Abstract
Objective: Patellofemoral pain syndrome (PFPS) is a common clinical entity seen by the sports medicine specialist. The ultimate goal of rehabilitation is to return the patient to the highest functional level in the most efficient manner. Therefore, it is necessary to assess the progress of patients with PFPS using reliable functional performance tests. Our purpose was to evaluate the intrarater reliability of 5 functional performance tests in patients with PFPS.
Design and Setting: We used a test-retest reliability design in a clinic setting.
Subjects: Two groups of subjects were studied: those with PFPS (n = 29) and those with no known knee condition (n = 11). The PFPS group included 19 women and 10 men with a mean age of 27.6 ± 5.3 years, height of 169.80 ± 10.5 cm, and weight of 69.59 ± 15.8 kg. The normal group included 7 women and 4 men with a mean age of 30.3 ± 5.2 years, height of 169.55 ± 9.9 cm, and weight 69.42 ± 14.6 kg.
Measurements: The reliability of 5 functional performance tests (anteromedial lunge, step-down, single-leg press, bilateral squat, balance and reach) was assessed in 15 subjects with PFPS. Secondly, the relationship of the 5 functional tests to pain was assessed in 29 PFPS subjects using Pearson product moment correlations. The limb symmetry index (LSI) was calculated in the 29 PFPS subjects and compared with the group of 11 normal subjects.
Results: The 5 functional tests proved to have fair to high intrarater reliability. Intrarater reliability coefficients (ICC 3,1) ranged from .79 to .94. For the PFPS subjects, a statistical difference existed between limbs for the anteromedial lunge, step-down, single-leg press, and balance and reach. All functional tests correlated significantly with pain except for the bilateral squat; values ranged from .39 to .73. The average LSI for the PFPS group was 85%, while the average LSI for the normal subjects was 97%.
Conclusions: The 5 functional tests proved to have good intrarater reliability and were related to changes in pain. Future research is needed to examine interrater reliability, validity, and sensitivity of these clinical tests.
Keywords: step-down, squat, limb symmetry, knee
Patellofemoral pain syndrome (PFPS) is a common clinical entity used to describe a variety of pathologic conditions associated with the articulation between the undersurface of the patella and the femoral condyles. Patellofemoral pain syndrome can be caused by a variety of factors, including quadriceps weakness, increased Q angle, faulty lower extremity mechanics, overuse, and lateral retinaculum tightness.1,2 The major complaints of patients with PFPS are diffuse knee pain, patellar crepitus and locking, knee joint stiffness, and decreased activity levels.3–7 Onset of symptoms is usually insidious and may occur bilaterally. Activities such as prolonged sitting, stair descent, and squatting often exacerbate the pain.8
The ultimate goal of rehabilitation for patients with PFPS is return to the highest functional level in the most efficient manner.9 Accompanying this goal is the need for a testing method that is objective, reliable, and sensitive to the changing status of PFPS. Common objective measures of knee function include pain assessment, goniometry, girth measurement, manual muscle testing, and isokinetic evaluation. However, these tests have been shown to be poor predictors of function.6,10
Functional testing is an attempt to evaluate the knee joint under conditions that mimic realistic functional demands. Performance on functional tests depends on many variables, including pain, swelling, crepitus, neuromuscular coordination, muscular strength, and joint stability.11 The tests should be time efficient and simple to perform with minimal instruction; they should require minimal staff training and be conducted within a clinical setting. Several functional knee tests are described in the literature and include the shuttle run, stair-running test, vertical jump test, and hop tests.10–12 These tests are useful after ligamentous knee injuries or other sport-related injuries, such as muscle strains or meniscus injuries, and are not specific to the patellofemoral joint.
Functional performance tests that are specific for PFPS should be chosen based on clinical evidence and the ease of replication among clinics and facilities. Pain is a factor associated with PFPS and is commonly used as a measurement to determine functional improvement. Chesworth et al13 evaluated the visual analog scale (a measure of pain) in patients with PFPS, finding poor day-to-day reliability but good sensitivity to clinical changes. In addition to measuring pain directly, performance of a functional test may add information regarding muscle strength, endurance, proprioception, and balance.
