Abstract
Objective: To compare postural stability, single-leg hop, and isokinetic strength measurements in subjects after anterior cruciate ligament (ACL) reconstruction with an age- and activity-matched control group.
Design and Setting: Subjects reported to a sports medicine/athletic training research laboratory for testing. Subjects reported for one testing session for a total test time of 1 hour.
Subjects: Twenty subjects with ACL reconstructions (ACLRs) and 20 age- and activity-matched controls were selected to participate in this study. An arthroscopically assisted central one-third bone-patellar tendon procedure was used to repair the ACLs.
Measurements: We measured concentric and eccentric peak torque (Nm) measurements of the knee extensors and flexors at 120° and 240°/second on an isokinetic dynamometer. Unilateral and bilateral dynamic postural stability was measured as a stability index in the anterior-posterior and medial-lateral planes with the Biodex Stability System. We tested single-leg hop for distance to measure objective function.
Results: We found no significant difference between the ACLR and control subjects for stability index or knee-flexion peak torque scores. On the single-leg hop for distance, the ACLR subjects hopped significantly shorter distances with the involved limb than the uninvolved limb. Furthermore, the ACLR subjects' single-leg hop distance was significantly less when the involved limb was compared with the control-group matched involved limb, and the ACLR subjects performed significantly better when the uninvolved limb was compared with the control-group matched uninvolved limb. The ACLR subjects produced significantly greater torque in the uninvolved leg than in the involved leg. In addition, the peak torque was significantly less for the involved limb in the ACLR group when compared with the matched involved limb of the control group.
Conclusions: After ACLR (mean = 18 ± 10 months), single-leg hop-for-distance scores and quadriceps strength were not within normal limits when compared with the contralateral limb. Our results suggest that bilateral and single-limb postural stability in the ACLR group was not significantly different than the control group at an average follow-up of 18 months after surgery.
Keywords: ACL reconstruction, balance, single-leg hop, isokinetic strength, Biodex stability system
Injury to the anterior cruciate ligament (ACL) results in mechanical and functional instability. Athletes often find it difficult to return to full function after injury to the ACL, and surgery is frequently indicated.1 The purpose of surgery is to reestablish joint stability; surgeons attempt to minimize disruption to surrounding soft tissue during reconstruction. However, the implantation of a substitute for the ACL does not restore the sensorimotor sensory system, which may result in a compromised afferent neural system.2,3
Failure of stretched or damaged ligaments to provide adequate sensory feedback in the injured knee may contribute to loss of function and result in degeneration of the knee.4 Proprioceptive afferent neural input is also important in functional control during sport activities.5 It has been suggested that, after surgery, the ability to perform functional activities and balance may be decreased6–11 deficits have been found in the muscular and sensory processes after reconstructive surgery. Specifically, after ACL reconstruction with the bone-patellar tendon-bone procedure, strength deficits of 5% to 34% have been reported in the involved extremity compared with the contralateral limb after rehabilitation.12 Muscle control,13–17 gait,15 functional activities,7,14,15,17–21 and proprioception7,16,18,19,22,23 have been evaluated after ACL reconstruction, while the effect of dynamic postural stability has been minimally evaluated.24 Joint injury and articular disease have been shown to adversely affect joint position sense, movement sense, and function.7–9,11,23,25 Damage to receptors in the skin, muscles, tendons, and articular structures affects the ability to detect body movement and position. Without the normal integration of these processes, a person may be unable to perform physical activity in an efficient manner.
The use of force platforms has provided a sensitive method for measuring postural stability.26 However, the limited movement of the force platform is not indicative of normal joint movement during normal activities.27 Advances in technology have now made it possible to evaluate postural control more extensively than previously: for example, computer-interfaced devices enable postural stability to be quantified. The Biodex Stability System ([BSS] Biodex Medical Systems, Shirley, NY) is a device that is purported to reliably assess a patient's neuromuscular control in a closed-chain manner.28 A multiplane test is used to quantify the ability of a patient to maintain dynamic unilateral or bilateral postural stability on an unstable surface.28
The purpose of our study was to compare postural stability, single-leg hop, and isokinetic strength measurements in subjects after ACL reconstruction with an age- and activity-matched control group.
