Abstract
Objectives
To determine whether a required course addressing complementary and alternative medicine would change students' attitudes and perceptions toward the subject and the likelihood that they would recommend various complementary and alternative medicine therapies
Methods
A survey instrument was administered to all third-year PharmD students on the first and last days of the course. The degree of change in response for each question was assessed and analyzed in order to determine the impact of the course.
Results
Fifty-five students (93%) completed both the preintervention and postintervention survey instrument. Over half of the students had changes in their attitudes regarding their future competence, their personal interest and experience with complementary and alternative medicine, and their personal beliefs towards the subject after completion of the course. A large proportion of students also had changes in the likelihood that they would recommend a natural product for various conditions and that they would recommend complementary and alternative medicine therapies in general.
Conclusions
A required course addressing complementary and alternative medicine and natural products significantly changed students' attitudes and perceptions toward the subject, as well as their likelihood to recommend various complementary and alternative medicine therapies and natural products in a professional setting.
Keywords: complementary medicine, alternative medicine
INTRODUCTION
The 2002 National Health Interview Survey (NHIS) reported that 50% of all adults in the United States have used some form of complementary and alternative medicine (when prayer is not included).1 The use of natural products, defined by the CDC as herbal and botanical medicines; functional foods, such as garlic; vitamins and minerals; and animal-based supplements, such as glucosamine, has increased from 14.2% of adults in 1998-1999 to 18.8% in 2002.2
The increased use of natural products impacts the practice of pharmacy. Studies show that pharmacists are frequently asked about natural products.3,4 A large number of pharmacists have recommended natural products to patients and/or family and friends.4,5 Even while making these recommendations, these pharmacists felt that they needed more training on the subject and that the information available to them was inadequate.3,4 Students also feel that pharmacists have a responsibility to provide information on herbal supplements, but few feel that they have adequate knowledge to provide that information.6
The need for more training in the area of complementary and alternative medicine, specifically natural products, was reiterated when a competency specifically addressing dietary supplements was added to the North American Pharmacist Licensure Examination (NAPLEX) in May 2005.7 As of 2003, a study by Shields and colleagues showed that only 51 of 64 (80%) responding pharmacy schools offered any exposure to complementary and alternative medicine topics. Forty of them offered courses exclusively on the subject, mostly in the form of electives.8 This percentage will be increasing, however, with the implementation of the 2005 Accreditation Council for Pharmacy Education (ACPE) Standards for Accreditation, which recommends didactic coursework addressing patient use of dietary supplements, alternative medical treatments, the evaluation of the efficacy and safety of complementary and alternative medicine , and herbal-drug interactions, as well as exposure to these products during advanced pharmacy practice experiences.9
Course Structure
South University created a required course entitled Complementary and Preventive Medicine, for the third-professional year curriculum prior to beginning advanced pharmacy professional experiences. This 3-hour course includes 20 contact hours devoted to complementary and alternative medicine topics and 10 contact hours devoted to general personal wellness. The desired course outcomes, as related to complementary and alternative medicine, were to prepare the students to:
Discuss the scope of various complementary medicine practices.
Evaluate available information pertaining to herbal and natural products and make sound recommendations as to their use.
The course coordinator and instructors attempted to present information in an unbiased manner and allow the students to form their own opinions. Topics covered in the course included alternative medical systems, such as Chinese and Ayuverdic medicine and homeopathy; body-based/manipulative therapies, such as chiropractic care and massage; mind-body interventions, such as hypnosis, meditation, deep-breathing, and therapeutic touch; quality assurance of natural products; and literature evaluation. Specific natural products were covered in 15- to 20-minute student presentations, in which groups of 4-5 students were required to present the general information on the product (proposed mechanism, proposed uses, adverse effects, interactions, dosage forms available, etc) and conduct a literature evaluation of 1 or 2 assigned clinical trials. In addition to the presentation, students were required to create a brochure-sized patient handout. This project accounted for 25% of the final course grade. The students were also responsible for 5 out-of-class assignments (5% each), 3 of which pertained to complementary and alternative medicine: a literature evaluation of 1 of 10 selected clinical trials; designing a clinical trial to demonstrate the safety or efficacy of an assigned natural product; and a short writing assignment regarding the need and utility of including a course such as this in the PharmD curriculum. Lastly, 2 examinations were administered, each counting 25% of the course grade. The first examination included all of the personal wellness topics, as well as quality assurance of natural products and alternative medicine systems. The second examination only tested knowledge of specific natural products covered by the student presentations.
