Abstract
Antigen capture enzyme-linked immunosorbent assay (ELISA) is one of the most useful methods to detect Ebola virus rapidly. We previously developed an antigen capture ELISA using a monoclonal antibody (MAb), 3-3D, which reacted not only to the nucleoprotein (NP) of Zaire Ebola virus (EBO-Z) but also to the NPs of Sudan (EBO-S) and Reston Ebola (EBO-R) viruses. In this study, we developed antigen capture ELISAs using two novel MAbs, Res2-6C8 and Res2-1D8, specific to the NP of EBO-R. Res2-6C8 and Res2-1D8 recognized epitopes consisting of 4 and 8 amino acid residues, respectively, near the C-terminal region of the EBO-R NP. The antigen capture ELISAs using these two MAbs detected the EBO-R NP in the tissues from EBO-R-infected cynomolgus macaques. The antigen capture ELISAs using Res2-6C8 and Res2-1D8 are useful for the rapid detection of the NP in EBO-R-infected cynomolgus macaques.
The family Filoviridae includes the genera Marburgvirus and Ebolavirus. The genus Ebolavirus has four species: Zaire Ebola virus (EBO-Z), Sudan Ebola virus (EBO-S), Côte-d'Ivoire Ebola virus (EBO-CI), and Reston Ebola virus (EBO-R) (6, 11, 13, 27, 34). Ebola virus has a negative-stranded RNA genome that encodes nucleoprotein (NP), P protein (VP35), matrix protein (VP40), glycoprotein (GP), an NP that influences the synthesis of viral mRNA (VP30), a protein associated with the membrane (VP24), and RNA-dependent RNA polymerase (L) (6, 26, 27, 34).
Cynomolgus macaques infected with EBO-R, which is thought to be endemic in the Philippines, were exported to the United States and Italy (2-4, 12, 16, 25, 30, 38). As with other species of Ebola virus, EBO-R causes fatal illness in nonhuman primates (7, 17), while symptomatic EBO-R infection has not been reported in humans (3, 4, 25, 38).
The origin in nature of Ebola virus remains a mystery; however, humans can be infected by close contact with patients (34, 36, 37). Rapid laboratory diagnosis of Ebola hemorrhagic fever is important for preventing the expansion of infection. Virus isolation (19, 23, 34), transmission electron microscopy (19, 23, 34), immunohistochemistry (39), reverse transcription-PCR (RT-PCR) (2, 21, 35), the fluorogenic 5′ nuclease assay (10), and antigen capture enzyme-linked immunosorbent assay (ELISA) (18, 29) have been used for the laboratory diagnosis of Ebola virus infection. Since the viral load in the blood reaches extremely high levels in Ebola virus infections (5, 7, 17, 31), the detection of Ebola antigens by antigen capture ELISA is suitable as a method of laboratory diagnosis (18, 29).
Monoclonal antibodies (MAbs) that discriminate Ebola virus species have been reported (28). However, an antigen capture ELISA that discriminates Ebola virus species has not been reported. In the present study, we developed antigen capture ELISAs using two novel MAbs to the NP specific to EBO-R. The ELISAs will be a useful tool for rapid discrimination of EBO-R infection from those by other Ebola virus species, especially in monkey quarantine or field studies.
MATERIALS AND METHODS
Cell culture.
P3/Ag568 was used as the parental cell line for hybridomas. The cells were maintained in RPMI 1640 (Gibco BRL, Rockville, Md.) supplemented with 10% fetal bovine serum and antibiotics (streptomycin and penicillin; Gibco BRL). Hypoxanthine-aminopterin-thymidine supplement (HAT) (Gibco BRL) was added to the medium for the selection of hybridomas according to the manufacturer's instructions. Hypoxanthine-thymidine supplement (HT) (Gibco BRL) was added to the medium to switch the medium from HAT to RPMI 1640.
Clinical specimens.
Livers (monkey no. 2882 and 2877), spleens (monkey no. 2877, 2882, and 2885), and sera (monkey no. 2866 and 2612), which were collected from EBO-R-infected cynomolgus macaques during the EBO-R outbreak in the Philippines in 1996 (14, 25) and kept frozen at −80C, were used in the study. EBO-R-NP antigens or genomic RNA were detected in these samples by antigen capture ELISA using 3-3D (29), immunohistochemistry (14), or RT-PCR using primers RES-Nf2 (5′-TGAGCTCCGGAAGAAGGACGGTGT-3′) and RES-Nr2 (5′-ACCATCATGTGTCCAACTGATTGC-3′). Five liver specimens and 79 serum specimens from EBO-R-noninfected cynomolgus macaques were used as the negative controls. Liver and spleen tissues were homogenized at approximately 10% (wt/vol) in phosphate-buffered saline (PBS) containing 0.05% Tween 20, 1% Triton X-100, and 5% nonfat milk (Triton-milk-PBS-T). After centrifugation at 15,800 × g for 10 min, the supernatants were used in the experiments. Sera were diluted with Triton-milk-PBS-T and used in the experiments.
Preparation of histidine-tagged Ebola virus rNPs (His-EBO-R-NP and His-EBO-Z-NP) for antigen capture ELISA.
