Abstract
The role of gastrointestinal hormones in the regulation of appetite is reviewed. The gastrointestinal tract is the largest endocrine organ in the body. Gut hormones function to optimize the process of digestion and absorption of nutrients by the gut. In this capacity, their local effects on gastrointestinal motility and secretion have been well characterized. By altering the rate at which nutrients are delivered to compartments of the alimentary canal, the control of food intake arguably constitutes another point at which intervention may promote efficient digestion and nutrient uptake. In recent decades, gut hormones have come to occupy a central place in the complex neuroendocrine interactions that underlie the regulation of energy balance.
Many gut peptides have been shown to influence energy intake. The most well studied in this regard are cholecystokinin (CCK), pancreatic polypeptide, peptide YY, glucagon-like peptide-1 (GLP-1), oxyntomodulin and ghrelin. With the exception of ghrelin, these hormones act to increase satiety and decrease food intake. The mechanisms by which gut hormones modify feeding are the subject of ongoing investigation.
Local effects such as the inhibition of gastric emptying might contribute to the decrease in energy intake. Activation of mechanoreceptors as a result of gastric distension may inhibit further food intake via neural reflex arcs. Circulating gut hormones have also been shown to act directly on neurons in hypothalamic and brainstem centres of appetite control. The median eminence and area postrema are characterized by a deficiency of the blood–brain barrier. Some investigators argue that this renders neighbouring structures, such as the arcuate nucleus of the hypothalamus and the nucleus of the tractus solitarius in the brainstem, susceptible to influence by circulating factors. Extensive reciprocal connections exist between these areas and the hypothalamic paraventricular nucleus and other energy-regulating centres of the central nervous system. In this way, hormonal signals from the gut may be translated into the subjective sensation of satiety. Moreover, the importance of the brain–gut axis in the control of food intake is reflected in the dual role exhibited by many gut peptides as both hormones and neurotransmitters. Peptides such as CCK and GLP-1 are expressed in neurons projecting both into and out of areas of the central nervous system critical to energy balance.
The global increase in the incidence of obesity and the associated burden of morbidity has imparted greater urgency to understanding the processes of appetite control. Appetite regulation offers an integrated model of a brain–gut axis comprising both endocrine and neurological systems. As physiological mediators of satiety, gut hormones offer an attractive therapeutic target in the treatment of obesity.
Keywords: pancreatic polypeptide, peptide YY, ghrelin, glucagon-like peptide 1, oxyntomodulin, cholecystokinin
1. Introduction
It was with the discovery of gut hormones a century ago that the field of endocrinology was born. It is therefore fitting that in the last decade or so, gut peptides have taken on an increasingly central role in one of the most pressing public health problems facing the world today, namely that of obesity. The brain–gut axis provides a means by which the gastrointestinal tract signals energy status to the brain. In this review, we shall describe the key part played by gastrointestinal hormones in regulating energy intake.
2. Historical perspectives
For centuries, Western medical thought was dominated by the doctrine of the humours, and the gut, in particular, was accorded a central role. However, it was not until the early twentieth century that the notion of circulating regulators of gut function was set onto a more sound experimental footing with the work of Bayliss & Starling (1902). They demonstrated that infusion of an acidic solution into a denervated loop of jejunum stimulated pancreatic secretion, whereas intravenous acid did not. Moreover, intravenous injection of an extract of duodenal mucosa reproduced this effect. The putative agent responsible was named ‘secretin’ and conferred upon its discoverers the distinction of founding a novel branch of physiology. The advent of the 1960s saw the application of a number of novel techniques to the field and rapid progress flowed from the successive isolation, purification and measurement in the plasma of secretin, gastrin and other gut hormones (Lin & Chey 2003; Dockray 2004; Rehfeld 2004).
The gastro-entero-pancreatic system is now regarded as the largest endocrine organ in the body, and the range of identified hormones secreted by the gut is extensive (see table 1). The primary function of the gut is, of course, the digestion and absorption of nutrients. The gut neuroendocrine system, and at a higher level, the brain–gut axis, functions to optimize this process. The regulation of appetite, and therefore the regulation of the delivery of nutrients to various gut compartments, may be regarded as another facet of this. Many gut hormones therefore alter food intake directly and indirectly, the majority acting to reduce food intake and limit meal size.
Table 1.
Overview of the major gut hormones. (CCK, cholecystokinin; CNS, central nervous system; GH, growth hormone; GIP, glucose-dependent insulinotropic polypeptide; GLP-1 and -2, glucagon-like peptides-1 and -2; GRP, gastrin-releasing polypeptide; ICV, intracerebroventricular; PHI, peptide histidine isoleucine; PHV, peptide histidine valine; PP, pancreatic polypeptide; PYY, peptide YY; OXM, oxyntomodulin.)
| peptide | primary sites of synthesis | major actions | important references |
|---|---|---|---|
| CCK | I-cells of duodenum, jejunum; widespread CNS expression | promotes gallbladder contraction | Gibbs et al. (1973), Kissileff et al. (1981) |
| increases secretion of pancreatic enzymes and bicarbonate | |||
| inhibits gastric acid secretion | |||
| slows gastric emptying | |||
| reduces food intake | |||
| gastrin | G-cells of gastric antrum | increases gastric acid | Conover et al. (1989) |
| promotes gastric epithelial cell proliferation | |||
| no known effect on food intake | |||
| ghrelin | A-cells of gastric fundus; small and large intestine; hypothalamic nuclei | promotes release of GH and other pituitary hormones | Tschop et al. (2000), Wren et al. (2001a) |
| increases food intake | |||
| promotes gastric motility | |||
| promotes PP release | |||
| inotropic effect on heart | |||
| vasodilatation | |||
| GIP | K-cells of duodenum and jejunum | incretin effect on insulin secretion | Woods et al. (1981), Meier et al. (2002), Holst (2004) |
| increases fatty acid synthesis in adipose tissue | |||
| enterogastrone effect | |||
| diminishes intestinal motility | |||
| increases mesenteric blood flow | |||
| effects on food intake unknown—fourth ventricle administration has no effect | |||
| GLP-1 | L-cells of distal small and large intestine; immunoreactivity in hypothalamus, dorsovagal complex, pituitary | incretin effect on insulin secretion | Turton et al. (1996), Meeran et al. (1999), Edwards et al. (2001), Tang-Christensen et al. (2001), Verdich et al. (2001a), Baggio et al. (2004) |
| suppresses glucagon release | |||
| promotes pancreatic β-cell growth | |||
| inhibits gastric emptying | |||
| inhibits gastric secretion | |||
| inhibits energy intake | |||
| effects on cardiovascular system | |||
| GLP-2 | L-cells of distal small and large intestine; immunoreactivity in hypothalamus, dorsovagal complex, pituitary | promotes tissue repair and intestinal mucosal growth | Tang-Christensen et al. (2000), Schmidt et al. (2003) |
| enhances digestive and absorptive capacities of intestine | |||
| inhibits gastric secretion | |||
| inhibits feeding when administered centrally; no effect of peripheral administration | |||
| motilin | proximal small intestine; some reports of immunoreactivity in CNS | prokinetic action on gut, mediates migrating motor complexes | Olson et al. (1980), Garthwaite (1985), Asakawa et al. (1998) |
| stimulates gallbladder contraction | |||
| promotes enzyme secretion in stomach and pancreas | |||
| stimulates PP release | |||
| effects on food intake equivocal | |||
| oxyntomodulin | L-cells of distal small and large intestine; immunoreactivity in hypothalamus, dorsovagal complex, pituitary | inhibits gastric acid production | Dakin et al. (2001), Dakin et al. (2002), Cohen et al. (2003), Wynne et al. (2005b) |
| reduces gastric motility | |||
| role as incretin equivocal | |||
| inhibits food intake | |||
| PHI/PHV | gastrointestinal tract; heart; lungs; kidney; central and peripheral nervous systems | main physiological effects unclear | Olszewski et al. (2003) |
| PHI-injected ICV inhibits feeding | |||
| PP | pancreatic islets of Langerhans; some reports of expression in hypothalamus, pineal gland, pituitary, substantia nigra, hippocampus | relaxation of gallbladder | Batterham et al. (2003b) |
| inhibition of pancreatic exocrine secretion | |||
| equivocal effect on gastric emptying | |||
| inhibits food intake | |||
| PYY3-36 | L-cells of distal small and large intestine; immunoreactivity in hypothalamus, medulla, pons | inhibits food intake | Batterham et al. (2002), Batterham et al. (2003a) |
| inhibits gallbladder secretion | |||
| reduces gut motility | |||
| inhibits pancreatic secretion | |||
| enterogastrone effect | |||
| secretin | S-cells of the duodenum | stimulates pancreatic exocrine secretions | Conover et al. (1989) |
| inhibits gastric secretion | |||
| promotes PP secretion | |||
| no known effect on food intake | |||
| somatostatin | multiple organ systems, notably the D-cells of the gut and pancreas; hypothalamus | multiple actions across numerous organ systems | Lotter et al. (1981), Levine & Morley (1982), Morley et al. (1983) |
| inhibits gastric secretions | |||
| reduces gut motility | |||
| inhibits release of numerous other gut hormones, including insulin, glucagon, CCK, gastrin, OXM, PP | |||
| reduces food intake when administered peripherally—physiological importance of this effect unclear |
3. Central nervous system appetite circuits
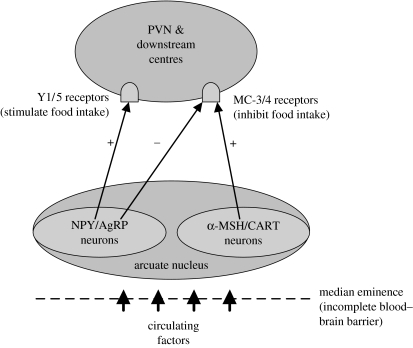
It is now recognized that these peptides act as true endocrine hormones and exert effects at distant target organs. In particular, in the context of food intake, many gut hormones act on hypothalamic and brainstem centres of appetite control. This provides one means by which the gut may signal energy status to the seat of satiety, the central nervous system (CNS). These CNS neuronal circuits are reviewed in greater detail elsewhere in this issue, but, briefly, the arcuate nucleus (ARC) acts as the site of integration of a number of neurological and blood-borne signals, due to its privileged location near the median eminence. This latter region lacks a complete blood–brain barrier (Peruzzo et al. 2000), and therefore some investigators have argued that the ARC is rendered susceptible to influence by circulating factors (Cone et al. 2001). Circulating factors modify the activity of two populations of neuron within the ARC. One population co-expresses cocaine- and amphetamine-related transcript (CART) and proopiomelanocortin (POMC) and inhibits food intake. Among the products of cleavage of POMC is α-melanocyte-stimulating hormone, which is a ligand for the melanocortin-4 receptor. The importance of the melanocortin system in the mediation of food intake is illustrated by the observation that up to 6% of monogenetic obesity in humans results from defects in the melanocortin-4 receptor. The second population of neurons increases food intake and co-expresses neuropeptide Y (NPY) and agouti-related protein (Cone et al. 2001; Ellacott & Cone 2004; Farooqi & O'Rahilly 2005). Both populations project to the paraventricular nucleus (PVN) and other areas important in the regulation of food intake (figure 1; Schwartz et al. 2000).
Figure 1.
Schematic of the two main appetite-regulating populations of neurons in the hypothalamic arcuate nucleus. α-MSH, α-melanocyte-stimulating hormone (product of proopiomelanocortin cleavage); AgRP, agouti-related protein; CART, cocaine- and amphetamine-related transcript; MC-3/4, melanocortin-3 and -4 receptors; NPY, neuropeptide Y; PVN, paraventricular nucleus; + denotes stimulation of a receptor; − denotes inhibition.
Extensive reciprocal connections exist between the hypothalamus and the brainstem, particularly the nucleus of the tractus solitarius (NTS; van der Kooy et al. 1984; Ter Horst et al. 1989). Like the ARC, the brainstem is well placed to receive signals from the blood due to its proximity to other regions with an incomplete blood–brain barrier, e.g. the area postrema. In addition, the brainstem receives vagal afferent neurons from the gastrointestinal tract, and therefore acts as another site of integration between endocrine and neuronal signals.
4. Cholecystokinin
The first gut peptide to be implicated in the control of appetite was cholecystokinin (CCK). CCK is derived from a 115-amino acid precursor, pro-CCK, and selective cleavage gives rise to a number of bioactive forms (Rehfeld 2004). Biological activity resides in the amidated C-terminus of the peptide and all the active species of CCK share a C-terminal heptapeptide sequence that also includes an O-sulphated tyrosine. The major circulating forms in man are CCK-58, -33, -22 and -8 (Rehfeld et al. 2001). Non-sulphated forms of CCK also exist, but they constitute minor species of peptide and their biological role remains unclear.
CCK is synthesized in a number of tissues in humans, including the I-cells of the small intestine (Buffa et al. 1976), from where it is rapidly released into the circulation in response to a meal (Liddle et al. 1985). The basal plasma concentration of CCK is approximately 1 pM, and levels rise to 5–8 pM postprandially (Liddle et al. 1985), although many assays for CCK also detect fragments of the peptide. Whether all the CCK measured in plasma is bioactive remains to be established. The concentration of CCK in the circulation remains elevated for up to 5 hours after a meal, and dietary fat and protein, or the products of their digestion, are more potent stimulators of CCK release than carbohydrate (Liddle et al. 1985).
CCK also has a dual role as a neurotransmitter, in both the enteric and CNSs (Barden et al. 1981; Hutchison et al. 1981). The post-translational modification of CCK is tissue-specific, with CCK-8 the predominant form in nervous tissue, whereas longer species are preferentially synthesized in the endocrine cells of the gut (Rehfeld et al. 2003).
Two G-protein-coupled receptors for CCK have been identified and may be distinguished by their characteristic pharmacological profiles (Wank 1995). Previously known as the CCK-A and gastrin/CCK-B receptors, they are now designated the CCK-1 and CCK-2 receptors, respectively. Both receptor subtypes are distributed throughout the CNS and gut, although CCK-1 receptors predominate in the alimentary tract, and CCK-2 receptors in the brain (Wank 1995).
CCK acts to cause gallbladder contraction, relaxation of the sphincter of Oddi, stimulation of somatostatin release (and thus inhibition of gastric acid secretion) and stimulation of pancreatic growth and enzyme release via the CCK-1 receptor (Wank 1995). The CCK-2 receptor has been implicated in schizophrenic and anxiety states, and other CNS actions of CCK (Wank 1995; Zachrisson et al. 1999; Miyasaka et al. 2002). Inevitably, however, the overlap in distribution is reflected in an overlap in function (Morisset et al. 2000; Sanjuan et al. 2004; Jang et al. 2005). Moreover, the hormone gastrin is structurally related to CCK, and its actions on the gastric mucosa are mediated via the CCK-2 receptor, which also binds gastrin with high affinity (Dockray et al. 2001).
In addition to those effects summarized above, CCK also alters appetite. Gibbs et al. (1973) first demonstrated a dose-dependent effect of exogenous CCK in reducing food intake in rats. This effect occurred without evidence of toxicity and was specific to food intake, CCK having no effect on water intake in water-deprived rats. This finding was subsequently confirmed in humans, in whom an intravenous infusion of the terminal octapeptide of CCK reduced meal size and duration (Kissileff et al. 1981). This effect of CCK is short-lived. When administered more than 30 minutes prior to the start of a meal, CCK did not alter food intake (Gibbs et al. 1973).
The mechanism by which CCK might exert this effect on appetite is still a matter of ongoing debate. It has been proposed that the inhibitory effect of CCK on gastrointestinal motility, and, in particular, its inhibition of gastric emptying, might be contributory to its inhibitory actions on feeding. Some authors have suggested that in this way, CCK may promote stimulation of gastric mechanoreceptors, and thus invoke neural feedback from the gut to appetite centres in the brain. In support of this hypothesis, low doses of CCK reduced food intake in rhesus monkeys only after a gastric preload of saline (Moran & McHugh 1982). Similarly, in humans, gastric distension was found to augment the reduction of nutrient intake effected by intravenous CCK-8 (Kissileff et al. 2003). The use of antagonists to the serotonin receptor subtype 3 (5-HT3) has recently pointed towards a role for serotonin in the mediation of this effect (Hayes et al. 2004).
However, CCK also alters food intake through other pathways that are independent of its effects on the stomach (Moran & McHugh 1988). While the induction of satiety at higher doses of CCK may be attenuated by surgical removal of the pyloric sphincter, lower doses continue to be effective in inhibiting food intake. Lesioning of the vagus nerve abolishes the effects of CCK at the lower doses of the dose–response curve (Moran & Kinzig 2004). The induction of satiety by CCK at physiological concentrations may therefore rely crucially on direct activation of vagal afferent fibres. Others, however, argue that our notion of ‘physiological levels’ of CCK has been inaccurate in the past due to deficiencies in the assays used, and that the reduction of food intake seen with CCK is pharmacological rather than physiological (Lieverse et al. 1993; Baldwin et al. 1998; Rehfeld 1998).
CCK-1 receptors are present on afferent fibres of the vagus nerve, and also in the brainstem and dorsomedial nucleus of the hypothalamus (DMH). The use of specific CCK-1 and CCK-2 receptor antagonists has implicated the CCK-1 receptor in the reduction of food intake by CCK (Moran et al. 1992). Chronic administration of CCK-1 receptor antagonists or anti-CCK antibodies accelerates weight gain in rodents, though without significant hyperphagia (McLaughlin et al. 1985; Meereis-Schwanke et al. 1998). The Otsuka–Long–Evans–Tokushima Fatty (OLETF) rat, which lacks CCK-1 receptors, is both hyperphagic and obese (Moran et al. 1998; Schwartz et al. 1999). Peripherally administered CCK induces c-fos, a marker of neuronal activity, in the brainstem (Zittel et al. 1999), and food intake in rats is also reduced following direct injection of CCK into a number of hypothalamic nuclei (Blevins et al. 2000). Work in OLETF rats has implicated the orexigenic peptide NPY in the mediation of the effects of CCK in the DMH (Bi et al. 2001). Thus, the anorectic effects of CCK appear to be mediated by a number of mechanisms, both direct and indirect.
The usefulness of CCK as a therapeutic target in the treatment of obesity, however, may be limited by the short-lived nature of its effects on appetite. Repeated administration does not alter body weight in rats, for although food intake is reduced, meal frequency increases, and so overall intake is unchanged (West et al. 1984, 1987a,b). When given to rats as a continuous intraperitoneal infusion, the anorectic effect of CCK is lost after 24 hours (Crawley & Beinfeld 1983) and Glaxo-Smithkline recently halted trials of its CCK-1 receptor antagonist 181771 after the results made it commercially non-viable (Fong 2005). From the point of view of body weight regulation, CCK may play more of an indirect role in its interaction with signals of longer-term energy balance, such as leptin (Matson et al. 2000; Morton et al. 2005). The therapeutic potential of this relationship remains to be determined and the physiological or pharmacological nature of the actions of CCK on food intake also awaits further clarification.
5. Polypeptide-fold proteins
The polypeptide-fold (PP) family of proteins consists of NPY and two peptides of the gastrointestinal–pancreatic endocrine system, pancreatic PP and peptide YY (PYY). Members of this family of peptides are 36 amino acids in length (with the exception of chicken PYY, which contains 37 amino acids) and undergo C-terminal amidation as a necessary requirement for biological activity. All share a common tertiary structure consisting of a type II proline helix and α-helix connected by a β turn. This structural motif is known as the PP-fold (Fuhlendorff et al. 1990). Of this group of peptides, NPY shows the greatest conservation across species, and PP the least (Conlon 2002).
