Abstract
The src family kinases p56lck (Lck) and p59fyn (Fyn) are the most proximal signaling molecules to be activated downstream of the T-cell receptor. Using an inducible transgenic model, we can regulate the expression of Lck in primary T cells and ask how the signaling cascade and differentiation potential are affected by the absence or the presence of reduced levels of Lck. We show that in naïve T cells, Lck controls the threshold of activation by preferentially regulating multiple signaling pathways that result in the mobilization of Ca2+ through activation of phospholipase C-gamma and protein kinase C as well as activation of the extracellular signal-regulated kinase (ERK)/mitogen-activated protein kinase (MAPK) pathway. Fyn is also able to stimulate the ERK/MAPK pathway in primary T cells but has little influence on the mobilization of Ca2+. Only Lck efficiently stimulates production of diacylglycerol and therefore RasGRP1 recruitment to the plasma membrane and phosphorylation of Shc, suggesting that Fyn activates ERK via a different upstream signaling route. Finally, we show that signals through Lck are essential for the development of T-cell-effector potential, particularly for effective cytokine transcription.
Signaling through the T-cell receptor (TCR) can result in positive or negative selection of immature thymocytes and activation or anergy of mature T cells. The biochemical pathways that trigger these opposed outcomes are not well understood. The most proximal signaling molecules to be activated upon TCR engagement are the Src family kinases, p56lck (Lck) and p59fyn (Fyn), and genetic and biochemical studies have shown them to be essential for signaling through the TCR/CD3 complex (17). Moreover, altering Lck availability has been shown to influence cell fate (18, 26, 55), indicating that the activation of these proximal signaling molecules is central in determining the outcome of TCR engagement.
Following TCR engagement, Lck and/or Fyn phosphorylates immunoreceptor tyrosine-based activation motifs (ITAMs) in CD3 and TCRζ (45, 49), enabling ZAP-70 to bind (6). In addition, Lck and Fyn contribute to ZAP-70 activation, promoting recruitment of downstream adaptor molecules and kinases, which initiates a signaling cascade required for proliferation and differentiation of both developing thymocytes and mature T cells (17). In Lck−/− thymocytes, the basal level of TCRζ phosphorylation is low and does not increase substantially after TCR cross-linking and, furthermore, no ZAP-70 phosphorylation can be detected (49). Similarly, Lck−/− cell lines show profound defects in early TCR activation and fail to mobilize Ca2+ in response to TCR triggering (2, 8, 22, 45). However, little is known about how lack of Lck influences the response of primary peripheral T cells, as the production of mature lymphocytes is profoundly compromised in Lck−/− mice (32). One report used mice expressing an Lck transgene solely in the thymus, to overcome the developmental block associated with the Lck−/− background, and showed that primary Lck−/− T cells have an impairment in Ca2+ mobilization and defective proliferation (47). However, these authors also showed that T cells expressing an excess of a catalytic, inactive Lck were capable of fluxing Ca2+, suggesting that Lck kinase activity is not essential to its ability to mobilize intracellular Ca2+. Therefore, many questions still remain about how Lck interfaces with downstream signaling components of primary lymphocytes.
Although both Lck and Fyn are expressed throughout the T-cell lineage, the relative levels of these two kinases vary during differentiation (33). Moreover, Lck and Fyn function both as kinases and as adapter proteins, through interactions via their SH2 and SH3 domains, which have been shown to interact with overlapping as well as unique target proteins within the cell (57). Analyses of cells from Lck- and Fyn-deficient mice and of cell lines expressing only one or the other kinase (4, 9, 44, 45, 47, 48, 50) have indicated that both of these kinases function as amplifiers of TCR-mediated signaling, increasing sensitivity to stimulation and potentially influencing the differentiation outcome after TCR triggering. However, recent data have suggested that Fyn may also play a role as a negative regulator of T-cell responses, as it interacts specifically with molecules such as the adapter PAG, which may influence the activation of the src kinases themselves (56), and with SLAM and SAP, which have been shown to influence T-cell proliferation and differentiation (7, 24). These observations suggest that Lck and Fyn may have distinct roles in regulating the activation of naive T cells that have not been apparent previously.
We have been examining the functions of Lck and Fyn in primary T cells by using a transgenic mouse model in which the expression of Lck is regulated inducibly under the control of a tetracycline-regulated element (26). On an Lck−/− background, transgene expression is maintained by feeding the mice doxycycline (DOX), which restores thymopoiesis, permitting the development of a relatively normal peripheral-T-cell repertoire. In adult mice, removal of DOX caused rapid thymic atrophy associated with loss of Lck expression; however, the peripheries of these mice remain unaltered, with the continued survival of naïve and memory T cells (38, 39). We showed that although either Lck or Fyn was able to deliver TCR-mediated survival signals (40), expression of Lck was required to facilitate TCR-driven proliferation in response to lymphopenia and to antibody (Ab)-mediated TCR stimulation (38). However, proliferation of naïve T cells did occur in the absence of Lck, although considerably less efficiently, presumably mediated through Fyn.
In order to understand how Lck and Fyn influence signals through the TCR, we present here a comprehensive analysis of the signaling pathways in naïve CD4 T cells mediated either by Fyn alone (in the absence of Lck) or by Fyn in the presence of limiting quantities of Lck. Using Lck−/− cells, we show that Lck is primarily responsible for initiating phospholipase C-gamma 1 (PLC-γ1) phosphorylation, with consequent activation of the inositol phospholipid pathway and mobilization of intracellular Ca2+, leading to the induction of interleukin 2 (IL-2) synthesis and entry into proliferation. Surprisingly, however, the activation of MEK and ERK is only partially defective in the absence of Lck, as Fyn is able to trigger this pathway in a proportion of cells. Moreover, Lck and Fyn seem to target the mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) pathway through distinct Ras activators, with Lck but not Fyn efficiently activating diacylglycerol (DAG) production and translocation of RasGRP1 to the plasma membrane. Additionally, we show that cross-linking CD4 with the TCR can enhance signal transduction even in the absence of Lck, indicating that the coreceptors facilitate signal transduction through interaction with signaling molecules other than Lck in primary T cells.
MATERIALS AND METHODS
Mice.
Lck-inducible mice (Lck1ind) on Lck−/− and Fyn−/− backgrounds have been described previously (26, 40) and where indicated were backcrossed to F5 Rag1−/− TCR-transgenic mice. Lckind mice were heterozygous for the F5 TCR, whereas Fyn−/− mice were homozygous for the F5 TCR; therefore, appropriate F5 controls were matched for each group. Mice were fed DOX in food (1 mg/g) from birth, and cohorts of mice from 6 to 12 wks old were taken off DOX for >1 week prior to analysis. C57BL/10 or C57BL/6 mice served as wild-type (WT) controls. Mice were maintained under United Kingdom Home Office Guidelines.
T-cell purification and stimulation.
Cell suspensions from lymph nodes (LNs) were resuspended in air-buffered Iscove's modified Dulbecco's medium. CD4 T cells were isolated by negative selection using a cocktail of biotinylated Abs (GL3, B220, CD8, Mac1, and Dx5) and Streptavidin magnetic beads (Dynal, Oslo, Norway) and were typically ≥80% pure. Cells were either unstimulated (ice) or preincubated with biotinylated anti-CD3ɛ (145-2C11) and/or biotinylated anti-CD4 (RM4-5, 10 μg each; BD Pharmingen) on ice for 20 min. Ab-bound cells were pelleted and resuspended in phosphate-buffered saline containing 20 μg/ml avidin and transferred to 37°C. Cells were lysed in 1% Triton X-100 or 1% β-d-octylglucopyranoside, 50 mM Tris-Cl (pH 7.5), 150 mM NaCl, 10 mM NaF, 10 mM disodium pyrophosphate, 1 mM sodium orthovanadate, 1 mM 4-(2-aminoethyl)benzenesulfonyl fluoride hydrochloride (AEBSF; Sigma), and a cocktail of small peptide inhibitors. Postnuclear supernatants were precipitated with 1.5 volumes acetone overnight at −20°C. Pellets were washed with ice-cold 70% ethanol and redissolved in 3× reducing sample buffer for several hours with shaking at 4°C. Samples were heated to 95°C and separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE).
Western blot analyses, immunoprecipitation, and intracellular staining.
The following Abs were used for immunoblotting: anti-pY monoclonal Ab (mAb) (4G10; Upstate Biotechnology), anti-pY319-ZAP-70 (Cell Signaling Technology) and anti-ZAP-70 (Transduction Laboratories) mAbs, anti-pY783-PLC-γ1 (Biosource international), anti-PLC-γ1 (Upstate Biotechnology) rabbit Ab, anti-pERK1/2 (Biosource International) and anti-ERK2 (C-14; Santa Cruz Biotechnology) rabbit Abs, anti-pMEK1/2 and anti-MEK1/2 (Cell Signaling Technology) rabbit Abs, anti-pT538-protein kinase Cθ (PKCθ) (Cell Signaling Technology), anti-PKCθ-horseradish peroxidase (Transduction Laboratories), anti-pY171 human LAT and anti-p4191 human LAT (Cell Signaling Technology), anti-pY226 human LAT (Upstate Biotechnology), anti-LAT rabbit Ab M41 (gift from M. Turner, Babraham Institute, United Kingdom), anti-pY239/240-Shc (Santa Cruz Biotechnology) and anti-Shc (Upstate Biotechnology) rabbit Abs, anti-RasGRP1 (Santa Cruz Biotechnology) mouse mAb, anti-actin (Sigma) rabbit Ab, and anti-pS916-PKD (gift from D. Cantrell, University of Dundee, United Kingdom). The polyclonal anti-LAT pY136 was generated by immunizing rabbits with a synthetic phosphopeptide (keyhole limpet hemocyanin coupled) corresponding to residues surrounding Y136 of the murine LAT. Serum was purified by protein A and affinity chromatography.