Functional tests specific to PFPS should include weight-bearing stress with various knee-flexion angles because these are common aggravating positions and require dynamic muscular control. Post and Fulkerson8 found that 86% of patients with patellofemoral pain have pain during stair climbing and 85% have pain with squatting. The increase in pain with these activities is correlated with an increase in patellofemoral joint reaction force.3,4,8,14 At present, no functional tests specific to the patellofemoral joint have been reported in the literature.
We evaluated the following functional performance tests in this study: anteromedial lunge, step-down, single-leg press, bilateral squat, and balance and reach. The anteromedial lunge is a multiplanar movement designed to challenge the lateral patellofemoral articulation with the valgus stress placed on the knee during the maneuver.15 Theoretically, as an individual lunges and the center of gravity moves forward and across the body, the pull of the quadriceps muscle causes compressive loading of the lateral patellofemoral articulation, a common site of patellofemoral symptoms. The step-down mimics the function of stair descent, a common aggravating factor. The load of the patellofemoral joint with stair descent has been reported to be 3.5 times body weight.16 A single-leg press test was chosen to stress the patellofemoral joint in a partial weight-bearing mode. This test can be administered early in rehabilitation when a full squat may be too aggravating. To further challenge the patellofemoral joint, a second test is a full weight-bearing bilateral squat. The joint reaction force of a squat to 90° is approximately 7.5 times body weight.3 The balance-and-reach test, described by Gray,15 specifically challenges single-leg balance.
The primary purpose of our study was to determine the intrarater reliability of 5 functional performance tests on patients with PFPS. Secondary purposes were to determine limb symmetry index (LSI) differences for involved and uninvolved limbs and to assess the relationship between the 5 functional tests and pain ratings.
METHODS
Subjects
Two groups of subjects were included in this study, one group with PFPS (n = 29) and a second group with no known knee condition (n = 11). The PFPS group included 19 women and 10 men with a mean age of 27.6 ± 5.3 years, height of 169.80 ± 10.5 cm, and weight of 69.59 ± 15.8 kg. Data from 15 of these 29 subjects were used for the reliability testing. Inclusion criteria for the subjects in the PFPS group were 2 of the following on initial assessment: pain on direct compression of the patella against the femoral condyles with the knee in full extension, tenderness on palpation of the lateral surface of the patella, pain on resisted knee extension, or pain with isometric quadriceps contraction against suprapatellar resistance with the knee in slight flexion. These subjects' symptoms were consistent with the excessive lateral pressure syndrome as described by Wilk et al.17 Exclusion criteria for both groups included a history of patellar trauma; subluxation; dislocation; confirmed ligamentous, meniscal, or fat-pad damage; evidence of tendinitis, bursitis, or effusion; evidence of referred pain from the back or hip; osteochondral or chondral fractures; or upper or lower motor neuron lesion.18,19 The duration of patellofemoral pain averaged 5.2 months for the PFPS group. The normal group included 7 women and 4 men with a mean age of 30.3 ± 5.2 years, height of 169.55 ± 9.9 cm, and weight of 69.42 ± 14.6 kg. The normal subjects were used to compare the LSIs.
Experimental measurements
Anteromedial lunge, left and right For the anteromedial lunge, the subject is lined up behind a start line. The test is performed by having the subject lunge forward with the uninvolved limb so that the front leg is bent to 90° and crosses the midline. The subject must maintain good balance and an erect trunk posture. Distance is recorded from the start line to the heel of the lead limb during the lunge-out position. The maximal distance of 3 trials is recorded and marked. Eighty percent of the maximal distance is calculated and marked with a piece of tape as a target for the series of timed lunges. The subject is then asked to complete as many lunges as possible in 30 seconds; lunges less than the 80% mark are not recorded. If the subject deviates from the path of motion or takes an extra step, the lunge is not included in the count. The involved limb is then tested, using the 80% mark from the uninvolved limb (Figure 1).
Figure 1.
