Abstract
Objective: To describe a treatment strategy for paradoxical vocal-cord dysfunction (PVCD) as it applies to an athletic population.
Background: Paradoxical vocal-cord dysfunction has been identified as a cause of dyspnea and stridor in athletes. The basic element of PVCD is an inappropriate closure of the vocal cords during respiration, resulting in airway obstruction. This condition is familiar to speech-language pathologists and otolaryngologists yet remains poorly understood in the sports medicine community. Treatment strategies are even less understood. A therapeutic exercise program designed to promote diaphragmatic breathing may allow an athlete to gain control during episodes of dyspnea. Elimination of contributing or concomitant conditions is critical to resolution of the condition.
Description: The treatment of PVCD requires an understanding of the pathoanatomy of the condition. The focus of the exercise program is on relaxation of the larynx and conscious activation of the diaphragm and abdominal muscles during respiration. The athlete must have a sense of laryngeal control while performing the exercises. In addition, the patient and practitioner must realize the amount of neuromuscular reeducation required to change breathing patterns.
Clinical Advantages: This therapy may allow the athlete to gain control over episodic dyspnea, participate in athletic activities with fewer complications, and, perhaps, reduce or eliminate medications prescribed to treat suspected bronchospasm.
Keywords: dyspnea, stridor, larynx, speech therapy
Over the past decade, paradoxical vocal-cord dysfunction (PVCD) has been well studied, although little information has been presented in sports medicine journals. Most of the literature has addressed the recognition of PVCD in contrast to other reactive airway diseases.1–7 Authors have stressed the need for complete diagnostic testing, including visual examination of the vocal cords for subjects with exercise-induced dyspnea. Certainly, recognition of PVCD is critical to resolution of the condition. Treatment strategies, however, are often overlooked or presented with little detail. Indeed, much of the existing literature focuses on the emotional component associated with PVCD, although this is not necessarily a primary trigger for athletic subjects.8–10
A common pattern is presented in the literature: a patient reports episodes of dyspnea or shortness of breath during exercise, and medications prescribed to relieve symptoms are ineffective. The continued symptoms, coupled with the failure of the medication and the patient's inability to complete assigned “fitness” drills, increases the emotional stress the athlete feels during practice. If the cause of respiratory distress is unrecognized and uncontrolled (as with undiagnosed PVCD), the resultant emotional stress can exacerbate PVCD symptoms. It has been our experience that, over time, the misdiagnosed athlete becomes less able to perform necessary cardiovascular fitness exercises (including practice drills) and less able to meet the demands of athletic participation. In addition, one should not underestimate the effect the labored breathing may have on the patient's coaches and teammates, who may be concerned for his or her mortality.
In some instances, patients with acute PVCD have been directed to an emergency department for treatment of uncontrolled shortness of breath.1 More commonly, the continued symptoms and dissatisfaction with the course of treatment prompt further testing and, ultimately, the diagnosis of PVCD. This is often a diagnosis of exclusion, perhaps resulting from a lack of familiarity with the condition. A health care professional with a high index of suspicion and an understanding of the signs and symptoms of PVCD is in a position to direct the athlete to the appropriate specialist for definitive care, thereby avoiding exhaustive testing and inappropriate medication and prompting a quicker resolution of the condition.
Current literature emphasizes the treatment of psychological and emotional stressors; speech therapy is recognized as a treatment strategy, but little detail is provided.1–3,8–10 Indeed, some form of psychological dysfunction may be involved in PVCD. It has been suggested that athletes with a history of clinical depression or abuse (physical, sexual, or verbal) are at risk for PVCD.6 More commonly, athletic individuals with PVCD are identified as high achievers who strive for external validation and are likely to avoid situations involving confrontation.11 Further, these individuals' perceptions of third-party (ie, parents', coaches') expectations may be exaggerated, and they are likely to feel alienated from their teammates. Thus, a pattern unfolds in which an individual sets goals that may be intended to please a third party but then fails to meet those goals. A physical malady (in this case, severe narrowing of the larynx) may be manifested to explain the failure; poor understanding of the malady or its causes may exacerbate the level of stress and the intensity of the symptoms. This physical malady may also prevent the individual from normal participation in an event, thereby complicating the previously mentioned issues.