For analysis of Lck expression, LN cells were stimulated with anti-CD3ɛ plus anti-CD28 for 24 or 48 h or lysed directly. Lck expression was determined by probing total cell lysates (1 × 106 to 2 × 106 cell equivalents/lane) with rabbit anti-Lck Ab (kind gift of A. Magee, Imperial College, London, United Kingdom). Aliquots of cells were stained for CD4 (RM4-5; Pharmingen), CD8 (53-6.7; Pharmingen), and TCR (H57-597; Pharmingen) and analyzed on a FACSCalibur (Becton Dickinson). CD4 immunoprecipitations were performed for 2 h at 4°C with anti-CD4 (YTA 3.1) coupled to Sepharose beads and resolved on SDS-PAGE gels. Associated Lck and the presence of CD4 (anti-CD4 peptide antiserum; Santa Cruz) were analyzed by immunoblotting.
To detect RasGRP1 translocation, CD8-depleted LN T cells from WT and LckON mice were stimulated in vitro for 72 h with anti-CD3 and anti-CD28 Abs. CD4 blasts were washed in IL-2-containing media for 7 to 10 days in the absence of DOX. Cells were stimulated as described above, and subcellular fractionation of membranes was carried out as described previously (36).
For Western blot analyses, primary antibodies were detected as indicated in the figure legends, either with secondary reagents coupled to horseradish peroxidase, developed with chemiluminescence (ECL Amersham), and quantified by scanning on a Bio-Rad GS-710 calibrated densitometer using Quantity One software or with secondary reagents coupled to infrared dyes (AlexaFluor 680 and IRDye800) and quantified using a Li-Cor Odyssey scanner, which precludes signal saturation.
Intracellular staining for pERK was performed as described previously (23), using anti-pERK rabbit mAb (Cell Signaling Technology) and fluorescein isothiocyanate anti-rabbit F(ab′)2 (Jackson Labs) on F5 LN cells stimulated for 15 min with NP68 peptide or 100 nM PDBu. Negative controls were preincubated with 20 μM MEK inhibitor UO126 (Promega) for 15 min before addition of peptide.
In vitro kinase assay.
Purified CD4 T cells (5 × 106) were stimulated for 2 min with cross-linked anti-CD3 plus anti-CD4. Cells were lysed in 0.5% Triton-X lysis buffer, and supernatants were precipitated with protein A-Sepharose coupled to rabbit anti-ZAP-70 (3.3.1; J. Tite, GlaxoSmithKline, United Kingdom). Immunoprecipitates were washed three times with lysis buffer and once with kinase buffer (50 mM Tris, 20 mM MgCl2, 0.1 mM EGTA, and 0.1% 2-mercaptoethanol) and resuspended in kinase buffer containing 0.1 mM ATP, 5 μCi of [γ-32P]ATP, and 1.69 μg of a LAT-glutathione S-transferase (GST) fusion protein (Upstate Biotechnology) for 20 min at room temperature. Kinase reactions were terminated by the addition of 3× SDS sample buffer and heated to 95°C. Reaction products were separated by SDS-PAGE, and 32P-labeled proteins were visualized by autoradiography. An aliquot of beads was retained prior to kinase reactions and bound protein analyzed by immunoblotting for ZAP-70 for loading.
Intracellular Ca2+ analysis.
LN T cells were resuspended in medium and loaded with 1 μg/ml indo-1 acetoxymethyl ester (Molecular Probes) for 30 min at 37°C. Cells were incubated with 10 μg/ml of each biotinylated anti-CD3 and anti-CD4 together with anti-CD8-phycoerythrin and anti-CD44-fluorescein isothiocyanate for 15 min at room temperature. Cells were washed and acquired on an LSR (Becton Dickinson) for 30 s before cross-linking anti-CD3 and anti-CD4 molecules with 20 μg/ml avidin. Data were analyzed using FlowJo (Treestar) software gating on CD8− CD44l° lymphocytes.
In vitro stimulations and IL-2 production assays.
CD4 T cells were purified by including anti-CD25 Ab in the depletion. Cells were incubated with 5 μM carboxyfluorescein diacetate succinimidyl ester (CFSE) for 10 min at room temperature in prewarmed phosphate-buffered saline and washed once. Triplicate cultures at 2 × 105 cells per well were set up with soluble anti-CD3 (as indicated in Fig. 1) plus anti-CD28 at 1 μg/ml in the presence of antigen-presenting cells (1 × 104 bone marrow-derived dendritic cells or 1 × 104 Rag-1−/− splenocytes). Alternatively, cells were stimulated with 10 ng/ml 12,13-phorbol dibutyrate (PDBu) and 100 nM ionomycin (Sigma). After 72 h, cells were stained with anti-CD4 plus anti-CD5 (53-7.3; Pharmingen) and analyzed on a FACSCalibur using Flow Jo (Treestar) software. Proliferation of CFSE-labeled cells was calculated by determining the frequency (F) of cells that had undergone different numbers of division (d). Adjusted frequencies (AdF) were calculated by dividing F by 2d. The percentage of cells triggered to divide was calculated by the equation 1 − (AdF0/ΣAdF) × 100. Alternatively, purified CD4 T cells were stimulated with the above-indicated Ab for 24 h. Cells were stained with anti-CD4, anti-CD5, and anti-CD25 Abs. Supernatants were harvested and used in an alamar blue-based cytotoxic T-lymphocyte line 2 assay. Results are percentages of the maximum value for supernatant diluted 1 in 3. TCR and CD69 (H1.2F3; Pharmingen) levels were determined 18 h after stimulation of total LN with 1 μg/ml anti-CD3 and anti-CD28 Abs.
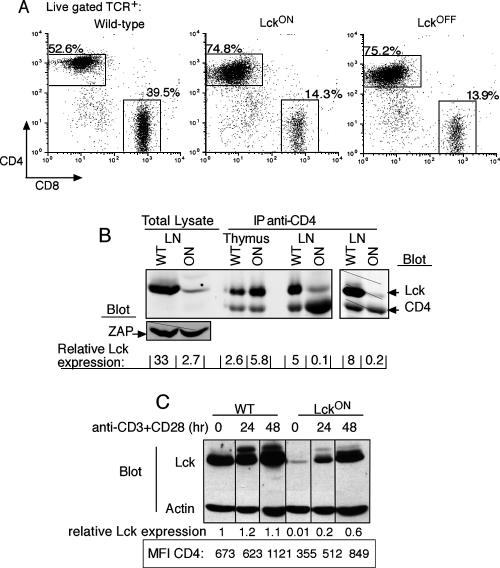
FIG. 1.
Expression of the Lck1 transgene in Lck1ind mice is upregulated following activation. (A) CD4 and CD8 expression on gated live TCRhi cells from LNs of WT and Lck1ind mice on DOX (LckON) or off DOX (LckOFF) (1 to 2 weeks). (B) Cell lysates were prepared from LNs and analyzed by Western blot analysis for Lck and ZAP-70 as a loading control. CD4 was immunoprecipitated from the thymus and LN, and blots were probed for Lck and CD4. Relative Lck expression levels were determined by normalizing data to those for ZAP-70 or CD4. As the CD4-associated Lck was greatly reduced in Lckind mice, samples were loaded to maximize the Lck signal, and the right panel shows the loading controls for immunoprecipitates from equivalent cell numbers. Quantitation was by infrared imaging using the Li-Cor Odyssey system. (C) LN cells were stimulated with 1 μg/ml CD3 and 1 μg/ml CD28 for 24 and 48 h. Cell lysates were blotted with anti-Lck and antiactin and visualized by chemiluminescence. Relative Lck expression levels were normalized to data for actin, and the unstimulated WT value was set to 1. The CD4 MFIs are presented for comparison.
RESULTS
Inducible Lck is upregulated following TCR stimulation.
We have previously reported mice in which expression of Lck is controlled by the induction of a tet-responsive transgene (26). These mice are on an Lck−/− background, and induction of transgene expression with DOX successfully overcomes the lack of endogenous Lck and restores normal thymopoiesis (26). Withdrawal of the mice from DOX for at least 7 days (Lck1OFF) is sufficient to remove all residual protein (38). The periphery of DOX-fed, LckON, and LckOFF mice is populated with near-normal T-cell numbers, although there is an increase in the ratio of CD4+ to CD8+ T cells relative to that for WT mice (Fig. 1A). The phenotype of naïve peripheral T cells is normal, with the exception of the level of CD4 on the cell surface, which is clearly lower and correlates with reduced expression of Lck from the transgene in peripheral T cells even when mice are maintained on DOX (38).