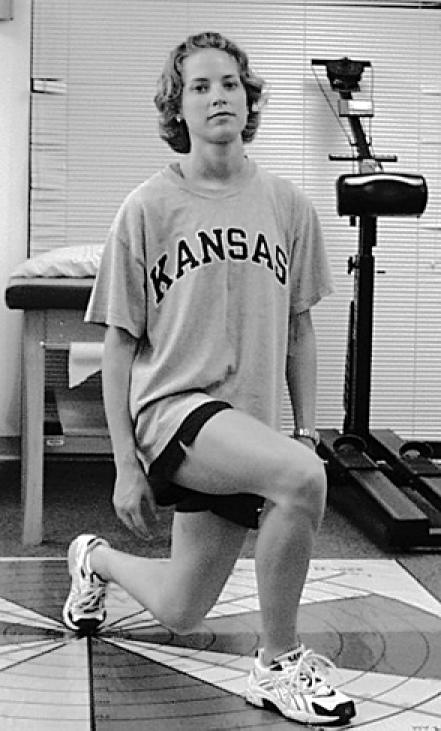
Anteromedial lunge test.
Step-down, left and right The step-down is a unilateral test performed from a platform 8 inches (20.32 cm) high. Subjects step forward and down toward the floor. The down limb only brushes the floor with the heel and then returns to full knee extension. This counts as one repetition. Each repetition must be completed such that the step limb is not used to accelerate back onto the step. The number of repetitions the subject performs in 30 seconds is recorded. Both limbs are tested (Figure 2).
Figure 2.

Step-down test.
Single-leg press Subjects are positioned on the Total Gym (Fitness Quest Inc, Canton, OH) at level 7, which is considered to be 50% of the subject's body weight. Subjects begin with the test knee in full extension. One repetition consists of a complete cycle of full knee extension to 90° of knee flexion and return to full knee extension. The number of unilateral squats completed in 30 seconds is recorded. Both limbs are tested (Figure 3).
Figure 3.

Single-leg press test.
Bilateral squat Subjects start this test standing with the knees in full extension, shoulder-width apart, and weight evenly distributed on both limbs. Subjects lower their bodies to a knee position of 90° and then return to full extension. One repetition consists of a complete cycle of straight standing to 90° of knee flexion and return to straight standing. The number of bilateral squats completed in 30 seconds is recorded.
Balance and reach The subject starts the test behind a start line. The subject reaches straight forward with one leg so that the heel touches the floor, with most of the body weight remaining on the back (test) leg. The uninvolved limb is tested first. Distance is recorded from the start line to the heel of the lead limb. The maximal distance of 3 trials is recorded and marked. Eighty percent of the maximal distance is calculated and marked with a piece of tape. During the 30-second test period, the subject performs as many balance-and-reach lunges as possible. Only lunges in which the subject's heel touches beyond the 80% mark are recorded. The involved limb is then tested using the 80% mark from the uninvolved limb (Figure 4).
Figure 4.

Balance-and-reach test.
Visual Analog Scale (VAS) A 10-cm horizontal line was used to assess patellofemoral knee pain over the 24 hours before the testing period. The far left is “pain free,” and the extreme right represents severe pain. The marked value was measured with a standard ruler and then converted to a pain score. The VAS has been previously validated in the literature20 and used in patients with PFPS.13
Procedure
The University of Kansas Medical Center's Internal Review Board approved the study. Before participating, subjects were screened with questions regarding previous lower extremity injuries. After being selected to participate, each subject completed an informed consent form followed by the VAS. After completing the VAS, the subject was instructed in the proper technique for each of the functional performance tests. The subject performed each of the functional tests in random order, and both lower extremities were tested. The beginning test leg was randomly assigned for the single-leg press and the step-down test. Each test was performed once, without the use of tape or a brace. Pain level during the test was monitored, and subjects were instructed that they could stop due to pain, but pain level was not a stopping criterion.