Recombinant NPs (rNP) of EBO-R (His-EBO-R-NP) and EBO-Z (His-EBO-Z-NP) were prepared to be the antigens in antigen capture ELISA. The recombinant baculoviruses, which expressed His-EBO-R-NP (referred to as Ac [Autographa californica]-His-EBO-R-NP) or His-EBO-Z-NP (referred to as Ac-His-EBO-Z-NP), were produced as described previously (15, 33). Ac-His-EBO-R-NP or Ac-His-EBO-Z-NP was grown in Tn5 insect cells as reported previously (24). Tn5 cells infected with the recombinant baculoviruses were washed twice with PBS after 3 days of culture at 26°C and then incubated for 15 min in PBS containing 1% NP-40. After sonication for 1 min, the lysates were used in the experiments.
Preparation of MAbs.
MAbs were prepared as described previously (29). Briefly, BALB/c mice were subcutaneously immunized with His-EBO-R-NP together with Freund complete adjuvant (Becton Dickinson, Franklin Lakes, N.J.) and boosted subcutaneously three times with IMJECT-ALUM (Pierce, Rockford, Ill.) at 2-week intervals. Three days after the last immunization, the spleens were removed, and the spleen cells were fused with P3/Ag568 cells by using polyethylene glycol 4000 (catalog no. 4030-035; Gibco BRL) according to the manufacturer's instructions. The supernatants of the hybridoma cells were screened in an immunoglobulin G (IgG) ELISA (29) with His-EBO-R-NP as an antigen. Crude hybridomas were isolated from ELISA-positive wells, and the hybridoma clones were established by the limiting dilution method. MAbs were purified from the culture supernatants with a MAb Trap GII antibody purification kit (Amersham Pharmacia Biotech, Little Chalfont, United Kingdom) according to the manufacturer's instructions. The isotypes of the MAbs were determined with a mouse MAb isotyping kit from Gibco BRL.
Preparation of polyclonal antibodies.
Rabbit antisera to the glutathione S-transferase (GST)-tagged EBO-R NP C-terminal half (amino acids [aa] 360 to 739) (GST-EBO-R-ΔNP) (15) and to His-EBO-Z-NP (32, 33) were prepared as described previously. Briefly, rabbits were immunized four times subcutaneously with GST-EBO-R-ΔNP or His-EBO-Z-NP together with IMJECT-ALUM (Pierce). Serum was obtained 7 days after the last immunization.
IFA.
Indirect immunofluorescence assays (IFAs) using HeLa cells expressing the entire NPs of EBO-R or EBO-Z were performed as described previously (15, 32). IFA slides coated with Vero E6 cells infected with EBO-S and gamma irradiated were kindly supplied by the Centers for Disease Control and Prevention, Atlanta, Ga. The well of the slide was spotted with 20 μl of each MAb at a concentration of 100 ng/μl, and the slides were incubated under humidified conditions at 37°C for 1 h. After being washed with PBS, the slides were reacted with fluorescein isothiocyanate-conjugated goat anti-mouse IgG (H+L) antiserum (catalog no. 62-6511; Zymed Laboratories, Inc., South San Francisco, Calif.) at a dilution of 1:100. The slides were washed with PBS and examined for the staining pattern under a fluorescent microscope.
Epitope mapping with GST-truncated EBO-R rNP fusions.
A series of truncated EBO-R rNPs were prepared to determine the epitopes recognized by Res2-6C8 and Res2-1D8. Table 1 shows the primers used for the construction of the peptides. A truncated EBO-R NP corresponding to aa 631 to 739 was prepared as follows. PCR using the primers RES-N8F and RES-N8R (29) was performed to amplify the corresponding region of EBO-R cDNA. The PCR fragment was subcloned into a pGEX-2T vector (Amersham Pharmacia Biotech) to construct pGEX-ΔNP631-739. The insert sequences were confirmed to be identical to the originals. Then the GST-tagged truncated EBO-R NP was expressed in Escherichia coli (BL-21 strain) and purified by glutathione Sepharose 4B column chromatography according to the manufacturer's instructions (Amersham Pharmacia Biotech). PCR was also performed with the forward primers R635f, R636f, R637f, and R638f and a reverse primer, RES-N8R. As described above, each of the truncated EBO-R NPs corresponding to aa 635 to 739, 636 to 739, 637 to 739, and 638 to 739 was expressed and purified. The plasmids to express the truncated EBO-R NP corresponding to aa 631 to 638, 631 to 639, 631 to 640, 631 to 641, 631 to 642, and 631 to 643 were constructed by replacing a corresponding codon with a stop codon by site-directed mutagenesis of pGEX-ΔNP631-739 using the primer pairs Mu639f/Mu639r, Mu640f/Mu640r, Mu641f/Mu641r, Mu642f/Mu642r, Mu643f/Mu643r, and Mu644f/Mu644r according to the manufacturer's instructions (QuikChange site-directed mutagenesis kit; Stratagene, La Jolla, Calif.). Each of the truncated EBO-R NPs was expressed and purified as described above. Then, the reactivity of Res2-6C8 and Res2-1D8 to truncated EBO-R rNPs was examined by IgG ELISA.
TABLE 1.
