Abstract
Objectives
To develop and implement a series of progressive evidence-based, oral presentation activities within the therapeutics series to strengthen interprofessional oral communication and literature evaluation skills.
Design
A step-wise progression of oral presentations was created to establish interprofessional communication skills and reinforce such skills in successive modules. Students progressed from a basic oral presentation to a brief clinical trial presentation, followed by a full journal club, culminating with a therapeutic debate. Guidelines and assessment tools were developed for each presentation focusing on style, content and organization, and analytic approach. Feedback was obtained from students and faculty members through the administration of survey instruments at the midpoint of advanced pharmacy practice experiences (APPE).
Assessment
The majority of students successfully completed each oral presentation. Most felt prepared for APPE presentations due to increased Microsoft PowerPoint skills, literature exposure/evaluation, and comfort/confidence in presenting before an audience. Faculty members stated that the innovation organized students’ thoughts and increased presentation clarity, resulting in less need to offer student assistance during APPEs.
Conclusion
Our progressive approach to oral presentations has been successful and well received by students and faculty members. Our innovation has fostered oral interprofessional communication skills in our pharmacy students, and we will continue to utilize this approach.
Keywords: communication, presentation skills, interprofessional education, assessment, therapeutics
INTRODUCTION
Pharmacy education should concentrate on preparing students to provide patient-centered, evidence-based pharmaceutical care.1 Pharmacists must be able to collaborate with other healthcare professionals and share the responsibility for drug therapy outcomes.1 To achieve these desired outcomes, students must be given curricular opportunities to develop and strengthen oral communication and literature evaluation skills.
Pharmacy schools traditionally teach a stand-alone communications course early in the professional curriculum.2 Results from a survey performed by Billow in 1990 showed that 80% of responding US colleges of pharmacy required students to complete a communications course.2 Generally, communication courses are taught by pharmacy faculty members and focus on pharmacist-patient interactions and/or interpersonal communication skills.
While this type of instruction in communication skills is essential, it does not adequately prepare students to communicate and collaborate with other healthcare professionals using an evidence-based approach. Educators and accrediting organizations recognize that effective and efficient communication between healthcare professionals is increasingly important in today's healthcare environment. For example, in a collaborative initiative in 3 colleges of medicine, Kalet and colleagues developed a communications competency document for their clinical clerkships. The document identified 3 core areas of communication skills: communication with the patient, communication about the patient, and communication about medicine and science.3
In addition, the Institute of Medicine (IOM) has demanded improvement in this area. The IOM report on Health Professions Education, released in 2003, stated that educators should ensure that students maintain proficiency in practicing evidence-based medicine and working as part of interdisciplinary teams.4 The educational outcomes established by the Center for the Advancement of Pharmaceutical Education (CAPE) also advocate that students be able to “communicate and collaborate with prescribers, patients, care givers, and other involved health care providers” and “retrieve, analyze, and interpret the professional, lay, and scientific literature to provide drug information to patients, their families, and other involved health care providers.”5
The School of Pharmacy's curriculum offers multiple opportunities for communication with patients, beginning in the second preprofessional year with Communication Skills for Pharmacists, an introductory course designed to provide students with various frameworks for understanding and practical tools for engaging in effective interpersonal communication with particular emphasis on healthcare contexts. The course covers basic skills, such as open-ended questions and the 3 questions to ask every patient, in preparation for students’ first introductory pharmacy practice experience (IPPE). The School of Pharmacy has an extensive and integrated IPPE program as part of Northeastern's cooperative education mission. The Department of Cooperative Education places about 5,000 students each year with more than 2,000 cooperative employers in Boston, across the United States, and in many other locations around the world. Unlike most cooperative education universities, Northeastern offers cooperative programs in virtually every undergraduate area of study. As part of cooperative experiences, pharmacy students are placed in community pharmacies and hospitals where they have the opportunity to interact with patients and other health care professionals. Students also progress to our pharmacy care laboratory in their third-professional year, which consists of live mock patient interactions, and simulated phone calls to physician offices. The curricular thread of communication culminates with advanced pharmacy practice experiences (APPEs).
