Abstract
Objectives
To compare the attitudes of third-year pharmacy students and pharmacy graduates towards people with schizophrenia and severe depression.
Methods
Third-year pharmacy students (n = 216) and pharmacy graduates (n = 232) completed a survey instrument with 21 common items. The third-year students had not yet received any mental health lectures or tutorials as part of their pharmacy course. The graduates had completed their university education, including mental health lectures and tutorials, plus 6 months of supervised clinical practice in the pharmacy workplace.
Results
There were no significant differences between the third-year students and pharmacy graduates in terms of social distance from people with schizophrenia. The rates of stigmatization of people with schizophrenia and severe depression were also similar between the groups.
Conclusions
Mental health lectures and tutorials delivered by pharmacists and supervised clinical practice in the pharmacy workplace may not decrease students' social distance or stigmatization of people with mental illness. The results of our study suggest that more comprehensive education and training programs are needed to improve the ability of pharmacists to meet the needs of people with mental illness.
Keywords: schizophrenia, depression, mental illness
INTRODUCTION
Services provided by pharmacists are potentially well suited to optimize the use of medications for mental illness.1 Provision of information about psychotropic medications by pharmacists, however, may be limited by poor communication with and suboptimal attitudes towards people with mental illnesses. Canadian community pharmacists have reported being less comfortable providing pharmaceutical services to people with mental illnesses than to those with cardiovascular conditions,2 and Finnish pharmacists were less likely to provide directions for use of psychotropic medications than for 8 other medication classes studied.3 The attitudes of health professionals in Australia have been cited as a barrier to the reform of mental health care delivery.4 Health professionals may also contribute to the stigma experienced by people with a mental illness.5,6 The fear of stigmatization among people with mental illnesses may be linked to their reluctance to seek help when symptoms first appear. Up to two thirds of people with mental illnesses in the United States do not seek treatment.7 In Australia general medical practitioners conducted more than 10.4 million mental health-related consultations in 2003-2004; however, fewer than 40% of people with mental illnesses received care specific to their condition.8
The concordant approach to medication counseling is based on the formation of a therapeutic alliance between pharmacist and patient.9 Understanding peoples' experiences of their illness is an important aspect of providing concordant medication counseling. The beliefs among health professionals that people with mental illnesses are hard to talk with, have different feelings, and are unpredictable are thought to contribute to social distance.10 Social distance has been defined as the relative willingness to associate with or enter into relationships of varying degrees of intimacy with a person.11 A large social distance between health professionals and people with mental illnesses may mean that health professionals do not understand peoples' experiences with mental illness.10 Measurements of social distance have been used as a surrogate for behavior associated with discrimination.12,13 Instruments that assess social distance have also been used to evaluate education and clinical placement programs for health professionals.14,15
Clinical practice experience in the pharmacy workplace has become a core component of pharmacy education in many countries. Given the volume of prescriptions dispensed for psychotropic medications, graduates undertaking supervised clinical practice in a community pharmacy interact with people with mental illnesses on a daily basis. Promoting contact with people with mental illness may be a useful strategy to decrease stigma and improve attitudes.16 Of 3 educational strategies studied to improve attitudes among community college students in the United States, providing contact with people with mental illnesses was found to be the most effective.17 Familiarity with mental illness is associated with more positive attitudes toward people with mental illness.18
Several studies have reported the attitudes of pharmacists and pharmacy students towards people with mental illnesses,2,19–21 yet few studies have assessed the impacts of mental health education programs for pharmacy students. The aim of this study was to compare third-year pharmacy students' and pharmacy graduates' social distance and stigmatization of people with schizophrenia and severe depression.
METHODS
A survey instrument was developed that included the 7-item Social Distance Scale (SDS) and 14 items related to stigmatization of people with severe depression and schizophrenia. The SDS is a widely used scale for which the reliability and validity has previously been established.13,18,22,23 The SDS requires respondents to indicate their willingness to associate with a person previously hospitalized with schizophrenia on 4-point Likert scales, ranging from “definitely willing” (1) to “definitely unwilling” (4). The 14 items related to mental health stigma were scored on 5-point Likert scales, ranging from “strongly agree” (1) to “strongly disagree” (5). These items were derived from 2 earlier surveys of the British general public10 and British medical students and medical practitioners working in a London hospital.24 Demographic information collected from each of the respondents included age, gender, country of birth, personal experience of mental illness, and whether respondents had visited a psychiatric facility.