As the pool of Lck associated with the coreceptor CD4 is the most relevant for initiation of the response in primary T cells, we checked whether Lck found in LckON mice is CD4 associated. In contrast to thymocytes, CD4 immunoprecipitates from Lck1ON LN T cells showed a 40- to 50-fold reduction of CD4-associated Lck and an overall 10-fold reduction in total intracellular Lck compared to that in WT cells (Fig. 1B) (40). Despite this, peripheral T cells from Lck1ON mice respond comparably after antigen or anti-TCR stimulation, although with a delay (38), so we asked whether expression of the Lck transgene altered as the cells became metabolically active (Fig. 1C). Ex vivo cells from LckON mice in this experiment had less Lck than was usually seen (compare Fig. 1B), probably due to contamination of irrelevant cells, which would overrepresent the actin loading control. However, following stimulation with anti-CD3 and anti-CD28 in the presence of DOX, intracellular Lck was upregulated to within twofold compared to WT levels at 48 h. In addition, a slower-migrating species of Lck that most likely represents the species resulting from phosphorylation of ser-59 by MAPKs (43, 53) was detected following TCR stimulation. Concomitant with Lck upregulation, expression of CD4 was also increased, as shown by an >2-fold increase in the mean fluorescence intensity (MFI) of CD4 relative to that of ex vivo CD4 T cells at 48 h.
Using peripheral T cells from these mice, we could examine the biochemical outcome of TCR triggering in the absence of Lck as well as in the presence of low levels (1 to 20%) of the kinase by using ex vivo T cells from LckON mice. Furthermore, we specifically addressed the relevance of coreceptor-associated Lck by comparing the stimulation of primary CD4 T cells with either cross-linked anti-CD3 alone or anti-CD3 plus anti-CD4.
Lck is required for Ca2+ responses.
It has been shown previously that T cells lacking Lck are defective in Ca2+ mobilization after stimulation (45, 47); therefore, we asked whether this was also true for CD4+ T cells from our inducible mice expressing either low levels or no Lck. T cells from WT, LckON, and LckOFF mice were loaded with indo-1, and the Ca2+ flux was measured after stimulation with cross-linked anti-CD3 or anti-CD3 plus anti-CD4 (Fig. 2A). WT T cells produced robust Ca2+ fluxes with either stimulus; however, CD3 alone was unable to produce a detectable flux in cells expressing either reduced levels of Lck (LckON) or no Lck (LckOFF). When CD4 was cross-linked with CD3, the Ca2+ flux of T cells from LckON mice was restored, presumably because the remaining Lck molecules were more efficiently targeted to the TCR through their association with CD4. Somewhat surprisingly, CD3-plus-CD4 cross-linking, but not CD3 alone, also induced a detectable Ca2+ response in cells which lacked Lck. The initial Ca2+ spike was absent; however, a proportion of cells fluxing Ca2+ was detected at >100 s in LckOFF cells. It should be noted that the ability of Lck−/− CD4 T cells to mobilize Ca2+ is not due to residual Lck expression, as the same results were obtained with cells from mice withdrawn from the DOX diet for >1 month. These data suggest that CD4 can contribute to T-cell signaling independently of its association with Lck, perhaps by recruiting other signaling molecules, such as the recently described adapter LIME (5, 20).
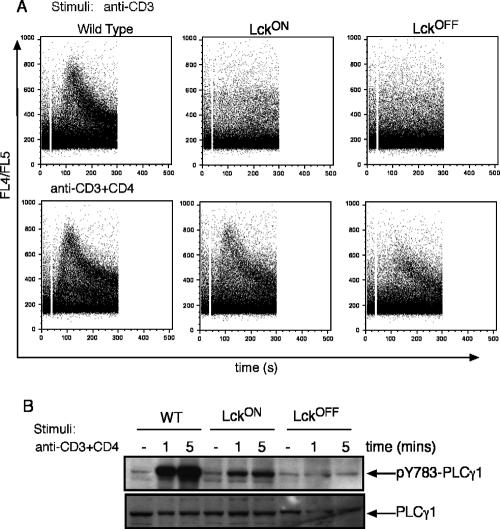
FIG. 2.
Defective Ca2+ and PLC-γ1 phosphorylation in LckOFF T cells. (A) LN cells were loaded with indo-1 and stimulated with cross-linked anti-CD3 or anti-CD3 plus anti-CD4. FACS plots show the ratios of indo-1 fluorescence against time for CD4 cells. (B) Purified CD4+ T cells were stimulated as shown and blotted with anti-PLC-γ1 pY783 or total anti-PLC-γ1 for loading and visualized by chemiluminescence. Data shown are representative of at least three experiments. Percent relative expression was calculated by densitometric analysis of bands and normalizing data for individual phospho bands to those for their loading controls, and the maximal signal was set to 100%.
The mobilization of Ca2+ in T cells has been shown to be downstream of the activation of PLC-γ1 (54), and Lck, ZAP-70, and ITK have been shown to be important for full PLC-γ1 activation (30). Furthermore, spatial localization of PLC-γ1 through its ability to associate with both LAT and Slp-76 is critical for its function (27). TCR engagement causes both the phosphorylation and the increased catalytic activity of PLC-γ1. Specifically, phosphorylation of Y783 of PLC-γ1 has been shown to be essential for coupling the TCR to IL-2 promoter activity in Jurkat T cells (21). We showed that phosphorylation of PLC-γ1 Y783 correlates directly with expression of Lck (Fig. 2B), with only background bands observed after stimulation of peripheral T cells in the absence of Lck and ∼20% of the WT signal visible when low levels of Lck are available (LckON cells). Therefore, there is good correspondence between the requirement for Lck to activate PLC-γ1 and to initiate a Ca2+ flux after stimulation.
Defective signaling to ZAP-70 and LAT in the absence of Lck.
The initial substrates to be phosphorylated after TCR triggering are the ITAM motifs on the TCRζ and CD3 chains. In resting primary T cells ex vivo, there is basal phosphorylation of TCRζ, indicative of the cells receiving TCR-associated survival signals. We showed previously that, in the absence of Lck, Fyn maintains the level of the p21ζ in vivo (40), indicating that either of these Src kinases is capable of phosphorylating the TCRζ chain. In order to address the requirement for Lck to induce the hyperphosphorylated 23-kDa form of the TCRζ chain after activation, purified CD4+ T cells were stimulated with cross-linked CD3 or CD3 plus CD4. In contrast to what was found for WT cells, inducible p23ζ was barely detectable after stimulation if Lck was reduced or absent, although constitutive p21ζ was seen in all samples (Fig. 3A). This was true regardless of whether the cells were stimulated with anti-CD3 alone or anti-CD3 plus anti-CD4, regardless of the fact that inclusion of anti-CD4 Abs greatly enhanced the production of p23ζ in WT cells.
FIG. 3.
Proximal TCR signals are defective in the absence of Lck. CD4 T cells were stimulated with anti-CD3, anti-CD3 plus anti-CD4, or anti-CD3 plus anti-Thy1, as shown, for 2 min. Total cell lysates were run on SDS-PAGE gels, immunoblotted for TCRζ chain phosphorylation with anti-pY and reprobed for TCR-ζ (A), and immunoblotted for pY319-ZAP-70 (pZAP) and total ZAP-70 (tZAP) (B and C). (D) ZAP-70 kinase activity from ZAP immunoprecipitates was measured by 32P incorporation in vitro on GST-LAT substrate. Total ZAP-70 indicates loading. (E) Immunoblots probed with phospho-specific LAT Abs for pY136, pY175, pY195, and pY235 and those shown in panels A to D were visualized with chemiluminescence. (F) Graphs quantifying individual phospho-LAT residues either from the densitometries of ECL blots or directly from a Li-Cor Odyssey infrared imager for three to five replicate experiments are normalized to data for their loading controls and expressed as percentages of the maximum stimulation level, set to 100% based on WT cells stimulated with CD3 plus CD4. (G) T cells expressing Lck plus Fyn (LckON), Fyn only (LckOFF), Lck only (LckON Fyn−/−), or neither kinase (LckOFF Fyn−/−) were stimulated as described above and lysates probed for pLAT 175 and total LAT to control for loading and visualized with a Li-Cor infrared imager.