METHODS
Subjects
Postural stability, functional assessment, and isokinetic strength measures were evaluated in 20 subjects (11 men, 9 women) with a history of one surgery for ACL reconstruction (age = 25.8 ± 8.1 years, height = 175.8 ± 8.5 cm, weight = 73.3 ± 14.0 kg) and 20 age- and activity-matched subjects (11 men, 9 women) who served as the control group (age = 24.5 ± 6.9 years, height = 175.8 ± 8.3 cm, weight = 71.4 ± 12.1 kg). Recruited subjects all had ACL reconstruction performed in a similar fashion (arthroscopically assisted central bone-patellar tendon-bone graft). The mean time since surgery was 18 ± 10 months. Activity was matched as closely as possible using sections B and C on the Sports Participation Survey originally described by Seto et al.14 The study was approved by an institutional review board, and all subjects signed an informed consent form before participating.
Criteria for Participation
Subjects were selected to participate if they met the following criteria: (1) had only one surgery for a tear of the ACL that did not include a concomitant tear of the posterior cruciate ligament, (2) no evidence of collateral ligament repair at the time of surgery, (3) no history of surgery or traumatic injury to the contralateral knee, (4) no history of surgery or traumatic injury to the ankle joint on the reconstructed side, (5) no history of surgery or traumatic injury to either hip joint, and (6) no history of a medical problem that limited activities within the 6 weeks before testing. All subjects were released from a formal rehabilitation program before participation; however, standardization of the programs was not possible.
Testing Procedures
Subjects reported to the sports medicine/athletic training research laboratory for one testing session for a total test time of 1 hour. Before testing, subjects filled out the informed consent agreement and the Sports Participation Survey. The testing order for the postural stability, strength, and single-leg hop tests was counterbalanced to avoid a learning or fatigue effect. The testing session commenced by riding a Fitron (Cybex Corp, Ronkonkoma, NY) stationary bicycle for a 5-minute warm-up. Subjects were then instructed to perform several lower body flexibility exercises.
Biodex Stability System
Dynamic postural stability was assessed with the BSS. The support platform of the BSS can be placed at 6 levels. The resistance of the foot platform changes at each level. A setting of 6 is the most stable foot platform setting, and a setting of 1 is the least stable setting. At any level, the foot platform can move a full 20° in any direction. The measure of postural stability was the anterior-posterior and medial-lateral stability indexes (SI). The SI represents the standard deviation of foot platform deflection in degrees from the level position during a test. A high number indicates substantial movement away from the subject's center of balance; a low number indicates minimal movement during the test. The order of testing was counterbalanced to avoid any learning or fatigue effect. Intratester reliability for a protocol with decreasing stability levels on the BSS has been previously reported to be clinically reliable, with intraclass correlation coefficients ranging from .80 to .43.28
Pretest We assessed single-limb and bilateral stance. Order of testing was counterbalanced to control for bias and fatigue. Subjects were asked to step on the platform of the BSS and assume a comfortable position on the platform while maintaining slight flexion in the knees (10° to 15°). When the subjects felt comfortable, they were instructed that the platform would be released so that movement of 5° of deflection was possible. When the platform was released, the subjects were asked to position themselves so that they were comfortable standing on the platform. Once this position was attained, the platform was locked, the subjects' feet were centered on the platform, and we recorded foot-position coordinates.
Testing Procedure The testing procedure consisted of the support platform's progressively moving from level 6 (most stable) to level 1 (least stable) during a 30-second time period. We assessed single-limb (right and left) and bilateral stance postural stability. Subjects were given 2 practice trials to reduce any learning effects.27 Subjects were asked to stand with the knees flexed to 10° to 15° and to look straight ahead at an X marked directly in front of them while attempting to maintain the platform in a level position. They were given a 1-minute rest between testing conditions.
Single-Leg Hop-for-Distance Test
The single-leg hop for distance is a commonly used functional measurement designed to test both strength and confidence in the tested leg29 that correlates positively with muscular strength.14 The first extremity to be tested was randomly chosen. The single-leg hop was performed 3 times with each leg. Subjects were asked to hop as far as possible from a predetermined line and to land on the same leg. Use of arm swing was not discouraged, as subjects were asked to perform with maximal effort. The best distance of the 3 tests was recorded in centimeters and used as the dependent score.
