Abstract
Many strategies are commonly used to influence physician behavior in managed care organizations. This review examines the effectiveness of three mechanisms to influence physician behavior: financial incentives directed at providers or patients, policies/procedures for managing care, and the selection/education of both providers and patients. We reach three conclusions. First, all health care systems use financial incentives, but these mechanisms are shifting away from financial incentives directed at the physician to those directed at the consumer. Second, heavily procedural strategies such as utilization review and gatekeeping show some evidence of effectiveness but are highly unpopular due to their restrictions on physician and patient choice. Third, a future system built on consumer choice is contradicted by mechanisms that rely solely on narrow networks of providers or the education of physicians. If patients become the new locus of decision-making in health care, provider-focused mechanisms to influence physician behavior will not disappear but are likely to decline in importance.
Keywords: Managed care, physician behavior, incentives, utilization management
INTRODUCTION
Traditionally, physicians were the primary decision-makers controlling the use of health care resources. Over the last decade, employers, insurers, and some physician organizations attempted to constrain these decisions through a host of managed care mechanisms such as utilization review and capitation. These attempts have been deemed a partial economic success but a complete political failure (Robinson 2001). The business of managing care has become the business of un-managing care, as physician panels are broadened, gatekeeping and utilization review restrictions are removed, and fee-for-service payments increase. The era of the consumer has been declared, with patients seen as the new locus of decision-making in the health care system (Robinson 2001).
However, it is unlikely that we will develop a completely consumer-driven health care system (Robinson 2001). Many consumers are ill-prepared to understand the trade-offs between quality and health care prices and to navigate our complex health care system. Differences in health and wealth could also inhibit a consumer’s ability to pool risk effectively through the purchase of insurance. As a result, insurers, employers, government, and physicians will continue to play important roles in health care decision-making. This suggests that current strategies to control health care utilization will not disappear completely—some will evolve to new forms based on twin criteria of effectiveness and political feasibility. The purpose of this paper is to examine the evolution of these strategies according to these two criteria. We expect that some strategies will be transformed to the new model and some will be fundamentally incompatible with a consumer-driven health care system. It is likely that highly effective or highly popular strategies will evolve and continue to exist in the new system, while strategies that are neither will stagnate or decline.
NEW CONTRIBUTION
The proliferation of ever-new and changing strategies to manage care hinders the practical application of the existing literature. It also provides little guidance for those seeking information on the effectiveness of newer strategies that have not yet been rigorously evaluated. We contribute to the current literature by evaluating strategies to influence physician behavior according to both their effectiveness and political feasibility in a new and rapidly-evolving model of consumer-driven health care. Our goal is to assist health care organizations, researchers, and policy makers in identifying and choosing effective strategies to manage care from the broad and evolving array of current approaches.
CONCEPTUAL FRAMEWORK
Our conceptual framework describes three different mechanisms to influence provider behavior either directly or indirectly (Ouchi 1979; Landon, Wilson, and Cleary 1998; Hibbard, Slovic, and Jewett 1997). These mechanisms include financial incentives directed at providers or patients, policies and procedures for managing care, and the selection and education of both providers and patients (see Figure). Financial incentives use prices to convey all of the information necessary for efficient decision-making. The resulting incentives are a critical component of both traditional and managed care systems. Provider-focused financial incentives include payment methods, bonuses or withholds, and limits on financial losses. Patient-focused financial incentives may also indirectly influence provider decisions about care, and typically include cost-sharing and benefit provisions. Policies and procedures have been a hallmark of managed care. They rely on closely evaluating the physician, prescribing the decision-making processes, and holding the physician accountable to standard procedures. This approach has traditionally included utilization review to authorize individual physician’s decisions, as well as approaches to care planning such as case managers, discharge planners, and disease management programs. However, procedural mechanisms often incorporate financial incentives in addition to their development of standard procedures and rules. For example, gatekeepers authorize access to specialty care but may have their number of specialty care referrals linked to financial incentives. In these cases the financial incentives are intended to supplement the primary mechanism of influence over provider behavior. Selection and education can refer to the selection and organization of providers and patients, educational interventions directed at either patients or providers, and the comparison of providers to their peers. Provider selection and education attempt to eliminate goal incongruence between individual providers by relying on a relatively complete socialization process. This begins with selecting similar providers and organizing them into groups, and extends to include a wide variety of educational interventions based on the belief that, once informed about the best approach to care, providers will “do the right thing.” The selection and organization of providers into networks can also incorporate financial incentives for patients to see providers within the network. Patient selection and education also impact utilization. Voluntary patient selection into health plans may result in a more homogeneous group of “high-utilizing” or “low-utilizing” enrollees in any specific plan, while direct and indirect patient education improve understanding of the most effective therapies and enhance the participation of patients in their care. Peer comparisons are additional provider-focused mechanisms that directly compare providers with their peers, including audit with feedback and profiling.
Figure.
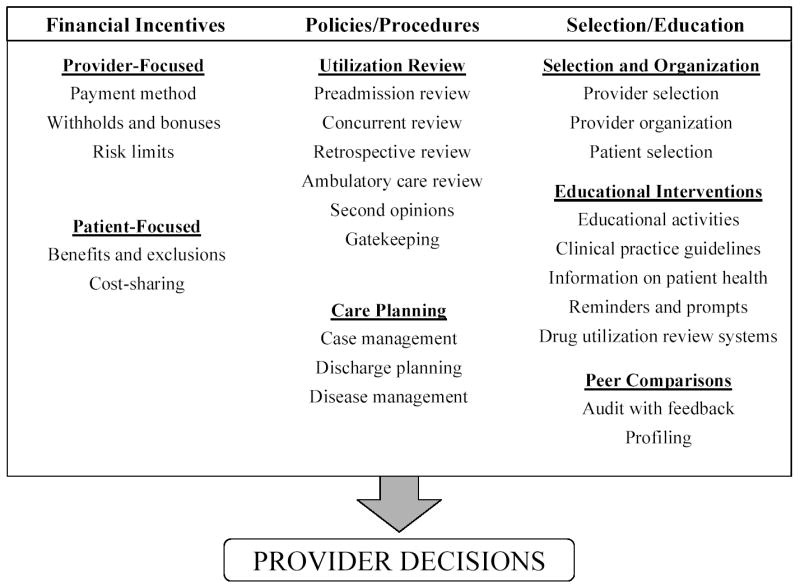
Mechanisms to control physician behavior
FINANCIAL INCENTIVES
Financial incentives rely on monetary prices to convey information for decision-making. All payment systems provide financial incentives, and these incentives are a critical component of both traditional and managed care systems. However, the financial incentives in managed care have received the most attention, particularly risk-based capitation schemes that may discourage appropriate but costly care (Hillman 1987). Financial incentives may be directed at either providers or patients, but both types of incentives may ultimately influence provider decision-making. Provider-focused financial incentives include basic payment methods, bonuses/withholds, and limits on financial losses, while patient-focused incentives typically include cost-sharing and benefit provisions. Managed care has traditionally controlled costs by placing providers at financial risk for their decisions and has relied less on the use of patient cost-sharing and restrictions in covered benefits. These strategies have forced providers into the unpopular dual role of cost-container and patient advocate while leading patients to expect unrestrained access to all covered services. The managed care backlash has begun to reverse these trends by again focusing incentives on the patient, rather than the provider. Employers are viewing increases in cost-sharing and reductions in benefits as supporting rather than restricting employee choices, as exemplified by the shift from defined benefit to defined contribution plans (Robinson 2001).
Provider-focused
Payment methods
Providers can be paid through several mechanisms, including capitation, fee-for-service, or salary. In their simplest form, capitation payments can encourage underuse of expensive services, while fee-for-service payments can encourage overuse, and salary payments encourage neither underuse nor overuse. The average quality of research in this area is quite poor; a recent review of the impact of payment mechanisms on primary care physician behavior identified only six randomized controlled trials and interrupted time series studies that met inclusion criteria out of an initial 5381 gathered by computerized searches of the literature (Gosden et al. 2001). This review concluded that there is some evidence to support an effect on behavior—fee-for-service payment resulted in a higher quantity of primary care services provided compared with either capitation or salary payment, although the impact on the quantity of secondary care services was unclear. However, the complexity of physician payment mechanisms is not completely accounted for by this simple classification for two reasons. First, health plans may contract directly with individual physicians (two-tier plans) or indirectly with physicians through provider groups (three-tier plans), and the effects of physician payment mechanisms at multiple levels are not fully understood (Gold 1999; Kralewski et al. 2000; Conrad et al. 1998). Second, previous analyses have not accounted for spillover effects from physicians who contract with more than one health plan, as financial incentives from one health plan may affect how a physician treats patients in other health plans (Hellinger 1996). Irrespective of these uncertainties about the actual effect of physician payment methods, there has been a shift away from methods such as capitation that put physicians at substantial financial risk.
