Abstract
Objective: To describe the functional anatomy of the ankle complex as it relates to lateral ankle instability and to describe the pathomechanics and pathophysiology of acute lateral ankle sprains and chronic ankle instability.
Data Sources: I searched MEDLINE (1985–2001) and CINAHL (1982–2001) using the key words ankle sprain and ankle instability.
Data Synthesis: Lateral ankle sprains are among the most common injuries incurred during sports participation. The ankle functions as a complex with contributions from the talocrural, subtalar, and inferior tibiofibular joints. Each of these joints must be considered in the pathomechanics and pathophysiology of lateral ankle sprains and chronic ankle instability. Lateral ankle sprains typically occur when the rearfoot undergoes excessive supination on an externally rotated lower leg. Recurrent ankle sprain is extremely common; in fact, the most common predisposition to suffering a sprain is the history of having suffered a previous ankle sprain. Chronic ankle instability may be due to mechanical instability, functional instability, or most likely, a combination of these 2 phenomena. Mechanical instability may be due to specific insufficiencies such as pathologic laxity, arthrokinematic changes, synovial irritation, or degenerative changes. Functional instability is caused by insufficiencies in proprioception and neuromuscular control.
Conclusions/Recommendations: Lateral ankle sprains are often inadequately treated, resulting in frequent recurrence of ankle sprains. Appreciation of the complex anatomy and mechanics of the ankle joint and the pathomechanics and pathophysiology related to acute and chronic ankle instability is integral to the process of effectively evaluating and treating ankle injuries.
Keywords: ankle sprain, talocrural joint, subtalar joint, mechanical instability, functional instability
Injuries to the lateral ligaments of the ankle complex are among the most common injuries incurred by athletes.1 Lateral ankle sprains are thought to be suffered by men and women at approximately the same rates; however, one recent report2 suggests that female interscholastic and intercollegiate basketball players have a 25% greater risk of incurring grade I ankle sprains than their male counterparts. More than 23 000 ankle sprains have been estimated to occur per day in the United States, which equates to one sprain per 10 000 people daily.3 The most common predisposition to suffering a lateral ankle sprain is the history of at least one previous ankle sprain.4–8 In sports such as basketball, recurrence rates have been reported to exceed 70%.4,9 Repetitive sprains have also been linked to increased risk of osteoarthritis and articular degeneration at the ankle.10,11
Residual symptoms after lateral ankle sprain affect 55% to 72% of patients at 6 weeks to 18 months.12,13 The frequency of complications and breadth of longstanding symptoms after ankle sprain has led to the suggestion of a diagnosis of the “sprained ankle syndrome”14 and to the conclusion “that there is no such thing as a simple ankle sprain.”15 It has also been estimated that 55% of individuals suffering ankle sprains do not seek injury treatment from a health care professional.4,8 Thus, the severity of ankle sprains may often be underestimated by athletes, and current treatment strategies for lateral ankle sprains may not be effective in preventing recurrent injuries or residual symptoms.
Lateral ankle sprains are also referred to as inversion ankle sprains or occasionally as supination ankle sprains. Individuals who suffer numerous repetitive ankle sprains have been reported as having functional instability,16–18 chronic instability,19 and residual instability.20 The multitude of terms used to describe the phenomenon of repetitive ankle sprains has led to confusion in terminology. For the purposes of this article, the following definitions will apply: lateral ankle instability refers to the existence of an unstable ankle due to lateral ligamentous damage caused by excessive supination or inversion of the rearfoot. This term does not differentiate whether the instability is acute or chronic. Chronic ankle instability (CAI) denotes the occurrence of repetitive bouts of lateral ankle instability, resulting in numerous ankle sprains.
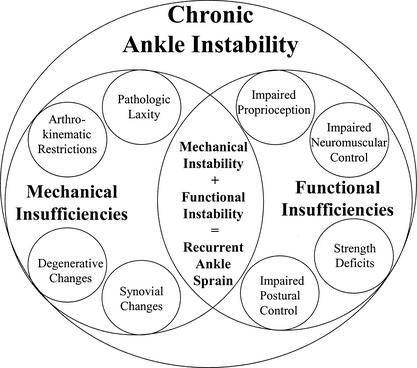
Traditionally, CAI has been attributed to 2 potential causes: mechanical instability and functional instability. Tropp et al21 discussed the notion of mechanical instability as a cause of CAI due to pathologic laxity after ankle-ligament injury. Freeman et al16,17 first described functional instability in 1965 when they attributed CAI to proprioceptive deficits after ligament injury. A more recent definition of functional instability is the occurrence of recurrent ankle instability and the sensation of joint instability due to the contributions of proprioceptive and neuromuscular deficits.22 While the dichotomy of functional and mechanical instability helps explain 2 common potential causes of CAI, it does not adequately reflect the complete spectrum of pathologic conditions leading to CAI. Specific insufficiencies interact to create either mechanical instability or functional instability. Functional instability may be caused by specific insufficiencies in proprioception, neuromuscular control, postural control, or strength. Mechanical instability may be caused by factors that alter the mechanics of one or more joints within the ankle complex. Potential mechanical insufficiencies include pathologic laxity, impaired arthrokinematics, synovial inflammation and impingement, and degenerative changes. Chronic ankle instability may be caused by mechanical instability, functional instability, or a combination of these entities.21,23
The purposes of this review article are to describe the functional anatomy of the ankle complex as it relates to lateral ankle instability and to discuss the pathomechanics and pathophysiology of acute lateral ankle sprain and CAI.
FUNCTIONAL ANATOMY
The ankle complex comprises 3 articulations: the talocrural joint, the subtalar joint, and the distal tibiofibular syndesmosis. These 3 joints work in concert to allow coordinated movement of the rearfoot. Rearfoot motion is often defined as occurring in the cardinal planes as follows: sagittal-plane motion (plantar flexion-dorsiflexion), frontal-plane motion (inversion-eversion), and transverse-plane motion (internal rotation-external rotation).24 Rearfoot motion, however, does not occur in isolation in the individual planes; rather, coordinated movement of the 3 joints allows the rearfoot to move as a unit about an axis of rotation oblique to the long axis of the lower leg. Rearfoot motion does not occur strictly in the cardinal planes because the talocrural and subtalar joints each have oblique axes of rotation. Coupled rearfoot motion is best described as pronation and supination. In the open kinetic chain, pronation consists of dorsiflexion, eversion, and external rotation, while supination consists of plantar flexion, inversion, and internal rotation.25 In the closed kinetic chain, pronation consists of plantar flexion, eversion, and external rotation, while supination consists of dorsiflexion, inversion, and internal rotation.25
The 3 major contributors to stability of the ankle joints are (1) the congruity of the articular surfaces when the joints are loaded, (2) the static ligamentous restraints, and (3) the musculotendinous units, which allow for dynamic stabilization of the joints. The functional aspect of each of these as it relates to lateral ankle instability will be discussed later.