METHODS
The willingness of pharmacists to recommend natural products in spite of perceived lack of knowledge lead the authors to question whether a required course addressing complementary and alternative medicine would change students' attitudes and perceptions toward the subject and the likelihood that they would recommend various complementary and alternative medicine therapies. A 3-part survey instrument was developed to assess changes in students' attitudes/perceptions and the likelihood that they would recommend various complementary and alternative medicine therapies.
Part 1 was made up of 16 items based upon the tool used by Dutta and colleagues and assessed students' attitudes and perceptions towards complementary and alternative medicine, as related to 5 major categories/factors:
Future concerns for professional competence
Personal interest in complementary and alternative medicine
Personal experience with complementary and alternative medicine
Personal beliefs towards complementary and alternative medicine
Philosophical congruence
Students were required to rate each item based on a Likert-type scale with “strongly agree” responses valued at 5 and “strongly disagree” responses valued at 1.10 Part 2 consisted of a list of 10 common indications for the use of natural products as reported by Kelly and colleagues.2 Students were asked to rate their likelihood of recommending an herbal product as both primary and adjunct therapy for each indication. A response of “very likely to recommend” was valued at 5 and a response of “not at all likely to recommend” was valued at 1.
Part 3 of the survey consisted of a list of 6 commonly used complementary and alternative medicine therapies, as reported in the 2002 NHIS data.1 Students were asked to rate their likelihood of recommending the therapies as primary therapy and adjunct therapy. A response of “very likely to recommend” was valued at 5 and a response of “not at all likely to recommend” was valued at 1.
The authors administered the survey instrument to all third-professional year PharmD students on the first and last days of the course. Both times, the survey instruments were collected by a student and returned to an administrative assistant, who assigned an identifying number to each student, then removed the cover sheet, which contained the student's name. The administrative assistant then returned the numbered survey instruments to the authors.
As the hypothesis of the study was that students' scores would change as a result of the course, the direction of the change was not taken into account. For each item on the survey instrument, the percentage of students whose responses changed by at least 1 unit was reported, as was the percentage of students whose responses changed by 2 or more units, which was deemed significant by the authors as it reflected a strong opinion shift. A paired-difference t test was conducted for each survey instrument to determine whether the absolute value of the change was statistically significant. Cronbach alpha coefficients of 0.83, 0.93, and 0.75, for parts 1, 2, and 3 of the presurvey, respectively, indicated that the survey instrument was reliable and internally consistent.
Approval was granted by the St. Joseph/Candler Institutional Review Board on July 22, 2005. Students signed a consent that stated the purpose of the survey and assured them of confidentiality and blinding of the faculty members who served as the study investigators.
RESULTS
Fifty-five of 59 (93%) students successfully completed both the preintervention and postintervention survey instruments. Paired difference t tests on the absolute value of the change in responses between preintervention and postintervention survey instruments yielded p values of <0.001 for each of the 48 survey instrument questions, denoting that there was a significant change in the scores.
