Abstract
Objective
Establish a 3-year hospital internship within a drug use and disease state management program that would provide doctor of pharmacy students with experiential learning while still completing their classroom studies.
Design
As paid interns, students engaged in group and individual activities that assessed clinical practice guidelines. Patient monitoring and clinical intervention techniques were learned through prospective evaluation of drug therapy. Students designed evidence-based treatment guidelines and participated in all phases of development, including multidisciplinary approval, implementation, and evaluation stages.
Assessment
Student competency was continually monitored through direct observation by a preceptor and written examinations. Patient case studies, group discussions, and poster presentations allowed assessment of student growth in knowledge and communication skills.
Conclusion
The comprehensive structure of this internship provides a broad perspective for understanding the role of the hospital pharmacist in providing pharmaceutical care. Close supervision maximizes student learning potential and fosters a mentoring relationship for both personal and professional growth.
Keywords: experiential learning, internship, disease state management, clinical practice guidelines, hospital practice
INTRODUCTION
Experiential learning, which is the application of classroom learning in a real-life interactive environment, is a teaching strategy that is commonly used by colleges and schools of pharmacy. It often takes the form of individualized mentoring by site preceptors and discussions of concepts as they relate to scenarios encountered in daily practice. An example of experiential learning is an advanced pharmacy practice experience (APPE), which can occur for a limited duration such as 1 month, or involve a longitudinal experience, consisting of several hours of service learning per week throughout the school year.1
Typically, credit hours are earned for experiential learning programs, and dedicated time for off-site (non-classroom) learning is built into the curriculum. Several articles have been published on activities performed by students as part of pharmacy school courses.1-3 However, published information is limited for structured learning opportunities that are part of hospital pharmacy healthcare delivery models involving direct patient care but not part of a college's core curriculum.
Student internships in hospital pharmacy practice normally have responsibilities related to medication preparation and distribution, since these skills are critical to pharmacy practice. This type of internship typically does not provide advanced learning opportunities such as performing medication management interventions, performing prospective drug use evaluations, interacting with healthcare team members to design new clinical initiatives within the hospital, or creating results-oriented presentations at national meetings.
It is essential to train pharmacists to be versed not only in pharmacology and therapeutics, but also in literature review and critique, protocol development, and patient outcome evaluation. A novel method of providing this advanced training is through a longitudinal internship practice model for pharmacy students within the hospital environment.
A unique 3-year pharmacy internship program was created as part of an ongoing effort to enhance experiential learning in the doctor of pharmacy program, through a partnership between the University of Pittsburgh School of Pharmacy clinical faculty and the University of Pittsburgh Medical Center (UPMC), the hospital where faculty members provide clinical services. This program allows students to actively learn strategies for designing and implementing treatment guidelines and outcome-driven health care initiatives, while developing verbal and written communication and clinical problem-solving skills. This learning experience provides a broad base for understanding the important role of the pharmacist in improving patient care in a hospital setting. It is not a degree requirement of the pharmacy curriculum; in fact, only a small number of highly motivated students are accepted for the internship. This opportunity is sought by students interested in pursuing postdoctoral training because of the broad scope of experience and the highly individualized attention that is provided.
DESIGN
Educational Goals
The Accreditation Council for Pharmacy Education (ACPE) has established standards for curriculum, students, and faculty members of colleges and schools of pharmacy.4 The professional competencies and expectations can be organized into 3 major components of learning: critical thinking, systems/process management, and communication. Student achievement should be evaluated throughout the curriculum by measuring learning in these areas. Case-based learning, use of classroom technology, and application of concepts to patient scenarios are encouraged.
The ACPE recommends that faculty members in advanced-practice learning sites be involved in direct patient care and also be role models for teaching and learning. The American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education (CAPE) was created to organize the framework for outcomes for the pharmacy curriculum, and its work continues to be centered on provision of pharmaceutical care. A particular focus of the CAPE outcomes beyond individualized pharmaceutical care is on population-based medicine and public health promotion, with a heavy emphasis on medication use systems and information management.5 Curricula for colleges and schools of pharmacy should be designed with consideration to both ACPE and CAPE recommendations. Application of these outcomes to hospital-based learning programs, outside of the School's formal curriculum, is the fundamental mission of our student intern program.