Each subject began the assessment session with a warm-up period that consisted of low-resistance, lower extremity cycling. The task-specific warm-up included practice for each functional performance test (3 to 5 repetitions with a 30-second rest before the actual testing). A written description of each test was read to the subject, followed by a demonstration of the test by the tester (Appendix). Participants received no verbal encouragement during actual testing. Subjects were allowed a 1-minute rest between functional performance tests.
Reliability For intrarater reliability, 15 subjects with PFPS were tested on 2 occasions, 48 to 72 hours apart. The random order of functional testing was matched between day 1 and day 2. Visual analog scale scores had to match within 0.5 from test day 1 to test day 2 (eg, a subject who scored 6.5 on day 1 had to score between 6.0 and 7.0 on day 2). Pain has motivational, affective, cognitive, behavioral, and sensory dimensions,21 and these factors can hinder a test-retest design. Therefore, for reliability testing, subjects had to score within 0.5 on the VAS from test day 1 to test day 2 to prevent confounding of the pain variable.
Correlation The scores on day 1 of the 15 reliability subjects were added to the scores of 14 other individuals with unilateral PFPS who had completed the VAS and 5 functional tests. This information was used to establish a relationship between the VAS and functional test scores. All subjects scored within this range except for 2. Both subjects were asked to return within 48 hours and repeat the VAS. Upon return, 1 of the 2 subjects scored within the acceptable VAS range; the other did not and was dropped from the study.
Limb Symmetry Index The PFPS limb scores were compared and an LSI was established.11 The group of 11 subjects with normal knees also performed the 5 functional tests to determine the LSI.
Data Analyses
We compiled descriptive characteristics for each subject and all performance scores in a Microsoft Excel (Microsoft Inc, version 2000, Redmond, WA) spreadsheet. Data from the VAS were recorded as a single score to one decimal place. Data from each of the functional performance tests were recorded as number of repetitions. We recorded repetitions for right and left anteromedial lunge, right and left step-down, right and left leg press, bilateral squat, and right and left balance and reach.
SPSS for Windows (version 10, SPSS Inc, Chicago, IL) statistical software was used to analyze the data. Statistical significance was set at P < .05. Subject characteristics (age, height, and weight) were compared between the groups using a 2-sample t test.
Reliability We used the intraclass correlation coefficient (ICC) to evaluate intrarater reliability (ICC 3,1). Standard error of the mean (SEM) was calculated to describe the precision of the measurement.
Correlation Correlation analyses between the VAS and functional tests were evaluated using the Pearson correlation coefficient.
Limb Symmetry Index Statistical difference between individual subjects' limbs for the unilateral functional tests was determined using a paired t test. Bonferroni correction was applied to these 4 tests, setting the alpha level to .05/4 = 0.013. The statistical difference between subjects with PFPS and normal subjects on functional test scores was determined with independent t tests. Bonferroni correction was applied to these 4 tests, setting the alpha level to .05/4 = 0.013. Limb symmetry index was calculated with the formula (involved/uninvolved) × 100 for each group.
RESULTS
Reliability
Intraclass correlation coefficients and SEMs for the intratester mean scores are summarized in Table 1. Intraclass correlation coefficients ranged from .79 to .94, and SEMs ranged from .38 to .68. The highest ICC was found with the step-down test and the lowest ICC with the bilateral squat test.
Table 1. Intrarater Reliability Estimates for Functional Tests

Correlation
The correlation matrix from the Pearson correlation coefficient analyses is found in Table 2. Correlation values between the VAS and the functional tests ranged from .386 to .730. Only the bilateral-squat test did not correlate significantly with the VAS.
Table 2. Pearson Correlation Coefficients

Limb Symmetry Index
Limb difference in the PFPS group was statistically significant (P < .013) for all unilateral functional tests. Limb difference in the normal subjects was not statistically significant for any of the unilateral functional tests. The LSI ranged from 95.1% to 100.6% in the normal group and 80.0% to 89.8% in the PFPS group.
When comparing the right limb of normal subjects with the involved limb of the PFPS group, the normal group scored more repetitions on the step-down, leg press, and bilateral squat. Test scores between groups were statistically different for the step-down test (P < .013).
