Abstract
Objective: To compare the effects of 3 treatments on ankle dorsiflexion range of motion: prolonged long-duration stretching, pulsed shortwave diathermy followed by stretching, and pulsed shortwave diathermy, stretching, and ice combined.
Design and Setting: A 2 × 5 × 15 repeated-measures (on 2 factors) design guided this study. Range-of-motion change in triceps surae flexibility was the dependent variable. The 3 independent variables were treatment group, pretest and posttest measurements, and day. Treatment group had 4 levels: control, stretching (10 minutes of stretching via the weight and pulley), diathermy and stretching (20 minutes of diathermy and 10 minutes of stretching), and diathermy, stretching, and ice (20 minutes of diathermy, 10 minutes of stretching applied after 15 minutes of diathermy, and 5 minutes of ice applied during the last 5 minutes of stretching). Each subject received 14 treatments throughout 3 weeks, with a follow-up measurement taken 6 days after the last treatment.
Subjects: Forty-four healthy college-student volunteers not involved in any flexibility program.
Measurements: We measured ankle dorsiflexion using a digital inclinometer before and after treatment.
Results: After 14 days of treatment, the range-of-motion increase was greater after heat and stretching than after stretching alone. After 6 additional days of rest, the heat and stretching range-of-motion increase was greater than that for stretching alone.
Conclusion: Pulsed shortwave diathermy application before prolonged long-duration static stretching was more effective than stretching alone in increasing flexibility throughout 3 weeks. After 14 treatments, prolonged long-duration stretching combined with pulsed shortwave diathermy followed by ice application caused greater immediate and net range-of-motion increases than prolonged long-duration stretching alone.
Keywords: ice, deep heating, flexibility
Flexibility programs are used clinically for their many benefits, including muscle relaxation, posture improvement, body symmetry, relief of low-back pain, relief of muscle cramps and soreness, and injury prevention.1,2 To improve the effects of stretching, combinations of heat and stretching have been used by clinicians in a variety of ways.3–6 Deep vigorous heating in combination with stretching requires a temperature increase of more than 4°C over core temperature at a depth of 3 to 5 cm without damaging superficial tissue.7 Deep heating is thought to lessen nerve sensitivity, increase blood flow, increase tissue metabolism, decrease muscle spindle sensitivity to stretch, cause muscle relaxation, and increase tissue flexibility.7 It is assumed that, when used in conjunction with stretching, the benefits of deep vigorous heating allow greater tissue flexibility than stretching alone.
Researchers previously studied heat and stretching techniques by using hot packs, whirlpools, and ultrasound as thermal agents. Ice has been applied after stretching in an effort to cool tissues in their elongated state.7 These studies on animals and humans have produced mixed results.3,4,7–11
Pulsed shortwave diathermy is used for deep vigorous heating.12 Used clinically, it heats tissue at depths of 3 to 5 cm by transferring energy into deep tissue through high-frequency current.12 Tissue temperature is controlled by the length of application, with maximum increases of 4°C to 6°C.12 Diathermy heats large areas of muscle and, as such, may be more suitable than ultrasound for improving flexibility in large muscles.13
The purposes of our study were to compare the effects of combining pulsed shortwave diathermy, with or without ice, with prolonged long-duration calf stretching on (1) daily (short-term) changes in flexibility, (2) day-to-day (long-term) changes in flexibility, and (3) retention of flexibility 6 days after cessation of treatment.
METHODS
A 2 × 5 × 15 repeated-measures (on 2 factors) design guided this study. Triceps surae flexibility, measured by range-of-motion (ROM) change, was the dependent variable. The 3 independent variables were treatment mode, pretest and posttest measurements, and day. Change in ROM was affected by one independent variable: the treatment mode. Treatment mode had 5 possible interventions, including control, control with measurements, stretching only, diathermy and stretching, and diathermy, stretching, and ice. Each independent variable was compared with the control group.
Subjects
Sixty healthy college students volunteered to participate and gave informed consent after being advised of their rights and risks of participation. Forty-four subjects (21 men, 23 women; age, 22.5 ± 2.0 years; height, 171.0 ± 9.0 cm; weight, 72.6 ± 12.8 kg) completed the study. We instructed subjects to continue their normal daily routine or exercise habits throughout the study. We excluded subjects if they were involved in any flexibility or strength training for the calf, had a recent ankle injury or history of ankle injury that would be adversely affected by static stretching, had metal plates or screws in the right leg, were pregnant, or had any allergies to cold. The university institutional review board reviewed and approved this study.
