Abstract
Objectives
To determine learning-style scores of second-year pharmacy students before and after a problem-based learning (PBL) teaching experience and to evaluate the relationships between scores and demographic variables.
Methods
The Grasha-Reichmann Student Learning Style Scale (GRSLSS) was given to pharmacotherapy laboratory students before and after a semester-long problem-based learning class.
Results
Only one of the GRSLSS score variables was reported as “high” (“collaborative”) and none were reported as “low.” Students’ “avoidant” mean score increased and “participant” mean score decreased after completing the PBL experience (p ≤ 0.05).
Conclusion
While PBL appears to be a teaching style that is conducive to the learning preferences of this cohort of pharmacy students, significant changes in learning styles were noted after completing the PBL experience. These changes may reflect difficulties that occured in adapting from a didactic teaching style to PBL, and specifically, difficulties in adjusting to participating in a group learning experience. A major limitation was that the teaching style of the facilitator was not measured.
Keywords: problem-based learning, Grasha-Reichmann student learning style scale, pharmacotherapy laboratory
INTRODUCTION
Researchers in medical and pharmaceutical education are becoming increasingly aware that using a variety of teaching methods may ultimately improve retention of material, as well as enhance students’ adaptability in problem-solving situations.1–3 In addition, current research suggests that understanding a student's leaning style is helpful in providing a successful learning experience, no matter what teaching method is utilized.4,5
In the past decade, problem-based learning (PBL) has been introduced into pharmacy school curricula as an adjunct and/or alternative to a traditional didactic, classroom-based model of teaching.6–8 This teaching method, first developed at McMaster University in the 1960s, uses problems or cases to stimulate the students to construct the most appropriate solution. The method has several major characteristics.2,9 Learning is student-centered and occurs in small groups which are led by facilitators. The organizing focus of learning is the problem, which is selected to enhance the overall curricula and ultimately becomes the stimulus for the learning process. The problem may have multiple solutions and multiple sources are available to the student to derive these solutions. Wood made the following statement regarding the desired outcome in a healthcare-education setting: “Presentation of clinical material as the stimulus for learning enables students to understand the relevance of underlying scientific knowledge and principles in clinical practice.”10
The introduction of PBL may be an uncomfortable experience for the didactically trained student.6,11 The student's role is transformed from passive to active, requiring communication skills, independent responsibility for learning, and ability to work with a team to solve problems. One way to facilitate students’ adaptation to PBL is to evaluate their learning styles. The term learning style was defined by Cassidy as “the ways in which individuals characteristically approach different learning tasks.”5 Brown described learning style as “a particular set of behaviors and attitudes related to learning context.”4 There are a variety of definitions, theories, and models that measure the concept of “learning styles.” Authors such as Cassidy have noted that the topic has become fragmented as the field of research has grown over the past 40 years and increasingly has been applied to a diverse variety of areas, including medical and pharmaceutical education, psychology, management, and industry.5
Cassidy also points out that selecting an instrument to measure a student's learning style can be difficult.5 The Curry Onion Model12,13 is commonly used to help to generalize categories from which to investigate learning styles in order to accomplish this task.5,14 The outermost layer of this model uses scales such as the Dunn et al Learning Style Inventory to investigate the student's instructional preferences.15 The next layer investigates how the student interacts in a learning situation, and how these interactive characteristics affect learning preferences. An example of a related learning-style instrument is the Grasha Reichmann Student Learning Style Scale (GRSLSS).16,17 The next layer investigates the preferred approach the student uses for information processing with instruments such as Kolb's Learning Style Inventory,18 and the Felder and Solomon Index of Leaning Styles.19 The final layer of the Curry Onion Model evaluates a student's cognitive personality style and how it influences preferred ways to acquire and integrate information with scales such as the Meyers Briggs Type Indicator.20
Two studies have evaluated learning styles in pharmaceutical education. Pungente et al evaluated learning styles of first-year pharmacy students in relation to preferences associated with different PBL-related activities using the Kolb's Learning Styles Inventory. In the second study, Austin used the Kolb Learning Styles Inventory and the Pharmacist's Inventory of Learning Styles to evaluate the impact of learning styles on the career decisions, practice patterns, and teaching method preferences of established pharmacists.21
The Pharmacist's Inventory of Learning Styles (PILS) was first described in the literature in 2004 and is specific to pharmacy practice and education.22 This instrument was based on the work of Kolb, and includes an emphasis on psychometric measures of reliability and construct validity.23 This later emphasis is of vital importance in this field because of the noted weakness in reliability and validity of the majority of the currently available learning-style instruments.5,12 Evaluation of these metrics was performed in 3 settings at 3 times, with 2 samples consisting of hospital pharmacists (n1 = 12 and n2 = 15) and 1 sample of community pharmacists (n = 21). Reliability using Cronbach's alpha was 0.847 to 0.898 for each group. Construct validity was determined to be in the moderate to high range, and the evaluation suggested the instrument particularly lent itself to identifying the more dominant learning styles of the student.