The survey instrument was administered to all pharmacy graduates attending a seminar (not mental health related) held in Sydney. The seminar was a compulsory event for all preregistration pharmacy graduates in the state of New South Wales (NSW). In Australia, pharmacy students graduate after completing a 4-year degree course and then undertake 12 months supervised clinical practice before being eligible to complete the state board examinations for registration as a pharmacist. Prior to attending the seminar, each graduate had completed approximately 6 out of the required 12 months of supervised clinical practice. During these 6 months the pharmacy graduates were required to undertake supervised work as a pharmacist in either a hospital or community pharmacy. This work included dispensing prescriptions and providing medication counseling to people with mental illnesses. The majority of graduates seeking registration in NSW undertook their degree course in pharmacy at the University of Sydney, where they attended a series of 7 lectures on common mental illnesses, and received 1 mental health tutorial delivered by a pharmacist tutor. Graduates seeking registration in NSW who did not attend the University of Sydney completed a degree course in pharmacy either elsewhere in Australia or internationally that was deemed equivalent by the New Zealand and Australian Pharmacy Schools Accreditation Committee (NAPSAC) or the Australian Pharmacy Examining Council (APEC).
A survey instrument that included the SDS and 14 items related to stigmatization of people with severe depression and schizophrenia was also administered to all third-year pharmacy students at the University of Sydney. The pharmacy students completed the instrument prior to their attendance at the series of mental health lectures and the mental health tutorial. The third-year pharmacy students had not received any specific training in mental health care offered by the Faculty of Pharmacy, either practical or theoretical, prior to completing the instrument.
The study was approved by the Northern Sydney Health Human Research Ethics Committee, and permission to survey the pharmacy graduates was granted by the Postgraduate Training Course Committee (body responsible for organizing the graduates' seminar). All respondents completed the instrument anonymously. Completion of the survey instrument was voluntary, and graduates and students had the option not to answer specific questions. Data were coded and entered in the Statistical Package for Social Sciences (Version 11.5). Descriptive statistics were computed. Differences in demographic characteristics between the 2 groups were compared using chi-square tests. Independent t tests were used to compare survey responses of the third-year students and pharmacy graduates.
RESULTS
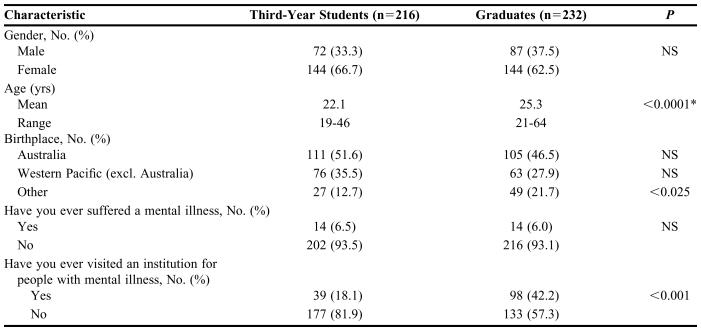
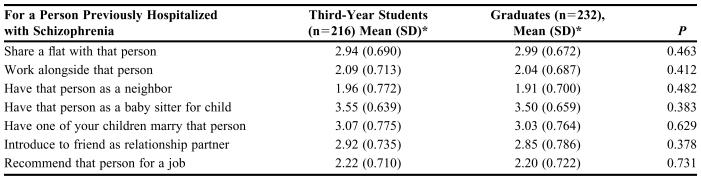
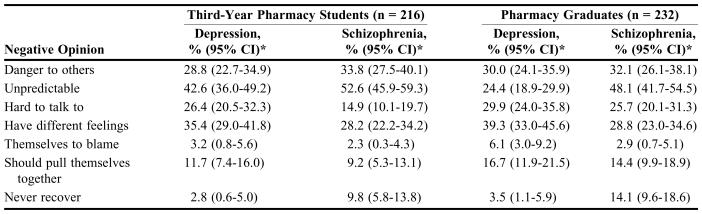
A completed survey instrument was returned by 232 out of 270 pharmacy graduates (86% response rate) and 216 out of 229 third-year pharmacy students (94% response rate). The demographic characteristics of respondents are outlined in Table 1. Pharmacy graduates were older and significantly more likely to have visited a psychiatric facility than the third-year pharmacy students. The SDS scores for the graduates and pharmacy students are outlined in Table 2. There were no significant differences in social distance between graduates and pharmacy students for any of the 7 social distance items. The internal consistency of the SDS, measured using Cronbach's alpha, was 0.86. The proportions of students and graduates holding negative views (who either agreed or strongly agreed) about each of the 7 aspects of stigmatization items are outlined in Table 3.