Procedures
Subjects were randomly assigned to 1 of 5 groups: control 1, control 2, stretching, heat and stretching, and heat, stretching, and ice. The control 2 group was not stretched and was measured twice: at the beginning and end of the study. Subjects in the control 1, stretching, heat and stretching, and heat, stretching, and ice groups were stretched 14 times in 3 weeks, once daily except for weekends. In these latter 4 groups, ROM was measured before and after each treatment and 6 days after the last treatment. Subjects reported at the same time every day for their treatments and measurements.
We measured ankle position on a treatment table set up with a weight-and-pulley system so that constant tension could repeatedly be applied to the triceps surae (Figure 1). To place each subject in a consistent position for each measurement, the subjects lay prone on the treatment table, with their feet hanging over the edge. We placed reference marks, used to take measurements, with a permanent ink pen. The first mark was placed on the lateral side of the calf 10 cm proximal from the middle of the lateral malleolus. The second mark was placed on the posterior side of the calf, forming a line that connected the first and second reference points and was perpendicular to the line connecting the lateral malleolus and the first reference mark. The third reference mark was placed on the flattest part of the plantar aspect of the heel of the subject's shoe. We secured the subject to the table with a strap to prevent sliding due to the pull of the weights. Next, we applied the stretching to the subject's foot using a rope and pulley with approximately one third of the body weight attached. We instructed the subject to relax while we lined up the digital inclinometer with the first mark and allowed it to stabilize. Then we zeroed the device and moved it to the second reference point on the heel of the subject and allowed it to stabilize before taking the reading (Figure 2A and B). The elapsed time from applying tension until the measurement was recorded was less than 30 seconds.
Figure 1.
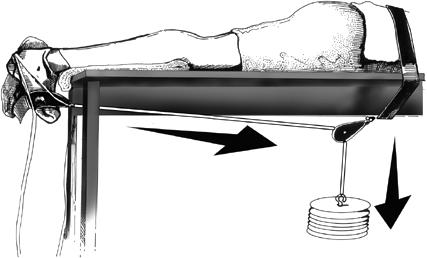
Bottom view of the weight and pulley used to apply a constant, low-load, prolonged stretch.
Figure 2.
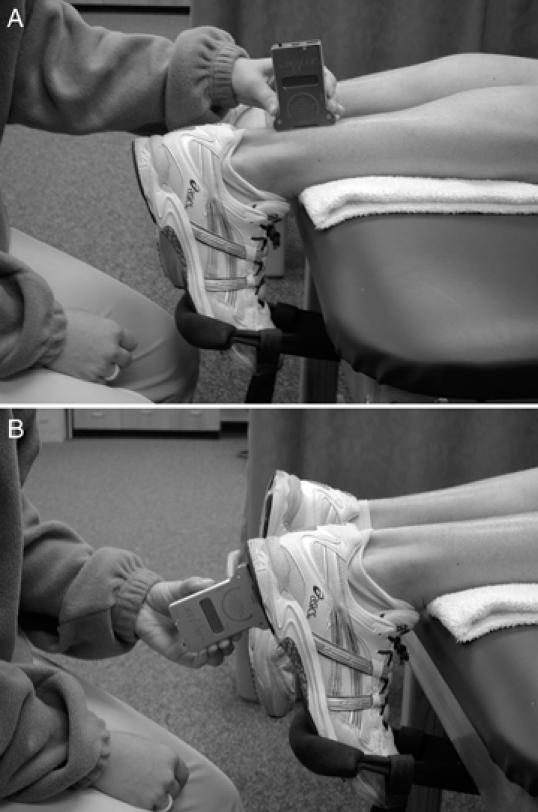
A, We placed the inclinometer on the posterior part of the calf using the 10-cm mark as a reference point and then zeroed the inclinometer after the reading had stabilized. B, Once the inclinometer had stabilized and been zeroed, it was then placed on the plantar surface of the shoe, where a reference mark had been placed to ensure consistent positioning.
The stretching group received a 10-minute static stretch on the table with the weight and pulley. We previously performed a pilot study to determine how much weight to apply. Our pilot study revealed that applying the same weight to subjects for 10 minutes was uncomfortable for some subjects and ineffective for larger subjects. Using our pilot study data, we chose to apply approximately one third of the subject's body weight to the calf. The only time we strayed from this formula was when this weight was too difficult for the subject. Our procedure was similar to that of Wessling et al,3 who applied a 23.1-kg load for 1 minute.
