., Heuser J., McGraw T. E., Ryan T. A. Targeted chemical disruption of clathrin function in living cells. Mol. Biol. Cell. 2003;14:4437–4447. doi: 10.1091/mbc.E03-04-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross S. A., Herbst J. J., Keller S. R., Lienhard G. E. Trafficking kinetics of the insulin-regulated membrane aminopeptidase in 3T3–L1 adipocytes. Biochem. Biophys. Res. Commun. 1997;239:247–251. doi: 10.1006/bbrc.1997.7459. [DOI] [PubMed] [Google Scholar]
- Sajan M. P., Rivas J., Li P., Standaert M. L., Farese R. V. Repletion of atypical protein kinase C following RNA interference-mediated depletion restores insulin-stimulated glucose transport. J. Biol. Chem. 2006;281:17466–17473. doi: 10.1074/jbc.M510803200. [DOI] [PubMed] [Google Scholar]
- Saltiel A. R., Pessin J. E. Insulin signaling in microdomains of the plasma membrane. Traffic. 2003;4:711–716. doi: 10.1034/j.1600-0854.2003.00119.x. [DOI] [PubMed] [Google Scholar]
- Sano H., Kane S., Sano E., Miinea C. P., Asara J. M., Lane W. S., Garner C. W., Lienhard G. E. Insulin-stimulated phosphorylation of a Rab GTPase-activating protein regulates GLUT4 translocation. J. Biol. Chem. 2003;278:14599–14602. doi: 10.1074/jbc.C300063200. [DOI] [PubMed] [Google Scholar]
- Semiz S., Park J. G., Nicoloro S. M., Furcinitti P., Zhang C., Chawla A., Leszyk J., Czech M. P. Conventional kinesin KIF5B mediates insulin-stimulated GLUT4 movements on microtubules. EMBO J. 2003;22:2387–2399. doi: 10.1093/emboj/cdg237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shewan A., Marsh B., Melvin D., Martin S., Gould G., James D. The cytosolic C-terminus of the glucose transporter GLUT4 contains an acidic cluster endosomal targeting motif distal to the dileucine signal. Biochem. J. 2000;350:99–107. [PMC free article] [PubMed] [Google Scholar]
- Standaert M. L., et al. Insulin activates protein kinases C-zeta and C-lambda by an autophosphorylation-dependent mechanism and stimulates their translocation to GLUT4 vesicles and other membrane fractions in rat adipocytes. J. Biol. Chem. 1999;274:25308–25316. doi: 10.1074/jbc.274.36.25308. [DOI] [PubMed] [Google Scholar]
- Subtil A., Lampson M. A., Keller S. R., McGraw T. E. Characterization of the insulin-regulated endocytic recycling mechanism in 3T3-L1 adipocytes using a novel reporter molecule. J. Biol. Chem. 2000;275:4787–4795. doi: 10.1074/jbc.275.7.4787. [DOI] [PubMed] [Google Scholar]
- Thurmond D., Kanzaki M., Khan A., Pessin J. Munc18c function is required for insulin-stimulated plasma membrane fusion of GLUT4 and insulin-responsive amino peptidase storage vesicles. Mol. Cell. Biol. 2000;20:379–388. doi: 10.1128/mcb.20.1.379-388.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong P., Khayat Z. A., Huang C., Patel N., Ueyama A., Klip A. Insulin-induced cortical actin remodeling promotes GLUT4 insertion at muscle cell membrane ruffles. J. Clin. Investig. 2001;108:371–381. doi: 10.1172/JCI12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dam E. M., Govers R., James D. E. Akt activation is required at a late stage of insulin-induced GLUT4 translocation to the plasma membrane. Mol. Endocrinol. 2005;19:1067–1077. doi: 10.1210/me.2004-0413. [DOI] [PubMed] [Google Scholar]
- Wang Q., Somwar R., Bilan P. J., Liu Z., Jin J., Woodgett J. R., Klip A. Protein kinase B/Akt participates in GLUT4 translocation by insulin in L6 myoblasts. Mol. Cell. Biol. 1999;19:4008–4018. doi: 10.1128/mcb.19.6.4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson R. T., Pessin J. E. Bridging the GAP between insulin signaling and GLUT4 translocation. Trends Biochem. Sci. 2006;31:215–222. doi: 10.1016/j.tibs.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Xu Z., Kandror K. V. Translocation of small preformed vesicles is responsible for the insulin activation of glucose transport in adipose cells. Evidence from the in vitro reconstitution assay. J. Biol. Chem. 2002;277:47972–47975. doi: 10.1074/jbc.C200486200. [DOI] [PubMed] [Google Scholar]
- Yeh J. I., Verhey K. J., Birnbaum M. J. Kinetic analysis of glucose transporter trafficking in fibroblasts and adipocytes. Biochemistry. 1995;34:15523–15531. doi: 10.1021/bi00047a018. [DOI] [PubMed] [Google Scholar]
- Zeigerer A., Lampson M., Karylowski O., Sabatini D., Adesnik M., Ren M., McGraw T. GLUT4 retention in adipocytes requires two intracellular insulin-regulated transport steps. Mol. Biol. Cell. 2002;13:2421–2435. doi: 10.1091/mbc.E02-02-0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeigerer A., McBrayer M. K., McGraw T. E. Insulin stimulation of GLUT4 exocytosis, but not its inhibition of endocytosis, is dependent on RabGAP AS160. Mol. Biol. Cell. 2004;15:4406–4415. doi: 10.1091/mbc.E04-04-0333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., et al. Discovery of 2,3,5-trisubstituted pyridine derivatives as potent Akt1 and Akt2 dual inhibitors. Bioorg. Med. Chem. Lett. 2005;15:905–909. doi: 10.1016/j.bmcl.2004.12.062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.