(a) Receptors
Five receptors for the PP-fold family of peptides have been cloned in mammals thus far. Named Y1, Y2, Y4, Y5 and y6 (Michel et al. 1998), the y6 receptor is truncated and non-functional in man. All are coupled to inhibitory G-proteins (Gi), and therefore mediate an inhibition of intracellular cyclic-adenosine monophosphate (cAMP) synthesis (Mullins et al. 2002). However, they also exhibit a degree of heterogeneity in their coupling to other intracellular signalling pathways. Mullins et al. (2002), for instance, showed that while blockade of the protein kinase C pathway completely abolished the effects of Y5 receptor activation, it only diminished the downstream effects mediated by the receptors Y1, Y2 and Y4.
The receptors are diverse in their distribution and this is reviewed in detail elsewhere (Berglund et al. 2003). Of particular note in the context of appetite regulation is the mainly presynaptic location of the Y2 receptor subtype in the hypothalamus and elsewhere. Here, it acts as an autoreceptor and inhibits further neurotransmitter release (Smith-White et al. 2001). The receptors are classified according to their affinity for different ligands. PYY binds with high affinity to all five receptor subtypes, but the cleavage product PYY3-36 shows selectivity for Y2 and Y5 receptors (see table 2). This diversity in ligand affinity coupled with the differing distributions of the five receptor subtypes ensures that there is scope for this family of peptides to mediate a wide range of biological effects.
Table 2.
Summary of agonist affinities of Y-family receptor subtypes. (NPY, neuropeptide Y; PP, pancreatic polypeptide; PYY, peptide YY (see also Berglund et al. 2003).)
| receptor | high-affinity agonists | intermediate-affinity agonists | low-affinity agonists |
|---|---|---|---|
| Y1 | NPY, PYY, Leu31,Pro34NPY/PYY | NPY2-36, NPY3-36, NPY13-36 | PP |
| Y2 (presynaptic) | NPY, PYY, PYY3-36 | Leu31,Pro34NPY/PYY | PP |
| Y4 | PP, NPY, PYY, Leu31,Pro34NPY/PYY | NPY2-36 | NPY/PYY fragments PYY3-36 |
| Y5 | NPY, PYY, NPY2-36, NPY3-36, PYY3-36, Leu31,Pro34NPY/PYY | PP, NPY13-36, PYY13-36 | NPY/PYY fragments |
| y6 | non-functional in man |
(b) Peptide YY
PYY was first isolated from porcine intestine using a technique for the assay of C-terminal amidated peptides (Tatemoto 1982). It is secreted by the L-cells of the gastrointestinal tract, and is widely expressed throughout the gut. Levels of PYY immunoreactivity are low in the proximal small intestine, but increase in the ileum, and continue to rise in the large intestine towards the rectum (Adrian et al. 1985a). PYY immunoreactivity has also been identified in the human adrenal medulla (Ekblad & Sundler 2002) and in areas of the CNS of the rat, including the hypothalamus, medulla, pons and spinal cord (Ekman et al. 1986).
(i) General physiology
PYY is released into the circulation in response to a meal in proportion to the calories ingested and in relation to the meal composition (Adrian et al. 1985a). Higher plasma levels of PYY are seen following isocaloric meals of fat compared with meals consisting of protein or carbohydrate. PYY has been invoked as contributing to the ‘ileal brake’ effect, acting to inhibit further food intake once nutrients have reached the distal small intestine. Interestingly, however, PYY release has been shown to be similar whether intraluminal fat is confined to the proximal or distal half of the small intestine. The release of PYY in response to fat in the proximal small intestine is atropine-sensitive, raising the possibility that a neural reflex (likely involving the vagus nerve) may also mediate PYY release (Fu-Cheng et al. 1997; Lin & Chey 2003; Lin & Taylor 2004). Other stimulants of PYY release include intraluminal bile acids, gastric acid and CCK (Onaga et al. 2002).
Studies of the actions of PYY initially focused on its local effects within the alimentary tract. At doses of 0.2 pmol kg−1 min−1 and above, PYY infused into healthy volunteers caused a significant suppression of pentagastrin-stimulated gastric secretions (Adrian et al. 1985b). It delays gastric emptying (Allen et al. 1984; Moran et al. 2005) and has an inhibitory effect on gallbladder emptying, an effect probably mediated by the vagus nerve (Hoentjen et al. 2001). In common with other hormones of the gastrointestinal tract, PYY also exhibits mitogenic properties, which has led to interest in its effects in pathological states, such as acute pancreatitis (Kazanjian et al. 2003).
(ii) Appetite control: PYY injected into the CNS
Similarly, the role of PYY in the regulation of appetite and food intake continues to be debated. Initial experiments, in which PYY was administered into the lateral ventricle in rats, suggested the peptide to be a mediator of orexigenic behaviour (Morley et al. 1985). Other studies subsequently also found that PYY administered into the CNS increased food intake in rodents (Clark et al. 1987; Corp et al. 1990, 2001). Observations have also been made of differences in levels of PYY in the cerebrospinal fluid (CSF) of abstaining patients with bulimia nervosa, compared with the same patients shortly after binge eating and vomiting, or compared with healthy controls and patients with anorexia nervosa (Berrettini et al. 1988). This has led some researchers to speculate on the place of PYY, acting as a neurotransmitter, in the aetiology of eating disorders. Others, however, point to normalization of these differences in the context of long-term remission as indicative that changes in CSF PYY concentration are a consequence of eating disorders, rather than a cause (Gendall et al. 1999).
Matters are complicated by the existence of two species of PYY and multiple receptors (see table 2). As well as the full-length peptide, a truncated form, PYY3-36, is created by cleavage of the N-terminal residues by dipeptidyl peptidase IV (DPP-IV; Eberlein et al. 1989; Grandt et al. 1994). As described above, PYY3-36 demonstrates relative specificity for the Y2 receptor. When injected into the cerebroventricular system, PYY3-36 also mediates an increase in food intake (Kanatani et al. 2000). This effect is attenuated in Y1 and Y5 knockout mice. Injection directly into the ARC, however, inhibits feeding in rodents (Batterham et al. 2002). The inhibitory Y2 autoreceptor is highly expressed on orexigenic NPY neurons in the ARC (Broberger et al. 1997), whereas Y1 and Y5 receptors are distributed in areas such as the PVN. It has therefore been suggested that the orexigenic effects of ICV-administered PYY and PYY3-36 are mediated by action at Y1 and Y5 receptors. The ARC, however, is associated with a relative deficiency of blood–brain barrier, and is therefore more exposed to circulating PYY3-36 than other appetite regulatory areas of the hypothalamus. Fasting results in an increase in NPY message and peptide expression in the ARC, and it has been proposed that circulating PYY3-36 acts on Y2 receptors in the ARC to reduce NPY expression and thus also reduce food intake. An understanding of the differential distribution of Y-type receptors, and their relative affinities for ligands of the PP-fold family of peptides, is therefore crucial to fully understanding the mechanisms underlying gut hormone regulation of feeding.
(iii) Appetite control: peripheral injection
Batterham et al. (2002) administered intraperitoneal (IP) injections of PYY3-36 to rats and demonstrated a reduction of food intake in fasted rats, and in non-fasted rats freely feeding during the dark phase (again, when NPY levels in the ARC are high), without a detectable effect on gastric emptying. The dose of PYY3-36 sufficient to bring about this inhibition of feeding resulted in peak plasma levels 15 minutes post-injection that were comparable with physiological postprandial levels of PYY3-36 and resulted in significant induction of c-fos expression in the ARC. Incubation of hypothalamic explants in vitro with PYY3-36 resulted in a decrease in NPY release and an increase in α-MSH secretion, and IP injection of PYY3-36 to rats significantly decreased hypothalamic NPY mRNA expression and non-significantly increased POMC mRNA expression (Batterham et al. 2002). More recent evidence from studies in which POMC and melanocortin-4 receptor knockout mice have been shown to retain sensitivity to the anorectic actions of PYY3-36 have suggested that the melanocortin system may not be essential for the mediation of the inhibitory effects of PYY3-36 on energy intake (Challis et al. 2004; Halatchev et al. 2004).
The effect of peripheral PYY3-36 on feeding has since been replicated in a number of species, including non-human primates (Challis et al. 2003; Adams et al. 2004; Halatchev et al. 2004; Pittner et al. 2004; Chelikani et al. 2005; Moran et al. 2005; Scott et al. 2005; Talsania et al. 2005), though with varying effects on gastric emptying. Furthermore, unlike CCK, this feeding effect does not appear to be subject to attenuation with more chronic administration of the peptide. Twice-daily IP injections of PYY3-36 for a period of seven days resulted in reduced food intake and weight gain in rats (Batterham et al. 2002).
In support of the hypothesis that peripherally administered PYY3-36 acts via the Y2 receptor, the peptide's anorectic actions are not seen in Y2-null mice (Batterham et al. 2002). Nor does endogenous or exogenous PYY3-36 inhibit feeding in rats that have been injected with BIIE0246, a selective antagonist of the Y2 receptor, directly into the ARC (Abbott et al. 2005b).
Evidence also exists, however, that runs counter to the ‘leaky ARC’ model described above, and some authors favour alternative mechanisms through which the anorectic effects of PYY3-36 may be mediated. Y2 receptor mRNA is also expressed in the NTS and the nodose ganglion of the vagus nerve (Gustafson et al. 1997; Koda et al. 2005). This observation and the reciprocal connections that exist between the ARC and NTS have led some investigators to suggest that PYY3-36 may inhibit feeding via an effect on the vagus. Abbott and co-workers have demonstrated that both bilateral subdiaphragmatic vagotomy and transectioning of the brainstem–hypothalamic neuronal pathways abolish the anorectic effects of peripheral PYY3-36. Interestingly, these procedures also attenuate the induction of c-fos in the ARC in response to PYY3-36, lending support to the case against an effect of circulating PYY3-36 directly on the ARC (Abbott et al. 2005a). Similar observations have been made by other researchers (Koda et al. 2005). Clearly, a comprehensive model of the mechanism of appetite regulation by PYY3-36 will need to bring together these disparate and occasionally contradictory observations.
Controversy also extends to the robustness of the suppression of caloric intake seen with both acute and chronic peripheral administration of PYY3-36. Some groups have had difficulty in replicating the initial findings of Batterham et al. (Tschop et al. 2004). The reasons for this are unclear, but seem to be confined to rodents. Stress is known to reduce food intake in rodents through effects in the ARC (Halatchev et al. 2004), and differences in acclimatization to the experimental procedure may account for the lack of efficacy of PYY3-36 in some studies. The effect in primates appears to be more robust, and arguably provides a better model for appetite regulation in humans.
(iv) Role in humans
That PYY3-36 performs a significant role in the control of appetite in humans is supported by a number of observations. In disease states characterized by weight-loss, such as inflammatory bowel disease, tropical sprue and cardiac cachexia, PYY3-36 levels are elevated (Adrian et al. 1986; El Salhy et al. 2002; Le Roux et al. 2005). Gastrointestinal surgery currently constitutes the most effective treatment for obesity, and the mechanism by which surgery effects weight loss is thought to involve a loss of appetite (Atkinson & Brent 1982). This appetite loss may be secondary to changes in the signals of energy balance released by the gut (Hanusch-Enserer & Roden 2005). In particular, gastric bypass surgery has been shown to result in an exaggerated postprandial PYY3-36 response, which may contribute to the durability of postoperative weight loss (Alvarez et al. 2002; Korner et al. 2005). Conversely, in obese humans, fasting plasma concentrations of PYY3-36 are reduced (Batterham et al. 2003a) and overweight subjects have a relative deficiency of postprandial PYY3-36 release associated with reduced satiety.
Intravenous infusion of PYY3-36 at a rate of 0.8 pmol kg−1 min−1 into lean humans increased mean plasma PYY3-36 levels from 8.3 to 43.5 pM, and mimicked postprandial PYY3-36 concentrations (Batterham et al. 2002). Plasma PYY3-36 returned to baseline concentrations within 30 minutes of the end of the infusion. Despite this, at a free-choice buffet meal 2 hours after the end of the infusion, there was a significant reduction in calorie intake of approximately 36%, with no effect on fluid intake or on gastric emptying as assessed by paracetamol absorption (Batterham et al. 2002).
Despite lower basal levels of PYY3-36 in obese humans, obesity does not appear to be associated with resistance to the effects of PYY3-36. Infusion of PYY3-36 into a group of obese volunteers resulted in a comparable reduction in calorie intake when compared with lean controls (Batterham et al. 2003a). This preservation of the effects of PYY3-36 in the obese, in the context of apparent abnormal postprandial release of the hormone, raises the possibility that PYY3-36 may be involved in the pathogenesis of obesity, and is therefore an attractive therapeutic target. Both Merck & Co. and Amylin Pharmaceuticals are currently in various stages of development of PYY3-36-based therapies for obesity.
(c) Pancreatic polypeptide
PP is principally released by a population of cells located at the periphery of the pancreatic islets, although some is also synthesized in the exocrine pancreas and distal gut (Larsson et al. 1975; Adrian et al. 1976; Ekblad & Sundler 2002). In contrast to other gut hormones, the presence of PP in the CNS is a matter of debate. Early reports of widespread PP-like immunoreactivity have now largely been ascribed to cross-reaction of the antibodies used with NPY (DiMaggio et al. 1985). Some researchers have reported the presence of PP immunoreactivity in extracts of porcine hypothalamus, pineal gland, substantia nigra, hippocampus and pituitary gland (Inui et al. 1985), but other groups have failed to demonstrate the presence of PP mRNA in the brains of rodents (Ekblad & Sundler 2002), and the matter remains unresolved.
PP secretion into the circulation is subject to an underlying circadian rhythm, with levels in fasting individuals increasing gradually during the day to peak at approximately 21.00 hours, before falling and reaching a nadir at 02.00 hours (Track et al. 1980). However, food intake is the main stimulus to PP secretion, and feeding promotes release of the hormone into the blood. The biphasic manner of this release becomes more marked over the course of the day and the percentage contribution of the first phase of PP release increases with each subsequent meal (Track et al. 1980). Postprandial PP release is proportional to the caloric intake and plasma levels remain elevated for up to 6 hours after feeding (Adrian et al. 1976).
Both basal and postprandial PP release is subject to control by the vagus nerve. Evidence of vagal involvement takes the form of elimination of the circadian rhythm of PP secretion and a marked reduction in postprandial release by propantheline, a drug with antimuscarinic actions (Track et al. 1980). Truncal vagotomy and atropine, another antimuscarinic agent, have also been shown to reduce meal-induced PP release in dogs (Niebel et al. 1987), and humans (Konturek et al. 1987; Meguro et al. 1995). PP secretion is also controlled by other factors, including the gut hormones ghrelin, motilin and secretin, all of which stimulate PP release, and somatostatin, which potently inhibits (Funakoshi et al. 1989; Gomez et al. 1997; Mochiki et al. 1997; Arosio et al. 2003).
More recent studies in which human PP was infused into healthy subjects have suggested that PP may exert an inhibitory effect on gastric emptying, as well as delaying the postprandial rise in insulin (Schmidt et al. 2005). A delay in gastric emptying is also seen in mice injected IP with murine PP (Asakawa et al. 2003). The early infusion studies in humans used bovine PP rather than native human peptide. Of the PP-fold proteins, PP shows the least conservation across species (Lundell et al. 1995). It is thought to be the most recently evolved of the family and to have arisen by duplication of the PYY gene (Hort et al. 1995). PP differs across species mainly in its N-terminus, which seems to be crucial for receptor recognition (Gingerich et al. 1991). While a species difference is one possible explanation for the discrepancy in the effects of PP on the stomach, bovine PP differs from the human protein by only two amino acids and demonstrates an affinity for the human Y4 receptor that is similar to human PP (Gehlert et al. 1996).
The function served by PP in signalling energy status is no less controversial. Genetically obese ob/ob mice lack PP cells in the pancreas, and replacement therapy with twice daily IP injections of bovine PP was found to reduce feeding and body weight gain (Malaisse-Lagae et al. 1977). Asakawa and co-workers have built upon this finding and have recently published work in which the effects of PP on energy balance in wild-type and genetically obese mice were extensively described. Synthetic murine PP injected IP into fasted mice significantly reduced feeding within 20 minutes of administration (the earliest timepoint studied) and this effect was apparent in cumulative feeding data over the 24 hours following injection (Asakawa et al. 2003). Repeated administration of PP over six days to ob/ob mice resulted in a significant reduction in body weight gain and an improvement in blood glucose and lipid profiles.
In humans, abnormal patterns of PP secretion have been found in patients with Prader–Willi syndrome, a disease entity characterized by hyperphagia and obesity (Zipf et al. 1981). The situation in non-syndromic obese patients is less clear. Some authors have reported an impairment of PP response (Lassmann et al. 1980; Glaser et al. 1988), whereas others report similar levels of circulating PP in obese subjects with stable body weight (Jorde & Burhol 1984; Meryn et al. 1986; Wisen et al. 1992). In anorexic individuals, there is evidence that PP responses are exaggerated (Uhe et al. 1992; Fujimoto et al. 1997). After gastric surgery, levels of PP in the circulation appear reduced (Amland et al. 1984; Meryn et al. 1986), though interestingly, levels seem to be increased after jejunoileal bypass, and may contribute to the weight loss associated with this latter operation (Jorde & Burhol 1982).
The effects of exogenous PP on appetite are less equivocal. When infused into subjects with Prader–Willi syndrome, PP induced a reduction in appetite and food intake (Berntson et al. 1993). Similarly, infusion intravenously into lean humans resulted in a decrease in appetite that persisted and was reflected in reduced food intake recorded in food diaries 24 hours after the infusion (Batterham et al. 2003b). It is this prolonged action of PP on food intake that makes it an attractive candidate for the development of an antiobesity therapy. This notion is supported by the observation that mice chronically over-expressing PP to supraphysiological levels are lean with reduced food intake (Asakawa et al. 2003), suggesting that chronic exposure to high levels of PP does not result in the development of resistance to the anorectic actions of the hormone.
As with PYY3-36, the mechanism through which PP effects its anorectic actions comprises a number of integrated elements. Some authors have suggested that the delay in gastric emptying seen with peripheral PP administration might underlie the inhibition of appetite (Katsuura et al. 2002), although others have demonstrated an appetite effect independent of changes in gastric motility (Batterham et al. 2003b). PP also increases oxygen consumption when administered IP to mice, supporting a role for increased energy expenditure in the mediation of weight loss by PP (Asakawa et al. 2003).
Vagal signalling appears to be necessary for the PP-mediated inhibition of feeding as this effect is abolished in vagotomized mice (Asakawa et al. 2003). In addition, changes in expression of a number of genes in the hypothalamus point to the involvement of CNS appetite circuits. IP injection of PP into fasted mice was shown to reduce mRNA expression in the hypothalamus of the orexigenic neuropeptides NPY and orexin by approximately 60%. Conversely, expression of mRNA of the anorectic urocortin was increased by 132%. A similar pattern of mRNA expression, though attenuated and not statistically significant when compared to control mice, was seen following IP injection of PP into non-fasted mice (Asakawa et al. 2003).
The interplay between these two sites of action is unclear. PP injected intracerebroventricularly (ICV) acts to increase food intake (Asakawa et al. 1999). As with PYY, this apparent non-concordance between the actions of CNS- and peripherally administered PP may be due to differential receptor activation and distribution. PP does not readily cross the blood–brain barrier (Banks et al. 1995), and thus may act preferentially in those areas of the hypothalamus that are more easily accessible due to a deficient blood–brain barrier. Alternatively, PP may act on the vagus nerve and thus modify the activity of hypothalamic circuits via projections from vagal nuclei in the brainstem. The area postrema in the brainstem also has an incomplete blood–brain barrier and demonstrates high binding of 125I-labelled PP in vivo, providing another level at which PP may directly act (Whitcomb et al. 1990).