DISCUSSION
Functional outcome measures should be simple to administer, inexpensive, reliable, and valid. Most of the functional tests previously reported in the literature are targeted to patients after anterior cruciate ligament injury.22 The purpose of our investigation was to determine the intrarater reliability of 5 functional performance tests. In addition, the relationship between pain and functional test scores was assessed.
Intrarater reliability measures the consistency of a test's score with respect to time and the evaluator. If a change does occur in the measure, one can attribute the change to true change and not chance. In this study, intrarater reliability was fair to high with a range from 0.79 to 0.94. The SEMs for all tests were less than one repetition, indicating high precision.23
Pain is a common symptom of individuals with PFPS. Therefore, a functional test for this population should correlate somewhat with a pain measure. All unilateral functional tests correlated significantly with the VAS. This finding indicates that these 4 functional tests were sensitive to changes in pain level. As pain level decreased, the number of repetitions performed increased. The bilateral squat correlated the least with the VAS and resulted in the lowest reliability. This result is probably due to the bilateral nature of the test. Because weight distribution was not monitored, subjects could shift weight to the uninvolved limb to avoid overloading the involved side.
Table 3. Group Data*
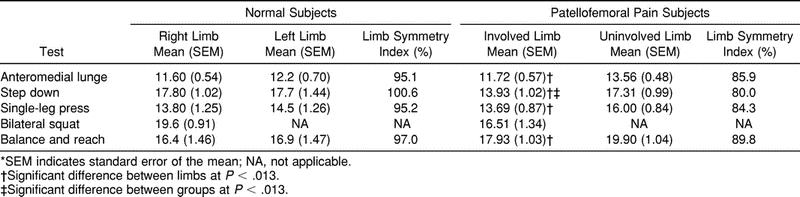
The 5 functional tests were tested on subjects with unilateral PFPS and, therefore, we hypothesized that there would be a difference in performance between the 2 limbs. For all tests, the uninvolved limb scored higher. Results from the paired t tests reached significance for the anteromedial lunge (P < .013), step-down (P < .013), leg press (P < .013), and balance and reach (P < .013).
We also compared the involved limbs of the PFPS group and the right limbs of the normal group. Surprisingly, the step-down was the only test that was significantly different between the PFPS group and the normal group (P < .013). The normal subjects scored more repetitions on the step-down and leg press but not on the anteromedial lunge or balance and reach. Both the anteromedial lunge and balance-and-reach tests require some work from both limbs, and this may interfere with a differential score.
Since only the step-down test was significantly different between groups, perhaps the LSI is a better indicator of PFPS discrimination. The LSI has been described in the literature as a return-to-sport criterion. Barber et al11 suggested an LSI of 85% as a satisfactory level for determining normalcy in the anterior cruciate ligament-reconstructed patient. For the 5 PFPS functional tests, the LSI ranged from 80.0% in the step-down to 89.8% in the balance and reach. The normal group averaged 95% for the unilateral tests. Because PFPS is so variable and function depends on the presence of pain, a higher LSI of 93 to 95% for each functional test may be a better predictor of normalcy in this patient population.
Because only intrarater reliability was statistically tested in this study, the results cannot be generalized to other clinicians. Further work is underway to determine the interrater reliability and sensitivity of these 5 functional tests before and after rehabilitation. Clinically, we have noted that subjects with PFPS improve on all the functional test scores and increase their LSI as they progress through rehabilitation.
CONCLUSIONS
The purpose of our study was to investigate the intrarater reliability of 5 functional performance tests. The intrarater reliability proved to be fair to high, with the highest reliability occurring with the step-down test and the lowest with the bilateral squat. The unilateral functional tests correlated significantly with the visual analog scale and differentiated between the involved and uninvolved extremities. However, the limb symmetry index is probably a better discriminator of patellofemoral pain syndrome than the absolute number of repetitions obtained on each test. The key to the reliability of the tests is that the clinician follow standard protocol. Further reliability testing among clinicians needs to be investigated.