In the athletic patient, the emotional component may often be secondary to the dyspnea and failure to control it.10 The focus of speech therapy for PVCD patients is generally on respiratory control and diaphragmatic breathing patterns. As the athlete gains control over breathing patterns, he or she may realize a sense of control of this condition and reduce the emotional stress associated with dyspnea. Speech therapy, alone or in combination with other treatment interventions, has proven to be successful in reducing or eliminating the paroxysms of wheezing, stridor, and dyspnea.1,3–5,11
The patient must also be evaluated for coexisting medical conditions, such as asthma, exercise-induced asthma (EIA), gastroesophageal reflux disease (GERD), and pharyngeal erythema (secondary to postnasal drip); the latter 2 conditions can increase the sensitivity of the larynx.9,10,12 Habitual coughing and throat clearing can also increase sensitivity of the larynx, increasing the likelihood of PVCD. Finally, the hydration level of the vocal cords affects not only the mucus covering of the tissue but also the viscoelastic properties of the cords.13
The purpose of this paper is to describe a treatment strategy for PVCD. Those readers interested in diagnostic testing are referred to the first article in this series. The treatment strategy described in this paper has been used successfully with collegiate and high school athletes and has been administered in both chronic and acute settings by speech-language pathologists and certified athletic trainers. It must be stressed that any effort to resolve PVCD must address (or unequivocally eliminate) concomitant medical conditions such as asthma, EIA, GERD, and rhinitis and behavioral deficiencies including throat clearing and insufficient fluid intake.
Management of Paradoxical Vocal-Cord Dysfunction
With normal breathing, the vocal cords are in an abducted position during inspiration and move slightly toward the midline during expiration to control airflow (Figure 1).14,15 Under physical or emotional stress, laryngeal spasm can cause the vocal cords to adduct considerably, narrowing or even closing the glottis, creating the dyspnea that is often misattributed to EIA.2 Because of the potential sequelae associated with EIA, differentiating between these conditions can be difficult. However, an athlete with PVCD typically identifies the neck or throat as the source of airway restriction, while the EIA sufferer usually indicates the chest as the source of tightness. In addition, wheezing, which is more closely associated with EIA, is characterized by whistling sounds resulting from the narrowing of the respiratory tract; stridor, produced at the level of the larynx, is characterized by a harsher noise, like that of sawing.
Figure 1.
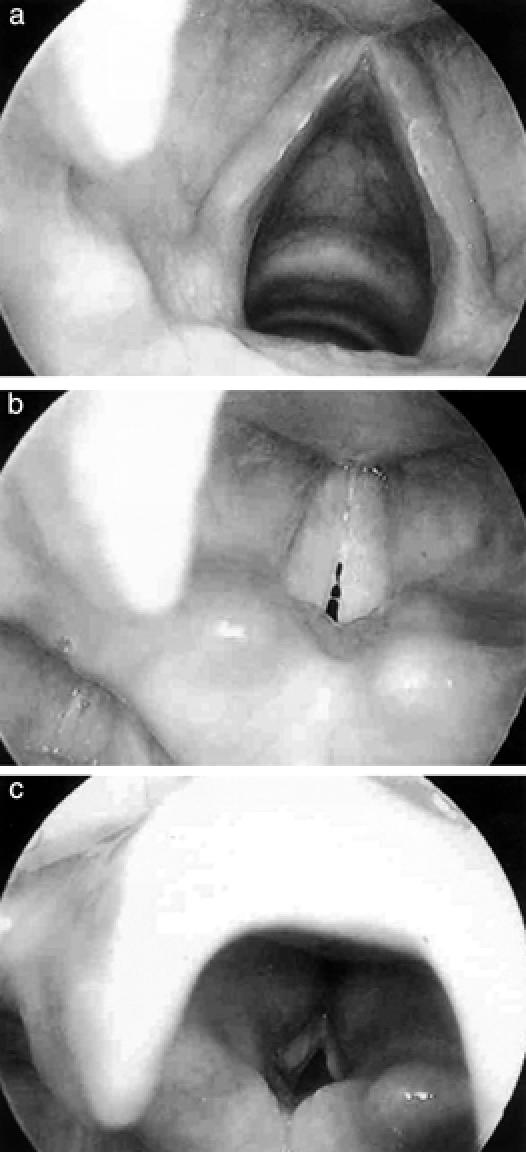
a, Vocal-cord abduction during normal inhalation. b, Vocal cords during normal phonation. c, Severe vocal-cord adduction (paradoxical movement). This clearly illustrates the “diamond-shaped posterior chink.”