Talocrural Joint Anatomy
The talocrural, or tibiotalar, joint is formed by the articulation of the dome of the talus, the medial malleolus, the tibial plafond, and the lateral malleolus. The shape of the talocrural joint allows torque to be transmitted from the lower leg (internal and external rotation) to the foot (pronation and supination) during weight bearing. This joint is sometimes called the “mortise” joint and, in isolation, may be thought of as a hinge joint that allows the motions of plantar flexion and dorsiflexion. The axis of rotation of the talocrural joint passes through the medial and lateral malleoli. It is slightly anterior to the frontal plane as it passes through the tibia but slightly posterior to the frontal plane as it passes through the fibula. Isolated movement of the talocrural joint is primarily in the sagittal plane, but small amounts of transverse- and frontal-plane motion also occur about the oblique axis of rotation.26
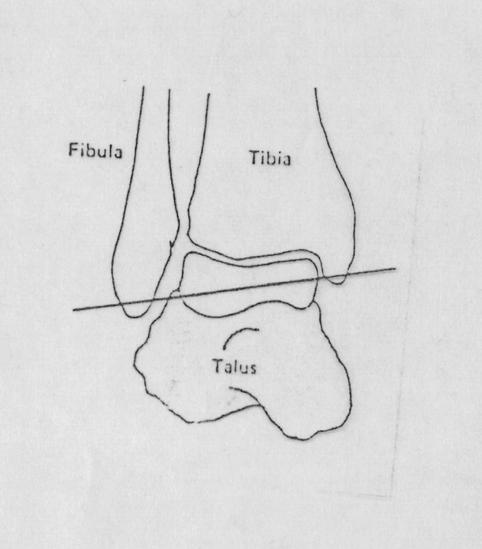
In an in vivo study of loaded ankles in the closed kinetic chain, 30° of physiologic plantar flexion (actual motion) from the neutral position was composed of 28° sagittal-plane movement (plantar flexion), 1° transverse-plane movement (internal rotation), and 4° frontal-plane movement (inversion).26 Comparatively, 30° of physiologic dorsiflexion (actual motion) in the closed kinetic chain was composed of 23° sagittal-plane movement (dorsiflexion), 9° transverse-plane movement (external rotation), and 2° frontal-plane movement (eversion).26 Closed kinetic chain dorsiflexion occurs when the tibia moves anteriorly on the fixed talus during weight bearing. The concept of triplanar motion at the talocrural motion is important in understanding the stability of the talocrural joint (Figure 1).
Figure 1.
The talocrural axis of rotation.
When the ankle complex is fully loaded, the articular surfaces are the primary stabilizers against excessive talar rotation and translation27; however, the contribution of the ligaments to talocrural joint stability is crucial. The talocrural joint receives ligamentous support from a joint capsule and several ligaments, including the anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), calcaneofibular ligament (CFL), and deltoid ligament. The ATFL, PTFL, and CFL support the lateral aspect of the ankle, while the deltoid ligament provides medial support.
The ATFL lies on the dorsolateral aspect of the foot and courses from the lateral malleolus anteriorly and medially toward the talus at an angle of approximately 45° from the frontal plane.28 The ATFL is an average of 7.2 mm wide and 24.8 mm long.28 In vitro kinematic studies have shown that the ATFL prevents anterior displacement of the talus from the mortise and excessive inversion and internal rotation of the talus on the tibia.27, 29–32 The strain in the ATFL increases as the ankle moves from dorsiflexion into plantar flexion.29 The ATFL demonstrates lower maximal load and energy to failure values under tensile stress as compared with the PTFL, CFL, anterior inferior tibiofibular ligament, and deltoid ligament.33 This may explain why the ATFL is the most frequently injured of the lateral ligaments.34
The CFL courses from the lateral malleolus posteriorly and inferiorly to the lateral aspect of the calcaneus at a mean angle of 133° from the long axis of the fibula.28 The CFL restricts excessive supination of both the talocrural and subtalar joints. In vitro experiments have demonstrated that the CFL restricts excessive inversion and internal rotation of the rearfoot and is most taut when the ankle is dorsiflexed.27,32,35 The CFL is the second most-often injured of the lateral talocrural ligaments.19
The PTFL runs from the lateral malleolus posteriorly to the posterolateral aspect of the talus. The PTFL has broad insertions on both the talus and fibula28 and provides restraint to both inversion and internal rotation of the loaded talocrural joint.27 It is the least commonly sprained of the lateral ankle ligaments.19
Subtalar Joint Anatomy
The subtalar joint is formed by the articulations between the talus and the calcaneus and, like the talucrural joint, it converts torque between the lower leg (internal and external rotation) and the foot (pronation and supination). The subtalar joint allows the motions of pronation and supination and consists of an intricate structure with 2 separate joint cavities. The posterior subtalar joint is formed between the inferior posterior facet of the talus and the superior posterior facet of the calcaneus.25 The anterior subtalar, or talocalcaneonavicular, joint is formed from the head of the talus, the anterior-superior facets, the sustentaculum tali of the calcaneus, and the concave proximal surface of the tarsal navicular. This articulation is similar to a ball-and-socket joint, with the talar head being the ball and the anterior calcaneal and proximal navicular surfaces forming the socket in conjunction with the spring ligament.36 Viladot et al37 reported great individual variation in the architecture of the anterior subtalar joint.
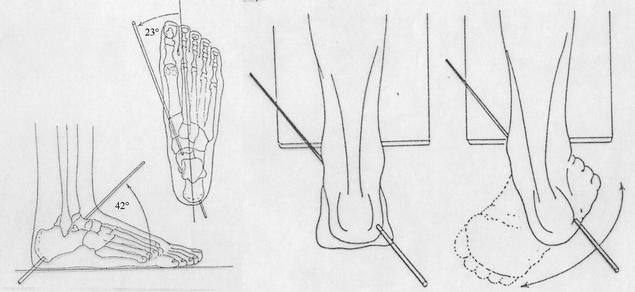
The anterior and posterior subtalar joints have separate ligamentous joint capsules and are separated from each other by the sinus tarsi and canalis tarsi.37 The anterior joint lies farther medial and has a higher center of rotation than the posterior joint, but the 2 joints share a common axis of rotation.36,37 This discrepancy results in an oblique axis of rotation of the subtalar joint, which averages a 42° upward tilt and a 23° medial angulation from the perpendicular axes of the foot (Figure 2).38 Great variations have been identified in the position of the axis of rotation across individuals.38
Figure 2.
The subtalar axis of rotation allows the triplanar motions of pronation and supination. This picture illustrates these motions in the open kinetic chain.
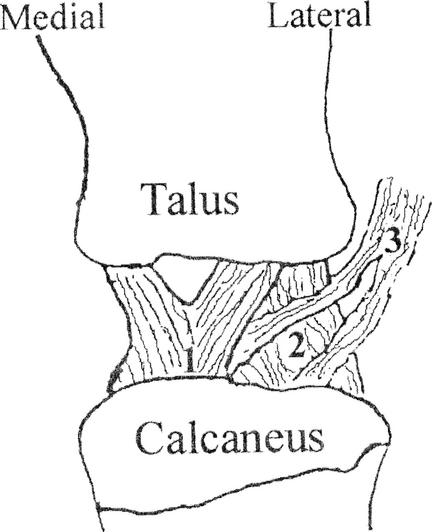
The ligamentous support of the subtalar joint is extensive and not well understood. Marked discrepancies exist in the literature regarding the terminology for the individual ligaments and the functions these ligaments serve.37,39 Essentially, the lateral ligaments may be divided into 3 groups: (1) deep ligaments, (2) peripheral ligaments, and (3) retinacula (Figure 3).37,40
Figure 3.
