Intermittent claudication is pain affecting the calf, and less commonly the thigh and buttock, that is induced by exercise and relieved by rest. Symptom severity varies from mild to severe. Intermittent claudication occurs as a result of muscle ischaemia during exercise caused by obstruction to arterial flow. It is a common problem, with a prevalence of 0.6-10%1 which increases significantly with age. Almost a fifth of the population over the age of 65 has intermittent claudication,2 and, as a result of demographic changes in many developed countries, its prevalence in the general population is likely to rise dramatically over the next 20 years.
Summary points
Intermittent claudication is a common condition and in most cases is easily diagnosed
It is associated with a significantly increased risk of death from cardiovascular disease
Only a small proportion of patients with claudication require revascularisation
The main treatment aim is to reduce the risk of mortality from cardiovascular events
Smoking cessation, control of hypertension and diabetes, and prescription of statins and antiplatelet drugs are key elements for treating the condition
Exercise, angioplasty, and bypass surgery can improve symptoms of claudication
Intermittent claudication has a negative impact on various aspects of quality of life3 and on affected people's ability to continue to work. Its socioeconomic impact has not been evaluated but is likely to be considerable. More importantly, people with intermittent claudication have a significantly increased mortality risk. However, many people with the condition do not consult a doctor, and often doctors are unaware that their patients have the condition.w1 Early diagnosis and risk factor control by primary care doctors is critical to reducing the mortality associated with claudication. This review presents current knowledge on the diagnosis, natural course, and management of intermittent claudication.
Search strategy
I searched the Cochrane Library for relevant systematic reviews on management of intermittent claudication and used Clinical Evidence to assess clinically relevant benefits and harms of different treatments. I performed Medline searches to find relevant reviews on the natural course, diagnosis, and treatment of the condition.
Who gets it?
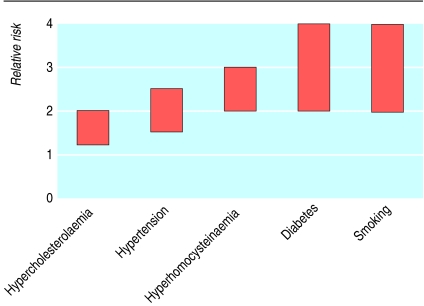
In the vast majority of cases atherosclerosis is the underlying pathology in intermittent claudication. Cigarette smoking is by far the most potent risk factor for development of peripheral atherosclerosis and intermittent claudication (fig 1), increasing the risk at least threefold, and the higher the numbers of pack years the more severe the disease.4 Other major risk factors are increasing age,5 diabetes,6 hypertension,4 hyperlipidaemia,w2 and hyperhomocysteinaemia.w3 In younger patients intermittent claudication may be caused by conditions such as popliteal artery entrapment,w4 cystic adventitial disease,w5 fibromuscular dysplasia,w6 and external compression syndromes (which occur in high intensity athletes such as professional cyclists).w7
Fig 1 Effects of various risk factors on relative risk of developing intermittent claudication4 6 w2 w3
How is it diagnosed?
The diagnosis of intermittent claudication is based on a classic history of cramping muscle pain that occurs after the same degree of exercise and which is quickly relieved by rest. However, other conditions such as nerve root compression, spinal stenosis, hip arthritis, symptomatic Baker's cyst, venous claudication, and chronic compartment syndrome may mimic the symptoms of intermittent claudication. Typically the pain from nerve root compression tends to radiate down the back of the leg and is described as sharp lancinating pain, which is sometimes relieved by adjusting the position of the back (such as leaning forward). In spinal stenosis motor weakness may be present. Concomitant lumbosacral spine disease and peripheral arterial disease may cause difficulty in identifying which of the two conditions is the main cause of symptoms.
Absent or reduced peripheral pulses or the presence of audible bruits supports the diagnosis of intermittent claudication, but some patients with the condition will have normally palpable pulses and no bruits. A low ankle-brachial pressure index (<0.9) also supports the diagnosis. However, the presence of palpable pulses or a normal resting ankle-brachial pressure index (>0.9) does not rule out the diagnosis. If the clinical history is highly suggestive of intermittent claudication and the ankle-brachial pressure index is normal, an exercise ankle-brachial pressure index should be performed. If a substantial drop in ankle pressure is observed after exercise and at the same time as symptoms develop, a diagnosis of intermittent claudication can confidently be made.w8 In patients with an ankle-brachial pressure index >1.3 the result is likely to be artefactual secondary to heavily calcified vessels, and a toe-ankle brachial pressure index should be calculated.
What is the prognosis?