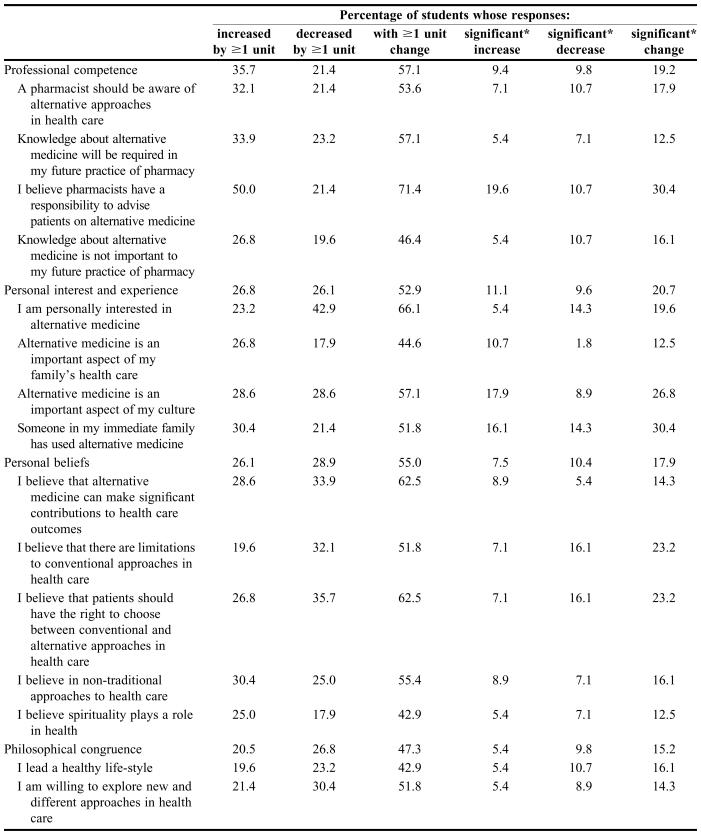
Table 1 shows the results of Part 1 of the survey instrument. Over half of the students had an average change of at least one unit in their response to the questions assessing students' concerns about their future competence, personal interest and experience, and personal beliefs (57.1, 52.9, 55.0%, respectively). Just under half (47.3%) had a 1-unit change in their responses to questions on philosophical congruence. As would be expected, fewer students' responses reflected a “significant” change (2 or more units), but that percentage ranged from 15.2% (philosophical congruence) to 20.7% (personal interest and experience).
Table 1.
Changes in Pharmacy Students' Responses on Part One of a Survey Instrument Regarding Attitudes and Perceptions Toward Complementary and Alternative Medicine Administered After Completion of a Required Course, %
*Significant = ≥2 units
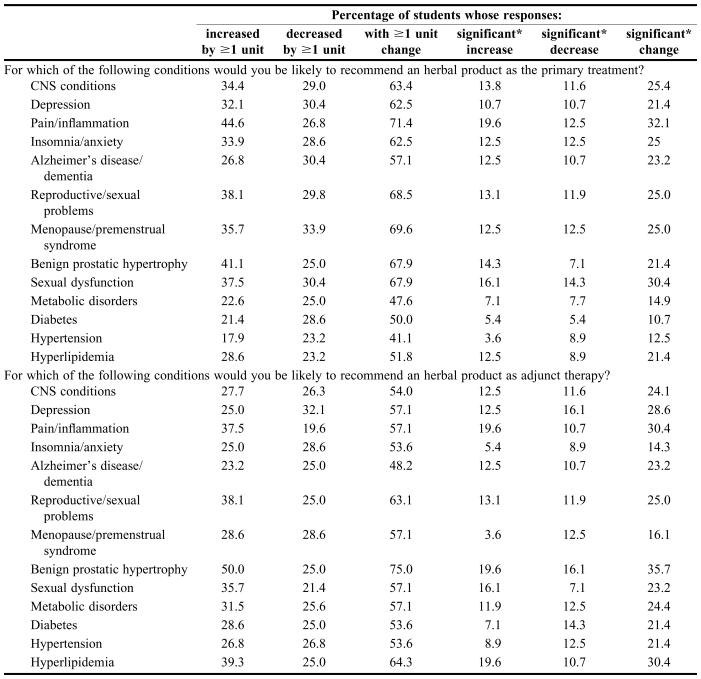
Table 2 shows the results of Part 2 of the survey instrument. Over half of all students' responses changed by one or more units on the question concerning their likelihood to recommend an herbal product as a primary or adjunct therapy for CNS conditions and reproductive/sexual problems, as well as adjunct therapy for metabolic conditions. Likewise, approximately one fourth of students' responses changed significantly (2 units or more) for the question regarding their likelihood to recommend an herbal product for all conditions except as primary therapy for metabolic conditions.
