Abstract
Objective: To present recommendations for the prevention, recognition, and treatment of exertional heat illnesses and to describe the relevant physiology of thermoregulation.
Background: Certified athletic trainers evaluate and treat heat-related injuries during athletic activity in “safe” and high-risk environments. While the recognition of heat illness has improved, the subtle signs and symptoms associated with heat illness are often overlooked, resulting in more serious problems for affected athletes. The recommendations presented here provide athletic trainers and allied health providers with an integrated scientific and practical approach to the prevention, recognition, and treatment of heat illnesses. These recommendations can be modified based on the environmental conditions of the site, the specific sport, and individual considerations to maximize safety and performance.
Recommendations: Certified athletic trainers and other allied health providers should use these recommendations to establish on-site emergency plans for their venues and athletes. The primary goal of athlete safety is addressed through the prevention and recognition of heat-related illnesses and a well-developed plan to evaluate and treat affected athletes. Even with a heat-illness prevention plan that includes medical screening, acclimatization, conditioning, environmental monitoring, and suitable practice adjustments, heat illness can and does occur. Athletic trainers and other allied health providers must be prepared to respond in an expedient manner to alleviate symptoms and minimize morbidity and mortality.
Keywords: heat cramps, heat syncope, heat exhaustion, heat stroke, hyponatremia, dehydration, exercise, heat tolerance
Heat illness is inherent to physical activity and its incidence increases with rising ambient temperature and relative humidity. Athletes who begin training in the late summer (eg, football, soccer, and cross-country athletes) experience exertional heat-related illness more often than athletes who begin training during the winter and spring.1–5 Although the hot conditions associated with late summer provide a simple explanation for this difference, we need to understand what makes certain athletes more susceptible and how these illnesses can be prevented.
PURPOSE
This position statement provides recommendations that will enable certified athletic trainers (ATCs) and other allied health providers to (1) identify and implement preventive strategies that can reduce heat-related illnesses in sports, (2) characterize factors associated with the early detection of heat illness, (3) provide on-site first aid and emergency management of athletes with heat illnesses, (4) determine appropriate return-to-play procedures, (5) understand thermoregulation and physiologic responses to heat, and (6) recognize groups with special concerns related to heat exposure.
ORGANIZATION
This position statement is organized as follows:
Definitions of exertional heat illnesses, including exercise-associated muscle (heat) cramps, heat syncope, exercise (heat) exhaustion, exertional heat stroke, and exertional hyponatremia;
Recommendations for the prevention, recognition, and treatment of exertional heat illnesses;
Background and literature review of the diagnosis of exertional heat illnesses; risk factors; predisposing medical conditions; environmental risk factors; thermoregulation, heat acclimatization, cumulative dehydration, and cooling therapies;
Special concerns regarding exertional heat illnesses in prepubescent athletes, older athletes, and athletes with spinal-cord injuries;
Hospitalization and recovery from exertional heat stroke and resumption of activity after heat-related collapse; and
Conclusions.
DEFINITIONS OF EXERTIONAL HEAT ILLNESSES
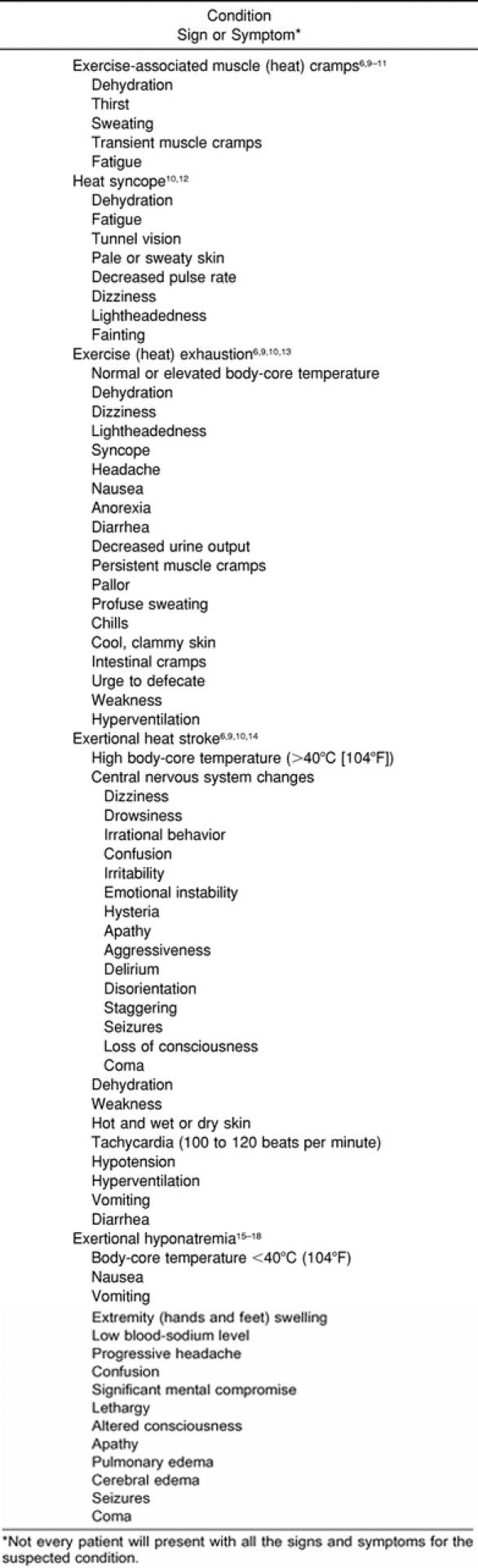
The traditional classification of heat illness defines 3 categories: heat cramps, heat exhaustion, and heat stroke.6–8 However, this classification scheme omits several other heat- and activity-related illnesses, including heat syncope and exertional hyponatremia. The signs and symptoms of the exertional heat illnesses are listed in Table 1.
Table 1. Signs and Symptoms of Exertional Heat Illnesses
Heat illness is more likely in hot, humid weather but can occur in the absence of hot and humid conditions.
Exercise-Associated Muscle (Heat) Cramps
Exercise-associated muscle (heat) cramps represent a condition that presents during or after intense exercise sessions as an acute, painful, involuntary muscle contraction. Proposed causes include fluid deficiencies (dehydration), electrolyte imbalances, neuromuscular fatigue, or any combination of these factors.6,9–11,19
Heat Syncope
Heat syncope, or orthostatic dizziness, can occur when a person is exposed to high environmental temperatures.19 This condition is attributed to peripheral vasodilation, postural pooling of blood, diminished venous return, dehydration, reduction in cardiac output, and cerebral ischemia.10,19 Heat syncope usually occurs during the first 5 days of acclimatization, before the blood volume expands,12 or in persons with heart disease or those taking diuretics.10 It often occurs after standing for long periods of time, immediately after cessation of activity, or after rapid assumption of upright posture after resting or being seated.
Exercise (Heat) Exhaustion
Exercise (heat) exhaustion is the inability to continue exercise associated with any combination of heavy sweating, dehydration, sodium loss, and energy depletion. It occurs most frequently in hot, humid conditions. At its worst, it is difficult to distinguish from exertional heat stroke without measuring rectal temperature. Other signs and symptoms include pallor, persistent muscular cramps, urge to defecate, weakness, fainting, dizziness, headache, hyperventilation, nausea, anorexia, diarrhea, decreased urine output, and a body-core temperature that generally ranges between 36°C (97°F) and 40°C (104°F).6,9,10,13,19
Exertional Heat Stroke
Exertional heat stroke is an elevated core temperature (usually >40°C [104°F]) associated with signs of organ system failure due to hyperthermia. The central nervous system neurologic changes are often the first marker of exertional heat stroke. Exertional heat stroke occurs when the temperature regulation system is overwhelmed due to excessive endogenous heat production or inhibited heat loss in challenging environmental conditions20 and can progress to complete thermoregulatory system failure.19,21 This condition is life threatening and can be fatal unless promptly recognized and treated. Signs and symptoms include tachycardia, hypotension, sweating (although skin may be wet or dry at the time of collapse), hyperventilation, altered mental status, vomiting, diarrhea, seizures, and coma.6,10,14 The risk of morbidity and mortality is greater the longer an athlete's body temperature remains above 41°C (106°F) and is significantly reduced if body temperature is lowered rapidly.22–24
Unlike classic heat stroke, which typically involves prolonged heat exposure in infants, elderly persons, or unhealthy, sedentary adults in whom body heat-regulation mechanisms are inefficient,25–27 exertional heat stroke occurs during physical activity.28 The pathophysiology of exertional heat stroke is due to the overheating of organ tissues that may induce malfunction of the temperature-control center in the brain, circulatory failure, or endotoxemia (or a combination of these).29,30 Severe lactic acidosis (accumulation of lactic acid in the blood), hyperkalemia (excessive potassium in the blood), acute renal failure, rhabdomyolysis (destruction of skeletal muscle that may be associated with strenuous exercise), and disseminated intravascular coagulation (a bleeding disorder characterized by diffuse blood coagulation), among other medical conditions, may result from exertional heat stroke and often cause death.25
Exertional Hyponatremia
Exertional hyponatremia is a relatively rare condition defined as a serum-sodium level less than 130 mmol/L. Low serum-sodium levels usually occur when activity exceeds 4 hours.19 Two, often-additive mechanisms are proposed: an athlete ingests water or low-solute beverages well beyond sweat losses (also known as water intoxication), or an athlete's sweat sodium losses are not adequately replaced.15–18 The low blood-sodium levels are the result of a combination of excessive fluid intake and inappropriate body water retention in the water-intoxication model and insufficient fluid intake and inadequate sodium replacement in the latter. Ultimately, the intravascular and extracellular fluid has a lower solute load than the intracellular fluids, and water flows into the cells, producing intracellular swelling that causes potentially fatal neurologic and physiologic dysfunction. Affected athletes present with a combination of disorientation, altered mental status, headache, vomiting, lethargy, and swelling of the extremities (hands and feet), pulmonary edema, cerebral edema, and seizures. Exertional hyponatremia can result in death if not treated properly. This condition can be prevented by matching fluid intake with sweat and urine losses and by rehydrating with fluids that contain sufficient sodium.31,32
RECOMMENDATIONS
The National Athletic Trainers' Association (NATA) advocates the following prevention, recognition, and treatment strategies for exertional heat illnesses. These recommendations are presented to help ATCs and other allied health providers maximize health, safety, and sport performance as they relate to these illnesses. Athletes' individual responses to physiologic stimuli and environmental conditions vary widely. These recommendations do not guarantee full protection from heat-related illness but should decrease the risk during athletic participation. These recommendations should be considered by ATCs and allied health providers who work with athletes at risk for exertional heat illnesses to improve prevention strategies and ensure proper treatment.
Prevention
Ensure that appropriate medical care is available and that rescue personnel are familiar with exertional heat illness prevention, recognition, and treatment. Table 2 provides general guidelines that should be considered.7 Ensure that ATCs and other health care providers attending practices or events are allowed to evaluate and examine any athlete who displays signs or symptoms of heat illness33,34 and have the authority to restrict the athlete from participating if heat illness is present.
Conduct a thorough, physician-supervised, preparticipation medical screening before the season starts to identify athletes predisposed to heat illness on the basis of risk factors34–36 and those who have a history of exertional heat illness.
Adapt athletes to exercise in the heat (acclimatization) gradually over 10 to 14 days. Progressively increase the intensity and duration of work in the heat with a combination of strenuous interval training and continuous exercise.6,9,14,33,37–44 Well-acclimatized athletes should train for 1 to 2 hours under the same heat conditions that will be present for their event.6,45,46 In a cooler environment, an athlete can wear additional clothing during training to induce or maintain heat acclimatization. Athletes should maintain proper hydration during the heat-acclimatization process.47
Educate athletes and coaches regarding the prevention, recognition, and treatment of heat illnesses9,33,38,39,42,48–51 and the risks associated with exercising in hot, humid environmental conditions.
Educate athletes to match fluid intake with sweat and urine losses to maintain adequate hydration.* (See the “National Athletic Trainers' Association Position Statement: Fluid Replacement in Athletes.”52) Instruct athletes to drink sodium-containing fluids to keep their urine clear to light yellow to improve hydration33,34,52–55 and to replace fluids between practices on the same day and on successive days to maintain less than 2% body-weight change. These strategies will lessen the risk of acute and chronic dehydration and decrease the risk of heat-related events.