Primers used for epitope mapping recognized by Res2-6C8 and Res2-1D8
| Primer | Sequence (5′ to 3′)a | Template of reaction |
|---|---|---|
| R635f | CAAGGATCCGAAGACCCTGATATC | pGEX-ΔNP631-739 |
| R636f | TTGGGATCCGACCCTGATATCGGTCAATC | cDNA of EBO-R |
| R637f | TTGAATGGATCCCCTGATATCGGT | pGEX-ΔNP631-739 |
| R638f | AATGAAGGATCCGATATCGGTCAA | pGEX-ΔNP631-739 |
| Mu639f | TGAAGACCCTGATTAAGGTCAATCAAAGT | pGEX-ΔNP631-739 |
| Mu639r | ACTTTGATTGACCTTAATCAGGGTCTTCA | pGEX-ΔNP631-739 |
| Mu640f | AGACCCTGATATCTAACAATCAAAGTCTA | pGEX-ΔNP631-739 |
| Mu640r | TAGACTTTGATTGTTAGATATCAGGGTCT | pGEX-ΔNP631-739 |
| Mu641f | CCCTGATATCGGTTAATCAAAGTCTATGC | pGEX-ΔNP631-739 |
| Mu641r | GCATAGACTTTGATTAACCGATATCAGGG | pGEX-ΔNP631-739 |
| Mu642f | TGATATCGGTCAATAAAAGTCTATGCAAA | pGEX-ΔNP631-739 |
| Mu642r | TTTGCATAGACTTTTATTGACCGATATCA | pGEX-ΔNP631-739 |
| Mu643f | TATCGGTCAATCATAATCTATGCAAAAAT | pGEX-ΔNP631-739 |
| Mu643r | ATTTTTGCATAGATTATGATTGACCGATA | pGEX-ΔNP631-739 |
| Mu644f | CGGTCAATCAAAGTAAATGCAAAAATTAG | pGEX-ΔNP631-739 |
| Mu644r | CTAATTTTTGCATTTACTTTGATTGACCG | pGEX-ΔNP631-739 |
BamHI restriction site is underlined. Introduced stop codon is in boldface.
Antigen capture ELISA.
Antigen capture ELISA was performed as described previously (29). Briefly, a microtiter plate (Becton Dickinson) was coated with purified MAbs (100 ng per well in 100 μl of PBS) overnight at 4°C. The three MAbs Res2-6C8, Res2-1D8, and 3-3D were used as the capture antibodies in the assay. MAb 3-3D was prepared against EBO-Z NP and was previously reported to detect the NPs of EBO-Z, EBO-R, and probably EBO-S in the antigen capture ELISA (29). After washing the plates three times with PBS containing 0.05% Tween 20 (PBS-T), 200 μl of PBS-T containing 5% nonfat milk (milk-PBS-T) was added to the wells for blocking for 1 h at 37°C. The milk-PBS-T was then removed, and 100 μl of the samples was added to the wells, which were then incubated for 1 h at 37°C. Triton-milk-PBS-T was used as the dilution buffer for the samples. After being washed three times with PBS-T, anti-GST-EBO-R-ΔNP rabbit serum and anti-His-EBO-Z-rNP rabbit serum at a dilution of 1:1,000 were added to the wells of the plates coated with the Res2-6C8 or Res2-1D8 and 3-3D, respectively. The plates were incubated for 1 h at 37°C and washed three times with PBS-T. Then, horseradish peroxidase-conjugated goat anti-rabbit IgG (H+L) antiserum (catalog no. 62-6120; Zymed Laboratories, Inc.) was added to the wells at a dilution of 1:1,000, and the plates were incubated for 1 h at 37°C. After being washed three times with PBS-T, 2,2′-azinobis[3-ethylbenziazoline-6-sulfonic acid] (ABTS) substrate (ABTS tablet and buffer; Roche Diagnostics, Mannheim, Germany) was added to the wells. The plates were then incubated for 30 min at room temperature, and the optical density at 405 nm (OD) was recorded.
In the antigen capture ELISAs using Res2-6C8, Res2-1D8, and 3-3D, the mean + 3 standard deviations (SDs) of OD of 79 sera from EBO-R-uninfected macaques were 0.11, 0.07, and 0.11, respectively, and those of 5 livers from EBO-R-uninfected macaques were 0.15, 0.08, and 0.15, respectively. Therefore, we defined the cutoff value as 0.2 in the assay.
RESULTS
Development of two MAbs specific to the EBO-R NP.
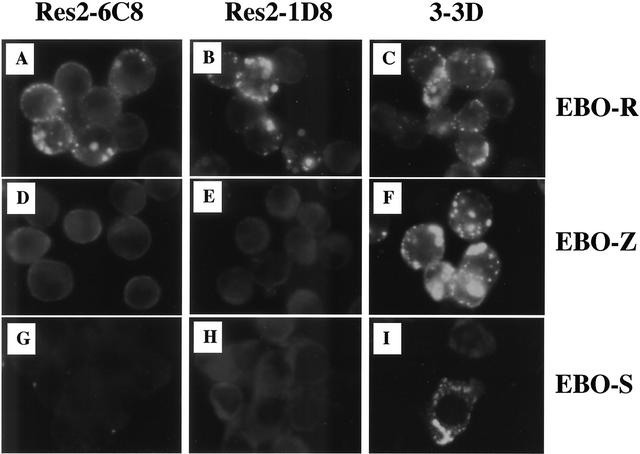
Thirty-two hybridoma clones secreting MAbs to EBO-R rNP were established, and the reactivities of these MAbs to His-EBO-R-NP were examined in the antigen capture ELISA format (data not shown). Two MAbs, Res2-6C8 and Res2-1D8, were reactive in the antigen capture ELISA format and were used in the present study. The isotypes of Res2-6C8 and Res2-1D8 were IgG2b and IgG1, respectively. Ebola virus species specificity of Res2-6C8 and Res2-1D8 was examined by IFA with HeLa cells that expressed the rNP of EBO-R or EBO-Z or by using Vero E6 cells infected with EBO-S. These two MAbs reacted to EBO-R NP (Fig. 1A and B), but not to EBO-Z NP (Fig. 1D and E) or EBO-S NP (Fig. 1G and H).