Phosphorylation of the TCR-associated ITAMs allows recruitment of the ZAP-70 PTK and its activation. Measurement of total Tyr phosphorylation from ZAP-70 immunoprecipitates after stimulation revealed that while pZAP-70 could be detected from WT cells stimulated with CD3 plus CD4, none was detectable in immunoprecipitates from LckON or LckOFF T cells (data not shown). However, improved detection of pZAP-70 was achieved with antisera specific for pY319, which is known to be required for the positive regulation of ZAP-70 (10, 52). As seen for phosphorylation of TCRζ, there was a profound dependence on the presence of Lck for phosphorylation of Y319 of ZAP-70 (Fig. 3B, LckOFF). Furthermore, cells expressing low levels of Lck (Fig. 3B, LckON) required cross-linking of CD4 with CD3 before pY319 was detected, and CD3-plus-CD4 cross-linking greatly increased pZAP-70 even in WT cells. The enhancement of signaling was specific for CD4 cross-linked with CD3, as cross-linking CD3 with Thy-1 in WT cells showed no enhancement of ZAP-70 phosphorylation compared to anti-CD3 alone (Fig. 3C). Together, these results indicate that Lck is the main kinase for the phosphorylation of this residue on ZAP-70 and that the physical juxtaposition of the TCR with CD4-associated Lck greatly enhances this activity. Tyrosine phosphorylation of ZAP-70 is known to increase kinase activity, and ZAP-70 Y319 mutants have decreased catalytic activities (10). We asked whether Lck−/− T cells show any ZAP-70 kinase activity, by immunoprecipitating ZAP 70 from CD4+ T cells stimulated with anti-CD3 plus anti-CD4 Abs and examining the phosphorylation of an exogenous substrate in vitro. For these experiments, we chose a recombinant LAT-GST fusion protein as the most physiologically relevant ZAP-70 substrate. As shown in Fig. 3D, there was small but detectable ZAP-70 kinase activity after CD3-plus-CD4 stimulation even in the absence of Lck. Therefore, while Lck is required for optimal activation of ZAP-70, it is clear that some residual kinase activity can be stimulated in the absence of Lck. It is most likely that Fyn was responsible for this activity, as we found comparable levels of Fyn protein in T cells from all of these mouse strains and all contained equivalent pools of Fyn in the active state, as judged by the phosphorylation of the active residue, Y417 (data not shown).
To address whether the ZAP-70 kinase activity that we detected in vitro was relevant for downstream signaling cascades in vivo, we assessed LAT phosphorylation after stimulation in CD4 T cells lacking Lck. TCR-induced phosphorylation of LAT was detected initially by probing total cell lysates with Ab to pY. A protein that migrated at the same size as LAT could be detected in WT cells stimulated with anti-CD3 as well as anti-CD3 plus anti-CD4 (Fig. 3E, top panel). As with pζ and pZAP-70, the induction of pLAT by CD3 plus CD4 was much better than that by CD3 alone for both WT and especially LckON CD4 T cells. Consistent with the weak ZAP-70 kinase activity that was detected in LckOFF cells, a small amount of pLAT activation could also be observed in Lck−/− cells, particularly after stimulation with anti-CD3 plus anti-CD4 Abs.
LAT contains nine Tyr residues which when phosphorylated are thought to allow other proteins to bind via their SH2 domains (29). The distal four residues, Y136, Y175, Y195, and Y235, have been shown to be crucial for linking LAT to the activation of both PLC-γ1 and the Ras/ERK pathways in Jurkat T cells (59). Furthermore, knock-in mutant mice in which these four residues are mutated resemble LAT−/− mice with thymocyte development arrested at the double-negative stage and no mature T cells (41). More specifically, LAT Y136 has been shown to be important for PLC-γ1 recruitment, thus linking LAT to activation of the Ca2+ pathway, while Y175, Y195, and Y235 interact with Grb2 and GADS (28, 34, 59). Using antisera specific for individual pYs on LAT, even in the absence of Lck, we could readily detect the phosphorylation of residues Y175 and Y235 but much weaker phosphorylation on residues Y136 and Y195 (Fig. 3E). In fact, normalization of the data showed that the patterns of phosphorylation levels for residues Y136, Y175, and Y195 were similar between the different cell types, with the highest signal seen with pY175 and the weakest with Y136 (Fig. 3F). At this point, we cannot distinguish whether this reflects differences in the efficiencies with which these individual residues are targets for phosphorylation or simply disparities in the potencies of the specific anti-phospho antisera. However, there remains a direct correlation between the reduced ability of these cells to activate PLC-γ1 and the poor phosphorylation of Y136 when Lck is reduced or absent. As before, the induction of LAT phosphorylation was considerably improved by cross-linking CD4 plus CD3 compared to CD3 alone, even in the absence of Lck; however, it is clear that the optimal phosphorylation of these downstream kinases and adaptor molecules occurred when Lck was activated.
We asked whether Fyn was responsible for the LAT Y175 phosphorylation in the absence of Lck by stimulating cells from Lckind mice crossed to a Fyn−/− background. Switching off Lck in these mice produces T cells lacking both kinases, and upon stimulation with anti-CD3 plus anti-CD4, such cells showed no detectable phosphorylation of LAT residues (Fig. 3G), confirming that Fyn can initiate limited signaling downstream of the TCR in the absence of Lck.
ERK phosphorylation in Lck−/− T cells.
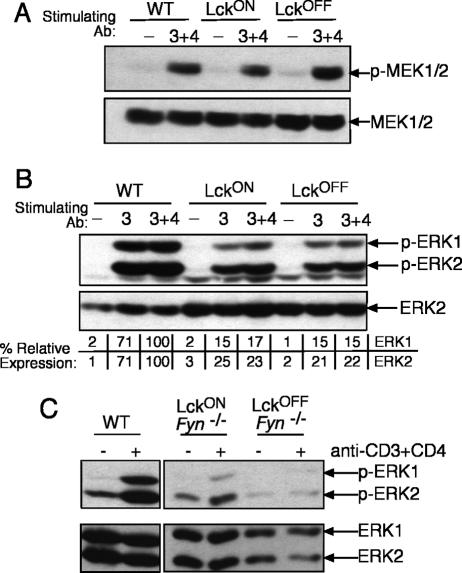
In view of the defects in activation that we saw among upstream kinases and adapters in Lck−/− cells, we looked further downstream at the activation of the MEK/ERK MAPK pathway. Surprisingly, we found a much smaller reduction in the activation of MEK or ERKs in the absence of Lck by Western blotting than we observed for other upstream signaling molecules. Robust phosphorylation of MEK was detected in the absence of Lck (Fig. 4A), as was phosphorylation of ERK1 and ERK2 (Fig. 4B). Quantitation of several Western blots indicated that levels of ERK phosphorylation in the absence of Lck were consistently in the order of 10 to 30% of those found in WT cells, which contrasts with a reduction of >95% in the phosphorylation of upstream kinases, such as ZAP-70 and PLC-γ1. Moreover, unlike activation of ZAP-70, PLC-γ1, or LAT, inducible ERK phosphorylation was remarkably similar in Lck-sufficient cells stimulated with either anti-CD3 alone or anti-CD3 plus anti-CD4 Ab, further indicating that in WT cells, recruitment of Lck via CD4 has little additive effect on ERK activity. Furthermore, we could confirm that the residual ERK activity in the absence of Lck was primarily mediated via Fyn, as the inducible signal was lost in cells lacking both Lck and Fyn (Fig. 4C).
FIG. 4.
Efficient MEK and ERK activation in the absence of Lck. pMEK1/2 (A) or pERK1/2 (B) is shown for purified CD4 T cells stimulated for 2 min at 37°C. pERK activation was mediated via Fyn, as no inducible signal was found in cells which express neither Lck nor Fyn (C). Loading was assessed by probing with specific antisera for total protein and visualized with chemiluminescence. Each blot is representative of two to four replicates, and percent relative expression was determined as for Fig. 2.
The ability of Lck−/− T cells to activate the ERK pathway was surprising in view of the profound defects in the activation of upstream kinases and adapter molecules and suggested that Fyn could activate the ERK pathway independently of Lck. In order to better understand how these two Src kinases activated the ERK pathway, we moved to a fluorescence-activated cell sorter (FACS)-based assay to monitor ERK activation at a single-cell level. In addition, we looked at an antigen-specific response by using Lckind and Fyn−/− mice that were crossed with the F5 TCR transgene on a Rag1−/− background. Upon peptide stimulation, F5 CD8 T cells behaved comparably to CD4 T cells by Western blot analysis, in that they showed profound defects in the phosphorylation of upstream kinases, such as ZAP-70 and PLC-γ1, and in Ca2+ mobilization, while the pERK signal was similar to that observed in Fig. 4B (A. Filby, B. Seddon, M. Veldkoen, J. M. Sanchez-Morgado, M. Smida, J. A. Lindquist, and R. Zamoyska, unpublished data).