Encourage athletes to sleep at least 6 to 8 hours at night in a cool environment,41,35,50 eat a well-balanced diet that follows the Food Guide Pyramid and United States Dietary Guidelines,56–58 and maintain proper hydration status. Athletes exercising in hot conditions (especially during twice-a-day practices) require extra sodium from the diet or rehydration beverages or both.
-
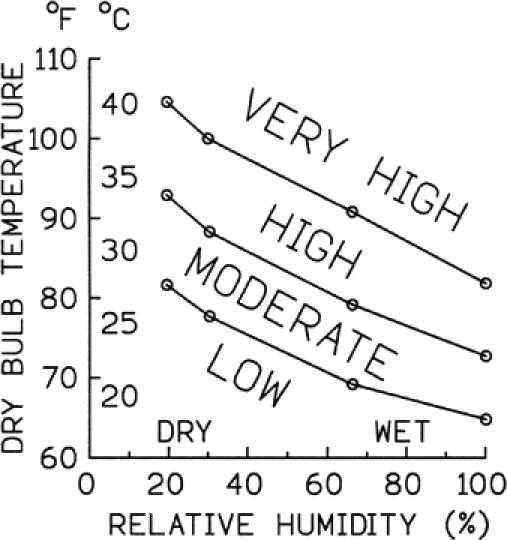
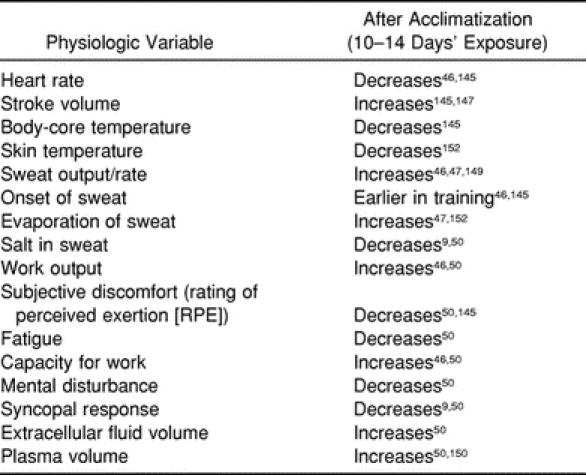
Develop event and practice guidelines for hot, humid weather that anticipate potential problems encountered based on the wet-bulb globe temperature (WBGT) (Table 3) or heat and humidity as measured by a sling psychrometer (Figure 1), the number of participants, the nature of the activity, and other predisposing risk factors.14,51 If the WBGT is greater than 28°C (82°F, or “very high” as indicated in Table 3, Figure 1), an athletic event should be delayed, rescheduled, or moved into an air-conditioned space, if possible.69–74 It is important to note that these measures are based on the risk of environmental stress for athletes wearing shorts and a T-shirt; if an athlete is wearing additional clothing (ie, football uniform, wetsuit, helmet), a lower WBGT value could result in comparable risk of environmental heat stress (Figure 2).75,76 If the event or practice is conducted in hot, humid conditions, then use extreme caution in monitoring the athletes and be proactive in taking preventive steps. In addition, be sure that emergency supplies and equipment are easily accessible and in good working order. The most important factors are to limit intensity and duration of activity, limit the amount of clothing and equipment worn, increase the number and length of rest breaks, and encourage proper hydration.
Modify activity under high-risk conditions to prevent exertional heat illnesses.19,21 Identify individuals who are susceptible to heat illnesses. In some athletes, the prodromal signs and symptoms of heat illnesses are not evident before collapse, but in many cases, adept medical supervision will allow early intervention.
Check the environmental conditions before and during the activity, and adjust the practice schedule accordingly.29,38,41,42,60 Schedule training sessions to avoid the hottest part of the day (10 AM to 5 PM) and to avoid radiant heating from direct sunlight, especially in the acclimatization during the first few days of practice sessions.9,29,33,34,38,40,50,60
Plan rest breaks to match the environmental conditions and the intensity of the activity.33,34 Exercise intensity and environmental conditions should be the major determinants in deciding the length and frequency of rest breaks. If possible, cancel or postpone the activity or move it indoors (if air conditioned) if the conditions are “extreme or hazardous” (see Table 3) or “very high” (see Figure 1) or to the right of the circled line (see Figure 2). General guidelines during intense exercise would include a work:rest ratio of 1:1, 2:1, 3:1, and 4:1 for “extreme or hazardous” (see Table 3) or “very high” (see Figure 1), “high,” “moderate,” or “low” environmental risk, respectively.41,77 For activities such as football in which equipment must be considered, please refer to Figure 2 for equipment modifications and appropriate work:rest ratios for various environmental conditions. Rest breaks should occur in the shade if possible, and hydration during rest breaks should be encouraged.
Implement rest periods at mealtime by allowing 2 to 3 hours for food, fluids, nutrients, and electrolytes (sodium and potassium) to move into the small intestine and bloodstream before the next practice.34,50,77
Provide an adequate supply of proper fluids (water or sports drinks) to maintain hydration9,34,38,40,50,60 and institute a hydration protocol that allows the maintenance of hydration status.34,49 Fluids should be readily available and served in containers that allow adequate volumes to be ingested with ease and with minimal interruption of exercise.49,52 The goal should be to lose no more than 2% to 3% of body weight during the practice session (due to sweat and urine losses).78–82 (See the “National Athletic Trainers' Association Position Statement: Fluid Replacement in Athletes.”52)
Weigh high-risk athletes (in high-risk conditions, weigh all athletes) before and after practice to estimate the amount of body water lost during practice and to ensure a return to prepractice weight before the next practice. Following exercise athletes should consume approximately 1–1.25 L (30–34 oz) of fluid for each kilogram of body water lost during exercise.†
Minimize the amount of equipment and clothing worn by the athlete in hot or humid (or both) conditions. For example, a full football uniform prevents sweat evaporation from more than 60% of the body.29,33,40,51,77 Consult Figure 2 for possible equipment and clothing recommendations. When athletes exercise in the heat, they should wear loose-fitting, absorbent, and light-colored clothing; mesh clothing and new-generation cloth blends have been specially designed to allow more effective cooling. ‡
Minimize warm-up time when feasible, and conduct warm-up sessions in the shade when possible to minimize the radiant heat load in “high” or “very high” or “extreme or hazardous” (see Table 3, Figure 1) conditions.77
Allow athletes to practice in shaded areas and use electric or cooling fans to circulate air whenever feasible.66
-
Include the following supplies on the field, in the locker room, and at various other stations:
- A supply of cool water or sports drinks or both to meet the participants' needs (see the “National Athletic Trainers' Association Position Statement: Fluid Replacement in Athletes”52 for recommendations regarding the appropriate composition of rehydration beverages based on the length and intensity of the activity)29,34,38
Notify local hospital and emergency personnel before mass participation events to inform them of the event and the increased possibility of heat-related illnesses.41,89
-
Mandate a check of hydration status at weigh-in to ensure athletes in sports requiring weight classes (eg, wrestling, judo, rowing) are not dehydrated. Any procedures used to induce dramatic dehydration (eg, diuretics, rubber suits, exercising in a sauna) are strictly prohibited.52 Dehydrated athletes exercising at the same intensity as euhydrated athletes are at increased risk for thermoregulatory strain (see the “National Athletic Trainers' Association Position Statement: Fluid Replacement in Athletes”52).
Recognition and Treatment
-
Exercise-associated muscle (heat) cramps:
- An athlete showing signs or symptoms including dehydration, thirst, sweating, transient muscle cramps, and fatigue is likely experiencing exercise-associated muscle (heat) cramps.
- To relieve muscle spasms, the athlete should stop activity, replace lost fluids with sodium-containing fluids, and begin mild stretching with massage of the muscle spasm.
- Fluid absorption is enhanced with sports drinks that contain sodium.52,60,87 A high-sodium sports product may be added to the rehydration beverage to prevent or relieve cramping in athletes who lose large amounts of sodium in their sweat.19 A simple salted fluid consists of two 10-grain salt tablets dissolved in 1 L (34 oz) of water. Intravenous fluids may be required if nausea or vomiting limits oral fluid intake; these must be ordered by a physician.6,7,52,90,91
- A recumbent position may allow more rapid redistribution of blood flow to cramping leg muscles.
-
Heat syncope:
- If an athlete experiences a brief episode of fainting associated with dizziness, tunnel vision, pale or sweaty skin, and a decreased pulse rate but has a normal rectal temperature (for exercise, 36°C to 40°C [97°F to 104°F]), then heat syncope is most likely the cause.19
- Move the athlete to a shaded area, monitor vital signs, elevate the legs above the level of the head, and rehydrate.
-
Exercise (heat) exhaustion:
- Cognitive changes are usually minimal, but assess central nervous system function for bizarre behavior, hallucinations, altered mental status, confusion, disorientation, or coma (see Table 1) to rule out more serious conditions.
- If feasible, measure body-core temperature (rectal temperature) and assess cognitive function (see Table 1) and vital signs.19 Rectal temperature is the most accurate method possible in the field to monitor body-core temperature.34,74,75,87,88 The ATC should not rely on the oral, tympanic, or axillary temperature for athletes because these are inaccurate and ineffective measures of body-core temperature during and after exercise.75,89,92
- Remove the athlete to a cool or shaded environment if possible.
-
Exertional heat stroke:
- Measure the rectal temperature if feasible to differentiate between heat exhaustion and heat stroke. With heat stroke, rectal temperature is elevated (generally higher than 40°C [104°F]).19
- Assess cognitive function, which is markedly altered in exertional heat stroke (see Table 1).
- Lower the body-core temperature as quickly as possible.34,70,77 The fastest way to decrease body temperature is to remove clothes and equipment and immerse the body (trunk and extremities) into a pool or tub of cold water (approximately 1°C to 15°C [35°F to 59°F]).32,91,92,97–99 Aggressive cooling is the most critical factor in the treatment of exertional heat stroke. Circulation of the tub water may enhance cooling.
- If a physician is present to manage the athlete's medical care on site, then initial transportation to a medical facility may not be necessary so immersion can continue uninterrupted. If a physician is not present, aggressive first-aid cooling should be initiated on site and continued during emergency medical system transport and at the hospital until the athlete is normothermic.
- Activate the emergency medical system.
- During transport and when immersion is not feasible, other methods can be used to reduce body temperature: removing the clothing; sponging down the athlete with cool water and applying cold towels; applying ice bags to as much of the body as possible, especially the major vessels in the armpit, groin, and neck; providing shade; and fanning the body with air.39,95
- In addition to cooling therapies, first-aid emergency procedures for heat stroke may include airway management. Also a physician may decide to begin intravenous fluid replacement.87
- Monitor for organ-system complications for at least 24 hours.
-
Exertional hyponatremia:
- Attempt to differentiate between hyponatremia and heat exhaustion. Hyponatremia is characterized by increasing headache, significant mental compromise, altered consciousness, seizures, lethargy, and swelling in the extremities. The athlete may be dehydrated, normally hydrated, or overhydrated.19
- Attempt to differentiate between hyponatremia and heat stroke. In hyponatremia, hyperthermia is likely to be less (rectal temperature less than 40°C [104°F]).19 The plasma-sodium level is less than 130 mEq/L and can be measured with a sodium analyzer on site if the device is available.
- If hyponatremia is suspected, immediate transfer to an emergency medical center via the emergency medical system is indicated. An intravenous line should be placed to administer medication as needed to increase sodium levels, induce diuresis, and control seizures.
- An athlete with suspected hyponatremia should not be administered fluids until a physician is consulted.