Internship Practice Site
The practice site for the internship was established within a specialized hospital pharmacy setting at the UPMC: the Drug Use and Disease State Management (DUDSM) program. The UPMC Presbyterian (UPMC-P) Department of Pharmacy and Therapeutics implemented this DUDSM Program in July 1996.6 Faculty members, hospital-based clinical staff pharmacists, clinical scientist associates, a pharmacy technician, and pharmacy students provide the infrastructure of the program. The primary goal of the DUDSM program is to design, implement, and actively promote evidence-based clinical practice guidelines that ensure safe and cost-effective drug therapy. Impact of the drug use criteria and disease state management algorithms on improving patient care is evaluated using principles of continuous quality improvement.
Multidisciplinary collaboration and systematic implementation are essential components of DUDSM guideline development, in addition to economic, process, and clinical outcome assessment. Guidelines developed by the DUDSM program are presented to and approved by the UPMC-P medical staff Pharmacy and Therapeutics Committee, a peer-review group that is responsible for formulary decision-making in the hospital. The DUDSM program leads these efforts for the multi-facility UPMC health system, one of the largest academic health systems in the country, consisting of 14 member hospitals, and providing care for over 75,000 inpatients and 1 million outpatients at its different facilities each year.
Currently, over 175 clinical guidelines are active at UPMC-P through the DUDSM program, comprising 6 categories: (1) dose/route optimization; (2) therapeutic interchange (eg, drug class selection); (3) patient safety; (4) disease management; (5) operational (eg, drug shortage plans); and (6) off-label medication usage. To share learning and promote evidence-based practice, numerous DUDSM guidelines have been published and presented at national meetings. Notably, DUDSM efforts have received awards from local, regional, and national quality and hospital pharmacy organizations. Contributions to patient care include optimizing antibiotic selection and duration, decreasing use of dangerous drugs in the elderly, promoting evidence-base use of medications, and increasing inpatient vaccination rates.7-11
Program Structure
The internship program was designed to enhance students’ clinical skills in a hospital-based advanced practice site through all aspects of the DUDSM Program, including guideline identification, development and implementation, as well as medication management intervention and patient outcome monitoring. Students spend roughly 50% of their internship time on projects or guideline development and 50% on direct patient care activities. Understanding the impact of preventative and cost-effective healthcare management programs in today's environment is another goal of the student experience.
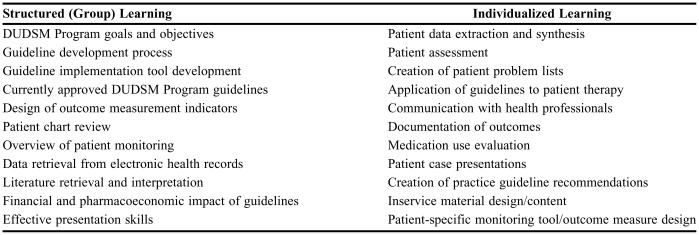
The internship program includes small group and individualized structured-learning activities (Table 1). Structured learning not only occurs in the initial orientation, but throughout each student's participation in the program. Individualized involvement in DUDSM projects builds progressively under the supervision of DUDSM team members. Application of learning to hospitalized patients is evaluated through real-time active interventions performed with a pharmacist mentor.
Table 1.
DUDSM Program Structured and Individualized Learning Focal Points
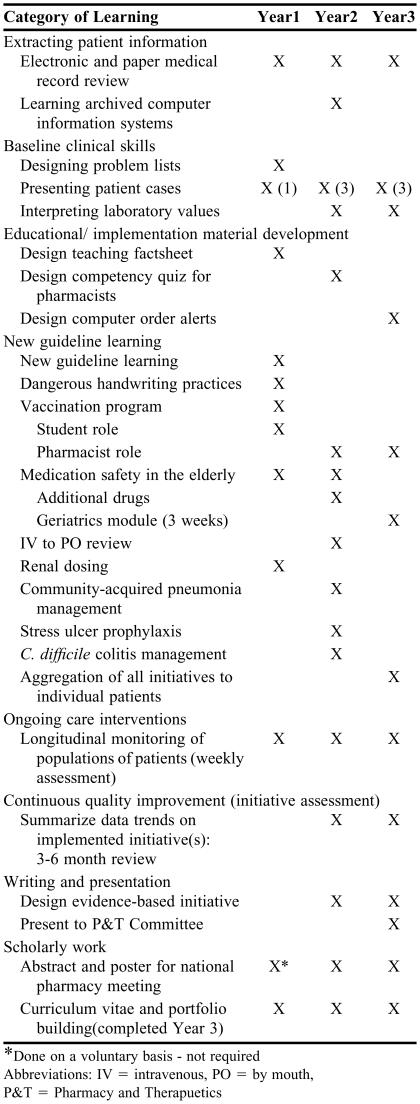
The progression of student learning in the internship is deliberate and aggregated over the 3 years of learning as depicted in Table 2. Over the course of their internship, students develop guidelines on their own. Projects are provided on an individual basis, according to the needs of the hospital and the abilities and demonstrated competencies of the students. A high level of supervision is provided by the DUDSM program director for project development and the guidelines developed by students are extensively reviewed by DUDSM faculty members prior to presentation to the UPMC-P Pharmacy and Therapeutics Committee.