Although it binds to all members of the Y receptor family, PP exhibits greatest affinity for the Y4 receptor subtype. Y4 receptor mRNA has been localized to areas of the hypothalamus, including the ARC (Parker & Herzog 1999). Receptor mRNA is also expressed widely in key appetite-regulating areas of the brainstem, including the area postrema (Larsen & Kristensen 1997).
In some species, including humans, though not in rats, PP also binds with moderately high affinity to Y5 receptors. In Y5 knockout mice, the orexigenic actions of CNS-injected human and bovine PP are blunted (Kanatani et al. 2000), suggesting involvement of the Y5 receptor in the stimulation of food intake by CNS PP. It has therefore been proposed that Y4 receptors accessible to circulating PP may be responsible for the mediation of the hormone's anorectic actions, whereas other receptors, such as Y5 receptors, might mediate the antagonistic effects of CNS-administered PP. Y4 receptors have, however, also been noted on orexin neurons in the lateral hypothalamic area (LHA). Injection of PP into the LHA stimulates feeding behaviour in rats, though to a lesser extent than injection of NPY. PP does, however, induce c-fos expression in LHA orexin neurons (Campbell et al. 2003). The integration of these observations into a unified model that explains the disparate actions of CNS and peripherally injected PP will require further data.
6. Products of preproglucagon cleavage
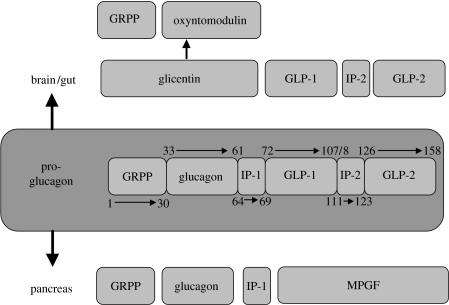
Preproglucagon is a 160-amino acid prohormone with a 20-amino acid signal sequence at the N-terminal end (Kieffer & Habener 1999). It is synthesized in the α-cells of the pancreatic islets, the L-cells of the intestinal mucosa and within the CNS. Preproglucagon undergoes differential cleavage by prohormone convertase 1 and 2, resulting in the tissue-specific production of a number of biologically active fragments (figure 2; Kieffer & Habener 1999). In the intestine and CNS, the products glucagon-like peptides-1 and -2 (GLP-1 and -2) and oxyntomodulin (OXM) have been implicated in the regulation of appetite, and will be considered in turn below. The actions of pancreatic glucagon on appetite are reviewed elsewhere in this issue. Briefly, peripheral administration induced satiety. Specifically, glucagon appears to affect the processes related to meal termination and acts synergistically with other intermediaries, most notably CCK. Glicentin administered into rats ICV or directly into the PVN does not affect food intake (Dakin et al. 2001).
Figure 2.
The products of preproglucagon cleavage. Numbers denote amino acid residues at which cleavage occurs. GLP-1 and GLP-2, glucagon-related peptides 1 and 2; GRPP, glicentin-related polypeptide; IP-1 and IP-2, intervening peptides 1 and 2; MPGF, major proglucagon fragment.
(a) Glucagon-like peptide-1
GLP-1 is cleaved from preproglucagon within the intestine, where it is co-localized in the endocrine L-cells of the distal gut with OXM and PYY (Eissele et al. 1992; Wettergren et al. 1997). It is highly conserved across a number of species, implying an important physiological role.
Like PYY, GLP-1 exists in a number of forms in the circulation. GLP-1 is cleaved from preproglucagon as a 36- or 37-amino acid molecule, depending on whether the C-terminal glycine is present. Neither GLP-11-36amide nor GLP-11-37 demonstrated significant biological activity. GLP-11-36amide promotes insulin release from isolated rat pancreatic cells only at supraphysiological levels (Schmidt et al. 1985). It was with the realization that further N-terminal truncation is required for biological activity that the effects of GLP-1 were recognized (Mojsov et al. 1986). Both peptide isoforms are equipotent in those biological activities thus far examined, although GLP-17-36amide is present in the circulation in greater quantities (Orskov et al. 1994b).
(i) General physiology
The action of GLP-17-36amide that has attracted most attention, both from a physiological and a therapeutic viewpoint, is its potent incretin effect (Holst 2005). The peptide mediates glucose-dependent insulinotropic effects in a number of species, including man (Holst et al. 1987; Kreymann et al. 1987; Mojsov et al. 1987). It also inhibits gastric acid secretion and gastric emptying, as well as suppressing glucagon release and promoting an increase in pancreatic β-cell mass (Tolessa et al. 1998; Edvell & Lindstrom 1999; Naslund et al. 1999b). GLP-17-36amide also exerts effects in the cardiovascular system. In animals, these appear to be stimulatory and to involve CNS and adrenal mechanisms (Edwards et al. 1997; Yamamoto et al. 2002). In humans, the situation is less clear, and in fact GLP-17-36amide infusion may improve outcomes post-myocardial infarction in some circumstances (Nikolaidis et al. 2004).
Consistent with its role as an incretin, GLP-17-36amide is released into the circulation in response to a meal in proportion to the calories ingested (Ghatei et al. 1983; Kreymann et al. 1987; Orskov et al. 1994a). Although the majority of L-cells are located in the distal gut, the presence of nutrients in the proximal small intestine stimulates GLP-17-36amide release independently of the presence of nutrients within the ileum and colon (Roberge & Brubaker 1991). This effect is abolished by vagotomy, implying the influence of neural inputs on GLP-17-36amide release (Rocca & Brubaker 1999). The similarity of this mechanism to that governing the release of PYY3-36 has led to the proposal of GLP-17-36amide as another candidate mediator of the ‘ileal brake’ phenomenon.
(ii) Role in energy balance
Lately, however, increasing research has been directed at dissecting out the role of GLP-17-36amide in the regulation of energy balance. In common with other gut peptides, GLP-17-36amide also functions within the CNS as a neurotransmitter. It is present within the dorsovagal complex, the thalamus and the pituitary. GLP-1-immunoreactive neurons are also found in key areas of the hypothalamus involved in appetite-regulation, including the PVN and the DMH (Kreymann et al. 1989; Larsen et al. 1997a).
Further evidence for the involvement of GLP-17-36amide in signalling energy status to CNS appetite circuits includes the distribution of the GLP-17-36amide receptor. The GLP-1 receptor was originally cloned by selective screening of a rat pancreatic cDNA library, and the human homologue was subsequently isolated (Thorens 1992; Dillon et al. 1993). It is a G-protein-coupled, seven-transmembrane domain protein and binding of GLP-17-36amide results in an increase in intracellular cyclic AMP (Gallwitz et al. 1993). Binding studies and reverse transcriptase polymerase chain reaction (RT-PCR) data for receptor mRNA have confirmed the presence of GLP-1 receptors in a number of areas of the brain important in appetite control. These include the ARC, the PVN and the supraoptic nucleus (SON) of the hypothalamus and the area postrema of the brainstem (Wei & Mojsov 1995; Shughrue et al. 1996).
Finally, the peptide exendin-4 has proved a useful tool in determining the mechanisms by which the actions of GLP-17-36amide on appetite are mediated. This is a 39-amino acid peptide extracted from the saliva of the Gila monster, Heloderma suspectum. It is structurally related to GLP-1 and is a potent agonist at GLP-1 receptors, whereas the truncated form, exendin9-39, acts as a competitive antagonist (Thorens et al. 1993). Recently, evidence has been accumulating that some of the actions of GLP-17-36amide in some organs, notably adipose, muscle and liver tissue, may be mediated by an alternative GLP-1 receptor. The activity of GLP-1 at its receptor in these tissues is associated with a decrease in intracellular cAMP, in contrast to its actions at its recognized receptor. This putative alternative receptor also appears to be stimulated by both full-length exendin-4 and exendin9-39, again contrasting with the antagonistic effects of exendin9-39 at the established GLP-1 receptor (Montrose-Rafizadeh et al. 1997; Yang et al. 1998). The role played by this novel receptor in the appetite-regulating actions of GLP-17-36amide remains to be clarified.
Both CNS-injected and peripherally administered GLP-17-36amide inhibit food intake in a number of species. In both instances, the site of action appears to be the brainstem–hypothalamus axis.
Turton et al. administered GLP-17-36amide via the ICV route to rats and demonstrated a significant inhibition of food intake. This effect was associated with induction of c-fos in the PVN and the central nucleus of the amygdala. Both the feeding effect and the induction of c-fos were inhibited by the presence of exendin9-39. Significantly, exendin9-39 alone had no effect in fasted rats, but powerfully increased feeding in satiated rats, implying the involvement of central GLP-17-36amide signalling in the physiological regulation of appetite (Turton et al. 1996). Furthermore, repeated ICV injection of GLP-17-36amide into rats over six days resulted in a significantly reduced body weight when compared with saline-injected animals (Meeran et al. 1999). Again, injection of exendin9-39 resulted in the opposite effect, suggesting underlying physiological GLP-17-36amide signalling in the regulation of feeding behaviour in rats.
Other groups have subsequently confirmed this finding, and reported activation of c-fos by GLP-17-36amide in other areas of the brain. These include the NTS and the area postrema in the brainstem, and the SON in the hypothalamus (van Dijk et al. 1996; Rowland et al. 1997; Larsen et al. 1997b). ICV-administered GLP-17-36amide has also been reported to weakly induce c-fos within the ARC (van Dijk et al. 1996; Larsen et al. 1997b), although with such a high density of GLP-1 receptors localized in the ARC, it is perhaps surprising that the effect is not more pronounced.
(iii) Appetite regulation versus visceral illness
Mice lacking the GLP-1 receptor, while glucose intolerant, exhibit normal food intake and body weight (Scrocchi et al. 1996). Compensatory upregulation of alternative satiety pathways or alternative GLP-1 receptor types may underlie this observation, but coupled with the observation that ICV-injected GLP-17-36amide may induce the phenomenon of conditioned taste aversion (CTA), this has led some investigators to question the physiological importance of GLP-17-36amide-induced anorexia.
In particular, the pattern of c-fos activation seen with ICV GLP-17-36amide resembles that seen with administration of the toxin lithium chloride, a potent inducer of a visceral illness response in rodents (Kinzig et al. 2002; Lachey et al. 2005). Moreover, ICV administration of the GLP-1 receptor antagonist exendin9-39 to rats is able to attenuate the effects of IP lithium chloride, suggesting that CNS GLP-1 is important in the visceral illness actions of lithium chloride (Seeley et al. 2000), although exendin9-39 also binds to the receptors of other peptides, such as glucose-dependent insulinotropic polypeptide (Wheeler et al. 1995). Interestingly, the actions of lithium chloride are preserved in GLP-1 receptor null mice. In addition, ICV GLP-17-36amide does not induce CTA in these knockout mice, whereas it does in their wild-type counterparts (Lachey et al. 2005). Species differences may account for the ability of lithium chloride to induce CTA in mice lacking the GLP-1 receptor, or it is possible that other minor pathways take on greater prominence in the absence of GLP-1 signalling.
When the data on energy intake and those on CTA are taken together, it is clear that GLP-17-36amide injected ICV causes anorexia, but that the mechanisms underlying this, and the importance in a physiological setting, are the subject of contention. One model by which some of the divergent data may be reconciled is to invoke a role for GLP-17-36amide in both the regulation of energy balance, and in the mediation of a visceral illness response, as distinct functions of the peptide. Injection of GLP-17-36amide into the fourth and lateral ventricles gave rise to anorexia, but lateral ventricular administration also induced CTA. Direct injection into the central nucleus of the amygdala did not reduce food intake, but did induce CTA, suggesting that responses to GLP-1 in the PVN and brainstem are involved in the mediation of the peptide's anorectic effects, whereas CTA results from activation of amygdala GLP-1 receptors (Moran et al. 2005). An alternative model proposes that satiety and nausea are mediated by the same pathway, and that with low levels of stimulation, satiety predominates. Nausea results at high levels of stimulation of the pathway.
Peripheral administration of GLP-17-36amide or GLP-1 receptor agonists such as exendin-4 into rodents also reduces feeding and induces c-fos expression in the brainstem and PVN, but not in the ARC (Tang-Christensen et al. 2001; Baggio et al. 2004; Dakin et al. 2004; Abbott et al. 2005a). The anorectic actions of IP GLP-17-36amide are not attenuated by injection directly into the ARC of the receptor antagonist exendin9-39 (Dakin et al. 2004). Furthermore, the observation that the effect of IP GLP-17-36amide on feeding is reduced by vagotomy or ablation of brainstem–hypothalamic connections (Abbott et al. 2005a) raises interesting questions regarding the pathways through which GLP-17-36amide acts to reduce food intake.
CNS-produced GLP-17-36amide may act on appetite circuits within the brain, or GLP-17-36amide released into the circulation postprandially may gain access to important areas of the hypothalamus and brainstem, and thus induce a feeling of satiety. These two scenarios are not mutually exclusive. An integrative model may best account for the importance of the vagus nerve and brainstem–hypothalamic connections, the effects of GLP-17-36amide injected directly into specific hypothalamic nuclei such as the PVN and the pattern of c-fos induction seen on CNS and peripheral administration of the peptide. Circulating GLP-17-36amide acting on the vagus, or entering the brainstem through the deficient blood–brain barrier at the area postrema (Orskov et al. 1996) may in turn influence neuronal activity in important hypothalamic nuclei. GLP-17-36amide may itself be involved as a neurotransmitter in this process at the level of the hypothalamus or brainstem. Injection of a retrograde tracer confirmed that GLP-containing neurons project from the NTS to the PVN (Larsen et al. 1997a). Different circuits, involving the amygdala, may mediate GLP-17-36amide-induced nausea.
(iv) Role in humans
In humans, some authors have suggested that circulating GLP-17-36amide levels are reduced in obesity, and normalize with weight loss (Verdich et al. 2001b). Other investigators, however, have failed to reproduce these findings (Feinle et al. 2002; Vilsboll et al. 2003).
The food intake data from human studies are concordant with the animal studies. GLP-17-36amide dose-dependently decreases appetite and caloric intake in lean and obese humans and patients with diabetes (Gutzwiller et al. 1999a,b; Naslund et al. 1999a). Exendin-4 also reduced food intake when given to healthy volunteers (Edwards et al. 2001). In a recent meta-analysis, it was concluded that infusion of GLP-17-36amide reduces both appetite and food intake, the latter by an average of 11.7% acutely. The magnitude of this reduction is similar in lean and obese men. Furthermore, this was achieved without adverse effects on subject well-being, such as nausea (Verdich et al. 2001a).
(v) Clinical potential
This preservation of the anorectic effect of GLP-17-36amide in the obese has led to interest in the therapeutic potential of the hormone. Prandial subcutaneous injections of GLP-17-36amide given to obese but otherwise healthy subjects for 5 days resulted in a weight loss of 0.55 kg (Naslund et al. 2004).
One barrier to the use of native GLP-17-36amide in a clinical setting is its short half-life. GLP-17-36amide is a substrate for DPP-IV, although unlike PYY, the enzyme inactivates GLP-17-36amide. The half-life of a bolus of GLP-17-36amide administered intravenously to rats is approximately 2 minutes, and this is extended to 10 minutes in DPP-IV-deficient rats (Kieffer et al. 1995). Although DDP-IV is not the sole route by which GLP-17-36amide is degraded, any therapeutic application of GLP-17-36amide would need to overcome this obstacle (Deacon 2004; Holst 2005). Two main strategies have been employed. Some pharmaceutical companies have developed potent long-acting GLP-1 receptor agonists, such as exendin-4 (exenatide, Amylin Pharmaceuticals), or albumin-based forms of GLP-1, such as liraglutide (NovoNordisk), that are resistant to the actions of DPP-IV. The other strategy comprises the use of DDP-IV inhibitors, such as that currently under development by Novartis. Of these, exenatide has recently been granted approval by the Federal Food and Drug Administration for use as an adjunctive therapy in poorly controlled type 2 diabetic patients, and all are at various stages of clinical testing for use specifically as therapies for obesity.
With the use of such gut hormone-based treatments, however, unforeseen side effects may arise. DPP-IV, for instance, plays a role in immune regulation (in which context it is known as CD26; Gorrell et al. 2001). Given its effects on β-cell proliferation, changes in plasma levels of GLP-1 following gastric bypass surgery have also been tentatively linked to the development of nesidioblastosis as a possible long-term postoperative complication (Service et al. 2005). Long-term safety data on GLP-17-36amide-based treatments is awaited.
One possible means by which the side effects of any therapy could be ameliorated might be to combine lower doses of two or more gut hormones in order to achieve the desired reduction in food intake. It is likely that physiologically, interactions between different gut hormones are just as important as the actions of the hormones themselves. Certainly, the co-localization of GLP-17-36amide and PYY3-36 in the L-cells and their co-secretion in response to a meal argues in favour of a synergistic interaction. Indeed, co-administration of exendin-4 and PYY3-36 results in a larger reduction in food intake than either peptide alone at the same dose (Talsania et al. 2005). Theoretically, the side effect profile of such a therapeutic strategy in man would be superior to the use of higher doses of individual gut hormone-based treatments.
(b) Glucagon-like peptide-2
Like GLP-17-36amide, GLP-2 is synthesized by the action of prohormone convertase 1 on preproglucagon in the CNS and intestinal L-cells (Damholt et al. 1999). It is released into the circulation in a biphasic manner following nutrient ingestion. Fat and carbohydrates are potent stimulators of GLP-2 release (Xiao et al. 1999). In common with other hormones secreted by L-cells in the distal gut, the early phase release appears to be mediated by a neuroendocrine reflex involving the vagus, whereas the later peak is likely a result of the action of intestinal nutrients directly on L-cells (Dube & Brubaker 2004).
GLP-2 acts via its own distinct seven-transmembrane domain receptor and increases intracellular cAMP levels (Munroe et al. 1999). This is distributed widely in the periphery and CNS. Through a combination of Northern blot, RT-PCR and immunocytochemical techniques, GLP-2 receptor mRNA has been detected in rat stomach, duodenum, jejunum, ileum and colon and in the hypothalamus, brainstem and lung (Yusta et al. 2000).
From the perspective of energy balance, GLP-2 injected ICV into rats does inhibit food intake (Tang-Christensen et al. 2000). Peripherally administered GLP-2, however, does not appear to affect energy intake in rodents, nor does it affect appetite and feeding in humans (Scott et al. 1998; Schmidt et al. 2003).
As with GLP-17-36amide, circulating GLP-2 is rapidly rendered inactive by the actions of DDP-IV (Xiao et al. 1999). This leaves open the possibility that DDP-IV inhibitors developed for their actions on GLP-17-36amide may also prolong the plasma half-life of GLP-2, resulting in unwanted GLP-2-mediated side effects on the bowel such as uncontrolled cell growth.
(c) Oxyntomodulin
The expression pattern of OXM (formerly known as enteroglucagon) mirrors that of the other preproglucagon-derived hormones discussed above. It is released into the blood following ingestion of food in proportion to the calories ingested (Ghatei et al. 1983; Le Quellec et al. 1992). Physiologically, it acts to reduce gastric motility and secretion in rodents and man (Dubrasquet et al. 1982; Schjoldager et al. 1988, 1989; Dakin et al. 2004). In addition, OXM has been found to exert an incretin effect (Schjoldager et al. 1988; Wynne et al. 2005b), though the magnitude of the rise in insulin is smaller than that seen with GLP-17-36amide and some investigators have failed to detect any increase in postprandial insulin following administration of exogenous OXM (Cohen et al. 2003).