Return to activity
Table 2. Prevention Checklist for the Certified Athletic Trainer*
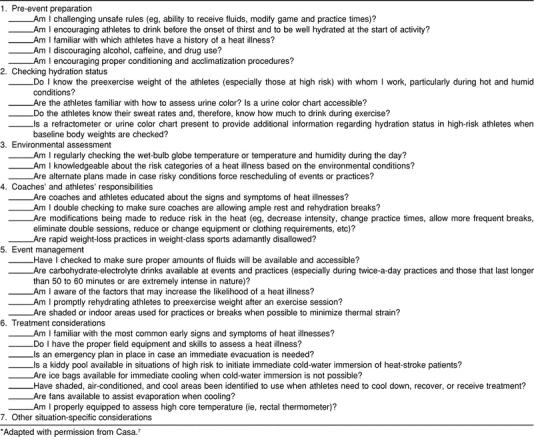
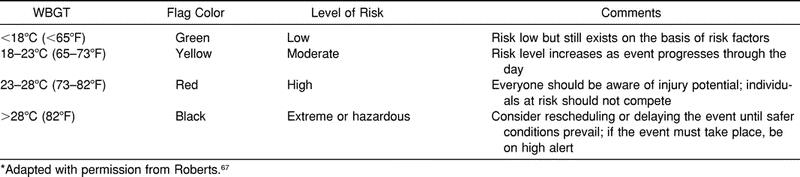
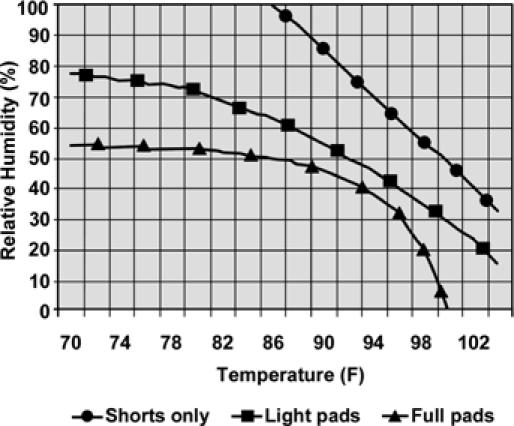
Figure 1.
Risk of heat exhaustion or heat stroke while racing in hot environments. However, Figure 2 may be better suited for estimating heat-stroke risk when equipment is worn. Reprinted with permission from Convertino VA, Armstrong LE, Coyle EF, et al. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 1996;28:i–vii.31
Figure 2.
Heat stress risk temperature and humidity graph. Heat-stroke risk rises with increasing heat and relative humidity. Fluid breaks should be scheduled for all practices and scheduled more frequently as the heat stress rises. Add 5° to temperature between 10 AM and 4 PM from mid May to mid September on bright, sunny days. Practices should be modified for the safety of the athletes to reflect the heat-stress conditions. Regular practices with full practice gear can be conducted for conditions that plot to the left of the triangles. Cancel all practices when the temperature and relative humidity plot is to the right of the circles; practices may be moved into air-conditioned spaces or held as walk-through sessions with no conditioning activities.
Conditions that plot between squares and circles: increase rest-to-work ratio with 5- to 10-minute rest and fluid breaks every 15 to 20 minutes; practice should be in shorts only with all protective equipment removed.
Conditions that plot between triangles and squares: increase rest-to-work ratio with 5- to 10-minute rest and fluid breaks every 20 to 30 minutes; practice should be in shorts with helmets and shoulder pads (not full equipment).
Adapted with permission from Kulka J, Kenney WL. Heat balance limits in football uniforms: how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30(7):29–39.68
In cases of exercise-associated muscle (heat) cramps or heat syncope, the ATC should discuss the athlete's case with the supervising physician. The cases of athletes with heat exhaustion who were not transferred to the physician's care should also be discussed with the physician. After exertional heat stroke or exertional hyponatremia, the athlete must be cleared by a physician before returning to athletic participation.92 The return to full activity should be gradual and monitored.8,87
BACKGROUND AND LITERATURE REVIEW
Diagnosis
To differentiate heat illnesses in athletes, ATCs and other on-site health care providers must be familiar with the signs and symptoms of each condition (see Table 1). Other medical conditions (eg, asthma, status epilepticus, drug toxicities) may also present with similar signs and symptoms. It is important to realize, however, that an athlete with a heat illness will not exhibit all the signs and symptoms of a specific condition, increasing the need for diligent observation during athletic activity.
Nonenvironmental Risk Factors
Athletic trainers and other health care providers should be sensitive to the following nonenvironmental risk factors, which could place athletes at risk for heat illness.
Dehydration Sweating, inadequate fluid intake, vomiting, diarrhea, certain medications,89,101–103 and alcohol104,105 or caffeine106 use can lead to fluid deficit. Body-weight change is the preferred method to monitor for dehydration in the field, but a clinical refractometer is another accurate method (specific gravity should be no more than 1.020).34,49,107–110 Dehydration can also be identified by monitoring urine color or body-weight changes before, during, and after a practice or an event and across successive days.53,54
The signs and symptoms of dehydration are thirst, general discomfort, flushed skin, weariness, cramps, apathy, dizziness, headache, vomiting, nausea, heat sensations on the head or neck, chills, decreased performance, and dyspnea.52 Water loss that is not regained by the next practice increases the risk for heat illness.110
Barriers to Evaporation Athletic equipment and rubber or plastic suits used for “weight loss” do not allow water vapor to pass through and inhibit evaporative, convective, and radiant heat loss.111,112 Participants who wear equipment that does not allow for heat dissipation are at an increased risk for heat illness.113 Helmets are also limiting because a significant amount of heat is dissipated through the head.
Illness Athletes who are currently or were recently ill may be at an increased risk for heat illness because of fever or dehydration.114–116
History of Heat Illness Some individuals with a history of heat illness are at greater risk for recurrent heat illness.8,117
Increased Body Mass Index (Thick Fat Layer or Small Surface Area) Obese individuals are at an increased risk for heat illness because the fat layer decreases heat loss.118 Obese persons are less efficient and have a greater metabolic heat production during exercise. Conversely, muscle-bound individuals have increased metabolic heat production and a lower ratio of surface area to mass, contributing to a decreased ability to dissipate heat.119–121
Wet-Bulb Globe Temperature on Previous Day and Night When the WBGT is high to extreme (see Table 3), the risk of heat-related problems is greater the next day; this appears to be one of the best predictors of heat illness.121 Athletes who sleep in cool or air-conditioned quarters are at less risk.
Poor Physical Condition Individuals who are untrained are more susceptible to heat illness than are trained athletes. As the ![]() O2max of an individual improves, the ability to withstand heat stress improves independent of acclimatization and heat adaptation.122 High-intensity work can easily produce 1000 kcal/h and elevate the core temperature of at-risk individuals (those who are unfit, overweight, or unacclimatized) to dangerous levels within 20 to 30 minutes.123
O2max of an individual improves, the ability to withstand heat stress improves independent of acclimatization and heat adaptation.122 High-intensity work can easily produce 1000 kcal/h and elevate the core temperature of at-risk individuals (those who are unfit, overweight, or unacclimatized) to dangerous levels within 20 to 30 minutes.123
Excessive or Dark-Colored Clothing or Equipment Excessive clothing or equipment decreases the ability to thermoregulate, and dark-colored clothing or equipment may cause a greater absorption of heat from the environment. Both should be avoided.113
Overzealousness Overzealous athletes are at a higher risk for heat illness because they override the normal behavioral adaptations to heat and decrease the likelihood of subtle cues being recognized.
Lack of Acclimatization to Heat An athlete with no or minimal physiologic acclimatization to hot conditions is at an increased risk of heat-related illness.8,37,83,124
Medications and Drugs Athletes who take certain medications or drugs, particularly medications with a dehydrating effect, are at an increased risk for a heat illness.101–106,125–136 Alcohol, caffeine, and theophylline at certain doses are mild diuretics.106,137,138 Caffeine is found in coffee, tea, soft drinks, chocolate, and several over-the-counter and prescription medications.139 Theophylline is found mostly in tea and anti-asthma medications.140
Electrolyte Imbalance Electrolyte imbalances do not usually occur in trained, acclimatized individuals who engage in physical activity and eat a normal diet.141 Most sodium and chloride losses in athletes occur through the urine, but athletes who sweat heavily, are salty sweaters, or are not heat acclimatized can lose significant amounts of sodium during activity.142 Electrolyte imbalances often contribute to heat illness in older athletes who use diuretics.143,144
Predisposing Medical Conditions
The following predisposing medical conditions add to the risk of heat illness.
Malignant Hyperthermia Malignant hyperthermia is caused by an autosomal dominant trait that causes muscle rigidity, resulting in elevation of body temperature due to the accelerated metabolic rate in the skeletal muscle.145–147
Neuroleptic Malignant Syndrome Neuroleptic malignant syndrome is associated with the use of neuroleptic agents and antipsychotic drugs and an unexpected idiopathic increase in core temperature during exercise.148–151
Arteriosclerotic Vascular Disease Arteriosclerotic vascular disease compromises cardiac output and blood flow through the vascular system by thickening the arterial walls.115,152
Scleroderma Scleroderma is a skin disorder that decreases sweat production, thereby decreasing heat transfer.149,153
Cystic Fibrosis Cystic fibrosis causes increased salt loss in sweat and can increase the risk for hyponatremia.154,155
Sickle Cell Trait Sickle cell trait limits blood-flow distribution and decreases oxygen-carrying capacity. The condition is exacerbated by exercise at higher altitudes.156,157
Environmental Risk Factors
When the environmental temperature is above skin temperature, athletes begin to absorb heat from the environment and depend entirely on evaporation for heat loss.113,158,159 High relative humidity inhibits heat loss from the body through evaporation.61
The environmental factors that influence the risk of heat illness include the ambient air temperature, relative humidity (amount of water vapor in the air), air motion, and the amount of radiant heat from the sun or other sources.2,9,41 The relative risk of heat illness can be calculated using the WBGT equation.2,43,50,69,77,160,161 Using the WBGT index to modify activity in high-risk settings has virtually eliminated heat-stroke deaths in United States Marine Corps recruits.159 Wet-bulb globe temperature is calculated using the wet-bulb (wb), dry-bulb (db), and black-globe (bg) temperature with the following equation49,62,85,162,163:
When there is no radiant heat load, Tdb = Tbg, and the equation is reduced62 to
This equation is used to estimate risk as outlined in Table 3.13,40,50,61,85 This index was determined for athletes wearing a T-shirt and light pants.158 The WBGT calculation can be performed using information obtained from electronic devices42 or the local meteorologic service, but conversion tables for relative humidity and Tdb are needed to calculate the wet-bulb temperature.50,162 The predictive value from the meteorologic service is not as accurate as site-specific data for representing local heat load but will suffice in most situations. When WBGT measures are not possible, environmental heat stress can be estimated using a sling psychrometer (see Figures 1, 2).
Several recommendations have been published for distance running, but these can also be applied to other continuous activity sports. The Canadian Track and Field Association recommended that a distance race should be cancelled if the WBGT is greater than 26.7°C (80°F).39 The American College of Sports Medicine guidelines from 1996 recommended that a race should be delayed or rescheduled when the WBGT is greater than 27.8°C (82°F).31,72,73 In some instances, the event will go on regardless of the WBGT; ATCs should then have an increased level of suspicion for heat stroke and focus on hydration, emergency supplies, and detection of exertional heat illnesses.
Thermoregulation
Thermoregulation is a complex interaction among the central nervous system (CNS), the cardiovascular system, and the skin to maintain a body-core temperature of 37°C.9,43,51,164 The CNS temperature-regulation center is located in the hypothalamus and is the site where the core temperature setpoint is determined.9,43,82,158,164–166 The hypothalamus receives information regarding body-core and shell temperatures from peripheral skin receptors and the circulating blood; body-core temperature is regulated through an open-ended feedback loop similar to that in a home thermostat system.158,165,167,168 Body responses for heat regulation include cutaneous vasodilation, increased sweating, increased heart rate, and increased respiratory rate.38,43,51,164,165
Body-core temperature is determined by metabolic heat production and the transfer of body heat to and from the surrounding environment using the following heat-production and heat-storage equation166,167:
where S is the amount of stored heat, M is the metabolic heat production, R is the heat gained or lost by radiation, K is the conductive heat lost or gained, Cv is the convective heat lost or gained, and E is the evaporative heat lost.
Basal metabolic heat production fasting and at absolute rest is approximately 60 to 70 kcal/h for an average adult, with 50% of the heat produced by the internal organs. Metabolic heat produced by intense exercise may approach 1000 kcal/h,51,164 with greater than 90% of the heat resulting from muscle metabolism.9,40,42,166
Heat is gained or lost from the body by one or more of the following mechanisms9,85:
Radiation The energy is transferred to or from an object or body via electromagnetic radiation from higher to lower energy surfaces.9,43,51,85,166
Conduction Heat transfers from warmer to cooler objects through direct physical contact.9,43,51,85,166 Ice packs and cold-water baths are examples of conductive heat exchange.