The intrinsic subtalar ligaments: (1) interosseous ligament, (2) cervical ligament, and (3) deep fibers of the extensor retinaculum. Reprinted with permission of Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508; Lippincott Williams & Wilkins.41
The deep ligaments consist of the cervical and interosseous ligaments. Together these ligaments stabilize the subtalar joint and form a barrier between the anterior and posterior joint capsules. These ligaments, which cross obliquely through the canalis tarsi, have been described as the “cruciate ligaments of the subtalar joint.”37 The cervical ligament lies anterior and lateral to the interosseous ligament and runs from the cervical tubercle of the calcaneus anteriorly and medially to the talar neck. The cervical ligament lies within the sinus tarsi and provides support to both the anterior and posterior joints.42 It is the strongest of the subtalar ligaments and has been shown to resist supination during in vitro kinematic experiments.30,37,39
The interosseous ligament lies just posterior to, and courses more medially than, the cervical ligament. The interosseous ligament originates on the calcaneus just anterior to the posterior subtalar joint capsule and runs superiorly and medially to its insertion on the talar neck. Because of its diagonal orientation and oblique fiber arrangement across the joint, portions of the interosseous ligament are taut throughout pronation and supination.30,37,39 This ligament is sometimes called the ligament of the canalis tarsi.30
Fibers of the inferior extensor retinacula (IER) have also been proposed to provide support to the lateral aspect of the subtalar joint.40 Three roots of the IER have been identified within the sinus tarsi: lateral, intermediate, and medial. Only the lateral root of the IER has been shown to significantly affect subtalar joint stability37; however, injury to any of the roots has been suggested in the cause of sinus tarsi syndrome.43
The peripheral ligaments of the subtalar joint include the CFL and lateral talocalcaneal (LTCL) and fibulotalocalcaneal (FTCL) ligaments. The CFL is integral in preventing excessive inversion and internal rotation of the calcaneus in relation to the talus.30,31,34,35 While the CFL does not normally connect the calcaneus to the talus, various attachments of the anterior aspect of the CFL to the talus have been reported.40
Lateral Ankle Ligaments
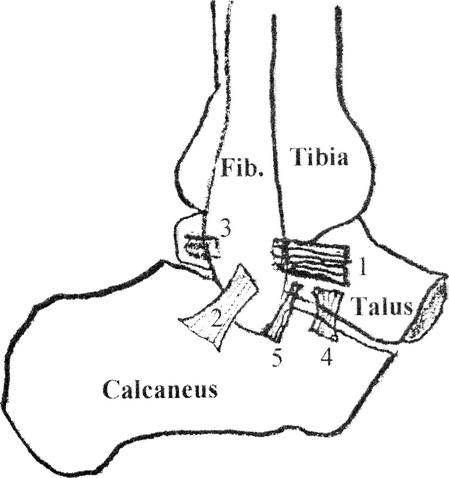
The LTCL runs parallel and anterior to the CFL but only crosses the posterior subtalar joint (Figure 4). While the LTCL is smaller and weaker than the CFL, it helps prevent excessive supination of the subtalar joint.28,30,37 Various shapes of the LTCL have been reported, and occasionally its fibers are continuous with those of the CFL.28,40 The FTCL, or ligament of Rouviere, runs from the posterior surface of the lateral malleolus to the posterolateral surface of the talus and then to the posterolateral calcaneus. It lies distinctly posterior to the CFL and assists in resisting excessive supination.37
Figure 4.
The lateral ligaments of the ankle: (1) anterior talofibular ligament, (2) calcaneofibular ligament, (3) posterior talofibular ligament, (4) cervical ligament, and (5) lateral talocalcaneal ligament. Reprinted with permission of Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508; Lippincott Williams & Wilkins.41
The bifurcate ligament also deserves mention as a static supporter of the lateral ankle complex. It consists of 2 branches: (1) dorsal calcaneocuboid, and (2) dorsal calcaneonavicular. This ligament resists supination of the midfoot and is often injured in conjuction with hypersupination mechanisms associated with lateral ankle sprain.34
Distal Tibiofibular Joint Anatomy
The third joint of the ankle complex is the distal articulation between the tibia and fibula. This joint is a syndesmosis that allows limited movement between the 2 bones; however, accessory gliding at this joint is crucial to normal mechanics throughout the entire ankle complex.44 The joint is stabilized by a thick interosseous membrane and the anterior and posterior inferior tibiofibular ligaments. The structural integrity of the sydesmosis is necessary to form the stable roof for the mortise of the talocrural joint. The anterior inferior tibiofibular ligament is often injured in conjunction with eversion injuries, and damage results in the so-called high ankle sprain rather than the more common lateral ankle sprain.45
Muscles and Tendons
When contracted, musculotendinous units generate stiffness, which leads to dynamic protection of joints. The muscles that cross the ankle complex are often described based on their concentric actions; however, when considering their role in providing dynamic stability to joints, it may be helpful to think about eccentric functions. The peroneal longus and brevis muscles are integral to the control of supination of the rearfoot and protection against lateral ankle sprains.46
In addition to the peroneals, the muscles of the anterior compartment of the lower leg (anterior tibialis, extensor digitorum longus, extensor digitorum brevis, and peroneus tertius) may also contribute to the dynamic stability of the lateral ankle complex by contracting eccentrically during forced supination of the rearfoot. Specifically, these muscles may be able to slow the plantar-flexion component of supination and thus prevent injury to the lateral ligaments.47
Innervation
The motor and sensory supplies to the ankle complex stem from the lumbar and sacral plexes. The motor supply to the muscles comes from the tibial, deep peroneal, and superficial peroneal nerves. The sensory supply comes from these 3 mixed nerves and 2 sensory nerves: the sural and saphenous nerves. The lateral ligaments and joint capsule of the talocrural and subtalar joints have been shown to be extensively innervated by mechanoreceptors that contribute to proprioception.37,48,49 The major importance of muscle spindles, especially of those in the peroneal muscles, to proprioception about the ankle complex has been described.50
PATHOMECHANICS OF ACUTE LATERAL ANKLE SPRAIN
Lateral ankle sprains most commonly occur due to excessive supination of the rearfoot about an externally rotated lower leg soon after initial contact of the rearfoot during gait or landing from a jump.5,7 Excessive inversion and internal rotation of the rearfoot, coupled with external rotation of the lower leg, results in strain to the lateral ankle ligaments. If the strain in any of the ligaments exceeds the tensile strength of the tissues, ligamentous damage occurs. Increased plantar flexion at initial contact appears to increase the likelihood of suffering a lateral ankle sprain.51
The ATFL is the first ligament to be damaged during a lateral ankle sprain, followed most often by the CFL.52,53 Cadaveric-sectioning studies have demonstrated that after the ATFL is ruptured, the amount of transverse-plane motion (internal rotation) of the rearfoot increases substantially, thus further stressing the remaining intact ligaments.39 This phenomenon has been described as “rotational instability” of the ankle and is often overlooked when considering laxity patterns in the sprained ankle.54 Concurrent damage to the talocrural joint capsule and the ligamentous stabilizers of the subtalar joint is also common with lateral ankle sprains. Martin et al55 demonstrated significantly greater strain in the cervical ligament after complete disruption to the CFL. The incidence of subtalar joint injury has been reported to be as high as 80% among patients suffering acute lateral ankle sprains.56 Injury to the PTFL is typical only in severe ankle sprains and is often accompanied by fractures or dislocations or both.57
A pathomechanical model described by Fuller58 suggested that the cause of lateral ankle sprain is an increased supination moment at the subtalar joint. The increased supination moment is caused by the position and magnitude of the vertically projected ground-reaction force at initial foot contact. Fuller hypothesized that a foot with its center of pressure (COP) medial to the subtalar-joint axis has a greater supination moment from the vertical ground-reaction force than a foot with a more lateral relationship between the COP and the joint axis.58 This increased supination moment could thus cause excessive inversion and internal rotation of the rearfoot in the closed kinetic chain and potentially lead to injury of the lateral ligaments. Individuals with a rigid supinated foot would be expected to have a more laterally deviated subtalar axis of rotation and a calcaneal varus (inverted rearfoot) malalignment, which could predispose those with a rigid supinated foot to lateral ankle sprains.