Withholds, bonuses, and risk limits
Additional financial payments and risk limits can be used to offset the inherent incentives associated with the basic method of physician payment. Although there is little known about the effects of these factors on physician behavior, it does not appear that withholds or bonuses are strongly associated with change in physician practice regardless of whether the intervention targeted cost control (Meyer et al. 2000) or quality improvement (Hillman et al. 1998). The impact of risk limits on physician behavior has not been evaluated. However, as fewer physicians are willing to accept significant financial risk, these types of financial arrangements are likely to increase as a way to create incentives that support high quality care but do not place the provider at substantial risk and do not limit patient choice.
Patient-focused
Benefits and exclusions
Managed care plans traditionally offer a broader range of benefits, but in the current environment broad benefits are also seen as contributing to consumer expectations of unrestrained access. To address this issue, employers are shifting from a defined benefit to a defined contribution system of health insurance coverage (Robinson 2001). From the employers’ perspective, this allows them to remove themselves from the business of determining benefit packages while simultaneously increasing patient choice.
Cost-sharing
Similar to covered benefits, traditional managed care relied less on creating incentives such as cost-sharing that were directed at the patient. But because the percentage of consumer cost-sharing can be varied, it represents an incentive that can be easily “fine-tuned” in response to consumer concerns. In contrast, techniques such as pre-authorization are relatively blunt instruments. The use of cost-sharing is increasing—nominal cost-sharing in managed care plans quadrupled between 1987 and 1993 (Gabel 1997). A cost-sharing requirement may not only reduce the use of services, as demonstrated by the randomized RAND health insurance experiment that started in 1974 (Manning et al. 1987), it can also be used to encourage the use of in-network providers.
POLICIES AND PROCEDURES
Utilization review is a relatively intrusive mechanism of influence that requires physicians to follow a predetermined set of authorization procedures. Utilization review mechanisms include several types of review (preadmission, concurrent, retrospective, and ambulatory care), second opinions, and gatekeeping. Care planning strategies such as case management are usually less intrusive than utilization review and often focus on the small number of patients who are responsible for a large proportion of an organization’s health care costs (Meenan et al. 1999). Care planning mechanisms include case management, discharge planning, and disease management.
Utilization Review
Preadmission review
Preadmission review authorizes hospital admission and approves a certain number of days for the initial hospital stay. Early studies, though often uneven in methodological rigor, suggested that preadmission review for hospitalization was highly effective in reducing hospital admissions by 10 to 15 percent (Wickizer 1990) and use rapidly increased to 80% of all hospital admissions in 1990 (Sullivan and Rice 1991). However, more recent studies of single utilization management programs have concluded that preadmission review rarely denies requests for admission (Wickizer and Lessler 1998b; Lessler and Wickizer 2000; Wickizer and Lessler 1998a; Wickizer, Lessler, and Boyd-Wickizer 1999). This might suggest that preadmission review is not an effective mechanism to control costs, but this finding could also be the result of a sentinel effect, i.e., physicians do not request admission for patients with marginal indicators chiefly because they know their request is going to be reviewed (Lessler and Wickizer 2000). Health care market conditions that permit unnecessary use may be the ones under which preadmission review programs can be most effective (Wheeler and Wickizer 1990), albeit politically unpopular. However, the overall effectiveness of preadmission review is still questioned given evidence that physicians may substitute outpatient for inpatient care (Wickizer, Wheeler, and Feldstein 1991).
Concurrent review
Concurrent review evaluates and approves requests for additional days beyond the initial stay. Approximately one-third of patients approved by preadmission review for inpatient care later request a longer stay through concurrent review (Wickizer and Lessler 1998b; Wickizer, Lessler, and Franklin 1999; Wickizer, Lessler, and Boyd-Wickizer 1999). Concurrent review reduces the average length of stay by 5 to 10 percent (Lessler and Wickizer 2000; Wickizer and Lessler 1998b; Wickizer, Lessler, and Boyd-Wickizer 1999; Wickizer, Lessler, and Franklin 1999) and may reduce costs (Khandker and Manning 1992). Little is known about the effects of concurrent review on patient outcomes, though a few studies have suggested an increased likelihood of readmission (Lessler and Wickizer 2000; Wickizer, Lessler, and Boyd-Wickizer 1999). The overall effectiveness of concurrent review is also unclear, as it is widely believed that physicians assume their request for hospital days is going to be reduced and so regularly inflate the initial request. In addition, if a threshold exists for reductions in length of stay, concurrent review may become less effective as we approach this threshold.
Retrospective review
Retrospective review examines hospital discharge abstract data and patient charts to assess the appropriateness of care after the hospital claim has been submitted for reimbursement (Scheffler, Sullivan, and Ko 1991; Wickizer 1990). This assessment may lead to denial of payment if the hospitalization or treatment patterns were deemed inappropriate or unnecessary. Although it is highly unpopular because payment is denied after services have been rendered, there are several advantages to retrospective review including lower cost and ease of sampling. Unfortunately, this approach relies on the quality of medical records and can produce high rates of inappropriate hospital utilization due to omissions in the medical records (Santos-Eggimann et al. 1997). Only a few studies have evaluated the effectiveness of retrospective review programs. Blue Cross/Blue Shield plans with payment denial programs studied over a nine-year period had 2% lower admissions, 4.4% lower inpatient days, and 2.2% lower lengths of stay, for a total $2 billion savings (Scheffler, Sullivan, and Ko 1991). However, a Canadian survey of hospital CEOs suggested that retrospective review alone was less successful in reducing inappropriate utilization than either concurrent review or combined concurrent and retrospective review (Anderson, Sheps, and Cardiff 1990).
Ambulatory care review
With outpatient costs increasing rapidly, health plans expanded the scope of UR programs to ambulatory care (Wickizer 1995). The preauthorization process for ambulatory care is similar to preadmission and concurrent review of the hospital stay, referring to initial problem assessment and subsequent referral of patients to a specific provider for a fixed number of visits. However, recent evidence from analysis of a large, single UM program representing a national sample of workers’ compensation patients suggests that preauthorization requests are rarely denied for outpatient procedures, and the majority of these denials were eventually reversed after a follow-up request (Wickizer, Lessler, and Franklin 1999). Two exceptions are tonsillectomies for children (Wickizer, Lessler, and Boyd-Wickizer 1999) and outpatient mental health therapy (Koike, Klap, and Unutzer 2000). Two additional types of outpatient expenses often incorporate utilization review, including drugs and durable medical equipment. Prior authorization and formularies appear to be highly cost-effective approaches to decreasing the use of certain expensive drugs that are not indicated by prescribing protocols (Smalley et al. 1995; Motheral and Henderson 1999; Monane, Nagle, and Kelly 1998), although unintended substitution effects may occur (Soumerai et al. 1993). Implementation of a UR program for durable medical equipment also showed significant reductions in order requests, supplier charges, and claims payments; but the cost-saving effects of this program were likely due to reductions in orders because physicians knew their request would be reviewed (the “sentinel effect”) (Wickizer 1995).
Second opinion programs
Second opinion programs require a second physician opinion before approval is given for a procedure. Second surgical opinion programs have been used since the early 1970s to reduce risks and costs attributable to unnecessary and inappropriate surgery, although a rigorous review of this literature concluded that their value remained an open question (Lindsey and Newhouse 1990). Dramatic financial savings in one recent randomized trial ($8.74 for every dollar spent) led the authors to suggest that mandatory second surgical opinion programs may be the most cost-effective program within managed care (Rosenberg et al. 1991). However, others have seen initial reductions in inpatient days and payments but rising inpatient days and payments in subsequent years (Scheffler, Sullivan, and Ko 1991). In an environment where consumers are demanding choice and managed care plans are trying to control costs, second opinions are seen as a way to increase consumer information, choice, and access to care. Six states now require health plans to provide or authorize second opinions (Wagner and Wagner 1999). There is currently widespread use of second opinions; according to data from a nationally representative telephone survey by the Commonwealth Fund, of persons who visited a doctor in the previous year, one in five received a second opinion at an estimated cost of $3.2 billion (Wagner and Wagner 1999).
