Abstract
Objective: To compare the effects of shoulder bracing on active joint-reposition sense in subjects with stable and unstable shoulders.
Design and Setting: Two subject groups, with stable and unstable shoulders, participated in an active joint-reposition test of the shoulder under braced and unbraced conditions.
Subjects: Forty subjects (22 men, 18 women; age = 21.85 ± 3.12 years; height = 173.97 ± 10.08 cm; weight = 71.27 ± 11.68 kg) were recruited to participate in this study. Twenty Division I athletes were referred to us for shoulder instability, which was subsequently confirmed with clinical assessment. The remaining 20 subjects were recruited from a similar student population and assessed as having stable shoulders.
Measurements: Each subject's ability to perceive joint position sense in space was tested by actively reproducing 3 preset angles (10° from full external rotation, 30° of external rotation, and 30° of internal rotation) with and without a shoulder brace. Full, active external-rotation range of motion was assessed before active joint-reposition sense testing.
Results: While wearing the shoulder brace, the group with unstable shoulders demonstrated significant improvement in the accuracy of active joint repositioning at 10° from full external rotation in comparison with the stable group. Furthermore, those with unstable shoulders demonstrated significantly less full external rotation than did those with stable shoulders, and the brace reduced full external rotation only for those with stable shoulders.
Conclusions: Our findings suggest that shoulder active joint-reposition sense in subjects with unstable shoulders can be improved at close to maximal external rotation by wearing a shoulder brace. This effect does not appear to be related to restriction of shoulder external rotation.
Keywords: proprioception, glenohumeral joint, bracing
The shoulder joint sacrifices stability for mobility and, therefore, coordinated dynamic control of the muscles about the joint is necessary for stability during arm motion.1 Shoulder instability is a clinical condition in which the patient is unable to control the translation of the humeral head during dynamic functional activities, thus compromising the comfort and function of the shoulder.2 Many patients who suffer initial dislocations continue to complain of symptomatic instability without actual redislocation. Patients may complain of not “trusting the shoulder” or a feeling of it “slipping in and out.”3 The lack of dynamic muscular control may be due to deficits in proprioception, which may occur as the glenohumeral joint's mechanism of providing feedback for reflexive muscular contraction is interrupted.1,4–6
Several authors have studied the effect of shoulder instability on proprioception and found that passive joint-reposition sense is negatively affected by injury.1,4,7 Subjects who have chronic, traumatic anterior shoulder instability demonstrate deficits in passive reproduction of passive positioning when compared with the contralateral normal shoulder and when compared with healthy individuals.1,7 As a result of stress and injury to the support structures of the glenohumeral joint, deficits in joint and muscle receptor input compromise the individual's ability to process proprioceptive information.1,4,7
Various bracing devices and taping techniques are used by athletic trainers prophylactically or when returning an athlete to play after injury. These methods provide stability8,9 and aid in decreasing proprioceptive deficits that result from injury.10–12 Extensive literature exists on bracing of the ankle and knee in the lower extremity,10,11,13–20,21 and elastic knee bandages have been shown to have positive effects on joint position sense.11,13,17,19,21 In both healthy and injured individuals, application of a knee bandage11,13,17,19,21 and taping or bracing of ankles16,20,22 improved joint position as measured through reproduction of a set joint angle.
No studies concerning the effect of shoulder bracing on joint position sense were found in our literature search for this paper. Based on findings from knee and ankle bracing studies, we hypothesized that a neoprene shoulder stabilizer for anterior glenohumeral instability would enhance joint position sense. Enhanced joint position sense may be a result of stimulation of cutaneous nerve receptors or mechanoreceptors in the muscles, ligaments, and joint capsule, or both.11,16 It is speculated that enhanced neuromuscular feedback as a result of bracing and taping may possibly help decrease future incidences of injury.11,16 If the use of a shoulder brace helps to increase active joint-position sense, the improved proprioceptive mechanisms may help prevent recurring dislocations, subluxations, or feelings of instability. Therefore, the purpose of our study was to examine the effect of a neoprene shoulder stabilizer on active joint-reposition sense in subjects with stable and unstable shoulders.