Isokinetic Evaluation
Strength testing was performed for knee flexion and knee extension at 120° per second and 240° per second on the Kin-Com dynamometer (Chattanooga Group, Hixson, TN) in the seated position. Concentric and eccentric contractions were performed at each velocity. The first extremity and velocity to be tested were counterbalanced to prevent fatigue or learning effects. Subjects were seated on the dynamometer and stabilized with chest and leg hook-and-loop straps according to the manufacturer's guidelines. The axis of rotation of the Kin-Com was adjusted so as to align with the joint margin of the knee. The distal pad of the dynamometer arm was placed just proximal to the malleoli. Before testing, we asked subjects to extend the leg; the weight of the limb was recorded and corrected for gravity using the Kin-Com software package. Before data collection, subjects performed 4 practice repetitions for each velocity setting at 75% of subjective maximal effort. Each concentric contraction was followed by an eccentric contraction for both extension and flexion of the knee joint. After this warm-up phase, a 2-minute rest was given. The evaluation phase consisted of 3 repetitions of maximal concentric and eccentric contractions for extension and flexion of each leg. We informed subjects that they needed “to push or pull as hard and fast as they can” against the resistance provided by the dynamometer. Order of testing was counterbalanced to prevent a fatigue or learning effect. A 5-minute rest period was given before the opposite leg was tested. Peak torque values were used as the dependent measure of muscle strength.
Statistical Analyses
Extremity matching was achieved by matching the injured extremity (right/left) from the ACL-reconstruction (ACLR) subject with the same extremity in the uninjured subject. We used a repeated-measures analysis of variance (ANOVA) with 1 between-subjects factor (group) and 1 within-subjects factor (plane) to determine if differences existed for bilateral postural stability assessed with the BSS. With a repeated-measures ANOVA with 1 between-subjects factor (group) and 2 within-subjects factors (extremity and plane), we examined differences in single-limb postural stability. A repeated-measures ANOVA with 1 between-subjects factor (group) and 1 within-subjects factor (extremity) was calculated to assess differences in the single-leg hop-for-distance test. We assessed differences between hamstrings and quadriceps knee muscle strength with 2 repeated-measures ANOVAs with 1 between-subjects factor (group) and 3 within-subjects factors (extremity, contraction, and velocity). Tukey Honestly Significant Differences post hoc comparisons were performed for all significant interactions, and all statistical tests were considered significant at the P < .05 level.
RESULTS
The postural stability, single-leg hop test, and strength descriptive data are found in Tables 1,2,3,4,5,6. We found no differences between the ACLR and control subjects for the single-limb and bilateral stability index scores. For the single-leg hop test, the group-by-extremity interaction was significant (F1,38 = 37.88, P < .01). Additionally, the analysis revealed a main effect for extremity (F1,38 = 27.09, P < .01). Using Tukey post hoc analysis, we noted that ACLR subjects hopped a significantly shorter distance with the involved limb than with the uninvolved limb (P < .01). Furthermore, the ACLR subjects' performance for the hop test was significantly worse when the involved limb was compared with the control group's matched limb (P < .05), and the ACLR subjects performed significantly better when the uninvolved limb was compared with the control group's matched limb (P < .01).