During treatment session 1 of the stretching, weight was adjusted in 5-lb (2.27-kg) increments until it was one third of the subject's body weight. If the subject could not tolerate this much weight, we decreased it until the subject could tolerate it while feeling a firm stretch of the triceps surae. By treatment 2, subjects were being stretched for 10 minutes total, with approximately one third of their body weight applied by the pulley apparatus. The heat and stretching group received a 20-minute diathermy treatment while lying on the table. With the skin dried to remove excess moisture, the diathermy drum was placed over the musculotendinous junction of the triceps surae (Figure 3). The pulsed shortwave diathermy output was set at 800 bursts per second, 400-microsecond burst duration, 800-microsecond interburst interval, with a peak root mean square amplitude of 150 W per burst and an average root mean square output of 48 W.12,13 At the 15-minute mark, we applied the stretching (one third of body weight) for 10 minutes. The heat, stretching, and ice treatment plan repeated the heat and stretching treatment plan except that at the end of 20 minutes of diathermy, a 1-kg ice bag was applied to the musculotendinous junction with an elastic wrap for 5 minutes.
Figure 3.

Pulsed shortwave diathermy setup. We centered the diathermy drum on the musculotendinous junction.
Instruments
We used 2 Megapulse (Accelerated Care Plus, Sparks, NV) shortwave diathermy machines operating at a frequency of 27.12 MHz. The units housed a 200-cm2 induction coil with an air space plate of 2 cm. The manufacturer calibrated both machines before we began our study.
We used a Dualer Electronic Inclinometer (Jtech Medical Industries, Heber City, UT) for all ankle measurements. The electronic inclinometer used eccentric encoding wheels that were accurate to ±1° and had a repeatability of ±1°. We followed the manufacturer's instructions at all times to ensure accuracy. The measurement was reliable (r = 0.99; intraclass correlation coefficient [ICC] of the control pretreatment and posttreatment measurements).
The stretching equipment consisted of weights in 5- to 10-lb (2.27- to 4.54-kg) increments attached to 4 rope-and-pulley sets constructed by the researchers. All 4 sets applied equal tension on the subjects.
Statistical Analysis
We used the raw data in degrees to look at several differences. Pretreatment to posttreatment was the difference between the measurements taken before and after treatment each day. Days was the difference between the measurements taken before treatment each day. Group was the difference between the groups. We calculated the mean changes in ankle position from the 14 single-treatment sessions for the control 2, stretching, heat and stretching, and heat, stretching, and ice groups.
To test for main and interaction effects, we used a 2 × 5 × 15 analysis of variance (ANOVA) (pretreatment to posttreatment, days, groups) with raw scores (α P < .05). Because there were interactions in the overall ANOVA, we performed a series of simple main-effects tests. We performed a 2 × 2 ANOVA (control 1, control 2, first and last day) to see what effect taking measurements every day would have on ankle position. Because there was no difference, we eliminated control 2 from subsequent analysis. To measure the effect of our treatments, we performed a 4 × 15 ANOVA (groups, days) with pretreatment scores. To measure changes immediately after treatment, we performed a 4 × 14 ANOVA using the differences between the pretreatment and posttreatment measurements. We used a series of Scheffé post hoc tests to test for simple effects.
We performed further Scheffé post hoc testing to determine if individual comparisons were significant for the differences between groups and days using raw scores, change scores, and pretreatment to posttreatment scores. Using the same test, we compared the difference between pretreatment and posttreatment on each day for each group and the pretreatment to posttreatment means of all groups.