Although our curriculum offered many opportunities for students to improve their communication skills with patients, there was little opportunity for students to practice communication skills with other health care providers. To meet these increasing educational demands, we developed and implemented a series of evidence-based, oral-presentation activities within the therapeutics series designed to strengthen interprofessional oral communication and literature evaluation skills.
DESCRIPTION OF INNOVATION
Therapeutics Course Description
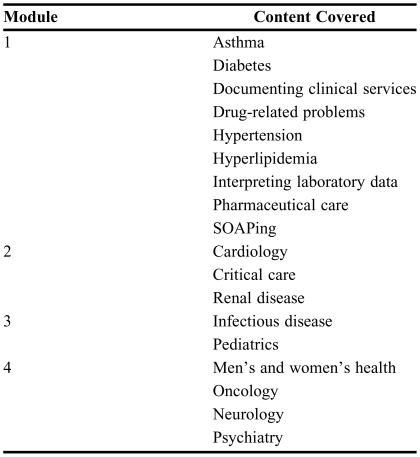
The therapeutics course series consists of four 4-credit modules taught over 2 semesters. The modules expose students to the clinical management of diseases most frequently encountered in pharmacy practice (Table 1). Instructors emphasize application of knowledge acquired from pharmacology and pathophysiology to provide pharmaceutical care to patients in both inpatient and ambulatory settings. Clinical skills, including recognition of efficacious and/or toxic drug effects, and identification and management of drug-related problems are emphasized. At the end of the course series, students should be able to explain the considerations and precautions required for the proper selection and dosing of drugs most frequently used for management of common disease states. The therapeutics courses are prerequisites to the APPE.
Table 1.
Content of Modules for a Therapeutics Course
Accompanying the didactic portion of the therapeutics course series, breakout sections of 12-14 students meet each week for 3-hour seminars to discuss the previous week's topics in a more applied, patient-centered, and case-based format. The therapeutics seminars provide students with opportunities to gather and interpret clinical data and relevant medical literature and use this information in addressing identified patient drug-related problems. The seminars are designed to facilitate accomplishment of the course objectives using an active-learning format. During the weekly seminar sessions, students break into small groups and discuss patient cases. Student leaders are expected to facilitate group discussions and, in turn, represent group responses to given patient problems. In solving such problems, students are encouraged to verbalize, integrate, and apply information presented in lectures and readings from previous and concurrent course work.
The goals of the course series are to develop skills that will enable the student to: (1) build the information base needed to design a therapeutic regimen; (2) design, implement, monitor, evaluate, and modify patient specific therapeutic regimens in accordance with established, evidence-based standards of practice; (3) identify, assess, and resolve drug-related problems, and develop clinical judgment as to the continuing effectiveness of individualized therapeutic plans and intended therapeutic outcomes; (4) retrieve, evaluate, and manage professional information and literature; (5) communicate with patients and health care professionals regarding rational drug therapy, wellness, and health promotion, and document therapeutic interventions appropriately.
Implemented Changes
In 2003, the University converted from a quarter to a semester calendar. This provided us with an opportunity to evaluate goals and objectives and redesign the Therapeutics course series. Feedback from student and faculty member surveys revealed that the series was preparing students well in most areas. However, 2 areas of improvement were identified: the need to improve teaching and assessment of students’ literature evaluation, and the need to strengthen interprofessional communication skills.