That OXM may be involved in appetite control is suggested not only by its distribution and secretion pattern, but also by observations of elevated plasma levels in illness characterized by weight loss, such as tropical sprue (Besterman et al. 1979). Additionally, OXM levels rise after gastric bypass surgery, paralleling the rise in levels of appetite-suppressing gut hormones such as GLP-17-36amide and PYY3-36 (Holst et al. 1979; Sarson et al. 1981).
More direct evidence takes the form of experimental data. Injection of OXM ICV or into the PVN of fasted rats caused a reduction in food intake compared to controls (Dakin et al. 2001). The effect was also seen in non-fasted rats injected at the start of the dark phase, and OXM was of a comparable potency in reducing food intake to GLP-17-36amide in its effects on feeding. IP injection of OXM was also found to reduce food intake in rats (Dakin et al. 2002). While some researchers have not found IP injection of OXM to lessen feeding in mice (Baggio et al. 2004), the findings have since been replicated in humans (Cohen et al. 2003). Intravenous infusion of OXM into lean volunteers resulted in a reduction of energy intake at a buffet meal of 19.3%, and 12 hour cumulative energy intake was also reduced by 11.3% (Cohen et al. 2003). Volunteers reported no nausea or adverse effects on meal palatability with infusion of OXM. Part of the mechanism by which OXM reduces appetite may involve suppression of the orexigenic hormone ghrelin (Cohen et al. 2003).
As well as short term effects on feeding, repeated administration of exogenous OXM results in a sustained reduction in caloric intake and weight loss in both rodents and humans. Repeated ICV injection of OXM into rats over 7 days resulted in a significantly lower body weight compared to both saline-injected controls and pair-fed saline injected controls. This suggests that the reduction in weight gain was brought about not only by a reduction in food intake, but also by an enhancement of energy expenditure (Dakin et al. 2002). Supporting this model, core temperature was noted to be higher in rats injected with OXM, and deposits of white and brown adipose tissue were found to be reduced. Similarly, repeated pre-prandial subcutaneous injection of OXM in obese human subjects resulted in a 2.3 kg reduction in body weight over the course of four weeks, compared with 0.5 kg in the saline-treated controls (p=0.0106; Wynne et al. 2005b).
A unique receptor for OXM has yet to be identified. OXM does bind to the GLP-1 receptor, but with an affinity that is approximately two orders of magnitude lower than GLP-17-36amide (Fehmann et al. 1994). However, there is evidence, both circumstantial and more direct, that the effects of OXM may be mediated via the GLP-1 receptor. In in vitro assays, OXM is able to stimulate intracellular events in rat parietal cells enriched with the GLP-1 receptor (Schepp et al. 1996). The pattern of c-fos activation seen with peripheral administration of OXM in mice mirrors closely that seen with GLP-1 (Baggio et al. 2004). The anorectic effects of OXM are lost in GLP-1 receptor null mice, and are also inhibited by co-administration of the GLP-1 receptor antagonist exendin9-39 (Dakin et al. 2001; Baggio et al. 2004).
Some data, however, are discordant with this model. Dakin et al. noted marked Fos-like immunoreactivity in the ARC in response to IP injection of OXM in rats (Dakin et al. 2004). While exendin9-39 injected directly into the ARC inhibited the anorectic effects of IP OXM, it had no effect on the actions of GLP-17-36amide on feeding (Dakin et al. 2004). Although the GLP-1 receptor is known to be present in the ARC (see above), exendin9-39 exhibits a degree of non-specificity in its receptor binding, as discussed previously. It is therefore possible that OXM may act upon a novel receptor at which it is also antagonized by exendin9-39.
Thus, although the physiological importance of its actions on appetite and energy intake remains uncertain, OXM offers another promising target in the development of a therapy for obesity. In particular, its less marked incretin effect compared to that mediated by GLP-17-36amide may make it a more attractive option in the treatment of non-diabetic obese patients.
7. Ghrelin and motilin
The gut hormones ghrelin and motilin are structurally related peptides released from distinct areas of the gastrointestinal tract. Both have been found to exert an orexigenic effect.
(a) Ghrelin
Ghrelin is the endogenous ligand for the previously orphan growth hormone secretagogue (GHS) receptor (Kojima et al. 1999). Briefly, the major source of circulating ghrelin is the stomach, although mRNA is also present elsewhere in the gastrointestinal tract (Kojima et al. 1999; Date et al. 2000). Among its actions, ghrelin stimulates growth hormone secretion from the anterior pituitary, stimulates the hypothalamo–pituitary–adrenal axis, mediates an increase in gastric motility, induces a positive inotropic effect on the heart and causes vasodilatation (Korbonits et al. 2004; van der Lely et al. 2004).
It is a peripherally active appetite-stimulating gut hormone. Levels rise during fasting, and fall upon eating, which has led to the suggestion that ghrelin may be involved in meal initiation (Cummings et al. 2001). Plasma levels of ghrelin are inversely correlated with body weight in humans and rise after weight loss (Cummings et al. 2002). An increase in ghrelin levels may explain why some individuals find weight loss difficult to maintain and have a tendency to regain weight after a period of dieting. The lower levels of ghrelin seen in obesity may constitute a feedback mechanism to reduce appetite (Tschop et al. 2001). Systemic injection of ghrelin increases food intake in rodents and man and chronic administration induces obesity in rodents (Tschop et al. 2000; Wren et al. 2001a,b).
From a clinical perspective, preliminary work has been carried out to investigate the effects of administration of ghrelin in diseases characterized by cachexia. Infusion of ghrelin into subjects with appetite loss due to cancer (Neary et al. 2004) increased energy intake by 31% at a subsequent buffet meal. This compares with an increase in energy intake of 28% when ghrelin was administered to healthy human volunteers (Wren et al. 2001a). The patients with cancer had high baseline plasma ghrelin levels, possibly as a reflection of negative energy balance. The ability of exogenous ghrelin to overcome the anorexia associated with cancer, to a similar degree as that seen in healthy subjects, and despite elevated endogenous ghrelin may make manipulation of GHS receptors a rewarding strategy in the treatment of conditions associated with cachexia.
The intravenous route, it may be argued, is impractical, but a recent study has built upon the findings of the earlier work, and specifically considered the effectiveness of subcutaneously injected ghrelin in patients with chronic renal failure and mild to moderate malnutrition (Wynne et al. 2005a). Results were again encouraging, with energy intake more than doubled acutely following injection and maintained for 24 hours after the intervention. In particular in these patients with renal dysfunction, no acute adverse cardiovascular effects were noted. Indeed, other investigators have found that ghrelin may improve cardiac function and exercise capacity in patients suffering from chronic heart failure (Nagaya et al. 2004).
(b) Motilin
Released by cells in the upper part of the duodenum (Usellini et al. 1984), circulating motilin levels peak every 100 minutes in the fasted state and fall postprandially (Itoh 1997). Its main physiological role is thought to be as a regulator of interdigestive gut motility. It also stimulates gallbladder contraction and enzyme secretion in the stomach and pancreas (Itoh 1997).
A number of authors have reported the presence of motilin in the CNS, as evidenced by the presence of motilin immunoreactivity in a number of brain areas in a variety of species (O'Donohue et al. 1981; Beinfeld & Bailey 1985). Other investigators, however, question the accuracy of the detection methods (Nilaver et al. 1988).
ICV injection of motilin into rodents has an orexigenic effect (Rosenfeld & Garthwaite 1987; Asakawa et al. 1998). IP injection of motilin at doses of 5 and 10 μg kg−1 stimulated feeding in rats. Interestingly, this effect was seen only in fasted, but not fed, rats (Garthwaite 1985). Injection of 100 μg kg−1 IP, however, has been found to inhibit feeding, without a detectable affect on behaviour otherwise (Olson et al. 1980). It is possible that this effect on feeding may be secondary to the hormone's primary actions on gut motility. The function of motilin in the physiological regulation of food intake therefore awaits better definition.
8. Somatostatin
Synthesis of this well-characterized hormone occurs in many organ systems throughout the body, where it fulfils myriad autocrine, paracrine, endocrine and neurocrine functions. A detailed description of the physiology of somatotrophin release inhibitory factor (SRIF; somatostatin) is beyond the scope of this review. However, within the alimentary tract, SRIF is synthesized in the D-cells of the gut and endocrine pancreas (Reichlin 1983). Its functions are broadly antisecretory. SRIF inhibits release of other hormones such as gastrin, CCK, secretin, motilin, vasoactive intestinal polypeptide and OXM, it inhibits gastric acid production, prolongs gastric emptying, reduces intestinal motility and decreases splanchnic blood flow, and it inhibits release of insulin, glucagon and release of exocrine pancreatic secretions (Reichlin 1983; Bell et al. 1995).
Similarly, the effects of SRIF on feeding are inhibitory, although it appears to reduce food intake only in animals with a mild degree of hunger (Lotter et al. 1981; Levine & Morley 1982). Feeding hydrolysed gluten to humans physiologically increases somatostatin levels in the circulation, but this had no effect on feeding or appetite (Morley et al. 1983). Thus the physiological importance of this effect of SRIF is unclear.
The mechanisms by which SRIF might act to reduce appetite are largely unresearched. Vagotomy abolishes the effect (Levine & Morley 1982). It may be that this mild effect on food intake is brought about indirectly, by reducing levels of ghrelin (Silva et al. 2005), although desensitization to the inhibitory effects of SRIF on circulating ghrelin may preclude any therapeutic application of this effect.
9. Other gastroenteropancreatic peptides
A number of other peptides also affect food intake. One of these, amylin, is now available as an adjunctive therapy for diabetic patients with poor glycaemic control and is currently undergoing trials as a treatment for obesity per se (pramlintide, Amylin Pharmaceuticals). It is co-secreted with insulin by pancreatic β-cells and inhibits gastric secretion and emptying (Ludvik et al. 1997). Both ICV and peripheral injection of amylin inhibits food intake (Chance et al. 1991, 1993; Lutz et al. 1994; Rushing et al. 2000). This appears to be independent of the vagus nerve (Lutz et al. 1995).
Apolipoprotein A-IV (apoA-IV) is a 46kDa protein synthesized by enterocytes in response to intake of lipids, and secreted together with triglyceride-rich lipoproteins (chylomicrons and very low density lipoproteins; Fujimoto et al. 1992). Physiologically, as well as functioning as a lipoprotein, it also inhibits gastric secretions and intestinal motility (Okumura et al. 1996; Glatzle et al. 2002). ApoA-IV is also present in the CNS, and in particular in the ARC (Liu et al. 2003). Fasting causes a marked reduction in hypothalamic expression of apoA-IV mRNA levels in the hypothalamus (Liu et al. 2001).
Peripheral administration of apoA-IV reduces feeding in rats without adversely affecting their behaviour (Fujimoto et al. 1992). Furthermore, ICV injection of apoA-IV also results in a decrease in food intake in rats, and ICV injection of apoA-IV antisera into rats promoted feeding during the light phase, when rats do not normally exhibit feeding behaviour, suggesting a role for tonic apoA-IV signalling in the hypothalamus in the regulation of feeding (Fujimoto et al. 1993). While these data are promising, much remains unknown about the mechanisms by which apoA-IV reduces food intake, about the physiological role of apoA-IV in the short- and long-term regulation of appetite, and about its interaction with more established intestinal satiety signals. Whether it will prove to be the basis for a useful therapy for obesity remains to be seen.
Leptin, the hormone product of the ob gene, is mainly synthesized in white adipose tissue. Initial high expectations regarding its role in energy balance have been revised following recognition of the phenomenon of leptin resistance in the obese state. Leptin is also synthesized by cells in the gastric mucosa, however, raising the possibility that it may yet play a role in meal termination (Peters et al. 2005). Levels in the stomach, however, are comparatively low, and the physiological importance of gastric leptin remains uncertain.
10. Conclusions
In the century since the first gut hormones were described, much has been discovered regarding their physiological actions. As part of their function to optimize the digestive process, it was perhaps inevitable that they should also act to regulate appetite and food intake. The prize being sought is an effective treatment for one of the most pressing public health issues of the new millennium, and while there is much that we still do not understand, recent advances in our knowledge of the integration of endocrine and neurological signals as a means by which the periphery signals energy status to the brain could soon bring that prize within our grasp.
Acknowledgments
Owais Chaudhri is supported by the Wellcome Trust.
Footnotes
One contribution of 16 to a Theme Issue ‘Appetite’.
References
- Abbott C.R, Monteiro M, Small C.J, Sajedi A, Smith K.L, Parkinson J.R, Ghatei M.A, Bloom S.R. The inhibitory effects of peripheral administration of peptide YY(3-36) and glucagon-like peptide-1 on food intake are attenuated by ablation of the vagal–brainstem–hypothalamic pathway. Brain Res. 2005a;1044:127–131. doi: 10.1016/j.brainres.2005.03.011. doi:10.1016/j.brainres.2005.03.011 [DOI] [PubMed] [Google Scholar]
- Abbott C.R, Small C.J, Kennedy A.R, Neary N.M, Sajedi A, Ghatei M.A, Bloom S.R. Blockade of the neuropeptide Y Y2 receptor with the specific antagonist BIIE0246 attenuates the effect of endogenous and exogenous peptide YY(3-36) on food intake. Brain Res. 2005;1043:139–144. doi: 10.1016/j.brainres.2005.02.065. doi:10.1016/j.brainres.2005.02.065 [DOI] [PubMed] [Google Scholar]
- Adams S.H, Won W.B, Schonhoff S.E, Leiter A.B, Paterniti J.R., Jr Effects of peptide YY[3-36] on short-term food intake in mice are not affected by prevailing plasma ghrelin levels. Endocrinology. 2004;145:4967–4975. doi: 10.1210/en.2004-0518. doi:10.1210/en.2004-0518 [DOI] [PubMed] [Google Scholar]
- Adrian T.E, Bloom S.R, Bryant M.G, Polak J.M, Heitz P.H, Barnes A.J. Distribution and release of human pancreatic polypeptide. Gut. 1976;17:940–944. doi: 10.1136/gut.17.12.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adrian T.E, Ferri G.L, Bacarese-Hamilton A.J, Fuessl H.S, Polak J.M, Bloom S.R. Human distribution and release of a putative new gut hormone, peptide YY. Gastroenterology. 1985a;89:1070–1077. doi: 10.1016/0016-5085(85)90211-2. [DOI] [PubMed] [Google Scholar]
- Adrian T.E, Savage A.P, Sagor G.R, Allen J.M, Bacarese-Hamilton A.J, Tatemoto K, Polak J.M, Bloom S.R. Effect of peptide YY on gastric, pancreatic, and biliary function in humans. Gastroenterology. 1985b;89:494–499. doi: 10.1016/0016-5085(85)90442-1. [DOI] [PubMed] [Google Scholar]
- Adrian T.E, Savage A.P, Bacarese-Hamilton A.J, Wolfe K, Besterman H.S, Bloom S.R. Peptide YY abnormalities in gastrointestinal diseases. Gastroenterology. 1986;90:379–384. doi: 10.1016/0016-5085(86)90936-4. [DOI] [PubMed] [Google Scholar]
- Allen J.M, Fitzpatrick M.L, Yeats J.C, Darcy K, Adrian T.E, Bloom S.R. Effects of peptide YY and neuropeptide Y on gastric emptying in man. Digestion. 1984;30:255–262. doi: 10.1159/000199117. [DOI] [PubMed] [Google Scholar]
