Abstract
Objectives
To assess a community geriatrics advanced pharmacy practice experience (APPE) that aimed to improve students' attitudes towards older adults and provide a student-directed learning experience.
Design
Students provided blood pressure monitoring and medication counseling to older adults living in a low-income residential facility as part of a required 6-week ambulatory care service-learning APPE. Pre-experience and post-experience essays on students' perceptions of the elderly and their intended and actual learning were retrospectively reviewed using a qualitative process to determine whether the course objectives were met.
Assessment
Many students initially described older adults in factual terms or using negative descriptors. Most expressed a desire to increase their knowledge of diseases commonly occurring in and drugs commonly prescribed for the elderly or to improve specific skills. Many students initially had difficulty articulating clear and measurable learning objectives and appropriate assessment metrics, which are important components of self-directed learning. The final essays revealed many students learned more about the humanistic aspects of care than they had anticipated.
Conclusion
This community-based geriatrics experience improved students' attitudes towards working with older adults and provided practice in developing and assessing their personal learning objectives.
Keywords: student-directed learning, community pharmacy geriatrics, advanced pharmacy practice experience, service learning
INTRODUCTION
Students graduating from colleges and schools of pharmacy today will serve a rapidly growing elderly population over the course of their careers. Currently, 1 in 8 Americans (over 35 million people) is 65 years of age or older. With the aging of baby boomers, the number of older Americans is expected to double to 71.5 million people by 2030. Thus, 20% of the US population will be 65 years of age or older within the next quarter of a century.1
The ability to provide patient-centered care is a key educational outcome for pharmacy students.2 It requires developing trust and a caring relationship with the patient. Having empathy, which is the ability to understand a patient's situation and concerns without passing judgment, is part of developing an effective therapeutic alliance.3 Negative stereotypes or unfavorable attitudes towards the elderly could potentially interfere with developing an empathetic and caring relationship with an older adult. Pharmacy students may have negative views of older adults as a result of the generation gap or the prevalent ageism in our society.4 In addition, previous course work may have overemphasized the frail elderly; however, that group is not representative of all older adults. Pharmacy students may also have formed opinions about the elderly population as a result of their previous exposure to older adults in the health care system.
Smith et al framed the challenge of preparing today's pharmacy graduates to care for an aging population, which is known to have a disproportionate share of chronic medical conditions, medication use, and potential for drug-related problems.5 She and her colleagues described a community-based geriatric advanced pharmacy practice experience (APPE) based upon the pedagogy of service-learning. Student learning was assessed using both qualitative and quantitative measures, including students' written reflections. Students gained a greater awareness of the health practices, beliefs, and challenges facing older adults and a better understanding of how pharmacists can play a role in improving health outcomes in older adults, demonstrating the effectiveness of this service-learning model.
Service-learning as a pedagogy suitable for pharmacy education was described by Nickman in 1998.6 She noted that experiential education focused more on the development of clinical skills than caring skills and recognized a need to foster the humanistic aspects of practice. When revising a course on the social and behavioral aspects of health care, she introduced a service-learning component that provided opportunity for students to visit homebound elderly clients of 3 not-for-profit agencies. Others have since reported incorporating service-learning into the pharmacy curriculum, although there has been significant variability among colleges and schools in the types of service-learning experiences provided and its placement in the curriculum.5,7-15 Few, however, have reported using this pedagogy at the advanced practice experience level.5,15
Life-long learning, a foundation for maintaining professional competence, is another essential competency in pharmacy.2 It requires that practitioners be self-directed in assessing, pursuing, and evaluating accomplishment of their learning needs. To address this, pharmacy educators have introduced more active, participatory teaching-learning processes into their curricula. However, most APPEs remain faculty- or preceptor-centered. Generally, it is the faculty member who determines the goals, learning objectives, and specific learning activities for a given practice experience. Students may have input to varying degrees; but typically, it is the preceptor who determines what the student will learn and do “in my rotation.” Correspondingly, preceptors generally evaluate student performance based upon pre-determined performance criteria developed by the faculty members.