The first objective of this study was to identify learning styles of students upon entering a PBL experience. This objective was set, in part, to determine the appropriateness of this teaching method for the cohort of students who were tested, and to anticipate possible adjustments to teaching styles that might be required based on the student’ preference of teaching style (as indicated by their learning-style scores). The second objective was to determine whether students’ learning styles differed before and after exposure to a PBL course. This objective was based on the suggestion that students may prefer certain styles of learning, but these preferences may change according to how a class is structured, demands of teachers, assignments, or evaluations.17 This objective was also set to determine whether changes in learning-style scores occurred secondary to changes in social interactive variables that occurred over the semester. The third objective was to evaluate the relationships between learning styles and demographic variables both before and after PBL exposure.
METHODS
The instrument chosen for this study (with actual administration occurring in fall 2003) was the GRSLSS. This instrument, selected prior to the publication of the PILS, was chosen for several reasons. The GRSLSS is useful because it focuses on the student's interaction with the facilitator, other students, and the learning process itself. As noted above, the GRSLSS is an instrument that measures learning styles in relation to social interaction, and therefore, allows for the introduction of social and affective dimensions.24 The instrument allows for evaluation of a student's learning style, and Grasha has extensively described the teaching style environments that a student may prefer based on the derived learning-style scores.17 The social and affective dimensions of the instrument allow for an evaluation of potential problems that students may encounter with the introduction of a group-PBL experience.6 The use of the GRSLSS, therefore, allowed for measurement of learning style, identification of potential preferences for teaching style, and measurement of social interaction.
The instrument is self-administered, and consists of a 60-item questionnaire that is constructed to identify 6 major learning styles. Ten questions are assigned to each learning style construct and answers are recorded using a 5-point Likert scale. The individual learning styles have been described by Grasha in the following ways.17 The “independent” learner is described as a student who likes to think for himself or herself and often prefers to work alone. The “avoidant” learner is uninterested, does not participate, and may be overwhelmed by the class activities. The “collaborative” learner is characterized as a student who enjoys sharing ideas and knowledge, and works well with both students and facilitators. The “dependent” learner is classified by Grasha as a student who works well when specific guidelines are established by authority figures and performs duties that are required. The “competitive” learner performs as the term describes; he or she competes and generally enjoys the recognition that accompanies excelling. The “participant” learner is eager, and Grasha describes this student as one who takes part in as much of the course activity as possible.