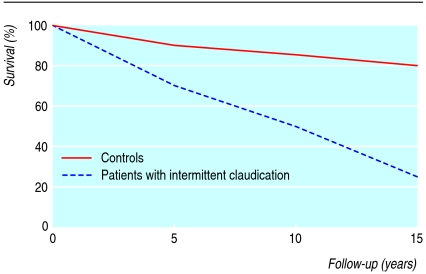
Patients with intermittent claudication have a significantly higher mortality than age matched controls, about 12% a year (fig 2).6 Of these deaths, 66% are due to heart disease, and 10% are due to strokes. Increasing age, cigarette smoking, diabetes and lower ankle-brachial pressure index are independent risk factors for mortality.
Fig 2 Survival in patients with intermittent claudication compared with age matched healthy controls6
The natural course of intermittent claudication is benign for the leg affected, with few patients ever requiring intervention or amputation. Only one in four patients with intermittent claudication will develop any deterioration in symptoms. Multiple longitudinal studies have shown that the amputation rate in this group of patients is only 1-7% at 5-10 years.7 w9 w10 At 10 years, fewer than one in five patients will undergo any form of revascularisation of the leg.7
Tips for non-specialists
Recognise the symptoms of intermittent claudication early
Ideally, confirm the diagnosis by measuring ankle-brachial pressure indices in the community
Identify risk factors for atherosclerosis and start treatments to control them—smoking cessation, diabetic control, antiplatelet drugs, antihypertensives, statins—and encourage exercise
Refer patients to a specialist if the diagnosis is uncertain or if claudication is disabling
How is it treated?
People with peripheral arterial disease have the same risk of death from cardiovascular causes as those with a history of coronary or cerebrovascular disease.8 Treatment of intermittent claudication should therefore be on two fronts. Firstly, treatment should be targeted at reducing the risk from cardiovascular events through secondary prevention. Secondly, treatment should aim to improve the symptoms of claudication.
Secondary risk factor modification
Smoking cessation
Smoking cessation reduces the risk of death from cardiovascular causes. Patients with peripheral arterial disease who continue to smoke have an increased rate of progression of atherosclerosis as well as an increased risk of amputation.9 With regard to symptoms of intermittent claudication, a systematic review of observational studies found only inconclusive results as to whether smoking cessation improved walking distance or reduced symptom progression.w11 Nevertheless, the consensus opinion is that smoking cessation is a key part of treating intermittent claudication. There is clear evidence that use of nicotine replacement therapy,10 bupropion, and nortriptyline11 increases the proportion of patients successfully stopping smoking by 50-100%.
Antiplatelet drugs
There is clear evidence that antiplatelet drugs reduce major cardiovascular events. They also reduce the risk of arterial occlusion and the requirement for revascularisation procedures.w12 w13 Various guidelines, including those of the Scottish Intercollegiate Guidelines Network, recommend antiplatelet treatment for patients with peripheral arterial disease.12 w14
Statins
Statins reduce the risk of cardiovascular events in this group of patients.13 There is also some evidence that statins improve the symptoms of claudication, increasing walking distance and pain-free walking time.13 Unless there is a major contraindication, all patients should be prescribed statins.w14
Diabetes control
The prevalence of diabetes is higher among patients with intermittent claudication than in the general population, and such patients need to be screened for diabetes. Tight control of blood glucose concentration significantly reduces the incidence of cardiovascular events in people with diabetes but has had no effect on the risk of peripheral arterial disease.14 Intensive therapy reduces the incidence of myocardial infarction but has no effect on the risk of leg amputation.w15
Blood pressure control
Good control of hypertension confers protection against cardiovascular events.15 w16 In diabetic patients intensive blood pressure control is more effective at reducing cardiovascular events and mortality.16 There is, however, no evidence that lowering blood pressure alters the natural course of intermittent claudication, and a Cochrane review concluded that the evidence for the various drug classes is poor for peripheral arterial disease and that no recommendations could be made.w17 The joint British recommendations for prevention of coronary heart disease, however, suggest that in peripheral arterial disease the treatment target should be a systolic blood pressure <140 mm Hg and a diastolic pressure <85 mm Hg.17
Symptomatic treatment
Exercise
Regular exercise, at least three times weekly, has been shown to improve total walking distance and maximal exercise time.18 There is some suggestion that supervised exercise may be more beneficial than non-supervised exercise.w18
Oral treatment
After 12-24 weeks' treatment, cilostazol significantly improves walking distance compared with placebo. However, the drug is associated with common side effects such as headache, diarrhoea, and palpitations.13 There is no convincing evidence that pentoxifylline, buflomedil, vitamin E, or omega 3 fatty acids have any significant effect on the symptoms of intermittent claudication.w19-w22