Table 2.
Changes in Pharmacy Students' Responses on Part Two of a Survey Instrument Regarding Attitudes and Perceptions Toward Complementary and Alternative Medicine Administered After Completion of a Required Course, %
*Significant = ≥2 units
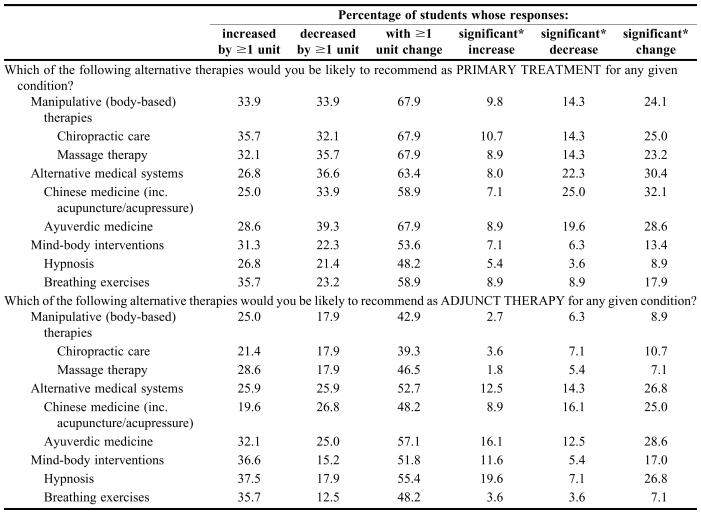
Table 3 shows the results of Part 3 of the survey instrument, which varied more greatly than the other 2 parts of the survey instrument. Over half of students changed their response concerning the likelihood that they would recommend all therapies as primary or adjunct therapy by at least 1 unit except manipulative (body-based) interventions as adjunct therapy. Those with a significant change ranged from 8.9% (manipulative interventions as adjunct therapy) to 30.4% (alternative medicine systems as adjunct therapy).
Table 3.
Changes in Pharmacy Students' Changes in Reponses Responses on Part Three of a Survey Instrument Regarding Attitudes and Perceptions Toward Complementary and Alternative Medicine Administered After Completion of a Required Course, %
*Significant = ≥2 units
DISCUSSION
The results of the student survey instrument revealed that a required course in complementary and alternative medicine changed a majority of students' attitudes and perceptions. In some cases, these changes were significant, from “strongly agree” or “strongly disagree” to a neutral response, or from “agree” to “disagree” (or vice versa). One of the instructor's goals for the course was to provide students with unbiased information that allowed them to form their own opinions on the topic. The fact that there was no clear pattern as to whether students' attitudes changed in a positive or negative direction is evidence that this goal was achieved. In addition, this demonstrates that students have the ability to formulate their own decisions when presented with conflicting information such as that available for complementary and alternative medicine.
Further evidence showing that course outcomes were met is available in the form of course evaluations, in which 90% of responding students either agreed or strongly agreed with the statement that that they had developed the ability to discuss the scope of complementary medicine practices, and 93.3% agreed or strongly disagreed that they had developed the ability to evaluate the information available on herbal/natural products and make sound recommendations as to their use. This is significant, due to both the recent inclusion of natural products on the NAPLEX, as well as the frequency with which practicing pharmacists are questioned about, and make recommendations regarding, complementary and alternative medicine. In light of the changes that occurred subsequent to this course, the question should be raised as to whether material similar to that offered in this course should be required in all PharmD curriculums, in order to better prepare graduating students for practice in which they will be expected to have some level of comfort with this topic.
