Abstract
Objective: To identify differences in postural control among healthy individuals with different architectural foot types.
Design and Setting: We compared postural control during single-leg stance in healthy individuals with cavus, rectus, and planus foot types in our athletic training research laboratory.
Subjects: Thirty healthy, young adults (15 men, 15 women; age, 21.9 ± 2.0 years; mass, 71.6 ± 16.7 kg; height, 168.4 ± 13.6 cm) had their feet categorized based on rearfoot and forefoot alignment measures. The right and left feet of a subject could be classified into different categories, and each foot was treated as a subject. There were 19 cavus, 23 rectus, and 18 planus feet.
Measurements: Subjects performed three 10-second trials of single-leg stance on each leg with eyes open while standing on a force platform. Dependent measures were center-of-pressure (COP) excursion area and velocity.
Results: Subjects with cavus feet used significantly larger COP excursion areas than did subjects with rectus feet. However, COP excursion velocities were not significantly different among foot types.
Conclusions: Clinicians and researchers assessing postural control in single-leg stance with measures of COP excursion area must be cognizant of preexisting differences among foot types. If individuals' foot types are not taken into account, the results of clinical and research investigations assessing COP excursion area after injury may be confounded.
Keywords: stabilometry, postural sway, pes cavus, pes planus, pes rectus, foot classification
Instrumented assessment of postural control has been used to quantify functional impairment in patients with various orthopaedic injuries, such as lateral ankle sprains,1–6 anterior cruciate ligament injuries,7–9 and lumbosacral pain.10–13 In the past decade, the use of balance tasks to assess and rehabilitate postural control in injured athletes has become more commonplace. Despite this increased interest in the assessment of postural control in the sports medicine setting, very few studies have been performed to examine if common lower extremity malalignments, such as foot type, have a role in performance on instrumented postural control tests. Athletic trainers who use instrumented measures of postural control in clinical or research settings may benefit from a better understanding of the effects of common malalignments on such measures.
Postural control is often quantified by having a subject stand on a force platform as ground reaction forces and moments are measured. Center-of-pressure (COP) excursions are computed from the ground reaction forces. Moments and excursions in COP position provide an indication of postural control during quiet standing.14 An individual with a high magnitude or velocity of COP excursions is thought to have impaired postural control.14 During single-leg stance, control of upright posture is accomplished largely through corrective movements at the ankle joint. Subjects use visual, vestibular, and somatosensory information to plan and execute motor commands to maintain balance. Because muscles that act on the ankle complex contract in an effort to control a stable upright posture, changes in ground reaction forces lead to COP migrations within the base of support.
Despite the fact that much assessment of postural control in the sports medicine setting occurs in the barefoot condition,1–6 no published research reports have addressed the effect of different architectural foot types on postural control measures. Root et al15 described 3 common types of foot postures: cavus feet are high arched and associated with excessive rearfoot varus, planus feet are flat arched and associated with rearfoot valgus and excessive forefoot varus, and rectus feet are “normal” and not associated with excessive forefoot or rearfoot malalignment. It is feasible that the interface between differently shaped feet and a forceplate could influence ground reaction forces and, thus, postural control measures during objective assessment of postural stability during single-leg stance. If such differences do exist, they may influence the way measures of postural control in single-leg stance are interpreted in clinical and research settings. Therefore, the purpose of our study was to determine if differences exist in postural sway area and velocity among individuals with different architectural foot types.
METHODS
Subjects
Thirty healthy, young adults (15 men, 15 women; age, 21.9 ± 2.0 years; mass, 71.6 ± 16.7 kg; height, 168.4 ± 13.6 cm) volunteered as subjects. Subjects were reported to be free of cerebral concussions, vestibular disorders, and lower extremity orthopaedic injuries in the 6 months before testing. All subjects read and signed an informed consent form approved by the institutional review board (which also approved the study) before participating.