Percutaneous transluminal angioplasty
Despite percutaneous transluminal angioplasty being widely used to treat intermittent claudication, its role is still controversial. The 2005 guidelines from the American Heart Association and American College of Cardiology for managing peripheral arterial disease state that, patients with intermittent claudication should not even undergo an evaluation for revascularisation unless they have significant functional impairment with a reasonable likelihood of symptomatic improvement and absence of other disease that might limit activity even if the claudication were improved (see box).w14
Indications for revascularisation in intermittent claudication
A predicted or observed lack of response to exercise or drug treatment
Presence of severe disability, patient being unable to work or perform important activities
Absence of other disease that would limit exercise even if claudication were improved (such as angina, chronic respiratory disease)
Patient's anticipated natural history and prognosis
Morphology of lesion makes it suitable for revascularisation
There is some evidence that percutaneous angioplasty improves walking distance at six months compared with conservative treatment13 and that it improves quality of life.19 A Cochrane review concluded that angioplasty may have some benefit but only a short term one.20 A separate Cochrane review concluded that there is insufficient evidence to conclude whether use of stents provides benefit compared with angioplasty alone for intermittent claudication.21
The Transatlantic Inter-Society Consensus Working Group recommends angioplasty only in patients with single stenoses <3 cm long in the common or external iliac artery, with single stenoses or occlusions ≤5 cm long in the femoropopliteal segment, or with multiple lesions each <3 cm long and not involving the distal popliteal artery.22
Bypass surgery
As for angioplasty, there is wide variation in opinion as to whether patients with intermittent claudication should be offered surgery. There is little doubt that, for patients with debilitating symptoms who are not suitable for angioplasty, surgery may provide effective treatment, but this may be associated with an increased risk of morbidity (2-30%) and mortality (0-5%). One systematic review has found that surgery improves primary patency after 12-24 months compared with angioplasty, but there was no significant difference at four years.23
Whatever type of revascularisation is offered, the patients should also be given information about exercise treatment and pharmacotherapy, receive comprehensive risk factor modification and antiplatelet treatment, have a significant disability, and have peripheral arterial disease anatomy such that the procedure being offered has a high chance of immediate and long term success and a low risk of complications.w14
What new treatments can we expect?
Promising potential treatments include debulking procedures that remove atheromatous plaque from arteries using various techniques. Remote superficial femoral artery endarterectomy, minimally invasive atherectomy using a mechanical device, and excimer percutaneous transluminal laser angioplasty are some of the new techniques used to treat stenoses and occlusions of the arteries in the lower limbs. Initial reports are encouraging, but the long term results are unknown.
Efforts continue to develop new drugs to treat peripheral arterial disease and atherosclerosis, and particularly to cause regression of atherosclerotic plaque. These include DG041, a potent antagonist of the EP3 receptor for prostaglandin E2, and PPAR (peroxisome proliferators activated receptor) and LXR (liver X receptor) agonists which influence the ABCA1 (ATP binding cassette A1) transporter, which has an important role in lipoprotein metabolism.
Therapeutic angiogenesis, the development of new blood vessels to improve the blood flow to the limb, can be achieved with direct administration of angiogenic growth factors. Various growth factors such as vascular endothelial growth factor and hepatocyte growth factors are undergoing trials to assess their potential beneficial effect in leg ischaemia.
Conclusion
Intermittent claudication is the first clinical manifestation of peripheral arterial disease, which in most cases is itself a manifestation of atherosclerosis. The word “peripheral” in the disease name is probably responsible for the fact that doctors fail to recognise the importance of the condition and patients' significantly increased risk of death from cardiovascular disease. Intermittent claudication should be seen not as “peripheral” but as an important “central” warning signal to start as early as possible the measures highlighted to reduce the risk of death and major vascular events. Symptomatic treatment of the leg pain should not overshadow the more important aim of reducing cardiovascular risk. Treatment of the condition should not be perceived as solely the responsibility of vascular surgeons and interventionists. Primary care doctors have a major role too—saving lives.