Table 1. Single-Limb Postural Stability Index (°) for Anterior Cruciate Ligament–Reconstructed (ACLR) and Control Subjects (Mean ± SD)
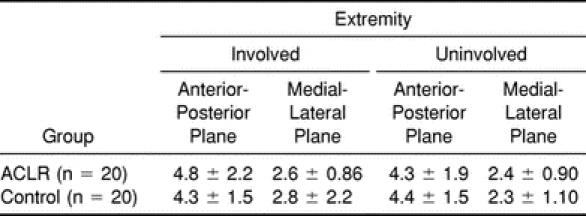
Table 2. Bilateral Limb Postural Stability Index (°) for Anterior Cruciate Ligament–Reconstructed (ACLR) and Control Subjects (Mean ± SD)
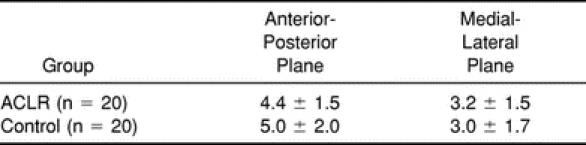
Table 3. Knee-Flexion Values Measured as Peak Torque (N·m) for Anterior Cruciate Ligament–Reconstructed (ACLR) and Control Subjects (Mean ± SD)
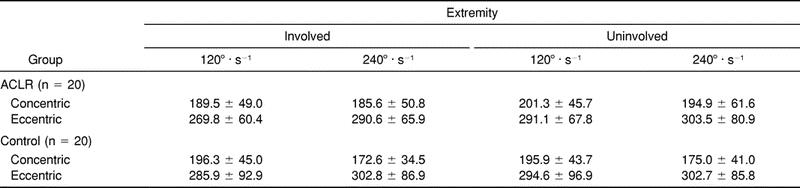
Table 4. Knee-Extension Values Measured as Peak Torque (N·m) for Anterior Cruciate Ligament–Reconstructed (ACLR) and Control Subjects (Mean ± SD)
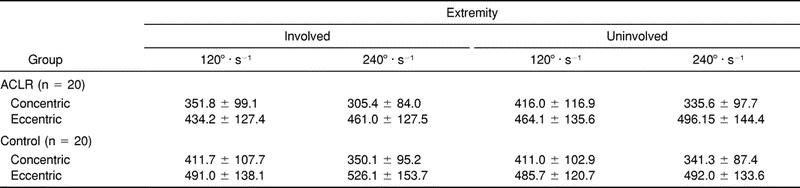
Table 5. Group-by-Extremity Interaction for the Single-Leg Hop-for-Distance Test (cm) for Anterior Cruciate Ligament Reconstructed (ACLR) and Control Subjects (Mean ± SD)
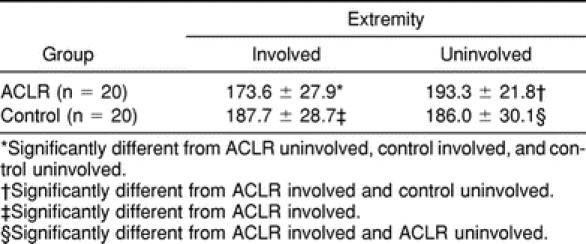
Table 6. Group-by-Extremity Interaction for Knee Extension as above (Mean ± SD)
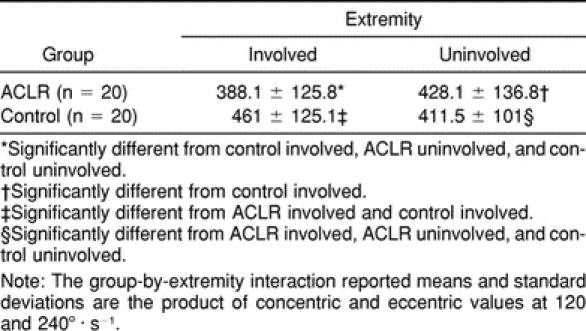
For knee-flexion strength, there was no significant differences between the ACLR and control groups or between extremities. For knee-extension strength, there was a significant interaction for group by extremity (F1,38 = 9.40, P < .01). Additional significant 2-way interactions were found for extremity by velocity (F1,38 = 6.03, P < .05) and contraction by velocity (F1,38 = 103.7, P < .01). Tukey post hoc analysis revealed that ACLR subjects produced significantly greater torque in the uninvolved leg than the involved leg, and the involved limb of the ACLR group produced significantly less torque compared with the matched involved limb of the control subjects (P < .05).