RESULTS
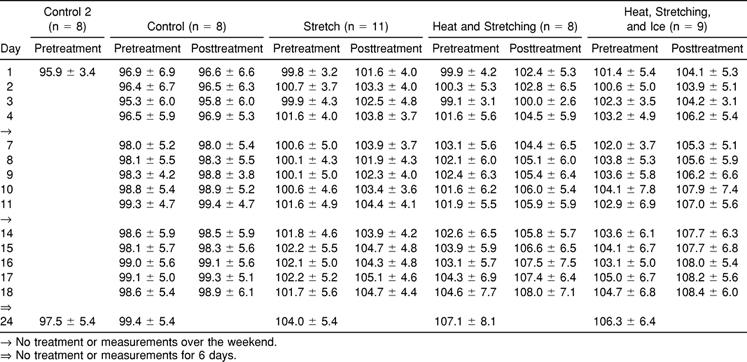
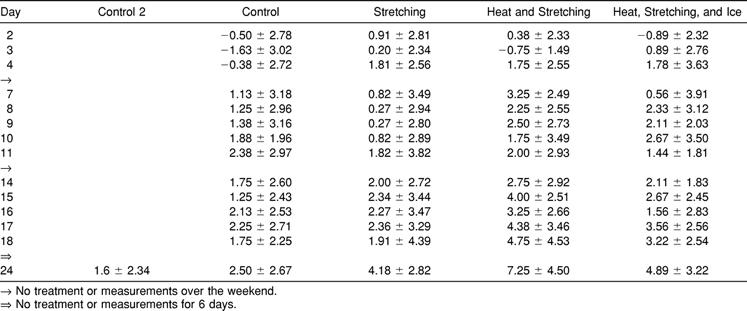
Results are displayed in Figure 4. Ankle position in the control 1 and treatment groups was approximately 96° to 101° (or 6° to 11° beyond neutral) at the beginning of the experiment and increased to 99° to 105° after the last treatment and 98° to 107° after a week of no treatment (Table 1). The ROM was not different between the 2 control groups (F1,31 = 0.13, P = .72, power = 0.06), indicating that daily measurements in the first control group did not induce changes. Therefore, the control 2 group was eliminated from further analysis.
Figure 4.
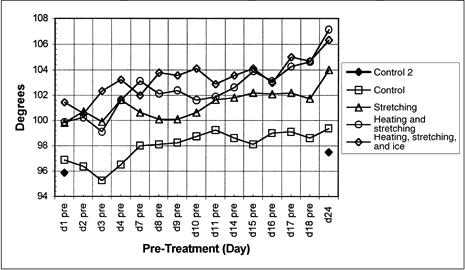
Pretreatment range-of-motion changes for all 5 groups on days 1 through 24.
Table 1. Ankle Position (Degrees; Mean ± SD)
Overall, ankle position differed among groups (F3,32 = 2.92, P = .049, power = 0.639, η2 = .215), days (F13,416 = 16.03, P =. 001, power = 1.00, η2 = .334), and pretreatment to posttreatment (F1,416 = 163.63, P = .001, power = 1.00, η2 = .836). Also, the interactions among groups and days (F39,416 = 1.48, P = .036, power = 0.994, η2 = .122), groups and pretreatment to posttreatment (F3,32 = 15.54, P = .001, power = 1.00, η2 = .593), and days and pretreatment to posttreatment (F13,416 = 2.22, P = .008, power = 0.962, η2 = .065) were significant.
The immediate effects of treatment (pretreatment to posttreatment or intrasession ankle-position changes) were different among groups (F3,32 = 15.54, P = .001, power = 1.00, η2 = .593) and days (F14,416 = 6.76, P = .008, power = 1.00, η2 = .334), but the interaction among groups and days was not significant. Daily changes in the control 1 group ranged from −0.25° to 0.30° per day, which was significantly less than those in the 3 treatment groups, which ranged from 1.25° to 4.38° per day (stretching-alone average, 2.47°/d; heat and stretching average, 2.94°/d; heat, stretching, and ice average, 3.30°/d) (F3,33 = 15.5, P = .001, power = 1.00, η2 = .593). There was no difference among the 3 treatment groups (Scheffé P > .05).
Net effects of treatment (cumulative, residual, or intersession ROM changes) were analyzed using pretreatment measurements. There was a day-by-group interaction (F42,448 = 1.43, P = .043, power = 0.995, η2 = .118), so further analysis involved simple main-effects testing. Net ROM did not change in either the control or stretch groups (Scheffé P < .05) but was significantly different in the heat and stretching group between days 1 and 18 and in both the heat and stretching and heat, stretching, and ice groups between days 1 and 25.