The functional tests are designed to be used independently or together. Each test has a particular, unique contribution to the total functional picture. For patients who are unable to tolerate a single-leg squat, the single-leg press can be used to assess quadriceps function. As patients progress, the following 3 tests can be used: (1) the step-down requires balance and eccentric control of the quadriceps, (2) the anteromedial lunge requires a greater range of knee flexion, and (3) the balance and reach requires single-leg balance, limb stability, and proprioception. Before discharge, a patient with patellofemoral dysfunction should be able to complete the unilateral tests with the involved limb and score within 10% of the uninvolved limb.
Acknowledgments
ACKNOWLEDGMENTS
This study was funded by the American Physical Therapy Association Sports Physical Therapy Section's Small Grant Program.
Appendix
APPENDIX
Instruction for Functional Performance Tests
-
Anteromedial lunge: “You will stand behind a start line and perform 3 lunges with the uninvolved limb. The maximum distance achieved will be used to calculate the 80% target distance. The target distance will be marked on the floor with tape and recorded on the data form. Then, you will stand with your feet straddling the middle line. Your toes must stay behind the central line. Then, you will step out with your ___ leg so that your heel passes the marked distance (tester will demonstrate). You will continue the lunges for 30 seconds. Do you have any questions?”
Criteria: Only lunges in which the subject's heel touches beyond the 80% mark will be recorded.
-
Step-down: “You will stand on this 8-inch step with both legs. When I say go, you will lower your ___ leg so that your heel touches the ground. You will then return this leg to the platform and touch the top of the platform. You will continue this sequence until I say stop. The test is run for 30 seconds. Do not push off the ground as you lower your heel. Do you have any questions?”
Criteria: Heel must make contact with a slight hesitation both at the down phase and the start phase. Do not allow the subjects to vault up with their touch leg.
-
Single-leg press: “You will start with your back against the sled and your knees fully extended. Place your feet hip-width apart on the standing platform. When I say go, you will bend your ___ knee and lower your body on the sled to approximately 90° of knee flexion. I will tell you when you achieved the appropriate knee bend. You will continue performing the knee bends for 30 seconds. Do you have any questions?”
Criteria: Foot must remain flat on the Total Gym platform, no vaulting. Full 90° must be achieved (sled must touch platform).
-
Bilateral squat: “You will stand with your feet hip-width apart and squat down so that your knees bend to 90° like this (tester demonstrates). Your seat will touch this chair. Do not rest on the chair. You will return to the start position and repeat this activity for 30 seconds. Do you have any questions?”
Criteria: Buttock must touch seat. Subject must reach full standing with full knee extension.
-
Balance and reach: “You will stand behind a start line and perform 3 lunges with the uninvolved limb. The maximum distance achieved will be used to calculate the 80% target distance. The target distance will be marked on the floor with tape and recorded on the data form. Stand with your feet straddling the middle line. Your toes must stay behind the central line. You will step out with your ___ leg so that your heel passes the marked distance (tester will demonstrate). Do not rest your foot down when you reach the target distance. You will continue the reaches for 30 seconds. Do you have any questions?”
Criteria: Only reaches in which the subject's heel touches beyond the 80% mark will be recorded.