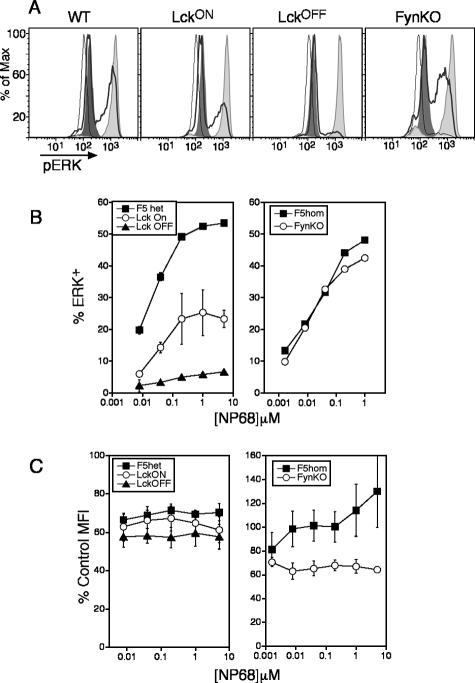
Stimulation of WT F5 T cells revealed that at the highest peptide doses, up to 55% of cells had substantial upregulation of intracellular pERK at 15 min (Fig. 1A), and the proportions of cells responding titrated linearly with increasing doses of peptide (Fig. 1B). The specificity of the pERK Ab was controlled by pretreating samples stimulated with the highest dose of peptide with the MEK inhibitor, UO126, which reduced staining to background levels (Fig. 5A). The availability of Lck had a direct effect on the number of cells that were able to phosphorylate ERK, which was about 10 to 15% of that for WT cells, and this percentage was consistent across the antigen titration (Fig. 5A and B). However, lack of Lkc had much less influence on the quantity of intracellular pERK per cell, as the MFI values were reduced by about 20% (Fig. 5C). Moreover, defects in ERK activity were shown to be restricted to signals downstream of the TCR, as stimulation with phorbol esters provoked equivalent responses in all samples (Fig. 5A). Interestingly, stimulation of Fyn−/− CD8 T cells showed dose response curves identical to those of WT cells in terms of the numbers of cells that were stimulated (Fig. 5A and B) but, on average, greater reductions in MFI (∼40%) than those for cells lacking Lck. Moreover, the durations of the ERK responses in all groups were equivalent and could be followed from 5 min to at least 4 h (data not shown). These data indicate that signals downstream of Fyn play a substantial role in the activation of the ERK/MAPK pathway in primary T cells by influencing the magnitude of the pERK signal, whereas signals downstream of Lck seem primarily to regulate the threshold of triggering.
FIG. 5.
Fyn contributes to the magnitude of ERK activation in F5 T cells in response to peptide stimulation. (A) FACS histograms showing intracellular pERK staining following stimulation for 15 min with medium (thin line), 1 μM NP68 peptide (thick line), 1 μM NP68 peptide plus UO126 MEK inhibitor (dark fill), or PDBu (light fill) for F5 T cells on the indicated backgrounds. (B) Dose-response curves for triplicate samples ± standard errors, showing the percentages of ERK+ cells after 15 min of stimulation with peptide. Data are representative of at least three independent experiments. (C) Mean MFIs ± standard errors for ERK+ cells in response to peptide titration from three to four independent experiments calculated from the formula (exp − b/g)/(total − b/g) × 100%, where exp is the MFI of the ERK+ gate from the peptide-stimulated sample, b/g is the MFI of the UO126-inhibited sample, and total is the MFI of the ERK+ gate from the PDBu-stimulated sample.
Lck and Fyn activate ERKs through different pathways.
Given the profound defect in PLC-γ1 activation in the LckOFF cells, we asked which signaling pathways might be activating ERK downstream of Lck and Fyn. One effector of Ras in T cells is the guanine nucleotide exchange factor (GEF) RasGRP1, which is recruited to the plasma membrane upon T-cell stimulation. Signals through the TCR generally result in PLC-γ1 activation, which converts phosphotidylinosoitol 4,5 bisphosphate (PIP2) into inositol 3,4,5 triphosphate (InsP3) and DAG, with the latter promoting membrane recruitment of RasGRP1 through its DAG binding C1 domain (12). In Lck−/− cells, there was poor phosphorylation of LAT Y136, the main residue which recruits PLC-γ1, concomitant with reduced phosphorylation of PLC-γ1 itself, suggesting that DAG production was likely to be compromised. To see whether this was true, we looked for DAG production in two ways, first, by looking for recruitment of RasGRP1 to the plasma membrane after activation, and second, by investigating the activation of PKD, which is also dependent on DAG (31).
To facilitate subcellular fractionation, which is difficult to achieve cleanly with resting naïve peripheral T cells, CD4+ T cell blasts were generated from WT and LckOFF mice, allowed to rest, and then restimulated with anti-CD3 plus anti-CD4 in order to examine RasGRP1 translocation to the plasma membrane. Importantly, restimulation of CD4 T-cell blasts was comparable to that of naïve CD4 T cells in that both had severely reduced ZAP-70/PLC-γ1 activation and both retained ERK activation (data not shown). Membrane fractions were prepared from stimulated cells, run on SDS-PAGE gels, and analyzed by Western blotting for the presence of RasGRP1. In WT cells, a significant fraction of RasGRP1 could be seen to translocate to the plasma membrane after stimulation with CD3 plus CD4, whereas in the absence of Lck, the RasGRP signal after stimulation was the same as that of the background, indicating a clear reduction in DAG production and RasGRP recruitment in these cells (Fig. 6A). Again, we could show that there were no global defects in RasGRP translocation in the absence of Lck, as recruitment to the membrane occurred in all samples after phorbol ester treatment. To confirm that DAG production was impaired in the absence of Lck in primary ex vivo T cells also, we examined the phosphorylation of PKD on S916, which has previously been shown to be dependent on DAG (31). Stimulation of naïve CD4 T cells from either WT or LckON mice with CD3-plus-CD4 Ab resulted in the distinct appearance of a phosphorylated PKD species at 2 min, which was recognized by S916-specific antisera (Fig. 6B). In contrast, LckOFF cells lacked this species, confirming that DAG production is compromised in cells lacking Lck. Together, these data suggest that the activation of ERKs in the absence of Lck is via a pathway which does not involve PLC-γ1/RasGRP1.
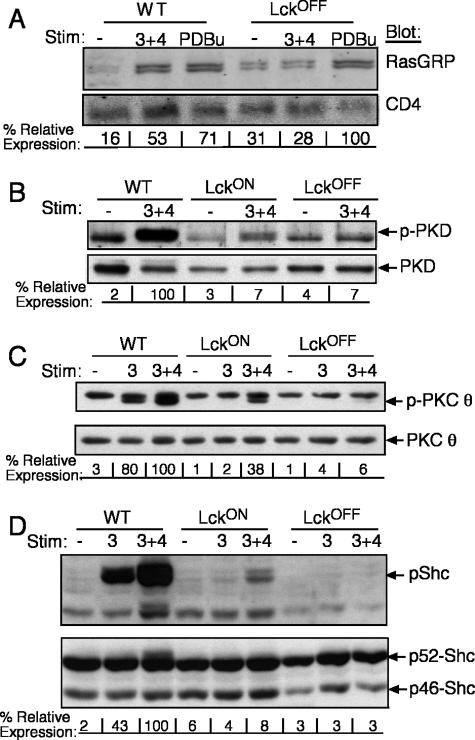
FIG. 6.
Absence of Lck compromises recruitment of RasGRP, DAG production, and phosphorylation of PKCθ and Shc. CD4 T-cell blasts were stimulated with anti-CD3 plus anti-CD4 Abs or PDBu, as indicated, for 2 min at 37°C. (A) Cell membranes were prepared and probed for RasGRP and CD4, and relative RasGRP expression was quantified by infrared imaging using the Li-Cor Odyssey system. Total cell lysates from naïve, purified CD4 T cells were stimulated and probed for PKD pS916 (B), pPKCθ on T538 (C), and pShc Y239/240 (D) and visualized with chemiluminescence. Each blot is representative of two to four replicates, and percent relative expression was determined as for Fig. 2.
Production of DAG also results in the membrane localization and activation of PKCθ, which is required for the activation of mature T cells and the production of IL-2 (3). We found that in WT cells, CD3 and CD3-plus-CD4 stimulation resulted in robust phosphorylation of T538 on PKCθ, while cells from LckOFF mice showed little to no PKCθ phosphorylation (Fig. 6C). Once again, in the presence of low levels of Lck (LckON T cells), CD4 coligation with the TCR during stimulation was required to reveal good phosphorylation of PKCθ, confirming that its activation is also dependent on the activity of Lck.
Finally, another TCR-associated molecule whose activation has been suggested to feed into the Ras MAPK pathway is the adapter molecule Shc. By means of its SH3 domain, Shc has been shown to bind Grb2-SOS and hence activate the Ras/ERK pathway (58). However, we found that in the absence of Lck, there was a severe decrease in both the p46 and the p52 phosphorylated forms of Shc upon activation (Fig. 6D). Moreover, CD4 coengagement increased phosphorylation of Shc considerably, especially in the presence of low levels of Lck, confirming previous reports that Shc is a good substrate of Lck (15, 51, 58) and that Shc is unlikely to be contributing to activation of the ERK pathway in the absence of Lck.
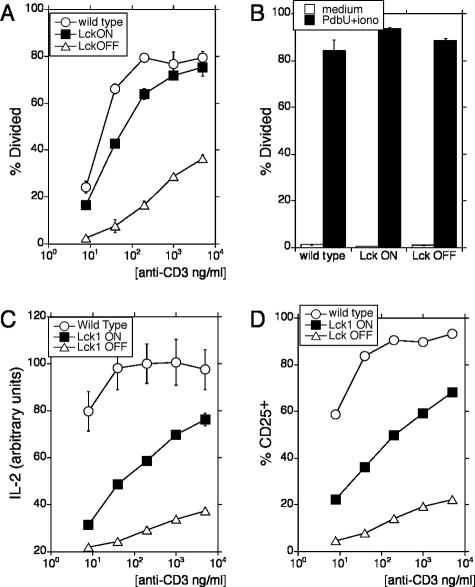
Lck is required for proliferation and cytokine production.