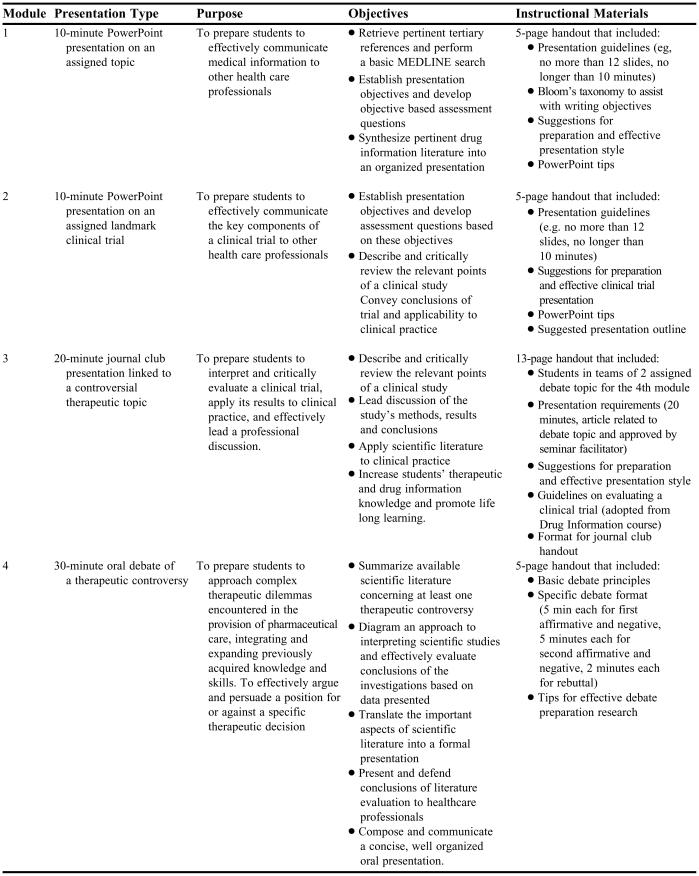
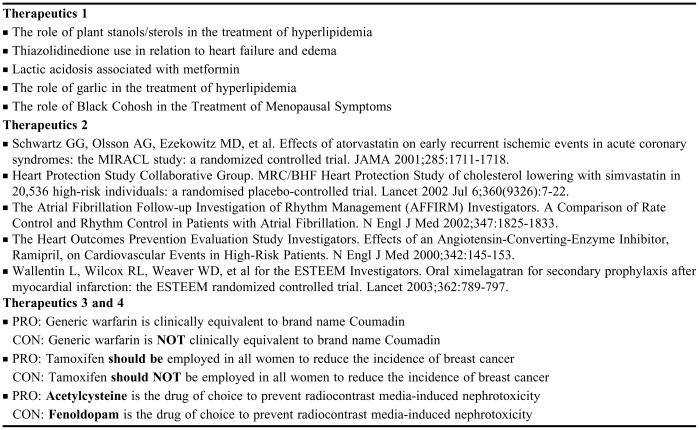
Based on these results, we created a stepwise progression of oral presentation assignments to address the following course objectives: (1) verbalize clear, concise thoughts to peers and to other health professionals in a group setting, and (2) accurately and concisely summarize scientific literature and apply this information to drug therapy. The complexity of assignments increased in terms of therapeutic content and level of drug information retrieval and evaluation skills over the 4 modules (Table 2). The initial module started with basic communication and literature evaluation skills and subsequent modules required additional skills. The sequence was designed to help students develop skills for successful presentations commonly required during APPEs and in clinical pharmacy practice. To accomplish this and to ensure student competency, individualized feedback was given. Students were required to submit presentation learning objectives and assessment questions for facilitator review weeks before the presentation. They were also required to meet with facilitators for progress reports at various times. Topics for each presentation type were purposely chosen because they were not covered in depth in the didactic portion of the course series. This was done to increase student awareness and knowledge of natural and herbal remedies, specific landmark clinical trials, and current therapeutic controversies (Table 3).
Table 2.
Oral Presentation Assignments in a Therapeutics Course Series
Table 3.