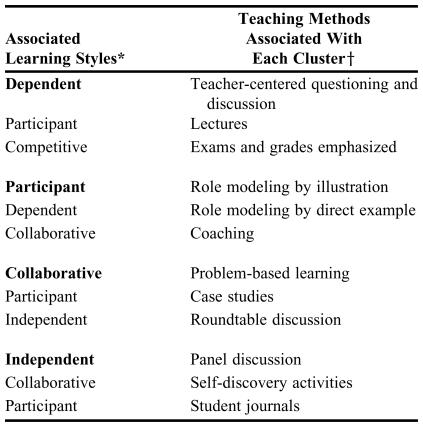
Certain relationships have been identified between clusters of primary learning styles and teaching styles. A summary of these relationships is shown in Table 1. Grasha links the 6 primary learning styles into groups of 3, listing the variables in order of importance. Students who prefer a teaching style that utilizes PBL fall into a cluster of learning styles that includes a triad of “collaborative,” “participant,” and “independent” characteristics, with “collaborative” being the most important variable in this particular combination.19
Table 1.
Clusters of Learning Styles and Associated Preferred Teaching Methods
Source: Grasha, AF. An integrated model of teaching and learning style. In: Grasha, AF. Teaching with style: a practical guide to enhancing learning by understanding teaching and learning styles. San Bernardino, Calif: Alliance Publishers; 1996:158, 177. Printed with permission from Alliance Publishers.
*Listed in order of importance
Teaching methods are not necessarily correlated with the adjacent listed learning style
While the GRSLSS allows for the above advantages, one disadvantage of using this instrument is the paucity of evidence on its reliability and validity, which as noted above, is a concern for most of the learning-style instruments.25 Another disadvantage is a lack of previous use of the GRSLSS in pharmacy research.
The initial sequence of pharmacotherapy laboratory courses at the University of Texas at Austin, which are taught in the second year of the professional program, are one of the earliest introductions of PBL in the pharmacy curriculum. The students examined in this analysis (119 in total) were divided into 14 laboratory sections (3 sections held on Monday through Thursday afternoons, and 2 sections on Friday). The laboratory period lasted 3 hours each week. Each section consisted of 8 or 9 students, except for 1 section which contained 6 students. These groups were randomly assigned by the pharmacy school administration without regards to any demographic variable.
The students were given 1 introductory hour-long session in a classroom format the week prior to the first laboratory session. This session explained the requirements for the course and grading, which was described comprehensively in a course syllabus. The first week of laboratory consisted of a team-building exercise that was non-pharmaceutical in nature. This session allowed the students to meet each other, their facilitator (with 6 of the 14 sections having 2 facilitators who shared responsibilities), and their teaching assistant. These 2 sessions (a classroom encounter and an introductory laboratory session served) as the only introduction to PBL before the actual course material was introduced.
A facilitator worked with only 1 group during the semester. There were 21 facilitators including 4 full-time faculty members, 11 local practitioners (representing hospital practice, pharmaceutical industry, and retail environments), and 6 residents associated with pharmacy school-affiliated programs. Nineteen of the facilitators held a doctor of pharmacy degree, 1 held a doctor of philosophy degree, and 1 held a bachelor of science degree.
All cases were selected from Schwinghammer's Pharmacotherapy Casebook.26 All groups received the same case. Introductory cases in the first 2 weeks allowed for a “training period” to introduce the student about how to analyze case material, synthesize it, and develop the “subjective,” “objective,” “assessment” and “plan” sections of a SOAP note. In the subsequent 8 weeks, the students were presented clinical case examples from the casebook for discussion at approximately the same time of the semester that relevant basic and clinical science material was presented in the didactically taught pharmacotherapy course. Students were asked to read the case prior to their laboratory session. The students were encouraged to bring appropriate “hard-copy” resources (including class notes, texts, and treatment guidelines) to class to help with case analysis and discussion and this type of participation was reflected in his or her grade. Internet connections were also available in each laboratory to allow for classroom access to resource material.
The case, including the hypothetical patient's subjective and objective information was read aloud at the beginning of the lab. The group discussion was “guided” by the facilitator who may or may not have been an “expert” on a particular case topic. The required output for the course consisted of a group-derived SOAP note that was primarily completed in the laboratory but finished by a different student in the group each week. Each individual student was also asked to turn in a written note each week describing how the patient would be “counseled” about taking one of the hypothetically prescribed medications in a clinical pharmacy setting.