We examined the downstream consequences of receptor triggering for primary CD4+ cells in the absence of Lck. We showed previously that CD69 upregulation occurs in the absence of Lck but that the proportion of cells stimulated and the extent of CD69 expression are both reduced (38). In total peripheral LN preparations, CD8 cells respond more vigorously than CD4 cells and dominate the culture; therefore, we examined the fate of purified CD4 cells after stimulation with Ab, although similar data have been obtained for CD8 T cells (Filby et al., unpublished data). We used the cell-tracking dye CFSE to monitor proliferation and assessed early activation events, such as CD25 expression and IL-2 production. Purified CFSE-labeled CD4+ T cells were stimulated in vitro with soluble anti-CD3 plus anti-CD28. After 72 h, the percentage of cells in each CFSE peak was enumerated and used to calculate the percentage of the starting population which had entered division. WT and LckON cells behave remarkably similarly over a range of Ab concentrations (Fig. 7A), suggesting that despite some early deficiencies in Lck-mediated signaling, upregulation of Lck upon activation (Fig. 1) restored the capacity of these cells to respond. As previously reported (38, 47), Lck-deficient CD4 T cells responded poorly to anti-CD3 stimulation, suggesting that the threshold for triggering such cells into division is substantially altered. At higher concentrations of CD3 Ab, Lck−/− cells did enter division, and remarkably, for those cells that had crossed this threshold, the numbers of divisions that they underwent were close to those achieved by WT cells, with division indexes of 2.6 for WT, 2.8 for LckON, and 1.8 for LckOFF cells. Treatment with PDBu in combination with ionomycin restored the ability of Lck−/− T cells to proliferate to a level comparable to those for both WT and Lck1ON CD4+ T cells (Fig. 7B). This result indicated that there were no other intrinsic defects in Lck−/− cells that could not be circumvented by bypassing TCR-dependent activation of DAG and Ca2+.
FIG. 7.
Impaired T-cell proliferation and IL-2 secretion in the absence of Lck. Proliferation of CFSE-labeled, purified CD4+ T cells stimulated with anti-CD3 plus anti-CD28 (A) or PDBu plus ionomycin (B) for 72 h. (C) IL-2 was measured from supernatant after 24 h culture, in response to anti-CD3 plus 1 μg/ml anti-CD28, and (D) expression of CD25 was determined. Graphs show means ± standard deviations for triplicate points.
Consistent with the defects in Ca2+, PLC-γ1, and PKCθ activation, Lck-deficient cells were very poor in secreting IL-2 (Fig. 7C). In addition, upregulation of CD25 was compromised (Fig. 7D). These parameters were also defective in the cells which expressed low levels of Lck. At first sight, this seems to be contradictory to the proliferation data, which were the same between WT and LckON cells. However, proliferation was assessed at 72 h, by which time the expression of Lck was substantially upregulated (Fig. 1) in contrast to what was found for the CD25 and IL-2 measurements, which were carried out at 24 h. The upregulation of CD25 and the transcription of the IL-2 gene in the initial part of the response are driven directly by TCR signals, which are highly dependent on Lck expression. In contrast, maintenance of proliferation seems to be less dependent on Lck.
DISCUSSION
Transgenic mice expressing Lck in an inducible fashion provide a novel opportunity to assess the role of Lck in the induction of T-cell responses in primary naïve T cells. By examining proximal biochemical signals transduced by ligation of the TCR either alone or in combination with CD4, we were able to discriminate pathways that were primarily induced by Lck from those that were correspondingly influenced by activation of both Lck and Fyn. From these data, we showed that Lck profoundly influences the threshold at which cells are triggered, and biochemically, this correlated with the ability of Lck to induce signaling pathways leading to PLC-γ1 activation, inositol phospholipid hydrolysis, and the mobilization of intracellular Ca2+. In contrast, we found that both Lck and Fyn contributed to activation of the ERK/MAPK pathway and that they seem to access this pathway through distinct upstream mediators.
The influence of Lck on early signaling events, such as activation of ZAP-70, was evident by the absence of the phosphorylation of ZAP Y319 in Lck−/− cells and its reduced kinase activity, resulting in the decreased phosphorylation of LAT on several key residues. Phosphorylation of LAT Y136 is important for recruitment of PLC-γ1 (1, 28, 34, 42, 59), and diminished phosphorylation of this residue could largely explain the inability of Lck−/− cells to link to the phosphatidylinositol and PKC signaling pathways. In addition, mutation of LAT Y195 was shown to disrupt interaction with the adapter molecule GADS, which is responsible for the recruitment of Slp-76. We found that phosphorylation of Slp-76 was also severely defective in the absence of Lck (data not shown), suggesting that the GADS/Slp-76/PLC-γ1 complex would be unlikely to assemble efficiently, which could also contribute to the failure to activate PLC-γ1. Surprisingly, despite these defects in PLC-γ1 signaling, a proportion of Lck−/− cells were triggered to respond. By single-cell FACS analysis, these cells were shown to phosphorylate ERK at levels that were ∼80% of those for WT cells. This ability to activate ERKs required expression of Fyn, and moreover, for WT primary T cells, we showed that Fyn contributes substantially to the magnitude of ERK phosphorylation.
There are two major GEFs for Ras in T cells, RasGRP1 and SOS (16). The former is recruited to the membrane by the production of DAG and has been shown to be important for thymocyte differentiation and peripheral T-cell expansion (11, 35) and recently to be the major activator of ERKs in Jurkat T cells (37). However, it is unlikely that RasGRP1 was the major contributor to the activation of the Ras/ERK pathway in the absence of Lck, as there appeared to be insufficient DAG production to result in Ser phosphorylation of PKD or to recruit RasGRP1 to the plasma membrane efficiently. Moreover, activation of PKCθ was also severely compromised in the absence of Lck, which may have contributed to the failure to activate RasGRP1, as activation of novel PKCs has recently been shown to contribute to RasGRP1 signaling in Jurkat cells (37). It is likely, therefore, that the activation of ERK in the absence of Lck proceeded primarily via SOS, although this was unlikely to involve the adapter Shc, whose phosphorylation, as confirmed here, is extremely dependent on the activation of Lck (15). The most likely scenario in the absence of Lck is that Grb2/SOS is directly recruited to LAT and acts as the Ras GEF, which results in the partial phosphorylation of ERKs. Certainly, Fyn was able to promote limited kinase activity for ZAP-70 and some LAT Tyr phosphorylation, particularly at Y175 and Y235, residues known to bind Grb2. We were unable to demonstrate experimentally a direct association between LAT and Grb2/SOS in either primary WT or Lck-deficient cells, suggesting that such an association could be at low stoichiometry. It seems, therefore, that unlike in Jurkat cells, where ERK activation proceeds almost exclusively through RasGRP1 and cannot be compensated by recruitment of SOS (37), in primary T cells, both Src kinases contribute to ERK activity. The expression of Fyn has been reported to be very low in some Jurkat cell lines (9), in contrast to the high expression in primary T cells, which may well explain some of these differences.
The primary consequence of the lack of Lck in naïve T cells was to raise the activation threshold, resulting in a 100-fold shift in the dose-response curve. The percentage of cells that were triggered to divide corresponded to the proportion that were able to phosphorylate ERK and that showed an increased Ca2+ flux at later time points. It is possible that although the initial Ca flux is severely compromised in these cells because of the deficiency in PLC-γ1 activation and InsP3 production, there remains sufficient residual activity of these signaling pathways or even activation of other second messengers, such as cyclic ADP-ribose, which can result in the opening of Ca2+ release-activated Ca2+ channels in the plasma membrane and thereby increase intracellular Ca (54). Certainly, the ability to induce IL-2 transcription is severely compromised in the absence of Lck, suggesting that NFAT activation is considerably reduced. Interestingly, if intracellular IL-2 is visualized following recall with a 4-h PDBu and ionomycin pulse, a significant proportion of the cells are found to produce IL-2 (data not shown). Therefore, the signals received in the absence of Lck are sufficient to open the locus but insufficient to induce normal levels of IL-2 transcription.
It is clear from these data that Lck and Fyn play distinct roles in primary T-cell activation even though some signaling pathways may be targeted by both kinases. One critical difference between Lck and Fyn is that, by virtue of their unique N-terminal domains, each is resident in a separate subcellular compartment of the plasma membrane. Fyn is mainly associated with lipid rafts and the TCR, while Lck is associated with the coreceptors, and the active pool seems to be held outside lipid rafts (14, 56). Signaling through anti-CD3 alone is clearly less efficient than signaling through CD3 plus CD4, and the former is particularly compromised in naïve T cells that lack Fyn, even though their response to CD3-plus-CD4 coligation is relatively normal (46). In addition, coaggregation of TCR and CD4 can greatly increase basal Fyn activity (13). It has been suggested that one role of Fyn is to provide partial signals, such as those delivered by antagonist ligands (19), and our data would suggest that this may be through Fyn providing partial phosphorylation of LAT and thus separating the activation of the ERK pathway from the inositol phosphate/protein kinase C pathways. These data, together with the demonstration that Fyn and not Lck preferentially interacts with molecules that are negative regulators of T-cell activation, such as the PAG/Csk (29) and SAP/SLAM (25), suggest that the primary role of Fyn is to dampen T-cell responses, while Lck acts to amplify them.