DISCUSSION
Our primary finding was that after ACLR, subjects had deficits in hop and strength performance but did not have deficits in postural stability. A major area of focus in our study was to examine dynamic postural stability after ACLR. We found no significant difference in dynamic postural stability at an average of 18 months after ACLR. To our knowledge, study of postural stability after ACLR has been limited.24,30 Others have evaluated static postural stability30 and static and dynamic postural stability.24 Our findings are consistent with those of Harrison et al,30 who found no significant difference between the ACLR and uninvolved knees during eyes-open testing on the Chattecx Balance System (Chattecx Corp, Chattanooga, TN). However, our findings are in contrast to Hoffman et al,24 who reported increased dynamic phase duration when the ACLR group was compared with a control group. The difference noted between Hoffman et al24 and our study may be explained by methodologic differences. Hoffman et al24 evaluated postural control after a muscularly induced perturbation and measured the time it took for sway variability to return to prestimulation levels. Postural stability was measured in the sagittal direction only. Our subjects attempted to maintain balance on a moving platform; postural stability was assessed in the sagittal and frontal planes. In addition, our subjects were 18 ± 10 months post-ACLR, while the mean time from surgery was 9.53 months for subjects studied by Hoffman et al.24
Mizuta et al25 compared a group of ACL-deficient patients who were functionally stable with a group of patients who were functionally unstable. Functional stability was defined as full return, without giving way, to the same sport at the same level as before injury.25 The authors found that the functionally unstable group swayed significantly more than the functionally stable group. Therefore, deficits in postural stablity have been demonstrated in ACL-deficient patients who complain of the knee “giving way” but not in a group of patients who were identified as functionally stable. It appears that some ACL-deficient patients are able to function without the knee “giving way.” Some ACL-deficient patients may compensate neuromuscularly in adapting to the loss of the ACL.31,32 Similar to the results of the functionally stable group in the Mizuta et al25 study, our results revealed no differences in postural stability for a group of subjects after ACLR.
Deficits in proprioception exist after ACLR. In subjects 11 to 26 months postsurgery, Lephart et al23 demonstrated a significant kinesthetic deficit in the ACLR knee compared with the uninvolved knee, from a starting position of 15° moving into both flexion and extension. The time since surgery and the angle of the knee during testing were similar to our study. However, their testing was performed in a nonweight-bearing position whereas our study used a weight-bearing position. The lack of significant differences in postural stability between the reconstructed and uninvolved knees and between the reconstructed knee and the matched extremity of the control group in our study indicates that, after ACLR and rehabilitation, any loss in the ability to maintain dynamic postural stability returns to normal. It may be that the lack of significant differences in postural stability in our study is the result of a combination of restoring mechanical stability via the reconstruction, restoring neuromuscular control via the rehabilitation process, and performing the test in a weight-bearing position. Therefore, it may be that proprioceptive deficits exist as described by Lephart et al23 but that the interval from surgery in our subjects was long enough that proprioception in the joint was restored. However, it may be more likely that muscle afferent receptors dominated sensory feedback during the balance episodes.
Single-Leg Hop-For-Distance Test
The single-leg hop-for-distance test was chosen as an objective functional test that would provide stress to the knee joint while also allowing us to evaluate strength and confidence in the tested extremity. Subjects who underwent ACLR hopped farther with the uninvolved limb than with the involved limb. The significant difference in the single-leg hop-for-distance test scores between the involved and uninvolved extremities for the ACLR group suggests that, at an average of 18 months postreconstruction, this measure of functional performance was not within normal limits. Furthermore, ACLR subjects were unable to hop as far as the control group when the “involved” limbs were compared. This finding suggests that the ACLR subjects' ability to perform a single-leg hop-for-distance test was not within normal limits when compared with a matched control group. However, the ACLR subjects were able to hop a significantly greater distance when the uninvolved limb was compared with the uninvolved limb of the control group. This result suggests that strength was significantly increased in the ACLR subjects' uninvolved leg when compared with the uninvolved leg of the matched control subjects. The increased strength in the uninvolved leg may have occurred to compensate for the loss of function after the injury and subsequent surgical reconstruction.
Single-leg hop-for-distance scores are commonly expressed as a limb symmetry index. The limb symmetry index is calculated as the mean score of the involved limb divided by the mean score of the uninvolved limb, with the result multiplied by 100.
Noyes et al10 assessed the sensitivity of 4 types of single-leg hop tests for a group of ACL-deficient patients. The 4 hop tests were the single-leg hop for distance, the timed hop, the triple hop for distance, and the crossover hop for distance. Noyes et al10 described a limb symmetry score of below 85% as abnormal. In a similar study, Wilk et al21 examined the relationship between isokinetic testing and functional testing for a group of ACLR patients. They compared 3 functional tests: the single-leg hop for distance, the single-leg timed hop, and the single-leg crossover. We chose to assess only the single-leg hop-for-distance test because of time and fatigue considerations.