Table 2.
Student Intern Learning Activities
* Done on a voluntary basis - not required
Abbreviations: IV = intravenous, PO = by mouth, P&T = Pharmacy and Therapuetics
Students evaluate patient medication regimens as part of ongoing quality improvement monitoring according to the medical staff Pharmacy and Therapeutics Committee-approved guidelines. Students perform both traditional drug utilization evaluations and concurrent medication management interventions on hospitalized patients. All direct patient care activities and projects are completed with proper supervision and approval from a licensed pharmacist. Through this structure, students have the opportunity to see the impact of clinical practice guidelines on patients.
Student Recruitment and Selection
Interest in the DUDSM internship is solicited each year via a meeting with first-professional year pharmacy students as well as through a position availability notice which is sent to students by electronic mail. The goals and requirements of the internship are also provided in the notice. The recruitment process itself is designed to prepare students to apply for residencies and employment postgraduation. Students interested in pursuing the internship program are asked to submit a letter of intent as well as curriculum vitae or resume. Students are interviewed and selected based on interest level, experience, and motivation. Hospital pharmacy experience is desired but not required for students in the internship program.
The students who enter the DUDSM internship are embarking on a career track to be clinical pharmacists; they are focused toward pursuing a pharmacy residency upon graduation. Essential characteristics of these students include effective communication skills and a desire to interact directly with patients and health care providers in the institutional setting. Students who have been active in pharmacy organizations and/or community service, who can describe examples of teamwork, leadership, and problem-solving from prior work, school, and/or life experiences, along with those currently working during the school year, are attractive candidates, as these characteristics denote drive, planning and organization, communication, and self-directed learning (orientation) dimensions of performance.
Students selected for the DUDSM internship are hired as paid employees of UPMC-P, since they contribute to the DUDSM program productivity through their projects and clinical intervention efforts. The number of students employed in the DUDSM program varies from year to year depending on funding resources and the qualified applicant pool. On average, 3 new student interns per year are hired into the program. As students begin the internship, they apply to the State Board of Pharmacy to get an internship license if they do not already have one.
Student Training and Supervision
Student interns work full-time during the summer month, and approximately 10-12 hours per week throughout the school year. Initially they must undergo new hospital employee training and complete hospital-based certification modules in occupational health and safety, regulatory compliance, and patient confidentiality. An extensive 1-month orientation is given to new student interns to inform them about goals and objectives for the DUDSM program as well as requirements for the internship. The importance of DUDSM programs in institutional practice today and the pharmacist's role in the programs are also covered.
The extensive training provided by the DUDSM team over the summer months includes both individual and group learning opportunities (Table 1). During the first summer of the internship, approximately 3 days per week are spent learning the basics of patient assessment as described below. Group learning sessions also occur on these days, led by different members of the DUDSM team depending on the topic. For example, the session on ”data retrieval from electronic health records” is facilitated by our data analyst pharmacy technician. In addition, weekly group sessions are held with the Director of the DUDSM program to discuss student projects. The students share their experiences with patient/healthcare practitioner encounters and project work with the group so all can learn from the different obstacles encountered and solutions developed.