- Alvarez B.M, Borque M, Martinez-Sarmiento J, Aparicio E, Hernandez C, Cabrerizo L, Fernandez-Represa J.A. Peptide YY secretion in morbidly obese patients before and after vertical banded gastroplasty. Obes. Surg. 2002;12:324–327. doi: 10.1381/096089202321088084. [DOI] [PubMed] [Google Scholar]
- Amland P.F, Jorde R, Kildebo S, Burhol P.G, Giercksky K.E. Effects of a gastric partitioning operation for morbid obesity on the secretion of gastric inhibitory polypeptide and pancreatic polypeptide. Scand. J. Gastroenterol. 1984;19:857–861. [PubMed] [Google Scholar]
- Arosio M, Ronchi C.L, Gebbia C, Cappiello V, Beck-Peccoz P, Peracchi M. Stimulatory effects of ghrelin on circulating somatostatin and pancreatic polypeptide levels. J. Clin. Endocrinol. Metab. 2003;88:701–704. doi: 10.1210/jc.2002-021161. doi:10.1210/jc.2002-021161 [DOI] [PubMed] [Google Scholar]
- Asakawa A, Inui A, Momose K, Ueno N, Fujino M.A, Kasuga M. Motilin increases food intake in mice. Peptides. 1998;19:987–990. doi: 10.1016/s0196-9781(97)00477-4. doi:10.1016/S0196-9781(97)00477-4 [DOI] [PubMed] [Google Scholar]
- Asakawa A, Inui A, Ueno N, Fujimiya M, Fujino M.A, Kasuga M. Mouse pancreatic polypeptide modulates food intake, while not influencing anxiety in mice. Peptides. 1999;20:1445–1448. doi: 10.1016/s0196-9781(99)00155-2. doi:10.1016/S0196-9781(99)00155-2 [DOI] [PubMed] [Google Scholar]
- Asakawa A, et al. Characterization of the effects of pancreatic polypeptide in the regulation of energy balance. Gastroenterology. 2003;124:1325–1336. doi: 10.1016/s0016-5085(03)00216-6. doi:10.1016/S0016-5085(03)00216-6 [DOI] [PubMed] [Google Scholar]
- Atkinson R.L, Brent E.L. Appetite suppressant activity in plasma of rats after intestinal bypass surgery. Am. J. Physiol. 1982;243:R60–R64. doi: 10.1152/ajpregu.1982.243.1.R60. [DOI] [PubMed] [Google Scholar]
- Baggio L.L, Huang Q, Brown T.J, Drucker D.J. Oxyntomodulin and glucagon-like peptide-1 differentially regulate murine food intake and energy expenditure. Gastroenterology. 2004;127:546–558. doi: 10.1053/j.gastro.2004.04.063. doi:10.1053/j.gastro.2004.04.063 [DOI] [PubMed] [Google Scholar]
- Baldwin B.A, Parrott R.F, Ebenezer I.S. Food for thought: a critique on the hypothesis that endogenous cholecystokinin acts as a physiological satiety factor. Prog. Neurobiol. 1998;55:477–507. doi: 10.1016/s0301-0082(98)00005-7. doi:10.1016/S0301-0082(98)00005-7 [DOI] [PubMed] [Google Scholar]
- Banks W.A, Kastin A.J, Jaspan J.B. Regional variation in transport of pancreatic polypeptide across the blood–brain barrier of mice. Pharmacol. Biochem. Behav. 1995;51:139–147. doi: 10.1016/0091-3057(94)00412-c. doi:10.1016/0091-3057(94)00412-C [DOI] [PubMed] [Google Scholar]
- Barden N, Merand Y, Rouleau D, Moore S, Dockray G.J, Dupont A. Regional distributions of somatostatin and cholecystokinin-like immunoreactivities in rat and bovine brain. Peptides. 1981;2:299–302. doi: 10.1016/s0196-9781(81)80123-4. doi:10.1016/0196-9781(81)90048-6 [DOI] [PubMed] [Google Scholar]
- Batterham R.L, et al. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 2002;418:650–654. doi: 10.1038/nature00887. doi:10.1038/nature00887 [DOI] [PubMed] [Google Scholar]
- Batterham R.L, Cohen M.A, Ellis S.M, Le Roux C.W, Withers D.J, Frost G.S, Ghatei M.A, Bloom S.R. Inhibition of food intake in obese subjects by peptide YY3-36. N. Engl. J. Med. 2003a;349:941–948. doi: 10.1056/NEJMoa030204. doi:10.1056/NEJMoa030204 [DOI] [PubMed] [Google Scholar]
- Batterham R.L, Le Roux C.W, Cohen M.A, Park A.J, Ellis S.M, Patterson M, Frost G.S, Ghatei M.A, Bloom S.R. Pancreatic polypeptide reduces appetite and food intake in humans. J. Clin. Endocrinol. Metab. 2003b;88:3989–3992. doi: 10.1210/jc.2003-030630. doi:10.1210/jc.2003-030630 [DOI] [PubMed] [Google Scholar]
- Bayliss H.P, Starling E.H. Mechanism of pancreatic secretion. J. Physiol. Lond. 1902;28:325–353. doi: 10.1113/jphysiol.1902.sp000920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beinfeld M.C, Bailey G.J. The distribution of motilin-like peptides in rhesus monkey brain as determined by radioimmunoassay. Neurosci. Lett. 1985;54:345–350. doi: 10.1016/s0304-3940(85)80102-6. [DOI] [PubMed] [Google Scholar]
- Bell G.I, Yasuda K, Kong H, Law S.F, Raynor K, Reisine T. Molecular biology of somatostatin receptors. Ciba Found. Symp. 1995;190:65–79. doi: 10.1002/9780470514733.ch5. [DOI] [PubMed] [Google Scholar]
- Berglund M.M, Hipskind P.A, Gehlert D.R. Recent developments in our understanding of the physiological role of PP-fold peptide receptor subtypes. Exp. Biol. Med. (Maywood.) 2003;228:217–244. doi: 10.1177/153537020322800301. [DOI] [PubMed] [Google Scholar]
- Berntson G.G, Zipf W.B, O'Dorisio T.M, Hoffman J.A, Chance R.E. Pancreatic polypeptide infusions reduce food intake in Prader–Willi syndrome. Peptides. 1993;14:497–503. doi: 10.1016/0196-9781(93)90138-7. doi:10.1016/0196-9781(93)90138-7 [DOI] [PubMed] [Google Scholar]
- Berrettini W.H, Kaye W.H, Gwirtsman H, Allbright A. Cerebrospinal fluid peptide YY immunoreactivity in eating disorders. Neuropsychobiology. 1988;19:121–124. doi: 10.1159/000118446. [DOI] [PubMed] [Google Scholar]
- Besterman H.S, Cook G.C, Sarson D.L, Christofides N.D, Bryant M.G, Gregor M, Bloom S.R. Gut hormones in tropical malabsorption. Br. Med. J. 1979;2:1252–1255. doi: 10.1136/bmj.2.6200.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi S, Ladenheim E.E, Schwartz G.J, Moran T.H. A role for NPY overexpression in the dorsomedial hypothalamus in hyperphagia and obesity of OLETF rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;281:R254–R260. doi: 10.1152/ajpregu.2001.281.1.R254. [DOI] [PubMed] [Google Scholar]
- Blevins J.E, Stanley B.G, Reidelberger R.D. Brain regions where cholecystokinin suppresses feeding in rats. Brain Res. 2000;860:1–10. doi: 10.1016/s0006-8993(99)02477-4. doi:10.1016/S0006-8993(99)02477-4 [DOI] [PubMed] [Google Scholar]
- Broberger C, Landry M, Wong H, Walsh J.N, Hokfelt T. Subtypes Y1 and Y2 of the neuropeptide Y receptor are respectively expressed in pro-opiomelanocortin- and neuropeptide-Y-containing neurons of the rat hypothalamic arcuate nucleus. Neuroendocrinology. 1997;66:393–408. doi: 10.1159/000127265. [DOI] [PubMed] [Google Scholar]
- Buffa R, Solcia E, Go V.L. Immunohistochemical identification of the cholecystokinin cell in the intestinal mucosa. Gastroenterology. 1976;70:528–532. [PubMed] [Google Scholar]
- Campbell R.E, Smith M.S, Allen S.E, Grayson B.E, Ffrench-Mullen J.M, Grove K.L. Orexin neurons express a functional pancreatic polypeptide Y4 receptor. J. Neurosci. 2003;23:1487–1497. doi: 10.1523/JNEUROSCI.23-04-01487.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Challis B.G, Pinnock S.B, Coll A.P, Carter R.N, Dickson S.L, O'Rahilly S. Acute effects of PYY3-36 on food intake and hypothalamic neuropeptide expression in the mouse. Biochem. Biophys. Res. Commun. 2003;311:915–919. doi: 10.1016/j.bbrc.2003.10.089. doi:10.1016/j.bbrc.2003.10.089 [DOI] [PubMed] [Google Scholar]
- Challis B.G, et al. Mice lacking pro-opiomelanocortin are sensitive to high-fat feeding but respond normally to the acute anorectic effects of peptide-YY(3-36) Proc. Natl Acad. Sci. USA. 2004;101:4695–4700. doi: 10.1073/pnas.0306931101. doi:10.1073/pnas.0306931101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chance W.T, Balasubramaniam A, Zhang F.S, Wimalawansa S.J, Fischer J.E. Anorexia following the intrahypothalamic administration of amylin. Brain Res. 1991;539:352–354. doi: 10.1016/0006-8993(91)91644-g. doi:10.1016/0006-8993(91)91644-G [DOI] [PubMed] [Google Scholar]
- Chance W.T, Balasubramaniam A, Stallion A, Fischer J.E. Anorexia following the systemic injection of amylin. Brain Res. 1993;607:185–188. doi: 10.1016/0006-8993(93)91505-m. doi:10.1016/0006-8993(93)91505-M [DOI] [PubMed] [Google Scholar]
- Chelikani P.K, Haver A.C, Reidelberger R.D. Intravenous infusion of peptide YY(3-36) potently inhibits food intake in rats. Endocrinology. 2005;146:879–888. doi: 10.1210/en.2004-1138. doi:10.1210/en.2004-1138 [DOI] [PubMed] [Google Scholar]
- Clark J.T, Sahu A, Kalra P.S, Balasubramaniam A, Kalra S.P. Neuropeptide Y (NPY)-induced feeding behavior in female rats: comparison with human NPY ([Met17]NPY), NPY analog ([norLeu4]NPY) and peptide YY. Regul. Pept. 1987;17:31–39. doi: 10.1016/0167-0115(87)90030-9. doi:10.1016/0167-0115(87)90030-9 [DOI] [PubMed] [Google Scholar]
- Cohen M.A, Ellis S.M, Le Roux C.W, Batterham R.L, Park A, Patterson M, Frost G.S, Ghatei M.A, Bloom S.R. Oxyntomodulin suppresses appetite and reduces food intake in humans. J. Clin. Endocrinol. Metab. 2003;88:4696–4701. doi: 10.1210/jc.2003-030421. doi:10.1210/jc.2003-030421 [DOI] [PubMed] [Google Scholar]
- Cone R.D, Cowley M.A, Butler A.A, Fan W, Marks D.L, Low M.J. The arcuate nucleus as a conduit for diverse signals relevant to energy homeostasis. Int. J. Obes. Relat. Metab. Disord. 2001;25(Suppl. 5):S63–S67. doi: 10.1038/sj.ijo.0801913. [DOI] [PubMed] [Google Scholar]
- Conlon J.M. The origin and evolution of peptide YY (PYY) and pancreatic polypeptide (PP) Peptides. 2002;23:269–278. doi: 10.1016/s0196-9781(01)00608-8. doi:10.1016/S0196-9781(01)00608-8 [DOI] [PubMed] [Google Scholar]
- Conover K.L, Collins S.M, Weingarten H.P. Gastric emptying changes are neither necessary nor sufficient for CCK-induced satiety. Am. J. Physiol. 1989;256:R56–R62. doi: 10.1152/ajpregu.1989.256.1.R56. [DOI] [PubMed] [Google Scholar]
- Corp E.S, Melville L.D, Greenberg D, Gibbs J, Smith G.P. Effect of fourth ventricular neuropeptide Y and peptide YY on ingestive and other behaviors. Am. J. Physiol. 1990;259:R317–R323. doi: 10.1152/ajpregu.1990.259.2.R317. [DOI] [PubMed] [Google Scholar]
- Corp E.S, McQuade J, Krasnicki S, Conze D.B. Feeding after fourth ventricular administration of neuropeptide Y receptor agonists in rats. Peptides. 2001;22:493–499. doi: 10.1016/s0196-9781(01)00359-x. doi:10.1016/S0196-9781(01)00359-X [DOI] [PubMed] [Google Scholar]
- Crawley J.N, Beinfeld M.C. Rapid development of tolerance to the behavioural actions of cholecystokinin. Nature. 1983;302:703–706. doi: 10.1038/302703a0. doi:10.1038/302703a0 [DOI] [PubMed] [Google Scholar]
- Cummings D.E, Purnell J.Q, Frayo R.S, Schmidova K, Wisse B.E, Weigle D.S. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–1719. doi: 10.2337/diabetes.50.8.1714. [DOI] [PubMed] [Google Scholar]
- Cummings D.E, Weigle D.S, Frayo R.S, Breen P.A, Ma M.K, Dellinger E.P, Purnell J.Q. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 2002;346:1623–1630. doi: 10.1056/NEJMoa012908. doi:10.1056/NEJMoa012908 [DOI] [PubMed] [Google Scholar]
- Dakin C.L, Gunn I, Small C.J, Edwards C.M, Hay D.L, Smith D.M, Ghatei M.A, Bloom S.R. Oxyntomodulin inhibits food intake in the rat. Endocrinology. 2001;142:4244–4250. doi: 10.1210/endo.142.10.8430. doi:10.1210/en.142.10.4244 [DOI] [PubMed] [Google Scholar]
- Dakin C.L, Small C.J, Park A.J, Seth A, Ghatei M.A, Bloom S.R. Repeated ICV administration of oxyntomodulin causes a greater reduction in body weight gain than in pair-fed rats. Am. J. Physiol. Endocrinol. Metab. 2002;283:E1173–E1177. doi: 10.1152/ajpendo.00233.2002. [DOI] [PubMed] [Google Scholar]
- Dakin C.L, Small C.J, Batterham R.L, Neary N.M, Cohen M.A, Patterson M, Ghatei M.A, Bloom S.R. Peripheral oxyntomodulin reduces food intake and body weight gain in rats. Endocrinology. 2004;145:2687–2695. doi: 10.1210/en.2003-1338. doi:10.1210/en.2003-1338 [DOI] [PubMed] [Google Scholar]
- Damholt A.B, Buchan A.M, Holst J.J, Kofod H. Proglucagon processing profile in canine L cells expressing endogenous prohormone convertase 1/3 and prohormone convertase 2. Endocrinology. 1999;140:4800–4808. doi: 10.1210/endo.140.10.7068. doi:10.1210/en.140.10.4800 [DOI] [PubMed] [Google Scholar]
- Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal M.S, Suganuma T, Matsukura S, Kangawa K, Nakazato M. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000;141:4255–4261. doi: 10.1210/endo.141.11.7757. doi:10.1210/en.141.11.4255 [DOI] [PubMed] [Google Scholar]
- Deacon C.F. Therapeutic strategies based on glucagon-like peptide 1. Diabetes. 2004;53:2181–2189. doi: 10.2337/diabetes.53.9.2181. [DOI] [PubMed] [Google Scholar]
- Dillon J.S, Tanizawa Y, Wheeler M.B, Leng X.H, Ligon B.B, Rabin D.U, Yoo-Warren H, Permutt M.A, Boyd A.E., III Cloning and functional expression of the human glucagon-like peptide-1 (GLP-1) receptor. Endocrinology. 1993;133:1907–1910. doi: 10.1210/endo.133.4.8404634. doi:10.1210/en.133.4.1907 [DOI] [PubMed] [Google Scholar]
- DiMaggio D.A, Chronwall B.M, Buchanan K, O'Donohue T.L. Pancreatic polypeptide immunoreactivity in rat brain is actually neuropeptide Y. Neuroscience. 1985;15:1149–1157. doi: 10.1016/0306-4522(85)90259-3. doi:10.1016/0306-4522(85)90259-3 [DOI] [PubMed] [Google Scholar]
- Dockray G.J. Clinical endocrinology and metabolism. Gastrin. Best Pract. Res. Clin. Endocrinol. Metab. 2004;18:555–568. doi: 10.1016/j.beem.2004.07.003. doi:10.1016/j.beem.2004.07.003 [DOI] [PubMed] [Google Scholar]
- Dockray G.J, Varro A, Dimaline R, Wang T. The gastrins: their production and biological activities. Annu. Rev. Physiol. 2001;63:119–139. doi: 10.1146/annurev.physiol.63.1.119. doi:10.1146/annurev.physiol.63.1.119 [DOI] [PubMed] [Google Scholar]
- Dube P.E, Brubaker P.L. Nutrient, neural and endocrine control of glucagon-like peptide secretion. Horm. Metab. Res. 2004;36:755–760. doi: 10.1055/s-2004-826159. [DOI] [PubMed] [Google Scholar]
- Dubrasquet M, Bataille D, Gespach C. Oxyntomodulin (glucagon-37 or bioactive enteroglucagon): a potent inhibitor of pentagastrin-stimulated acid secretion in rats. Biosci. Rep. 1982;2:391–395. doi: 10.1007/BF01119301. doi:10.1007/BF01119301 [DOI] [PubMed] [Google Scholar]
- Eberlein G.A, et al. A new molecular form of PYY: structural characterization of human PYY(3-36) and PYY(1-36) Peptides. 1989;10:797–803. doi: 10.1016/0196-9781(89)90116-2. doi:10.1016/0196-9781(89)90116-2 [DOI] [PubMed] [Google Scholar]
- Edvell A, Lindstrom P. Initiation of increased pancreatic islet growth in young normoglycemic mice (Umea +/?) Endocrinology. 1999;140:778–783. doi: 10.1210/endo.140.2.6514. doi:10.1210/en.140.2.778 [DOI] [PubMed] [Google Scholar]
- Edwards C.M, Edwards A.V, Bloom S.R. Cardiovascular and pancreatic endocrine responses to glucagon-like peptide-1(7-36) amide in the conscious calf. Exp. Physiol. 1997;82:709–716. doi: 10.1113/expphysiol.1997.sp004059. [DOI] [PubMed] [Google Scholar]
- Edwards C.M, Stanley S.A, Davis R, Brynes A.E, Frost G.S, Seal L.J, Ghatei M.A, Bloom S.R. Exendin-4 reduces fasting and postprandial glucose and decreases energy intake in healthy volunteers. Am. J. Physiol. Endocrinol. Metab. 2001;281:E155–E161. doi: 10.1152/ajpendo.2001.281.1.E155. [DOI] [PubMed] [Google Scholar]
- Eissele R, Goke R, Willemer S, Harthus H.P, Vermeer H, Arnold R, Goke B. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur. J. Clin. Invest. 1992;22:283–291. doi: 10.1111/j.1365-2362.1992.tb01464.x. [DOI] [PubMed] [Google Scholar]
- Ekblad E, Sundler F. Distribution of pancreatic polypeptide and peptide YY. Peptides. 2002;23:251–261. doi: 10.1016/s0196-9781(01)00601-5. doi:10.1016/S0196-9781(01)00601-5 [DOI] [PubMed] [Google Scholar]
- Ekman R, Wahlestedt C, Bottcher G, Sundler F, Hakanson R, Panula P. Peptide YY-like immunoreactivity in the central nervous system of the rat. Regul. Pept. 1986;16:157–168. doi: 10.1016/0167-0115(86)90059-5. doi:10.1016/0167-0115(86)90059-5 [DOI] [PubMed] [Google Scholar]
- Ellacott K.L, Cone R.D. The central melanocortin system and the integration of short- and long-term regulators of energy homeostasis. Recent Prog. Horm. Res. 2004;59:395–408. doi: 10.1210/rp.59.1.395. doi:10.1210/rp.59.1.395 [DOI] [PubMed] [Google Scholar]
- El Salhy M, Suhr O, Danielsson A. Peptide YY in gastrointestinal disorders. Peptides. 2002;23:397–402. doi: 10.1016/s0196-9781(01)00617-9. doi:10.1016/S0196-9781(01)00617-9 [DOI] [PubMed] [Google Scholar]
- Farooqi I.S, O'Rahilly S. Monogenic obesity in humans. Annu. Rev. Med. 2005;56:443–458. doi: 10.1146/annurev.med.56.062904.144924. doi:10.1146/annurev.med.56.062904.144924 [DOI] [PubMed] [Google Scholar]
- Fehmann H.C, Jiang J, Schweinfurth J, Wheeler M.B, Boyd A.E, III, Goke B. Stable expression of the rat GLP-I receptor in CHO cells: activation and binding characteristics utilizing GLP-I(7-36)-amide, oxyntomodulin, exendin-4, and exendin(9-39) Peptides. 1994;15:453–456. doi: 10.1016/0196-9781(94)90204-6. doi:10.1016/0196-9781(94)90204-6 [DOI] [PubMed] [Google Scholar]