Inman38 described great variation in the alignment of the subtalar-joint axis across individuals, and it is possible that those with a more laterally deviated subtalar-joint axis may be predisposed to recurrent ankle sprains. A foot with a laterally deviated subtalar-joint axis would have a greater area on the medial side of the joint axis. Thus, during initial foot contact, the likelihood is greater that COP would be medial to the subtalar-joint axis and the ground-reaction force would cause a supination moment at the subtalar joint. Additionally, the further medial the COP is in relation to the subtalar-joint axis, the longer the supination moment arm is. If the magnitude of this supination moment exceeds the magnitude of a compensatory pronation moment (produced by the peroneal muscles and the lateral ligaments), excessive inversion and internal rotation of the rearfoot occur, likely causing injury to the lateral ligaments.58
Some have questioned whether the peroneal muscles are able to respond quickly enough to protect the lateral ligaments from being injured once the ankle begins rapid inversion.59,60 Ashton-Miller et al46 estimated that the span of the inversion motion upon landing may be as short as 40 milliseconds. Konradsen et al60 reported that a dynamic protective reaction from the peroneal muscles would take at least 126 milliseconds to occur after sudden, unexpected inversion perturbation of the ankle. This includes 54 milliseconds for reaction time of initial electromyographic activity after the onset of inversion perturbation and 72 milliseconds of electromechanical delay needed to generate force in the muscle after electromyographic activity has been initiated.60 This value assumes no preparatory electromyographic activity in the peroneal muscles before initial contact of the heel with the ground. In fact, the peroneal muscles are active before initial foot contact during stair descent61 and landing after a jump.62 This preparatory activity, along with similar activity in the other muscle groups that cross the ankle, is likely to create stiffness in tendons before initial foot contact with the ground.47,63 If the peroneal muscles are to protect against unexpected inversion of the rearfoot, preparatory muscle activation before foot contact with the ground is necessary.47,60
Relatively few research reports in the literature have described predispositions to first-time ankle sprains. Structural predispositions included increased tibial varum64 and nonpathologic talar tilt,64 whereas functional predispositions included poor postural-control performance,65,66 impaired proprioception,67 and higher eversion-to-inversion and plantar flexion-to-dorsiflexion strength ratios.68 Further research into prevention programs based on these predisposing factors is clearly warranted.
After acute injury, the ankle typically becomes swollen, tender, and painful with movement and full weight bearing. Depending on the severity of the injury, function usually returns over the course of a few days to a few months. What remains elusive to clinicians and researchers is why most individuals who suffer an initial ankle sprain are prone to recurrent sprains.
PATHOMECHANICS OF CHRONIC INSTABILITY
The mechanism of recurrent ankle injury is not thought to be different than that of initial acute ankle sprains; however, adverse changes that occur after primary injury are believed to predispose individuals to recurrent sprains.54 Two theories of the cause of CAI have traditionally been postulated: mechanical instability and functional instability. These 2 terms, however, do not adequately describe the full spectrum of abnormal conditions related to CAI. By further clarifying the potential insufficiencies leading to each type of instability, we can better describe the full complement of potential causes of CAI. Mechanical instability and functional instability are probably not mutually exclusive entities but more likely form a continuum of pathologic contributions to CAI (Figure 5).
Figure 5.
Paradigm of mechanical and functional insufficiencies that contribute to chronic ankle instability.
Mechanical Instability
Mechanical instability of the ankle complex occurs as a result of anatomic changes after initial ankle sprain, which lead to insufficiencies that predispose the ankle to further episodes of instability. These changes include pathologic laxity, impaired arthrokinematics, synovial changes, and the development of degenerative joint disease, which may occur in combination or isolation.
Pathologic Laxity. Ligamentous damage often results in pathologic laxity of injured joints, thus causing these joints to be mechanically unstable. The extent of pathologic laxity of the ankle depends on the amount of ligamentous damage to the lateral ligaments. Pathologic laxity can result in joint instability when the ankle is put in vulnerable positions during functional activities, resulting in subsequent injury to joint structures. Pathologic laxity may be assessed clinically with physical examination, stress radiography,69,70 or instrumented arthrometry.71,72 After lateral ankle sprain, pathologic laxity most often occurs in the talocrural and subtalar joints.69
Talocrural instability is caused primarily by injury to the ATFL and CFL.73 Injury to the ATFL is often assessed by determining the amount of anterior displacement of the talus from the tibiofibular mortise using an anterior drawer test. Integrity of the ATFL may also be assessed by inverting the talus with the talocrural joint in a plantar-flexed position and determining the amount of talar tilt present. Calcaneofibular ligament integrity is best assessed by determining the amount of talar tilt present when inverting the rearfoot with the talocrural joint in a dorsiflexed position. The amount of inversion talar tilt assessed with stress radiography increases dramatically with combined lesions of the ATFL and CFL.32 Whereas pathologic laxity is often present in those with CAI, 11% of healthy individuals also have asymmetric ankle laxity as assessed by the anterior drawer and talar tilt tests.74
Mechanical instability of the talocrural joint is traditionally explained in single planes, although this disregards the normal triplanar movement allowed at this joint. An excessive anterior drawer represents laxity in the transverse plane, while increased talar tilt indicates laxity in the frontal plane. These simplifications disregard the fact that the talocrural joint normally moves about a triplanar axis and ignore the issue of rotary instability of the talocrural joint. Specifically, in the absence of an intact ATFL, the talus is able to excessively supinate, with a large internal-rotation component in relation to the tibia.75 Comprehensive assessment of the unstable talocrural joint should focus on uniplanar and triplanar instability patterns.
Injury to the CFL also causes pathologic laxity of the subtalar and talocrural joints. On arthrography, many injuries to the CFL are accompanied by injury to the subtalar-joint capsule, cervical ligament, and other lateral ligaments.56,76 Rupture of the LTCL has also been implicated in chronic instability of the lateral subtalar joint.42 Stress radiography has been used to quantify the amount of subtalar tilt77,78 and anterior displacement of the calcaneus from the talus,79 although the validity of the most common method used for these assessments, the modified Broden view, has been challenged.80 Hertel et al41 described the medial subtalar glide test, which assesses the amount of medial translation of the calcaneus on the talus in the transverse plane (Figure 6). The results of the medial subtalar glide test compared favorably with the results of stress radiography.41
Figure 6.
The medial subtalar glide test is performed by translating the calcaneus medially in the transverse plane. Reprinted with permission of Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508; Lippincott Williams & Wilkins.41
Arthrokinematic Impairments. Another potential insufficiency contributing to mechanical instability of the ankle is impaired arthrokinematics at any of the 3 joints of the ankle complex. One arthrokinematic restriction related to repetitive ankle sprains involves a positional fault at the inferior tibiofibular joint. Mulligan44 suggested that individuals with CAI may have an anteriorly and inferiorly displaced distal fibula. If the lateral malleolus is indeed stuck in this displaced position, the ATFL may be more slack in its resting position. Thus, when the rearfoot begins to supinate, the talus can go through a greater range of motion before the ATFL becomes taut. This positional fault of the fibula may result in episodes of recurrent instability, leading to repetitive ankle sprains. The findings of 2 case studies81,82 and one pilot study83 present preliminary evidence for restriction of posterior fibular glide after lateral ankle sprain, suggesting that the lateral malleolus may be subluxated in an anteriorly displaced position.