Table 1.
Demographic Characteristics of Respondents to a Survey on Attitudes Towards People With Mental Illness
*The mean age of third-year pharmacy students and pharmacy graduates was compared using an independent t test
NS = not significant
Table 2.
Responses to a Social Distance Scale Assessing Pharmacy Students' and Graduates' Attitudes Towards A Person With Schizophrenia
*Lower scores are indicative of less social distance. Items were scored on a 4-point Likert scale on which 1 = definitely willing and 4 = definitely unwilling
DISCUSSION
The pattern of responses on the SDS among third-year pharmacy students and pharmacy graduates was similar. It appears that workplace contact with people with mental illness, and university-based mental health education, were not associated with changes in social distance. Although promoting contact with people with mental illness has been demonstrated to reduce stigma and improve attitudes,16 our study indicates that this may not be the case when contact takes place in the community or hospital pharmacy setting. Promoting contact with people with mental illness is most effective as a strategy to reduce stigma when both health professionals and people with mental illness share equal status.16 During their clinical practice experience, the pharmacy graduates and people with mental illness were in a health care provider-patient relationship, and therefore equal status was unlikely to have been perceived.
The clinical practice experience involved the graduates working in general hospital and community pharmacy settings under the supervision of registered pharmacists with a minimum of 3 years practice experience. The clinical practice experience was not specifically focused on provision of psychiatric pharmacy services, although a significantly higher percentage of graduates had visited psychiatric facilities compared to the third-year students. This may be because graduates undertook their placements in hospitals with inpatient mental health facilities or community pharmacies that supplied medications to community mental health centers. Beyond attending continuing professional education lectures, some of which may have been related to mental health, the majority of graduates' supervisors would not have received specialist training in mental health. Graduates' attitudes may be reinforced by the attitudes of their supervisors, and therefore educating graduates' supervisors about mental illness may also be important.
The results of our study substantiate those of an earlier investigation of clinical psychiatry rotations undertaken by pharmacy students in the United States.14 In that study social distance was found to be unchanged before and after students' attendance at a psychiatric facility. Clinical placement programs for medical and nursing students, however, have been associated with improvements in social distance.15,25 A possible reason may be that although the pharmacy students and graduates frequently interacted with users of medications for mental illness, discussion may have been limited to how to take medications rather than peoples' experiences of their illness. Similarly, undergraduate pharmacy mental health education has tended to focus on the properties of medications rather than the experiences of people. Members of the general public with a medical understanding of schizophrenia had greater social distance than those who perceived schizophrenia as a life crisis.26 Given that social distance between health professionals and people with mental illness may mean that health professionals do not understand peoples' experiences of their illness,10 it is a concern that present educational strategies may not lead to improvements in social distance. Understanding and considering peoples' experiences of their illness is fundamental to the provision of concordant medication counseling. Lack of appreciation of consumer perspectives in treatment decision making is a key component of dissatisfaction reported by people with mental illness.27
Overall the pharmacy students and graduates held less stigmatizing attitudes in relation to dangerousness and unpredictability than the British general public10 or British medical students and practitioners.24 Unlike the British general public or medical students and practitioners, neither the pharmacy students nor graduates distinguished between people with severe depression or schizophrenia in terms of dangerousness to others. Previous studies of pharmacists' attitudes toward people with mental illness have examined attitudes to mental illness in general rather than attitudes to specific illnesses.2,14,19–21 Although schizophrenia has been more heavily stigmatized than other mental illnesses,7 this was not reflected in the way that the pharmacy students and graduates responded. This unexpected result may indicate that the pharmacy students and graduates viewed different types of mental illness in the same way. Given that mental illness encompasses a wide variety of conditions, this may suggest a lack of awareness about specific illnesses. Further research is needed to clarify the extent to which pharmacy students and graduates have different attitudes towards people with different types of mental illnesses. The pharmacy graduates were less likely to describe people with severe depression as unpredictable than were the pharmacy students, medical students and medical practitioners,24 and general public.10 Conversely, pharmacy graduates indicated that people with schizophrenia were harder to talk to than did the pharmacy students. Significantly more pharmacy students and graduates indicated that people with severe depression and schizophrenia “should pull themselves together” than the medical students and practitioners.24 This suggests that these pharmacy students and graduates may not have a comprehensive understanding of the nature of these illnesses.