This community-based geriatrics APPE was developed to meet 2 perceived needs: to improve student attitudes towards older adults and to foster self-directed learning. A service-learning model was utilized to provide students with an opportunity to interact and develop relationships with community-dwelling elders outside of the established health care system. Few existing APPEs provided such an opportunity to learn about how an older person's lifestyle, living environment, and psychosocial support system impact health and well being. By exposing students to older adults in their living environment, it was thought that students would gain a better understanding of the health-related issues that seniors face in everyday life. To engage students in their own learning, they were asked to develop their own learning objectives and assessment metrics for the APPE and participate in evaluating the learning that subsequently occurred.
DESIGN
The University of California, Davis (UCD) Program, 1 of 5 regional experiential programs of the University of California at San Francisco (UCSF) School of Pharmacy, accepts up to 16 students for an entire calendar year. Students assigned to the program complete eight 6-week APPEs in the metropolitan Sacramento area. This includes 2 acute care, 2 ambulatory care, 1 community practice, and 3 elective APPEs. Since 1997-1998, all students in the UCD-Sacramento program were assigned to a half-time community geriatrics experience as part of 1 of the required ambulatory care APPEs.
The School of Pharmacy secured a formal affiliation agreement with Greenfair Retirement Apartments prior to assigning any students to the site. To reside at the facility, seniors must be eligible for social security, have limited income, and be able to live independently with minimal assistance. Greenfair Apartments is not licensed as an assisted living or skilled nursing facility.
A pilot elective experience was conducted at the site prior to the 1997-1998 academic year. Students provided a “Medicine Check Up” service at a set time and place each week. However, few residents took advantage of the program and student participation was intermittent. This led to incorporating a blood pressure monitoring component, which was intended to attract more residents and provide opportunity for discussions about medications. This proved successful and led to the current design.
Instructional Design
Students, working in pairs or triads, provided medication counseling, blood pressure monitoring, and home visits to Greenfair residents 2 days per week. The blood pressure clinics were held at regularly scheduled times each week in common areas. Residents attended on a drop-in basis. While on site, the students were supervised by the facility's social services coordinator. The social services coordinator also worked with students to identify 2-3 residents per week who might benefit from students visiting them in their apartments (home visits).
The student team met with a pharmacist preceptor offsite one half day per week. During these conferences, students discussed their resident encounters and home visits. Time was set aside to reflect on the students' activities and learning and to discuss current events that were generally related to older adults and health care. A separate orientation was scheduled at the beginning of each 6-week rotation to discuss mutual expectations, the self-directed nature of the experience, and potential situations that could arise and how these should be handled. The use of blood pressure equipment and proper technique for measuring blood pressure were also reviewed during the orientation.
Students were asked to complete an essay describing their “perceptions of the elderly and their pharmaceutical care needs” and bring this to the orientation. They were also asked to write 3-5 personal learning objectives for the experience and describe how they would assess accomplishment of these. The learning objectives and assessment metrics were discussed during the conference and revised as necessary so that they would be clear and measurable. Students maintained a portfolio that included the initial essay, their learning objectives and assessment plan, weekly reflective essays describing their experiences and what they had learned, and a final essay revisiting their initial perceptions and personal learning objectives. Other than general guidelines about the length of the initial, reflective, and final essays, there was no specific format required, nor was a definition of older adults provided. Upon completion of the rotation, the portfolios, which became the basis for the final grade (pass/no pass), were turned in and discussed. A debriefing session was held during the last scheduled conference.
Instructional Effectiveness
Pre-experience and post-experience essays from the student portfolios were reviewed retrospectively using a qualitative process to determine students' initial attitudes towards the elderly and if these had changed as a result of the experience. The study also sought to capture the students' intended and actual learning in their own words. For the purposes of this analysis, the written learning objectives and assessment metrics that were submitted prior to any revisions were used.
Essays were coded for student name, gender, and year. A photocopy with students' names and the dates of the rotation removed was used as the working document. A dozen essays were selected randomly for initial review to generate the categories of themes to track. All essays were then read and coded for the predominate themes contained, which were noted in a database. Themes were then tabulated to determine frequency of mention of each. The UCSF institutional review board reviewed and exempted this study.
ASSESSMENT
Since 1997-1998, 117 students have completed the Greenfair APPE. From this group, 10 portfolios were either lost or missing 1 of the essays. Of the 107 complete portfolios, 86 (80%) were submitted by female students and 21 (20%) were submitted by male students, which corresponds to the gender ratio of all students matriculating through the UCD-Sacramento program during this 8-year period.