Additional educational resources
Cassar K, Bachoo P. Peripheral arterial disease. Clin Evid 2006;(15):164-76
Cochrane Database of Systematic Reviews (www.cochrane.org/review/clibaccess.htm)
ACC/AHA 2005 guidelines for the management of peripheral arterial disease. J Am Coll Cardiol 2006;47:1239-312
Antithrombotic therapy in peripheral arterial occlusive disease: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;125:609-26S
Information for patients
British Heart Foundation. Peripheral arterial disease. Heart information series number 16. www.bhf.org.uk/publications/uploaded/download-his16.pdf
Patient UK. Peripheral vascular disease. www.patient.co.uk/showdoc/23068800
Supplementary Material
References
- 1.Garcia LA. Epidemiology and pathophysiology of peripheral arterial disease. J Endovasc Ther 2006;13(suppl 2):II3-9. [DOI] [PubMed]
- 2.Diehm C, Kareem S, Lawall H. Epidemiology of peripheral arterial disease. Vasa 2004;33:183-9. [DOI] [PubMed] [Google Scholar]
- 3.Marquis P. Evaluation of the impact of peripheral obliterative arteriopathy on quality of life. Drugs 1998;56(suppl 3):25-35. [DOI] [PubMed]
- 4.Murabito JM, D'Agostino RB, Silbershatz H, Wilson WF. Intermittent claudication: a risk profile from the Framingham heart study. Circulation 1997;96:44-9. [DOI] [PubMed] [Google Scholar]
- 5.Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on the prevalence of peripheral arterial disease: the San Luis Valley diabetes study. Circulation 1995;91:1472-9. [DOI] [PubMed] [Google Scholar]
- 6.Muluk SC, Muluk VS, Kelley ME, Whittle JC, Tierney JA, Webster MW, et al. Outcome events in patients with claudication: a 15-year study in 2777 patients. J Vasc Surg 2001;33:251-7. [DOI] [PubMed] [Google Scholar]
- 7.Dormandy JA, Murray GD. The fate of the claudicant—a prospective study of 1969 claudicants. Eur J Vasc Surg 1991;5:131-3. [DOI] [PubMed] [Google Scholar]
- 8.Newman AB, Siscovick DS, Manoglio TA, Polak J, Fride LP, Borhani NO, et al. Ankle-arm index as a marker of atherosclerosis in the cardiovascular health study. Circulation 1993;88:837-45. [DOI] [PubMed] [Google Scholar]
- 9.Leng GC, Papacosta O, Whincup P, Wannamethee G, Walker M, Ebrahim S, et al. Femoral atherosclerosis in an older British population: prevalence and risk factors. Atherosclerosis 2000;152:167-74. [DOI] [PubMed] [Google Scholar]
- 10.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2004;(3):CD000146. [DOI] [PubMed]
- 11.Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev 2004;(4):CD000031. [DOI] [PubMed]
- 12.Scottish Intercollegiate Guidelines Network. Drug therapy for peripheral vascular disease: a national clinical guideline. Edinburgh: SIGN, 1998. (www.sign.ac.uk/pdf.sign27.pdf)
- 13.Cassar K, Bachoo P. Peripheral arterial disease. Clin Evid 2006;(15):164-76. [PubMed]
- 14.Effect of intensive diabetes management on macrovascular events and risk factors in the diabetes control and complications trial. Am J Cardiol 1995;75:894-903. [DOI] [PubMed] [Google Scholar]
- 15.Staessen JA, Fagard R, Thijs L, for the Systolic Hypertension in Europe Trial Investigators. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet 1997;350:757-64. [DOI] [PubMed] [Google Scholar]
- 16.Vijan S. Hypertension in diabetes. Clin Evid 2005;(14):491-500. [PubMed]
- 17.Wood D, Durrington P, Poulter N, McInnes G, Rees A, Wray R. Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart 1998;80(suppl 2):S1-29. [PMC free article] [PubMed]
- 18.Leng GC, Fowler B, Ernst E. Exercise for intermittent claudication. Cochrane Database Syst Rev 2000;(2):CD000990. [DOI] [PubMed]
- 19.Cassar K, Bachoo P, Brittenden J. The impact of peripheral percutaneous transluminal angioplasty on quality of life in intermittent claudication. Eur J Vasc Endovasc Surg 2003;26:130-6. [DOI] [PubMed] [Google Scholar]
- 20.Fowkes FGR, Gillespie IN. Angioplasty (versus non surgical management) for intermittent claudication. Cochrane Database Syst Rev 1998;(2):CD000017. [DOI] [PubMed]
- 21.Bachoo P, Thorpe P. Endovascular stents for intermittent claudication. Cochrane Database Syst Rev 2002;(4):CD003228. [DOI] [PubMed]
- 22.Transatlantic Inter-Society Consensus (TASC) Working Group. Management of peripheral arterial occlusive disease: TASC document. J Vasc Surg 2000;31(suppl):S1-27. [PubMed]
- 23.Leng GC, Davis M, Baker D. Bypass surgery for chronic lower limb ischaemia. Cochrane Database Syst Rev 2000;(3):CD002000. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.