Gatekeeping
Most often the role of gatekeeper is to authorize access to specialty care and diagnostic tests. This view implies that the physician has essentially been co-opted to review utilization decisions as an agent of the insurance plan, not the patient. Competing views would define the role of the gatekeeper as patient advocate (Franks, Clancy, and Nutting 1992) or as a coordinator of care (Bodenheimer, Lo, and Casalino 1999). However, gatekeeping (as currently practiced) is a profoundly unpopular approach to managing care. Specialists have rebelled against primary care providers in the gatekeeper role, seeing them as competitors rather than colleagues (Bodenheimer, Lo, and Casalino 1999). Patients may also see primary care gatekeepers as interfering with receiving specialty care (Albertson et al. 2000), although many patients do prefer to see their primary care provider first (Grumbach et al. 1999). The unpopularity of gatekeeping overshadows its apparent ability to reduce costs (Rask et al. 1999; Rich et al. 1998; Schoenman, Evans, and Schur 1997), although two recent studies have found conflicting results (Kralewski et al. 2000; Kapur et al. 2000).
Care Planning
Case management and discharge planning
Case management programs focus on identifying high-cost patients as early as possible, assessing alternative treatment plans, and managing health care benefits for these patients as cost effectively as possible (Scheffler, Sullivan, and Ko 1991). The effectiveness of a case management program appears to be highly dependent on the characteristics of the defined cases but may be more effective in selected high-risk populations when the intervention targets cost control (Weinberger et al. 1988), quality improvement (Hickey et al. 2000) or both (Naylor et al. 1994; Naylor et al. 1999). However, other studies have suggested that case management targeting quality improvement may even increase utilization (perhaps related to increased contact with the health care provider) (Weinberger, Oddone, and Henderson 1996; Gagnon et al. 1999) Hospital discharge planning is similar to case management, but limits itself to assessing patients’ needs for treatment after hospitalization and effecting a timely and appropriate discharge (Scheffler, Sullivan, and Ko 1991). Because both strategies are less intrusive than utilization review, they tend to be viewed as relatively beneficial for patients and less burdensome for providers, although some organizations have combined utilization review, internal case management, and discharge planning into one unit, typically named “Transitional Care Planning” or “Continuity of Care Planning” (Potthoff, Kane, and Franco 1997).
Disease management
Disease management is a prospective, disease-specific approach to medical care, born of the pharmaceutical company (Harris 1996; Homer 1997; Bodenheimer 1999; Plocher 1996). These programs either enhance an existing provider network or use a carve-out model that is based on a separate provider network (Plocher 1996). Disease management may be preferable to conventional case management for patients with specific diseases because it focuses on prevention, education, and improvements in long-term outcomes (Plocher 1996; Rector and Venus 1999), although concerns have been raised about the potential for these programs to fragment care (Harris 1996) or lead to undertreatment of unrelated disorders (Redelmeier, Tan, and Booth 1998). The top five diseases for which disease management succeeds, according to pharmaceutical manufacturer’s cost versus benefit analyses, are congestive heart failure (CHF), adolescent and refractory asthma, type I diabetes, AIDS, and carve-out managed cancer (Plocher 1996). However, at least in the case of CHF, the quality of these studies has been questioned because the reported effectiveness of CHF management programs is greater than would be expected based on a review of clinical trials and historical utilization data (Rector and Venus 1999).
SELECTION AND EDUCATION
The selection and education of providers and patients is a relatively indirect and less intrusive mechanism to influence provider decisions. These mechanisms operate through selection and organization processes, educational interventions, or peer comparisons. Managed care organizations select (or attract) providers who fit their needs and who may more closely conform to organizational priorities, then organize them into groups and networks. Patients may also select into certain types of managed care. Once patients and providers are selected for inclusion and organized into a specific structure, educational interventions and peer comparisons encourage further conformity and assume that, once informed, providers and patients will make similar appropriate decisions regarding care. Educational interventions attempt to change specific provider or patient decisions by educating or reminding them about appropriate care, while peer comparisons rely on the provider’s concerns about reputation and desire to conform to profession-wide standards.
Selection and Organization
Provider selection
Physician and hospital networks are important components of managed care. There is little doubt that higher hospital volume is associated with better outcome for a wide variety of surgical procedures and medical conditions (Hewitt 2000). Dudley et al. looked at high quality studies of eleven conditions and estimated that 602 deaths at low volume hospitals were potentially avoidable had those patients been treated at high-volume hospitals (Dudley et al. 2000). Selective HMO contracting for inpatient hospital care has had a major impact on hospital markets (Melnick et al. 1992; Zwanziger, Melnick, and Bamezai 1994), although it is unknown whether the quality of care in these hospitals differs from hospitals with few HMO patients (Schulman et al. 1997).
It is unlikely that health plans systematically manipulate the composition of physician networks on the basis of physician demographic characteristics (Bindman et al. 1998). However, “economic credentialing” to exclude providers with costly practice profiles is believed to be widespread (Blum 1996), and denials and terminations from managed care contracts are relatively common (Bindman et al. 1998). The consequences of this selection process are not completely known. In some cases, quality may be improved by contracting with selected providers, e.g., the reduction in mortality obtained from the use of high volume physicians for percutaneous transluminal coronary angioplasty and percutaneous coronary interventions (McGrath et al. 2000; Hannan et al. 1997). However, consumers and physicians perceive tightly restricted networks as barriers to access rather than quality improvements. Consequently, many managed care organizations are rapidly widening their physician and hospital networks.
Provider organization
Most managed care organizations encourage or require patients to use selected providers (Glied 1999). Staff-model HMOs are organizations that take on risk and usually have a limited number of hospitals and physician employees, while group-model HMOs are usually comprised of a fixed group of physicians who contract exclusively with an organization that takes on insurance risk. These two types of HMOs generally provide the most tightly managed care, and although they predominated in the early 1980s, their market share has declined considerably since then (Wholey et al. 1997). Independent practice associations (IPAs) are an alternative form of HMO organization that operate through non-exclusive contracts with providers and are the most popular form of HMO. Preferred provider organizations (PPOs) also use non-exclusive contracts but negotiate discounted rates with a group of providers. Most importantly, many current health plans combine features that were traditionally associated with one type of organizational form, so the distinctions among types of health plans are becoming blurred (Bazzoli 1998). Given the retreat from tightly managed care, it is likely that the decline in staff-model and group-model plans will continue, while organizational forms that facilitate broad networks of providers will expand and grow.
Patient selection
Because individuals choose their health insurance based on plan characteristics, sicker patients and “high-utilizers” may select into plans with more generous (and expensive) coverage (Frank, Glazer, and McGuire 1998). A health plan might also choose certain coverage characteristics (e.g. child care) to attract young healthy families. There is evidence that consumers may choose plans based on a wide variety of information on price, quality, provider choice, benefits, convenience, demographic characteristics, and health status (Scanlon, Chernew, and Lave 1997). This phenomenon of adverse selection based on plan characteristics has been a major theoretical concern in health insurance markets (Cutler and Zeckhauser 1997). There is considerable empirical evidence that adverse selection has existed (Cutler and Zeckhauser 1997; Glied et al. 1997; Cutler and Reber 1996), although the magnitude of the selection effect may have become smaller over time with the near-disappearance of traditional indemnity plans and the current shift away from closely managed care (Pauly and Nicholson 1999). More recently, the public availability of consumer information on health plans has been a highly popular and widely touted mechanism to improve the consumer decision-making process for plan selection (Edgman-Levitan and Cleary 1996). It is unclear what the impact of these public report cards will be on the selection process; consumers may not have well-defined preferences for performance information and may be vulnerable to manipulation based on how the information is presented (Hibbard, Slovic, and Jewett 1997). However, given their popularity, report cards will likely continue based on the widespread hope that they aid consumers in making informed decisions about their health care.