- Feinle C, Chapman I.M, Wishart J, Horowitz M. Plasma glucagon-like peptide-1 (GLP-1) responses to duodenal fat and glucose infusions in lean and obese men. Peptides. 2002;23:1491–1495. doi: 10.1016/s0196-9781(02)00087-6. doi:10.1016/S0196-9781(02)00087-6 [DOI] [PubMed] [Google Scholar]
- Fong T.M. Advances in anti-obesity therapeutics. Expert. Opin. Invest. Drugs. 2005;14:243–250. doi: 10.1517/13543784.14.3.243. doi:10.1517/13543784.14.3.243 [DOI] [PubMed] [Google Scholar]
- Fu-Cheng X, Anini Y, Chariot J, Castex N, Galmiche J.P, Roze C. Mechanisms of peptide YY release induced by an intraduodenal meal in rats: neural regulation by proximal gut. Pflugers Arch. 1997;433:571–579. doi: 10.1007/s004240050316. doi:10.1007/s004240050316 [DOI] [PubMed] [Google Scholar]
- Fuhlendorff J, Johansen N.L, Melberg S.G, Thogersen H, Schwartz T.W. The antiparallel pancreatic polypeptide fold in the binding of neuropeptide Y to Y1 and Y2 receptors. J. Biol. Chem. 1990;265:11 706–11 712. [PubMed] [Google Scholar]
- Fujimoto K, Cardelli J.A, Tso P. Increased apolipoprotein A-IV in rat mesenteric lymph after lipid meal acts as a physiological signal for satiation. Am. J. Physiol. 1992;262:G1002–G1006. doi: 10.1152/ajpgi.1992.262.6.G1002. [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Fukagawa K, Sakata T, Tso P. Suppression of food intake by apolipoprotein A-IV is mediated through the central nervous system in rats. J. Clin. Invest. 1993;91:1830–1833. doi: 10.1172/JCI116395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto S, et al. Increased cholecystokinin and pancreatic polypeptide responses to a fat-rich meal in patients with restrictive but not bulimic anorexia nervosa. Biol. Psychiatry. 1997;41:1068–1070. doi: 10.1016/S0006-3223(97)00044-9. doi:10.1016/S0006-3223(97)00044-9 [DOI] [PubMed] [Google Scholar]
- Funakoshi A, Miyazaki K, Nawata H. Effect of secretin and caerulein on pancreatic polypeptide and on insulin secretion from the isolated perfused ventral area of the rat pancreas. Regul. Pept. 1989;24:111–116. doi: 10.1016/0167-0115(89)90216-4. doi:10.1016/0167-0115(89)90216-4 [DOI] [PubMed] [Google Scholar]
- Gallwitz B, Witt M, Folsch U.R, Creutzfeldt W, Schmidt W.E. Binding specificity and signal transduction of receptors for glucagon-like peptide-1(7-36)amide and gastric inhibitory polypeptide on RINm5F insulinoma cells. J. Mol. Endocrinol. 1993;10:259–268. doi: 10.1677/jme.0.0100259. [DOI] [PubMed] [Google Scholar]
- Garthwaite T.L. Peripheral motilin administration stimulates feeding in fasted rats. Peptides. 1985;6:41–44. doi: 10.1016/0196-9781(85)90074-9. doi:10.1016/0196-9781(85)90074-9 [DOI] [PubMed] [Google Scholar]
- Gehlert D.R, Schober D.A, Beavers L, Gadski R, Hoffman J.A, Smiley D.L, Chance R.E, Lundell I, Larhammar D. Characterization of the peptide binding requirements for the cloned human pancreatic polypeptide-preferring receptor. Mol. Pharmacol. 1996;50:112–118. [PubMed] [Google Scholar]
- Gendall K.A, Kaye W.H, Altemus M, McConaha C.W, La Via M.C. Leptin, neuropeptide Y, and peptide YY in long-term recovered eating disorder patients. Biol. Psychiatry. 1999;46:292–299. doi: 10.1016/s0006-3223(98)00292-3. doi:10.1016/S0006-3223(98)00292-3 [DOI] [PubMed] [Google Scholar]
- Ghatei M.A, Uttenthal L.O, Christofides N.D, Bryant M.G, Bloom S.R. Molecular forms of human enteroglucagon in tissue and plasma: plasma responses to nutrient stimuli in health and in disorders of the upper gastrointestinal tract. J. Clin. Endocrinol. Metab. 1983;57:488–495. doi: 10.1210/jcem-57-3-488. [DOI] [PubMed] [Google Scholar]
- Gibbs J, Young R.C, Smith G.P. Cholecystokinin decreases food intake in rats. J. Comp. Physiol. Psychol. 1973;84:488–495. doi: 10.1037/h0034870. [DOI] [PubMed] [Google Scholar]
- Gingerich R.L, Akpan J.O, Gilbert W.R, Leith K.M, Hoffmann J.A, Chance R.E. Structural requirements of pancreatic polypeptide receptor binding. Am. J. Physiol. 1991;261:E319–E324. doi: 10.1152/ajpendo.1991.261.3.E319. [DOI] [PubMed] [Google Scholar]
- Glaser B, Zoghlin G, Pienta K, Vinik A.I. Pancreatic polypeptide response to secretin in obesity: effects of glucose intolerance. Horm. Metab. Res. 1988;20:288–292. doi: 10.1055/s-2007-1010817. [DOI] [PubMed] [Google Scholar]
- Glatzle J, Kalogeris T.J, Zittel T.T, Guerrini S, Tso P, Raybould H.E. Chylomicron components mediate intestinal lipid-induced inhibition of gastric motor function. Am. J. Physiol. Gastrointest. Liver Physiol. 2002;282:G86–G91. doi: 10.1152/ajpgi.2002.282.1.G86. [DOI] [PubMed] [Google Scholar]
- Gomez G, Udupi V, Greeley G.H., Jr Comparison of somatostatin and pancreastatin on secretion of gastrin, pancreatic polypeptide, and peptide YY. Proc. Soc. Exp. Biol. Med. 1997;215:165–167. doi: 10.3181/00379727-215-44123. [DOI] [PubMed] [Google Scholar]
- Gorrell M.D, Gysbers V, McCaughan G.W. CD26: a multifunctional integral membrane and secreted protein of activated lymphocytes. Scand. J. Immunol. 2001;54:249–264. doi: 10.1046/j.1365-3083.2001.00984.x. doi:10.1046/j.1365-3083.2001.00984.x [DOI] [PubMed] [Google Scholar]
- Grandt D, Schimiczek M, Beglinger C, Layer P, Goebell H, Eysselein V.E, Reeve J.R., Jr Two molecular forms of peptide YY (PYY) are abundant in human blood: characterization of a radioimmunoassay recognizing PYY 1-36 and PYY 3-36. Regul. Pept. 1994;51:151–159. doi: 10.1016/0167-0115(94)90204-6. doi:10.1016/0167-0115(94)90204-6 [DOI] [PubMed] [Google Scholar]
- Gustafson E.L, Smith K.E, Durkin M.M, Walker M.W, Gerald C, Weinshank R, Branchek T.A. Distribution of the neuropeptide Y Y2 receptor mRNA in rat central nervous system. Brain Res. Mol. Brain Res. 1997;46:223–235. doi: 10.1016/s0169-328x(97)00017-x. doi:10.1016/S0169-328X(97)00017-X [DOI] [PubMed] [Google Scholar]
- Gutzwiller J.P, Drewe J, Goke B, Schmidt H, Rohrer B, Lareida J, Beglinger C. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am. J. Physiol. 1999a;276:R1541–R1544. doi: 10.1152/ajpregu.1999.276.5.R1541. [DOI] [PubMed] [Google Scholar]
- Gutzwiller J.P, Goke B, Drewe J, Hildebrand P, Ketterer S, Handschin D, Winterhalder R, Conen D, Beglinger C. Glucagon-like peptide-1: a potent regulator of food intake in humans. Gut. 1999b;44:81–86. doi: 10.1136/gut.44.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halatchev I.G, Ellacott K.L, Fan W, Cone R.D. Peptide YY3-36 inhibits food intake in mice through a melanocortin-4 receptor-independent mechanism. Endocrinology. 2004;145:2585–2590. doi: 10.1210/en.2003-1754. doi:10.1210/en.2003-1754 [DOI] [PubMed] [Google Scholar]
- Hanusch-Enserer U, Roden M. News in gut–brain communication: a role of peptide YY (PYY) in human obesity and following bariatric surgery? Eur. J. Clin. Invest. 2005;35:425–430. doi: 10.1111/j.1365-2362.2005.01514.x. doi:10.1111/j.1365-2362.2005.01514.x [DOI] [PubMed] [Google Scholar]
- Hayes M.R, Moore R.L, Shah S.M, Covasa M. 5-HT3 receptors participate in CCK-induced suppression of food intake by delaying gastric emptying. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;287:R817–R823. doi: 10.1152/ajpregu.00295.2004. [DOI] [PubMed] [Google Scholar]
- Hoentjen F, Hopman W.P, Jansen J.B. Effect of circulating peptide YY on gallbladder emptying in humans. Scand. J. Gastroenterol. 2001;36:1086–1091. doi: 10.1080/003655201750422710. doi:10.1080/003655201750422710 [DOI] [PubMed] [Google Scholar]
- Holst J.J. On the physiology of GIP and GLP-1. Horm. Metab. Res. 2004;36:747–754. doi: 10.1055/s-2004-826158. doi:10.1055/s-2004-826158 [DOI] [PubMed] [Google Scholar]
- Holst J.J. Glucagon-like peptide-1: physiology and therapeutic potential. Curr. Opin. Endocrinol. Diab. 2005;12:56–62. doi:10.1097/01.med.0000151395.52819.47 [Google Scholar]
- Holst J.J, Sorensen T.I, Andersen A.N, Stadil F, Andersen B, Lauritsen K.B, Klein H.C. Plasma enteroglucagon after jejunoileal bypass with 3:1 or 1:3 jejunoileal ratio. Scand. J. Gastroenterol. 1979;14:205–207. doi: 10.3109/00365527909179871. [DOI] [PubMed] [Google Scholar]
- Holst J.J, Orskov C, Nielsen O.V, Schwartz T.W. Truncated glucagon-like peptide I, an insulin-releasing hormone from the distal gut. FEBS Lett. 1987;211:169–174. doi: 10.1016/0014-5793(87)81430-8. doi:10.1016/0014-5793(87)81430-8 [DOI] [PubMed] [Google Scholar]
- Hort Y, Baker E, Sutherland G.R, Shine J, Herzog H. Gene duplication of the human peptide YY gene (PYY) generated the pancreatic polypeptide gene (PPY) on chromosome 17q21.1. Genomics. 1995;26:77–83. doi: 10.1016/0888-7543(95)80085-z. doi:10.1016/0888-7543(95)80085-Z [DOI] [PubMed] [Google Scholar]
- Hutchison J.B, Dimaline R, Dockray G.J. Neuropeptides in the gut: quantification and characterization of cholecystokinin octapeptide-, bombesin- and vasoactive intestinal polypeptide-like immunoreactivities in the myenteric plexus of the guinea-pig small institute. Peptides. 1981;2:23–30. doi: 10.1016/s0196-9781(81)80007-1. [DOI] [PubMed] [Google Scholar]
- Inui A, Mizuno N, Ooya M, Suenaga K, Morioka H, Ogawa T, Ishida M, Baba S. Cross-reactivities of neuropeptide Y and peptide YY with pancreatic polypeptide antisera: evidence for the existence of pancreatic polypeptide in the brain. Brain Res. 1985;330:386–389. doi: 10.1016/0006-8993(85)90704-8. doi:10.1016/0006-8993(85)90704-8 [DOI] [PubMed] [Google Scholar]
- Itoh Z. Motilin and clinical application. Peptides. 1997;18:593–608. doi: 10.1016/s0196-9781(96)00333-6. doi:10.1016/S0196-9781(96)00333-6 [DOI] [PubMed] [Google Scholar]
- Jang J.Y, Kim S.W, Ku J.L, Park Y.H, Park J.G. Presence of CCK-A, B receptors and effect of gastrin and cholecystokinin on growth of pancreatobiliary cancer cell lines. World J. Gastroenterol. 2005;11:803–809. doi: 10.3748/wjg.v11.i6.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorde R, Burhol P.G. Effect of jejunoileal bypass operation and Billroth II resection on postprandial plasma pancreatic polypeptide release. Scand. J. Gastroenterol. 1982;17:613–617. doi: 10.3109/00365528209181067. [DOI] [PubMed] [Google Scholar]
- Jorde R, Burhol P.G. Fasting and postprandial plasma pancreatic polypeptide (PP) levels in obesity. Int. J. Obes. 1984;8:393–397. [PubMed] [Google Scholar]
- Kanatani A, et al. Role of the Y1 receptor in the regulation of neuropeptide Y-mediated feeding: comparison of wild-type, Y1 receptor-deficient, and Y5 receptor-deficient mice. Endocrinology. 2000;141:1011–1016. doi: 10.1210/endo.141.3.7387. doi:10.1210/en.141.3.1011 [DOI] [PubMed] [Google Scholar]
- Katsuura G, Asakawa A, Inui A. Roles of pancreatic polypeptide in regulation of food intake. Peptides. 2002;23:323–329. doi: 10.1016/s0196-9781(01)00604-0. doi:10.1016/S0196-9781(01)00604-0 [DOI] [PubMed] [Google Scholar]
- Kazanjian K.K, Towfigh S, McFadden D.W. Peptide YY exhibits a mitogenic effect on pancreatic cells while improving acute pancreatitis in vitro. J. Surg. Res. 2003;114:95–99. doi: 10.1016/s0022-4804(03)00218-x. doi:10.1016/S0022-4804(03)00218-X [DOI] [PubMed] [Google Scholar]
- Kieffer T.J, Habener J.F. The glucagon-like peptides. Endocr. Rev. 1999;20:876–913. doi: 10.1210/edrv.20.6.0385. doi:10.1210/er.20.6.876 [DOI] [PubMed] [Google Scholar]
- Kieffer T.J, McIntosh C.H, Pederson R.A. Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV. Endocrinology. 1995;136:3585–3596. doi: 10.1210/endo.136.8.7628397. doi:10.1210/en.136.8.3585 [DOI] [PubMed] [Google Scholar]
- Kinzig K.P, D'Alessio D.A, Seeley R.J. The diverse roles of specific GLP-1 receptors in the control of food intake and the response to visceral illness. J. Neurosci. 2002;22:10 470–10 476. doi: 10.1523/JNEUROSCI.22-23-10470.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissileff H.R, Pi-Sunyer F.X, Thornton J, Smith G.P. C-terminal octapeptide of cholecystokinin decreases food intake in man. Am. J. Clin. Nutr. 1981;34:154–160. doi: 10.1093/ajcn/34.2.154. [DOI] [PubMed] [Google Scholar]
- Kissileff H.R, Carretta J.C, Geliebter A, Pi-Sunyer F.X. Cholecystokinin and stomach distension combine to reduce food intake in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;285:R992–R998. doi: 10.1152/ajpregu.00272.2003. [DOI] [PubMed] [Google Scholar]
- Koda S, et al. The role of the vagal nerve in peripheral PYY3-36-induced feeding reduction in rats. Endocrinology. 2005;146:2369–2375. doi: 10.1210/en.2004-1266. doi:10.1210/en.2004-1266 [DOI] [PubMed] [Google Scholar]
- Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–660. doi: 10.1038/45230. doi:10.1038/45230 [DOI] [PubMed] [Google Scholar]
- Konturek S.J, Popiela T, Slowiaczek M, Bielanski W. Gastric acid and pancreatic polypeptide responses to modified sham feeding. Effects of truncal and parietal cell vagotomy. Gut. 1987;28:280–286. doi: 10.1136/gut.28.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korbonits M, Goldstone A.P, Gueorguiev M, Grossman A.B. Ghrelin—a hormone with multiple functions. Front. Neuroendocrinol. 2004;25:27–68. doi: 10.1016/j.yfrne.2004.03.002. doi:10.1016/j.yfrne.2004.03.002 [DOI] [PubMed] [Google Scholar]
- Korner J, Bessler M, Cirilo L.J, Conwell I.M, Daud A, Restuccia N.L, Wardlaw S.L. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J. Clin. Endocrinol. Metab. 2005;90:359–365. doi: 10.1210/jc.2004-1076. doi:10.1210/jc.2004-1076 [DOI] [PubMed] [Google Scholar]
- Kreymann B, Williams G, Ghatei M.A, Bloom S.R. Glucagon-like peptide-1 7-36: a physiological incretin in man. Lancet. 1987;2:1300–1304. doi: 10.1016/s0140-6736(87)91194-9. doi:10.1016/S0140-6736(87)91194-9 [DOI] [PubMed] [Google Scholar]
- Kreymann B, Ghatei M.A, Burnet P, Williams G, Kanse S, Diani A.R, Bloom S.R. Characterization of glucagon-like peptide-1-(7-36)amide in the hypothalamus. Brain Res. 1989;502:325–331. doi: 10.1016/0006-8993(89)90628-8. doi:10.1016/0006-8993(89)90628-8 [DOI] [PubMed] [Google Scholar]
- Lachey J.L, D'Alessio D.A, Rinaman L, Elmquist J.K, Drucker D.J, Seeley R.J. The role of central glucagon-like peptide-1 in mediating the effects of visceral illness: differential effects in rats and mice. Endocrinology. 2005;146:458–462. doi: 10.1210/en.2004-0419. doi:10.1210/en.2004-0419 [DOI] [PubMed] [Google Scholar]
- Larsen P.J, Kristensen P. The neuropeptide Y (Y4) receptor is highly expressed in neurones of the rat dorsal vagal complex. Brain Res. Mol. Brain Res. 1997;48:1–6. doi: 10.1016/s0169-328x(97)00069-7. doi:10.1016/S0169-328X(97)00069-7 [DOI] [PubMed] [Google Scholar]
- Larsen P.J, Tang-Christensen M, Holst J.J, Orskov C. Distribution of glucagon-like peptide-1 and other preproglucagon-derived peptides in the rat hypothalamus and brainstem. Neuroscience. 1997a;77:257–270. doi: 10.1016/s0306-4522(96)00434-4. doi:10.1016/S0306-4522(96)00434-4 [DOI] [PubMed] [Google Scholar]
- Larsen P.J, Tang-Christensen M, Jessop D.S. Central administration of glucagon-like peptide-1 activates hypothalamic neuroendocrine neurons in the rat. Endocrinology. 1997;138:4445–4455. doi: 10.1210/endo.138.10.5270. doi:10.1210/en.138.10.4445 [DOI] [PubMed] [Google Scholar]
- Larsson L.I, Sundler F, Hakanson R. Immunohistochemical localization of human pancreatic polypeptide (HPP) to a population of islet cells. Cell Tissue Res. 1975;156:167–171. doi: 10.1007/BF00221800. doi:10.1007/BF00221800 [DOI] [PubMed] [Google Scholar]
- Lassmann V, Vague P, Vialettes B, Simon M.C. Low plasma levels of pancreatic polypeptide in obesity. Diabetes. 1980;29:428–430. doi: 10.2337/diab.29.6.428. [DOI] [PubMed] [Google Scholar]
- Le Quellec A, Kervran A, Blache P, Ciurana A.J, Bataille D. Oxyntomodulin-like immunoreactivity: diurnal profile of a new potential enterogastrone. J. Clin. Endocrinol. Metab. 1992;74:1405–1409. doi: 10.1210/jcem.74.6.1592887. doi:10.1210/jc.74.6.1405 [DOI] [PubMed] [Google Scholar]
- Le Roux C.W, Ghatei M.A, Gibbs J.S, Bloom S.R. The putative satiety hormone PYY is raised in cardiac cachexia associated with primary pulmonary hypertension. Heart. 2005;91:241–242. doi: 10.1136/hrt.2003.026880. doi:10.1136/hrt.2003.026880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine A.S, Morley J.E. Peripherally administered somatostatin reduces feeding by a vagal mediated mechanism. Pharmacol. Biochem. Behav. 1982;16:897–902. doi: 10.1016/0091-3057(82)90041-7. doi:10.1016/0091-3057(82)90041-7 [DOI] [PubMed] [Google Scholar]
- Liddle R.A, Goldfine I.D, Rosen M.S, Taplitz R.A, Williams J.A. Cholecystokinin bioactivity in human plasma. Molecular forms, responses to feeding, and relationship to gallbladder contraction. J. Clin. Invest. 1985;75:1144–1152. doi: 10.1172/JCI111809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieverse R.J, Jansen J.B, van de Z.A, Samson L, Masclee A.A, Lamers C.B. Effects of a physiological dose of cholecystokinin on food intake and postprandial satiation in man. Regul. Pept. 1993;43:83–89. doi: 10.1016/0167-0115(93)90410-a. doi:10.1016/0167-0115(93)90410-A [DOI] [PubMed] [Google Scholar]