Acknowledgments
We thank Ben Seddon and Victor Tybulewicz for helpful discussions.
This work was supported by the LRF and MRC (United Kingdom).
Footnotes
Published ahead of print on 11 September 2006.
REFERENCES
- 1.Aguado, E., S. Richelme, S. Nunez-Cruz, A. Miazek, A. M. Mura, M. Richelme, X. J. Guo, D. Sainty, H. T. He, B. Malissen, and M. Malissen. 2002. Induction of T helper type 2 immunity by a point mutation in the LAT adaptor. Science 296:2036-2040. [DOI] [PubMed] [Google Scholar]
- 2.al-Ramadi, B. K., T. Nakamura, D. Leitenberg, and A. L. Bothwell. 1996. Deficient expression of p56(lck) in Th2 cells leads to partial TCR signaling and a dysregulation in lymphokine mRNA levels. J. Immunol. 157:4751-4761. [PubMed] [Google Scholar]
- 3.Altman, A., and M. Villalba. 2003. Protein kinase C-theta (PKCtheta): it's all about location, location, location. Immunol. Rev. 192:53-63. [DOI] [PubMed] [Google Scholar]
- 4.Appleby, M. W., J. A. Gross, M. P. Cooke, S. D. Levin, X. Qian, and R. M. Perlmutter. 1992. Defective T cell receptor signaling in mice lacking the thymic isoform of p59fyn. Cell 70:751-763. [DOI] [PubMed] [Google Scholar]
- 5.Brdickova, N., T. Brdicka, P. Angelisova, O. Horvath, J. Spicka, I. Hilgert, J. Paces, L. Simeoni, S. Kliche, C. Merten, B. Schraven, and V. Horejsi. 2003. LIME: a new membrane raft-associated adaptor protein involved in CD4 and CD8 coreceptor signaling. J. Exp. Med. 198:1453-1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan, A. C., M. Iwashima, C. W. Turck, and A. Weiss. 1992. ZAP-70: a 70 kd protein-tyrosine kinase that associates with the TCR zeta chain. Cell 71:649-662. [DOI] [PubMed] [Google Scholar]
- 7.Davidson, D., X. Shi, S. Zhang, H. Wang, M. Nemer, N. Ono, S. Ohno, Y. Yanagi, and A. Veillette. 2004. Genetic evidence linking SAP, the X-linked lymphoproliferative gene product, to Src-related kinase FynT in T(H)2 cytokine regulation. Immunity 21:707-717. [DOI] [PubMed] [Google Scholar]
- 8.Denny, M. F., H. C. Kaufman, A. C. Chan, and D. B. Straus. 1999. The lck SH3 domain is required for activation of the mitogen-activated protein kinase pathway but not the initiation of T-cell antigen receptor signaling. J. Biol. Chem. 274:5146-5152. [DOI] [PubMed] [Google Scholar]
- 9.Denny, M. F., B. Patai, and D. B. Straus. 2000. Differential T-cell antigen receptor signaling mediated by the Src family kinases Lck and Fyn. Mol. Cell. Biol. 20:1426-1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Bartolo, V., D. Mege, V. Germain, M. Pelosi, E. Dufour, F. Michel, G. Magistrelli, A. Isacchi, and O. Acuto. 1999. Tyrosine 319, a newly identified phosphorylation site of ZAP-70, plays a critical role in T cell antigen receptor signaling. J. Biol. Chem. 274:6285-6294. [DOI] [PubMed] [Google Scholar]
- 11.Dower, N. A., S. L. Stang, D. A. Bottorff, J. O. Ebinu, P. Dickie, H. L. Ostergaard, and J. C. Stone. 2000. RasGRP is essential for mouse thymocyte differentiation and TCR signaling. Nat. Immunol. 1:317-321. [DOI] [PubMed] [Google Scholar]
- 12.Ebinu, J. O., D. A. Bottorff, E. Y. Chan, S. L. Stang, R. J. Dunn, and J. C. Stone. 1998. RasGRP, a Ras guanyl nucleotide-releasing protein with calcium- and diacylglycerol-binding motifs. Science 280:1082-1086. [DOI] [PubMed] [Google Scholar]
- 13.Filipp, D., B. L. Leung, J. Zhang, A. Veillette, and M. Julius. 2004. Enrichment of lck in lipid rafts regulates colocalized fyn activation and the initiation of proximal signals through TCR alpha beta. J. Immunol. 172:4266-4274. [DOI] [PubMed] [Google Scholar]
- 14.Filipp, D., J. Zhang, B. L. Leung, A. Shaw, S. D. Levin, A. Veillette, and M. Julius. 2003. Regulation of Fyn through translocation of activated Lck into lipid rafts. J. Exp. Med. 197:1221-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fukushima, A., Y. Hatanaka, J. W. Chang, M. Takamatsu, N. Singh, and M. Iwashima. 2005. Lck couples Shc to TCR signaling. Cell. Signal. 18:1182-1189. [DOI] [PubMed] [Google Scholar]
- 16.Genot, E., and D. A. Cantrell. 2000. Ras regulation and function in lymphocytes. Curr. Opin. Immunol. 12:289-294. [DOI] [PubMed] [Google Scholar]
- 17.Hermiston, M. L., Z. Xu, R. Majeti, and A. Weiss. 2002. Reciprocal regulation of lymphocyte activation by tyrosine kinases and phosphatases. J. Clin. Investig. 109:9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hernandez-Hoyos, G., S. J. Sohn, E. V. Rothenberg, and J. Alberola-Ila. 2000. Lck activity controls CD4/CD8 T cell lineage commitment. Immunity 12:313-322. [DOI] [PubMed] [Google Scholar]
- 19.Huang, J., K. Sugie, D. M. La Face, A. Altman, and H. M. Grey. 2000. TCR antagonist peptides induce formation of APC-T cell conjugates and activate a Rac signaling pathway. Eur. J. Immunol. 30:50-58. [DOI] [PubMed] [Google Scholar]
- 20.Hur, E. M., M. Son, O. H. Lee, Y. B. Choi, C. Park, H. Lee, and Y. Yun. 2003. LIME, a novel transmembrane adaptor protein, associates with p56lck and mediates T cell activation. J. Exp. Med. 198:1463-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irvin, B. J., B. L. Williams, A. E. Nilson, H. O. Maynor, and R. T. Abraham. 2000. Pleiotropic contributions of phospholipase C-γ1 (PLC-γ1) to T-cell antigen receptor-mediated signaling: reconstitution studies of a PLC-γ1-deficient Jurkat T-cell line. Mol. Cell. Biol. 20:9149-9161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karnitz, L., S. L. Sutor, T. Torigoe, J. C. Reed, M. P. Bell, D. J. McKean, P. J. Leibson, and R. T. Abraham. 1992. Effects of p56lck deficiency on the growth and cytolytic effector function of an interleukin-2-dependent cytotoxic T-cell line. Mol. Cell. Biol. 12:4521-4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krutzik, P. O., and G. P. Nolan. 2003. Intracellular phospho-protein staining techniques for flow cytometry: monitoring single cell signaling events. Cytometry A 55:61-70. [DOI] [PubMed] [Google Scholar]
- 24.Latour, S., R. Roncagalli, R. Chen, M. Bakinowski, X. Shi, P. L. Schwartzberg, D. Davidson, and A. Veillette. 2003. Binding of SAP SH2 domain to FynT SH3 domain reveals a novel mechanism of receptor signalling in immune regulation. Nat. Cell Biol. 5:149-154. [DOI] [PubMed] [Google Scholar]
- 25.Latour, S., and A. Veillette. 2003. Molecular and immunological basis of X-linked lymphoproliferative disease. Immunol. Rev. 192:212-224. [DOI] [PubMed] [Google Scholar]
- 26.Legname, G., B. Seddon, M. Lovatt, P. Tomlinson, N. Sarner, M. Tolaini, K. Williams, T. Norton, D. Kioussis, and R. Zamoyska. 2000. Inducible expression of a p56Lck transgene reveals a central role for Lck in the differentiation of CD4 SP thymocytes. Immunity 12:537-546. [DOI] [PubMed] [Google Scholar]
- 27.Leo, A., and B. Schraven. 2001. Adapters in lymphocyte signalling. Curr. Opin. Immunol. 13:307-316. [DOI] [PubMed] [Google Scholar]
- 28.Lin, J., and A. Weiss. 2001. Identification of the minimal tyrosine residues required for linker for activation of T cell function. J. Biol. Chem. 276:29588-29595. [DOI] [PubMed] [Google Scholar]
- 29.Lindquist, J. A., L. Simeoni, and B. Schraven. 2003. Transmembrane adapters: attractants for cytoplasmic effectors. Immunol. Rev. 191:165-182. [DOI] [PubMed] [Google Scholar]
- 30.Lucas, J. A., A. T. Miller, L. O. Atherly, and L. J. Berg. 2003. The role of Tec family kinases in T cell development and function. Immunol. Rev. 191:119-138. [DOI] [PubMed] [Google Scholar]