During the summer, pharmacy students work full-time in the DUDSM program, spending approximately 50% of their time in direct patient care activities as noted above, and the remaining time on project development. Direct patient care time is mentored by faculty members and clinical pharmacists, in a one-on-one fashion, with a faculty member/pharmacist averaging 3 hours per day with a student, similar to that of work rounds during an APPE. During group patient care sessions, pharmacy students learn together, especially as the senior interns teach the new intern class. To expose the students to the widest variety of clinical practice approaches, interns work with all of the DUDSM staff members throughout their internship. A monthly training calendar is created so the students and team know the topic and trainers in advance. This creates an organized work environment and allows trainers to plan their time while continuing with other job responsibilities.
The structure of this internship fosters student independence and self-directed learning, so overall the amount of training and direct supervision by DUDSM staff members diminishes over time. The students continue to receive approximately 1 to 3 hours per week of direct supervision during the school year, provided mainly by the DUDSM Director and the data analyst pharmacy technician. During this time, students are given feedback on guideline projects and retrospective evaluations through individual meetings and/or written communication. At evaluation time points, the DUDSM Director discusses progress on projects and clinical skills development with each pharmacy student.
Student Experiential Learning
Clinical Practice Guidelines
Students learn to systematically search and evaluate the published literature on an assigned topic. They evaluate baseline prescribing practices in the hospital, and as they gain these essential skills and background information, students begin to develop hospital-specific evidence-based clinical practice guidelines. Students participate in all activities related to creating new guidelines, from initial assessment through necessary hospital approval processes. Guideline development may involve application of an existing published national guideline (eg, preventing deep venous thromobosis) to our institution, or creation of a new guideline not yet in existence. Through participation in multidisciplinary UPMC committees that collaboratively develop the clinical practice guidelines, students acquire skills for facilitating group consensus. They also perform financial impact evaluations, create successful implementation strategies, design clinical outcome indicators, and evaluate patient outcomes.
In a complex university teaching hospital such as UPMC-P, implementation of approved guidelines is an intricate multifaceted and multidisciplinary process. A combined approach of written, verbal, and electronic means for educating pharmacists, nurses, nurse practitioners, medical housestaff, faculty physicians, and private practice physicians is required. The essential steps are reviewed with the students, focusing on practitioner education, the pharmacist's role in intervention, educational material design, effective teaching methods, competency assessment, online learning methods, and financial impact evaluation. Implementation tools such as training fact sheets, clinical information systems order alerts, prospective monitoring reports, and/or preprinted physician order sets are designed by the students according to specific operational needs.
Patient Care
Patient monitoring is an important focus of the internship. Students are instructed regarding the confidential nature of patient data and are subsequently given access to clinical information systems to retrieve patient data and pharmacist clinical documentation, as well as financial data for initiative development and monitoring. They are also oriented to the layout of the patient medical record and instructed in retrieval of pertinent patient data required for decision-making and the eventual intervention process. Prospective and retrospective chart reviews are performed to familiarize students with patient information retrieval from the medical record. Group discussions facilitate learning about types of outcomes and the continuous quality improvement (CQI) techniques used to design project outcomes.
Instruction includes basic concepts of patient monitoring and the importance of following the appropriate parameters to evaluate drug therapy. Templates assist students with designing problem lists and performing medication histories. Patient drug-therapy monitoring forms aid students in evaluating individualized patient drug therapy regimens. As students learn the approved guidelines, they monitor and assess patient drug therapy and identify potential interventions in care. Students and pharmacist mentors role-play to plan approaches for discussing drug therapy interventions with physicians. Students perform interventions under supervision of the licensed pharmacist, but are encouraged to interact directly with the nurses and physicians as their comfort level and confidence increases. Students do not propose recommendations to change patient drug therapy without first discussing it with the pharmacist.
Students are expected to present one formal patient case study to the DUDSM team monthly during the summer portion of the internship, starting in the summer prior to their third-professional year (optional for summer prior to second-professional year). This prepares them for didactic case-based and experiential learning APPEs to reinforce the importance of individualized patient monitoring. Discussions following patient case presentations serve as a vehicle to enhance learning. Emphasis is placed on individualizing patient problem lists, creating care plans, and reviewing disease state topics to teach pharmacotherapeutic management strategies that are found in the literature.