Preconceived Notions
About one third (35%) of the initial essays provided a factual description of older adults, without any judgment labels. These essays described older adults in terms of their health characteristics only, such as the number or name of chronic diseases that they had, whether they took multiple medications, or what physiologic changes were associated with aging in this population. Another 20% used primarily negative descriptors such as sad, lonely, difficult, slow, angry, bitter, forgetful, isolated, and a burden to others to describe older adults. A similar percentage (19%) did not stereotype this population, indicating that older adults fell across a broad spectrum in terms of personality and/or socioeconomic status. Another 11% viewed older adults as belonging to 1 of 2 distinct, generally opposing groups, based upon either extremes of health or socioeconomic status. Some compared their own family members (positive descriptors) to patients they had previously encountered (negative descriptors). Only 7% described older adults using mostly positive descriptors, such as pleasant, friendly, sociable, and having many interesting stories to tell. The remaining students did not answer the question or only described 1 person, such as a family member or neighbor.
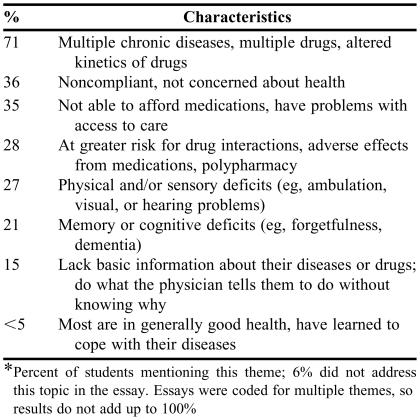
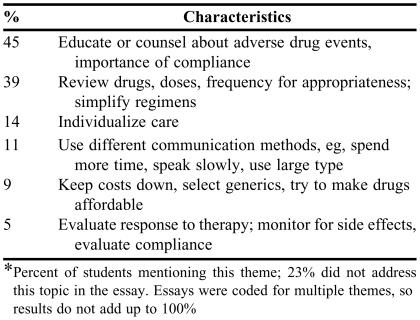
The initial essays were categorized further according to perceptions of the health status of older adults (Table 1) and perceptions of their pharmaceutical care needs (Table 2). The majority of students described the health status of older adults in terms of multiple diseases or chronic conditions, multiple drugs, and/or physiologic changes that would lead to altered pharmacokinetics of drugs. Over one third of the students characterized the elderly as noncompliant or not concerned about their health, while a similar percentage thought affordability of and access to care was problematic for this population. The perceived pharmaceutical care needs of the elderly generally corresponded to perceived health status. Few students described older adults as generally in good health and able to enjoy life.
Table 1.
Perceived Health Status of Older Adults: Themes From Essays Written Prior to Starting the APPE*
Percent of students mentioning this theme; 6% did not address this topic in the essay. Essays were coded for multiple themes, so results do not add up to 100%
Table 2.
Perceived Pharmaceutical Care Needs of Older Adults: Themes from Essays Written Prior to Starting the APPE*
Percent of students mentioning this theme; 23% did not address this topic in the essay. Essays were coded for multiple themes, so results do not add up to 100%
Intended Learning
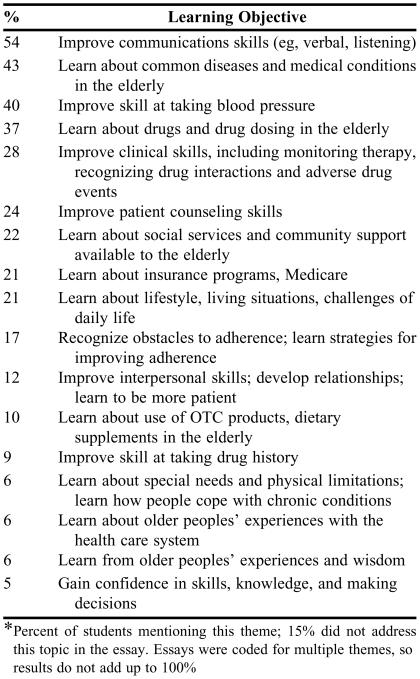
Ninety-one students (85%) wrote explicit personal learning objectives as instructed, with most listing 2-3 objectives (range 1-12). The remainder either listed personal goals for the experience, such as providing a service (eg, developing a handout or teaching a class on nonprescription drugs), or did not indicate what they intended to learn. Of those who listed their intended learning objectives, the most frequently mentioned items were improving communication skills, learning about common diseases in the elderly, becoming more proficient at taking blood pressures, learning about the drugs commonly used and proper dosing in this population, and improving clinical skills such as recognizing drug interactions or monitoring for drug-related problems. The learning objectives that were most frequently mentioned are listed in Table 3.