FIG. 1.
IFA using HeLa cells expressing rNP of EBO-R (A to C) or EBO-Z (D-F) and using Vero cells infected with EBO-S (G to I). The reactivities of Res2-6C8 (A, D, and G), Res2-1D8 (B, E, and H), and 3-3D (C, F, and I) to NP of EBO-R, EBO-Z, and EBO-S are shown. Res2-6C8 and Res2-1D8 reacted to EBO-R NP, but not to the NPs of EBO-Z and EBO-S. The MAb 3-3D reacts to the NPs of all three Ebola virus species.
Epitopes recognized by Res2-6C8 and Res2-1D8.
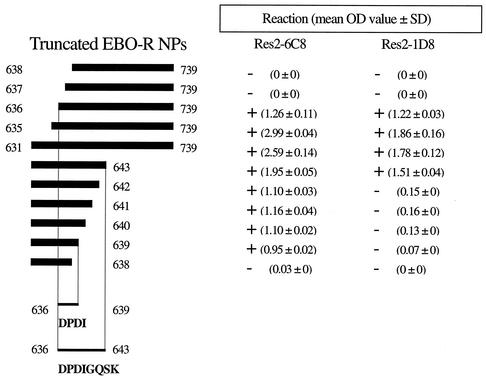
The epitopes recognized by Res2-6C8 and Res2-1D8 were determined by IgG ELISAs using the truncated EBO-R rNPs (Fig. 2). Res2-6C8 and Res2-1D8 recognized the amino acid residues between aa 631 and 739, and the minimum epitopes were further determined. Res2-6C8 reacted to the truncated EBO-R rNPs corresponding to aa 636 to 739 and 631 to 639, but not to aa 637 to 739 and 631 to 638. On the other hand, Res2-1D8 reacted to the truncated EBO-R NP corresponding to aa 636 to 739 and 631 to 643, but not to aa 637 to 739 and 631 to 642. These results showed that the epitopes recognized by Res2-6C8 and Res2-1D8 were aa 636 to 639 (4 aa residues, 636DPDI639) and aa 636 to 643 (8 aa residues, 636DPDIGQSK643) of EBO-R NP, respectively. The amino acid sequences of the epitopes were aligned to that of EBO-R Pennsylvania isolate in 1989 to 1990, EBO-Z, and EBO-S. The 8 aa residues were identical to those of the EBO-R Pennsylvania isolate in 1989 to 1990 (Table 2). The amino acid sequences of EBO-Z and EBO-S NPs corresponding to the amino acids of EBO-R, 636DPDIGQSK643, were NQDSDNTQ and EALPINSK, respectively (Table 2).
FIG. 2.
Reactivities of Res2-6C8 and Res2-1D8 to the truncated EBO-R rNPs in IgG ELISA. Res2-6C8 recognizes the amino acid residues between aa 636 and 639 (sequence, DPDI). Res2-1D8 recognizes the amino acid residues between aa 636 and 643 (sequence, DPDIGQSK). The mean OD value ± SD in the IgG ELISA is shown.
TABLE 2.
Comparison of the epitopes of Res2-6C8 and Res2-1D8
| Ebola virus speciesa | Amino acids corresponding to epitope of:
|
|
|---|---|---|
| Res2-6C8 | Res2-1D8 | |
| EBO-R, 1996 | 636DPDI639 | 636DPDIGQSK643 |
| EBO-R, 1989/1990 | 636DPDI639 | 636DPDIGQSK643 |
| EBO-Z, 1976 | 636NQDS639 | 636NQDSDNTQ643 |
| EBO-S, 1976 | 636EALP639 | 636EALPINSK643 |
Development of the antigen capture ELISAs using these novel MAbs.
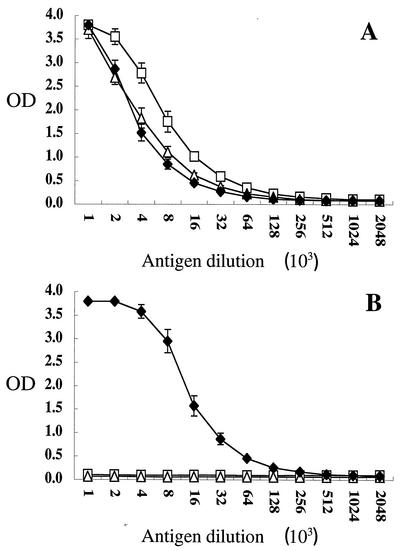
The sensitivity of the antigen capture ELISAs prepared with these two MAbs was tested. As shown in Fig. 3A, Res2-6C8 and Res2-1D8 detected His-EBO-R-NP up to dilutions of 1:128,000 and 1:64,000 in the antigen capture ELISA, respectively. The ELISA prepared with 3-3D detected His-EBO-R-NP up to the dilution of 1:32,000. As expected, Res2-6C8 and Res2-1D8 did not detect His-EBO-Z-NP in the antigen capture ELISA (Fig. 3B).