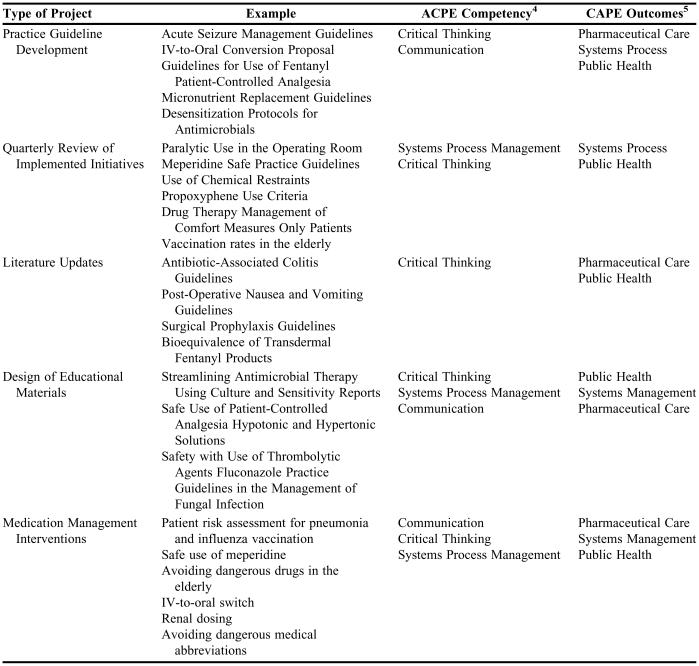
Student Projects and Activities
Examples of internship projects are provided in Table 3, along with the achieved ACPE competency and CAPE outcomes. Although guideline development and patient care activities are used as a vehicle for learning, these are not just educational exercises for the students. All guidelines developed by students are intended for implementation at UPMC, subsequent to the established approval process. Patient care assessments performed by students are part of the ongoing continuous quality improvement process that is used to evaluate implemented guidelines.
Table 3.
Examples of Completed DUDSM Student Intern Projects
ASSESSMENT
As students entered the internship program, their training was planned both in the area of structured core elements and individualized learning, as noted in Table 1. Progress on core elements was recorded in a competency checklist for each student. Training was accomplished through a combination of reading/reviewing documents, group instruction, and one-on-one case-based application. Competency was demonstrated via didactic examinations and/or direct observation by a preceptor.
Guideline development and implementation checklists were maintained and reviewed by DUDSM members to demonstrate student participation in the process from idea generation to implementation. Progress on guideline development was charted by longitudinal use of these tools as the guideline was designed, presented, and implemented. These documents clearly showed the comprehensive training that was afforded through long-range participation in the DUDSM program. Appendix 1 is an example of the tracking tools that were used. To evaluate student competency with medication management interventions, DUDSM patient monitoring forms were used to document gathered data and guide decision-making for drug therapy intervention. As students “worked up” patients for potential intervention, they presented their findings to their pharmacist mentor who reviewed the case and discussed it with the student. The pharmacist then signed the form to document completion. Intervention forms and patient assessment forms were available for each clinical guideline and were the tools used by the DUDSM team for documentation and training of new UPMC-P pharmacists, residents, clinical scientist associates, and students.
A case presentation evaluation form designed by School of Pharmacy clinical faculty members was used to evaluate student communication skills, case content, patient data gathering, and formulation of the medication management plan. With each formal case presentation, student interns were rated “needs improvement,” “acceptable,” or “excellent,” by the audience. The evaluations were then reviewed by the student and DUDSM Director to discuss performance and areas for improvement. For individual patient interventions, role-playing and shadowing were used to teach students how to present information regarding patient care to prescribers. This work was done by students during the summer after their first and second years of pharmacy school, which was much earlier than when they would typically receive specialized intensive training in this area.
Since students were hospital employees, the annual performance evaluation included a summary of their accomplishments and progression through core internship elements. The learning checklist was reviewed by the DUDSM Director at periodic intervals throughout each student's experience, specifically at the yearly evaluation point, before beginning full-time work in the summer, at the end of the summer, and at the start of each school term.
Aggregate Outcomes of Students
Twenty-four students have participated in the internship program since 1998. In the early years of the internship, students participated for an average of 18 months, which included the summer prior to their third-professional year and continued until clerkship rotations began in their fourth-professional year. Beginning with our most recent intern graduates (2005), participation started in the summer after their first-professional year, for a 3-year experience. Upon graduation, students were awarded a certificate recognizing their completion of the 3-year internship program. To date, all students beginning the internship have continued until graduation and have shown great satisfaction with the program in their written evaluations. Appendix 2 shows examples of student comments.