Analysis of differences in net ROM among groups was complicated by differences in initial ankle position. Net ankle position on the first day was less in the control 1 group (96.9° ± 6.9°) than in the 3 treatment groups (99.8° ± 3.2° to 101.4° ± 5.4°, Scheffé P < .05). Ideally, all groups would have the same ROM at the start. We computed change scores by subtracting day 1 pretreatment scores from each subsequent day pretreatment score (Table 2) and used these change scores for analysis. There were no differences among groups (change scores) on days 1 through 17 (Scheffé P > .05). On days 18 and 24, ROM changes were greater in the heat and stretching group (7.25° ± 4.5°) than in either the control 1 (2.5° ± 2.67°) or stretching (4.18° ± 2.82°; Scheffé P < .05) groups but not different than the heat, stretching, and ice group (4.89° ± 3.22°, Scheffé P > .05).
Table 2. Differences in Range of Motion From Day 1 (Degrees; Mean ± SD)
DISCUSSION
Prolonged Stretching Defined
The terms short-duration stretching,5 long-duration stretching,5,6,14 and prolonged stretching7 have been used in the research literature without specific definitions. We present the following definitions for our article and as a point of departure for discussion and debate concerning these terms.
Short-duration stretching: lasts less than 1 minute
Long-duration stretching: lasts longer than 1 minute
Prolonged stretching: extends throughout several days15
So the term prolonged stretching should be used only in combination with short or long duration, such as prolonged long-duration stretching.
We selected 1 minute as the demarcation between short duration and long duration because previous researchers have tested stretches with durations of 15 seconds,5 30 seconds,5 60 seconds,5,6 120 seconds,14 8 minutes,16 10 minutes,7 and 3 sets of 5 minutes.7 Readers should note that these are general descriptors, and individual treatments should include the duration (seconds, minutes) of the stretching and the number of sessions.
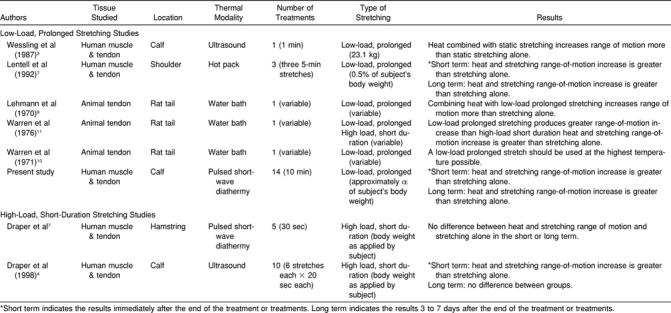
Using a heat-and-stretching regimen (with high-intensity, pulsed shortwave diathermy) for 3 weeks may result in greater changes in ROM than stretching alone. Our results concur with those of Lentell et al7 and Wessling et al3 while contradicting others14,17 (Table 3). Discrepancies among these studies may be the result of differences in any one or a combination of several variables: application of heat and the duration, intensity, and frequency of stretching.
Table 3. Research Comparing Stretching Alone with Heat and Stretching
Application of Heat
Our results and those from other studies suggest that vigorous deep heating combined with prolonged long-duration stretching is more effective than prolonged long-duration stretching alone in increasing flexibility throughout 3 weeks.18 Several areas of research on human and animal subjects form the nucleus of this idea. Static stretching is an effective method for increasing flexibility.8–10 Animal tendon properties change when put under a static stretch at temperatures greater than 37°C.10,11 This change in tendon properties allows for increased extensibility and plastic deformation of the stretched tissue.11,18–22 Wessling et al3 and Lentell et al7 reported that vigorous heating combined with static stretching was more effective than stretching alone in human subjects; however, they heated tendon only, whereas we heated a combination of tendon and muscle tissue. It is possible that the net ROM gains came primarily from the increased tendon flexibility that results from vigorous heating and stretching as shown with animal tendons.18–22
Despite evidence supporting the heat and stretching theory, research has not been conclusive. Draper et al17 reported no significant differences in immediate and net ROM between a heat and stretching group and a stretching-alone group. Draper et al4 reported that ROM was significantly greater in an ultrasound heat and stretching group than in a stretching group after 3 treatment sessions but not significantly different after 9 treatment sessions. It is possible that the type of heating modality used and other factors, such as the intensity, duration, and frequency of stretch, may be responsible for these apparent contradictions.