Limitations
One obvious limitation of this study is that the students surveyed are just one group of PharmD students from one school of pharmacy, a majority of whom are from the same geographic region of the country. Therefore, these results can not necessarily be extrapolated to all PharmD programs. In addition, this study included only students in the first class who matriculated into South University's new PharmD program. Administering the same survey instruments to students in future classes who take this required course would be useful in determining its full impact.
Another limitation involves the amount and type of primary literature that is available on natural products and complementary and alternative medicine therapies. Results of trials can be conflicting at best, and trial designs are often questionable. On occasion there is nothing but anecdotal evidence for the use of a certain treatment modality or product. The paucity of well-designed clinical trials and the conflicting results of what does exist could certainly affect students' attitudes toward a product and their willingness to recommend it. In addition to this concern, the available material was presented by pharmacy students in their third-professional year. There is a possibility that the presentation and research skills of the student presenters may have had either positive or negative effects on the opinions of the students in the audience.
CONCLUSIONS
This study shows that the inclusion of complementary treatments as a required course in a doctor of pharmacy program will influence the recommendations that the students are willing to make to patients. In addition, since the subject of complementary medicine is a complex one with information for and against its use, students may be honing critical thinking skills that they will need throughout their pharmacy career.
Acknowledgments
We are grateful to Dr. Roy Parish, PharmD, BCPS, for his assistance in statistical analysis and manuscript preparation.
REFERENCES
- 1. Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. CDC Advance Data Report #343. 2004. Available at: http://www.cdc.gov/nchs/data/ad/ad343.pdf. Accessed June 23, 2005.
- 2.Kelly JP, Kaufman DW, Kelley K, Rosenberg L, Anderson TE, Mitchell AA. Recent trends in use of herbal and other natural products. Arch Intern Med. 2005;165:281–6. doi: 10.1001/archinte.165.3.281. [DOI] [PubMed] [Google Scholar]
- 3.Dolder C, Lacro J, Dolder N, Gregory P. Pharmacists' use of and attitudes and beliefs about alternative medicine. Am J Health-Syst Pharm. 2003;60:1352–7. doi: 10.1093/ajhp/60.13.1352. [DOI] [PubMed] [Google Scholar]
- 4.Welna EM, Hadsall RS, Schommer JC. Pharmacists' personal use, professional practice behaviors, and perceptions regarding herbal and other natural products. J Am Pharm Assoc. 2003;43:602–11. doi: 10.1331/154434503322452247. [DOI] [PubMed] [Google Scholar]
- 5.Howard N, Tsorurounis C, Kapusnik-Uner J. Dietary supplement survey of pharmacists: personal and professional practices. J Alt Comp Med. 2001;7:667–80. doi: 10.1089/10755530152755225. [DOI] [PubMed] [Google Scholar]
- 6.Shah B, Singanga W, Mallya U, Shah S. Pharmacy student perspectives on classroom education about herbal supplements. Am J Pharm Educ. 2005:69. Article 102. [Google Scholar]
- 7. National Association of Boards of Pharmacy. Updated NAPLEX Blueprint and New Passing Standard. Available at: http://www.nabp.net/ftpfiles/NABP01/Updatedblueprintinfo.pdf. Accessed January 20, 2006.
- 8.Shields KM, McQueen CE, Bryant PJ. Natural product education in schools of pharmacy in the United States. Am J Pharm Educ. 2003:67. Article 10. [Google Scholar]
- 9. ACPE Board of Directors. Draft Revision of ACPE Standards 2000 and Proposed Guidelines. June 2005. Available at: http://www.acpe-accredit.org/pdf/ACPEDraftRevisedStandardsandGuidelinesJune2005final.pdf. Accessed January 20, 2006.
- 10.Dutta AP, Miederhoff PA, Pyles MA. Complementary and alternative medicine education: students' perspectives. Am J Pharm Educ. 2003;67:1–7. [Google Scholar]