Approximately half of the facilitators were new to the laboratories; they received an introduction to the format of the class immediately prior to the first introductory laboratory. Each week, in addition to the accompanying teaching material that was provided by the text's author for each case, a written SOAP note (prepared by at teaching assistant or facilitator familiar with that disease state) was given to the facilitator to help in leading the group.
Fifty percent of the student's grade was given by the group facilitator(s) and was based on variables such as leadership, performance, preparedness, and participation. In an effort to maintain consistency, each facilitator was monitored weekly for deviations from mean grading scores, and the reason that deviations might be occurring. The SOAP notes (25% of the final grade) and patient counseling written reports (25% of the final grade) were graded weekly in group sessions held by the teaching assistants to assure consistency in scoring. This analysis was not designed to evaluate the correlation of a specific learning style with final grades or a group's grade with their mean learning-style score.
The study sample consisted of all pharmacy students enrolled in the Pharmacotherapeutics I Laboratory in the fall semester of 2003. Institutional Review Board (IRB) approval was obtained prior to enrolling the students in the study and participation was voluntary. Informed consent was required in order to complete the IRB approval, which was authorized as an “exempt” protocol. No compensation was provided for completing the instrument.
The GRSLSS was given in a longitudinal panel design, with the first administration occurring on the first day of the laboratory, and the second administration occurring on the last day. Demographic questions were asked at the time of the first administration; these items included age, gender, level of education obtained prior to entry into pharmacy school (specifically, if a student had completed a degree prior to entering pharmacy school), and previous experience with PBL (specifically, if a student had taken a class that used this teaching method).
Student responses were analyzed both descriptively and inferentially. The means and standard deviations of pretest and posttest learning-style scores were calculated for the 6 learning styles. Paired samples t tests were then used to compare the pretest and posttest scores for each learning style. Independent samples t tests and bivariate correlation analyses were used to determine whether relationships existed between learning-style scores (pretest and posttest) and demographic variables (age, gender, prior degree, and prior experience with PBL). The facilitators in this study were not analyzed according to teaching style, and there was no formal analysis of the amount or type of interaction that occurred in any individual laboratory section. The a priori level of significance for all statistical analyses was p < 0.05. SPSS version 12.0 for Windows (SPSS, Inc, Chicago, Ill) was used for all statistical analyses.
RESULTS
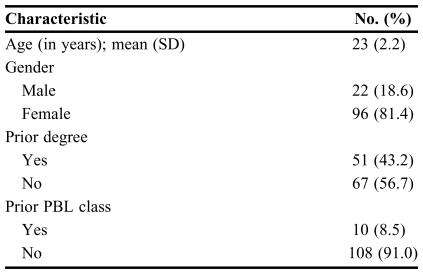
A total of 118 (99.2%) of the 119 students in the course participated in the survey. Table 2 shows demographic information about the survey participants. The students were predominately female (81.4%) and an average age of 23 years. Fewer than half of the students (42.5%) had acquired a previous degree prior to entering pharmacy school, and only 8.5 percent of the students had previously taken a PBL-style class.
Table 2.