When interpreting the results of our study, measurements of social distance and stigmatization do not necessarily reflect pharmacists' and pharmacy students' overall competence to provide pharmaceutical services. Our study assessed 2 frequently measured constructs, but there may be many components to students' ability and willingness to provide pharmaceutical services. Knowledge about mental disorders and the properties of psychotropic medications is one example. Some pharmacy students may have undertaken part-time work in pharmacies during the first 3 years of their degree course, and third-year pharmacy students at The University of Sydney are required to undertake a 3-hour per week structured internship in a hospital or community pharmacy. Our study did not assess whether attitudes of students or graduates changed over time, and it is possible that the pharmacy graduates had different attitudes to the third-year pharmacy students before commencing their supervised clinical practice. Additional studies with a parallel control group are required to make definitive conclusions about the impacts of pharmacy education programs on students' attitudes towards mental illness. Furthermore, as both undergraduate and postgraduate pharmacy education differs considerably across the world, our findings may not be generalizable to all settings and/or schools of pharmacy.
Notwithstanding the limitations described above, the results of our study suggest that more comprehensive education and training programs are needed to improve the ability of pharmacists to meet the needs of people with mental illness. Given the significant burden of mental illness, education about mental health care deserves much greater prominence in the curricula of most pharmacy schools. It is not sufficient for students and graduates to only understand about the pharmacology of psychiatric medications and how to counsel patients about potential adverse drug events. In order to provide effective health care, pharmacists must develop insights into the lives and challenges of people with mental illness. Further research into new models of mental health pharmacy education is warranted. Misconceptions about mental illness may be difficult to change through conventional educational strategies and are reinforced by media misrepresentation and the attitudes of peers.5 The use of “real patients” in the classroom to improve students' attitudes toward providing pharmaceutical care has been described;28 and the use of consumer educators to provide mental health education for community pharmacists has been piloted.29 Forming educational partnerships between consumer educators and pharmacy students may empower the consumers and be of educational value to students. This model of mental health education may allow pharmacy students to gain a better understanding of peoples' experiences of their illness.
CONCLUSIONS
The study suggests that traditional methods of pharmacy education, including mental health lectures and tutorials delivered by pharmacists, and clinical practice experience that takes place in the community or hospital pharmacy workplace, may not improve social distance or students' stigmatization of people with schizophrenia and severe depression. These forms of mental health education may not provide students or graduates with the insight required to understand peoples' experiences of their illness. The development of new models of pharmacy education may be required to improve communication between pharmacists and people with mental illness.
Table 3.
Pharmacy Students' and Graduates' Stigmatization of Patients With Serere Depression nad Schizophrenia
*Percentage who agreed or strongly agree with the statement
ACKNOWLEDGEMENTS
The authors thank the coordinators of the Pharmacy Graduate Training Course and the Pharmaceutical Society of Australia (NSW Branch) for their support and assistance.
REFERENCES
- 1.Bell S, McLachlan AJ, Aslani P, Whitehead P, Chen TF. Community pharmacy services to optimise the use of medications for mental illness: a systematic review. Aust New Zealand Health Policy. 2005;2:29. doi: 10.1186/1743-8462-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55:1434–6. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 3.Vainio KK, Airaksinen M, Hyykky TT, Enlund H. Effect of therapeutic class on counselling in community pharmacies. Ann Pharmacother. 2002;36:781–6. doi: 10.1345/aph.1A374. [DOI] [PubMed] [Google Scholar]
- 4.Happell B. Mental health nursing: challenging stigma and discrimination towards people experiencing a mental illness. Int J Ment Health Nurs. 2005;14:1–1. doi: 10.1111/j.1440-0979.2005.00339.x. [DOI] [PubMed] [Google Scholar]
- 5.Hocking B. Reducing mental illness stigma and discrimination - everybody's business. Med J Aust. 2003;178:S47– S48. doi: 10.5694/j.1326-5377.2003.tb05306.x. [DOI] [PubMed] [Google Scholar]
- 6.Crisp AH. The stigmatisation of sufferers with mental disorders. Br J Gen Pract. 1999;49:3–4. [PMC free article] [PubMed] [Google Scholar]
- 7. Mental health: a report of the surgeon general. United States Department of Health and Human Services, 1999 Available at: http://www.surgeongeneral.gov/library/mentalhealth/home.html Accessed December 12, 2005.