Assessment of Foot Type
Foot type was determined through an open kinetic chain assessment using the methods described by Root et al.15 Goniometric measurements of rearfoot and forefoot alignment in subtalar neutral positions were taken with subjects lying prone. The leg to be measured was extended over the end of the plinth. The contralateral limb was passively placed in a position of hip abduction and external rotation with knee flexion so that the contralateral ankle lay across the posterior thigh of the limb being measured. Subjects were manually placed in subtalar neutral positions for both measurements.
Rearfoot alignment was assessed by drawing a line that represented the proximal axis, which bisected the posterior aspect of the lower leg from the level of the musculotendinous junction of the triceps surae to approximately 10 cm proximal to the insertion of the Achilles tendon. The distal axis was drawn by longitudinally bisecting the calcaneal tuberosity. The center of the goniometer was placed at a point that bisected the posterior aspect of the ankle and equal in level with the distal tip of the lateral malleolus. The rearfoot angle was measured with the arms of the goniometer aligned with the line that bisected the lower leg and the line that bisected the calcaneus. Forefoot alignment was assessed by measuring the angle between a line parallel to the end of the plinth and a line parallel with the metatarsal heads.
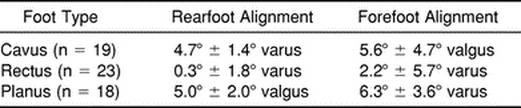
Subjects' feet were assigned to the cavus, rectus, or planus group based on the foot type classifications originally described by Root et al.15 Each foot was analyzed individually, and the right and left feet of the same subject could be classified into 2 different categories. There were 19 cavus feet, 23 rectus feet, and 18 planus feet (Table 1).
Table 1. Rearfoot and Forefoot Alignment Measures
Instrumentation
Postural control was assessed using an AMTI Accusway force platform (AMTI Corp, Watertown, MA) interfaced with a laptop computer using Swaywin software (AMTI). Three-dimensional ground reaction forces were recorded at 50 Hz, and COP excursions were calculated by the software program. The origin of the COP path was the initial point of COP during each trial. Dependent measures of postural control included COP excursion sway area and velocity. Area represented the magnitude of distribution of COP excursions during a trial, whereas velocity represented the average speed of COP movement during a trial.
Postural Control Task
Subjects performed 3 trials of quiet standing in single-leg stance on both the right and left limbs. Subjects stood with arms folded across their chest and eyes open while focusing on a stationary visual target located on a wall 1 m from the force platform. We instructed subjects to stand as motionless as possible. Each trial lasted 10 seconds. The initial stance leg was determined using a counterbalancing schedule. Trials were discarded and repeated if a touchdown (the nonstance leg touching the ground) occurred during the trial.
Statistical Analysis
The mean of the 3 trials for each dependent variable was calculated for each condition. Two separate analyses of variance were conducted, with foot type serving as the independent variable and mean COP excursion area and mean COP excursion velocity serving as the dependent variables. Post hoc analyses were performed using the Tukey test. The level of significance was preset at P ≪ .05.
RESULTS
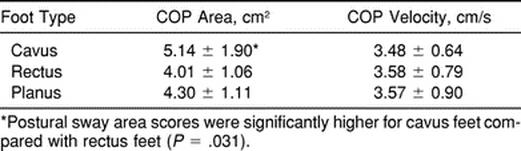
Means and SDs for COP excursion area and velocity are shown in Table 2. A significant main effect for foot type was found in measures of COP excursion area (F2,57 = 3.55, P = .035). Post hoc analysis revealed that cavus feet were associated with significantly larger COP excursion area measures than rectus feet (P = .031). No significant differences were found in COP excursion velocity measures among foot types (F2,57 = 0.10, P = .91, 1 − β = .06).
Table 2. Center-of-Pressure (COP) Excursion Area and Velocity
DISCUSSION
Differences in postural control during single-leg stance are typically examined either with side-to-side comparisons of unilaterally injured subjects4,6 or between healthy and injured subjects.1–3,5 Several studies have demonstrated no significant differences in postural control measures between the right and left limbs16–18 or dominant and nondominant limbs19 of healthy subjects standing in single-leg stance. Very few researchers have examined the role of lower extremity malalignments on postural control. Potter et al20 demonstrated that individuals with simulated knee-flexion contractures had impaired postural control in bipedal stance, whereas Mahar et al21 reported that subjects with simulated leg-length discrepancies had impaired postural control. Conversely, Murrell et al22 demonstrated that individuals with leg-length discrepancies did not exhibit postural control impairments when compared with those without discrepancies. Previous investigators23,24 have demonstrated that biomechanical measures, such as peak plantar pressure and malleolar valgus index, vary among different foot types during gait. To our knowledge, our study is the first to examine the effects of foot type on postural control in single-leg stance.