METHODS
Subjects
Forty subjects volunteered to participate in this study and completed an informed consent form approved by the institutional review board, which approved the study. All subjects were asked to complete a subject information questionnaire that included information such as height, weight, shoulder dominance, and any history of shoulder problems. The composition of each group was based on whether a previous dislocation was experienced. Group 1 subjects (stable group) (n = 20: 10 men, 10 women, age = 21.9 ± 2.5 years; height = 172.4 ± 12.3 cm; weight = 68.6 ± 10.5 kg), were recruited from the University population and had no self-reported history of a prior shoulder dislocation and no history of existing shoulder problems. Group 2 subjects (unstable group) (n = 20: 12 men, 8 women, age = 21.8 ± 3.7 years; height = 175.6 ± 7.2 cm; weight = 73.9 ± 12.5 kg) consisted of Division I athletes who had a self-reported history of one or more anterior glenohumeral dislocations and had not had surgery to correct the instability. These subjects were referred to us by individuals familiar with the subject's injury history. The unstable group provided additional information on the questionnaire by elaborating on their complaints of instability such as feelings of not trusting the shoulder or of it “giving out.” Clinical tests (apprehension test and anterior-posterior translation test) were performed only on the unstable group by the same certified athletic trainer (J.C.C.) to assess each subject's instability. These tests were performed in order to assess instability clinically, and the data gathered were considered along with the subjective complaints of each subject. Clinical tests were not performed on the stable group because we were not testing for shoulder laxity or congenital instability. Although the degrees of instability differed among subjects, all subjects in our unstable group met our criteria of having experienced a prior dislocation and demonstrating positive results on the clinical tests.
Bracing
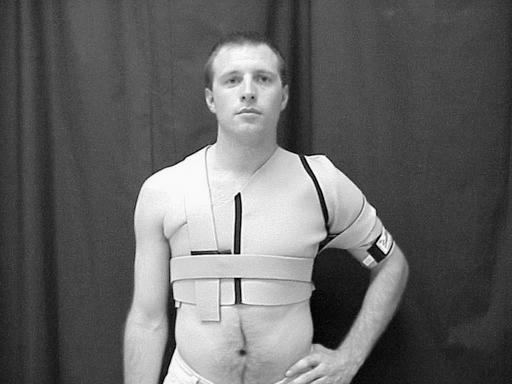
The Sully Shoulder Stabilizer (The Saunders Group Inc, Chaska, MN) was used in this study (Figure 1). The brace is made of perforated, breathable neoprene, which grips the skin. Elastic straps attached with hook-and-loop tape serve to functionally stabilize, assist, or restrict movement according to the specific needs of the athlete.
Figure 1.
The Sully Shoulder Stabilizer.
Assessment of Active Joint-Reposition Sense
The Cybex II isokinetic dynamometer (Lumex, Ronkonkoma, NY) was used to test active joint-reposition sense (Figure 2). The dominant shoulder, defined as the subject's throwing arm, was tested in the stable group, and the affected shoulder was tested in the unstable group. Each subject was positioned supine on the Upper Body Exercise Table (UBXT) (Lumex, Ronkonkoma, NY), with the shoulder joint axis aligned with the axis of rotation of the Cybex. The subject's upper extremity was placed in 90° of elbow flexion, 90° of shoulder abduction, and forearm pronation. The testing arm was strapped into the Cybex II shoulder rotation device with an elastic wrap placed around the forearm and wrist to minimize cutaneous sensation. A blindfold and headphones playing white noise were placed on the subject to decrease visual and audio cues, respectively. The order of testing with the shoulder brace on or off and the order of the preset testing angles were counterbalanced (ie, alternated).
Figure 2.
Positioning for active joint-reposition sense testing.
Before initiating the testing procedure, full external rotation was measured by having the subject actively externally rotate the testing shoulder while supine on the UBXT. Ten degrees were subtracted from full external rotation, and this angle was designated as the preset angle, 10° degrees from full external rotation. This preset angle differed for the braced and unbraced conditions because full external rotation should have been limited by wearing the shoulder brace. The other 2 preset angles (30° of external rotation and 30° of internal rotation) remained unchanged for the 2 test conditions.