Hypomobility, or diminished range of motion, may also be thought of as a mechanical insufficiency. Restricted dorsiflexion range of motion is thought to be a predisposition to lateral ankle sprain.84 If the talocrural joint is not able to fully dorsiflex, the joint will not reach its closed-pack position during stance and, therefore, will be able to invert and internally rotate more easily. Limited dorsiflexion in the closed kinetic chain is also typically compensated for by increased subtalar pronation. Some evidence demonstrates dorsiflexion restrictions in athletes with repetitive ankle sprains.85,86 Greene et al87 recently demonstrated that altered arthrokinematics may limit dorsiflexion after acute ankle sprain. Patients with acute ankle sprains who were treated with posterior mobilization of the talus on the tibia recovered their dorsiflexion range of motion more quickly than those not treated with joint mobilization. Denegar et al88 found restricted posterior talar glide in athletes 12 weeks after acute ankle sprain. Interestingly, these athletes did not have significantly decreased dorsiflexion range of motion as assessed through standard clinical measures. This suggests that dorsiflexion may be returned to normal ranges in the absence of normal arthrokinematics due to extensive stretching of the triceps surae. Further research is needed to elucidate the clinical implications of altered arthrokinematics after ankle sprain.
Synovial and Degenerative Changes. Mechanical instability of the ankle complex may also occur due to insufficiencies caused by synovial hypertrophy and impingement or the development of degenerative joint lesions. Synovial inflammation has been shown in the talocrural and posterior subtalar-joint capsules. Patients with synovial inflammation often report frequent episodes of pain and recurrent ankle instability, which are due to impingement of hypertrophied synovial tissue between the respective bones of the ankle complex. DiGiovanni et al89 identified anterolateral impingement syndrome of the talocrural joint in 67% and talocrural synovitis in 49% of patients requiring surgery for lateral instability. Sinus tarsi syndrome, or synovitis of the lateral aspect of the posterior subtalar joint, often occurs as a sequela to repetitive bouts of ankle instability.43,90
Repetitive bouts of ankle instability have also been related to degenerative changes in the ankle complex.10 Individuals undergoing surgery for ankle-ligament repair were 3.37 times more likely to have osteophytes, or loose bodies, than those with asymptomatic ankles.74 Similarly, Gross and Marti11 demonstrated more osteophytes and subchondral sclerosis in volleyball players with a history of repetitive ankle sprains compared with a group of healthy controls. Greater varus angulation of the tibial plafond has also been identified in subjects with CAI when compared with those suffering initial acute sprains.91 It is unclear whether this is a developmental change in response to numerous bouts of ankle instability or a structural predisposition to recurrent ankle sprains.
Functional Instability
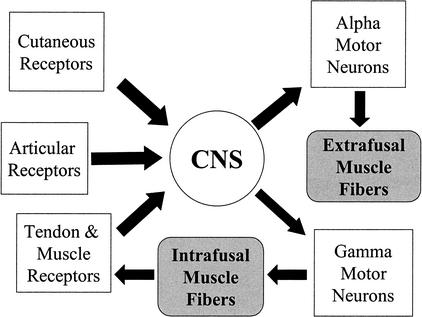
Injury to the lateral ligaments of the ankle results in adverse changes to the neuromuscular system that provides dynamic support to the ankle. Freeman et al16,17 first described the concept of functional instability in 1965. They attributed impaired balance in individuals with lateral ankle sprains to damaged articular mechanoreceptors in the lateral ankle ligaments, which resulted in proprioceptive deficits. The contribution of impaired proprioception, while important, does not fully explain why ankle-ligament injury predisposes athletes to functional ankle instability. The pathoetiologic model is not complete without including impaired neuromuscular control, thus resulting in inadequacies of the dynamic defense mechanism protecting against hypersupination of the rearfoot.92 Figure 7 illustrates the links between proprioception and neuromuscular control of joint stability. Over the past 2 decades, functional insufficiencies among individuals with either acute ankle sprains or CAI have been demonstrated by quantifying deficits in ankle proprioception, cutaneous sensation, nerve-conduction velocity, neuromuscular response times, postural control, and strength.
Figure 7.
Paradigm of proprioception and neuromuscular control. CNS indicates central nervous system.
Impaired Proprioception and Sensation. Proprioception at the ankle is impaired in individuals prone to repetitive ankle sprains on measures of kinesthesia93–95 and active replication of joint angles.96–98 While Gross99 did not find significant differences in active and passive replication of joint angles in subjects with unilateral CAI, most studies assessing proprioception in subjects with CAI demonstrate impairments. Recent evidence suggests that alteration in muscle-spindle activity in the peroneal muscles may be more important than altered articular mechanoreceptor activity in the manifestation of proprioceptive deficits at the ankle.50 The clinical relevance of proprioceptive deficits is not fully understood at this time, and whether proprioception is improved through rehabilitation exercises has not yet been conclusively demonstrated.100
Impaired cutaneous sensation101–104 and slowed nerve-conduction velocity102,105 have been reported as indicators of common peroneal nerve palsy after acute lateral ankle sprain, but no evidence exists that such impairments are present in patients with CAI. Further research in this area is warranted.
Impaired Neuromuscular-Firing Patterns. Impaired neuromuscular-recruitment patterns have been demonstrated in individuals with a history of repetitive lateral ankle sprain.104,106–111 This has been most commonly shown by assessing the reflexive response times of the peroneal muscles to inversion or supination perturbations. Conflicting results in the literature may be due to methodologic differences among investigators.59,112–116 If peroneal response is impaired in those with CAI, it may be due to impaired proprioception, slowed nerve-conduction velocity, or central impairments in neuromuscular-recruitment strategies. Evidence of the latter was presented by Bullock-Saxton et al,111 who found bilateral deficits of gluteus medius recruitment in subjects with a history of severe unilateral ankle sprain. This finding suggests that neuromuscular impairments are not only present in structures that cross the affected ankle but also exist along other neuromuscular pathways in both limbs, thus indicating central neural adaptations to peripheral joint conditions.