Examples of Student Presentation Topics Given in a Therapeutics Course Series
Module 1
The first module required the students to give a 10-minute oral presentation on a topic complimenting a disease state taught in the module. The main focus was to prepare students to retrieve pertinent medical literature and organize and deliver PowerPoint presentations to an audience of health care professionals. Students received specific objectives and instructions on the format of their presentation and tips on how to prepare. Students developed 2 presentation objectives, as well as 2 objective-based assessment questions. Students were evaluated based on presentation style (33%), organization (33%), and content (33%). A rubric was created with detailed descriptors to allow evaluators to assign 1 of the following 3 assessments for each item: (1) better than expected performance level, (2) average performance level, or (3) poorest anticipated performance level. The presentation was assessed in terms of the pace of delivery, eye contact and use of notes, audibility and speech flow, use of professional language, and effectiveness of PowerPoint slides to enhance the presentation. Organization was assessed in terms of use of allotted time, adherence to guidelines for presentation, students’ ability to explain clearly and concisely, and overall level of preparation. Content was evaluated in terms of students’ success in addressing each presentation objective, presenting pertinent background information, and discussing pertinent medical literature. Students’ ability to concisely summarize all information presented and emphasize important points in the conclusion, answer all questions, and format references appropriately were also evaluated.
Module 2
In the second module, students progressed to a brief presentation of a clinical trial. Landmark clinical trials were selected to complement the cardiology/critical care content area of this module. Students were expected to enhance their presentation skills based on the feedback provided during the previous module. An additional focus of this presentation was the critique and synthesis of a clinical trial and the skills necessary to convey their thoughts to a professional audience. Students were expected to utilize PowerPoint and were provided with specific presentation guidelines. Once again, students were required to write presentation objectives and assessment questions. The assessment rubric utilized was similar to that used during module 1, in that points were equally divided among areas of presentation style, organization, and content, but changes were made in the area of content assessment. Content was evaluated in terms of a student's ability to address each presentation objective and adequately and concisely summarize trial methods and results. In addition, students were to provide well-developed and complete critiques of trial strengths and weaknesses, make appropriate conclusions regarding the clinical utility/generalizability of the trial to practice, and have a working knowledge of the clinical trial so they could adequately answer questions.
Module 3
Students progressed next to preparing and delivering a full journal club presentation on a controversial therapeutic topic, which would be debated in Module 4. Students were placed in groups of 2 and assigned the pro or con side of a controversy. The focus of the journal club presentation was the identification and retrieval of appropriate literature, with a more detailed critical evaluation of a clinical trial and its application to clinical practice than in module 2. Seminar facilitators were asked to ensure that students performed adequate literature searches and identified pertinent scientific literature through individual student meetings. Students were required to present their findings using a specific journal club format6 and to lead a group discussion of the article. Each group was given 20 minutes which was equally divided between the 2 students, with 5 additional minutes allowed for questions and discussion. Students were asked to write 2 assessment questions for the audience to answer. PowerPoint was not used; however, students were required to prepare a handout containing background information on the study question, summarizing previous clinical trials, trial methods, results, and authors’ conclusions. They were also required to provide extensive critiques of the study methods and results, and supply their own conclusions and opinion of the applicability of the trial to clinical practice. Students were encouraged to use transparencies of tables and figures from the trial to summarize results and lead the discussion. An assessment rubric similar to those used during the first 2 modules was created to evaluate the style, organization and content, and analytic/synthetic approach of the students’ presentation. Presentation style (20%) was evaluated similarly to the first 2 modules, although assessment of PowerPoint utilization was replaced by appropriate use of audiovisual equipment and effectiveness of the handout. Organization and content (30%) evaluated the student's ability to present appropriate background information, discuss relevant previous clinical trials, emphasize important points, explain clearly, and use time appropriately. The students’ analytic/synthetic approach (50%) assessed their ability to critically evaluate methods and results, make their own conclusions, correlate the trial results to clinical practice, and answer audience questions.