To test active joint-reposition sense, each subject was instructed to slowly move the shoulder from neutral rotation (90° of shoulder abduction and 0° of internal rotation/external rotation) to one of the 3 preset target angles: 10° from full external rotation, 30° of external rotation, and 30° of internal rotation. Once the target angle had been reached, the electric goniometer was turned off and the shoulder held in this position for 10 seconds while the subject concentrated on this target angle. The subject then actively returned the shoulder to the starting position by moving to a mechanical stop set at 0°. After a 5-second pause, the subject was asked to actively reposition the shoulder and to say “stop” when he or she felt the previous target angle had been reached. The angle at which the subject stopped was recorded and subtracted from the initial preset angle. This difference was termed the degree of error. The procedure was repeated 2 more times at the same angle for a total of 3 trials. An average of the absolute value of the 3 errors was used for statistical analysis. This procedure was repeated for the remaining target angles.
The above procedure was repeated for either the braced or unbraced condition (depending on what was tested first) immediately after testing under the first condition. To offset potential learning effects, the 2 testing conditions and the 3 test angles were counterbalanced.
Assessment of Range of Motion
To test the effects of the brace on joint range of motion, maximum external rotation of the braced and unbraced conditions was compared for the stable and unstable shoulder groups. All range-of-motion testing was done before joint reposition-sense testing.
Data Analysis
For joint reposition sense, the average error scores were analyzed using a mixed-design analysis of variance (ANOVA) with group (stable, unstable) as the between-subjects variable and test condition (braced, unbraced) and angle (10° from full external rotation, 30° of external rotation, and 30° of internal rotation) as the 2 within-subjects variables. For range of motion, a separate mixed-design ANOVA was completed with group and bracing as between and within factors, respectively. Tukey post hoc analyses were performed for significant effects. An alpha level of P < .05 was set for all statistical analyses.
RESULTS
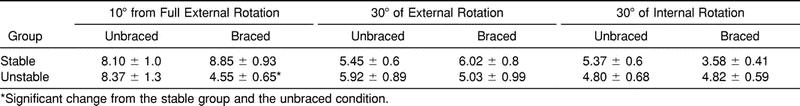
The ANOVA for joint reposition sense revealed a significant brace-by-angle-by-group interaction (F2,76 = 5.271, P < .05). Tukey post hoc analysis revealed that at 10° from full external rotation, the unstable group had significantly less mean error when tested under the braced condition in comparison with the unbraced condition (Table 1). At 10° from full external rotation, subjects had a significantly greater mean degree of error score (7.5° ± 0.562°) than at 30° of external rotation (5.6° ± 0.492°) and 30° of internal rotation (4.6° ± 0.314°). There was no significant difference in subjects' mean error between 30° of external rotation and 30° of internal rotation. A main effect for test angle was also found (F2,76 = 8.804, P < .001) but not considered important based on the presence of the interaction. We noted no main effect (F1,38 = 3.454, P = .071, observed power = .44) for braced versus unbraced test conditions and no difference (F1,38 = 1.674, P = .204, observed power = .243) between the stable and unstable groups.
Table 1. Joint-Reposition Sense Absolute Error Scores (Mean ± Standard Error) (°)
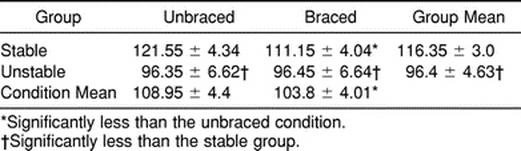
For external range of motion (Table 2), the ANOVA revealed a significant brace-by-group interaction (F1,38 = 8.466, P = .006). There was also a main effect for brace (F1,38 = 8.147, P = .007), with the braced group having less range of motion (unbraced = 109.0° ± 27.8°, braced = 103.8° ± 25.4°), and a main effect for group (F1,38 = 6.83, P = .013), with the stable group having more range of motion (stable = 116.4° ± 19.2°, unstable = 96.4° ± 29.3°). Post hoc analysis revealed that the brace reduced external rotation for the stable group but had no effect on the unstable group.