Impaired Postural Control. Impaired postural control during single-leg stance has been demonstrated frequently in individuals after acute ankle sprain16–17,104,117–126 and in those with a history of repetitive ankle sprains.21,93,127–132 Noninstrumented assessment of the modified Romberg test has been performed by having subjects stand as motionless as possible on one leg for a period usually ranging from 10 to 30 seconds. This task is performed while standing on the involved limb and then the uninvolved limb, first with eyes open and then with eyes closed. Both the subject and the examiner make a subjective judgment as to which limb either feels or appears to cause greater postural instability. Subjective assessment of postural control has consistently identified functional insufficiencies in those with chronically unstable ankles.16,17,93,129,132
Instrumented assessment of postural control has also been used to discriminate between functionally stable and unstable ankles. Piezoelectric force plates allow for assessment of the COP during single-leg standing. Two very common dependent measures of postural control include the overall length of the path of COP and the velocity of COP excursions during the duration of an entire trial of single-leg standing. Shorter length of COP displacement and slower velocity of COP excursions are associated with better postural control. Dozens of dependent measures of postural control have been reported related to balance deficits and ankle instability. Despite varying methods, postural-control deficits have consistently been demonstrated between stable and unstable ankles when using instrumented assessment, although conflicting findings exist.65,133–136
Postural-control deficits are likely due to a combination of impaired proprioception and neuromuscular control. When balancing in single-leg stance, the foot pronates and supinates in an effort to keep the body's center of gravity above the base of support. This is referred to as the “ankle strategy” of postural control. Individuals with CAI have been shown to use more of a “hip strategy” to maintain unilateral stance than uninjured individuals.137 The hip strategy is less efficient than the ankle strategy in maintaining unilateral stance. This alteration in postural-control strategy is likely due to changes in central neural control that occur in the presence of ankle-joint dysfunction. Further evidence of central changes in neuromuscular control were presented by Friden et al,117 who found bilateral impairment of postural control in subjects with acute ankle sprains.
Interestingly, side-to-side differences in postural control often return to insignificant levels in the weeks and months after initial injury, whether structured rehabilitation programs are adhered to or not.118,126,138 Holme et al126 reported that 4 months after acute ankle sprain, both subjects who did and those who did not perform a comprehensive rehabilitation program emphasizing balance and coordination exercises showed no significant postural-control deficits. However, subjects who did not undergo rehabilitation were more than twice as likely to suffer recurrent sprains than those who did rehabilitate their ankles. Thus, while quantification of postural control may not be able to predict those at risk of recurrent sprain in all instances, retraining of postural control after ankle sprain is nonetheless advantageous.
Strength Deficits. Strength deficits have been reported among individuals with CAI.20,139–142 Diminished strength has been reported for both eversion20,139,141,142 and inversion,140,142 although reports of no strength deficits also exist.95,132,134,143 Assuming that strength deficits do exist in some patients with CAI, the reason for such impairments is unclear. Is this weakness due to muscle damage or atrophy? Or could deficits be due to impaired neuromuscular recruitment in the presence of ankle-joint abnormality and, therefore, be causing functional insufficiency in the dynamic defense mechanism? Further research is needed to elucidate the role of strength deficits in CAI.
Relationships Between Functional Insufficiencies
The individual symptoms of functional ankle instability do not occur in isolation but are likely all components of a complex pathoetiologic paradigm. Joint injury results in proprioceptive decrements, which also lead to impairments in neuromuscular control. These changes limit the dynamic defense system of the ankle and predispose the ankle to recurrent episodes of instability. Altered muscle-spindle activity, as mediated through the γ-motoneuron system, may be the keystone to these interrelated symptoms.50 Figure 7 illustrates the feedback loop among the somatosensory system, the central nervous system, and the α- and γ-motoneuron systems. The key to treating functional insufficiency may lie in restoration of normal γ-motoneuron activity.
Relationships Between Mechanical and Functional Insufficiencies
The interactions between mechanical insufficiency and functional insufficiency and the relationships between the specific insufficiencies have not been clearly elucidated. Research is needed to examine the relationships between mechanical and functional insufficiencies and the effects of common treatment strategies on both types of insufficiency. While this new model of functional and mechanical insufficiency helps to explain the causative spectrum related to CAI, further developments are needed to improve the clinical outcomes of athletes who suffer from lateral ankle instability.
An example of an assessment technique that evaluates multiple insufficiencies is the Star Excursion Balance Tests. These tests are a series of dynamic postural-control tasks that require stabilization on one lower limb and a functional reach with the contralateral lower limb in different directions. In order to optimally execute these tasks, adequate postural control, strength, and range of motion must be present. Olmsted et al144 demonstrated impairment in performance on the Star Excursion Balance Tests among a group of athletes with CAI. Further research is needed to identify which specific mechanical and functional insufficiencies are related to such impaired performance on these tests of dynamic balance. The development of more evaluation tools will allow the assessment of multiple insufficiencies simultaneously during functional activities.
Prevention of Chronic Instability
The natural progression of acute ankle sprains is for subjects to report gradual improvement as the initial symptoms of pain, swelling, and loss of function subside in the weeks after injury.136 The conundrum facing clinicians is how to convince patients with an ankle sprain that is improving that they need to continue rehabilitation for several weeks or months after their initial symptoms have subsided. Comprehensive rehabilitation programs that emphasize proprioceptive, neuromuscular control, and balance training significantly reduce the risk of recurrent ankle sprains.126,145,146 While ankle taping and bracing also appear to be effective in preventing repetitive ankle sprains,145,147,148 it is unlikely that ankle taping or bracing alone is as effective as completion of a comprehensive rehabilitation program in combination with taping or bracing. Preventive measures to reduce the incidence of recurrent sprains must address pathologic laxity, arthrokinematic changes, and other mechanical insufficiencies related to mechanical instability and the proprioceptive and neuromuscular deficits seen with functional instability.
CONCLUSIONS
Lateral ankle sprains are among the most common injury seen in physically active populations, yet the treatment strategies being used by clinicians appear to be inadequate in preventing recurrence of these injuries. Appreciating the anatomy and mechanics of the rearfoot complex aids in understanding the pathomechanics of lateral ankle sprains and CAI. Mechanical instability of the ankle may be due to the specific insufficiencies of pathologic laxity, arthrokinematic restrictions, synovial irritation, or degenerative changes to the joints of the ankle complex. Functional instability is driven by insufficiencies in proprioception, neuromuscular control, postural control, and strength. The clinical management of patients with unstable ankles should include identifying symptoms of both mechanical and functional instabilities. Once specific insufficiencies have been identified, treatment efforts should focus on addressing these impairments and emphasis should be placed on reducing the risk of recurrent ankle sprains.