FIG. 3.
Reactivity of MAbs Res2-6C8 (□), Res2-1D8 (▵), and 3-3D (♦) to the rNPs of EBO-R and EBO-Z in the antigen capture ELISA. His-EBO-R-NP (A) and His-EBO-Z-NP (B) were used as antigens. The mean ± SD of four assays is shown.
Detection of EBO-R NP in the specimens from EBO-R-infected monkeys.
Serum, liver, and spleen specimens from EBO-R-infected macaques were examined for the presence of EBO-R NP by antigen capture ELISAs using Res2-6C8, Res2-1D8, and 3-3D. Res2-6C8 and Res2-1D8 detected the EBO-R NP antigens in the sera, livers, and spleens (Table 3). Res2-6C8 detected the NP in all of the samples, while Res2-1D8 and 3-3D detected the NP in six of seven and five of seven samples, respectively. The endpoint titers were higher in the ELISAs using Res2-6C8 and Res2-1D8 than in the ELISA using 3-3D.
TABLE 3.
Detection of EBO-R NP from clinical specimens
| Sample | Monkey no. | Titer by antigen capture ELISAa
|
Result by:
|
|||
|---|---|---|---|---|---|---|
| Res2-6C8 | Res2-1D8 | 3-3Db | RT-PCRc | IHCd | ||
| Serum | 2612 | 160 | 40 | 20 | + | + |
| 2866 | 320 | 320 | 160 | + | ND | |
| Liver | 2877 | 40 | <10 | 10 | NDe | ND |
| 2882 | 160 | 40 | 40 | + | + | |
| Spleen | 2877 | 320 | 160 | 80 | ND | ND |
| 2882 | 80 | 20 | <10 | ND | + | |
| 2885 | 160 | 40 | <10 | + | ND | |
Antigen titer in the specimens. The antigen titer in the ELISA was determined as the reciprocal of the highest dilution showing a positive reaction. The titer was determined by a single test. The cutoff OD value was 0.2.
Ebola virus species cross-reactive MAb (29).
RT-PCR with primers RES-Nf2 and RES-Nr2.
IHC, immunohistochemistry for the detection of Ebola virus NP (14).
ND, not done.
DISCUSSION
We previously established an antigen capture ELISA using the MAb 3-3D, which reacted to the NPs of EBO-Z, EBO-S, and EBO-R (29). The minimum epitope recognized by MAb 3-3D was mapped on 26 aa residues between aa 648 and 673 at the C-terminal region of the EBO-Z NP (29), and the amino acid residues between aa 631 and 739 and aa 633 and 738 were required for the cross-reaction to EBO-R NP and EBO-S NP, respectively (29). In the present study, we developed two novel MAbs to EBO-R NP, Res2-6C8 and Res2-1D8, which detected EBO-R NP with high sensitivity and specificity in the antigen capture ELISA format. The minimum epitopes recognized by Res2-6C8 and Res2-1D8 were found to be 636DPDI639 and 636DPDIGQSK643, respectively (Fig. 2). The amino acid sequence of EBO-R NP, 636DPDIGQSK643, was different from those of EBO-Z and EBO-S NP (Table 2). This is consistent with the result in which the two MAbs did not react to the NP of EBO-Z and EBO-S in the IFA (Fig. 1D, E, G, and H). The amino acid sequences of the epitopes recognized by the two MAbs were identical to those of EBO-R Pennsylvania isolate in 1989 to 1990 (Table 2) (11, 13). Considering the genetic stability among EBO-R isolates (11, 13), it is expected that antigen capture ELISA systems using Res2-6C8 and Res2-1D8 detect either EBO-R strain.
We determined the cutoff value in the antigen capture ELISA based on the mean OD value + 3 SDs of 79 sera and 5 liver specimens from EBO-R-uninfected cynomolgus macaques. Since the mean OD value + 3 SDs was lower than 0.2 in any specimen, the cutoff value was determined to be 0.2 in the present study. The sensitivity of the antigen capture ELISA using either Res2-6C8 or Res2-1D8 for His-EBO-R-NP was similar to that using 3-3D (Fig. 3A). On the other hand, His-EBO-Z-NP was not detected in the antigen capture ELISAs using Res2-6C8 and Res2-1D8 (Fig. 3B), as expected from the results in the IFA and the epitope sequences, demonstrating that the antigen capture ELISAs using Res2-6C8 and Res2-1D8 were specific to EBO-R.