Table 2. External Rotation Range of Motion (Mean ± Standard Error) (°)
DISCUSSION
The major finding of our study was that the braced condition significantly improved active joint-reposition sense at 10° from full external rotation in the unstable group. While wearing the brace, subjects with unstable shoulders were better able to perceive glenohumeral joint position near maximal external rotation compared with not wearing a brace. This effect was seen despite the brace's having no effect in reducing shoulder external rotation in the unstable group. Conversely, for the stable group, the brace did limit external rotation with no effect on reposition sense.
The improvement in active joint-reposition sense might be attributed to the increased cutaneous input received at the shoulder joint. A recent study of the healthy elbow joint revealed significant improvement in joint position sense with the application of an elastic bandage.23 Several authors have also found similar results at other joints of both healthy and injured subjects. For example, significant improvements in knee joint proprioception have been noted with the application of a knee bandage or brace.10,11,13,17,19,21 Perlau et al11 suggested that the movement of an elastic bandage on skin stimulates rapidly adapting superficial receptors in the skin and layers beneath muscle such as free nerve endings, hair end organs, and Merkel discs. These receptors react strongly to new stimuli, such as increased pressure of the bandage on underlying musculature and joint capsule. Elastic bandages and braces appear to provide cutaneous stimulation, which may enhance afferent input from proprioceptive mediators such as articular, muscular, and cutaneous structures.19,23
Subjects in our unstable group described feelings of the shoulder “giving out” and “not trusting it” during daily activities. Apprehension resulting from instability may explain why external rotation was significantly limited in the unstable group in the unbraced condition. By encompassing the entire glenohumeral joint, the brace may have increased the sense of stability for the subjects with unstable shoulders and possibly enhanced joint position sense. Furthermore, since the brace clearly did not limit maximal external rotation in the unstable group, mechanical restriction of external rotation does not explain our findings. Our supposition is supported by the findings of previous research on knee support devices. Elastic knee bandages, although offering little or no mechanical support, appear to provide injured subjects with the feeling of improved stability.13,21 Birmingham et al21 speculated that wearing a knee sleeve may affect subjects' cognitive interpretation of joint position in some way, thereby improving test performance. Based on previous studies, it appears that the feeling achieved while wearing a knee bandage or sleeve may help to improve the performance of patients with poor joint-position sense.13,21
Subjects in the stable group of our study showed no significant changes in active joint-reposition sense while wearing the shoulder brace despite a significant decrease in external rotation. Our finding contradicts those of previous studies,10,11 which found that bandaging or bracing improved proprioception in healthy knees. Differences between the shoulder and knee joints and in measuring active versus passive joint-reposition sense may have contributed to our findings.
We also found a main effect for angle at 10° from full external rotation. Both the stable and unstable groups showed a greater mean degree of error at this angle as compared with 30° of external rotation and 30° of internal rotation. Our findings concur with those of Zuckerman et al,24 who found that position sense was less accurate in the maximum ranges of flexion, abduction, and external rotation. In accordance with Smith and Brunolli,4 we hypothesize that, as the shoulder joint approaches extreme angles, more proprioceptive recruitment may be necessary to detect the sensation of joint position in space.
In the unbraced condition, the 2 groups were not different from each other in mean degree of error at any of the 3 preset angles. This finding differed from previous studies in which subjects with injured shoulders demonstrated decreased proprioception when compared with the contralateral uninvolved side of healthy subjects.1,4,7 Lephart et al7 tested subjects with histories of chronic, recurrent, traumatic anterior shoulder dislocation or subluxation and found significant differences between the unstable and uninvolved shoulders for both threshold to detection of motion and passive joint-reposition sense. Smith and Brunolli4 studied shoulder proprioception by measuring what they called threshold to sensation of movement, angular reproduction, and end-range reproduction (passive joint-reposition sense). They found that shoulder proprioception was significantly deficient in subjects with a history of anterior glenohumeral joint dislocation.4 These authors theorized that subjects who have experienced a previous dislocation suffer from damaged stabilizers of the glenohumeral joint. The consequent impaired ability to detect joint position and movement are possibly due to the reduced number of receptors available for activation after injuries such as glenohumeral dislocations and ankle sprains.4,25 Increased joint laxity as a result of repetitive trauma or stretching of capsular and ligamentous structures may cause articular receptor damage and result in a distortion of proprioception.25 Individuals with previously dislocated shoulders may have insufficient signals and motor reflexes, be subject to excessive movement, and, thus, be predisposed to recurrent dislocation.4 Subjects with previous dislocations performed significantly worse in the unstable shoulder in comparison with the uninvolved shoulder, possibly due to these interrupted proprioceptive pathways.3,4,7
Our findings may not agree with previous research because of the broad inclusion criteria established for the unstable group. Subjects of varying shoulder instabilities were accepted and tested for this group. The possibility that the lack of kinesthetic differences in the unbraced condition was due to the broad inclusion criteria is supported by Glencross and Thornton,25 who hypothesized that degree of error depended on severity of injury. Their results showed that the group with the most severely injured ankle joints had the greatest error, and the mildly injured group had the least error.25 Although all subjects in our study met the criteria of a previous anterior glenohumeral dislocation and positive clinical test findings, their degree of function differed greatly. For example, 7 of the 20 unstable subjects were Division I athletes, most of whom competed their entire season without any problems.