- 8.Hickie IB, Groom GL, McGorry PD, Davenport TA, Luscombe GM. Australian mental health reform: time for real outcomes. Med J Aust. 2005;182:401–06. doi: 10.5694/j.1326-5377.2005.tb06759.x. [DOI] [PubMed] [Google Scholar]
- 9.Weiss M, Britten N. What is concordance? Pharm J. 2003;271 [Google Scholar]
- 10.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illness. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 11.Bowman JT. Attitudes toward disabled persons: social distance and work competence. J Rehabil. 1987;53:41–4. [Google Scholar]
- 12.Holmes EP, Corrigan PW, Williams P. Changing attitudes about schizophrenia. Schizophr Bull. 1999;25:447–56. doi: 10.1093/oxfordjournals.schbul.a033392. [DOI] [PubMed] [Google Scholar]
- 13.Penn DL, Guyman K, Daily T. Dispelling the stigma of schizophrenia. Schizophr Bull. 1994;20:567–78. doi: 10.1093/schbul/20.3.567. [DOI] [PubMed] [Google Scholar]
- 14.Jermain DM, Crismon ML. Students' attitudes toward the mentally ill before and after clinical rotations. Am J Pharm Educ. 1991;55:45–8. [Google Scholar]
- 15.Mino Y, Yasuda N, Tsuda T, Shimodera S. Effects of a one hour educational program on medical students' attitudes to mental illness. Psychiatr Clin Neurosci. 2001;55:501–7. doi: 10.1046/j.1440-1819.2001.00896.x. [DOI] [PubMed] [Google Scholar]
- 16.Couture SM, Penn DL. Interpersonal contact and the stigma of mental illness: a review of the literature. J Ment Health. 2003;12:291–305. [Google Scholar]
- 17.Corrigan PW, River P, Lundin RK, Penn DL, et al. Three strategies for changing attributions about severe mental illness. Schizophr Bull. 2001;27:187–95. doi: 10.1093/oxfordjournals.schbul.a006865. [DOI] [PubMed] [Google Scholar]
- 18.Corrigan PW, Green A, Lundin RK, Kubiak MA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001;52:953–8. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- 19.Cates ME, Burton AR, Woolley T. Attitudes of pharmacists toward mental illness and providing pharmaceutical care to the mentally ill. Ann Pharmacother. 2005;39:1450–5. doi: 10.1345/aph.1G009. [DOI] [PubMed] [Google Scholar]
- 20.Crismon ML, Jermain DM, Torian SJ. Attitudes of pharmacy students toward mental illness. Am J Hosp Pharm. 1990;47:1369–73. [PubMed] [Google Scholar]
- 21.Bryant SG, Guernsey BG, Pearce EL, Hokanson JA. Pharmacists perception of mental health care, psychiatrists and mentally ill patients. Am J Hosp Pharm. 1985;42:1366–9. [PubMed] [Google Scholar]
- 22.Link B, Cullen F, Frank J, Wozniak J. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92:1461–500. [Google Scholar]
- 23.Corrigan PW, Edwards A, Green A, Diwan SL, Penn DL. Prejudice, social distance, and familiarity with mental illness. Schizophr Bull. 2001;27:219–25. doi: 10.1093/oxfordjournals.schbul.a006868. [DOI] [PubMed] [Google Scholar]
- 24.Mukherjee R, Fialho A, Wijetunge A, Checinski K, Surgenor T. The stigmatisation of psychiatric illness: the attitudes of medical students and doctors in a London teaching hospital. Psychiatr Bull. 2002;26:178–81. [Google Scholar]
- 25.Hicks J, Spaner F. Attitude change and mental hospital experience. J Abnorm Soc Psychol. 1962;65:112–20. [Google Scholar]
- 26.Lauber C, Nordt C, Falcato L, Rossler W. Factors influencing social distance toward people with mental illness. Community Ment Health J. 2004;40:265–73. doi: 10.1023/b:comh.0000026999.87728.2d. [DOI] [PubMed] [Google Scholar]
- 27.Happell B, Manias E, Roper C. Wanting to be heard: mental health consumers' experiences of information about medication. Int J Ment Health Nurs. 2004;13:242–8. doi: 10.1111/j.1440-0979.2004.00340.x. [DOI] [PubMed] [Google Scholar]
- 28.Chisholm MA, Wade WE. Using actual patients in the classroom to develop positive student attitudes toward pharmaceutical care. Am J Pharm Educ. 1999;63:296–9. [Google Scholar]
- 29.Bell JS, Whitehead P, Aslani P, Sacker S, Chen TF. Design and implementation of an educational partnership between community pharmacists and consumer educators in mental health care. Am J Pharm Educ. 2006;70 doi: 10.5688/aj700228. Article 28. [DOI] [PMC free article] [PubMed] [Google Scholar]