Module 4
The final oral presentation was a debate on a therapeutic controversy. In addition to the journal club article presented in module 3, the debate incorporated other relevant primary literature identified by students, and required teams of 2 students to provide an evidence-based case for or against the debated topic. Students were required not only to prepare an argument for their specific side of the debate (pro or con), but also to anticipate the arguments of the opposition and prepare evidence-based rebuttal remarks to persuade the audience. This activity required a higher level of skill than any of the previous oral presentations and included a “thinking on your feet” component. A specific debate format was developed and the basic debate principles and time limits for each debate exchange were explained. Each side had 5 minutes for initial statements, 5 minutes for rebuttal, and 2 minutes for concluding statements. An additional 5 minutes were allowed for questions and discussion. Student groups were required to meet with their seminar facilitators to review debate outlines weeks before the presentation. Facilitators provided students with feedback at the point of the meeting, and assessed student responses and incorporation of previous feedback into the final presentation. An assessment rubric similar to that used during module 3 was developed. In addition to the presentation skills (20%) assessed during the previous 3 modules, students were also assessed on their ability to address the opposing team with respect and professional courtesy, and their ability to persuade the audience through their credibility, goodwill, and sincerity. Content (30%) was assessed based on the student's overall knowledge of the topic, ability to follow the designated format, emphasize important points, and use time appropriately, and on their overall preparedness. The analytic/synthetic approach (50%) was assessed according to the student's ability to identify, synthesize, and present relevant scientific literature; critically evaluate, interpret, and develop an argument based on that literature; and make recommendations for clinical practice supported by the body of evidence presented.
EVALUATION AND ASSESSMENT
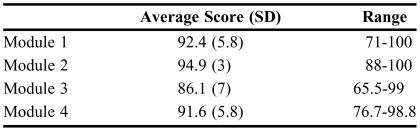
Multiple instructors were required to facilitate the 8 seminar sections per module. Every student received 1 evaluation for each presentation. (The evaluation form is available from the author.) Each facilitator was responsible for grading his or her 12-15 student presentations. Efforts were made to standardize expectations and evaluation of students during seminar in a number of ways. Coordinators of each module met with all facilitators before module initiation to orient them to seminar format and activities covered, and to provide strategies for effective facilitation. Facilitators completing the previous module were present to offer advice to new module facilitators in an attempt to maintain continuity in format and expectations. All facilitators were given each presentation's guidelines and the evaluation form, and both were discussed at the initiation of each module. Each module coordinator assessed all oral presentation evaluations to ensure consistency in grading between sections. If one facilitator's average grades for an oral presentation were significantly lower or higher than all other sections, the coordinator met with the facilitator to reach an equitable compromise. Presentation grades for each module are listed in Table 4. The majority of students were deemed competent (>73%), with a small number of failures in module 1 (2 of 79, 2.5%) and module 3 (3 of 76, 4%).
Table 4.
Assessment Results of Oral Presentations in a Therapeutics Course Series
Student and faculty questionnaires were distributed after the students completed all modules and 3 of their 6 required APPEs. The purpose of the surveys was to obtain feedback about the oral presentation structure, guidance, progression, and assessment, and any impact on preparation for APPE presentations.
Student survey questions focused on their perspective of facilitator guidance on the format and directions for each presentation, their ability to communicate with other health care professionals, and the ability to write presentation objectives and assessment questions. The impact of the innovation on students’ perceived preparedness for APPEs was also assessed. In addition, students were asked about the impact that the progression of oral presentations had on presentation skills and confidence, and finally, whether continuance of such a format was worthwhile.
Faculty survey questions focused on their awareness of the modifications to the presentations, utility of each activity, and opinion about whether the presentation innovation should be continued. In addition, faculty members were asked to compare students who had gone through the modified presentation format to previous students during APPEs. Specific questions assessed faculty member's perception of students’ ability to retrieve, evaluate, and manage professional information and literature, formally present in a self-assured manner (eg, good eye contact, talks to the audience, limited use of notes), adequately and concisely summarize data presented, emphasize important points in the conclusion in a professional manner, and use PowerPoint with little preceptor instruction. Many questions also focused on the level of preceptor instruction required with regard to the aforementioned student skills. Additional questions asked if the therapeutics series presentation modifications resulted in less instruction and individual assistance needed for oral presentations during APPEs and if student grades were higher than in previous years.