Demographic Characteristics of the Surveyed Pharmacy Students (N = 118)
PBL = problem-based learning
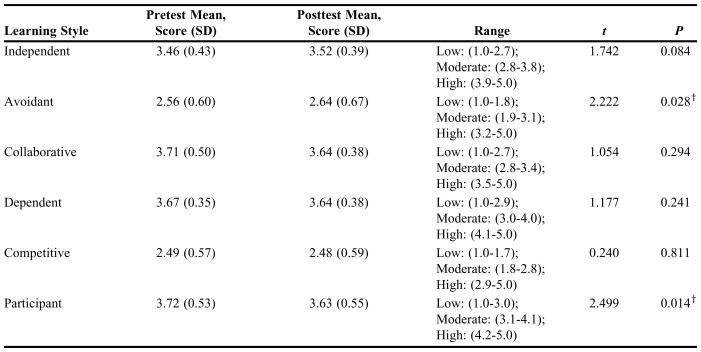
Table 3 shows the means and standard deviations of pretest and posttest scores for each learning style for the cohort, with the associated score designation (low, moderate, or high). The only learning style that did not fall into the moderate category was the “collaborative” score, which ranked as high in both the pretest and posttest survey. Significant differences were found between the pretest and posttest scores for the “avoidant” learning style, which increased by the time of the second survey instrument was administered, and the “participant” learning style, which decreased. A slight increase occurred in the “independent” learning-style score, and a slight decrease occurred in the “collaborative” and “competitive” scores, but these changes were not statistically significant.
Table 3.
Pretest and Posttest Mean Learning Scores*
The Likert scale used ranged from 1 to 5 with 1 being “strongly disagree” and 5 being “strongly agree.” Ten questions were assigned to each learning style. Each score for “low,” “moderate,” and “high” were determined by the authors of the instrument
†p < 0.05
Source: Grasha, AF. An integrated model of teaching and learning style. In: Grasha, AF. Teaching with style: a practical guide to enhancing learning by understanding teaching and learning styles. San Bernardino, Calif: Alliance Publishers; 1996:158, 177. Published with permission from Alliance Publishers.
Pearson correlation analyses showed no significant relationships between age and learning-style scores (both pretest and posttest) for any of the learning-style subscales. In terms of gender, before the PBL experience, female students had significantly lower “avoidant” scores (p = 0.002), and higher “participant” scores (p = 0.002) than males. Students who had obtained a prior degree or had a prior PBL experience had higher “competitive” scores than students with no prior degree (p = 0.038) or no prior PBL experience (p = 0.020), respectively.
After the PBL experience, female students still had significantly lower “avoidant” scores than male students (p = 0.027). Female students also had significantly higher “participant” scores than male students (p = 0.002). The only other significant difference noted on the posttest was that those students who had a prior PBL class still had significantly higher “competitive” scores than those students who had not been exposed to the teaching style prior to the pharmacotherapy laboratory experience (p = 0.014). In contrast to the pretest scores, no significant difference was found in posttest “competitive” scores with respect to prior degree status.
DISCUSSION
During the past decade, emphasis has been placed on changing pharmacy curricula in recognition of the importance of problem solving, critical thinking, and self-directed learning as vital skills required to address the types of clinical presentations that occur in today's pharmaceutical practice environment.27,28 PBL is one teaching method that may encourage these changes, as it encourages problem solving by hypothesis generation, with subsequent data collection and analysis, synthesizing prior-learned knowledge with additionally acquired basic science and clinical information.
The results of this survey analysis were encouraging for the use of PBL in this group of predominately female, second-year pharmacy students, who had little prior exposure to this teaching method. Overall, the scores for the learning-style preferences were moderate for all of the constructs except for the “collaborative” learning style. The relatively high scores found for the “collaborative” construct (the most important learning style listed for students who prefer PBL) supports the notion that this is an appropriate teaching style for this component of the pharmacotherapy curriculum, in that PBL classroom methods encourage collaborative, student-centered learning processes.17 The high scores for “collaborative” learning preferences may be a reflection, in part, of the high percentage of female students in the class (81.4%), as it has been consistently noted that female gender has a positive correlation with this construct.8 In addition, the moderate scores for the “participant” and “independent” learning styles (styles associated in the triad found among students who prefer PBL) suggested that, overall, this group of students would not have difficulties when introduced to this teaching method.