- Lin H.C, Chey W.Y. Cholecystokinin and peptide YY are released by fat in either proximal or distal small intestine in dogs. Regul. Pept. 2003;114:131–135. doi: 10.1016/s0167-0115(03)00115-0. doi:10.1016/S0167-0115(03)00115-0 [DOI] [PubMed] [Google Scholar]
- Lin H.C, Taylor I.L. Release of peptide YY by fat in the proximal but not distal gut depends on an atropine-sensitive cholinergic pathway. Regul. Pept. 2004;117:73–76. doi: 10.1016/j.regpep.2003.10.008. doi:10.1016/j.regpep.2003.10.008 [DOI] [PubMed] [Google Scholar]
- Liu M, Doi T, Shen L, Woods S.C, Seeley R.J, Zheng S, Jackman A, Tso P. Intestinal satiety protein apolipoprotein AIV is synthesized and regulated in rat hypothalamus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;280:R1382–R1387. doi: 10.1152/ajpregu.2001.280.5.R1382. [DOI] [PubMed] [Google Scholar]
- Liu M, Shen L, Doi T, Woods S.C, Seeley R.J, Tso P. Neuropeptide Y and lipid increase apolipoprotein AIV gene expression in rat hypothalamus. Brain Res. 2003;971:232–238. doi: 10.1016/s0006-8993(03)02402-8. doi:10.1016/S0006-8993(03)02402-8 [DOI] [PubMed] [Google Scholar]
- Lotter E.C, Krinsky R, McKay J.M, Treneer C.M, Porter D, Jr, Woods S.C. Somatostatin decreases food intake of rats and baboons. J. Comp. Physiol. Psychol. 1981;95:278–287. doi: 10.1037/h0077777. [DOI] [PubMed] [Google Scholar]
- Ludvik B, Kautzky-Willer A, Prager R, Thomaseth K, Pacini G. Amylin: history and overview. Diab. Med. 1997;14(Suppl. 2):S9–S13. doi: 10.1002/(sici)1096-9136(199706)14:2+<s9::aid-dia397>3.3.co;2-4. doi:10.1002/(SICI)1096-9136(199706)14:2+<S9::AID-DIA397>3.3.CO;2-4 [DOI] [PubMed] [Google Scholar]
- Lundell I, Blomqvist A.G, Berglund M.M, Schober D.A, Johnson D, Statnick M.A, Gadski R.A, Gehlert D.R, Larhammar D. Cloning of a human receptor of the NPY receptor family with high affinity for pancreatic polypeptide and peptide YY. J. Biol. Chem. 1995;270:29 123–29 128. doi: 10.1074/jbc.270.49.29123. doi:10.1074/jbc.270.49.29123 [DOI] [PubMed] [Google Scholar]
- Lutz T.A, Del P.E, Scharrer E. Reduction of food intake in rats by intraperitoneal injection of low doses of amylin. Physiol. Behav. 1994;55:891–895. doi: 10.1016/0031-9384(94)90076-0. doi:10.1016/0031-9384(94)90076-0 [DOI] [PubMed] [Google Scholar]
- Lutz T.A, Del P.E, Scharrer E. Subdiaphragmatic vagotomy does not influence the anorectic effect of amylin. Peptides. 1995;16:457–462. doi: 10.1016/0196-9781(94)00203-i. doi:10.1016/0196-9781(94)00203-I [DOI] [PubMed] [Google Scholar]
- Malaisse-Lagae F, Carpentier J.L, Patel Y.C, Malaisse W.J, Orci L. Pancreatic polypeptide: a possible role in the regulation of food intake in the mouse. Hypothesis. Experientia. 1977;33:915–917. doi: 10.1007/BF01951279. doi:10.1007/BF01951279 [DOI] [PubMed] [Google Scholar]
- Matson C.A, Reid D.F, Cannon T.A, Ritter R.C. Cholecystokinin and leptin act synergistically to reduce body weight. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000;278:R882–R890. doi: 10.1152/ajpregu.2000.278.4.R882. [DOI] [PubMed] [Google Scholar]
- McLaughlin C.L, Baile C.A, Buonomo F.C. Effect of CCK antibodies on food intake and weight gain in Zucker rats. Physiol. Behav. 1985;34:277–282. doi: 10.1016/0031-9384(85)90116-7. doi:10.1016/0031-9384(85)90116-7 [DOI] [PubMed] [Google Scholar]
- Meeran K, et al. Repeated intracerebroventricular administration of glucagon-like peptide-1-(7-36) amide or exendin-(9-39) alters body weight in the rat. Endocrinology. 1999;140:244–250. doi: 10.1210/endo.140.1.6421. doi:10.1210/en.140.1.244 [DOI] [PubMed] [Google Scholar]
- Meereis-Schwanke K, Klonowski-Stumpe H, Herberg L, Niederau C. Long-term effects of CCK-agonist and -antagonist on food intake and body weight in Zucker lean and obese rats. Peptides. 1998;19:291–299. doi: 10.1016/s0196-9781(97)00261-1. doi:10.1016/S0196-9781(97)00261-1 [DOI] [PubMed] [Google Scholar]
- Meguro T, Shimosegawa T, Kikuchi Y, Koizumi M, Toyota T. Effects of cisapride on gallbladder emptying and pancreatic polypeptide and cholecystokinin release in humans. J. Gastroenterol. 1995;30:237–243. doi: 10.1007/BF02348671. doi:10.1007/BF02348671 [DOI] [PubMed] [Google Scholar]
- Meier J.J, Nauck M.A, Schmidt W.E, Gallwitz B. Gastric inhibitory polypeptide: the neglected incretin revisited. Regul. Pept. 2002;107:1–13. doi: 10.1016/s0167-0115(02)00039-3. doi:10.1016/S0167-0115(02)00039-3 [DOI] [PubMed] [Google Scholar]
- Meryn S, Stein D, Straus E.W. Fasting- and meal-stimulated peptide hormone concentrations before and after gastric surgery for morbid obesity. Metabolism. 1986;35:798–802. doi: 10.1016/0026-0495(86)90218-0. doi:10.1016/0026-0495(86)90218-0 [DOI] [PubMed] [Google Scholar]
- Michel M.C, Beck-Sickinger A, Cox H, Doods H.N, Herzog H, Larhammar D, Quirion R, Schwartz T, Westfall T. XVI. International Union of Pharmacology recommendations for the nomenclature of neuropeptide Y, peptide YY, and pancreatic polypeptide receptors. Pharmacol. Rev. 1998;50:143–150. [PubMed] [Google Scholar]
- Miyasaka K, et al. Anxiety-related behaviors in cholecystokinin-A, B, and AB receptor gene knockout mice in the plus-maze. Neurosci. Lett. 2002;335:115–118. doi: 10.1016/s0304-3940(02)01176-x. doi:10.1016/S0304-3940(02)01176-X [DOI] [PubMed] [Google Scholar]
- Mochiki E, Inui A, Satoh M, Mizumoto A, Itoh Z. Motilin is a biosignal controlling cyclic release of pancreatic polypeptide via the vagus in fasted dogs. Am. J. Physiol. 1997;272:G224–G232. doi: 10.1152/ajpgi.1997.272.2.G224. [DOI] [PubMed] [Google Scholar]
- Mojsov S, Heinrich G, Wilson I.B, Ravazzola M, Orci L, Habener J.F. Preproglucagon gene expression in pancreas and intestine diversifies at the level of post-translational processing. J. Biol. Chem. 1986;261:11 880–11 889. [PubMed] [Google Scholar]
- Mojsov S, Weir G.C, Habener J.F. Insulinotropin: glucagon-like peptide I (7-37) co-encoded in the glucagon gene is a potent stimulator of insulin release in the perfused rat pancreas. J. Clin. Invest. 1987;79:616–619. doi: 10.1172/JCI112855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montrose-Rafizadeh C, Yang H, Wang Y, Roth J, Montrose M.H, Adams L.G. Novel signal transduction and peptide specificity of glucagon-like peptide receptor in 3T3-L1 adipocytes. J. Cell. Physiol. 1997;172:275–283. doi: 10.1002/(SICI)1097-4652(199709)172:3<275::AID-JCP1>3.0.CO;2-L. doi:10.1002/(SICI)1097-4652(199709)172:3<275::AID-JCP1>3.0.CO;2-L [DOI] [PubMed] [Google Scholar]
- Moran T.H, Kinzig K.P. Gastrointestinal satiety signals II. Cholecystokinin. Am. J. Physiol. Gastrointest. Liver Physiol. 2004;286:G183–G188. doi: 10.1152/ajpgi.00434.2003. doi:10.1152/ajpgi.00434.2003 [DOI] [PubMed] [Google Scholar]
- Moran T.H, McHugh P.R. Cholecystokinin suppresses food intake by inhibiting gastric emptying. Am. J. Physiol. 1982;242:R491–R497. doi: 10.1152/ajpregu.1982.242.5.R491. [DOI] [PubMed] [Google Scholar]
- Moran T.H, McHugh P.R. Gastric and nongastric mechanisms for satiety action of cholecystokinin. Am. J. Physiol. 1988;254:R628–R632. doi: 10.1152/ajpregu.1988.254.4.R628. [DOI] [PubMed] [Google Scholar]
- Moran T.H, Ameglio P.J, Schwartz G.J, McHugh P.R. Blockade of type A, not type B, CCK receptors attenuates satiety actions of exogenous and endogenous CCK. Am. J. Physiol. 1992;262:R46–R50. doi: 10.1152/ajpregu.1992.262.1.R46. [DOI] [PubMed] [Google Scholar]
- Moran T.H, Katz L.F, Plata-Salaman C.R, Schwartz G.J. Disordered food intake and obesity in rats lacking cholecystokinin A receptors. Am. J. Physiol. 1998;274:R618–R625. doi: 10.1152/ajpregu.1998.274.3.R618. [DOI] [PubMed] [Google Scholar]
- Moran T.H, Smedh U, Kinzig K.P, Scott K.A, Knipp S, Ladenheim E.E. Peptide YY(3-36) inhibits gastric emptying and produces acute reductions in food intake in rhesus monkeys. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;288:R384–R388. doi: 10.1152/ajpregu.00535.2004. [DOI] [PubMed] [Google Scholar]
- Morisset J, Wong H, Walsh J.H, Laine J, Bourassa J. Pancreatic CCK(B) receptors: their potential roles in somatostatin release and delta-cell proliferation. Am. J. Physiol. Gastrointest. Liver Physiol. 2000;279:G148–G156. doi: 10.1152/ajpgi.2000.279.1.G148. [DOI] [PubMed] [Google Scholar]
- Morley J.E, Levine A.S, Yamada T, Gebhard R.L, Prigge W.F, Shafer R.B, Goetz F.C, Silvis S.E. Effect of exorphins on gastrointestinal function, hormonal release, and appetite. Gastroenterology. 1983;84:1517–1523. [PubMed] [Google Scholar]
- Morley J.E, Levine A.S, Grace M, Kneip J. Peptide YY (PYY), a potent orexigenic agent. Brain Res. 1985;341:200–203. doi: 10.1016/0006-8993(85)91490-8. doi:10.1016/0006-8993(85)91490-8 [DOI] [PubMed] [Google Scholar]
- Morton G.J, Blevins J.E, Williams D.L, Niswender K.D, Gelling R.W, Rhodes C.J, Baskin D.G, Schwartz M.W. Leptin action in the forebrain regulates the hindbrain response to satiety signals. J. Clin. Invest. 2005;115:703–710. doi: 10.1172/JCI200522081. doi:10.1172/JCI200522081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins D.E, Zhang X, Hawes B.E. Activation of extracellular signal regulated protein kinase by neuropeptide Y and pancreatic polypeptide in CHO cells expressing the NPY Y(1), Y(2), Y(4) and Y(5) receptor subtypes. Regul. Pept. 2002;105:65–73. doi: 10.1016/s0167-0115(01)00388-3. doi:10.1016/S0167-0115(01)00388-3 [DOI] [PubMed] [Google Scholar]
- Munroe D.G, et al. Prototypic G protein-coupled receptor for the intestinotrophic factor glucagon-like peptide 2. Proc. Natl Acad. Sci. USA. 1999;96:1569–1573. doi: 10.1073/pnas.96.4.1569. doi:10.1073/pnas.96.4.1569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaya N, et al. Effects of ghrelin administration on left ventricular function, exercise capacity, and muscle wasting in patients with chronic heart failure. Circulation. 2004;110:3674–3679. doi: 10.1161/01.CIR.0000149746.62908.BB. doi:10.1161/01.CIR.0000149746.62908.BB [DOI] [PubMed] [Google Scholar]
- Naslund E, Barkeling B, King N, Gutniak M, Blundell J.E, Holst J.J, Rossner S, Hellstrom P.M. Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int. J. Obes. Relat. Metab. Disord. 1999a;23:304–311. doi: 10.1038/sj.ijo.0800818. doi:10.1038/sj.ijo.0800818 [DOI] [PubMed] [Google Scholar]
- Naslund E, Bogefors J, Skogar S, Gryback P, Jacobsson H, Holst J.J, Hellstrom P.M. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am. J. Physiol. 1999b;277:R910–R916. doi: 10.1152/ajpregu.1999.277.3.R910. [DOI] [PubMed] [Google Scholar]
- Naslund E, King N, Mansten S, Adner N, Holst J.J, Gutniak M, Hellstrom P.M. Prandial subcutaneous injections of glucagon-like peptide-1 cause weight loss in obese human subjects. Br. J. Nutr. 2004;91:439–446. doi: 10.1079/BJN20031064. doi:10.1079/BJN20031064 [DOI] [PubMed] [Google Scholar]
- Neary N.M, et al. Ghrelin increases energy intake in cancer patients with impaired appetite: acute, randomized, placebo-controlled trial. J. Clin. Endocrinol. Metab. 2004;89:2832–2836. doi: 10.1210/jc.2003-031768. doi:10.1210/jc.2003-031768 [DOI] [PubMed] [Google Scholar]
- Niebel W, Eysselein V.E, Singer M.V. Pancreatic polypeptide response to a meal before and after cutting the extrinsic nerves of the upper gastrointestinal tract and the pancreas in the dog. Dig. Dis. Sci. 1987;32:1004–1009. doi: 10.1007/BF01297191. doi:10.1007/BF01297191 [DOI] [PubMed] [Google Scholar]
- Nikolaidis L.A, Mankad S, Sokos G.G, Miske G, Shah A, Elahi D, Shannon R.P. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation. 2004;109:962–965. doi: 10.1161/01.CIR.0000120505.91348.58. doi:10.1161/01.CIR.0000120505.91348.58 [DOI] [PubMed] [Google Scholar]
- Nilaver G, Beinfeld M.C, Bond C.T, Daikh D, Godfrey B, Adelman J.P. Heterogeneity of motilin immunoreactivity in mammalian tissue. Synapse. 1988;2:266–275. doi: 10.1002/syn.890020315. doi:10.1002/syn.890020315 [DOI] [PubMed] [Google Scholar]
- O'Donohue T.L, et al. Identification, characterization and distribution of motilin immunoreactivity in the rat central nervous system. Peptides. 1981;2:467–477. doi: 10.1016/s0196-9781(81)80106-4. [DOI] [PubMed] [Google Scholar]
- Okumura T, Fukagawa K, Tso P, Taylor I.L, Pappas T.N. Apolipoprotein A-IV acts in the brain to inhibit gastric emptying in the rat. Am. J. Physiol. 1996;270:G49–G53. doi: 10.1152/ajpgi.1996.270.1.G49. [DOI] [PubMed] [Google Scholar]
- Olson R.D, Kastin A.J, von Almen T.K, Coy D.H, Olson G.A. Systemic injections of gastro-intestinal peptides alter behavior in rats. Peptides. 1980;1:383–385. doi: 10.1016/0196-9781(80)90018-2. doi:10.1016/0196-9781(80)90018-2 [DOI] [PubMed] [Google Scholar]
- Olszewski P.K, Wirth M.M, Shaw T.J, Grace M.K, Levine A.S. Peptides that regulate food intake: effect of peptide histidine isoleucine on consummatory behavior in rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;284:R1445–R1453. doi: 10.1152/ajpregu.00554.2002. [DOI] [PubMed] [Google Scholar]
- Onaga T, Zabielski R, Kato S. Multiple regulation of peptide YY secretion in the digestive tract. Peptides. 2002;23:279–290. doi: 10.1016/s0196-9781(01)00609-x. doi:10.1016/S0196-9781(01)00609-X [DOI] [PubMed] [Google Scholar]
- Orskov C, Rabenhoj L, Wettergren A, Kofod H, Holst J.J. Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes. 1994a;43:535–539. doi: 10.2337/diab.43.4.535. [DOI] [PubMed] [Google Scholar]
- Orskov C, Rabenhoj L, Wettergren A, Kofod H, Holst J.J. Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes. 1994b;43:535–539. doi: 10.2337/diab.43.4.535. [DOI] [PubMed] [Google Scholar]
- Orskov C, Poulsen S.S, Moller M, Holst J.J. Glucagon-like peptide I receptors in the subfornical organ and the area postrema are accessible to circulating glucagon-like peptide I. Diabetes. 1996;45:832–835. doi: 10.2337/diab.45.6.832. [DOI] [PubMed] [Google Scholar]
- Parker R.M, Herzog H. Regional distribution of Y-receptor subtype mRNAs in rat brain. Eur. J. Neurosci. 1999;11:1431–1448. doi: 10.1046/j.1460-9568.1999.00553.x. doi:10.1046/j.1460-9568.1999.00553.x [DOI] [PubMed] [Google Scholar]
- Peruzzo B, Pastor F.E, Blazquez J.L, Schobitz K, Pelaez B, Amat P, Rodriguez E.M. A second look at the barriers of the medial basal hypothalamus. Exp. Brain Res. 2000;132:10–26. doi: 10.1007/s002219900289. doi:10.1007/s002219900289 [DOI] [PubMed] [Google Scholar]
- Peters J.H, McKay B.M, Simasko S.M, Ritter R.C. Leptin-induced satiation mediated by abdominal vagal afferents. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;288:R879–R884. doi: 10.1152/ajpregu.00716.2004. [DOI] [PubMed] [Google Scholar]
- Pittner R.A, et al. Effects of PYY[3-36] in rodent models of diabetes and obesity. Int. J. Obes. Relat. Metab. Disord. 2004;28:963–971. doi: 10.1038/sj.ijo.0802696. doi:10.1038/sj.ijo.0802696 [DOI] [PubMed] [Google Scholar]
- Rehfeld J.F. How to measure cholecystokinin in tissue, plasma and cerebrospinal fluid. Regul. Pept. 1998;78:31–39. doi: 10.1016/s0167-0115(98)00133-5. doi:10.1016/S0167-0115(98)00133-5 [DOI] [PubMed] [Google Scholar]
- Rehfeld J.F. Clinical endocrinology and metabolism. Cholecystokinin. Best Pract. Res. Clin. Endocrinol. Metab. 2004;18:569–586. doi: 10.1016/j.beem.2004.07.002. doi:10.1016/j.beem.2004.07.002 [DOI] [PubMed] [Google Scholar]
- Rehfeld J.F, Sun G, Christensen T, Hillingso J.G. The predominant cholecystokinin in human plasma and intestine is cholecystokinin-33. J. Clin. Endocrinol. Metab. 2001;86:251–258. doi: 10.1210/jcem.86.1.7148. doi:10.1210/jc.86.1.251 [DOI] [PubMed] [Google Scholar]
- Rehfeld J.F, Bungaard J.R, Friis-Hansen L, Goetze J.P. On the tissue-specific processing of procholecystokinin in the brain and gut—a short review. J. Physiol. Pharmacol. 2003;54(Suppl. 4):73–79. [PubMed] [Google Scholar]
- Reichlin S. Somatostatin. N. Engl. J. Med. 1983;309:1495–1501. doi: 10.1056/NEJM198312153092406. [DOI] [PubMed] [Google Scholar]
- Roberge J.N, Brubaker P.L. Secretion of proglucagon-derived peptides in response to intestinal luminal nutrients. Endocrinology. 1991;128:3169–3174. doi: 10.1210/endo-128-6-3169. [DOI] [PubMed] [Google Scholar]
- Rocca A.S, Brubaker P.L. Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology. 1999;140:1687–1694. doi: 10.1210/endo.140.4.6643. doi:10.1210/en.140.4.1687 [DOI] [PubMed] [Google Scholar]