When the single-leg hop-for-distance scores in our study are expressed as a limb symmetry index, 43% of the ACLR patients had a limb symmetry score below 85%, versus 47% of the subjects described by Wilk et al.21 Our findings are similar to those of Wilk et al,21 although the time since surgery in their study was 6.45 months, versus 18.1 months in our study. The longer duration since surgery could account for the decreased number of abnormal limb symmetry scores in our study.
We found no difference when comparing the single-leg hop scores between the involved and uninvolved extremities of the control group, which is consistent with Greenberger and Paterno.33 Our results and others suggest that clinicians may want to concentrate on improving functional strength after ACLR.10,21
Isokinetic Strength
Knee Flexion Exercises that focus on strengthening the hamstring musculature are recommended after ACLR in an attempt to reduce anterior translation forces of the tibia. The lack of a difference in peak torque during knee flexion supports previous findings that after 12 to 14 weeks post-ACLR, knee-flexion strength returns to near-normal levels.34 Our findings are inconsistent with those of Seto et al,14 who reported that hamstring strength in the reconstructed limb was significantly less than that in the control leg at 120 and 240° per second for subjects who had an intra-articular ACLR. The reported differences between the Seto et al14 study and our investigation may be attributed to the more conservative rehabilitation process that was followed at the time that study was conducted.
Knee Extensionv Aggressive rehabilitation after ACLR commonly employs immediate motion, weight bearing, and exercise to initiate quadriceps contraction.34 However, quadriceps strength is slow to return to normal levels. Our results indicate that ACLR subjects produced significantly more torque with the uninvolved knee than with the reconstructed knee. The strength of the knee extensors for the ACLR subjects may not have returned to preinjury levels. Similarly, the matched involved knee of the control group produced significantly greater torque than the reconstructed knee of the ACLR subjects. As such, the quadriceps muscle strength of ACLR subjects in our study had not returned to near-normal levels after an average of 18 months after surgical repair. Our findings are consistent with those of Seto et al14 and Hoffman et al,24 who reported that quadriceps strength in the reconstructed limb was significantly less than that in the control leg for subjects who had an intra-articular ACLR. For comparison, patients in the Seto et al14 study underwent an intra-articular or extra-articular ACLR, and patients in the Hoffman et al24 study underwent an arthroscopically assisted patellar tendon graft.
The differences in strength and function but not in postural stability may be explained by the specificity of the exercise and possible compensation by other lower extremity muscle groups. The ability to perform a single-leg hop depends on the strength of the quadriceps muscle. A decrease in quadriceps strength would result in reduced loading capacity of the knee joint and the inability to absorb and generate force.35 In addition, the influence of the graft selection cannot be disregarded, as strength deficits of 5% to 34% have been reported after ACLR with the bone-patellar tendon-bone procedure and subsequent rehabilitation.12 The ability to balance on an unstable platform requires the coordinated activation of the lower leg musculature. While knee extension and the single-leg hop require maximal contraction of the supporting musculature, single-limb and double-limb balance do not. Therefore, the ability to balance on the dynamic platform may not have been a sufficient challenge. The use of different methods to maintain balance has been defined as a strategy. In 1990, Horak et al36 described these strategies as “stereotypical movement patterns in order to achieve or maintain postural stability during anterior/posterior sway with a fixed stance.” These strategies most often involve using primarily the ankle or the hip for neuromuscular control. Therefore, activation of other muscle groups (ie, ankle and hip) in addition to the quadriceps may have accounted for the lack of difference in single-limb and bilateral balance in our study.37
Limitations
One limitation with our study was that it was not possible to account for differences in rehabilitation programs among subjects. All the ACLR subjects were subjectively asked how long they participated in a physical therapy program; the average length of time was 8 to 10 weeks. Therefore, we could not account for the differences in rehabilitation programs, nor could we control individual compliance in these programs. A patellar-tendon autograft procedure was used to repair the torn ACL in all ACLR subjects. Every attempt was made to obtain all subjects from the same physician; however, due to difficulty in subject recruitment, 14 of the ACLR patients were operated on by the same surgeon, while the other 7 patients each had a different surgeon. Different physicians, rehabilitation programs, and compliance to the rehabilitation programs may have reduced the homogeneity of our group, making it more difficult to detect differences. It would be interesting to further investigate postural stability before the reconstruction process and with more control of the subjects and their rehabilitation after surgery. Further research should examine the length of time that postural stability deficits exist after surgery and when these approach normal. Further knowledge of this process would aid clinicians in their decision on when to return patients to full activity after ACLR.