A common approach in the management of PVCD is to treat it as a chronic condition with recurring episodes of acute dyspnea. Successful control of acute episodes can reduce the drama associated with respiratory distress. This is facilitated by a calm, reassuring presence and an empathetic approach. Initially in the management of acute dyspnea, the athlete is instructed to bend at the waist or crouch or kneel to promote diaphragmatic breathing. The athlete is further instructed to focus on controlled, relaxed exhalations through pursed lips, inhalations through the nose, and maintenance of a relaxed shoulder girdle. Some athletes achieve relaxation of the larynx and regain normal vocal-cord movement through panting or by taking small sips of water or talking.7,13,16 It is critical that the athlete has a sense of laryngeal control during these episodes. As breathing becomes controlled, the athlete is encouraged to stand upright while maintaining diaphragmatic breathing. Diaphragmatic breathing is preferred to clavicular breathing due to the increased laryngeal tension promoted through clavicular breathing (Figure 2).
Figure 2.
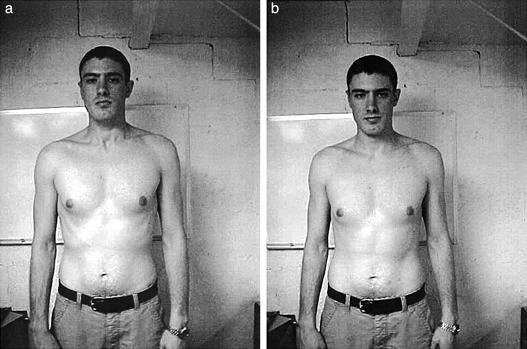
a, Clavicular breathing: note the increased tension in neck and larynx. This contributes to laryngeal tightness and spasm. b, Diaphragmatic breathing: note relaxed shoulder girdle and abdominal expansion.
Definitive treatment intervention to reduce or eliminate episodes may include therapeutic exercises, counseling, and medications to treat concomitant conditions. Certainly, therapeutic exercise is the area in which the certified athletic trainer can have great impact on this condition. Martin et al4 described behavioral or symptomatic therapy presented in a nonthreatening approach that facilitates laryngeal relaxation by maintaining continuous airflow through the vocal cords using diaphragmatic breathing.4 Therapy focusing on self-awareness encourages the individual to become aware of sensations of heightened laryngeal and respiratory tension in comparison with laryngeal sensations when voluntary control is exercised. Therapy techniques include laryngeal-control exercises using diaphragmatic breathing without laryngeal constriction or tension and focusing on prolonged exhalation.11 Athletes are encouraged to practice therapy techniques daily and to use the techniques at the first sign of laryngeal tightness or stridor.
The focus of the breathing pattern therapy is “relaxed-throat” breathing and maintaining laryngeal control during inhalation and exhalation (Table). Initially, the athlete is instructed in inhaling or “sniffing in” through the nose and exhaling gently through pursed lips. Attention is given to abdominal expansion during inhalation and abdominal relaxation during exhalation. In addition, visual imaging techniques are taught as a method of keeping the vocal cords open during rapid breathing. These include visualizing the throat being as wide open as a baseball during inhalation. Additional techniques used to help gain control over fast breathing include an open jaw and relaxed-tongue position while concentrating on diaphragmatic breathing. These exercises are initially instituted in a supine position, then standing, and finally during physical activity (ie, treadmill running).