Authentic EBO-R NP in the serum, liver, and spleen specimens from the macaques naturally infected with EBO-R was detected by the antigen capture ELISAs using the Res2-6C8, Res2-1D8, and 3-3D MAbs (Table 3). The sensitivity of the ELISA in detecting the authentic EBO-R NP was higher with Res2-6C8 and Res2-1D8 than with 3-3D. Since the clinical specimens used in this study were stored for 6 years, it is possible that the EBO-R NP was somewhat degraded and was detected with higher sensitivity by Res2-6C8, which recognizes 4 aa of the NP, than by 3-3D, which recognizes 109 aa. The results, nevertheless, indicated that both Res2-6C8 and Res2-1D8 were highly sensitive in detecting EBO-R NP in clinical specimens.
An outbreak of EBO-CI occurred among a troop of chimpanzees in the Taì National Park, Ivory Coast, in 1994 (20). It was also reported that Ebola hemorrhagic fever patients had been infected with Ebola virus while butchering dead chimpanzees in the first outbreak in Gabon during 1996 (1, 8, 9). Fatal infection with EBO-Z, EBO-S, EBO-CI, and EBO-R was also demonstrated in cynomolgus macaques (7). EBO-R caused outbreaks among cynomolgus macaques in the Philippines (2-4, 12, 16, 25, 30, 38) and is most likely to cause epizootics among Asian macaques. Since EBO-R has never caused symptomatic infection in humans (3, 4, 25, 38), rapid differentiation of the species of Ebola virus is crucial, especially when samples from nonhuman primates are tested. Although RT-PCR has higher sensitivity to Ebola virus than the antigen capture ELISA, the sequencing of the PCR products is essential for confirming Ebola virus infection (21-23, 30, 34, 35). The viral load in the blood and other organs has been shown to reach extremely high levels in Ebola virus-infected animals (5, 7, 17, 31). Thus, the newly developed antigen capture ELISAs using Res2-6C8 and Res2-1D8 might be a promising tool for the diagnosis of EBO-R infection, especially in monkey quarantine and field studies.
Acknowledgments
We gratefully acknowledge M. Ogata of the National Institute of Infectious Diseases and the staff of the Research Institute for Tropical Medicine for technical assistance.
This work was partly supported by a grant from the Ministry of Health, Labour, and Welfare, Japan.
REFERENCES
- 1.Baize, S., E. M. Leroy, M. C. Georges-Courbot, M. Capron, J. Lansoud-Soukate, P. Debre, S. P. Fisher-Hoch, J. B. McCormick, and A. J. Georges. 1999. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat. Med. 5:423-426. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 1996. Ebola-Reston virus infection among quarantined nonhuman primates—Texas, 1996. Morb. Mortal. Wkly. Rep. 45:314-316. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 1990. Epidemiologic notes and reports updates: filovirus infection in animal handlers. Morb. Mortal. Wkly. Rep. 39:221. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 1990. Update: filovirus infections among persons with occupational exposure to nonhuman primates. Morb. Mortal. Wkly. Rep. 39:266-273. [PubMed] [Google Scholar]
- 5.Connolly, B. M., K. E. Steele, K. J. Davis, T. W. Geisbert, W. M. Kell, N. K. Jaax, and P. B. Jahrling. 1999. Pathogenesis of experimental Ebola virus infection in guinea pigs. J. Infect. Dis. 179(Suppl. 1):S203-S217. [DOI] [PubMed] [Google Scholar]
- 6.Feldmann, H., H. D. Klenk, and A. Sanchez. 1993. Molecular biology and evolution of filoviruses. Arch. Virol. 7(Suppl.):S81-S100. [DOI] [PubMed] [Google Scholar]
- 7.Fisher-Hoch, S. P., T. L. Brammer, S. G. Trappier, L. C. Hutwagner, B. B. Farrar, S. L. Ruo, B. G. Brown, L. M. Hermann, G. I. Perez-Oronoz, C. S. Goldsmith, M. A. Hanes, and J. B. McCormick. 1992. Pathogenic potential of filoviruses: role of geographic origin of primate host and virus strain. J. Infect. Dis. 166:753-763. [DOI] [PubMed] [Google Scholar]
- 8.Georges, A. J., E. M. Leroy, A. A. Renaut, C. T. Benissan, R. J. Nabias, M. T. Ngoc, P. I. Obiang, J. P. Lepage, E. J. Bertherat, D. D. Benoni, E. J. Wickings, J. P. Amblard, J. M. Lansoud-Soukate, J. M. Milleliri, S. Baize, and M. C. Georges-Courbot. 1999. Ebola hemorrhagic fever outbreaks in Gabon, 1994-1997: epidemiologic and health control issues. J. Infect. Dis. 179(Suppl. 1):S65-S75. [DOI] [PubMed] [Google Scholar]
- 9.Georges-Courbot, M. C., A. Sanchez, C. Y. Lu, S. Baize, E. Leroy, J. Lansout-Soukate, C. Tevi-Benissan, A. J. Georges, S. G. Trappier, S. R. Zaki, R. Swanepoel, P. A. Leman, P. E. Rollin, C. J. Peters, S. T. Nichol, and T. G. Ksiazek. 1997. Isolation and phylogenetic characterization of Ebola viruses causing different outbreaks in Gabon. Emerg. Infect. Dis. 3:59-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibb, T. R., D. A. Norwood, Jr., N. Woollen, and E. A. Henchal. 2001. Development and evaluation of a fluorogenic 5′ nuclease assay to detect and differentiate between Ebola virus subtypes Zaire and Sudan. J. Clin. Microbiol. 39:4125-4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Groseth, A., U. Stroher, S. Theriault, and H. Feldmann. 2002. Molecular characterization of an isolate from the 1989/90 epizootic of Ebola virus Reston among macaques imported into the United States. Virus Res. 87:155. [DOI] [PubMed] [Google Scholar]