Educational Interventions
Educational activities
The effectiveness of provider-focused educational activities depends on the approach. According to a rigorous analysis of nearly 100 randomized controlled trials, traditional approaches to educating practicing physicians are relatively ineffective, with formal continuing medical education activities and the provision of educational materials alone having little impact on professional practice (Davis et al. 1995). In contrast to traditional approaches, outreach visits such as academic detailing (targeting individual physicians for education) and education by opinion leaders are effective strategies, though they are also more expensive and labor intensive. Interventions that used combinations of strategies were more effective; studies that used three or more educational strategies in combination had positive results more frequently (79%) than studies that used only two strategies in combination (64%), which, in turn, had positive results more frequently than studies that only used one strategy (60%) (Davis et al. 1995). Overall, these types of provider-focused educational strategies are unintrusive and support provider decision-making, but they do little to enhance consumer choice so they are unlikely to increase substantially in a consumer-focused system.
Two different types of consumer education exist, including direct patient education about specific conditions and the more indirect educational materials from increasingly available resources providing health information to consumers. A randomized controlled trial of a disease self-management program for patients with heart disease, lung disease, stroke, and arthritis suggests that such direct patient education programs are successful in improving behavior and health status and in decreasing rates of hospitalization (Lorig et al. 1999). In a recent randomized household survey, the increasing reliance of patients on more indirect educational materials such as medical reference books, advice nurses, and computers was associated with a decreased reliance on health professionals for information (Wagner, Hu, and Hibbard 2001). The Internet is an increasingly popular method for obtaining such information. Unfortunately, many sites that claim to evaluate health information on the Internet are potentially more harmful than helpful for consumers (Jadad and Gagliardi 1998). Because these educational strategies are directly linked to informing consumer choices, they are very likely to increase over the coming years, particularly as new technologies are developed that can enhance consumer participation in their own health care (e.g., home monitoring systems).
Clinical practice guidelines
Although guidelines are widely used by managed care organizations and medical group practices (Gold et al. 1995; Kerr et al. 1995; Malin et al. 2000), there is conflicting evidence on their effectiveness. Early scientifically rigorous studies suggested that guidelines were successful in improving both the process and outcomes of care (Grimshaw and Russell 1993), although the effectiveness of guidelines in actual clinical practice was questioned (Greco and Eisenberg 1993). A recent systematic review of randomized trials of patient outcomes (17 trials) and costs (1 trial only) found some evidence that guidelines are effective but advised caution in generalizing the results (Thomas et al. 2000). Guidelines appear particularly susceptible to the context in which they are used. For example, formal educational programs for guidelines may be effective in containing costs, while use of a larger number of different guideline applications increased costs (Rich et al. 1998). From the patient perspective, guidelines may also be negatively related to clinician-patient communication, interpersonal treatment, and trust (Safran et al. 2000). In addition, guidelines may become less popular from a provider perspective as physicians surveyed twice over a two-year period increasingly believed that guidelines were being used more for cost containment (71% vs. 92%) than quality improvement (85% vs. 67%) (Inouye et al. 1998). These negative perceptions of guidelines may limit their use in a system that focuses less on ensuring that physicians make “correct” decisions and more on consumer participation in the decision-making process.
Information on patient health status
The provision of feedback on patient health status to health professionals seems to have an effect on the process of care but less of an effect on health outcomes (Espallargues, Valderas, and Alonso 2000). Over half of controlled studies designed to assess feeding back information on perceived health status to health care professionals found differences in at least one of the process indicators (use of health services, diagnosis, or treatment) in the intervention group, but only one-third of these detected significant improvements in patient outcomes. Their conclusions were even more striking for mental health—interventions that evaluated feedback about the patient's mental health status showed a higher rate of diagnosis in the intervention group with no effect on treatment. But although this strategy does not seem highly effective, it is likely to be popular because it provides information to physicians to assist decision-making and increases the involvement of patients in their own care.
There are few studies that examine the effect of feeding back information on patient health status to the patient. Focus groups have suggested that sharing personal health information with the patient or consumer can improve patient understanding, increase motivation to adhere to treatment plans, and improve patient satisfaction (Tang and Newcomb 1998). However, a study of indigent and minority patients at two urban public hospitals indicated that many patients may not be able to use this information effectively due to inadequate health literacy (Williams et al. 1995). Information about a diagnosis can also reduce psychological distress; when 125 women with abnormal Pap smears were alternately assigned to receive a mailed educational brochure about abnormal Pap smears or not, women who received the brochure were significantly less distressed and anxious than were women not receiving the brochure (Stewart et al. 1993). Because the feedback of a patient’s own health information can enhance patient participation in specific health care decisions, this educational method should complement the increased interest in shared physician-patient decision-making (Wennberg 1994).
Reminders and prompts
Provider prompts and reminders are typically used to improve the provision of preventive care and appear to be highly successful approaches. In an analysis of 97 randomized, clinical trials of computerized clinical information services, provider reminders were among the most successful interventions (Balas, Austin et al. 1996). In a review of computerized reminders for preventive care, reminders had positive effects on the provision of care in 74% of 19 studies (Hunt et al. 1998). A recent meta-analysis of 33 randomized studies suggested the overall effect of prompting was to increase preventive care performance by 13% (Balas et al. 2000). Because these strategies enhance physicians’ ability to provide better care as well as consumer knowledge and choices, they are likely to be increasingly useful educational strategies.
Patient prompts and reminders are also successful. A review of randomized clinical trials suggests that these “clinical information systems” are effective in managing care and improving quality (Balas, Austin et al. 1996). Patient reminder systems in primary care settings improve immunization rates, based on a meta-analysis of 41 randomized and non-randomized studies (Szilagyi et al. 2000). Finally, a meta-analysis of over 150 studies assessing the value of interventions to improve patient compliance with medical regimens found that chronic disease patients, including those with diabetes, hypertension, cancer, and mental health problems benefited even more from interventions, but no single intervention was clearly superior (Roter et al. 1998). Interventions that combined cognitive, behavioral, and affective components were more effective than interventions that focused on only one aspect of the chronic disease (Roter et al. 1998). These strategies are both consumer-focused and complementary to provider-focused strategies, strongly enhancing their value in a consumer-focused system.
Drug utilization review systems
Prescription drugs have a high potential for iatrogeny and financial waste. Depending on the target disease, primary care physicians prescribed ineffective drugs in 32% to 88% of orders. Up to 40% of orders resulted in possible drug interactions, age problems, and overdosage (Coste and Venot 1999). Retrospective drug utilization review interventions appear to be effective in reducing prescription drug utilization (Seltzer et al. 2000) and producing significant cost savings (Moore, Gutermuth, and Pracht 2000), but it is not clear that they improve prescribing appropriateness (Spooner, Pickard, and Menon 2000). Computerized drug utilization review programs can evaluate problems in a prospective fashion by alerting the pharmacist immediately; this method has shown moderate success in improving drug prescribing behavior (Monane et al. 1998), but not all studies of online prospective drug utilization review have shown measurable effects (Kidder and Bae 1999). In contrast to online drug utilization review programs that alert the pharmacist, computerized physician order entry (CPOE) immediately alerts physicians about problems with their prescriptions (or other orders). CPOE appears to be a highly effective strategy to reduce adverse drug events (Kohn et al. 2000) and nonintercepted serious medication errors (Bates et al. 1998). Quality improvement strategies focusing on reductions in errors and adverse events are strongly supported by consumers and are increasing rapidly since the publication of the Institute of Medicine’s report on patient safety (Kohn et al. 2000). The necessity to address these serious patient safety concerns may counteract the trend to avoid micromanagement of physician decisions and increase the use of CPOE.
Peer Comparisons
Audit with feedback
Audit with feedback is a summary of a physician’s clinical performance, either alone or in comparison to a peer group or national standard, over a specific period of time (Thomson O'Brien et al. 2000). This strategy has had mixed results. A review of audit with feedback found 10 studies showing positive results and 14 showing negative; the method that was most effective was feedback in the form of chart review (Davis et al. 1995). A review of 37 randomized studies (through June 1997) of audit with feedback suggested that the small positive results of this method be used only in combination with other methods (Thomson O'Brien et al. 2000). The intrusiveness of this strategy depends, to some extent, on who is providing the feedback. Peer feedback is often viewed favorably, while audits by insurers may not be. However, this strategy does not directly support consumer information or choice and so it is unlikely to be affected strongly by the shift to a consumer-focused system.