- 31.Matthews, S. A., E. Rozengurt, and D. Cantrell. 1999. Characterization of serine 916 as an in vivo autophosphorylation site for protein kinase D/protein kinase Cmu. J. Biol. Chem. 274:26543-26549. [DOI] [PubMed] [Google Scholar]
- 32.Molina, T., K. Kishihara, D. Siderovski, W. van Ewijk, A. Narendran, E. Timms, A. Wakeham, C. Paige, K.-U. Hartmann, A. Veillette, D. Davidson, and T. Mak. 1992. Profound block in thymocyte development in mice lacking p56lck. Nature 357:161-163. [DOI] [PubMed] [Google Scholar]
- 33.Olszowy, M. W., P. L. Leuchtmann, A. Veillette, and A. S. Shaw. 1995. Comparison of p56lck and p59fyn protein expression in thymocyte subsets, peripheral T cells, NK cells, and lymphoid cell lines. J. Immunol. 155:4236-4240. [PubMed] [Google Scholar]
- 34.Paz, P. E., S. Wang, H. Clarke, X. Lu, D. Stokoe, and A. Abo. 2001. Mapping the Zap-70 phosphorylation sites on LAT (linker for activation of T cells) required for recruitment and activation of signalling proteins in T cells. Biochem. J. 356:461-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Priatel, J. J., S. J. Teh, N. A. Dower, J. C. Stone, and H. S. Teh. 2002. RasGRP1 transduces low-grade TCR signals which are critical for T cell development, homeostasis, and differentiation. Immunity 17:617-627. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds, L. F., C. de Bettignies, T. Norton, A. Beeser, J. Chernoff, and V. L. Tybulewicz. 2004. Vav1 transduces T cell receptor signals to the activation of the Ras/ERK pathway via LAT, Sos, and RasGRP1. J. Biol. Chem. 279:18239-18246. [DOI] [PubMed] [Google Scholar]
- 37.Roose, J. P., M. Mollenauer, V. A. Gupta, J. Stone, and A. Weiss. 2005. A diacylglycerol-protein kinase C-RasGRP1 pathway directs Ras activation upon antigen receptor stimulation of T cells. Mol. Cell. Biol. 25:4426-4441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seddon, B., G. Legname, P. Tomlinson, and R. Zamoyska. 2000. Long-term survival but impaired homeostatic proliferation of naive T cells in the absence of p56lck. Science 290:127-131. [DOI] [PubMed] [Google Scholar]
- 39.Seddon, B., P. Tomlinson, and R. Zamoyska. 2003. Interleukin 7 and T cell receptor signals regulate homeostasis of CD4 memory cells. Nat. Immunol. 4:680-686. [DOI] [PubMed] [Google Scholar]
- 40.Seddon, B., and R. Zamoyska. 2002. TCR signals mediated by Src family kinases are essential for the survival of naive T cells. J. Immunol. 169:2997-3005. [DOI] [PubMed] [Google Scholar]
- 41.Sommers, C. L., R. K. Menon, A. Grinberg, W. Zhang, L. E. Samelson, and P. E. Love. 2001. Knock-in mutation of the distal four tyrosines of linker for activation of T cells blocks murine T cell development. J. Exp. Med. 194:135-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sommers, C. L., C. S. Park, J. Lee, C. Feng, C. L. Fuller, A. Grinberg, J. A. Hildebrand, E. Lacana, R. K. Menon, E. W. Shores, L. E. Samelson, and P. E. Love. 2002. A LAT mutation that inhibits T cell development yet induces lymphoproliferation. Science 296:2040-2043. [DOI] [PubMed] [Google Scholar]
- 43.Stefanova, I., B. Hemmer, M. Vergelli, R. Martin, W. E. Biddison, and R. N. Germain. 2003. TCR ligand discrimination is enforced by competing ERK positive and SHP-1 negative feedback pathways. Nat. Immunol. 4:248-254. [DOI] [PubMed] [Google Scholar]
- 44.Stein, P. L., H. M. Lee, S. Rich, and P. Soriano. 1992. pp59fyn mutant mice display differential signaling in thymocytes and peripheral T cells. Cell 70:741-750. [DOI] [PubMed] [Google Scholar]
- 45.Straus, D. B., and A. Weiss. 1992. Genetic evidence for the involvement of the lck tyrosine kinase in signal transduction through the T cell antigen receptor. Cell 70:585-593. [DOI] [PubMed] [Google Scholar]
- 46.Sugie, K., M. S. Jeon, and H. M. Grey. 2004. Activation of naive CD4 T cells by anti-CD3 reveals an important role for Fyn in Lck-mediated signaling. Proc. Natl. Acad. Sci. USA 101:14859-14864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trobridge, P. A., and S. D. Levin. 2001. Lck plays a critical role in Ca(2+) mobilization and CD28 costimulation in mature primary T cells. Eur. J. Immunol. 31:3567-3579. [DOI] [PubMed] [Google Scholar]
- 48.Utting, O., S. J. Teh, and H. S. Teh. 1998. T cells expressing receptors of different affinity for antigen ligands reveal a unique role for p59fyn in T cell development and optimal stimulation of T cells by antigen. J. Immunol. 160:5410-5419. [PubMed] [Google Scholar]
- 49.van Oers, N. S., N. Killeen, and A. Weiss. 1996. Lck regulates the tyrosine phosphorylation of the T cell receptor subunits and ZAP-70 in murine thymocytes. J. Exp. Med. 183:1053-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van Oers, N. S., N. Killeen, and A. Weiss. 1994. ZAP-70 is constitutively associated with tyrosine-phosphorylated TCR zeta in murine thymocytes and lymph node T cells. Immunity 1:675-685. [DOI] [PubMed] [Google Scholar]
- 51.Walk, S. F., M. E. March, and K. S. Ravichandran. 1998. Roles of Lck, Syk and ZAP-70 tyrosine kinases in TCR-mediated phosphorylation of the adapter protein Shc. Eur. J. Immunol. 28:2265-2275. [DOI] [PubMed] [Google Scholar]
- 52.Williams, B. L., B. J. Irvin, S. L. Sutor, C. C. Chini, E. Yacyshyn, J. Bubeck Wardenburg, M. Dalton, A. C. Chan, and R. T. Abraham. 1999. Phosphorylation of Tyr319 in ZAP-70 is required for T-cell antigen receptor-dependent phospholipase C-gamma1 and Ras activation. EMBO J. 18:1832-1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Winkler, D. G., I. Park, T. Kim, N. S. Payne, C. T. Walsh, J. L. Strominger, and J. Shin. 1993. Phosphorylation of Ser-42 and Ser-59 in the N-terminal region of the tyrosine kinase p56lck. Proc. Natl. Acad. Sci. USA 90:5176-5180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Winslow, M. M., J. R. Neilson, and G. R. Crabtree. 2003. Calcium signalling in lymphocytes. Curr. Opin. Immunol. 15:299-307. [DOI] [PubMed] [Google Scholar]
- 55.Yamashita, M., K. Hashimoto, M. Kimura, M. Kubo, T. Tada, and T. Nakayama. 1998. Requirement for p56(lck) tyrosine kinase activation in Th subset differentiation. Int. Immunol. 10:577-591. [DOI] [PubMed] [Google Scholar]
- 56.Yasuda, K., M. Nagafuku, T. Shima, M. Okada, T. Yagi, T. Yamada, Y. Minaki, A. Kato, S. Tani-Ichi, T. Hamaoka, and A. Kosugi. 2002. Cutting edge: fyn is essential for tyrosine phosphorylation of csk-binding protein/phosphoprotein associated with glycolipid-enriched microdomains in lipid rafts in resting T cells. J. Immunol. 169:2813-2817. [DOI] [PubMed] [Google Scholar]
- 57.Zamoyska, R., A. Basson, A. Filby, G. Legname, M. Lovatt, and B. Seddon. 2003. The influence of the src-family kinases, Lck and Fyn, on T cell differentiation, survival and activation. Immunol. Rev. 191:107-118. [DOI] [PubMed] [Google Scholar]
- 58.Zhang, L., U. Lorenz, and K. S. Ravichandran. 2003. Role of Shc in T-cell development and function. Immunol. Rev. 191:183-195. [DOI] [PubMed] [Google Scholar]
- 59.Zhang, W., R. P. Trible, M. Zhu, S. K. Liu, C. J. McGlade, and L. E. Samelson. 2000. Association of Grb2, Gads, and phospholipase C-gamma 1 with phosphorylated LAT tyrosine residues. Effect of LAT tyrosine mutations on T cell angigen receptor-mediated signaling. J. Biol. Chem. 275:23355-23361. [DOI] [PubMed] [Google Scholar]