Survey Results
Twenty-two of 79 student survey instruments (28%) and 9 of 18 faculty survey instruments (50%) were returned. Student responses regarding the process and progression of the oral presentations were very positive. Fifteen students (68%) provided specific comments about the strength of the oral presentation format. The majority of students felt that the presentations prepared them well for APPE assignments and presentations by increasing their PowerPoint skills, exposing them to more literature evaluation, and increasing their therapeutics knowledge and their comfort and confidence with giving presentations before an audience. Application of knowledge and skills was reiterated by a number of students. Many students also believed that the 4 presentations allowed them to develop their own presentation style. Table 5 lists specific verbatim comments from students regarding the strengths of the innovation. One of the problems expressed by students with this process relates to the variability of seminar facilitators and their expectations. As the seminar component to the course series requires 8 facilitators per module, a number of faculty members as well as area pharmacy residents were involved with facilitation.
Table 5.
Student Comments Regarding Oral Presentations for a Therapeutics Course Series
Some students reported that the first oral presentation format was not explicit enough compared to guidelines for other presentations. These comments may be due to the fact that this was the first presentation assignment and their first exposure to therapeutics and their first interaction with clinical faculty members. As they progressed through the presentations, it is not surprising that they found successive presentation guidelines clearer and more easily adjusted to format modifications. While some students wanted more specific guidance, other students felt the format and guidelines were too rigid and were detrimental to students’ natural presentation style and ability. In response, we acknowledged the rigidity of the presentation guidelines, but believed that promoting well-accepted, standardized processes in the presentation and dissemination of information was vital at this level of the students’ education. While we were not trying to hinder creativity in our students, we agreed that a basic format should be followed to increase the effectiveness of our students during APPEs and in their professional lives.
Another weakness expressed by a number of students was a lack of guidance and supervision with the debate and its format. Comments indicated that students were not clear on the general purpose of the debate, and felt much less prepared for this presentation compared to the others. Some students suggested watching a “mock” debate to gain better insight to the format and the expectations. In order to improve student performance on the debate, as well as increase their understanding, we explained the results to the specific module coordinator, who will spend more time on the debate format and process with students.
Students were also asked to provide any suggestions for improving the progression of seminar oral presentations. Many viable suggestions were made, including:
Add self-reflection and peer comments and evaluation to each presentation to enhance learning.
Facilitators should meet individually with students after the presentation to provide verbal feedback about strengths and weaknesses rather than just written comments.
Extend the time for presentations from 10 minutes to 12 minutes in Therapeutics I and II.
Combine the first 2 presentations, and place the journal club 2 weeks before the oral debate. This would “decrease the stress of students because they would not have a major presentation due every 7 weeks, and might allow students to better apply the journal club to their debate.”
Allow students to choose the topic of one of their presentations in an area that is interesting to them. “Maybe during the debates, if there was a list of topics to choose from, student pairs would be able to pick the discussion that is most interesting to them and that they feel the most passionate about.”
Faculty members were overwhelmingly positive in their responses to the seminar oral presentation survey. Strengths cited by faculty members included increased organization of students’ thoughts and an increase in the clarity of their work. Development of PowerPoint skills was also considered a strength that was reiterated by a number of respondents, as they noticed that they had to assist students less than in previous years. In general, faculty members felt that students in the current APPE year were more experienced presenters and knew the basic format to approach different types of oral presentations. We feel that this is important, as many preceptors use variations of format for oral presentations and journal clubs during their APPEs. This student cohort seemed better able to adapt to multiple preceptor formats compared with students in previous years.