Table 3.
Students' Intended Learning: Themes from Essays Written Prior to Starting the APPE*
Percent of students mentioning this theme; 15% did not address this topic in the essay. Essays were coded for multiple themes, so results do not add up to 100%
Developing metrics for assessing personal learning objectives was more difficult. Most students submitted initial objectives that were unclear or not measurable and therefore had difficulty with developing appropriate assessment metrics. For example, many students indicated that they wanted to increase their knowledge base, using terms such as “to better understand” or “to learn about” something, but they were unable to postulate how they would measure whether they had done that. Similarly, many indicated a desire “to become more proficient at” or “increase confidence in” performing some type of skill, but could not articulate how they would measure improvement. This necessitated discussion during the initial conference to clarify and subsequently revise the learning objectives and assessment plan if necessary.
Actual Learning
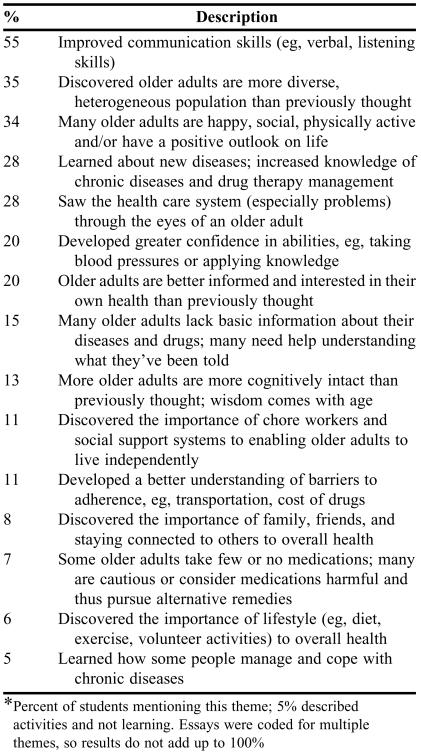
Ninety-five percent of the final essays described what the student learned as a result of the experience. The remainder described the students' activities while in the rotation, but not what they had learned. As they had intended, most students said they improved their communication skills, learned new disease states, increased their knowledge of common chronic diseases and associated drug therapy, and developed greater confidence in their abilities (Table 4). However, many students also spontaneously reported unintended learning, including discovering a more diverse and heterogeneous population than they had expected to encounter and that many older adults were physically active, happy, sociable, cognitively intact, and engaged in life. Some students were also surprised to learn that many older adults were more informed and interested in their health than they had anticipated.
Table 4.
Pharmacy Students' Assessment of What They Learned: Themes from Essays Written After Completing the APPE*
Percent of students mentioning this theme; 5% described activities and not learning. Essays were coded for multiple themes, so results do not add up to 100%
Half of the students spontaneously wrote that this rotation had resulted in developing more positive attitudes towards older adults and half of the students stated that it was a good or rewarding learning experience. In many of these essays, the student disclosed that he/she had previously concealed negative perceptions of the elderly in the initial essay and had now found these to be incorrect stereotypes. Over one third of the students said the experience validated previous perceptions, whether those were positive or negative. Some mentioned that as the result of this experience, they had a more positive attitude towards their own aging. Two students indicated that the Greenfair experience left them with a more negative view of older adults than they held prior to the experience.
DISCUSSION
Although some pharmacy students were careful not to disclose initial stereotypes, many of them were initially hesitant about working with older adults. Of those who revealed their initial attitudes, students were 3 times more likely to use mostly negative rather than positive descriptors to characterize older adults. In the final essay, without prompting from the instructor, half of the students wrote that this service-learning experience had improved their attitudes towards the elderly. Several of the themes from the students' final essays describing the learning that had transpired also refuted negative attitudes or stereotypes (eg, more older adults are cognitively intact than previously thought).