Convection Heat transfers to or from the body to surrounding moving fluid (including air).9,43,51,85,166 Moving air from a fan, cycling, or windy day produces convective heat exchange.
Evaporation Heat transfers via the vaporization of sweat § and is the most efficient means of heat loss.51,158,169 The evaporation of sweat from the skin depends on the water saturation of the air and the velocity of the moving air.170–172 The effectiveness of this evaporation for heat loss from the body diminishes rapidly when the relative humidity is greater than 60%.9,20,164
Cognitive performance and associated CNS functions deteriorate when brain temperature rises. Signs and symptoms include dizziness, confusion, behavior changes, coordination difficulties, decreased physical performance, and collapse due to hyperthermia.168,173 The residual effects of elevated brain temperature depend on the duration of the hyperthermia. Heat stroke rarely leads to permanent neurologic deficits51; however, some sporadic symptoms of frontal headache and sleep disturbances have been noted for up to 4 months.168,174,175 When permanent CNS damage occurs, it is associated with cerebellar changes, including ataxia, marked dysarthria, and dysmetria.174
Heat Acclimatization
Heat acclimatization is the physiologic response produced by repeated exposures to hot environments in which the capacity to withstand heat stress is improved.14,43,75,176,177 Physiologic responses to heat stress are summarized in Table 4. Exercise heat exposure produces progressive changes in thermoregulation that involve sweating, skin circulation, thermoregulatory setpoint, cardiovascular alterations, and endocrine adjustments.29,43,178 Individual differences affect the onset and decay of acclimatization.29,45,179 The rate of acclimatization is related to aerobic conditioning and fitness; more conditioned athletes acclimatize more quickly.43,45,180 The acclimatization process begins with heat exposure and is reasonably protective after 7 to 14 days, but maximum acclimatization may take 2 to 3 months.45,181,182 Heat acclimatization diminishes by day 6 when heat stress is no longer present.180,183 Fluid replacement improves the induction and effect of heat acclimatization.184–187 Extra salt in the diet during the first few days of heat exposure also improves acclimatization; this can be accomplished by encouraging the athlete to eat salty foods and to use the salt shaker liberally during meals.
Table 4. Physiologic Responses After Heat Acclimatization Relative to Nonacclimatized State
Cumulative Dehydration
Cumulative dehydration develops insidiously over several days and is typically observed during the first few days of a season during practice sessions or in tournament competition. Cumulative dehydration can be detected by monitoring daily prepractice and postpractice weights. Even though a small decrease in body weight (less than 1%) may not have a detrimental effect on the individual, the cumulative effect of a 1% fluid loss per day occurring over several days will create an increased risk for heat illness and a decrease in performance.110
During intense exercise in the heat, sweat rates can be 1 to 2.5 L/h (about 1 to 2.25 kilograms [2 to 5 pounds] of body weight per hour) or more, resulting in dehydration. Unfortunately, the volume of fluid that most athletes drink voluntarily during exercise replaces only about 50% of body-fluid losses.188 Ideally, rehydration involves drinking at a rate sufficient to replace all of the water lost through sweating and urination.60,77 If the athlete is not able to drink at this rate, he or she should drink the maximum tolerated. Use caution to ensure that athletes do not overhydrate and put themselves at risk for the development of hyponatremia. However, hydration before an event is essential to help decrease the incidence of heat illnesses. For more information on this topic, see the “National Athletic Trainers' Association Position Statement: Fluid Replacement in Athletes.”52
Cooling Therapies
The fastest way to decrease body-core temperature is immersion of the trunk and extremities into a pool or tub filled with cold water (between 1°C [35°F] and 15°C [59°F]).39,88,91,97 Conditions that have been associated with immersion therapy include shivering and peripheral vasoconstriction; however, the potential for these should not deter the medical staff from using immersion therapy for rapid cooling. Shivering can be prevented if the athlete is removed from the water once rectal temperature reaches 38.3°C to 38.9°C (101°F to 102°F). Peripheral vasoconstriction may occur, but the powerful cooling potential of immersion outweighs any potential concerns. Cardiogenic shock has also been a proposed consequence of immersion therapy, but this connection has not been proven in cooling heat-stroke patients.39 Cold-water immersion therapy was associated with a zero percent fatality rate in 252 cases of exertional heat stroke in the military.89 Other forms of cooling (water spray; ice packs covering the body; ice packs on axillae, groin, and neck; or blowing air) decrease body-core temperature at a slower rate compared with cold-water immersion.97 If immersion cooling is not being used, cooling with ice bags should be directed to as much of the body as possible, especially the major vessels in the armpit, groin, and neck regions (and likely the hands and feet), and cold towels may be applied to the head and trunk because these areas have been demonstrated on thermography173,189 to have the most rapid heat loss.
SPECIAL CONCERNS
Most research related to heat illness has been performed on normal, healthy adults. Child athletes, older athletes, and athletes with spinal-cord injuries have been studied less frequently. The following are suggestions for special populations or those with special conditions.
Children (Prepubescents)
Exercise in hot environments and heat tolerance are affected by many physiologic factors in children. These include decreased sweat gland activity,190 higher skin temperatures,191–193 decreased cardiac output (increased heart rate and lower stroke volume) due to increased peripheral circulation,194 decreased exercise economy,195 decreased ability to acclimatize to heat (slower and takes longer),192 smaller body size (issues related to body surface-to-mass ratio), maturational differences,190 and predisposing conditions (obesity, hypohydration, childhood illnesses, and other disease states).190,192,196
Decrease the intensity of activities that last longer than 30 minutes,197 and have the athlete take brief rests50 if the WBGT is between 22.8°C and 27.8°C (73°F and 82°F); cancel or modify the activity if the WBGT is greater than 27.8°C (82°F).31,69–73 Modification could involve longer and more frequent rest breaks than are usually permitted within the rules of the sport (eg, insert a rest break before halftime).
Encourage children to ingest some fluids at least every 15 to 30 minutes during activity to maintain hydration, even if they are not thirsty.197
Use similar precautions as listed earlier for adults.
Older Athletes (>50 Years Old)
The ability of the older athlete to adapt is partly a function of age and also depends on functional capacity and physiologic health status.198–206
The athlete should be evaluated by a physician before exercise, with the potential consequences of predisposing medical conditions and illnesses addressed.9,34–36 An increase has been shown in the exercise heart rate of 1 beat per minute for each 1°C (1.8°F) increase in ambient temperature above neutral (23.9°C [75°F]).207 Athletes with known or suspected heart disease should curtail activities at lower temperatures than healthy athletes and should have cardiovascular stress testing before participating in hot environments.
Older athletes have a decreased ability to maintain an adequate plasma volume and osmolality during exercise,198,208 which may predispose them to dehydration. Regular fluid intake is critical to avoid hyperthermia.
Athletes with Spinal-Cord Injuries
As sport participation for athletes with spinal-cord injuries increases from beginner to elite levels, understanding the disability,209,210 training methods, and causes of heat injury will help make competition safer.211 For example, the abilities to regulate heart rate, circulate the blood volume, produce sweat, and transfer heat to the surface vary with the level and severity of the spinal-cord lesion.208,212–218
Monitor these athletes closely for heat-related problems. One technique for determining hyperthermia is to feel the skin under the arms of the distressed athlete.211 Rectal temperature may not be as accurate for measuring core temperature as in other athletes due to decreased ability to regulate blood flow beneath the spinal-cord lesion.218–220
If the athlete is hyperthermic, provide more water, lighter clothing, or cooling of the trunk,211,213 legs,211 and head.213
HOSPITALIZATION AND RECOVERY
After an episode of heat stroke, the athlete may experience impaired thermoregulation, persistent CNS dysfunction,221,222 hepatic insufficiency, and renal insufficiency.39,223 For persons with exertional heat stroke and associated multisystem tissue damage, the rate of recovery is highly individualized, ranging up to more than 1 year.8,86,221 In one study, 9 of 10 patients exhibited normal heat-acclimatization responses, thermoregulation, whole-body sodium and potassium balance, sweat-gland function, and blood values about 2 months after the heat stroke.8 Transient or persistent heat intolerance was found in a small percentage of patients.83 For some athletes, a history of exertional heat stroke increases the chance of experiencing subsequent episodes.39
An athlete who experiences heat stroke may have compromised heat tolerance and heat acclimatization after physician clearance.35,224,225 Decreased heat tolerance may affect 15% to 20% of persons after a heat stroke-related collapse,226,227 and in a few individuals, decreased heat tolerance has persisted up to 5 years.35,224,228 Additional heat stress may reduce the athlete's ability to train and compete due to impaired cardiovascular and thermoregulatory responses.115,228–230
After recovery from an episode of heat stroke or hyponatremia, an athlete's physical activity should be restricted8,86 and the gradual return to sport individualized by his or her physician. The athlete should be monitored on a daily basis by the ATC during exercise.86 During the return-to-exercise phase, an athlete may experience some detraining and deconditioning not directly related to the heat exposure.8,86 Evaluate the athlete over time to determine whether there has been a complete recovery of exercise and heat tolerance.8,86
CONCLUSIONS
Athletic trainers and other allied health providers must be able to differentiate exercise-associated muscle (heat) cramps, heat syncope, exercise (heat) exhaustion, exertional heat stroke, and exertional hyponatremia in athletes.
This position statement outlines the NATA's current recommendations to reduce the incidence, improve the recognition, and optimize treatment of heat illness in athletes. Education and increased awareness will help to reduce both the frequency and the severity of heat illness in athletes.
Acknowledgments
ACKNOWLEDGMENTS
This pronouncement was reviewed for the NATA by the Pronouncements Committee, Edward R. Eichner, MD, FACSM, and William O. Roberts, MD, MS, FACSM. T. Kyle Eubanks, MA, ATC, and Paul C. Miller, PhD, provided assistance in the preparation of the manuscript.