Pulsed shortwave diathermy appears to be a more appropriate modality than ultrasound for heating tissues before stretching.4 First, pulsed shortwave diathermy not only heats tissues to similar peak temperatures as ultrasound, but it heats a much larger area of tissue.13 The Megapulse used in our study offered a heating area of 200 cm2, whereas ultrasound heads are typically 3 to 10 cm2.13 Second, tissue heated with pulsed shortwave diathermy retains heat 3 times longer than that treated with ultrasound.12
Duration, Intensity, and Frequency of Stretching
We believe that a low-load, long-duration stretch in place of a high-load, brief stretch is required to take advantage of the responses of connective tissue under tensile deformation while being heated. Warren et al10 reported that the greatest residual increases in rat-tail tendon ROM occurred after a low-load, long-duration static stretch was applied while the tissue was vigorously heated. Previous studies by Draper et al4 (20-second static stretch), Wessling et al3 (1-minute static stretch), and Draper et al17 (30-second static stretch) did not use a low-load, long-duration static stretch. All 3 sets of investigators used a large-force, short-duration static stretch. However, Lentell et al,7 who used a low-load, long-duration stretch, reported that combining superficial heat and low-load, long-duration stretching resulted in significantly greater increases in ROM than low-load, long-duration stretching without preheating.
Little prior research has indicated how much weight to apply to the calf to create a low-load, long-duration stretch. Lentell et al7 applied 0.5% body weight to the subject's shoulder to increase external rotation ROM. Wessling et al3 applied a 23.1-kg load for 1 minute, using a method similar to ours. Our pilot study revealed that applying the same weight to subjects for 10 minutes was uncomfortable for some subjects and ineffective for larger subjects. Using our pilot study data, we combined the previous 2 studies' methods and chose to apply approximately one third of the subject's body weight to the calf. The only time we strayed from this formula was when this weight was too difficult for the subject.
The time required to cause tensile deformation of tissue varies according to the type and duration of the force applied.10,11 A low-force stretching method requires more time to produce the same amount of elongation as a higher-force method; however, the proportion of tissue lengthening that remains after tensile stress is removed is greater for the low-load, long-duration stretching method.11,17 Higher-force, short-duration stretching favors recoverable, elastic-tissue deformation, whereas low-load, long-duration stretching enhances permanent, plastic deformation.10,11 Sapega et al18 wrote that this principle does not necessarily rule out combining higher forces with a long duration of stretch, but in the clinical setting, high-force application has a greater risk of causing pain and possibly tissue rupture. In addition, laboratory studies10,11,29 indicated that when connective tissue structures are permanently elongated, some degree of mechanical weakening takes place, even though outright rupture does not occur. The amount of weakening depends on the manner and degree of tissue stretching. Of particular interest is that, for the same amount of tissue elongation, a high-force stretching method produces more structural weakening than a low-force, slower method. Apparently a low-load, long-duration static stretch is effective and safe.10,11,20
Researchers3,4 have reported that heat and stretching can cause significant ROM changes in human tissue after just one treatment. However, these studies involved high-load, short-duration stretching, and investigators did not record ROM after the last treatment and after a period of rest to measure net gains. Only Lentell et al7 showed significantly greater ROM after one treatment using heat and stretching than stretching alone in combination with a low-load, long-duration stretch. Animal tendon research9–11 with heat and low-load, long-duration stretching supports the findings by Lentell et al.7 Our study contradicts these findings: the heat and stretching group did not have significantly greater ROM than the stretching group until after treatment 13.
Questions
Based on previous research, we could not explain some of our results. First, why did the control 2 group increase in ROM? Although this was a cause for concern, the ROM increase was not statistically significant. Also, this small increase was possibly due to the increased activity of the students during the spring months when we conducted the study.
Second, why did ROM increase in each of the treatment groups during the 6 days of rest? We noticed this phenomenon in another one of our studies23 and can only speculate that the increased flexibility during the 6 days of rest might be due to reduction in muscle guarding. Even though our technique involved prolonged long-duration stretching, the force of one third of the body weight might have been more than subjects were accustomed to. The 6 days of rest was apparently enough time to wash out the effects of muscle guarding, leading to increased ROM.
Third, although the heat, stretching, and ice group produced the same ROM gains as the heat and stretching group after treatment, why were those gains not retained? Previous researchers have shown that cold application may benefit ROM in short-term treatment by reducing muscle spasm and painful inhibition.18,24 These effects, however, have not been found to last very long.25
Perhaps other questions can be answered by further research incorporating some of the following modifications:
A randomized block design would allow the different groups to start at approximately the same ROM.