REFERENCES
- Garrick J G. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- Hosea T M, Carey C C, Harrer M F. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop. 2000;372:45–49. doi: 10.1097/00003086-200003000-00006. [DOI] [PubMed] [Google Scholar]
- Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle: operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305–312. [PubMed] [Google Scholar]
- Smith R W, Reischl S F. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- Ekstrand J, Tropp H. The incidence of ankle sprains in soccer. Foot Ankle. 1990;11:41–44. doi: 10.1177/107110079001100108. [DOI] [PubMed] [Google Scholar]
- Milgrom C, Shlamkovitch N, Finestone A, et al. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991;12:26–30. doi: 10.1177/107110079101200105. [DOI] [PubMed] [Google Scholar]
- Bahr R, Bahr I A. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7:166–171. doi: 10.1111/j.1600-0838.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- McKay G D, Goldie P A, Payne W R, Oakes B W. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung M S, Chan K M, So C H, Yuan W Y. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington K D. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61:354–361. [PubMed] [Google Scholar]
- Gross P, Marti B. Risk of degenerative ankle joint disease in volleyball players: study of former elite athletes. Int J Sports Med. 1999;20:58–63. doi: 10.1055/s-2007-971094. [DOI] [PubMed] [Google Scholar]
- Gerber J P, Williams G N, Scoville C R, Arciero R A, Taylor D C. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19:653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- Braun B L. Effects of ankle sprain in a general clinical population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8:143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- Fallat L, Grimm D J, Saracco J A. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37:280–285. doi: 10.1016/s1067-2516(98)80063-x. [DOI] [PubMed] [Google Scholar]
- Verhagen R A, de Keizer G, van Dijk C N. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114:92–96. doi: 10.1007/BF00422833. [DOI] [PubMed] [Google Scholar]
- Freeman M AR. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- Freeman M AR, Dean M RE, Hanham I WF. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Brand R L, Black H M, Cox J S. The natural history of the inadequately treated ankle sprain. Am J Sports Med. 1977;5:248–249. doi: 10.1177/036354657700500609. [DOI] [PubMed] [Google Scholar]
- Renstrom P AFH, Konradsen L. Ankle ligament injuries. Br J Sports Med. 1997;31:11–20. doi: 10.1136/bjsm.31.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosien W R, Staples O S, Russell S W. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37:1237–1243. [PubMed] [Google Scholar]
- Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- Wilkerson G B, Nitz A J. Dynamic ankle stability: mechanical and neuromuscular interrelationships. J Sport Rehabil. 1994;3:43–57. [Google Scholar]
- Huson A. Joints and movements of the foot: terminology and concepts. Acta Morphol Neerl Scand. 1987;25:117–130. [PubMed] [Google Scholar]
- Rockar P A., Jr The subtalar joint: anatomy and joint motion. J Orthop Sports Phys Ther. 1995;21:361–372. doi: 10.2519/jospt.1995.21.6.361. [DOI] [PubMed] [Google Scholar]
- Lundberg A, Goldie I, Kalin B, Selvik G. Kinematics of the ankle/foot complex: plantarflexion and dorsiflexion. Foot Ankle. 1989;9:194–200. doi: 10.1177/107110078900900409. [DOI] [PubMed] [Google Scholar]
- Stormont D M, Morrey B F, An K N, Cass J R. Stability of the loaded ankle: relation between articular restraint and primary and secondary static restraints. Am J Sports Med. 1985;13:295–300. doi: 10.1177/036354658501300502. [DOI] [PubMed] [Google Scholar]
- Burks R T, Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22:72–77. doi: 10.1177/036354659402200113. [DOI] [PubMed] [Google Scholar]
- Renstrom P, Wertz M, Incavo S, Pope M, Ostgaard H C, Arms S, Haugh L. Strain in the lateral ligaments of the ankle. Foot Ankle. 1988;9:59–63. doi: 10.1177/107110078800900201. [DOI] [PubMed] [Google Scholar]
- Stephens M M, Sammarco G J. The stabilizing role of the lateral ligament complex around the ankle and subtalar joints. Foot Ankle. 1992;13:130–136. doi: 10.1177/107110079201300304. [DOI] [PubMed] [Google Scholar]
- Cass J R, Settles H. Ankle instability: in vitro kinematics in response to axial load. Foot Ankle Int. 1994;15:134–140. doi: 10.1177/107110079401500308. [DOI] [PubMed] [Google Scholar]
- Hollis J M, Blasier R D, Flahiff C M. Simulated lateral ankle ligamentous injury: change in ankle stability. Am J Sports Med. 1995;23:672–677. doi: 10.1177/036354659502300606. [DOI] [PubMed] [Google Scholar]
- Attarian D E, McCrackin H J, DeVito D P, McElhaney J H, Garrett W E., Jr Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985;6:54–58. doi: 10.1177/107110078500600202. [DOI] [PubMed] [Google Scholar]
- Holmer P, Sondergaard L, Konradsen L, Nielsen P T, Jorgensen L N. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle. 1994;15:72–74. doi: 10.1177/107110079401500204. [DOI] [PubMed] [Google Scholar]
- Kjaersgaard-Andersen P, Wethelund J O, Helmig P, Nielsen S. Effect of the calcaneofibular ligament on hindfoot rotation in amputation specimens. Acta Orthop Scand. 1987;58:135–138. doi: 10.3109/17453678709146459. [DOI] [PubMed] [Google Scholar]
- Perry J. Anatomy and biomechanics of the hindfoot. Clin Orthop. 1983;177:9–15. [PubMed] [Google Scholar]
- Viladot A, Lorenzo J C, Salazar J, Rodriguez A. The subtalar joint: embryology and morphology. Foot Ankle. 1984;5:54–66. doi: 10.1177/107110078400500203. [DOI] [PubMed] [Google Scholar]
- Inman V T. Williams & Wilkins; Baltimore, MD: 1976. The Joints of the Ankle. [Google Scholar]
- Kjaersgaard-Andersen P, Wethelund J O, Helmig P, Soballe K. The stabilizing effect of the ligamentous structures in the sinus and canalis tarsi on movements in the hindfoot: an experimental study. Am J Sports Med. 1988;16:512–516. doi: 10.1177/036354658801600514. [DOI] [PubMed] [Google Scholar]
- Harper M C. The lateral ligamentous support of the subtalar joint. Foot Ankle. 1991;11:354–358. doi: 10.1177/107110079101100604. [DOI] [PubMed] [Google Scholar]
- Hertel J, Denegar C R, Monroe M M, Stokes W L. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508. doi: 10.1097/00005768-199911000-00002. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Eriksson B I, Renstrom P A. Subtalar ankle instability: a review. Sports Med. 1997;5:337–346. doi: 10.2165/00007256-199724050-00005. [DOI] [PubMed] [Google Scholar]
- Meyer J M, Lagier R. Post-traumatic sinus tarsi syndrome: an anatomical and radiological study. Acta Orthop Scand. 1977;48:121–128. doi: 10.3109/17453677708985122. [DOI] [PubMed] [Google Scholar]
- Mulligan B R. 3rd ed Plane View Services LTD; Wellington, New Zealand: 1995. Manual Therapy: “NAGS”, “SNAGS”, “MWMS”, Etc. [Google Scholar]
- Miller C D, Shelton W R, Barrett G R, Savoie F H, Dukes A D. Deltoid and syndesmosis ligament injury of the ankle without fracture. Am J Sports Med. 1995;23:746–750. doi: 10.1177/036354659502300618. [DOI] [PubMed] [Google Scholar]
- Ashton-Miller J A, Ottaviani R A, Hutchinson C, Wojtys E M. What best protects the inverted weightbearing ankle against further inversion? Evertor muscle strength compares favorably with shoe height, athletic tape, and three orthoses. Am J Sports Med. 1996;24:800–809. doi: 10.1177/036354659602400616. [DOI] [PubMed] [Google Scholar]