Footnotes
REFERENCES
- Hawley D A, Slentz K, Clark M A, Pless J E, Waller B F. Athletic fatalities. Am J Forensic Med Pathol. 1990;11:124–129. doi: 10.1097/00000433-199006000-00005. [DOI] [PubMed] [Google Scholar]
- Mueller F O, Schindler R D. Annual survey of football injury research 1931–1984. Athl Train J Natl Athl Train Assoc. 1985;20:213–218. [Google Scholar]
- Bijur P E, Trumble A, Harel Y, Overpeck M D, Jones D, Scheidt P C. Sports and recreation injuries in US children and adolescents. Arch Pediatr Adolesc Med. 1995;149:1009–1016. doi: 10.1001/archpedi.1995.02170220075010. [DOI] [PubMed] [Google Scholar]
- Tucker A M. Common soccer injuries: diagnosis, treatment and rehabilitation. Sports Med. 1997;23:21–32. doi: 10.2165/00007256-199723010-00003. [DOI] [PubMed] [Google Scholar]
- Martin D E. Influence of elevated climatic heat stress on athletic competition in Atlanta, 1996. New Stud Athl. 1997;12:65–78. [Google Scholar]
- Rich B. Environmental concerns: heat. In: Sallis E R, Massimino F, editors. Essentials of Sports Medicine. Mosby Year Book; St Louis, MO: 1997. pp. 129–133. [Google Scholar]
- Casa D J. Exercise in the heat, II: critical concepts in rehydration, exertional heat illnesses, and maximizing athletic performance. J Athl Train. 1999;34:253–262. [PMC free article] [PubMed] [Google Scholar]
- Armstrong L E, De Luca J P, Hubbard R W. Time course of recovery and heat acclimation ability of prior exertional heatstroke patients. Med Sci Sports Exerc. 1990;22:36–48. [PubMed] [Google Scholar]
- Brewster S J, O'Connor F G, Lillegard W A. Exercise-induced heat injury: diagnosis and management. Sports Med Arthrosc Rev. 1995;3:206–266. doi: 10.1097/00132585-199500340-00002. [DOI] [PubMed] [Google Scholar]
- Knochel J P. Environmental heat illness: an eclectic review. Arch Intern Med. 1974;133:841–864. [PubMed] [Google Scholar]
- Bergeron M F. Heat cramps during tennis: a case report. Int J Sport Nutr. 1996;6:62–68. doi: 10.1123/ijsn.6.1.62. [DOI] [PubMed] [Google Scholar]
- Hubbard R, Gaffin S, Squire D. Heat-related illness. In: Auerbach P S, editor. Wilderness Medicine. 3rd ed. Mosby Year Book; St Louis, MO: 1995. pp. 167–212. [Google Scholar]
- Armstrong L E, Hubbard R W, Kraemer W J, DeLuca J P, Christensen E L. Signs and symptoms of heat exhaustion during strenuous exercise. Ann Sports Med. 1987;3:182–189. [Google Scholar]
- Epstein Y. Exertional heatstroke: lessons we tend to forget. Am J Med Sports. 2000;2:143–152. [Google Scholar]
- Epstein Y, Armstrong L E. Fluid-electrolyte balance during labor and exercise: concepts and misconceptions. Int J Sport Nutr. 1999;9:1–12. doi: 10.1123/ijsn.9.1.1. [DOI] [PubMed] [Google Scholar]
- Maughan R J. Optimizing hydration for competitive sport. In: Lamb D R, Murray R, editors. Optimizing Sport Performance. Cooper Publishing; Carmel, IN: 1997. pp. 139–183. [Google Scholar]
- Armstrong L E, Curtis W C, Hubbard R W, Francesconi R P, Moore R, Askew W. Symptomatic hyponatremia during prolonged exercise in the heat. Med Sci Sports Exerc. 1993;25:543–549. [PubMed] [Google Scholar]
- Garigan T, Ristedt D E. Death from hyponatremia as a result of acute water intoxication in an Army basic trainee. Mil Med. 1999;164:234–238. [PubMed] [Google Scholar]
- Casa D J, Roberts W O. Considerations for the medical staff in preventing, identifying and treating exertional heat illnesses. In: Armstrong L E, editor. Exertional Heat Illnesses. Human Kinetics; Champaign, IL: 2003. (in press) [Google Scholar]
- Cabanac M, White M D. Core temperature thresholds of hyperpnea during passive hyperthermia in humans. Eur J Appl Physiol Occup Physiol. 1995;71:71–76. doi: 10.1007/BF00511235. [DOI] [PubMed] [Google Scholar]
- Casa D J, Armstrong L E. Heatstroke: a medical emergency. In: Armstrong L E, editor. Exertional Heat Illnesses. Human Kinetics; Champaign, IL: 2003. (in press) [Google Scholar]
- Vicario S J, Okabajue R, Haltom T. Rapid cooling in classic heatstroke: effect on mortality rates. Am J Emerg Med. 1986;4:394–398. doi: 10.1016/0735-6757(86)90185-3. [DOI] [PubMed] [Google Scholar]
- Assia E, Epstein Y, Shapiro Y. Fatal heatstroke after a short march at night: a case report. Aviat Space Environ Med. 1985;56:441–442. [PubMed] [Google Scholar]
- Graham B S, Lichtenstein M J, Hinson J M, Theil G B. Nonexertional heatstroke: physiologic management and cooling in 14 patients. Arch Intern Med. 1986;146:87–90. doi: 10.1001/archinte.146.1.87. [DOI] [PubMed] [Google Scholar]
- Hart G R, Anderson R J, Crumpler C P, Shulkin A, Reed G, Knochel J P. Epidemic classical heat stroke: clinical characteristics and course of 28 patients. Medicine (Baltimore) 1982;61:189–197. [PubMed] [Google Scholar]
- Thomas C, editor. Taber's Cyclopedic Medical Dictionary. FA Davis; Philadelphia, PA: 1993. [Google Scholar]
- Akhtar M J, Al-Nozha M, al-Harthi S, Nouh M S. Electrocardiographic abnormalities in patients with heat stroke. Chest. 1993;104:411–414. doi: 10.1378/chest.104.2.411. [DOI] [PubMed] [Google Scholar]
- Partin N. Internal medicine: exertional heatstroke. Athl Train J Natl Athl Train Assoc. 1990;25:192–194. [Google Scholar]
- Knochel J. Management of heat conditions. Athl Ther Today. 1996;1:30–34. [Google Scholar]
- Hubbard R W, Armstrong L E. Hyperthermia: new thoughts on an old problem. Physician Sportsmed. 1989;17(6):97–98,101,104,107–108,111–113. doi: 10.1080/00913847.1989.11709808. [DOI] [PubMed] [Google Scholar]
- Convertino V A, Armstrong L E, Coyle E F, et al. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 1996;28:i–vii. doi: 10.1097/00005768-199610000-00045. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Casa D J, Watson G. Exertional hyponatremia: unanswered questions and etiological perspectives. Int J Sport Nutr Exerc Metab. (in press)
- Francis K, Feinstein R, Brasher J. Optimal practice times for the reduction of the risk of heat illness during fall football practice in the Southeastern United States. Athl Train J Natl Athl Train Assoc. 1991;26:76–78,80. [Google Scholar]
- Shapiro Y, Seidman D S. Field and clinical observations of exertional heat stroke patients. Med Sci Sports Exerc. 1990;22:6–14. [PubMed] [Google Scholar]
- Epstein Y, Shapiro Y, Brill S. Role of surface area-to-mass ratio and work efficiency in heat intolerance. J Appl Physiol. 1983;54:831–836. doi: 10.1152/jappl.1983.54.3.831. [DOI] [PubMed] [Google Scholar]
- Kenney W L. Physiological correlates of heat intolerance. Sports Med. 1985;2:279–286. doi: 10.2165/00007256-198502040-00005. [DOI] [PubMed] [Google Scholar]
- Mitchell D, Senay L C, Wyndham C H, van Rensburg A J, Rogers G G, Strydom N B. Acclimatization in a hot, humid environment: energy exchange, body temperature, and sweating. J Appl Physiol. 1976;40:768–778. doi: 10.1152/jappl.1976.40.5.768. [DOI] [PubMed] [Google Scholar]
- Davidson M. Heat illness in athletics. Athl Train J Natl Athl Train Assoc. 1985;20:96–101. [Google Scholar]
- Brodeur V B, Dennett S R, Griffin L S. Exertional hyperthermia, ice baths, and emergency care at the Falmouth Road Race. J Emerg Nurs. 1989;15:304–312. [PubMed] [Google Scholar]
- Allman F L., Jr The effects of heat on the athlete. J Med Assoc Ga. 1992;81:307–310. [PubMed] [Google Scholar]
- Bernard T E. Risk management for preventing heat illness in athletes. Athl Ther Today. 1996;1:19–21. [Google Scholar]
- Delaney K A. Heatstroke: underlying processes and lifesaving management. Postgrad Med. 1992;91:379–388. doi: 10.1080/00325481.1992.11701266. [DOI] [PubMed] [Google Scholar]
- Haymes E M, Wells C L. Environment and Human Performance. Human Kinetics; Champaign, IL: 1986. pp. 1–41. [Google Scholar]
- Gisolfi C, Robinson S. Relations between physical training, acclimatization, and heat tolerance. J Appl Physiol. 1969;26:530–534. doi: 10.1152/jappl.1969.26.5.530. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Maresh C M. The induction and decay of heat acclimatisation in trained athletes. Sports Med. 1991;12:302–312. doi: 10.2165/00007256-199112050-00003. [DOI] [PubMed] [Google Scholar]
- Fortney S M, Vroman N B. Exercise, performance and temperature control: temperature regulation during exercise and implications for sports performance and training. Sports Med. 1985;2:8–20. doi: 10.2165/00007256-198502010-00002. [DOI] [PubMed] [Google Scholar]
- Dawson B. Exercise training in sweat clothing in cool conditions to improve heat tolerance. Sports Med. 1994;17:233–244. doi: 10.2165/00007256-199417040-00004. [DOI] [PubMed] [Google Scholar]
- Kleiner D M, Glickman S E. Medical considerations and planning for short distance road races. J Athl Train. 1994;29:145–146,149–151. [PMC free article] [PubMed] [Google Scholar]
- Murray B. Fluid replacement: the American College of Sports Medicine position stand. Sport Sci Exch. 1996;9(4S):63. [Google Scholar]
- Elias S R, Roberts W O, Thorson D C. Team sports in hot weather: guidelines for modifying youth soccer. Physician Sportsmed. 1991;19(5):67–68,72–74,77,80. [Google Scholar]
- Knochel J P. Heat stroke and related heat stress disorders. Dis Month. 1989;35:301–377. [PubMed] [Google Scholar]
- Casa D J, Armstrong L E, Hillman S K, et al. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35:212–224. [PMC free article] [PubMed] [Google Scholar]
- Armstrong L E, Maresh C M, Castellani J W, et al. Urinary indices of hydration status. Int J Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Soto J A, Hacker F T, Jr, Casa D J, Kavouras S A, Maresh C M. Urinary indices during dehydration exercise and rehydration. Int J Sport Nutr. 1997;8:345–355. doi: 10.1123/ijsn.8.4.345. [DOI] [PubMed] [Google Scholar]
- Armstrong L E. Performing in Extreme Environments. Human Kinetics; Champaign, IL: 2000. Heat and humidity; pp. 15–70. [Google Scholar]
- Nadel E R, Fortney S M, Wenger C B. Effect of hydration state on circulatory and thermal regulations. J Appl Physiol. 1980;49:715–721. doi: 10.1152/jappl.1980.49.4.715. [DOI] [PubMed] [Google Scholar]
- Keithley J K, Keller A, Vazquez M G. Promoting good nutrition: using the food guide pyramid in clinical practice. Medsurg Nurs. 1996;5:397–403. [PubMed] [Google Scholar]
- Achterberg C, McDonnell E, Bagby R. How to put the Food Guide Pyramid into practice. J Am Diet Assoc. 1994;94:1030–1035. doi: 10.1016/0002-8223(94)92198-9. [DOI] [PubMed] [Google Scholar]
- Laywell P. Guidelines for pre-event eating. Texas Coach. 1981;25:40–41,59. [Google Scholar]
- Terrados N, Maughan R J. Exercise in the heat: strategies to minimize the adverse effects on performance. J Sports Sci. 1995;13(suppl):55–62. doi: 10.1080/02640419508732278. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Hubbard R W, Szlyk P C, Matthew W T, Sils I V. Voluntary dehydration and electrolyte losses during prolonged exercise in the heat. Aviat Space Environ Med. 1985;56:765–770. [PubMed] [Google Scholar]