In a study involving college students, Ragan and Bowen found that subjects generally had negative attitudes towards the elderly at baseline.4 Providing accurate information about older adults resulted immediately in improved attitudes, which were sustained when reinforced. Many pharmacy students revealed unfavorable attitudes towards the elderly prior to the Greenfair experience, which improved as a result of the ongoing interactions with the residents. The weekly conferences provided opportunity for students to share their experiences, attitudes, and concerns resulting from the senior encounters and for the preceptor to reinforce the positive aspects of aging and point out the favorable attributes that some of the residents displayed. This preceptor reinforcement may have also influenced the change in student attitudes.
Key elements of service-learning, such as reciprocity and reflection, were incorporated into this experience.16 A single low-income retirement complex served as the community partner rather than a community service agency, although the intent to foster civic responsibility and address unmet needs of the community partner were present.5-11,13-16
Assessment of service-learning experiences, including evidence of student learning, have previously been based on structured pre-experience and post-experience assessments, including Likert-type surveys addressing student satisfaction or changes in attitudes, and to a lesser degree, notations in students' written reflections.5-11,14,15 This assessment differed in that it was based on systematic determination of what students said they intended to learn and what they said they actually learned in a self-directed experience, as described in their initial and final essays.
In addition to the residential setting and self-directed nature of this experience, this community geriatrics experience differed from traditional APPEs in other ways. The pharmacist preceptor did not directly supervise the activities of the students. Student teams worked independently, although the facility's social services coordinator provided oversight. Profiles were maintained on the residents who interacted with students, but the information obtained came from the residents and may or may not have been correct. Students had no access to the residents' medical records, although they were occasionally asked by a resident to interpret medical orders or laboratory data. Lastly, the students' role was slanted toward being a patient advocate and health educator than a provider of traditional pharmacy services. Students varied in their comfort level with these differences.
The preceptor observed that many students were initially uncomfortable with the less-structured learning environment and the self-directed nature of the experience, although most commented later that they were able to adapt to this. At the debriefing sessions, some students indicated they would have preferred a checklist of topics to discuss in the weekly conferences. A few said that having to identify and explore learning issues related to their resident encounters each week resulted in haphazard and unpredictable learning. Some also expressed frustration with the lack of medical data that were available to them, preferring to work instead in a data-rich environment such as an acute care setting. These same students tended to express dissatisfaction with the experience, because they could not intervene and adjust drug therapy as they had done in some of their other APPEs.
The majority of students initially had difficulty articulating personal learning objectives that were clear and measurable. Writing clear, concise, and measurable learning objectives is a skill that takes practice. Students may have had limited opportunities to practice this skill in other didactic courses or APPEs. Similarly, a few students could not differentiate learning from the activities that they performed, which may have resulted from limited experience with reflecting on educational activities and linking them to subsequent learning. These observations have implications for the future professional development of pharmacy graduates. To maintain professional competence, practitioners must be able to self-assess and identify their learning needs, develop and implement a plan, evaluate its effectiveness, and redirect their efforts as necessary.17 Many believe the current continuing education system is inadequate for assuring competence of licensed practitioners and advocate incorporating a quality improvement process such as continuing professional development (CPD), although practical and logistical concerns with the latter have been noted.17 Nevertheless, pharmacy educators should be preparing students to be independent self-directed learners at all levels of the curriculum. Self-directed APPE models, such as the one described, complement traditional practice experiences and should be encouraged.
There are several limitations to this study. The qualitative analysis was subjective and involved abstracting and tabulating themes from the students' pre-experience and post-experience essays. The essays were read and coded by 1 person, who may have misinterpreted what was written or intended. Since the notebooks used in the study were collected over a 7-year period, students in later years may have heard about the experience from previous students and written what they thought the preceptor wanted to hear. Other validated metrics are available for assessing student attitudes towards older adults, but these would not have captured the students' intended learning and thus were not used.4,18
CONCLUSION
This community-based geriatrics experience improved students' attitudes towards working with older adults and provided practice in developing and assessing one's own learning objectives. Although most students intended to learn about common drugs and diseases in the elderly or to improve their communications and blood pressure-taking skills, the unintended learning will also be valuable to their future pharmacy practices.