The results showed a significant pretest to posttest increase in the mean “avoidant” learning-style scores, and a significant pretest to posttest decrease in the mean “participant” learning-style scores. As noted in the introduction, students’ learning preferences may change according to how a class is structured, demands of teachers, assignments, or evaluations.17 The amount of time required for these types of changes is not well documented, and the short duration of this study (1 semester) may not allow for an accurate measurement of this variable. One specific variable that may have affected this change could have been the “stress” that occurs when PBL teaching methods are implemented.6,11,30 Students whose educations have been based mostly if not entirely on traditional didactic teaching methods tend to have difficulty when initially introduced to PBL, and this difficulty may continue until they become familiar with the teaching style.30
The changes noted in this analysis that move the overall cohort in a small, but significant direction away from adapting to PBL deserve examination. Some reports note that it takes students up to 2 years to become comfortable with PBL.31 Some of this difficulty appears to be related to tension between students and facilitators as they both become adjusted to this less-common teaching style. A limitation of the current study is that the facilitators who taught this cohort of students were not tested regarding their preferred teaching style; therefore, it is difficult to determine how much of the above noted change in learning styles could be related to the instructor, who may have had difficulty adapting to PBL or interacting with particular students.
In this cohort, only 8.5% of students had a previous PBL experience. Students may have problems learning to work in a group. Haworth et al suggest that problems arise due to lack of experience in both working in a group context and adjusting to the idea that each individual student must depend on the others in the group.6 In this cohort of student, group friction was occasionally noted throughout the semester and, in part, might explain the increase in “avoidant” and decrease in “participant” learning styles. Anecdotally, facilitators and teaching assistants noted what were described as occasional “personality conflicts” among students in this cohort. These conflicts may be on the level of “social interaction” as measured in the GRSLSS, but might be better measured using an instrument that evaluates the “personality” layer of learning styles, such as the Myers-Briggs Type Indicator.
The finding that students who had a previous PBL experience had higher “competitive” learning-style scores both before and after the PBL experience is not easily explained. This result may reflect a true difference in this subset of students or it may be due to the small number of students who had a previous PBL class (10 of 108).
Limitations
As evaluations of learning styles in relation to both designing educational curricula and examining the success of existing programs are a relatively new field, a discussion of the limitations of this study deserves examination. On a methodology level, a major limitation is that the GRSLSS is not well validated, and has not been used much in pharmacy education research. As there was a desire to examine social interaction with this study, an instrument that was better validated or had been previously used in pharmacy research may have been more appropriate. In addition, as there was a possibility that overall personality of the students in a cohort might have created conflict, a measure of learning styles in relation to personality might be warranted.
The teaching style of the facilitators was not measured. Therefore, it was impossible to determine how the findings of increased “avoidant” and decreased “participant” learning styles, a direction that indicated that the students were less likely to prefer PBL, were secondary to the teaching method or secondary to social interaction. In addition, the actual level of interaction of the facilitators, which influences the type of PBL experience that was introduced in the class, was not measured or required to be standardized.
While the overlying intent of the design of this course was to implement a “problem-based” educational method using Barrow's taxonomy for developing PBL curricula, many of our laboratories might more aptly be described as using the “case-method” using the same taxonomy.29 The “problem-based” method utilizes a problem and allows for free-inquiry by the students in the tutor-led groups, while the “case method” allows for cases that are discussed in tutor-facilitated discussion. Depending on the input from the facilitator assigned to the group, the overall educational method appears to have traversed the range between these 2 methods. This ultimately led to difficulties in interpreting our measurements because the level of interaction with the facilitator was not well documented and not well standardized.
Only minor changes have been made to the introductory semester of the laboratory since this study was completed, and the study findings have not discouraged the use of this teaching method. Several projects are planned to evaluate the use of PBL in the pharmacotherapy laboratories utilizing learning-style measurement tools. A longitudinal study is being planned that will evaluate a class of students from the fall through the summer semester, with an inclusion of an analysis of facilitator teaching styles. This will involve some logistic difficulty as the groups and facilitators change from semester to semester, but will allow for several important analyses. The first will be to investigate the potential change in learning styles with the introduction of PBL over a longer period of study. The study will also allow for a more in-depth analysis of the role of social interaction in group dynamics, and may point to the need for further study of the role of personality as far as success of the groups using appropriate learning-style instruments.