A second possible reason why we did not find a significant difference in joint reposition sense between groups in the unbraced condition may be that we measured active joint-reposition sense as opposed to passive joint-reposition sense, which was measured in previous shoulder proprioception studies.3,4,7 Although lower absolute error scores for shoulder active (active reproduction of active positioning) versus passive (passive reproduction of passive positioning) testing have been reported,26 this pattern is not consistent for the lower extremity.15,18 For example, Gross15 found that in both subjects with healthy ankles and those with recurrent lateral sprains, passive joint-reposition sense is significantly better (less error) than active joint-reposition sense, and Kaminski and Perrin18 found similar results in the healthy knee. Thus, it is possible that errors associated with active joint positioning were too great to allow detection of significant differences.
The degree to which proprioceptive receptors in the skin, muscles, and joint capsule each contribute to joint position sense and detection of motion remains controversial.23 In recent studies, no difference in passive position sense was detected after lidocaine injection of the glenohumeral and elbow joints.23,24 Zuckerman et al24 suggested that, after lidocaine injection is performed, extracapsular receptors provide the necessary feedback to ensure intact proprioceptive abilities.24 However, in addition to intraarticular receptors, processing and interpretation of input from muscle afferent and efferent structures may result in increased error during active movements.15,18 These errors may have led to the greater mean error scores in the unbraced condition observed in our study compared with the one conducted by Lephart et al.7
We conclude from our study that the brace improved active joint-reposition sense at 10° from full external rotation for subjects with unstable shoulders. This particular shoulder brace may help to minimize shoulder instability by enhancing proprioception. The facilitation of deficient neuromuscular input at the extreme ranges of shoulder external rotation may help to prevent or decrease recurrent dislocations or subluxations. By providing an increased sense of security, subjects with unstable shoulders may feel more stable wearing the brace.
Further research should be conducted on the effect of shoulder bracing on kinesthesia, as measured by threshold to detection of passive motion. Other commercial shoulder braces should also be studied to determine whether the results of our study can be generalized to all shoulder braces.
Acknowledgments
ACKNOWLEDGMENTS
We thank The Saunders Group Inc for their donation of the Sully Shoulder Stabilizers. This study was completed as a part of a master's thesis at the University of Virginia.