ACKNOWLEGEMENTS
The author wishes to thank Judith C. Barker, PhD, for her assistance with the study design. In addition, the author thanks Myrna D'Angelo, Social Services Coordinator; Mindy Hicks, Administrator; and the staff and residents of Greenfair Retirement Apartments for their participation in and support of this project.
REFERENCES
- 1. A profile of older Americans: 2004. Administration on Aging. U.S. Department of Health and Human Services. Available at: http://www.aarp.org/research/reference/statistics/aresearch-import-519.html. Accessed August 25, 2005.
- 2. Educational Outcomes. CAPE Advisory Panel, AACP, 2004. Available at: http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE204.pdf. Accessed August 25, 2005.
- 3.Berger BA. Listening and empathetic responding. In: Berger BA, editor. Communication Skills for Pharmacists: Building Relationships, Improving Patient Care. Second Edition. Washington, DC: American Pharmacists Association Publishers; 2005; 2005. pp. 49–58. [Google Scholar]
- 4.Ragan AM, Bowen AM. Improving attitudes regarding the elderly population: The effects of information and reinforcement for change. Gerontologist. 2001;41:511–5. doi: 10.1093/geront/41.4.511. [DOI] [PubMed] [Google Scholar]
- 5.Smith MAM, Koronowski MJ, Peterson NJ. Enhancing student learning through integrating community-based geriatric educational outreach into ambulatory care advanced practice experiential training. Am J Pharm Educ. 2004;68 Article 20. [Google Scholar]
- 6.Nickman NA. (Re-)learning to care: use of service-learning as an early professionalization experience. Am J Pharm Educ. 1998;62:380–7. [Google Scholar]
- 7.Lamsam GD. Development of a service-learning program. Am J Pharm Educ. 1999;63:41–5. [Google Scholar]
- 8.Piper B, De Young M, Lamsam GD. Student perceptions of a service-learning experience. Am J Pharm Educ. 2000;64:159–65. [Google Scholar]
- 9.Barner JC. First year pharmacy students' perceptions of a service-learning experience. Am J Pharm Educ. 2000;64:266–71. [Google Scholar]
- 10.Nichols-English GJ, White CA, Brooks PJ. Bridging community-based pharmacy outreach with service-learning principles. Am J Pharm Educ. 2002;66:124–31. [Google Scholar]
- 11.Carter JT, Cochran GA. Service-learning projects in a public health pharmacy course. Am J Pharm Educ. 2002;66:312–8. [Google Scholar]
- 12.Peters SJ, MacKinnon GE., III Introductory practice and service learning experiences in US pharmacy curricula. Am J Pharm Educ. 2004;68 Article SL2. [Google Scholar]
- 13.Nemire RE, Margulis L, Frenzel-Shepard E. Prescription for a healthy service-learning course: A focus on the partnership. Am J Pharm Educ. 2004;68 Article SL3. [Google Scholar]
- 14.Kearney KR. Students' self assessment of learning through service-learning. Am J Pharm Educ. 2004;68 Article SL4. [Google Scholar]
- 15.Kirwin JL, Van Amburgh JA, Napoli KM. Service-learning at a camp for children with asthma as part of an advanced pharmacy practice experience. Am J Pharm Educ. 2005;69 Article 49. [Google Scholar]
- 16.Jacoby B, Jacoby B, Jacoby B and, Associates . Service Learning in Higher Education: Concepts and Practices. San Francisco, Calif: Jossey-Bass Publishers; 1996; 1996. Service-learning in today's higher education; p. 5. [Google Scholar]
- 17.Janke KK. Continuing professional development: Staying focused on the goal. Am J Pharm Educ. 2003;67 Article 50. [Google Scholar]
- 18.Reuben DB, Lee M, Davis JW, Jr, Aslami MS, Osterweil DG, Melchiore S, Weintraub NT. Development and validation of a geriatrics attitudes scale for primary care residents. J Am Geriatric Soc. 1998;46:1425–30. doi: 10.1111/j.1532-5415.1998.tb06012.x. [DOI] [PubMed] [Google Scholar]