CONCLUSION
This study showed that PBL was an appropriate teaching method for the introductory pharmacotherapy laboratories at the College of Pharmacy at the University of Texas at Austin. The most significant changes in learning-style scores, the increases in “avoidant” and decreases in “participant” learning-style scores, may have been a reflection of the difficulty in adapting to the change in learning style from didactic to PBL as well as problems adapting to working in a group. A major limitation was that the teaching style of the facilitator was not measured. Further research is planned to evaluate learning-style changes with introduction of PBL on a long-term basis as well as to examine the effect of facilitator teaching-style preferences on these changes.
Acknowledgments
The authors thank Dr. A.F. Grasha for the generous use of his learning-style instrument, the Grasha-Riechmann Student Learning Style Scale.
REFERENCES
- 1.Vaughn L, Baker R. Teaching in the medical setting: balancing teaching styles, learning styles and teaching methods. Med Teach. 2001;23:610–2. doi: 10.1080/01421590120091000. [DOI] [PubMed] [Google Scholar]
- 2.Barrows HS. Problem-based learning in medicine and beyond: A brief overview. In: Wilkerson L, Gijselaers WH, editors. Bringing Problem-Based Learning to Higher Education: Theory and Practice. San Francisco, Ca: Jossey-Bass Inc., Publishers; 1996. pp. 3–12. [Google Scholar]
- 3.Pungente MD, Wasan KM, Moffett C. Using learning styles to evaluate first-year pharmacy student's preferences toward different activities associated with the problem-based learning approach. Am J Pharm Educ. 2002;66:119–24. [PMC free article] [PubMed] [Google Scholar]
- 4. Brown BL. Learning styles and vocational education practice. Columbus, Oh: Center on Adult, Career, and Vocational Education, The Ohio State University College of Education; 1998. Available at: http://www.cete.org/acve/docs/pab00007.pdf. Accessed May 20, 2003.
- 5.Cassidy S. Learning styles an overview of theories, models, and measures. Educ Psychol. 2004;24:419–44. [Google Scholar]
- 6.Haworth IS, Eriksen SP, Chait SH, et al. A problem based learning, case study approach to pharmaceutics: faculty and student perspectives. Am J Pharm Educ. 1998;62:398–405. [Google Scholar]
- 7.Borrego ME, Rhyne R, Hansbarger LC. Pharmacy student participation in rural interdisciplinary education using problem based learning (PBL) case tutorials. Am J Pharm Educ. 2000;64:355–63. [Google Scholar]
- 8.Romero RM, Eriksen SP, Haworth IS. A decade of teaching pharmaceutics using case studies and problem-based learning. Am J Pharm Educ. 2004;68 doi: 10.5688/aj740466. Article 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilkerson L, Gijselaers WH. Concluding comments. In: Wilkerson L, Gijselaers WH, editors. Bringing Problem-Based Learning to Higher Education: Theory and Practice. San Francisco, Ca: Jossey-Bass Inc., Publishers; 1996. pp. 101–4. [Google Scholar]
- 10.Wood DF. ABC of learning and teaching in medicine: problem based learning. BMJ. 2003;326:328–30. doi: 10.1136/bmj.326.7384.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duncan-Hewitt WC. A focus on process improves problem-based learning outcomes in large classes. Am J Pharm Educ. 1996;60:408–16. [Google Scholar]
- 12.Curry L. Patterns of learning styles across selected medical specialties. Educ Psychol. 1991;11:247–78. [Google Scholar]
- 13.Curry L. Ottawa, ON: Canadian College of Health Services Executives; 1987. Integrating concepts of cognitive or learning style. A review with attention to psychometric standards. [Google Scholar]
- 14. Griggs SA. Learning Styles Counseling ERIC Digest. 1991; ERIC Document 341890. Available at: http://www.ericae.net/edo/ED341890.htm. Accessed December 2, 2005.