Profiling
Provider profiling is the performance-based assessment of individual practitioners, known as practice profiles or “report cards” (Kassirer 1994), which identify patterns of care rather than specific clinical decisions (Welch, Miller, and Welch 1994). The use of provider profiling is widespread among managed care (Gold et al. 1995) and medical groups (Kerr et al. 1995). Providers may be profiled on a variety of utilization rates, including ambulatory specialty referrals, ambulatory tests and procedures, hospitalization rates, and pharmaceutical use. Profiling appears to have a modest but significant effect on physician behavior (Balas, Boren et al. 1996) and has been associated with significantly reduced costs in a study of 86 managed care clinics (Kralewski et al. 2000). However, provider profiling has raised a number of concerns. Public profiling (with resulting avoidance of poorly scoring providers) may decrease access to procedures without improving outcomes, although a recent study of bypass surgery providers did not support this (Peterson et al. 1998). Still, public profiling is likely to become an increasingly popular option as employers and insurers try to provide consumers with information to support their choices of providers and health plans. More recent studies have questioned the fundamental validity and reliability of provider profiles (Weiss and Wagner 2000), particularly as most profiles do not include even basic case-mix adjustment of patients in the physicians' panels (Kerr et al. 1995). Even more concerning, profiling individual physicians may encourage physicians to avoid or deselect patients with high prior cost or poor adherence or response to treatments (Hofer et al. 1999).
IMPLICATIONS
We have examined the effectiveness and political feasibility of current strategies to influence physician behavior from the perspective of a consumer-driven health care system. Several patterns are evident. First, all health care systems use financial incentives, but the predominant form of financial incentive is shifting away from physicians to consumers. As capitated payments return to fee-for-service payments, the financial risk faced by physicians is reduced. Instead, patient-focused incentives such as cost-sharing and benefit exclusions will increase in this new consumer-driven system, along with more information and choices. Some physician-focused financial incentives are likely to remain as a way to promote high quality care (e.g., withholds, bonuses, or risk limits), even in a system more focused on the consumer.
Second, heavily procedural strategies such as utilization review and gatekeeping show some evidence of effectiveness but are often highly unpopular due to their restrictions on physician and patient choice, and it is likely that their use will continue to decline. A notable exception is the use of second opinions, which are being viewed as a way to increase consumer information, choice, and access to care. Strategies such as case management and disease management are more popular than either utilization review or gatekeeping, but evidence of their effectiveness is even more uncertain.
Third, a system built on consumer choice is contradicted by provider-focused strategies such as the selection and organization of providers into restricted networks. To address these restrictions, provider networks are expanding to address consumer and provider concerns about barriers to access. In contrast, enhancing a patient’s ability to choose (i.e., select) a health plan is being aggressively pursued by employers and government agencies. Educational interventions (provider and patient) continue to increase in popularity in a consumer-driven system, including the provision of information on the health status of patients, the use of reminders and prompts, and the use of provider profiling. Each of these strategies moves away from the micromanagement of physician decisions and enhances consumer choice and information. Because they move in the opposite direction with regard to micromanagement, clinical practice guidelines may have more limited and voluntary use in a system that values patient participation in decision-making more than monitoring specific physician decisions. Finally, drug utilization review systems (particularly CPOE) may contradict this pattern of retreating from micromanagement. Given that patient safety is a significant political issue with strong consumer support, highly effective tools such as CPOE that address safety concerns may continue to increase as less effective attempts to manage physicians’ decisions disappear.
Based on this analysis, consumer evaluations will make and important contribution but will not be able to substitute completely for external evaluations of quality. Health care consumers do not always comprehend current information on quality (e.g., report cards), and substantial theoretical and empirical work from the decision-making literature finds little support for many assumptions underlying current information dissemination strategies (e.g., that more information is better and that simply providing information will assist consumers) (Hibbard, Slovic, and Jewett 1997). As a result, even in a highly consumer-driven system, some external evaluation of the appropriateness of care is likely to persist. Yet this requires the monitoring of physician decision-making, drawing us back in the direction of physician-focused care management rather than consumer-driven choice. Tools that are being developed to scrutinize patient safety highlight this contradiction and suggest that current strategies to manage health care utilization will not disappear in a consumer-driven health care system.
The cyclical nature of events also suggests that the current trend to consumerism may not continue indefinitely and may reverse over time. As managed care becomes less restrictive, it is losing the power to control costs (Lesser and Ginsberg 2001). If costs increase over time, as suggested by current trends in employer premiums (Gabel et al. 2001), we may see a return to more tightly managed care. Effective but unpopular strategies to control costs (e.g., gatekeeping and preadmission review) may become feasible once again in a political climate focused more on costs and utilization than on consumer choice.
The current movement towards a consumer-driven environment suggests several areas for future research. Few studies have examined interactions between multiple strategies in differing organizational settings over time. Most management strategies have limited effectiveness alone, but combinations of strategies may have synergistic effects. For example, a multifaceted intervention consisting of education, therapeutic reevaluation of eligible patients, and performance feedback, designed to change physician prescribing practices, saw significant positive results, with an estimated annual savings of $1.06 million (Brufsky et al. 1998). This is consistent with a recent systematic review suggesting that audit with feedback had small positive results but was better utilized in combination with other methods (Thomson O'Brien et al. 2000). The use of several slightly different strategies may also be effective. Simultaneous educational interventions based on multiple behavioral factors was more likely to influence doctors’ use of tests (Solomon et al. 1998), and retrospective review combined with concurrent review was also more successful in reducing inappropriate utilization than retrospective review alone (Anderson, Sheps, and Cardiff 1990). However, most of these studies have examined the usefulness of multiple simultaneous interventions of similar type (e.g. educational interventions). Little is known about the synergies between multiple consumer- and physician-focused strategies, and studies should be designed to explore these interactive effects. The relative effectiveness of consumer-focused interventions also needs to be compared to physician-focused interventions and weighed against their cost. Finally, this new environment also implies changes in the responsibilities of providers and consumers, signifying that the role of personal responsibility for health needs to be evaluated as well. As a result, the protection of vulnerable subgroups cannot be forgotten. A consumer-driven system requires that people are able to participate (Hibbard, Slovic, and Jewett 1997), and those who are unable to participate could be disadvantaged even further in this new environment.
Footnotes
Funding: This study was supported by a grant (RO1-AG-19747) from the National Institute on Aging. Kathryn Flynn was supported by funding from the Center for Demography in Health and Aging at the University of Wisconsin-Madison.