The average number of patient drug-therapy regimens evaluated by student interns exceeds 500 per student, with 200 active interventions performed per student over the course of the internship. To date students have designed a total of 16 clinical practice guidelines comprised of: 69% (11) patient safety; 19% (3) new drug reviews; and 12% (2) disease management topics. Students designed teaching materials for 14 different DUDSM guidelines, performed 13 quarterly assessments of implemented guidelines, and created 7 competency examinations for pharmacists, 5 of which are currently in use at UPMC-P.
Regarding the 19 students who completed the internship, 63% (12) went on to pursue a pharmacy practice and/or specialty residency, with 90%(17) now working in advanced practice sites in the institutional or community setting. Students presented 18 posters at national meetings of the American Society of Health-Systems Pharmacists (ASHP) on guidelines they created, compliance with existing guidelines, and/or their role in design of innovative programs at the UPMC. Most recently, the class of 2007 interns submitted a proposal to the AACP for consideration for the Department of Health and Human Services Secretary's Award for Student Health Promotion for their work with the inpatient standing orders program for vaccination of the elderly. The most recent intern class, consisting of 5 second-professional year students and 2 fourth-professional year students, completed 5 new initiative proposals, 6 teaching fact sheets, 10 aggregate initiative assessments, and presented 8 posters at the 2004 ASHP Midyear Clinical Meeting.
DISCUSSION
Pharmacy students grow both professionally and personally during their participation in the DUDSM internship program. This unique experience fosters self-directed learning, maturity, confidence, and collaboration with other health care professionals, as well as teaching the fundamentals of drug therapy monitoring and problem-solving. Appendix 2 displays student comments on the impact of the internship program. The program provides students with a unique set of clinical and communication skills that distinguish them from their peers. Through their participation, pharmacy students gain an appreciation for the changing dynamics of healthcare. In addition to developing fundamental clinical skills such as monitoring patient pharmacotherapy, they are given practical instruction in designing programs and managing projects. Students are also exposed to multidisciplinary health care teams and different approaches to professional interactions. This type of learning is not commonly available to doctor of pharmacy students. It is our experience that student interns appreciate and maximize this opportunity to learn in a patient care setting. They gain experience that extends beyond the usual pharmacy student intern positions, which are typically focused on drug distribution. Due to the broad scope of participation and the many parallels to a pharmacy practice residency, this 3-year program can be described as a longitudinal “mini-residency” program.
The DUDSM internship program was initiated with the intent of a 1-year timeframe; however, the positive response of participating students led to program expansion. Initially, only third-professional year students were recruited, but as students demonstrated interest during earlier years of the doctor of pharmacy program, the internship was tailored to include them. The internship opportunity now starts at the end of the first-professional year, increasing the extent of student experience to a total of 3 years. The work of the DUDSM program has been organized to create a progression of learned skills that complements student development. The benefit of the longitudinal progression for the students from the P1 to P4 year has been evident to DUDSM team members and to student interns themselves through written comments submitted postgraduation, and also through anecdotal comments from the students and other faculty members. The 3-year experience has also provided an opportunity for interns in later years to mentor interns in earlier years, thus creating a teaching role as well for the senior students. First-year student interns have demonstrated the capability of learning the background information and applying it to assigned projects. Pharmacy students are able to augment the learning experience by participating in more projects.
Through this internship, students are given the opportunity to build on their experience and knowledge base through progressive participation in more advanced projects. In addition, students gain satisfaction from directly applying what they learn and contributing to patient care. Students receive individualized mentoring similar to that received in a condensed fashion on a 1-month clerkship experience, with the added advantage that this relationship is fostered over 3 years of pharmacy school.
Benefits to Pharmacy Department
Selection of high achieving, self-motivated students is the key to the success of this program. First- year pharmacy students are recruited for the internship positions during their second semester. The program goals and objectives are intentionally rigorous and include a requirement to prepare and present a poster at a national meeting. This is intended to attract highly motivated students who are dedicated to their chosen field.