CONCLUSIONS
After ACLR (mean = 18 ± 10 months), subjects did not have significant loss in bilateral or single-limb postural stability when assessed with a Biodex Stability System. However, within the limits of our study, quadriceps strength and functional hop performance were not within normal limits when compared with the contralateral limb and a control group. Of clinical importance and in agreement with others38 is the fact that leg strength and functional performance (as assessed with a single-leg hop-for-distance test) may not return to normal (±5%) for up to 2 years. In addition, clinicians must emphasize that quadriceps femoris strength be maintained after organized therapy for ACLR. If the subjects in our study are indicative of the general population, deficits in strength and function may predispose them to limited performance and possibly further injury.
REFERENCES
- Fu F H, Bennett C H, Ma B, Menetrey J, Lattermann C. Current trends in anterior cruciate ligament reconstruction, part II: operative procedures and clinical correlations. Am J Sports Med. 2000;28:124–130. doi: 10.1177/03635465000280010801. [DOI] [PubMed] [Google Scholar]
- Nyland J, Brosky T, Currier D, Nitz A, Caborn D. Review of the afferent neural system of the knee and its contribution to motor learning. J Orthop Sports Phys Ther. 1994;19:2–11. doi: 10.2519/jospt.1994.19.1.2. [DOI] [PubMed] [Google Scholar]
- Noyes F R, Butler D L, Paulos L E, Grood E S. Intra-articular cruciate reconstruction, part I: perspectives on graft strength, vascularization and immediate motion after replacement. Clin Orthop. 1983;172:71–77. [PubMed] [Google Scholar]
- Kennedy J C, Alexander I J, Hayes K C. Nerve supply of the human knee and its functional importance. Am J Sports Med. 1982;10:329–335. doi: 10.1177/036354658201000601. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Barrack R L, Lund P J, Skinner H B. Knee joint proprioception revisited. J Sport Rehabil. 1994;3:18–42. [Google Scholar]
- Barrett D S. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991;73:833–837. doi: 10.1302/0301-620X.73B5.1894677. [DOI] [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- Barrack R L, Skinner H B, Cook S D, Haddad R J. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol. 1983;50:684–687. doi: 10.1152/jn.1983.50.3.684. [DOI] [PubMed] [Google Scholar]
- Noyes F R, Barber S D, Mangine R E. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- Barrett D S, Cobb A G, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73:53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- Hiemstra L A, Webber S, MacDonald P B, Kriellaars D J. Knee strength deficits after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2000;32:1472–1479. doi: 10.1097/00005768-200008000-00016. [DOI] [PubMed] [Google Scholar]
- Ghez C. Posture. In: Kandel E R, Schwartz J H, Jessell T M, editors. Principles of Neural Science. Elsevier Science; New York, NY: 1991. pp. 596–607. [Google Scholar]
- Seto J L, Orofino A S, Morrissey M C, Medeiros J M, Mason W J. Assessment of quadriceps/hamstring strength, knee ligament stability, functional and sports activity levels five years after anterior cruciate ligament reconstruction. Am J Sports Med. 1988;16:170–180. doi: 10.1177/036354658801600215. [DOI] [PubMed] [Google Scholar]
- Goldie P A, Bach T M, Evans O M. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510–517. [PubMed] [Google Scholar]
- Barrack R L, Skinner H B, Buckley S L. Proprioception in the anterior cruciate deficient knee. Am J Sports Med. 1989;17:1–6. doi: 10.1177/036354658901700101. [DOI] [PubMed] [Google Scholar]
- Harter R A, Osternig L R, Singer K M, James S L, Larson R L, Jones D C. Long-term evaluation of knee stability and function following surgical reconstruction for anterior cruciate ligament insufficiency. Am J Sports Med. 1988;16:434–443. doi: 10.1177/036354658801600502. [DOI] [PubMed] [Google Scholar]