While faculty members were positive overall, there were some negative comments about the seminar oral presentations. One responder commented about the time needed from a facilitator standpoint for the preparation of debates, which require multiple meetings with each student to monitor progress. Another faculty member commented that the oral presentations can be difficult logistically if the room is not equipped with appropriate audiovisual equipment. Another interesting comment acknowledged the strengths of the presentations and the logical progression, but commented that because the presentations must be kept short due to time constraints, it may detract from the applicability of the exercise to APPE presentations. Also, while the majority of faculty members did think that current APPE students were better able to retrieve and evaluate literature, use PowerPoint, give formal presentations in a self-assured manner, and answer questions appropriately and concisely, most stated that they did not see any improvement in students’ journal club or oral case presentation evaluations or grades. We feel that this observation, which at first seems contradictory, may be explained by the varying types of presentation subjects encountered in APPEs, and also the more intense focus on content rather than presentation skills on the APPE evaluations.
Faculty members also echoed students’ suggestions to demonstrate some or all of the seminar oral presentations to the therapeutics students to better understand the formatting and overall expectations. Other faculty members expressed the need to “make students take ownership for this information once they come to APPEs” and felt that the redesign of the progressive seminar oral presentations was a good step forward in setting realistic expectations for APPEs.
We believe that this innovation is easily transferable and practical for other pharmacy programs to implement. All schools of pharmacy contain a therapeutics based course, and most also have smaller breakout sections. Oral presentations described herein could be added or modified for this purpose. Alternatively, other courses could easily utilize a structured progressive format as described. Different presentation types could be assigned in different courses, yet could still maintain the progressive step-wise approach as long as the chosen courses occur in succession. However, this may be logistically difficult if other courses do not have smaller breakout sections, as each individual student or student pair must make a presentation.
We believe that our approach is innovative because it considers the issue from a logical curricular perspective as opposed to individual faculty teaching in detached “silos” and students learning a specific faculty member's expectations simply for assignment purposes. The approach incorporates drug information skills into the therapeutics series and shows a true progression through modules. It has also been a true team effort involving the entire pharmacy practice department. All members have been asked for their views about the course series and seminar and ways to improve, including developing oral presentation topics, role of facilitators, grading, and the role of coordinators. We conducted a complete assessment during this process including student self-reflection, faculty evaluations, coordinator self-reflections, group reflections, and subsequent course modifications. Our approach also shows that communication skills need to be revisited throughout the curriculum and not just in standalone courses such as communications or the current writing requirement for our students. It is also innovative because we were able to connect each therapeutics module with the next via the progression in difficulty of each presentation. Each presentation built on the previous one, which resulted in reinforcement of basic oral communication skills while adding new components with each successive module.
Our innovation was implemented because we identified the need to improve student preparation for APPEs. We were specifically attempting to improve students' inter-professional presentation skills, PowerPoint mastery, drug information retrieval, and literature evaluation skills. We also felt it extremely important to establish more links and consistency throughout the therapeutics course series. We recognized that using the debate format for each module would start at a skill level too advanced for the majority of our students, and we felt that they needed more guidance and experience with the building blocks of an oral presentation before they could reach the final integrated step (therapeutic debate).
We were disappointed in the response rates to our student and faculty surveys (28% and 50% respectively). However, in a meta-analysis of Web-based surveys conducted by Cook et al7 the representativeness of the population of a survey is emphasized more than the rate of response. The authors state that one can expect a 25%-30% response rate from an electronic survey instrument when no follow-up takes place, and an increased rate when a reminder is sent. Our response rates fall into this category. Although we did send a reminder, no incentives were offered for completing the survey instrument. The timing of the surveys may also have resulted in lower rates than reported due to the fact that they were conducted 6 months later.
Overall, we feel that our progressive approach to oral presentations in the Therapeutics course series has been very successful and well received from both a student and faculty perspective. Students felt that adequate guidance was provided for the majority of presentations and that the progression of such assignments was logical. They also felt that they were better prepared for APPEs in terms of PowerPoint skills, being exposed to more literature evaluation, and increasing their confidence with giving presentations. Faculty members concurred and conveyed that students seemed better prepared for oral presentations and required less individual preceptor assistance during APPEs than students in previous years. We think that the topics chosen complemented the course material, and improved the overall curriculum by focusing on content areas such as herbal products and drug-induced diseases that are often viewed as deficient. Students felt they emerged from the course series with tangible oral presentation skills and were well prepared for the last year of their pharmacy curriculum.