- 12.Hayes, C. G., J. P. Burans, T. G. Ksiazek, R. A. Del Rosario, M. E. Miranda, C. R. Manaloto, A. B. Barrientos, C. G. Robles, M. M. Dayrit, and C. J. Peters. 1992. Outbreak of fatal illness among captive macaques in the Philippines caused by an Ebola-related filovirus. Am. J. Trop. Med. Hyg. 46:664-671. [DOI] [PubMed] [Google Scholar]
- 13.Ikegami, T., A. B. Calaor, M. E. Miranda, M. Niikura, M. Saijo, I. Kurane, Y. Yoshikawa, and S. Morikawa. 2001. Genome structure of Ebola virus subtype Reston: differences among Ebola subtypes. Arch. Virol. 146:2021-2027. [DOI] [PubMed] [Google Scholar]
- 14.Ikegami, T., M. E. Miranda, A. B. Calaor, D. L. Manalo, N. J. Miranda, M. Niikura, M. Saijo, Y. Une, Y. Nomura, I. Kurane, T. G. Ksiazek, Y. Yoshikawa, and S. Morikawa. 2002. Histopathology of natural Ebola virus subtype Reston infection in cynomolgus macaques during the Philippine outbreak in 1996. Exp. Anim. 51:447-455. [DOI] [PubMed] [Google Scholar]
- 15.Ikegami, T., M. Saijo, M. Niikura, M. E. Miranda, A. B. Calaor, M. Hernandez, D. L. Manalo, I. Kurane, Y. Yoshikawa, and S. Morikawa. 2002. Development of an immunofluorescence method for the detection of antibodies to Ebola virus subtype Reston by the use of recombinant nucleoprotein-expressing HeLa cells. Microbiol. Immunol. 46:633-638. [DOI] [PubMed] [Google Scholar]
- 16.Jahrling, P. B., T. W. Geisbert, D. W. Dalgard, E. D. Johnson, T. G. Ksiazek, W. C. Hall, and C. J. Peters. 1990. Preliminary report: isolation of Ebola virus from monkeys imported to USA. Lancet 335:502-505. [DOI] [PubMed] [Google Scholar]
- 17.Jahrling, P. B., T. W. Geisbert, N. K. Jaax, M. A. Hanes, T. G. Ksiazek, and C. J. Peters. 1996. Experimental infection of cynomolgus macaques with Ebola-Reston filoviruses from the 1989-1990 U.S. epizootic. Arch. Virol. 11(Suppl.):S115-S134. [DOI] [PubMed] [Google Scholar]
- 18.Ksiazek, T. G., P. E. Rollin, P. B. Jahrling, E. Johnson, D. W. Dalgard, and C. J. Peters. 1992. Enzyme immunosorbent assay for Ebola virus antigens in tissues of infected primates. J. Clin. Microbiol. 30:947-950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ksiazek, T. G., P. E. Rollin, A. J. Williams, D. S. Bressler, M. L. Martin, R. Swanepoel, F. J. Burt, P. A. Leman, A. S. Khan, A. K. Rowe, R. Mukunu, A. Sanchez, and C. J. Peters. 1999. Clinical virology of Ebola hemorrhagic fever (EHF): virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J. Infect. Dis. 179(Suppl. 1):S177-S187. [DOI] [PubMed] [Google Scholar]
- 20.Le Guenno, B., P. Formentry, M. Wyers, P. Gounon, F. Walker, and C. Boesch. 1995. Isolation and partial characterization of a new strain of Ebola virus. Lancet 345:1271-1274. [DOI] [PubMed] [Google Scholar]
- 21.Leroy, E. M., S. Baize, C. Y. Lu, J. B. McCormick, A. J. Georges, M. C. Georges-Courbot, J. Lansoud-Soukate, and S. P. Fisher-Hoch. 2000. Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting. J. Med. Virol. 60:463-467. [PubMed] [Google Scholar]
- 22.Leroy, E. M., S. Baize, V. E. Volchkov, S. P. Fisher-Hoch, M. C. Georges-Courbot, J. Lansoud-Soukate, M. Capron, P. Debre, J. B. McCormick, and A. J. Georges. 2000. Human asymptomatic Ebola infection and strong inflammatory response. Lancet 355:2210-2215. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd, E. S., S. R. Zaki, P. E. Rollin, K. Tshioko, M. A. Bwaka, T. G. Ksiazek, P. Calain, W. J. Shieh, M. K. Konde, E. Verchueren, H. N. Perry, L. Manguindula, J. Kabwau, R. Ndambi, and C. J. Peters. 1999. Long-term disease surveillance in Bandundu region, Democratic Republic of the Congo: a model for early detection and prevention of Ebola hemorrhagic fever. J. Infect. Dis. 179(Suppl. 1):S274-S280. [DOI] [PubMed] [Google Scholar]
- 24.Matsuura, Y., R. D. Possee, H. A. Overton, and D. H. Bishop. 1987. Baculovirus expression vectors: the requirements for high level expression of proteins, including glycoproteins. J. Gen. Virol. 68:1233-1250. [DOI] [PubMed] [Google Scholar]
- 25.Miranda, M. E., T. G. Ksiazek, T. J. Retuya, A. S. Khan, A. Sanchez, C. F. Fulhorst, P. E. Rollin, A. B. Calaor, D. L. Manalo, M. C. Roces, M. M. Dayrit, and C. J. Peters. 1999. Epidemiology of Ebola (subtype Reston) virus in the Philippines, 1996. J. Infect. Dis. 179(Suppl. 1):S115-S119. [DOI] [PubMed] [Google Scholar]
- 26.Mühlberger, E., M. Weik, V. E. Volchkov, H. D. Klenk, and S. Becker. 1999. Comparison of the transcription and replication strategies of Marburg virus and Ebola virus by using artificial replication systems. J. Virol. 73:2333-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Netesov, S. V., H. Feldmann, P. B. Jahrling, H.-D. Klenk, and A. Sanchez. 2002. Family Filoviridae, p. 539-548. In M. H. V. van Regenmortel, C. M. Fauquet, D. H. L. Bishop, E. B. Carstens, M. K. Estes, S. M. Lemon, J. Maniloff, M. A. Mayo, D. J. McGeoch, C. R. Pringle, and R. B. Wickner (ed.), Virus taxonomy. The Seventh Report of the International Committee on Taxonomy of Viruses. Academic Press, San Diego, Calif.