Table 1.
Relaxed-Throat Breathing Exercises*
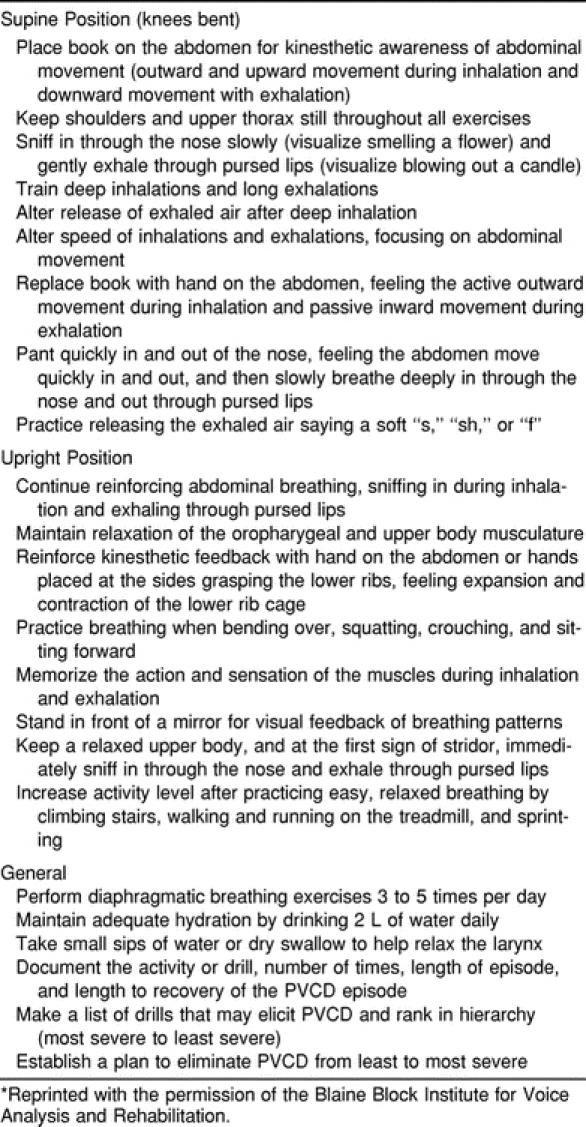
The athlete is encouraged to perform the exercises 3 to 5 times per day. Overload may be achieved in the form of increased resistance (ie, books on the abdomen while breathing) or increased physical stress (ie, running). These therapy techniques require a degree of neuromuscular reeducation. Both patient and practitioner must be aware of the learning process involved and the tendency to fall back into faulty patterns during periods of stress. It is important for the athlete to have verbal and physical cues to adjust breathing during practice and game settings.
Treatment of PVCD in athletes is multidisciplinary. The speech-language pathologist and certified athletic trainer work in concert to teach the athlete physical anatomy and how to control and maximize breathing when engaged in exercise. The team must include the treating physicians so that treatment and medication regimes can be adjusted as the athlete progresses through recovery. Asthma medications should be withdrawn at appropriate rates (per the treating physician) if the athlete does not have coexisting asthma but has been prescribed and is using asthma medications.
CONCLUSIONS
Athletes who do not respond to traditional treatment strategies for exercise-related asthma should be further evaluated to determine the underlying cause. The certified athletic trainer may be in the best position to identify these athletes and, therefore, initiate a referral to appropriate specialists (pulmonologist, otolaryngologist, speech-language pathologist). Paradoxical vocal-cord dysfunction is best addressed with a multidisciplinary team approach to differentially diagnose the presence or absence of organic causes of dyspnea. A complete examination with full visualization of the larynx is central to proper diagnosis and subsequent treatment of PVCD. Although it is recognized that other conditions (EIA, reflux, psychological dysfunction, etc) may be concomitant, PVCD is a separate entity that must be specifically addressed. Prompt recognition of PVCD and initiation of diaphragmatic breathing exercises in a stepwise fashion should allow a reduction or complete elimination of symptoms and attacks.