The hospital pharmacy department benefits from the participation of these highly capable pharmacy students through increased project completion. The high level of supervision and teaching provided by the DUDSM team is balanced by this departmental benefit of expanded productivity. Students contribute to the workload by providing new guideline proposals, outcome assessment tools, educational materials, quarterly initiative assessments, new literature reviews, formulary reviews, medical record reviews, and research proposals. In the first 4 years of the internship, unrestricted educational grant monies from the pharmaceutical industry funded the internship. The student contributions to the DUDSM program were so highly valued and integral to daily operations that the UPMC-P pharmacy administration provided funding for these positions as part of hospital pharmacy services over the last 3 years.
The success of this internship was instrumental in creating a similar hospital-pharmacist training program for UPMC in which pharmacy students are trained in a hospital-based, blended clinical distribution career track. This program became operational in 2004 as a joint effort of the DUDSM program and UPMC-P hospital pharmacy leadership. Students are now provided with new learning sites in drug information and investigational drug research as a result of this expansion of experiential learning opportunities
SUMMARY
This internship model of progressive experiential learning combined with structured learning provides a broad perspective for understanding the role of the pharmacist in improving patient care in a hospital setting. Students gain knowledge and practical experience through the process of designing, implementing, and assessing drug utilization guidelines from start to finish. The intern program is highly individualized, maximizing the learning opportunities for each student. Close supervision fosters development of a mentoring relationship that emphasizes both personal and professional growth.
ACKNOWLEGEMENTS
The contributions of Mary Hess, PharmD, to the concept and original design of the student internship are acknowledged. This project was presented as a poster on interdisciplinary models of practice at the American Society of Health Systems Pharmacists national meeting in New Orleans, La, in December 2003.
Appendix 1. UPMC Drug Use and Disease State Management Program Guideline Development and Implementation Strategy6
Steps in Guideline Proposal Development:
Progress Notes
-
Identify opportunity
High volume drug use or disease state occurrence
High cost of drug therapy or disease state
New pharmacologic entity with narrow therapeutic niche/limited clinical support
New consensus paper or other literature recommendations published
-
Write initiative proposal
Description of initiative (recommendations on front of document in text box)
Background literature support
Primary literature
Consensus papers
Pharmacoeconomic studies
Society/organization recommendations (UHC, AHCPR, ACCP, ASHP)
-
Review other similar institution practices
Review from pharmacy journals
Phone/web-based survey
Check with industry representatives
-
Assess current UPMC experience
Manual drug usage evaluation
Computer informatics report
Chart review/prevalence study
-
Determine current UPMC costs/usage of drug or disease state
Purchasing information
Archived computer usage data
Approximate projected annual savings
Cost analysis of new therapy versus current therapy
Quantify other costs such as reduced length of stay, avoidance of adverse drug events
Include references
-
Obtain multidisciplinary approval
Address major stakeholders - physicians, specialists, etc.
Identify physician champion
Presentation to committees (P&T, Formulary and Health System P&T Committee)
-
Design implementation plan
Develop strategy (DUDSM, order entry for enforcement, or both)
Automatic interchange or traditional intervention
Determine frequency of monitoring (focused initiative vs. unit-based analysis)
-
Monitor outcomes
Clinical (patient care impact → depends on individual initiative; ex. Reduction in HgA1c level, reduced bleeding episodes, reduced adverse events)
Economic (ex. dollars saved/doses changed)
Process (ex. % compliance: threshold ≥85%)
Appendix 2. Examples of student comments regarding internship
“Working in DUDSM has been one of the most valuable learning experiences I have had during my years as a pharmacy student. I feel very luck to have the opportunity…I have gained far more practical knowledge in a short time while in this position that in my past internship experiences and even much of my coursework in Pharmacy School… “
“ The DUDSM internship has been one of the best educational experiences of my life. It has afforded me the opportunity to learn about clinical pharmacy, professional communications, institutional operations, and drug information research. …. One of the most exciting activities I took part in was monitoring patient therapy… I now feel comfortable in searching for any necessary patient information and making changes in drug selection, routes of drug administration, and in drug dosage…Most importantly, working in the DUDSM office helped me to further develop independence, motivation, and confidence. I accepted a project or assignment, and conducted research to complete the requirements. Doing this further motivated me to learn more about pharmacy…I have developed a broader knowledge base, as well as more confidence in myself.”