REFERENCES
- Mariani P P, Caruso I. An electromyographic investigation of subluxation of the patella. J Bone Joint Surg Br. 1979;61:169–171. doi: 10.1302/0301-620X.61B2.438268. [DOI] [PubMed] [Google Scholar]
- Westfall D C, Worrell T W. Anterior knee pain syndrome: role of the vastus medialis oblique. J Sport Rehabil. 1992;1:317–325. [Google Scholar]
- Ficat R P. Lateral fascia release and lateral hyperpressure syndrome. In: Pickett J C, Radin E L, editors. Chondromalacia of the Patella. Williams & Wilkins; Baltimore, MD: 1983. pp. 95–112. [Google Scholar]
- Greenfield M A, Scott W N. Arthroscopic evaluation and treatment of the patellofemoral joint. Orthop Clin North Am. 1992;23:587–600. [PubMed] [Google Scholar]
- James S L. Chondromalacia of the patella in the adolescent. In: Kennedy J C, editor. The Injured Adolescent Knee. Williams & Wilkins; Baltimore, MD: 1979. pp. 205–251. [Google Scholar]
- Kannus P, Nittymaki S. Which factors predict outcome in the nonoperative treatment of patellofemoral pain syndrome? A prospective follow-up study. Med Sci Sports Exerc. 1994;26:289–296. [PubMed] [Google Scholar]
- Radin E L. Does chondromalacia patella exist? In: Pickett J C, Radin E L, editors. Chondromalacia of the Patella. Williams & Wilkins; Baltimore, MD: 1983. pp. 68–82. [Google Scholar]
- Post M D, Fulkerson M D. Knee pain diagrams: correlation with physical examination findings in patients with anterior knee pain. Arthroscopy. 1994;10:618–623. doi: 10.1016/s0749-8063(05)80058-1. [DOI] [PubMed] [Google Scholar]
- Malek M M, Mangine R E. Patellofemoral pain syndromes: a comprehensive and conservative approach. J Orthop Sports Phys Ther. 1981;2:108–116. doi: 10.2519/jospt.1981.2.3.108. [DOI] [PubMed] [Google Scholar]
- Risberg M A, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther. 1994;19:212–217. doi: 10.2519/jospt.1994.19.4.212. [DOI] [PubMed] [Google Scholar]
- Barber S D, Noyes F R, Mangine R E, McCloskey J W, Hartman W. Quantitative assessment of functional limitation in normal and anterior cruciate ligament-deficient knees. Clin Orthop. 1990;255:204–214. [PubMed] [Google Scholar]
- Bolgla L A, Keskula D R. Reliability of lower extremity functional performance tests. J Orthop Sports Phys Ther. 1997;26:138–142. doi: 10.2519/jospt.1997.26.3.138. [DOI] [PubMed] [Google Scholar]
- Chesworth B M, Culham E G, Tata G E, Peat M. Validation of outcome measures in patients with patellofemoral syndrome. J Orthop Sports Phys Ther. 1989;10:302–308. doi: 10.2519/jospt.1989.10.8.302. [DOI] [PubMed] [Google Scholar]
- Reilly D T, Martens M. Experimental analysis of the quadriceps muscle force and patellofemoral joint reaction force for various activities. Acta Orthop Scand. 1972;43:126–137. doi: 10.3109/17453677208991251. [DOI] [PubMed] [Google Scholar]
- Gray G W. Lower Extremity Functional Profile. Wynn Marketing Inc; Adrian, MI: 1995. [Google Scholar]
- Reid D C. Chondromalacia patellae. Can Athl Ther Assoc J. 1982;8:13–20. [Google Scholar]
- Wilk K E, Davies G J, Mangine R E, Malone T R. Patellofemoral disorders: a classification system and clinical guidelines for nonoperative rehabilitation. J Orthop Sports Phys Ther. 1998;28:307–322. doi: 10.2519/jospt.1998.28.5.307. [DOI] [PubMed] [Google Scholar]
- Insall J, Falvo K A, Wise D W. Chondromalacia patellae: a prospective study. J Bone Joint Surg Am. 1976;58:1–8. [PubMed] [Google Scholar]
- Robinson A R, Darracott J. Chondromalacia patellae: a survey conducted at the Army Medical Rehabilitation Unit, Chester. Ann Phys Med. 1970;10:286–290. doi: 10.1093/rheumatology/x.6.286. [DOI] [PubMed] [Google Scholar]
- Price D D, McGrath P A, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- Melzack R. Pain: an overview. Acta Anaesthesiol Scand. 1999;43:880–884. doi: 10.1034/j.1399-6576.1999.430903.x. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Perrin D H, Fu F H, Minger K. Functional performance tests for the anterior cruciate ligament insufficient athlete. Athl Train J Natl Athl Train Assoc. 1991;26:44–50. [Google Scholar]
- Portney L G, Watkins M P. Foundations of Clinical Research: Applications to Practice. Appleton and Lange; Norwalk, CT: 1993. [Google Scholar]