Our finding of greater COP excursion area scores among cavus feet is not easily explained. It may be that an individual with a cavus foot has less contact area between the plantar surface of the foot and the forceplate than an individual with a rectus or planus foot. Having less plantar contact area may inhibit postural control in 1 of 2 ways. First, as the cavus foot shifts the COP medially during pronation, there is no anatomic block between the medial aspect of the foot and the forceplate, as there may be with a rectus or planus foot. Instead, pronation is limited in the cavus foot by the physiologic limits of the subtalar and midtarsal joint ranges of motion. The second possibility is that a cavus foot has less plantar cutaneous sensory information on which to rely than a rectus or planus foot, because less overall area of the plantar surface of the cavus foot is in contact with the forceplate. Plantar afferent activity has been previously demonstrated to be important in the regulation of postural control.25,26 If individuals with cavus feet receive less afferent input from the plantar cutaneous receptors, they may have less efficient mechanisms of control of their upright posture during single-leg stance. Further research is needed to validate this hypothesis.
There is no accepted “gold standard” measure of postural control in the sports medicine literature. We chose to measure COP velocity (directly proportional to length) and sway area because these are the most commonly reported measures of postural control. We used an overall measure of COP excursion length rather than separating medial-lateral and anterior-posterior excursions because we thought it provided a more robust indication of postural control.
The differences found between cavus and rectus feet with area scores but not velocity scores are interesting. Velocities of COP excursion scores are proportional to length of COP excursion scores because velocity is simply the sum of the length of all excursions divided by the time of each trial (in our study, all trials lasted 10 seconds). The lack of significant differences in velocity scores, and thus COP length scores, appears to indicate no difference in the magnitude of COP excursions in individuals with different architectural foot types. However, individuals with cavus feet in our study used a significantly larger area to make their COP excursions than did those with rectus feet. It should be noted that one large COP excursion can drastically affect the area score. Because of the smaller base of support with cavus feet, it is possible that these subjects are at risk of making larger COP excursions. Further research in this area is warranted.
A limitation of this study is our collection of only 10 seconds of COP excursion data at 50 Hz. This provided us with 500 data points for determination of COP excursion area and velocity. Because balancing in single-leg stance is a very dynamic task, collection of more COP excursion data points may provide a more robust analysis of postural control.
The methods we used to classify foot types have been previously reported to have good intratester reliability and to be valid in discriminating between foot types24,27–29; however, the ideal method to classify foot type is the subject of considerable debate.27,30–32 Our use of open kinetic chain measurements of rearfoot and forefoot alignment and subsequent assessment of postural control in the closed kinetic chain may be open to debate, since previous authors have criticized the relationship between static foot posture and the functional kinematics of the rearfoot during the stance phase of gait.33,34 Also, other investigators have documented high correlations between assessment of static open kinetic chain foot alignment and closed kinetic chain foot function during dynamic activities.29,35
In conclusion, our results indicate that healthy individuals with cavus feet use a significantly larger area for COP excursions during single-leg stance than do individuals with rectus feet. Therefore, athletic trainers who are assessing postural control with measures of sway area for clinical or research purposes must be cognizant of potential differences in healthy individuals with different foot types. In the clinical setting, practitioners must be cautious when comparing postural control measures of patients with left and right feet of different foot types. In the research setting, we recommend that when selecting matched control subjects for single-leg stance postural control studies comparing healthy and injured subjects, subjects be matched for foot type and other characteristics, such as age, sex, and activity level.