To more precisely determine the net changes in ROM, future researchers should begin treatment on the second day (ie, only take a pretreatment measurement on the first day) and should have a posttreatment measurement 24 hours after the last day to determine the net effect of the last treatment.
Researchers could attempt to compare longer or shorter stretching times with a weight-and-pulley system as used in this study.
These methods could be applied to other parts of the body, such as the hamstrings, where a greater increase in ROM is possible.
Further research is needed to compare different lengths of diathermy treatments and numbers of treatments to find out which combination yields the greatest flexibility gains.
Further research is needed to address why the greatest ROM increases occurred 6 days after the last treatment. Investigators should look at various rest periods after training (stretching) and at various rest periods after standard training periods. One possibility is to train (stretch) different groups of subjects for 1 to 4 weeks and to test the effect of the different rest periods on net increases in ROM.
Finally, more research needs to be performed on the effect of prolonged long-duration stretching combined with thermal modalities on subjects who have connective tissue changes due to aging or pathologic conditions.
Limitations
When studying the effect of pulsed shortwave diathermy on prolonged long-duration stretch, it is important to be able to ensure even heating throughout all of the subjects. A limitation in this study is that we do not know how much temperature increase occurred inside the muscle because we did not measure intramuscular temperature. Our protocol was based on reports by Draper et al12 and Garrett et al,13 who produced temperatures of more than 40°C. Also, although shortwave diathermy with induction drum electrodes penetrates fat fairly well, varying thicknesses of the subcutaneous layer of fat around the calf of the individual subjects may have produced slightly higher muscle temperatures in lean individuals.12 A third limitation of this study is our inability to control the activity level of the subjects. Although we did not allow subjects who were regularly participating in a flexibility or strength training program involving the calf to join in our study, we were unable to control the daily activity level of those who participated. Increasing level of activity, beginning new activities, or varying the time of day of activity may have affected the temperature and stiffness of the subject's calf at the time of treatment.18 An additional limitation of this study is that prolonged long-duration stretching is most often used by clinicians with patients with ROM loss due to injury, surgery, or another pathologic condition. This study was performed on young, healthy college subjects; these results cannot be applied to older or injured subjects without further research. Finally, this stretching technique was performed with subjects non–weight bearing on the triceps surae, which is primarily involved in weight-bearing motor function. It is unclear how many of these flexibility gains would have been present if the subjects were tested in the weight-bearing position.
CONCLUSIONS
After 3 weeks of pulsed shortwave diathermy and prolonged long-duration stretching applied to the calf, ankle ROM increased more than with prolonged long-duration stretching alone. Pulsed shortwave diathermy before stretching is a safe and effective protocol for increasing tissue extensibility. However, a weight-and-pulley system may not be a practical way to stretch the triceps surae in the athletic training room setting. Ice has been shown to increase ROM by reducing pain and spasm in acute cases.18,24 Ice application after heat and stretching may not be of much benefit for increasing ROM due to chronic adhesions and muscle shortening.7,18,24
REFERENCES
- Medeiros J M, Smidt G L, Burmeister L F, Soderberg G L. The influence of isometric exercise and passive stretch on hip joint motion. Phys Ther. 1977;57:518–523. doi: 10.1093/ptj/57.5.518. [DOI] [PubMed] [Google Scholar]
- Beaulieu J E. Developing a stretching program. Physician Sportsmed. 1981;9(11):59–69. doi: 10.1080/00913847.1981.11711207. [DOI] [PubMed] [Google Scholar]