- Sandor R P. Heat illness: on-site diagnosis and cooling. Physician Sportsmed. 1997;25(6):35–40. doi: 10.3810/psm.1997.06.1400. [DOI] [PubMed] [Google Scholar]
- Squire D L. Heat illness: fluid and electrolyte issues for pediatric and adolescent athletes. Pediatr Clin North Am. 1990;37:1085–1109. doi: 10.1016/s0031-3955(16)36976-0. [DOI] [PubMed] [Google Scholar]
- Murray R. Fluid needs in hot and cold environments. Int J Sports Nutr. 1995;5(suppl):62–73. doi: 10.1123/ijsn.5.s1.s62. [DOI] [PubMed] [Google Scholar]
- Gisolfi C V. Fluid balance for optimal performance. Nutr Rev. 1996;54(4 Pt 2, suppl):159–168. doi: 10.1111/j.1753-4887.1996.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Sawka M N, Coyle E F. Influence of body water and blood volume on thermoregulation and exercise performance in the heat. Exerc Sport Sci Rev. 1999;27:167–218. [PubMed] [Google Scholar]
- Roberts W O. Medical management and administration manual for long distance road racing. In: Brown C H, Gudjonsson B, editors. IAAF Medical Manual for Athletics and Road Racing Competitions: A Practical Guide. International Amateur Athletic Federation Publications; Monaco: 1998. pp. 39–75. [Google Scholar]
- Kulka T J, Kenney W L. Heat balance limits in football uniforms: how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30(7):29–39. doi: 10.3810/psm.2002.07.377. [DOI] [PubMed] [Google Scholar]
- Department of the Army . Prevention Treatment and Control of Heat Injury. Department of the Army; Washington, DC: 1980. Technical bulletin TBMED 507:1–21. [Google Scholar]
- Hughson R L, Staudt L A, Mackie J M. Monitoring road racing in the heat. Physician Sportsmed. 1983;11(5):94–102. doi: 10.1080/00913847.1986.11708538. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine ACSM position statement: prevention of thermal injuries during distance running. Med Sci Sports Exerc. 1987;19:529–533. [PubMed] [Google Scholar]
- Armstrong L E, Epstein Y, Greenleaf J E, et al. American College of Sports Medicine position stand: heat and cold illnesses during distance running. Med Sci Sports Exerc. 1996;28:i–x. [PubMed] [Google Scholar]
- Rozycki T J. Oral and rectal temperatures in runners. Physician Sportsmed. 1984;12(6):105–110. [Google Scholar]
- Knight J C, Casa D J, McClung J M, Caldwell K A, Gilmer A M, Meenan P M, Goss P J. Assessing if two tympanic temperature instruments are valid predictors of core temperature in hyperthermic runners and does drying the ear canal help [abstract] J Athl Train. 2000;35(suppl):S21. [Google Scholar]
- Shapiro Y, Pandolf K B, Goldman R F. Predicting sweat loss response to exercise, environment and clothing. Eur J Appl Physiol Occup Physiol. 1982;48:83–96. doi: 10.1007/BF00421168. [DOI] [PubMed] [Google Scholar]
- Shvartz E, Saar E, Benor D. Physique and heat tolerance in hot dry and hot humid environments. J Appl Physiol. 1973;34:799–803. doi: 10.1152/jappl.1973.34.6.799. [DOI] [PubMed] [Google Scholar]
- Murray R. Dehydration, hyperthermia, and athletes: science and practice. J Athl Train. 1996;31:248–252. [PMC free article] [PubMed] [Google Scholar]
- Pichan G, Gauttam R K, Tomar O S, Bajaj A C. Effects of primary hypohydration on physical work capacity. Int J Biometerorol. 1988;32:176–180. doi: 10.1007/BF01045276. [DOI] [PubMed] [Google Scholar]
- Walsh R M, Noakes T D, Hawley J A, Dennis S C. Impaired high-intensity cycling performance time at low levels of dehydration. Int J Sports Med. 1994;15:392–398. doi: 10.1055/s-2007-1021076. [DOI] [PubMed] [Google Scholar]
- Cheung S S, McLellan T M. Heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol. 1998;84:1731–1739. doi: 10.1152/jappl.1998.84.5.1731. [DOI] [PubMed] [Google Scholar]
- Bijlani R, Sharma K N. Effect of dehydration and a few regimes of rehydration on human performance. Indian J Physiol Pharmacol. 1980;24:255–266. [PubMed] [Google Scholar]
- Nielsen B. Solar heat load: heat balance during exercise in clothed subjects. Eur J Appl Physiol Occup Physiol. 1990;60:452–456. doi: 10.1007/BF00705036. [DOI] [PubMed] [Google Scholar]
- Maughan R J, Shirreffs S M. Preparing athletes for competition in the heat: developing an effective acclimatization strategy. Sports Sci Exchange. 1997;10:1–4. [Google Scholar]
- Lloyd E L. ABC of sports medicine: temperature and performance—II: heat. BMJ. 1994;309:587–589. doi: 10.1136/bmj.309.6954.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe D D, Shanley L A, Smith E W. Clothing and exercise, I: biophysics of heat transfer between the individual clothing and environment. Sports Med. 1994;18:38–54. doi: 10.2165/00007256-199418010-00005. [DOI] [PubMed] [Google Scholar]
- Anderson M K, Hall S J. Sports Injury Management. Williams & Wilkins; Philadelphia, PA: 1995. pp. 66–75. [Google Scholar]
- Roberts W O. Assessing core temperature in collapsed athletes: what's the best method? Physician Sportsmed. 1994;22(8):49–55. doi: 10.1080/00913847.1994.11947680. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Maresh C M, Crago A E, Adams R, Roberts R O. Interpretation of aural temperatures during exercise, hyperthermia, and cooling therapy. Med Exerc Nutr Health. 1994;3:9–16. [Google Scholar]
- Adner M M, Scarlet J J, Casey J, Robinson W, Jones B H. The Boston Marathon medical care team: ten years of experience. Physician Sportsmed. 1988;16(7):99–108. doi: 10.1080/00913847.1988.11709556. [DOI] [PubMed] [Google Scholar]
- Casa D J, Maresh C M, Armstrong L E, et al. Intravenous versus oral rehydration during a brief period: responses to subsequent exercise in the heat. Med Sci Sports Exerc. 2000;32:124–133. doi: 10.1097/00005768-200001000-00019. [DOI] [PubMed] [Google Scholar]
- Noakes T. Failure to thermoregulate. In: Sutton J, Thompson M, Torode M, editors. Exercise and Thermoregulation. Vol. 37 The University of Sydney; Sydney, Australia: 1995. [Google Scholar]
- Deschamps A, Levy R D, Coslo M G, Marliss E B, Magder S. Tympanic temperature should not be used to assess exercise-induced hyperthermia. Clin J Sport Med. 1992;2:27–32. [Google Scholar]
- Gonzalez-Alonso J, Mora-Rodriguez R, Coyle E F. Supine exercise restores arterial blood pressure and skin blood flow despite dehydration and hyperthermia. Am J Physiol. 1999;277(2 Pt 2):H576–H583. doi: 10.1152/ajpheart.1999.277.2.H576. [DOI] [PubMed] [Google Scholar]
- Germain M, Jobin M, Cabanac M. The effect of face fanning during the recovery from exercise hyperthermia. Can J Physiol Pharmacol. 1987;65:87–91. doi: 10.1139/y87-017. [DOI] [PubMed] [Google Scholar]
- Roberts W O. Exercise-associated collapse in endurance events: a classification system. Physician Sportsmed. 1989;17(5):49–55. doi: 10.1080/00913847.1989.11709782. [DOI] [PubMed] [Google Scholar]
- Matthew C B. Treatment of hyperthermia and dehydration with hypertonic saline in dextran. Shock. 1994;2:216–221. [PubMed] [Google Scholar]
- Armstrong L E, Crago A E, Adams R, Roberts W O, Maresh C M. Whole-body cooling of hyperthermic runners: comparison to two field therapies. Am J Emerg Med. 1996;14:355–358. doi: 10.1016/S0735-6757(96)90048-0. [DOI] [PubMed] [Google Scholar]
- Marino F, Booth J. Whole body cooling by immersion in water at moderate temperature. J Sci Med Sport. 1998;1:73–82. doi: 10.1016/s1440-2440(98)80015-7. [DOI] [PubMed] [Google Scholar]
- Clements J M, Casa D J, Knight J C, et al. Ice-water immersion and cold-water immersion provide similar cooling rates in runners with exercise-induced hyperthermia. J Athl Train. 2002;37:146–150. [PMC free article] [PubMed] [Google Scholar]
- Ash C J, Cook J R, McMurry T A, Auner C R. The use of rectal temperature to monitor heat stroke. Mo Med. 1992;89:283–288. [PubMed] [Google Scholar]
- Brechue W F, Stager J M. Acetazolamide alters temperature regulation during submaximal exercise. J Appl Physiol. 1990;69:1402–1407. doi: 10.1152/jappl.1990.69.4.1402. [DOI] [PubMed] [Google Scholar]
- Kubica R, Nielsen B, Bonnesen A, Rasmussen I B, Stoklosa J, Wilk B. Relationship between plasma volume reduction and plasma electrolyte changes after prolonged bicycle exercise, passive heating and diuretic dehydration. Acta Physiol Pol. 1983;34:569–579. [PubMed] [Google Scholar]
- Claremont A D, Costill D L, Fink W, Van Handel P. Heat tolerance following diuretic induced dehydration. Med Sci Sports. 1976;8:239–243. [PubMed] [Google Scholar]
- Desruelle A V, Boisvert P, Candas V. Alcohol and its variable effect on human thermoregulatory response to exercise in a warm environment. Eur J Appl Physiol Occup Physiol. 1996;74:572–574. doi: 10.1007/BF02376775. [DOI] [PubMed] [Google Scholar]
- Kalant H, Le A D. Effect of ethanol on thermoregulation. Pharmacol Ther. 1983;23:313–364. doi: 10.1016/0163-7258(83)90018-9. [DOI] [PubMed] [Google Scholar]
- Vanakoski J, Seppala T. Heat exposure and drugs: a review of the effects of hyperthermia on pharmacokinetics. Clin Pharmacokinet. 1998;34:311–322. doi: 10.2165/00003088-199834040-00004. [DOI] [PubMed] [Google Scholar]
- Shirreffs S M, Maughan R J. Urine osmolality and conductivity as indices of hydration status in athletes in the heat. Med Sci Sports Exerc. 1998;30:1598–1602. doi: 10.1097/00005768-199811000-00007. [DOI] [PubMed] [Google Scholar]
- Kaplan A, Szabo L L, Opheim K E. Clinical Chemistry: Interpretations and Techniques. 2nd ed Lea & Febiger; Philadelphia, PA: 1983. [Google Scholar]
- Ross D, Neely A E. Textbook of Urinalysis and Body Fluids. Appleton-Century-Crofts; Norwalk, CT: 1983. [Google Scholar]
- Armstrong L. The impact of hyperthermia and hypohydration on circulation strength endurance and health. J Appl Sport Sci Res. 1998;2:60–65. [Google Scholar]
- Montain S J, Sawka M N, Cadarette B S, Quigley M D, McKay J M. Physiological tolerance to uncompensable heat stress: effects of exercise intensity, protective clothing, and climate. J Appl Physiol. 1994;77:216–222. doi: 10.1152/jappl.1994.77.1.216. [DOI] [PubMed] [Google Scholar]
- Kenney W L, Hyde D E, Bernard T E. Physiological evaluation of liquid-barrier, vapor-permeable protective clothing ensembles for work in hot environments. Am Ind Hyg Assoc J. 1993;54:397–402. doi: 10.1080/15298669391354865. [DOI] [PubMed] [Google Scholar]
- Mathews D K, Fox E L, Tanzi D. Physiological responses during exercise and recovery in a football uniform. J Appl Physiol. 1969;26:611–615. doi: 10.1152/jappl.1969.26.5.611. [DOI] [PubMed] [Google Scholar]
- Armstrong L E. The nature of heatstroke during exercise. Natl Strength Condition J. 1992;14:80. [Google Scholar]