REFERENCES
- Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- Cornwall M W, Murrell P M. Postural sway following inversion sprain of the ankle. J Am Podiatr Med Assoc. 1991;81:243–247. doi: 10.7547/87507315-81-5-243. [DOI] [PubMed] [Google Scholar]
- Goldie P A, Evans O M, Bach T M. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75:969–975. [PubMed] [Google Scholar]
- Perrin P P, Bene M C, Perrin C A, Durupt D. Ankle trauma significantly impairs postural control: a study in basketball players and controls. Int J Sports Med. 1997;18:387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- Hertel J, Denegar C R, Buckley W E, Sharkey N A, Stokes W L. Effect of rearfoot orthotics on postural control after lateral ankle sprain. Arch Phys Med Rehabil. 2001;82:1000–1003. doi: 10.1053/apmr.2001.22349. [DOI] [PubMed] [Google Scholar]
- Harrison E L, Duenkel N, Dunlop R, Russell G. Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther. 1994;74:245–252. doi: 10.1093/ptj/74.3.245. [DOI] [PubMed] [Google Scholar]
- Shiraishi M, Mizuta H, Kubota K, Otsuka Y, Nagamoto N, Takagi K. Stabilometric assessment in the anterior cruciate ligament-reconstructed knee. Clin J Sport Med. 1996;6:32–39. doi: 10.1097/00042752-199601000-00008. [DOI] [PubMed] [Google Scholar]
- Lysholm M, Ledin T, Odkvist L M, Good L. Postural control: a comparison between patients with chronic anterior cruciate ligament insufficiency and healthy individuals. Scand J Med Sci Sports. 1998;8:432–438. doi: 10.1111/j.1600-0838.1998.tb00464.x. [DOI] [PubMed] [Google Scholar]
- Luoto S, Taimela S, Hurri H, Aalto H, Pyykko I, Alaranta H. Psychomotor speed and postural control in chronic low back pain patients: a controlled follow-up study. Spine. 1996;21:2621–2627. doi: 10.1097/00007632-199611150-00012. [DOI] [PubMed] [Google Scholar]
- Luoto S, Aalto H, Taimela S, Hurri H, Pyykko I, Alaranta H. One-footed and externally disturbed two-footed postural control in patients with chronic low-back pain and healthy control subjects: a controlled study with follow-up. Spine. 1998;23:2081–2090. doi: 10.1097/00007632-199810010-00008. [DOI] [PubMed] [Google Scholar]
- Alexander K M, LaPier T L. Differences in static balance and weight distribution between normal subjects and subjects with chronic unilateral low back pain. J Orthop Sports Phys Ther. 1998;28:378–383. doi: 10.2519/jospt.1998.28.6.378. [DOI] [PubMed] [Google Scholar]
- Mientjes M I, Frank J S. Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clin Biomech. 1999;14:710–716. doi: 10.1016/s0268-0033(99)00025-x. [DOI] [PubMed] [Google Scholar]
- Guskiewicz K M, Perrin D H. Research and clinical applications of assessing balance. J Sport Rehabil. 1996;5:45–63. [Google Scholar]
- Root M L, Orien W P, Weed H J. Clinical Biomechanics: Normal and Abnormal Function of the Foot. VOL Clinical Biomechanics Corp; Los Angeles, CA: 1977. [Google Scholar]
- Dietz V, Horstmann G A, Berger W. Significance of proprioceptive mechanisms in the regulation of stance. Prog Brain Res. 1989;80:419–423. doi: 10.1016/s0079-6123(08)62238-4. [DOI] [PubMed] [Google Scholar]
- Goldie P, Back T M, Evans O M. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510–517. [PubMed] [Google Scholar]
- Geurts A C, Nienhuis B, Mulder T W. Intrasubject variability of selected force-platform parameters in the quantification of postural control. Arch Phys Med Rehabil. 1993;74:1144–1150. [PubMed] [Google Scholar]