- Wessling K C, DeVane D A, Hylton C R. Effects of static stretch versus static stretch and ultrasound combined on triceps surae muscle extensibility in healthy women. Phys Ther. 1987;67:674–679. doi: 10.1093/ptj/67.5.674. [DOI] [PubMed] [Google Scholar]
- Draper D O, Anderson C, Schulthies S S, Ricard M D. Immediate and residual changes in dorsiflexion range of motion using an ultrasound heat and stretch routine. J Athl Train. 1998;33:141–144. [PMC free article] [PubMed] [Google Scholar]
- Bandy W D, Irion J M. The effect of time of static stretch on the flexibility of the hamstring muscles. Phys Ther. 1994;74:845–850. doi: 10.1093/ptj/74.9.845. [DOI] [PubMed] [Google Scholar]
- Bandy W D, Irion J M, Briggler M. The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther. 1997;77:1090–1096. doi: 10.1093/ptj/77.10.1090. [DOI] [PubMed] [Google Scholar]
- Lentell G, Heatherington T, Eagan L, Morgan M. The use of thermal agents to influence the effectiveness of a low-load prolonged stretch. J Orthop Sports Phys Ther. 1992;16:200–207. doi: 10.2519/jospt.1992.16.5.200. [DOI] [PubMed] [Google Scholar]
- Gertsen J W. Effect of ultrasound on tendon extensibility. Am J Phys Med. 1955;34:362–369. [PubMed] [Google Scholar]
- Lehmann J F, Masock A J, Warren C G, Koblanski J N. Effect of therapeutic temperatures on tendon extensibility. Arch Phys Med Rehabil. 1970;51:481–487. [PubMed] [Google Scholar]
- Warren C G, Lehmann J F, Koblanski J N. Elongation of rat tail tendon: effect of load and temperature. Arch Phys Med Rehabil. 1971;52:465–474. [PubMed] [Google Scholar]
- Warren C G, Lehmann J F, Koblanski J N. Heat and stretch procedures: an evaluation using rat tail tendon. Arch Phys Med Rehabil. 1976;75:122–126. [PubMed] [Google Scholar]
- Draper D O, Knight K, Fujiwara T, Castel J C. Temperature change in human muscle during and after pulsed shortwave diathermy. J Orthop Sports Phys Ther. 1999;24:13–22. doi: 10.2519/jospt.1999.29.1.13. [DOI] [PubMed] [Google Scholar]
- Garrett C L, Draper D O, Knight K, Durrant E. Heat distribution in the lower leg from pulsed short wave diathermy and ultrasound treatments. J Athl Train. 2000;35:50–55. [PMC free article] [PubMed] [Google Scholar]
- Madding S, Wong J, Hallum A, Medeiros J. Effect of duration of passive stretch on hip abduction range of motion. J Orthop Sports Phys Ther. 1987;8:409–416. doi: 10.2519/jospt.1987.8.8.409. [DOI] [PubMed] [Google Scholar]
- Landau S I, editor. Funk & Wagnalls Standard Desk Dictionary. Harper & Row; New York, NY: 1985. [Google Scholar]
- Bohannon R W. Effect of repeated eight-minute muscle loading on the angle of straight-leg raising. Phys Ther. 1984;64:491–497. doi: 10.1093/ptj/64.4.491. [DOI] [PubMed] [Google Scholar]
- Draper D O, Miner L, Knight K, Ricard M. The carry-over effects of diathermy and stretching in developing flexibility. Athl Train. 2002;37:37–42. [PMC free article] [PubMed] [Google Scholar]
- Sapega A A, Quedenfeld T C, Moyer R A, Butler R A. Biophysical factors in range-of-motion exercise. Physician Sportsmed. 1981;9(12):57–65. doi: 10.1080/00913847.1981.11711229. [DOI] [PubMed] [Google Scholar]
- Brown M, Vaker R D. Effect of pulsed shortwave diathermy on skeletal muscle injury in rabbits. Phys Ther. 1987;67:208–213. doi: 10.1093/ptj/67.2.208. [DOI] [PubMed] [Google Scholar]
- Moore M A, Hutton R S. Electromyographic investigation of muscle stretching techniques. Med Sci Sports Exerc. 1980;12:322–329. [PubMed] [Google Scholar]
- Rigby B J, Hirai N, Spikes J D, Eyring J. The mechanical properties of rat tail tendon. J Gen Phys. 1959;43:645–649. doi: 10.1085/jgp.43.2.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigby B. The effect of mechanical extension under thermal stability of collagen. Biochim Biophys Acta. 1964;79:634–636. doi: 10.1016/0926-6577(64)90234-7. [DOI] [PubMed] [Google Scholar]
- Rubley M D, Knight K L, Ricard M D, Draper D O, Brucker J B. Retention of flexibility 3 weeks after a one-week training regime. J Athl Train. 2001;32:S34. [Google Scholar]
- Kottke F J, Pauley D L, Ptak R A. The rationale for prolonged stretching for correction of shortening of connective tissue. Arch Phys Med Rehabil. 1966;47:345–352. [PubMed] [Google Scholar]
- Newton R A. Effects of vapocoolants on passive hip flexion in healthy subjects. Phys Ther. 1985;65:1034–1036. doi: 10.1093/ptj/65.7.1034. [DOI] [PubMed] [Google Scholar]