REFERENCES
- Warner J J, Lephart S, Fu F H. Role of proprioception in pathoetiology of shoulder instability. Clin Orthop. 1996;330:35–29. doi: 10.1097/00003086-199609000-00005. [DOI] [PubMed] [Google Scholar]
- Wilk K E, Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993;18:365–378. doi: 10.2519/jospt.1993.18.1.365. [DOI] [PubMed] [Google Scholar]
- Warner J J, Micheli L J, Arslanian L E, Kennedy J, Kennedy R. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. 1990;18:366–375. doi: 10.1177/036354659001800406. [DOI] [PubMed] [Google Scholar]
- Smith R L, Brunolli J. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Phys Ther. 1989;69:106–112. doi: 10.1093/ptj/69.2.106. [DOI] [PubMed] [Google Scholar]
- Blasier R B, Carpenter J E, Huston L J. Shoulder proprioception: effect of joint laxity, joint position, and direction of motion. Orthop Review. 1994;23:45–50. [PubMed] [Google Scholar]
- Allegrucci M, Whitney S L, Lephart S M, Irrgang J J, Fu F H. Shoulder kinesthesia in healthy unilateral athletes participating in upper extremity sports. J Orthop Sports Phys Ther. 1995;21:220–226. doi: 10.2519/jospt.1995.21.4.220. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Warner J P, Borsa P A, Fu F H. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380. doi: 10.1016/S1058-2746(09)80022-0. [DOI] [PubMed] [Google Scholar]
- DeCarlo M, Malone K, Gerig B, Hunker M. Evaluation of shoulder instability braces. J Sport Rehabil. 1996;5:143–150. [Google Scholar]
- Gieck J. Shoulder strap to prevent anterior glenohumeral dislocations. Athl Train. 1976;11:18. [Google Scholar]
- McNair P J, Stanley S N, Strauss G R. Knee bracing: effects on proprioception. Arch Phys Med Rehabil. 1996;77:287–289. doi: 10.1016/s0003-9993(96)90114-8. [DOI] [PubMed] [Google Scholar]
- Perlau R, Frank C, Fick G. The effect of elastic bandages on human knee proprioception in the uninjured population. Am J Sports Med. 1995;23:251–255. doi: 10.1177/036354659502300221. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Pincivero D M, Giraldo J L, Fu F H. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- Barrett D S, Cobb A G, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73:53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Gross M T. Effects of recurrent lateral ankle sprains on active and passive judgements of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Heit E J, Lephart S M, Rozzi S L. The effect of ankle bracing and taping on joint position sense in the stable ankle. J Sport Rehabil. 1996;5:206–213. [Google Scholar]
- Jerosch J, Prymka M. Knee joint proprioception in normal volunteers and patients with ACL tears, taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg. 1996;115:162–166. doi: 10.1007/BF00434546. [DOI] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H. Effect of prophylactic knee bracing on balance and joint position sense. J Athl Train. 1996;31:131–136. [PMC free article] [PubMed] [Google Scholar]
- Lephart S M, Kocher M S, Fu F H, Borsa P A, Harner C D. Proprioception following anterior cruciate ligament reconstruction. J Sport Rehabil. 1992;1:188–196. [Google Scholar]
- Simoneau G G, Degner R M, Kramper C A, Kittleson K H. Changes in ankle joint proprioception resulting from strips of athletic tape applied over the skin. J Athl Train. 1997;32:141–147. [PMC free article] [PubMed] [Google Scholar]
- Birmingham T B, Kramer J F, Inglis J T, et al. Effect of a neoprene sleeve on knee joint position sense during sitting open kinetic chain and supine closed kinetic chain tests. Am J Sports Med. 1998;26:562–566. doi: 10.1177/03635465980260041601. [DOI] [PubMed] [Google Scholar]
- Jerosch J, Hoffstetter I, Bork H, Bischof M. The influence of orthoses on the proprioception of the ankle joint. Knee Surg Sports Traumatol Arthrosc. 1995;3:39–46. doi: 10.1007/BF01553524. [DOI] [PubMed] [Google Scholar]
- Khabie V, Schwartz M C, Rokito A S, Gallagher M A, Cuomo F, Zuckerman J D. The effect of intraarticular anesthesia and elastic bandaging on elbow proprioception. J Shoulder Elbow Surg. 1998;7:501–504. doi: 10.1016/s1058-2746(98)90202-6. [DOI] [PubMed] [Google Scholar]
- Zuckerman J D, Gallagher M A, Lehman C, Kraushaar B S, Choueka J. Normal shoulder proprioception and the effect of lidocaine injection. J Shoulder Elbow Surg. 1999;8:11–16. doi: 10.1016/s1058-2746(99)90047-2. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Lonn J, Crenshaw A G, Djupsjobacka M, Pederson J, Johansson H. Position sense testing: influence of starting position and type of displacement. Arch Phys Med Rehabil. 2000;81:592–597. doi: 10.1016/s0003-9993(00)90040-6. [DOI] [PubMed] [Google Scholar]