References
- Albertson GA, Lin CT, Kutner J, Schilling LM, Anderson SN, Anderson RJ. Recognition of patient referral desires in an academic managed care plan frequency, determinants, and outcomes. Journal of General Internal Medicine. 2000;15 (4):242–7. doi: 10.1111/j.1525-1497.2000.02208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Sheps SB, Cardiff K. Hospital-based utilization management: a cross-Canada survey. Canadian Medical Association Journal. 1990;143 (10):1025–30. [PMC free article] [PubMed] [Google Scholar]
- Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. The clinical value of computerized information services. A review of 98 randomized clinical trials. Archives of Family Medicine. 1996;5 (5):271–8. doi: 10.1001/archfami.5.5.271. [DOI] [PubMed] [Google Scholar]
- Balas EA, Boren SA, Brown GD, Ewigman BG, Mitchell JA, Perkoff GT. Effect of physician profiling on utilization. Meta-analysis of randomized clinical trials. Journal of General Internal Medicine. 1996;11 (10):584–90. doi: 10.1007/BF02599025. [DOI] [PubMed] [Google Scholar]
- Balas EA, Weingarten S, Garb CT, Blumenthal D, Boren SA, Brown GD. Improving preventive care by prompting physicians. Archives of Internal Medicine. 2000;160 (3):301–8. doi: 10.1001/archinte.160.3.301. [DOI] [PubMed] [Google Scholar]
- Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Journal of the American Medical Association. 1998;280 (15):1311–6. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ. Getting at the management of care within managed care. Health Services Research. 1998;32 (6):735–9. [PMC free article] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Vranizan K, Jaffe D, Osmond D. Selection and exclusion of primary care physicians by managed care organizations. Journal of the American Medical Association. 1998;279 (9):675–9. doi: 10.1001/jama.279.9.675. [DOI] [PubMed] [Google Scholar]
- Blum JD. The evolution of physician credentialing into managed care selective contracting. American Journal of Law and Medicine. 1996;22 (2–3):173–203. [PubMed] [Google Scholar]
- Bodenheimer T. Disease management--promises and pitfalls. New England Journal of Medicine. 1999;340 (15):1202–5. doi: 10.1056/NEJM199904153401511. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Lo B, Casalino L. Primary care physicians should be coordinators, not gatekeepers. Journal of the American Medical Association. 1999;281 (21):2045–9. doi: 10.1001/jama.281.21.2045. [DOI] [PubMed] [Google Scholar]
- Brufsky JW, Ross-Degnan D, Calabrese D, Gao X, Soumerai SB. Shifting physician prescribing to a preferred histamine-2-receptor antagonist. Effects of a multifactorial intervention in a mixed-model health maintenance organization. Medical Care. 1998;36 (3):321–32. doi: 10.1097/00005650-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Conrad DA, Maynard C, Cheadle A, Ramsey S, Marcus-Smith M, Kirz H, Madden CA, Martin D, Perrin EB, Wickizer T, Zierler B, Ross A, Noren J, Liang SY. Primary care physician compensation method in medical groups: does it influence the use and cost of health services for enrollees in managed care organizations? Journal of the American Medical Association. 1998;279 (11):853–8. doi: 10.1001/jama.279.11.853. [DOI] [PubMed] [Google Scholar]
- Coste J, Venot A. An epidemiologic approach to drug prescribing quality assessment: a study in primary care practice in France. Medical Care. 1999;37 (12):1294–307. doi: 10.1097/00005650-199912000-00012. [DOI] [PubMed] [Google Scholar]
- Cutler DM, Reber S. Paying for health insurance: the tradeoff between competition and adverse selection. Cambridge, MA: National Bureau of Economic Research; 1996. [Google Scholar]
- Cutler DM, Zeckhauser RJ. Adverse selection in health insurance. Cambridge, MA: National Bureau of Economic Research; 1997. [Google Scholar]
- Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. Journal of the American Medical Association. 1995;274 (9):700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. Journal of the American Medical Association. 2000;283 (9):1159–66. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- Edgman-Levitan S, Cleary PD. What information do consumers want and need? Health Affairs. 1996;15 (4):42–56. doi: 10.1377/hlthaff.15.4.42. [DOI] [PubMed] [Google Scholar]
- Espallargues M, Valderas JM, Alonso J. Provision of feedback on perceived health status to health care professionals: a systematic review of its impact. Medical Care. 2000;38 (2):175–86. doi: 10.1097/00005650-200002000-00007. [DOI] [PubMed] [Google Scholar]
- Frank RG, Glazer J, McGuire TG. Measuring adverse selection in managed health care. Cambridge, MA: National Bureau of Economic Research; 1998. [DOI] [PubMed] [Google Scholar]
- Franks P, Clancy CM, Nutting PA. Gatekeeping revisited--protecting patients from overtreatment. New England Journal of Medicine. 1992;327 (6):424–9. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- Gabel J. Ten ways HMOs have changed during the 1990s. Health Affairs (Millwood) 1997;16 (3):134–45. doi: 10.1377/hlthaff.16.3.134. [DOI] [PubMed] [Google Scholar]
- Gabel J, Levitt L, Pickreign J, Whitmore H, Holve E, Rowland D, Dhont K, Hawkins S. Job-based health insurance in 2001: inflation hits double digits, managed care retreats. Health Affairs (Millwood) 2001;20 (5):180–6. doi: 10.1377/hlthaff.20.5.180. [DOI] [PubMed] [Google Scholar]
- Gagnon AJ, Schein C, McVey L, Bergman H. Randomized controlled trial of nurse case management of frail older people. Journal of the American Geriatrics Society. 1999;47 (9):1118–24. doi: 10.1111/j.1532-5415.1999.tb05238.x. [DOI] [PubMed] [Google Scholar]
- Glied S. Managed care. Cambridge, MA: National Bureau of Economic Research; 1999. [Google Scholar]
- Glied S, Sisk J, Gorman S, Ganz M. Selection, marketing, and Medicaid managed care. Cambridge, MA: National Bureau of Economic Research; 1997. [Google Scholar]
- Gold M. Financial incentives: current realities and challenges for physicians. Journal of General Internal Medicine. 1999;14:S6–S12. doi: 10.1046/j.1525-1497.1999.00260.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MR, Hurley R, Lake T, Ensor T, Berenson R. A national survey of the arrangements managed-care plans make with physicians. New England Journal of Medicine. 1995;333 (25):1678–83. doi: 10.1056/NEJM199512213332505. [DOI] [PubMed] [Google Scholar]
- Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, Sergison M, Pedersen L. Impact of payment method on behaviour of primary care physicians: a systematic review. Journal of Health Services Research and Policy. 2001;6 (1):44–55. doi: 10.1258/1355819011927198. [DOI] [PubMed] [Google Scholar]
- Greco PJ, Eisenberg JM. Changing physicians' practices. New England Journal of Medicine. 1993;329 (17):1271–1273. doi: 10.1056/NEJM199310213291714. [DOI] [PubMed] [Google Scholar]
- Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342 (8883):1317–22. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Selby JV, Damberg C, Bindman AB, Quesenberry C, Jr, Truman A, Uratsu C. Resolving the gatekeeper conundrum: what patients value in primary care and referrals to specialists. Journal of the American Medical Association. 1999;282 (3):261–6. doi: 10.1001/jama.282.3.261. [DOI] [PubMed] [Google Scholar]
- Hannan EL, Racz M, Ryan TJ, McCallister BD, Johnson LW, Arani DT, Guerci AD, Sosa J, Topol EJ. Coronary angioplasty volume-outcome relationships for hospitals and cardiologists. Journal of the American Medical Association. 1997;277 (11):892–8. [PubMed] [Google Scholar]
- Harris JM., Jr Disease management: new wine in new bottles? Annals of Internal Medicine. 1996;124 (9):838–42. doi: 10.7326/0003-4819-124-9-199605010-00009. [DOI] [PubMed] [Google Scholar]
- Hellinger FJ. The impact of financial incentives on physician behavior in managed care plans: a review of the evidence. Medical Care Research and Review. 1996;53 (3):294–314. doi: 10.1177/107755879605300305. [DOI] [PubMed] [Google Scholar]
- Maria Hewitt. Interpreting the volume-outcome relationship in the context of health care quality. Washington D.C.: Institute of Medicine; 2000. [Google Scholar]
- Hibbard JH, Slovic P, Jewett JJ. Informing consumer decisions in health care: implications from decision- making research. Milbank Quarterly. 1997;75 (3):395–414. doi: 10.1111/1468-0009.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey ML, Cook EF, Rossi LP, Connor J, Dutkiewicz C, Hassan SM, Fay M, Lee TH, Fairchild DG. Effect of case managers with a general medical patient population. Journal of Evaluation in Clinical Practice. 2000;6 (1):23–9. doi: 10.1046/j.1365-2753.2000.00215.x. [DOI] [PubMed] [Google Scholar]