- 15.Dunn R, Dunn K, Price GE. Lawrence, Kan: Price Systems; 1989. Learning Styles Inventory. [Google Scholar]
- 16.Riechmann SW, Grasha AF. A rational approach to developing and assessing the construct validity of a student learning style scales instrument. J Psychol. 1974;87:213–23. [Google Scholar]
- 17.Grasha AF. Teaching with Style: A Practical Guide to Enhancing Learning by Understanding Teaching and Learning Styles. San Bernardino, Calif: Alliance Publishers; An integrated model of teaching and learning style. 1996. [Google Scholar]
- 18.Kolb DA. Self-Scoring Inventory and Interpretation Booklet. Boston, Mass: McBer and Co; 1985. Learning Style Inventory. [Google Scholar]
- 19. Felder R. Index of Learning Styles (ILS). Available at: http://www.ncsu.edu/felder-public/ILSpage.htm. Accessed December 2, 2005.
- 20.Myers I. Palo Alto, Ca: Consulting Psychologists Press; 1978. Myers-Briggs Type Indicator. [Google Scholar]
- 21.Austin Z. Learning styles of pharmacists: impact on career decisions, practice patterns and teaching method preferences. Pharm Educ. 2004;4:13–22. [Google Scholar]
- 22.Austin Z. Development and validation of the Pharmacists' Inventory of Learning Styles (PILS) Am J Pharm Educ. 2004;68 Article 37. [Google Scholar]
- 23.Merritt SL, Marshall JC. Reliability and construct validity of alternate forms of the CLS Inventory. Adv Nurs Sci. 1984;7:78–85. doi: 10.1097/00012272-198410000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Jonassen DH, Grabowski BL. Hillsdale, NJ: Lawrence Erlbaum Associates; 1993. Handbook of International Differences, Learning and Instruction. [Google Scholar]
- 25. Middle States Commission on Higher Education. Measures of Learning Style Originating from a Variety of Perspectives. Student Learning Assessment: Options and Resources-A Handbook. Philadelphia, Penn. Available at: http://www.msache.org/oldsite/s52.html. Accessed December 2, 2005.
- 26.Schwinghammer TL. 5th ed. New York, NY: McGraw-Hill; 2002. Pharmacotherapy Casebook: A Patient Focused Approach. [Google Scholar]
- 27.American College of Clinical Pharmacy. A vision of pharmacy's future roles, responsibilities, and man-power needs in the United States. Pharmacotherapy. 2000;20:991–1020. doi: 10.1592/phco.20.11.991.35270. [DOI] [PubMed] [Google Scholar]
- 28.Cisneros RM, Salisbury-Glennon JD, Anderson-Harper HM. Status of problem-based learning research in pharmacy education: a call for future research. Am J Pharm Educ. 2002;66:19–26. [Google Scholar]
- 29.Barrows HS. A taxonomy of problem-based learning methods. Med Educ. 1986;20:481–6. doi: 10.1111/j.1365-2923.1986.tb01386.x. [DOI] [PubMed] [Google Scholar]
- 30.Milfin BM, Campbell CB, Price DA. A lesson from the introduction of a problem-based, graduate entry course: the effects of different views of self-direction. Med Educ. 1999;33:801–7. doi: 10.1046/j.1365-2923.1999.00399.x. [DOI] [PubMed] [Google Scholar]
- 31.Des Marachais JE. A student-centered, problem-based curriculum: 5 years' experience. Can Med Assoc J. 1993;148:1567–72. [PMC free article] [PubMed] [Google Scholar]
- 32. O'Connor T. Using learning styles to adapt technology for higher education. Center for Teaching and Learning, Indiana State University. 1997. Available at: http://web.indstate.edu/ctl/styles/learning.htm. Accessed November 29, 2005.