- Wetterhall S F, Coulombier D M, Herndon J M, Zaza S, Cantwell J D. Medical care delivery at the 1996 Olympic Games: Centers for Disease Control and Prevention Olympics Surveillance Unit. JAMA. 1998;279:1463–1468. doi: 10.1001/jama.279.18.1463. [DOI] [PubMed] [Google Scholar]
- Cooper K E. Some responses of the cardiovascular system to heat and fever. Can J Cardiol. 1994;10:444–448. [PubMed] [Google Scholar]
- Epstein Y. Heat intolerance: predisposing factor or residual injury? Med Sci Sports Exerc. 1990;22:29–35. [PubMed] [Google Scholar]
- Chung N K, Pin C H. Obesity and the occurrence of heat disorders. Mil Med. 1996;161:739–742. [PubMed] [Google Scholar]
- Gardner J W, Kark J A, Karnei K, et al. Risk factors predicting exertional heat illness in male Marine Corps recruits. Med Sci Sports Exerc. 1996;28:939–944. doi: 10.1097/00005768-199608000-00001. [DOI] [PubMed] [Google Scholar]
- Hayward J S, Eckerson J D, Dawson B T. Effect of mesomorphy on hyperthermia during exercise in a warm, humid environment. Am J Phys Anthropol. 1986;70:11–17. doi: 10.1002/ajpa.1330700104. [DOI] [PubMed] [Google Scholar]
- Kark J A, Burr P Q, Wenger C B, Gastaldo E, Gardner J W. Exertional heat illness in Marine Corps recruit training. Aviat Space Environ Med. 1996;67:354–360. [PubMed] [Google Scholar]
- Piwonka R W, Robinson S, Gay V L, Manalis R S. Preacclimatization of men to heat by training. J Appl Physiol. 1965;20:379–384. doi: 10.1152/jappl.1965.20.3.379. [DOI] [PubMed] [Google Scholar]
- Noakes T D, Myburgh K H, du Plessis J, et al. Metabolic rate, not percent dehydration, predicts rectal temperature in marathon runners. Med Sci Sports Exerc. 1991;23:443–449. [PubMed] [Google Scholar]
- Nadel E R, Pandolf K B, Roberts M F, Stolwijk J A. Mechanisms of thermal acclimation to exercise and heat. J Appl Physiol. 1974;37:515–520. doi: 10.1152/jappl.1974.37.4.515. [DOI] [PubMed] [Google Scholar]
- Walter F F, Bey T A, Ruschke D S, Benowitz N L. Marijuana and hyperthermia. J Toxicol Clin Toxicol. 1996;34:217–221. doi: 10.3109/15563659609013773. [DOI] [PubMed] [Google Scholar]
- Watson J D, Ferguson C, Hinds C J, Skinner R, Coakley J H. Exertional heat stroke induced by amphetamine analogues: does dantrolene have a place? Anaesthesia. 1993;48:1057–1060. doi: 10.1111/j.1365-2044.1993.tb07526.x. [DOI] [PubMed] [Google Scholar]
- Epstein Y, Albukrek D, Kalmovitc B, Moran D S, Shapiro Y. Heat intolerance induced by antidepressants. Ann N Y Acad Sci. 1997;813:553–558. doi: 10.1111/j.1749-6632.1997.tb51746.x. [DOI] [PubMed] [Google Scholar]
- Stadnyk A N, Glezos J D. Drug-induced heat stroke. Can Med Assoc J. 1983;128:957–959. [PMC free article] [PubMed] [Google Scholar]
- Forester D. Fatal drug-induced heat stroke. JACEP. 1978;7:243–244. doi: 10.1016/s0361-1124(78)80386-4. [DOI] [PubMed] [Google Scholar]
- Sarnquist F, Larson C P., Jr Drug-induced heat stroke. Anesthesiology. 1973;39:348–350. doi: 10.1097/00000542-197309000-00023. [DOI] [PubMed] [Google Scholar]
- Zelman S, Guillan R. Heat stroke in phenothiazine-treated patients: a report of three fatalities. Am J Psychiatry. 1970;126:1787–1790. doi: 10.1176/ajp.126.12.1787. [DOI] [PubMed] [Google Scholar]
- Gordon N F, Duncan J J. Effect of beta-blockers on exercise physiology: implications for exercise training. Med Sci Sports Exerc. 1991;23:668–676. [PubMed] [Google Scholar]
- Freund B J, Joyner M J, Jilka S M, et al. Thermoregulation during prolonged exercise in heat: alterations with beta-adrenergic blockade. J Appl Physiol. 1987;63:930–936. doi: 10.1152/jappl.1987.63.3.930. [DOI] [PubMed] [Google Scholar]
- Kew M C, Hopp M, Rothberg A. Fatal heat-stroke in a child taking appetite-suppressant drugs. S Afr Med J. 1982;62:905–906. [PubMed] [Google Scholar]
- Lomax P, Daniel K A. Cocaine and body temperature: effect of exercise at high ambient temperature. Pharmacology. 1993;46:164–172. doi: 10.1159/000139042. [DOI] [PubMed] [Google Scholar]
- Chen W L, Huang W S, Lin Y F, Shieh S D. Changes in thyroid hormone metabolism in exertional heat stroke with or without acute renal failure. J Clin Endocrinol Metab. 1996;81:625–629. doi: 10.1210/jcem.81.2.8636279. [DOI] [PubMed] [Google Scholar]
- Wemple R D, Lamb D R, McKeever K H. Caffeine vs caffeine-free sports drinks: effect on urine production at rest and during prolonged exercise. Int J Sports Med. 1997;18:40–46. doi: 10.1055/s-2007-972593. [DOI] [PubMed] [Google Scholar]
- Odlind B. Site and mechanism of the action of diuretics. Acta Pharmacol Toxicol (Copenh) 1984;54(suppl 1):5–15. doi: 10.1111/j.1600-0773.1984.tb03625.x. [DOI] [PubMed] [Google Scholar]
- Stookey J D. The diuretic effects of alcohol and caffeine and total water intake misclassification. Eur J Epidemiol. 1999;15:181–188. doi: 10.1023/a:1007559725607. [DOI] [PubMed] [Google Scholar]
- Schlaeffer F, Engelberg I, Kaplanski J, Danon A. Effect of exercise and environmental heat on theophylline kinetics. Respiration. 1984;45:438–442. doi: 10.1159/000194651. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Hubbard R W, Askew E W, et al. Responses to moderate and low sodium diets during exercise-heat acclimation. Int J Sport Nutr. 1993;3:207–221. doi: 10.1123/ijsn.3.2.207. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Szlyk P C, DeLuca J P, Sils I V, Hubbard R W. Fluid-electrolyte losses in uniforms during prolonged exercise at 30 degrees C. Aviat Space Environ Med. 1992;63:351–355. [PubMed] [Google Scholar]
- Mendyka B E. Fluid and electrolyte disorders caused by diuretic therapy. AACN Clin Issues Crit Care Nurs. 1992;3:672–680. doi: 10.4037/15597768-1992-3014. [DOI] [PubMed] [Google Scholar]
- Melby J C. Selected mechanisms of diuretic-induced electrolyte changes. Am J Cardiol. 1986;58:1A–4A. doi: 10.1016/0002-9149(86)90874-x. [DOI] [PubMed] [Google Scholar]
- Bourdon L, Canini F. On the nature of the link between malignant hyperthermia and exertional heatstroke. Med Hypotheses. 1995;45:268–270. doi: 10.1016/0306-9877(95)90116-7. [DOI] [PubMed] [Google Scholar]
- Dixit S N, Bushara K O, Brooks B R. Epidemic heat stroke in midwest community: risk factors, neurological complications, and sequelae. Wis Med J. 1997;96:39–41. [PubMed] [Google Scholar]
- Hunter S L, Rosenberg H, Tuttle G H, DeWalt J L, Smodie R, Martin J. Malignant hyperthermia in a college football player. Physician Sportsmed. 1987;15(12):77–81. [Google Scholar]
- Lazarus A. Differentiating neuroleptic-related heatstroke from neuroleptic malignant syndrome. Psychosomatics. 1989;30:454–456. doi: 10.1016/S0033-3182(89)72256-8. [DOI] [PubMed] [Google Scholar]
- Rampertaap M P. Neuroleptic malignant syndrome. South Med J. 1986;79:331–336. doi: 10.1097/00007611-198603000-00018. [DOI] [PubMed] [Google Scholar]
- Addonizio G, Susman V. Neuroleptic malignant syndrome and heat stroke. Br J Psychiatry. 1984;145:556–557. doi: 10.1192/bjp.145.5.556. [DOI] [PubMed] [Google Scholar]
- Martin M L, Lucid E J, Walker R W. Neuroleptic malignant syndrome. Ann Emerg Med. 1985;14:354–358. doi: 10.1016/s0196-0644(85)80104-9. [DOI] [PubMed] [Google Scholar]
- Virmani R, Robinowitz M. Cardiac pathology and sports medicine. Hum Pathol. 1987;18:493–501. doi: 10.1016/s0046-8177(87)80034-5. [DOI] [PubMed] [Google Scholar]
- Buchwald I, Davis P J. Scleroderma with fatal heat stroke. JAMA. 1967;201:270–271. [PubMed] [Google Scholar]
- Smith H R, Dhatt G S, Melia W M, Dickinson J G. Cystic fibrosis presenting as hyponatraemic heat exhaustion. BMJ. 1995;310:579–580. doi: 10.1136/bmj.310.6979.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews C, Mango M, Venuto R C. Cystic fibrosis in adults. Ann Intern Med. 1978;88:128–129. doi: 10.7326/0003-4819-88-1-128_3. [DOI] [PubMed] [Google Scholar]
- Kerle K K, Nishimura K D. Exertional collapse and sudden death associated with sickle cell trait. Am Fam Physician. 1996;54:237–240. [PubMed] [Google Scholar]
- Gardner J W, Kark J A. Fatal rhabdomyolysis presenting as mild heat illness in military training. Mil Med. 1994;159:160–163. [PubMed] [Google Scholar]
- Kenney W L. Thermoregulation during exercise in the heat. Athl Ther Today. 1996;1:13–16. [Google Scholar]
- Tilley R I, Standerwick J M, Long G J. Ability of the Wet Bulb Globe Temperature Index to predict heat stress in men wearing NBC protective clothing. Mil Med. 1987;152:554–556. [PubMed] [Google Scholar]
- Rasch W, Cabanac M. Selective brain cooling is affected by wearing headgear during exercise. J Appl Physiol. 1993;74:1229–1233. doi: 10.1152/jappl.1993.74.3.1229. [DOI] [PubMed] [Google Scholar]
- Sheffield-Moore M, Short K R, Kerr C G, Parcell A C, Bolster D R, Costill D L. Thermoregulatory responses to cycling with and without a helmet. Med Sci Sports Exerc. 1997;29:755–761. doi: 10.1097/00005768-199706000-00004. [DOI] [PubMed] [Google Scholar]
- Shapiro Y, Pandolf K B, Avellini B A, Pimental N A, Goldman R F. Physiological responses of men and women to humid and dry heat. J Appl Physiol. 1980;49:1–8. doi: 10.1152/jappl.1980.49.1.1. [DOI] [PubMed] [Google Scholar]
- Yaglou C P, Minard D. Control of heat casualties at military training centers. Arch Ind Health. 1957;16:302–305. [PubMed] [Google Scholar]
- Bracker M O. Hyperthermia: man's adaptation to a warm climate. Sports Med Dig. 1991;13:1–2. [Google Scholar]
- Johnson S C, Ruhling R O. Aspirin in exercise-induced hyperthermia: evidence for and against its role. Sports Med. 1985;2:1–7. doi: 10.2165/00007256-198502010-00001. [DOI] [PubMed] [Google Scholar]
- Werner J. Central regulation of body temperature. In: Gisolfi C, editor. Exercise, Heat, and Thermoregulation. Cooper Publishing; Carmel, IN: 1993. pp. 7–35. [Google Scholar]
- Galaski M J. Hyperthermia. J Can Athl Ther. 1985;12:23–26. [Google Scholar]
- Yaqub B A. Neurologic manifestations of heatstroke at the Mecca pilgrimage. Neurology. 1987;37:1004–1006. doi: 10.1212/wnl.37.6.1004. [DOI] [PubMed] [Google Scholar]
- Armstrong L E. Keeping Your Cool in Barcelona: The Effects of Heat Humidity and Dehydration on Athletic Performance Strength and Endurance. United States Olympic Committee Sports Sciences Division; Colorado Springs, CO: 1992. pp. 1–29. [Google Scholar]
- Anderson G S, Meneilly G S, Mekjavic I B. Passive temperature lability in the elderly. Eur J Appl Physiol Occup Physiol. 1996;73:278–286. doi: 10.1007/BF02425488. [DOI] [PubMed] [Google Scholar]
- Candas V, Libert J P, Vogt J J. Influence of air velocity and heat acclimation on human skin wettedness and sweating efficiency. J Appl Physiol. 1979;47:1194–2000. doi: 10.1152/jappl.1979.47.6.1194. [DOI] [PubMed] [Google Scholar]
- Berglund L G, Gonzalez R R. Evaporation of sweat from sedentary man in humid environments. J Appl Physiol. 1977;42:767–772. doi: 10.1152/jappl.1977.42.5.767. [DOI] [PubMed] [Google Scholar]