- Hillman AL. Financial incentives for physicians in HMOs. Is there a conflict of interest? New England Journal of Medicine. 1987;317 (27):1743–8. doi: 10.1056/NEJM198712313172725. [DOI] [PubMed] [Google Scholar]
- Hillman AL, Ripley K, Goldfarb N, Nuamah I, Weiner J, Lusk E. Physician financial incentives and feedback: failure to increase cancer screening in Medicaid managed care. American Journal of Public Health. 1998;88 (11):1699–701. doi: 10.2105/ajph.88.11.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician "report cards" for assessing the costs and quality of care of a chronic disease. Journal of the American Medical Association. 1999;281 (22):2098–105. doi: 10.1001/jama.281.22.2098. [DOI] [PubMed] [Google Scholar]
- Homer CJ. Asthma disease management. New England Journal of Medicine. 1997;337 (20):1461–3. doi: 10.1056/NEJM199711133372010. [DOI] [PubMed] [Google Scholar]
- Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. Journal of the American Medical Association. 1998;280 (15):1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- Inouye J, Kristopatis R, Stone E, Pelter M, Sandhu M, Weingarten S. Physicians' changing attitudes toward guidelines. Journal of General Internal Medicine. 1998;13 (5):324–6. doi: 10.1046/j.1525-1497.1998.00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Gagliardi A. Rating health information on the Internet - Navigating to knowledge or to Babel? Journal of the American Medical Association. 1998;279 (8):611–614. doi: 10.1001/jama.279.8.611. [DOI] [PubMed] [Google Scholar]
- Kapur K, Joyce GF, Van Vorst KA, Escarce JJ. Expenditures for physician services under alternative models of managed care. Medical Care Research and Review. 2000;57 (2):161–81. doi: 10.1177/107755870005700202. [DOI] [PubMed] [Google Scholar]
- Kassirer JP. The use and abuse of practice profiles. New England Journal of Medicine. 1994;330 (9):634–636. doi: 10.1056/NEJM199403033300910. [DOI] [PubMed] [Google Scholar]
- Kerr EA, Mittman BS, Hays RD, Siu AL, Leake B, Brook RH. Managed care and capitation in California: how do physicians at financial risk control their own utilization? Annals of Internal Medicine. 1995;123 (7):500–504. doi: 10.7326/0003-4819-123-7-199510010-00004. [DOI] [PubMed] [Google Scholar]
- Khandker RK, Manning WG. The impact of utilization review on costs and utilization. Developments in Health Economics and Public Policy. 1992;1:47–62. doi: 10.1007/978-94-011-2392-1_3. [DOI] [PubMed] [Google Scholar]
- Kidder David, Jay Bae. Evaluation results from prospective drug utilization review: Medicaid demonstrations. Health Care Financing Review. 1999;20 (3):107–18. [PMC free article] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS Committee on Quality of Health Care in America, and Institute of Medicine. To err is human: building a safer health system. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Koike A, Klap R, Unutzer J. Utilization management in a large managed behavioral health organization. Psychiatric Services. 2000;51 (5):621–6. doi: 10.1176/appi.ps.51.5.621. [DOI] [PubMed] [Google Scholar]
- Kralewski JE, Rich EC, Feldman R, Dowd BE, Bernhardt T, Johnson C, Gold W. The effects of medical group practice and physician payment methods on costs of care. Health Services Research. 2000;35 (3):591–613. [PMC free article] [PubMed] [Google Scholar]
- Landon BE, Wilson IB, Cleary PD. A conceptual model of the effects of health care organizations on the quality of medical care. Journal of the American Medical Association. 1998;279 (17):1377–82. doi: 10.1001/jama.279.17.1377. [DOI] [PubMed] [Google Scholar]
- Lesser CS, Ginsberg PB. Back to the future? New cost and access challenges emerge. Washington D.C.: Center for Studying Health Systems Change; 2001. [PubMed] [Google Scholar]
- Lessler DS, Wickizer TM. The impact of utilization management on readmissions among patients with cardiovascular disease. Health Services Research. 2000;34 (6):1315–29. [PMC free article] [PubMed] [Google Scholar]
- Lindsey PA, Newhouse JP. The cost and value of second surgical opinion programs: a critical review of the literature. Journal of Health Politics, Policy and Law. 1990;15 (3):543–70. doi: 10.1215/03616878-15-3-543. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, Gonzalez VM, Laurent DD, Holman HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization - A randomized trial. Medical Care. 1999;37 (1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Malin JL, Kahn K, Dulai G, Farmer MM, Rideout J, Simon LP, Ganz PA. Organizational systems used by California capitated medical groups and independent practice associations to increase cancer screening. Cancer. 2000;88 (12):2824–31. [PubMed] [Google Scholar]
- Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS. Health insurance and the demand for medical care: evidence from a randomized experiment. American Economic Review. 1987;77 (3):251–277. [PubMed] [Google Scholar]
- McGrath PD, Wennberg DE, Dickens JD, Jr, Siewers AE, Lucas FL, Malenka DJ, Kellett, MA, Jr, Ryan TJ., Jr Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. Journal of the American Medical Association. 2000;284 (24):3139–44. doi: 10.1001/jama.284.24.3139. [DOI] [PubMed] [Google Scholar]
- Meenan RT, O'Keeffe-Rosetti C, Hornbrook MC, Bachman DJ, Goodman MJ, Fishman PA, Hurtado AV. The sensitivity and specificity of forecasting high-cost users of medical care. Medical Care. 1999;37 (8):815–23. doi: 10.1097/00005650-199908000-00011. [DOI] [PubMed] [Google Scholar]
- Melnick GA, Zwanziger J, Bamezai A, Pattison R. The effects of market structure and bargaining position on hospital prices. Journal of Health Economics. 1992;11 (3):217–33. doi: 10.1016/0167-6296(92)90001-h. [DOI] [PubMed] [Google Scholar]
- Meyer CM, Ladenson PW, Scharfstein JA, Danese MD, Powe NR. Evaluation of common problems in primary care: effects of physician, practice, and financial characteristics. American Journal of Managed Care. 2000;6 (4):457–69. [PubMed] [Google Scholar]
- Monane M, Matthias DM, Nagle BA, Kelly MA. Improving prescribing patterns for the elderly through an online drug utilization review intervention: a system linking the physician, pharmacist, and computer. Journal of the American Medical Association. 1998;280 (14):1249–52. doi: 10.1001/jama.280.14.1249. [DOI] [PubMed] [Google Scholar]
- Monane M, Nagle B, Kelly MA. Pharmacotherapy: strategies to control drug costs in managed care. Geriatrics. 1998;53(9):51–4. 63; quiz 64. [PubMed] [Google Scholar]
- Moore WJ, Gutermuth K, Pracht EE. Systemwide effects of Medicaid retrospective drug utilization review programs. Journal of Health Politics, Policy and Law. 2000;25 (4):653–88. doi: 10.1215/03616878-25-4-653. [DOI] [PubMed] [Google Scholar]
- Motheral BR, Henderson R. The effect of a closed formulary on prescription drug use and costs. Inquiry. 1999;36 (4):481–91. [PubMed] [Google Scholar]
- Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Annals of Internal Medicine. 1994;120 (12):999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. Journal of the American Medical Association. 1999;281 (7):613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Ouchi WG. A conceptual framework for the design of organizational control mechanisms. Management Science. 1979;25 (9):833–848. [Google Scholar]
- Pauly M, Nicholson S. Adverse consequences of adverse selection. Journal of Health Politics, Policy and Law. 1999;24 (5):921–30. doi: 10.1215/03616878-24-5-921. [DOI] [PubMed] [Google Scholar]
- Peterson ED, DeLong ER, Jollis JG, Muhlbaier LH, Mark DB. The effects of New York's bypass surgery provider profiling on access to care and patient outcomes in the elderly. Journal of the American College of Cardiology. 1998;32 (4):993–9. doi: 10.1016/s0735-1097(98)00332-5. [DOI] [PubMed] [Google Scholar]
- Plocher DW. Disease Management. In: Kongstvedt PR, editor. The Managed Health Care Handbook. Gatihersburg, Maryland: Aspen Publishers, Inc; 1996. [Google Scholar]
- Potthoff S, Kane RL, Franco SJ. Improving hospital discharge planning for elderly patients. Health Care Financing Review. 1997;19 (2):47–72. [PMC free article] [PubMed] [Google Scholar]
- Rask KJ, Deaton C, Culler SD, Kohler SA, Morris DC, Alexander WA, Pope RG, Weintraub WS. The effect of primary care gatekeepers on the management of patients with chest pain. American Journal of Managed Care. 1999;5 (10):1274–82. [PubMed] [Google Scholar]
- Rector TS, Venus PA. Judging the value of population-based disease management. Inquiry. 1999;36 (2):122–6. [PubMed] [Google Scholar]
- Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. New England Journal of Medicine. 1998;338 (21):1516–1542. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- Rich EC, Kralewski J, Feldman R, Dowd B, Bernhardt TS. Variations in the management of primary care: effect on cost in an HMO network. Archives of Internal Medicine. 1998;158 (21):2363–71. doi: 10.1001/archinte.158.21.2363. [DOI] [PubMed] [Google Scholar]
- Robinson JC. The end of managed care. Journal of the American Medical Association. 2001;285 (20):2622–8. doi: 10.1001/jama.285.20.2622. [DOI] [PubMed] [Google Scholar]
- Rosenberg SN, Perlis H, Lynne D, Leto L. A second look at second surgical opinions. Business and Health. 1991;9(2):14–6. 19, 22 passim. [PubMed] [Google Scholar]
- Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Medical Care. 1998;36 (8):1138–61. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Safran DG, Rogers WH, Tarlov AR, Inui T, Taira DA, Montgomery JE, Ware JE, Slavin CP. Organizational and financial characteristics of health plans: are they related to primary care performance? Archives of Internal Medicine. 2000;160 (1):69–76. doi: 10.1001/archinte.160.1.69. [DOI] [PubMed] [Google Scholar]
- Santos-Eggimann B, Sidler M, Schopfer D, Blanc T. Comparing results of concurrent and retrospective designs in a hospital utilization review. International Journal for Quality in Health Care. 1997;9 (2):115–20. doi: 10.1093/intqhc/9.2.115. [DOI] [PubMed] [Google Scholar]
- Scanlon DP, Chernew M, Lave JR. Consumer health plan choice: current knowledge and future directions. Annual Review of Public Health. 1997;18:507–28. doi: 10.1146/annurev.publhealth.18.1.507. [DOI] [PubMed] [Google Scholar]
- Scheffler RM, Sullivan SD, Ko TH. The impact of Blue Cross and Blue Shield Plan utilization management programs, 1980–1988. Inquiry. 1991;28 (3):263–75. [PubMed] [Google Scholar]
- Schoenman JA, Evans WN, Schur CL. Primary care case management for Medicaid recipients: evaluation of the Maryland Access to Care program. Inquiry. 1997;34 (2):155–70. [PubMed] [Google Scholar]
- Schulman KA, Rubenstein LE, Seils DM, Harris M, Hadley J, Escarce JJ. Quality assessment in contracting for tertiary care services by HMOs: a case study of three markets. Joint Commission Journal on Qualilty Improvement. 1997;23 (2):117–27. doi: 10.1016/s1070-3241(16)30304-2. [DOI] [PubMed] [Google Scholar]
- Seltzer JK, Kurt TL, Knodel LC, Dean B, Burch C. Drug utilization review of sedative/hypnotic agents in Texas Medicaid patients. Texas Medicaid Vendor Drug Program Drug Utilization Review Board. Journal of the American Pharmaceutical Association. 2000;40 (4):495–9. [PubMed] [Google Scholar]
- Smalley WE, Griffin MR, Fought RL, Sullivan L, Ray WA. Effect of a prior-authorization requirement on the use of nonsteroidal antiinflammatory drugs by Medicaid patients. New England Journal of Medicine. 1995;332 (24):1612–7. doi: 10.1056/NEJM199506153322406. [DOI] [PubMed] [Google Scholar]
- Solomon DH, Hashimoto H, Daltroy L, Liang MH. Techniques to improve physicians' use of diagnostic tests: a new conceptual framework. Journal of the American Medical Association. 1998;280 (23):2020–7. doi: 10.1001/jama.280.23.2020. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, Ross-Degnan D, Fortess EE, Abelson J. A critical analysis of studies of state drug reimbursement policies: research in need of discipline. Milbank Quarterly. 1993;71 (2):217–52. [PubMed] [Google Scholar]
- Spooner CH, Pickard AS, Menon D. Edmonton Quality Assessment Tool for Drug Utilization Reviews: EQUATDUR- 2: the development of a scale to assess the methodological quality of a drug utilization review. Medical Care. 2000;38 (9):948–58. doi: 10.1097/00005650-200009000-00008. [DOI] [PubMed] [Google Scholar]
- Stewart DE, Lickrish GM, Sierra S, Parkin H. The effect of educational brochures on knowledge and emotional distress in women with abnormal Papanicolaou smears. Obstetrics and Gynecology. 1993;81 (2):280–2. [PubMed] [Google Scholar]
- Sullivan CB, Rice T. The health insurance picture in 1990. Health Affairs. 1991;10 (2):104–15. doi: 10.1377/hlthaff.10.2.104. [DOI] [PubMed] [Google Scholar]
- Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, Rodewald LE. Effect of patient reminder/recall interventions on immunization rates: A review. Journal of the American Medical Association. 2000;284 (14):1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- Tang PC, Newcomb C. Informing patients: a guide for providing patient health information. Journal of the American Medical Informatics Association. 1998;5 (6):563–70. doi: 10.1136/jamia.1998.0050563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas L, Cullum N, McColl E, Rousseau N, Soutter J, Steen N. Guidelines in professions allied to medicine. Cochrane Database of Systematic Reviews. 2000;2 doi: 10.1002/14651858.CD000349. [DOI] [PubMed] [Google Scholar]
- Thomson O'Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews. 2000;2 doi: 10.1002/14651858.CD000259. [DOI] [PubMed] [Google Scholar]
- Wagner TH, Hu TW, Hibbard JH. The demand for consumer health information. Journal of Health Economics. 2001;20 (6):1059–1075. doi: 10.1016/s0167-6296(01)00107-2. [DOI] [PubMed] [Google Scholar]
- Wagner TH, Wagner LS. Who gets second opinions? Health Affairs. 1999;18 (5):137–45. doi: 10.1377/hlthaff.18.5.137. [DOI] [PubMed] [Google Scholar]
- Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. New England Journal of Medicine. 1996;334 (22):1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- Weinberger M, Smith DM, Katz BP, Moore PS. The cost-effectiveness of intensive postdischarge care. A randomized trial. Medical Care. 1988;26 (11):1092–102. doi: 10.1097/00005650-198811000-00007. [DOI] [PubMed] [Google Scholar]
- Weiss KB, Wagner R. Performance measurement through audit, feedback, and profiling as tools for improving clinical care. Chest. 2000;118 (2 Suppl):53S–58S. doi: 10.1378/chest.118.2_suppl.53s. [DOI] [PubMed] [Google Scholar]
- Welch HG, Miller ME, Welch WP. Physician profiling. An analysis of inpatient practice patterns in Florida and Oregon. New England Journal of Medicine. 1994;330 (9):607–12. doi: 10.1056/NEJM199403033300906. [DOI] [PubMed] [Google Scholar]
- Wennberg JE. Health care reform and professionalism. Inquiry. 1994;31 (3):296–302. [PubMed] [Google Scholar]
- Wheeler JR, Wickizer TM. Relating health care market characteristics to the effectiveness of utilization review programs. Inquiry. 1990;27 (4):344–51. [PubMed] [Google Scholar]
- Wholey DR, Christianson JB, Engberg J, Bryce C. HMO market structure and performance: 1985–1995. Health Affairs. 1997;16 (6):75–84. doi: 10.1377/hlthaff.16.6.75. [DOI] [PubMed] [Google Scholar]
- Wickizer TM. The effect of utilization review on hospital use and expenditures: a review of the literature and an update on recent findings. Medical Care Review. 1990;47 (3):327–63. doi: 10.1177/107755879004700303. [DOI] [PubMed] [Google Scholar]
- ———. Controlling outpatient medical equipment costs through utilization management. Medical Care. 1995;33 (4):383–91. doi: 10.1097/00005650-199504000-00005. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Lessler D. Do treatment restrictions imposed by utilization management increase the likelihood of readmission for psychiatric patients? Medical Care. 1998a;36 (6):844–50. doi: 10.1097/00005650-199806000-00008. [DOI] [PubMed] [Google Scholar]
- ———. Effects of utilization management on patterns of hospital care among privately insured adult patients. Medical Care. 1998b;36 (11):1545–54. doi: 10.1097/00005650-199811000-00004. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Lessler D, Boyd-Wickizer J. Effects of health care cost-containment programs on patterns of care and readmissions among children and adolescents. American Journal of Public Health. 1999;89 (9):1353–8. doi: 10.2105/ajph.89.9.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickizer TM, Lessler D, Franklin G. Controlling workers' compensation medical care use and costs through utilization management. Journal of Occupational and Environmental Medicine. 1999;41 (8):625. doi: 10.1097/00043764-199908000-00003. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Wheeler JR, Feldstein PJ. Have hospital inpatient cost containment programs contributed to the growth in outpatient expenditures? Analysis of the substitution effect associated with hospital utilization review. Medical Care. 1991;29 (5):442–51. doi: 10.1097/00005650-199105000-00005. [DOI] [PubMed] [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. Journal of the American Medical Association. 1995;274 (21):1677–82. [PubMed] [Google Scholar]
- Zwanziger J, Melnick GA, Bamezai A. Costs and price competition in California hospitals, 1980–1990. Health Affairs. 1994;13 (4):118–26. doi: 10.1377/hlthaff.13.4.118. [DOI] [PubMed] [Google Scholar]