- Ciccotti M G, Kerlan R K, Perry J, Pink M. An electromyographic analysis of the knee during functional activities, II: the anterior cruciate ligament-deficient and -reconstructed profiles. Am J Sports Med. 1994;22:651–658. doi: 10.1177/036354659402200513. [DOI] [PubMed] [Google Scholar]
- Ciccotti M G, Kerlan R K, Perry J, Pink M. An electromyographic analysis of the knee during functional activities, I: the normal profile. Am J Sports Med. 1994;22:645–650. doi: 10.1177/036354659402200512. [DOI] [PubMed] [Google Scholar]
- Bynum E B, Barrack R L, Alexander A H. Open versus closed chain kinetic exercises after anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 1995;23:401–406. doi: 10.1177/036354659502300405. [DOI] [PubMed] [Google Scholar]
- Wilk K E, Romaniello W T, Soscia S M, Arrigo C A, Andrews J R. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;2:60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- Harter R A, Osternig L R, Singer K M. Knee joint proprioception following anterior cruciate reconstruction. J Sport Rehabil. 1992;1:103–110. [Google Scholar]
- Lephart S M, Kocher M S, Fu F H, Borsa P A, Harner C D. Proprioception following anterior cruciate ligament reconstruction. J Sport Rehabil. 1992;1:188–196. [Google Scholar]
- Hoffman M, Schrader J, Koceja D. An investigation of postural control in postoperative anterior cruciate ligament reconstruction patients. J Athl Train. 1999;34:130–136. [PMC free article] [PubMed] [Google Scholar]
- Mizuta H, Shiraishi M, Kubota K, Kai K, Takagi K. A stabilometric technique for evaluation of functional instability in anterior cruciate ligament-deficient knee. Clin J Sport Med. 1992;2:235–239. [Google Scholar]
- Nashner L M, Peters J F. Dynamic posturography in the diagnosis and management of dizziness and balance disorders. Neurol Clin. 1990;8:331–349. [PubMed] [Google Scholar]
- Pincivero D M, Lephart S M, Henry T. Learning effects and reliability of the Biodex Stability System [abstract] J Athl Train. 1995;30:S48. [Google Scholar]
- Schmitz R J, Arnold B L. Intertester and intratester reliability of a dynamic balance protocol using the Biodex Stability System. J Sport Rehabil. 1998;7:95–101. [Google Scholar]
- Sachs R A, Daniel D M, Stone M L, Garfein R F. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17:760–765. doi: 10.1177/036354658901700606. [DOI] [PubMed] [Google Scholar]
- Harrison E L, Duenkel N, Dunlop R, Russell G. Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther. 1994;74:245–252. doi: 10.1093/ptj/74.3.245. [DOI] [PubMed] [Google Scholar]
- Andriacchi T P, Birac D. Functional testing in the anterior cruciate ligament-deficient knee. Clin Orthop. 1993;288:40–47. [PubMed] [Google Scholar]
- Rudolph K S, Eastlack M E, Axe M J, Snyder-Mackler L. 1998 Basmajian Student Award Paper: Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- Greenberger H B, Paterno M V. Relationship of knee extensor strength and hopping test performance in the assessment of lower extremity function. J Orthop Sports Phys Ther. 1995;22:202–206. doi: 10.2519/jospt.1995.22.5.202. [DOI] [PubMed] [Google Scholar]
- Wilk K E, Arrigo C A, Andrews J R, et al. Anterior cruciate ligament reconstruction rehabilitation: a 12 week follow-up of isokinetic testing in recreational athletes. Isokin Exerc Sci. 1992;2:82–91. [Google Scholar]
- Pfeifer K, Banzer W. Motor performance in different dynamic tests in knee rehabilitation. Scand J Med Sci Sports. 1999;9:19–27. doi: 10.1111/j.1600-0838.1999.tb00202.x. [DOI] [PubMed] [Google Scholar]
- Horak F B, Nashner L M, Diener H C. Postural strategies associated with somatosensory and vestibular loss. Exp Brain Res. 1990;82:167–177. doi: 10.1007/BF00230848. [DOI] [PubMed] [Google Scholar]
- Ernst G P, Saliba E, Diduch D R, Hurwitz S R, Ball D W. Lower extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000;80:251–260. [PubMed] [Google Scholar]
- Risberg M A, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]