REFERENCES
- Christopher K L, Wood R P, II, Eckert R C, Blager F B, Raney R A, Souhrada J F. Vocal cord dysfunction presenting as asthma. New Engl J Med. 1983;308:1566–1570. doi: 10.1056/NEJM198306303082605. [DOI] [PubMed] [Google Scholar]
- Lakin R C, Metzger W J, Haughey B H. Upper airway obstruction presenting as exercise-induced asthma. Chest. 1984;86:499–501. doi: 10.1378/chest.86.3.499. [DOI] [PubMed] [Google Scholar]
- McFadden E R, Jr, Zawadski D K. Vocal cord dysfunction masquerading as exercise-induced asthma: a physiologic cause for “choking” during athletic activities. Am J Respir Crit Care Med. 1996;153:942–947. doi: 10.1164/ajrccm.153.3.8630577. [DOI] [PubMed] [Google Scholar]
- Martin R J, Blager F B, Gay M L, Wood R B. Paradoxic vocal cord motion in presumed asthmatics. Semin Resp Med. 1987;8:332–337. [Google Scholar]
- Rupp N T. Diagnosis and management of exercise-induced asthma. Physician Sportsmed. 1996;24(1):77–87. doi: 10.3810/psm.1996.01.1213. [DOI] [PubMed] [Google Scholar]
- Brugman S M, Simons S M. Vocal cord dysfunction: don't mistake it for asthma. Physician Sportsmed. 1998;26(5):63–64,66,68–74,85. doi: 10.3810/psm.1998.05.1013. [DOI] [PubMed] [Google Scholar]
- Brugman S, Newman K. Vocal cord dysfunction. Med Sci Update. 1993;11:1–5. [Google Scholar]
- Altman K W, Mirza N, Ruiz C, Sataloff R T. Paradoxical vocal cord motion: presentation and treatment options. J Voice. 2000;14:99–103. doi: 10.1016/s0892-1997(00)80099-5. [DOI] [PubMed] [Google Scholar]
- Powell D M, Karanfilov B I, Beechler K B, Treole K, Trudeau M D, Forrest L A. Paradoxical vocal cord dysfunction in juveniles. Arch Otolaryngol Head Neck Surg. 2000;126:29–34. doi: 10.1001/archotol.126.1.29. [DOI] [PubMed] [Google Scholar]
- Koufman J A. The differential diagnosis of paradoxical vocal cord movement. [Center for Voice Disorders of Wake Forest University Web site] Available at: www.bgsm.edu/voice. Accessed April 1 2001.
- Johnson A, Jacobson B. Medical Speech-Language Pathology: A Practitioner's Guide. Thieme; New York, NY: 1998. pp. 550–555. [Google Scholar]
- Maceri D R, Zim S. Laryngospasm: an atypical manifestation of severe gastroesophageal reflux disease. Laryngoscope. 2001;111(11 Pt 1):1976–1979. doi: 10.1097/00005537-200111000-00020. [DOI] [PubMed] [Google Scholar]
- Chan R W, Tayama N. Effect of hydration on the dynamic properties of vocal cord tissues. J Acoustical Soc Am. 2001;109:2413–2414. [Google Scholar]
- England D J, Bartlett D., Jr Changes in respiratory movements of the human vocal cords during hyperpnea. J Appl Physiol. 1982;52:780–785. doi: 10.1152/jappl.1982.52.3.780. [DOI] [PubMed] [Google Scholar]
- Hurbis C, Schild J. Laryngeal changes during exercise and exercise-induced asthma. Ann Otol Rhinol Laryngol. 1991;100:34–37. doi: 10.1177/000348949110000106. [DOI] [PubMed] [Google Scholar]
- Sullivan M D, Heywood B M, Beukelman D R. A treatment for vocal cord dysfunction in female athletes: an outcome study. Laryngoscope. 2001;111:1751–1755. doi: 10.1097/00005537-200110000-00016. [DOI] [PubMed] [Google Scholar]