- 28.Niikura, M., T. Ikegami, M. Saijo, T. Kurata, I. Kurane, and S. Morikawa. 2003. Analysis of linear B-cell epitopes of the nucleoprotein of Ebola virus that distinguish Ebola virus subtypes. Clin. Diagn. Lab. Immunol. 10:83-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niikura, M., T. Ikegami, M. Saijo, I. Kurane, M. E. Miranda, and S. Morikawa. 2001. Detection of Ebola viral antigen by enzyme-linked immunosorbent assay using a novel monoclonal antibody to nucleoprotein. J. Clin. Microbiol. 39:3267-3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rollin, P. E., R. J. Williams, D. S. Bressler, S. Pearson, M. Cottingham, G. Pucak, A. Sanchez, S. G. Trappier, R. L. Peters, P. W. Greer, S. Zaki, T. Demarcus, K. Hendricks, M. Kelley, D. Simpson, T. W. Geisbert, P. B. Jahrling, C. J. Peters, and T. G. Ksiazek. 1999. Ebola (subtype Reston) virus among quarantined nonhuman primates recently imported from the Philippines to United States. J. Infect. Dis. 179(Suppl. 1):S108-S114. [DOI] [PubMed] [Google Scholar]
- 31.Ryabchikova, E. I., L. V. Kolesnikova, and S. V. Luchko. 1999. An analysis of features of pathogenesis in two animal models of Ebola virus infection. J. Infect. Dis. 179(Suppl. 1):S199-S202. [DOI] [PubMed] [Google Scholar]
- 32.Saijo, M., M. Niikura, S. Morikawa, and I. Kurane. 2001. Immunofluorescence method for detection of Ebola virus immunogloblin G, using HeLa cells which express recombinant nucleoprotein. J. Clin. Microbiol. 39:776-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saijo, M., M. Niikura, S. Morikawa, T. G. Ksiazek, R. F. Meyer, C. J. Peters, and I. Kurane. 2001. Enzyme-linked immunosorbent assays for detection of antibodies to Ebola and Marburg viruses using recombinant nucleoproteins. J. Clin. Microbiol. 39:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanchez, A., A. S. Khan, S. R. Zaki, G. J. Nabel, T. G. Ksiazek, and C. J. Peters. 2001. Filoviridae: Marburg and Ebola viruses, p. 1279-1304. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott, Williams & Wilkins, Philadelphia, Pa.
- 35.Sanchez, A., T. G. Ksiazek, P. E. Rollin, M. E. Miranda, S. G. Trappier, A. S. Khan, C. J. Peters, and S. T. Nichol. 1999. Detection and molecular characterization of Ebola viruses causing disease in human and nonhuman primates. J. Infect. Dis. 179(Suppl. 1):S164-S169. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. 1976. Ebola haemorrhagic fever in Sudan, 1976. Bull. W. H. O. 56:247-270. [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. 1978. Ebola haemorrhagic fever in Zaire, 1976. Report of an international commission. Bull. W. H. O. 56:271-293. [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization. 1992. Viral haemorrhagic fever in imported monkeys. Wkly. Epidemiol. Rec. 67:142-143. [PubMed] [Google Scholar]
- 39.Zaki, S. R., W. J. Shieh, P. W. Greer, C. S. Goldsmith, T. Ferebee, J. Katshitshi, F. K. Tshioko, M. A. Bwaka, R. Swanepoel, P. Calain, A. S. Khan, E. Lloyd, P. E. Rollin, T. G. Ksiazek, and C. J. Peters. 1999. A novel immunohistochemical assay for the detection of Ebola virus in skin: implications for diagnosis, spread, and surveillance of Ebola hemorrhagic fever. J. Infect. Dis. 179(Suppl. 1):S36-S47. [DOI] [PubMed] [Google Scholar]