“I appreciate the importance of communication, not only within pharmacists, but also with other health care professionals and patients. A good relationship between co-workers with the patients will make the work environment comfortable and bring the maximum effectiveness of our work… I have learned how to work independently and become efficient with on-going initiatives on a daily and monthly basis, and also provide the appropriate clinical summary and action plan for the patient.”
“Three main growth areas for me have been knowledge, clinical judgment, and communication skills. Working in DUDSM gives me another chance to review concepts taught in pharmacy school in a very practical way with hands-on experience…I went from a shy and shaky speaker to a more confident and assertive one. I used to feel frightened when I knew I had to give a presentation. Now, I want to do more…Working side-by-side by with the clinical pharmacists, I was given the opportunity to monitor the patients on a daily basis. This was challenging, but interesting. Day by day, I have developed my own clinical judgment toward situations such as drug interactions, drugs of choice, cost-effectiveness, adverse effects, etc. DUDSM has given a golden opportunity to take my pharmacy education to another level, professionalism….
“The exposure to the DUDSM approach to improving and optimizing patient care in the health-system setting is invaluable…Having the opportunity to see this type of practice as a pharmacy student has definitely helped direct my professional goals. On a personal level, I am grateful for the way the interns are welcomed into the program…Until DUDSM, I never had the feeling of being an equal or the sense of being a true professional…Throughout my orientation, there was never a glimmer of an inference that an intern was not capable, could not be counted on or trusted to do good work. I was given the freedom to tackle my projects without constant monitoring, but when I needed direction it was readily and happily available. It was truly the perfect combination of instruction, personal growth, self-direction, camaraderie, and professionalism…Every one of them (DUDSM staff) is a working model of professionalism, setting examples in the way they live and work…As you may know by now, I recommend this internship to every pharmacy student I know. I am a better person for the experience.”
REFERENCES
- 1.Drab S, Lamsam G, Connor S, DeYoung M, Steinmetz K, Herbert M. Incorporation of service-learning across four years of the PharmD curriculum. Am J Pharm Educ. 2004;68 Article 44. [Google Scholar]
- 2.Caspi A, Rozenfeld V, Kleyman J. Prevention of medication errors in the hospital setting: the role of pharmacy students. Pharmacol Ther. 2005;30:183–6. [Google Scholar]
- 3.Slaughter RL, Erickson SR, Thompson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28:665–70. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 4. Accreditation Standards. Accreditation Council for Pharmacy Education. Available at http://www.acpe-accredit.org/deans/standards.asp. Accessed May 10, 2005.
- 5. CAPE Educational Outcomes. American Association of Colleges of Pharmacy. Center for Advancement of Pharmaceutical Education. http://www.aacp.org/site/page.asp?TRACKID=&VID=1&CID=1031&DID=6074. Accessed May 10, 2005.
- 6.Skledar SJ, Hess MM. Implementation of a drug-use and disease-state management program. Am J Health-Syst Pharm. 2000;57:S23–9. doi: 10.1093/ajhp/57.suppl_4.S23. [DOI] [PubMed] [Google Scholar]
- 7.Skledar SJ, Hess MM, Ervin KE, et al. Designing a hospital-based pneumococcal vaccination program. Am J Health-Syst Pharm. 2003;60:1471–6. doi: 10.1093/ajhp/60.14.1471. [DOI] [PubMed] [Google Scholar]
- 8.Skledar SJ, Gross PR. Using a CQI process to change surgical antimicrobial prophylaxis practices. Formulary. 2000;35:53–64. [Google Scholar]
- 9.Tortorici M, Skledar SJ, Barnes B, Wasko MC. Promoting the safe use of intravenous colchicine. Am J Health-Syst Pharm. 2004;61:1496–2501. doi: 10.1093/ajhp/61.23.2496. [DOI] [PubMed] [Google Scholar]
- 10.Sheth H, Verrico MM, Skledar SJ, Towers AL. Promethazine adverse events after implementation of medication shortage interchange. Ann Pharmacother. 2005;39:255–61. doi: 10.1345/aph.1E361. [DOI] [PubMed] [Google Scholar]
- 11.Skledar SJ, Culley CM. Collaboratively designed practice guidelines promote appropriate use of intravenous proton pump inhibitors. Hosp Pharm. 2005;40:497–504. [Google Scholar]