We were disappointed to see that many students did not seem to grasp the debate concept and purpose. We feel that this may have been because they were not given adequate instruction on the format and directions for the debate. In fact, our student survey demonstrated almost 40% of students did not feel they received adequate guidance for this presentation. This is unfortunate, as the oral therapeutic debate is the culmination of the 3 previous oral presentations and combines many aspects of each into a single presentation. The oral debates also have the potential to be exciting and fun for students and faculty members alike, and we were disappointed that this did not come across. We are attempting to rectify this for the current therapeutics class by encouraging the module coordinator to describe the debates in detail to students, emphasize the purpose of the debates, clarify the role of the debates in student preparation, and allow enough time for student questions and feedback in the discussion and explanation. We will also focus on education of the seminar facilitators during this therapeutics module to increase consistency and increase understanding of the debate process among faculty members and adjunct faculty members. Consistency of facilitator grading has also been a high priority for us, with a focus on assessment of all module facilitators’ oral presentation evaluations to ensure reliable student grading among many different faculty members.
We plan to modify our approach in the upcoming year. The therapeutics course series has been given additional semester hours, and now contains 5 modules. Therefore, we have added a fifth communication presentation, a written pharmacokinetic consult note. In our discussions, we determined that adding a written communication component to the course series would provide an opportunity to assess another vital skill that students needed for APPEs and in clinical practice. We are incorporating the use of written SOAP notes into many seminar sessions in modules 1 and 2, where students will turn in their notes at the end of the seminar and the seminar facilitator will return them the next week with individualized feedback. SOAP notes have also been incorporated into some examinations. Students will now be required to write a formal pharmacokinetic consult note in module 3 for their seminar presentation evaluation. The purpose of the pharmacokinetic note is to evaluate students’ ability to manage pharmacotherapy that requires therapeutic drug monitoring often involving complicated calculations. It is designed to model a true pharmacokinetic consult service.
CONCLUSION
Our innovative approach has been well received by both faculty members and students and has made an impact on students’ ability to create and deliver effective presentations to other healthcare professionals. We will continue to utilize this format of progressive oral presentations during the therapeutics series with the modifications described to foster oral and written inter-professional communication skills in our pharmacy students. In addition, our approach creates another opportunity for students to enhance their literature evaluation skills.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Northeastern University Center for Effective University Teaching which awarded us with an Instructional Development Fund Grant to support this educational effort.
REFERENCES
- 1. Accreditation Council for Pharmacy Education. Accreditation standards. Available at: http://www.acpe-accredit.org/deans/standards.asp. Accessed on June 9, 2005.
- 2.Billow JA. The status of undergraduate instruction in communication skills in U.S. Colleges of Pharamcy. Am J Pharm Educ. 1990;54:23–6. [Google Scholar]
- 3.Kalet A, Pugnaire MP, Cole-Kelly K, et al. Teaching communication in clinical clerkships: models from the Macy Initiative in health communications. Acad Med. 2004;79:511–20. doi: 10.1097/00001888-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Greiner A, Knebel E. Committee on the Health Professions Education Summit.Health Professions Education: A Bridge to Quality. Washington, DC: National Academy Press; 2003. Institute of Medicine. [PubMed] [Google Scholar]
- 5. American Association of Colleges of Pharmacy, Center for Advancement of Pharmaceutics Education. Available at: http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf. Last accessed: June 9, 2005.
- 6.Baroletti D, Szumita PM. PIES method of critique. Vol. 3. Crit Pathways in Cardiol; 2004. PIES method of critique; pp. 205–8. [DOI] [PubMed] [Google Scholar]
- 7.Cook C, Heath F, Thomson R. A meta-analysis of response rates in web- or Internet-based surveys. Educ Psychol Meas. 2000;60:821–6. [Google Scholar]