- Gabrys J, Pieniazek W, Olejnik I, Pogorzelska T, Karpe J. Effects of local cooling of neck circulatory responses in men subjected to physical exercise in hyperthermia. Biol Sport. 1993;10:167–171. [Google Scholar]
- Royburt M, Epstein Y, Solomon Z, Shemer J. Long-term psychological and physiological effects of heat stroke. Physiol Behav. 1993;54:265–267. doi: 10.1016/0031-9384(93)90109-s. [DOI] [PubMed] [Google Scholar]
- Mehta A C, Baker R N. Persistent neurological deficits in heat stroke. Neurology. 1970;20:336–340. doi: 10.1212/wnl.20.4.336. [DOI] [PubMed] [Google Scholar]
- McArdle W D, Katch F I, Katch V L. Exercise Physiology. 3rd ed. Lea & Febiger; Philadelphia, PA: 1991. pp. 556–570. [Google Scholar]
- Avellini B A, Kamon E, Krajewski J T. Physiological responses of physically fit men and women to acclimation to humid heat. J Appl Physiol. 1980;49:254–261. doi: 10.1152/jappl.1980.49.2.254. [DOI] [PubMed] [Google Scholar]
- Geor R J, McCutcheon L J. Thermoregulatory adaptations associated with training and heat acclimation. Vet Clin North Am Equine Pract. 1988;14:97–120. doi: 10.1016/s0749-0739(17)30214-6. [DOI] [PubMed] [Google Scholar]
- Nielsen B. Heat stress and acclimation. Ergonomics. 1994;37:49–58. doi: 10.1080/00140139408963622. [DOI] [PubMed] [Google Scholar]
- Gisolfi C V, Wenger C B. Temperature regulation during exercise: old concepts, new ideas. Exerc Sport Sci Rev. 1984;12:339–372. [PubMed] [Google Scholar]
- Morimoto T, Miki K, Nose H, Yamada S, Hirakawa K, Matsubara D. Changes in body fluid and its composition during heavy sweating and effect of fluid and electrolyte replacement. Jpn J Biometeorol. 1981;18:31–39. [Google Scholar]
- Pandolf K B, Cadarette B S, Sawka M N, Young A J, Francesconi R P, Gonzalez R R. Thermoregulatory responses of middle-aged and young men during dry-heat acclimation. J Appl Physiol. 1998;65:65–71. doi: 10.1152/jappl.1988.65.1.65. [DOI] [PubMed] [Google Scholar]
- Pandolf K B, Burse R L, Goldman R F. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics. 1977;20:399–408. doi: 10.1080/00140137708931642. [DOI] [PubMed] [Google Scholar]
- Cadarette B S, Sawka M N, Toner M M, Pandolf K B. Aerobic fitness and the hypohydration response to exercise-heat stress. Aviat Space Environ Med. 1984;55:507–512. [PubMed] [Google Scholar]
- Buskirk E R, Iampietro P F, Bass D E. Work performance after dehydration: effects of physical conditioning and heat acclimatization. J Appl Physiol. 1958;12:789–794. doi: 10.1152/jappl.1958.12.2.189. [DOI] [PubMed] [Google Scholar]
- Adams J, Fox R, Grimby G, Kidd D, Wolff H. Acclimatization to heat and its rate of decay in man. J Physiol. 1960;152:26P–27P. [Google Scholar]
- Czerkawski J T, Meintod A, Kleiner D M. Exertional heat illness: teaching patients when to cool it. Your Patient Fitness. 1996;10:13–20. [Google Scholar]
- Wyndham C, Strydom N, Cooks H, et al. Methods of cooling subjects with hyperpyrexia. J Appl Physiol. 1959;14:771–776. doi: 10.1152/jappl.1959.14.5.771. [DOI] [PubMed] [Google Scholar]
- Hayward J S, Collis M, Eckerson J D. Thermographic evaluation of relative heat loss areas of man during cold water immersion. Aerosp Med. 1973;44:708–711. [PubMed] [Google Scholar]
- Tsuzuki-Hayakawa K, Tochihara Y, Ohnaka T. Thermoregulation during heat exposure of young children compared to their mothers. Eur J Appl Physiol Occup Physiol. 1995;72:12–17. doi: 10.1007/BF00964108. [DOI] [PubMed] [Google Scholar]
- Bar-Or O. Children's responses to exercise in hot climates: implications for performance and health. Sports Sci Exerc. 1994;7:1–5. [Google Scholar]
- Davies C T. Thermal responses to exercise in children. Ergonomics. 1981;24:55–61. doi: 10.1080/00140138108924830. [DOI] [PubMed] [Google Scholar]
- Docherty D, Eckerson J D, Hayward J S. Physique and thermoregulation in prepubertal males during exercise in a warm, humid environment. Am J Phys Anthropol. 1986;70:19–23. doi: 10.1002/ajpa.1330700105. [DOI] [PubMed] [Google Scholar]
- Armstrong L E, Maresh C M. Exercise-heat tolerance of children and adolescents. Pediatr Exerc Sci. 1995;7:239–252. [Google Scholar]
- Gutierrez G G. Solar injury and heat illness: treatment and prevention in children. Physician Sportsmed. 1995;23(7):43–48. doi: 10.1080/00913847.1995.11947812. [DOI] [PubMed] [Google Scholar]
- Nash H L. Hyperthermia: risks greater in children. Physician Sportsmed. 1987;15(2):29. [Google Scholar]
- American Academy of Pediatrics Committee on Sports Medicine Climatic heat stress and the exercising child. Pediatrics. 1982;69:808–809. [PubMed] [Google Scholar]
- Kenney W L, Hodgson J L. Heat tolerance, thermoregulation, and ageing. Sports Med. 1987;4:446–456. doi: 10.2165/00007256-198704060-00004. [DOI] [PubMed] [Google Scholar]
- Wagner J A, Robinson S, Tzankoff S P, Marino R P. Heat tolerance and acclimatization to work in the heat in relation to age. J Appl Physiol. 1972;33:616–622. doi: 10.1152/jappl.1972.33.5.616. [DOI] [PubMed] [Google Scholar]
- Pandolf K B. Heat tolerance and aging. Exp Aging Res. 1994;20:275–284. doi: 10.1080/03610739408253977. [DOI] [PubMed] [Google Scholar]
- Pandolf K B. Aging and human heat tolerance. Exp Aging Res. 1997;23:69–105. doi: 10.1080/03610739708254027. [DOI] [PubMed] [Google Scholar]
- Kenney W. The older athlete: exercise in hot environments. Sports Sci Exerc. 1993;6:1–4. [Google Scholar]
- Inoue Y, Shibasaki M, Hirata K, Araki T. Relationship between skin blood flow and sweating rate and age related regional differences. Eur J Appl Physiol Occup Physiol. 1998;79:17–23. doi: 10.1007/s004210050467. [DOI] [PubMed] [Google Scholar]
- Sagawa S, Shiraki K, Yousef M K, Miki K. Sweating and cardiovascular responses of aged men to heat exposure. J Gerontol. 1988;43:M1–M8. doi: 10.1093/geronj/43.1.m1. [DOI] [PubMed] [Google Scholar]
- Inoue Y, Shibasaki M. Regional differences in age-related decrements of the cutaneous vascular and sweating responses to passive heating. Eur J Appl Physiol Occup Physiol. 1996;74:78–84. doi: 10.1007/BF00376498. [DOI] [PubMed] [Google Scholar]
- Inoue Y, Shibasaki M, Ueda H, Ishizashi H. Mechanisms underlying the age-related decrement in the human sweating response. Eur J Appl Physiol Occup Physiol. 1999;79:121–126. doi: 10.1007/s004210050485. [DOI] [PubMed] [Google Scholar]
- Pandolf K B, Cafarelli E, Noble B J, Metz K F. Hyperthermia: effect on exercise prescription. Arch Phys Med Rehabil. 1975;56:524–526. [PubMed] [Google Scholar]
- Zappe D H, Bell G W, Swartzentruber H, Wideman R F, Kenney W L. Age and regulation of fluid and electrolyte balance during repeated exercise sessions. Am J Physiol. 1996;207(1 Pt 2):R71–R79. doi: 10.1152/ajpregu.1996.270.1.R71. [DOI] [PubMed] [Google Scholar]
- Binkhorst R A, Hopman M T. Heat balance in paraplegic individuals during arm exercise at 10 and 35°C. Med Sci Sports Exerc. 1995;27(suppl):83. [Google Scholar]
- Clark M W. The physically challenged athlete. Adolesc Med. 1998;9:491–499. [PubMed] [Google Scholar]
- Bloomquist L E. Injuries to athletes with physical disabilities: prevention implications. Physician Sportsmed. 1986;14(9):96–100,102,105. doi: 10.1080/00913847.1986.11709170. [DOI] [PubMed] [Google Scholar]
- Hopman M T, Binkhourst R A. Spinal cord injury and exercise in the heat. Sports Sci Exerc. 1997;10:1–4. [Google Scholar]
- Armstrong L E, Maresh C M, Riebe D, et al. Local cooling in wheelchair athletes during exercise-heat stress. Med Sci Sports Exerc. 1995;27:211–216. [PubMed] [Google Scholar]
- Sawka M N, Latzka W A, Pandolf K B. Temperature regulation during upper body exercise: able-bodied and spinal cord injured. Med Sci Sports Exerc. 1989;21(5 suppl):132–140. [PubMed] [Google Scholar]
- Hopman M T, Oeseburg B, Binkhorst R A. Cardiovascular responses in persons with paraplegia to prolonged arm exercise and thermal stress. Med Sci Sports Exerc. 1993;25:577–583. [PubMed] [Google Scholar]
- Petrofsky J S. Thermoregulatory stress during rest and exercise in heat in patients with a spinal cord injury. Eur J Appl Physiol Occup Physiol. 1992;64:503–507. doi: 10.1007/BF00843758. [DOI] [PubMed] [Google Scholar]
- Bracker M D. Environmental and thermal injury. Clin Sports Med. 1992;11:419–436. [PubMed] [Google Scholar]
- Hopman M T. Circulatory responses during arm exercise in individuals with paraplegia. Int J Sports Med. 1994;15:126–131. doi: 10.1055/s-2007-1021033. [DOI] [PubMed] [Google Scholar]
- Yamaski M, Kim K T, Choi S W, Muraki S, Shiokawa M, Kurokawa T. Characteristics of body heat balance of paraplegics during exercise in a hot environment. J Physiol Anthropol Appl Human Sci. 2001;20:227–232. doi: 10.2114/jpa.20.227. [DOI] [PubMed] [Google Scholar]
- Gass G C, Camp E M, Nadel E R, Gwinn T H, Engel P. Rectal and rectal vs. esophageal temperatures in paraplegic men during prolonged exercise. J Appl Physiol. 1998;64:2265–2271. doi: 10.1152/jappl.1988.64.6.2265. [DOI] [PubMed] [Google Scholar]
- Yaqub B A, Al-Harthi S S, Al-Orainey I O, Laajam M A, Obeid M T. Heat stroke at the Mekkah pilgrimage: clinical characteristics and course of 30 patients. Q J Med. 1986;59:523–530. [PubMed] [Google Scholar]
- Hubbard R W. The role of exercise in the etiology of exertional heatstroke. Med Sci Sports Exerc. 1990;22:2–5. [PubMed] [Google Scholar]
- Holman N D, Schneider A J. Multi-organ damage in exertional heat stroke. Neth J Med. 1989;35:38–43. [PubMed] [Google Scholar]
- Shibolet S, Coll R, Gilat T, Sohar E. Heatstroke: its clinical picture and mechanism in 36 cases. Q J Med. 1965;36:525–548. [PubMed] [Google Scholar]
- Gummaa K, El-Mahrouky S, Mahmoud H, Mustafa K, Khogall M. The metabolic status of heat stroke patients: the Makkah experience. In: Khogali M, Hale J R, editors. Heat Stroke and Temperature Regulation. Academic Press; New York, NY: 1983. pp. 157–169. [Google Scholar]
- Garcia-Rubira J C, Aguilar J, Romero D. Acute myocardial infarction in a young man after heat exhaustion. Int J Cardiol. 1995;47:297–300. doi: 10.1016/0167-5273(94)02204-v. [DOI] [PubMed] [Google Scholar]
- Senay L C, Kok R. Body fluid responses of heat-tolerant and intolerant men to work in a hot wet environment. J Appl Physiol. 1976;40:55–59. doi: 10.1152/jappl.1976.40.1.55. [DOI] [PubMed] [Google Scholar]
- Shvartz E, Shibolet S, Merez A, Magazanik A, Shapiro Y. Prediction of heat tolerance from heart rate and rectal temperature in a temperate environment. J Appl Physiol. 1977;43:684–688. doi: 10.1152/jappl.1977.43.4.684. [DOI] [PubMed] [Google Scholar]
- Strydom N B. Heat intolerance: its detection and elimination in the mining industry. S Afr J Sci. 1980;76:154–156. [Google Scholar]
- Robergs R A, Roberts S O. Exercise Physiology: Exercise, Performance, and Clinical Applications. Mosby; St Louis, MO: 1997. pp. 653–662. [Google Scholar]