- Rosenfeld D.J, Garthwaite T.L. Central administration of motilin stimulates feeding in rats. Physiol. Behav. 1987;39:753–756. doi: 10.1016/0031-9384(87)90261-7. doi:10.1016/0031-9384(87)90261-7 [DOI] [PubMed] [Google Scholar]
- Rowland N.E, Crews E.C, Gentry R.M. Comparison of Fos induced in rat brain by GLP-1 and amylin. Regul. Pept. 1997;71:171–174. doi: 10.1016/s0167-0115(97)01034-3. doi:10.1016/S0167-0115(97)01034-3 [DOI] [PubMed] [Google Scholar]
- Rushing P.A, Hagan M.M, Seeley R.J, Lutz T.A, Woods S.C. Amylin: a novel action in the brain to reduce body weight. Endocrinology. 2000;141:850–853. doi: 10.1210/endo.141.2.7378. doi:10.1210/en.141.2.850 [DOI] [PubMed] [Google Scholar]
- Sanjuan J, Toirac I, Gonzalez J.C, Leal C, Molto M.D, Najera C, De F.R. A possible association between the CCK-AR gene and persistent auditory hallucinations in schizophrenia. Eur. Psychiatry. 2004;19:349–353. doi: 10.1016/j.eurpsy.2004.06.015. [DOI] [PubMed] [Google Scholar]
- Sarson D.L, Scopinaro N, Bloom S.R. Gut hormone changes after jejunoileal (JIB) or biliopancreatic (BPB) bypass surgery for morbid obesity. Int. J. Obes. 1981;5:471–480. [PubMed] [Google Scholar]
- Schepp W, Dehne K, Riedel T, Schmidtler J, Schaffer K, Classen M. Oxyntomodulin: a cAMP-dependent stimulus of rat parietal cell function via the receptor for glucagon-like peptide-1 (7-36)NH2. Digestion. 1996;57:398–405. doi: 10.1159/000201367. [DOI] [PubMed] [Google Scholar]
- Schjoldager B.T, Baldissera F.G, Mortensen P.E, Holst J.J, Christiansen J. Oxyntomodulin: a potential hormone from the distal gut. Pharmacokinetics and effects on gastric acid and insulin secretion in man. Eur. J. Clin. Invest. 1988;18:499–503. doi: 10.1111/j.1365-2362.1988.tb01046.x. [DOI] [PubMed] [Google Scholar]
- Schjoldager B, Mortensen P.E, Myhre J, Christiansen J, Holst J.J. Oxyntomodulin from distal gut. Role in regulation of gastric and pancreatic functions. Dig. Dis. Sci. 1989;34:1411–1419. doi: 10.1007/BF01538078. doi:10.1007/BF01538078 [DOI] [PubMed] [Google Scholar]
- Schmidt W.E, Siegel E.G, Creutzfeldt W. Glucagon-like peptide-1 but not glucagon-like peptide-2 stimulates insulin release from isolated rat pancreatic islets. Diabetologia. 1985;28:704–707. doi: 10.1007/BF00291980. doi:10.1007/BF00291980 [DOI] [PubMed] [Google Scholar]
- Schmidt P.T, Naslund E, Gryback P, Jacobsson H, Hartmann B, Holst J.J, Hellstrom P.M. Peripheral administration of GLP-2 to humans has no effect on gastric emptying or satiety. Regul. Pept. 2003;116:21–25. doi: 10.1016/s0167-0115(03)00175-7. doi:10.1016/S0167-0115(03)00175-7 [DOI] [PubMed] [Google Scholar]
- Schmidt P.T, Naslund E, Gryback P, Jacobsson H, Holst J.J, Hilsted L, Hellstrom P.M. A role for pancreatic polypeptide in the regulation of gastric emptying and short term metabolic control. J. Clin. Endocrinol. Metab. 2005;90:5241–5246. doi: 10.1210/jc.2004-2089. doi:10.1210/jc.2004-2089 [DOI] [PubMed] [Google Scholar]
- Schwartz G.J, Whitney A, Skoglund C, Castonguay T.W, Moran T.H. Decreased responsiveness to dietary fat in Otsuka Long–Evans Tokushima fatty rats lacking CCK-A receptors. Am. J. Physiol. 1999;277:R1144–R1151. doi: 10.1152/ajpregu.1999.277.4.R1144. [DOI] [PubMed] [Google Scholar]
- Schwartz M.W, Woods S.C, Porte D, Jr, Seeley R.J, Baskin D.G. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- Scott R.B, Kirk D, MacNaughton W.K, Meddings J.B. GLP-2 augments the adaptive response to massive intestinal resection in rat. Am. J. Physiol. 1998;275:G911–G921. doi: 10.1152/ajpgi.1998.275.5.G911. [DOI] [PubMed] [Google Scholar]
- Scott V, Kimura N, Stark J.A, Luckman S.M. Intravenous peptide YY3-36 and Y2 receptor antagonism in the rat: effects on feeding behaviour. J. Neuroendocrinol. 2005;17:452–457. doi: 10.1111/j.1365-2826.2005.01330.x. doi:10.1111/j.1365-2826.2005.01330.x [DOI] [PubMed] [Google Scholar]
- Scrocchi L.A, Brown T.J, MaClusky N, Brubaker P.L, Auerbach A.B, Joyner A.L, Drucker D.J. Glucose intolerance but normal satiety in mice with a null mutation in the glucagon-like peptide 1 receptor gene. Nat. Med. 1996;2:1254–1258. doi: 10.1038/nm1196-1254. doi:10.1038/nm1196-1254 [DOI] [PubMed] [Google Scholar]
- Seeley R.J, Blake K, Rushing P.A, Benoit S, Eng J, Woods S.C, D'Alessio D. The role of CNS glucagon-like peptide-1 (7-36) amide receptors in mediating the visceral illness effects of lithium chloride. J. Neurosci. 2000;20:1616–1621. doi: 10.1523/JNEUROSCI.20-04-01616.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Service G.J, Thompson G.B, Service F.J, Andrews J.C, Collazo-Clavell M.L, Lloyd R.V. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N. Engl. J. Med. 2005;353:249–254. doi: 10.1056/NEJMoa043690. doi:10.1056/NEJMoa043690 [DOI] [PubMed] [Google Scholar]
- Shughrue P.J, Lane M.V, Merchenthaler I. Glucagon-like peptide-1 receptor (GLP1-R) mRNA in the rat hypothalamus. Endocrinology. 1996;137:5159–5162. doi: 10.1210/endo.137.11.8895391. doi:10.1210/en.137.11.5159 [DOI] [PubMed] [Google Scholar]
- Silva A.P, Bethmann K, Raulf F, Schmid H.A. Regulation of ghrelin secretion by somatostatin analogs in rats. Eur. J. Endocrinol. 2005;152:887–894. doi: 10.1530/eje.1.01914. doi:10.1530/eje.1.01914 [DOI] [PubMed] [Google Scholar]
- Smith-White M.A, Hardy T.A, Brock J.A, Potter E.K. Effects of a selective neuropeptide Y Y2 receptor antagonist, BIIE0246, on Y2 receptors at peripheral neuroeffector junctions. Br. J. Pharmacol. 2001;132:861–868. doi: 10.1038/sj.bjp.0703879. doi:10.1038/sj.bjp.0703879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talsania T, Anini Y, Siu S, Drucker D.J, Brubaker P.L. Peripheral exendin-4 and peptide YY3-36 synergistically reduce food intake through different mechanisms in mice. Endocrinology. 2005;146:3748–3756. doi: 10.1210/en.2005-0473. doi:10.1210/en.2005-0473 [DOI] [PubMed] [Google Scholar]
- Tang-Christensen M, Larsen P.J, Thulesen J, Romer J, Vrang N. The proglucagon-derived peptide, glucagon-like peptide-2, is a neurotransmitter involved in the regulation of food intake. Nat. Med. 2000;6:802–807. doi: 10.1038/77535. doi:10.1038/77535 [DOI] [PubMed] [Google Scholar]
- Tang-Christensen M, Vrang N, Larsen P.J. Glucagon-like peptide containing pathways in the regulation of feeding behaviour. Int. J. Obes. Relat. Metab. Disord. 2001;25(Suppl. 5):S42–S47. doi: 10.1038/sj.ijo.0801912. [DOI] [PubMed] [Google Scholar]
- Tatemoto K. Isolation and characterization of peptide YY (PYY), a candidate gut hormone that inhibits pancreatic exocrine secretion. Proc. Natl Acad. Sci. USA. 1982;79:2514–2518. doi: 10.1073/pnas.79.8.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Horst G.J, de Boer P, Luiten P.G, van Willigen J.D. Ascending projections from the solitary tract nucleus to the hypothalamus. A Phaseolus vulgaris lectin tracing study in the rat. Neuroscience. 1989;31:785–797. doi: 10.1016/0306-4522(89)90441-7. doi:10.1016/0306-4522(89)90441-7 [DOI] [PubMed] [Google Scholar]
- Thorens B. Expression cloning of the pancreatic beta cell receptor for the gluco-incretin hormone glucagon-like peptide 1. Proc. Natl Acad. Sci. USA. 1992;89:8641–8645. doi: 10.1073/pnas.89.18.8641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorens B, Porret A, Buhler L, Deng S.P, Morel P, Widmann C. Cloning and functional expression of the human islet GLP-1 receptor. Demonstration that exendin-4 is an agonist and exendin-(9-39) an antagonist of the receptor. Diabetes. 1993;42:1678–1682. doi: 10.2337/diab.42.11.1678. [DOI] [PubMed] [Google Scholar]
- Tolessa T, Gutniak M, Holst J.J, Efendic S, Hellstrom P.M. Inhibitory effect of glucagon-like peptide-1 on small bowel motility. Fasting but not fed motility inhibited via nitric oxide independently of insulin and somatostatin. J. Clin. Invest. 1998;102:764–774. doi: 10.1172/JCI942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Track N.S, McLeod R.S, Mee A.V. Human pancreatic polypeptide: studies of fasting and postprandial plasma concentrations. Can. J. Physiol. Pharmacol. 1980;58:1484–1489. doi: 10.1139/y80-223. [DOI] [PubMed] [Google Scholar]
- Tschop M, Smiley D.L, Heiman M.L. Ghrelin induces adiposity in rodents. Nature. 2000;407:908–913. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- Tschop M, Weyer C, Tataranni P.A, Devanarayan V, Ravussin E, Heiman M.L. Circulating ghrelin levels are decreased in human obesity. Diabetes. 2001;50:707–709. doi: 10.2337/diabetes.50.4.707. [DOI] [PubMed] [Google Scholar]
- Tschop M, et al. Physiology: does gut hormone PYY3-36 decrease food intake in rodents? Nature. 2004;430 doi: 10.1038/nature02665. doi:101038/nature02665 [DOI] [PubMed] [Google Scholar]
- Turton M.D, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379:69–72. doi: 10.1038/379069a0. doi:10.1038/379069a0 [DOI] [PubMed] [Google Scholar]
- Uhe A.M, Szmukler G.I, Collier G.R, Hansky J, O'Dea K, Young G.P. Potential regulators of feeding behavior in anorexia nervosa. Am. J. Clin. Nutr. 1992;55:28–32. doi: 10.1093/ajcn/55.1.28. [DOI] [PubMed] [Google Scholar]
- Usellini L, Buchan A.M, Polak J.M, Capella C, Cornaggia M, Solcia E. Ultrastructural localization of motilin in endocrine cells of human and dog intestine by the immunogold technique. Histochemistry. 1984;81:363–368. doi: 10.1007/BF00514330. doi:10.1007/BF00514330 [DOI] [PubMed] [Google Scholar]
- van der Kooy D, Koda L.Y, McGinty J.F, Gerfen C.R, Bloom F.E. The organization of projections from the cortex, amygdala, and hypothalamus to the nucleus of the solitary tract in rat. J. Comp. Neurol. 1984;224:1–24. doi: 10.1002/cne.902240102. doi:10.1002/cne.902240102 [DOI] [PubMed] [Google Scholar]
- van der Lely A.J, Tschop M, Heiman M.L, Ghigo E. Biological, physiological, pathophysiological, and pharmacological aspects of ghrelin. Endocr. Rev. 2004;25:426–457. doi: 10.1210/er.2002-0029. doi:10.1210/er.2002-0029 [DOI] [PubMed] [Google Scholar]
- van Dijk G, Thiele T.E, Donahey J.C, Campfield L.A, Smith F.J, Burn P, Bernstein I.L, Woods S.C, Seeley R.J. Central infusions of leptin and GLP-1-(7-36) amide differentially stimulate c-FLI in the rat brain. Am. J. Physiol. 1996;271:R1096–R1100. doi: 10.1152/ajpregu.1996.271.4.R1096. [DOI] [PubMed] [Google Scholar]
- Verdich C, et al. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J. Clin. Endocrinol. Metab. 2001a;86:4382–4389. doi: 10.1210/jcem.86.9.7877. doi:10.1210/jc.86.9.4382 [DOI] [PubMed] [Google Scholar]
- Verdich C, Toubro S, Buemann B, Lysgard M.J, Juul H.J, Astrup A. The role of postprandial releases of insulin and incretin hormones in meal-induced satiety—effect of obesity and weight reduction. Int. J. Obes. Relat. Metab. Disord. 2001b;25:1206–1214. doi: 10.1038/sj.ijo.0801655. doi:10.1038/sj.ijo.0801655 [DOI] [PubMed] [Google Scholar]
- Vilsboll T, Krarup T, Sonne J, Madsbad S, Volund A, Juul A.G, Holst J.J. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 2003;88:2706–2713. doi: 10.1210/jc.2002-021873. doi:10.1210/jc.2002-021873 [DOI] [PubMed] [Google Scholar]
- Wank S.A. Cholecystokinin receptors. Am. J. Physiol. 1995;269:G628–G646. doi: 10.1152/ajpgi.1995.269.5.G628. [DOI] [PubMed] [Google Scholar]
- Wei Y, Mojsov S. Tissue-specific expression of the human receptor for glucagon-like peptide-I: brain, heart and pancreatic forms have the same deduced amino acid sequences. FEBS Lett. 1995;358:219–224. doi: 10.1016/0014-5793(94)01430-9. doi:10.1016/0014-5793(94)01430-9 [DOI] [PubMed] [Google Scholar]
- West D.B, Fey D, Woods S.C. Cholecystokinin persistently suppresses meal size but not food intake in free-feeding rats. Am. J. Physiol. 1984;246:R776–R787. doi: 10.1152/ajpregu.1984.246.5.R776. [DOI] [PubMed] [Google Scholar]
- West D.B, Greenwood M.R, Marshall K.A, Woods S.C. Lithium chloride, cholecystokinin and meal patterns: evidence that cholecystokinin suppresses meal size in rats without causing malaise. Appetite. 1987a;8:221–227. doi: 10.1016/0195-6663(87)90021-3. doi:10.1016/0195-6663(87)90021-3 [DOI] [PubMed] [Google Scholar]
- West D.B, Greenwood M.R, Sullivan A.C, Prescod L, Marzullo L.R, Triscari J. Infusion of cholecystokinin between meals into free-feeding rats fails to prolong the intermeal interval. Physiol. Behav. 1987b;39:111–115. doi: 10.1016/0031-9384(87)90407-0. doi:10.1016/0031-9384(87)90407-0 [DOI] [PubMed] [Google Scholar]
- Wettergren A, Maina P, Boesby S, Holst J.J. Glucagon-like peptide-1 7-36 amide and peptide YY have additive inhibitory effect on gastric acid secretion in man. Scand. J. Gastroenterol. 1997;32:552–555. doi: 10.3109/00365529709025098. [DOI] [PubMed] [Google Scholar]
- Wheeler M.B, Gelling R.W, McIntosh C.H, Georgiou J, Brown J.C, Pederson R.A. Functional expression of the rat pancreatic islet glucose-dependent insulinotropic polypeptide receptor: ligand binding and intracellular signaling properties. Endocrinology. 1995;136:4629–4639. doi: 10.1210/endo.136.10.7664683. doi:10.1210/en.136.10.4629 [DOI] [PubMed] [Google Scholar]
- Whitcomb D.C, Taylor I.L, Vigna S.R. Characterization of saturable binding sites for circulating pancreatic polypeptide in rat brain. Am. J. Physiol. 1990;259:G687–G691. doi: 10.1152/ajpgi.1990.259.4.G687. [DOI] [PubMed] [Google Scholar]
- Wisen O, Bjorvell H, Cantor P, Johansson C, Theodorsson E. Plasma concentrations of regulatory peptides in obesity following modified sham feeding (MSF) and a liquid test meal. Regul. Pept. 1992;39:43–54. doi: 10.1016/0167-0115(92)90007-h. doi:10.1016/0167-0115(92)90007-H [DOI] [PubMed] [Google Scholar]
- Woods S.C, West D.B, Stein L.J, McKay L.D, Lotter E.C, Porte S.G, Kenney N.J, Porte D., Jr Peptides and the control of meal size. Diabetologia. 1981;20:305–313. doi: 10.1007/BF00254497. doi:10.1007/BF00254497 [DOI] [PubMed] [Google Scholar]
- Wren A.M, Seal L.J, Cohen M.A, Brynes A.E, Frost G.S, Murphy K.G, Dhillo W.S, Ghatei M.A, Bloom S.R. Ghrelin enhances appetite and increases food intake in humans. J. Clin. Endocrinol. Metab. 2001a;86:5992. doi: 10.1210/jcem.86.12.8111. doi:10.1210/jc.86.12.5992 [DOI] [PubMed] [Google Scholar]
- Wren A.M, et al. Ghrelin causes hyperphagia and obesity in rats. Diabetes. 2001b;50:2540–2547. doi: 10.2337/diabetes.50.11.2540. [DOI] [PubMed] [Google Scholar]
- Wynne K, et al. Subcutaneous ghrelin enhances acute food intake in malnourished patients who receive maintenance peritoneal dialysis: a randomized, placebo-controlled trial. J. Am. Soc. Nephrol. 2005a;16:2111–2118. doi: 10.1681/ASN.2005010039. doi:10.1681/ASN.2005010039 [DOI] [PubMed] [Google Scholar]
- Wynne K, et al. Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial. Diabetes. 2005b;54:2390–2395. doi: 10.2337/diabetes.54.8.2390. [DOI] [PubMed] [Google Scholar]
- Xiao Q, Boushey R.P, Drucker D.J, Brubaker P.L. Secretion of the intestinotropic hormone glucagon-like peptide 2 is differentially regulated by nutrients in humans. Gastroenterology. 1999;117:99–105. doi: 10.1016/s0016-5085(99)70555-x. doi:10.1016/S0016-5085(99)70555-X [DOI] [PubMed] [Google Scholar]
- Yamamoto H, et al. Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. J. Clin. Invest. 2002;110:43–52. doi: 10.1172/JCI15595. doi:10.1172/JCI200215595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Egan J.M, Wang Y, Moyes C.D, Roth J, Montrose M.H, Montrose-Rafizadeh C. GLP-1 action in L6 myotubes is via a receptor different from the pancreatic GLP-1 receptor. Am. J. Physiol. 1998;275:C675–C683. doi: 10.1152/ajpcell.1998.275.3.C675. [DOI] [PubMed] [Google Scholar]
- Yusta B, Huang L, Munroe D, Wolff G, Fantaske R, Sharma S, Demchyshyn L, Asa S.L, Drucker D.J. Enteroendocrine localization of GLP-2 receptor expression in humans and rodents. Gastroenterology. 2000;119:744–755. doi: 10.1053/gast.2000.16489. doi:10.1053/gast.2000.16489 [DOI] [PubMed] [Google Scholar]
- Zachrisson O, de B.J, Wendt K.R, Hirsch S, Lindefors N. Cholecystokinin CCK(B) receptor mRNA isoforms: expression in schizophrenic brains. Neuroreport. 1999;10:3265–3268. doi: 10.1097/00001756-199911080-00003. [DOI] [PubMed] [Google Scholar]
- Zipf W.B, O'Dorisio T.M, Cataland S, Sotos J. Blunted pancreatic polypeptide responses in children with obesity of Prader–Willi syndrome. J. Clin. Endocrinol. Metab. 1981;52:1264–1266. doi: 10.1210/jcem-52-6-1264. [DOI] [PubMed] [Google Scholar]
- Zittel T.T, Glatzle J, Kreis M.E, Starlinger M, Eichner M, Raybould H.E, Becker H.D, Jehle E.C. C-fos protein expression in the nucleus of the solitary tract correlates with cholecystokinin dose injected and food intake in rats. Brain Res. 1999;846:1–11. doi: 10.1016/s0006-8993(99)01842-9. doi:10.1016/S0006-8993(99)01842-9 [DOI] [PubMed] [Google Scholar]