- Hoffman M, Schrader J, Applegate T, Koceja D. Unilateral postural control of the functionally dominant and nondominant extremities of healthy subjects. J Athl Train. 1998;33:319–322. [PMC free article] [PubMed] [Google Scholar]
- Potter P J, Kirby R L, MacLeod D A. The effects of simulated knee-flexion contractures on standing balance. Am J Phys Med Rehabil. 1990;69:144–147. doi: 10.1097/00002060-199006000-00009. [DOI] [PubMed] [Google Scholar]
- Mahar R K, Kirby R L, MacLeod D A. Simulated leg-length discrepancy: its effect of mean center-of-pressure position and postural sway. Arch Phys Med Rehabil. 1985;66:822–824. [PubMed] [Google Scholar]
- Murrell P, Cornwall M W, Doucet S K. Leg-length discrepancy: effect on the amplitude of postural sway. Arch Phys Med Rehabil. 1991;72:646–648. [PubMed] [Google Scholar]
- Sneyers C J, Lysens R, Feys H, Andries R. Influence of malalignment of feet on the plantar pressure pattern in running. Foot Ankle Int. 1995;16:624–632. doi: 10.1177/107110079501601008. [DOI] [PubMed] [Google Scholar]
- Song J, Hillstrom H J, Secord D, Levitt J. Foot type biomechanics: comparison of planus and rectus foot types. J Am Podiatr Med Assoc. 1996;86:16–23. doi: 10.7547/87507315-86-1-16. [DOI] [PubMed] [Google Scholar]
- Watanabe I, Okubo J. The role of the plantar mechanoreceptor in equilibrium control. Ann N Y Acad Sci. 1981;374:855–864. doi: 10.1111/j.1749-6632.1981.tb30926.x. [DOI] [PubMed] [Google Scholar]
- Maki B E, Perry S D, Norrie R G, McIlroy W E. Effect of facilitation of sensation from plantar foot-surface boundaries on postural stabilization in young and older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M281–M287. doi: 10.1093/gerona/54.6.m281. [DOI] [PubMed] [Google Scholar]
- Dahle L K, Mueller M, Delitto A, Diamond J E. Visual assessment of foot type and relationship of foot type to lower extremity injury. J Orthop Sports Phys Ther. 1991;14:70–74. doi: 10.2519/jospt.1991.14.2.70. [DOI] [PubMed] [Google Scholar]
- Jonson S R, Gross M T. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sports Phys Ther. 1997;25:253–263. doi: 10.2519/jospt.1997.25.4.253. [DOI] [PubMed] [Google Scholar]
- Donatelli R, Wooden M, Ekedahl S R, Wilkes J S, Cooper J, Bush A J. Relationship between static and dynamic foot postures in professional baseball players. J Orthop Sports Phys Ther. 1999;29:316–325. doi: 10.2519/jospt.1999.29.6.316. [DOI] [PubMed] [Google Scholar]
- Cavanagh P R, Rodgers M M. The arch index: a useful measure from footprints. J Biomech. 1987;20:547–551. doi: 10.1016/0021-9290(87)90255-7. [DOI] [PubMed] [Google Scholar]
- Menz H B. Alternative techniques for the clinical assessment of foot pronation. J Am Podiatr Med Assoc. 1998;88:119–129. doi: 10.7547/87507315-88-3-119. [DOI] [PubMed] [Google Scholar]
- Demp P H. Geometric models that classify structural variations of the foot. J Am Podiatr Med Assoc. 1998;88:437–441. doi: 10.7547/87507315-88-9-437. [DOI] [PubMed] [Google Scholar]
- Hamill J, Bates B T, Knutzen K M, Kirkpatrick G M. Relationship between selected static and dynamic lower extremity measures. Clin Biomech. 1989;4:217–225. [Google Scholar]
- McPoil T, Cornwall M W. Relationship between neutral subtalar joint position and pattern of rearfoot motion during walking. Foot Ankle Int. 1994;15:141–145. doi: 10.1177/107110079401500309. [DOI] [PubMed] [Google Scholar]
- Elveru R A, Rothstein J M, Lamb R L, Riddle D L. Methods for taking subtalar joint measurements: a clinical report. Phys Ther. 1998;68:678–682. doi: 10.1093/ptj/68.5.678. [DOI] [PubMed] [Google Scholar]