- Sinkjaer T, Toft E, Andreassen S, Hornemann B C. Muscle stiffness in human ankle dorsiflexors: intrinsic and reflex components. J Neurophysiol. 1988;60:1110–1121. doi: 10.1152/jn.1988.60.3.1110. [DOI] [PubMed] [Google Scholar]
- Michelson J D, Hutchins C. Mechanoreceptors in human ankle ligaments. J Bone Joint Surg Br. 1995;77:219–224. [PubMed] [Google Scholar]
- Takebayashi T, Yamashita T, Minaki Y, Ishii S. Mechanosensitive afferent units in the lateral ligament of the ankle. J Bone Joint Surg Br. 1997;79:490–493. doi: 10.1302/0301-620x.79b3.7285. [DOI] [PubMed] [Google Scholar]
- Khin-Myo-Hla, Ishii T, Sakane M, Hayashi K. Effect of anesthesia of the sinus tarsi on peroneal reaction time in patients with functional instability of the ankle. Foot Ankle Int. 1999;20:554–559. doi: 10.1177/107110079902000903. [DOI] [PubMed] [Google Scholar]
- Wright I C, Neptune R R, van den Bogert A J, Nigg B M. The influence of foot positioning on ankle sprains. J Biomech. 2000;33:513–519. doi: 10.1016/s0021-9290(99)00218-3. [DOI] [PubMed] [Google Scholar]
- Broström L. Sprained ankles: I, anatomic lesions on recent sprains. Acta Chir Scand. 1964;128:483–495. [PubMed] [Google Scholar]
- Staples O S. Rupture of the fibular collateral ligaments of the ankle: result study of immediate surgical treatment. J Bone Joint Surg Am. 1975;57:101–107. [PubMed] [Google Scholar]
- Hintermann B. Biomechanics of the unstable ankle joint and clinical implications. Med Sci Sports Exerc. 1999;31(suppl 7):459–469. doi: 10.1097/00005768-199907001-00007. [DOI] [PubMed] [Google Scholar]
- Martin L P, Wayne J S, Monahan T J, Adelaar R S. Elongation behavior of calcaneofibular and cervical ligaments during inversion loads applied in an open kinetic chain. Foot Ankle Int. 1998;19:232–239. doi: 10.1177/107110079801900409. [DOI] [PubMed] [Google Scholar]
- Meyer J M, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain: a roentgenographic study. Clin Orthop. 1986;226:169–173. [PubMed] [Google Scholar]
- Safran M R, Benedetti R S, Bartolozzi A R, III, Mandelbaum B R. Lateral ankle sprains: a comprehensive review, part I: etiology, pathoanatomy, histopathogenesis, and diagnosis. Med Sci Sports Exerc. 1999;31(suppl 7):429–437. doi: 10.1097/00005768-199907001-00004. [DOI] [PubMed] [Google Scholar]
- Fuller E A. Center of pressure and its theoretical relationship to foot pathology. J Am Podiatr Med Assoc. 1999;89:278–291. doi: 10.7547/87507315-89-6-278. [DOI] [PubMed] [Google Scholar]
- Isakov E, Mizrahi J, Solzi P, Susak Z, Lotem M. Response of the peroneal muscles to sudden inversion stress during standing. Int J Sport Biomech. 1986;2:100–106. [Google Scholar]
- Konradsen L, Voigt M, Hojsgaard C. Ankle inversion injuries: the role of the dynamic defense mechanism. Am J Sports Med. 1997;25:54–58. doi: 10.1177/036354659702500110. [DOI] [PubMed] [Google Scholar]
- Greenwood R, Hopkins A. Landing from an unexpected fall and a voluntary step. Brain. 1976;99:375–386. doi: 10.1093/brain/99.2.375. [DOI] [PubMed] [Google Scholar]
- Dyhre-Poulsen P, Simonsen E B, Voigt M. Dynamic control of muscle stiffness and H reflex modulation during hopping and jumping in man. J Physiol. 1991;437:287–304. doi: 10.1113/jphysiol.1991.sp018596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz V. Human neuronal control of automatic functional movements: interaction between central programs and afferent input. Physiol Rev. 1992;72:33–69. doi: 10.1152/physrev.1992.72.1.33. [DOI] [PubMed] [Google Scholar]
- Beynnon B D, Renström P A, Alosa D M, Baumhauer J F, Vacek P M. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;9:213–220. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sport Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- McGuine T A, Greene J J, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- Payne K A, Berg K, Latin R W. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train. 1997;32:221–225. [PMC free article] [PubMed] [Google Scholar]
- Baumhauer J F, Alosa D M, Renstrom A F, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- Martin D E, Kaplan P A, Kahler D M, Dussault R, Randolph B J. Retrospective evaluation of graded stress examination of the ankle. Clin Orthop. 1996;328:165–170. doi: 10.1097/00003086-199607000-00026. [DOI] [PubMed] [Google Scholar]
- Frost S C, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9:40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- Kovaleski J E, Gurchiek L R, Heitman R J, Hollis J M, Pearsall A W., IV Instrumented measurement of anteroposterior and inversion-eversion laxity of the normal ankle joint complex. Foot Ankle Int. 1999;20:808–814. doi: 10.1177/107110079902001210. [DOI] [PubMed] [Google Scholar]
- Liu W, Siegler S, Techner L. Quantitative measurement of ankle passive flexibility using an arthrometer on sprained ankles. Clin Biomech (Bristol, Avon) 2001;16:237–244. doi: 10.1016/s0268-0033(00)00088-7. [DOI] [PubMed] [Google Scholar]
- Rasmussen O, Tovborg-Jensen I. Mobility of the ankle joint: recording of rotatory movements in the talocrural joint in vitro with and without the lateral collateral ligaments of the ankle. Acta Orthop Scand. 1982;53:155–160. doi: 10.3109/17453678208992194. [DOI] [PubMed] [Google Scholar]
- Scranton P E, Jr, McDermott J E, Rogers J V. The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot Ankle Int. 2000;21:657–664. doi: 10.1177/107110070002100805. [DOI] [PubMed] [Google Scholar]
- Bremer S W. The unstable ankle mortise–functional ankle varus. J Foot Surg. 1985;24:313–317. [PubMed] [Google Scholar]
- Sugimoto K, Samoto N, Takaoka T, Takakura Y, Tamai S. Subtalar arthrography in acute injuries of the calcaneofibular ligament. J Bone Joint Surg Br. 1998;80:785–790. doi: 10.1302/0301-620x.80b5.7921. [DOI] [PubMed] [Google Scholar]
- Harper M C. Stress radiographs in the diagnosis of lateral instability of the ankle and hindfoot. Foot Ankle. 1992;13:435–438. doi: 10.1177/107110079201300801. [DOI] [PubMed] [Google Scholar]
- van Hellemondt F J, Louwerens J WK, Sijbrandij E S, van Gils A PG. Stress radiography and stress examination of the talocrural and subtalar joint on helical computed tomography. Foot Ankle Int. 1997;18:482–488. doi: 10.1177/107110079701800805. [DOI] [PubMed] [Google Scholar]
- Ishii T, Miyagawa S, Fukubayashi T, Hayashi K. Subtalar stress radiography using forced dorsiflexion and supination. J Bone Joint Surg Br. 1996;78:56–60. [PubMed] [Google Scholar]
- Sijbrandij E S, van Gils A P, van Hellemondt F J, Louwerens J W, de Lange E E. Assessing the subtalar joint: the Broden view revisited. Foot Ankle Int. 2001;22:329–334. doi: 10.1177/107110070102200410. [DOI] [PubMed] [Google Scholar]
- Hetherington B. Lateral ligament strains of the ankle, do they exist? Man Ther. 1996;1:274–275. doi: 10.1054/math.1996.0279. [DOI] [PubMed] [Google Scholar]
- O'Brien T, Vicenzino B. A study of the effects of Mulligan's mobilization with movement treatment of lateral ankle pain using a case study design. Man Ther. 1998;3:78–84. [Google Scholar]
- Kavanagh J. Is there a positional fault at the inferior tibiofibular joint in patients with acute or chronic ankle sprains compared to normals? Man Ther. 1999;4:19–24. doi: 10.1016/s1356-689x(99)80005-8. [DOI] [PubMed] [Google Scholar]
- Tabrizi P, McIntyre W M, Quesnel M B, Howard A W. Limited dorsiflexion predisposes to injuries of the ankle in children. J Bone Joint Surg Br. 2000;82:1103–1106. doi: 10.1302/0301-620x.82b8.10134. [DOI] [PubMed] [Google Scholar]
- Leanderson J, Wykman A, Eriksson E. Ankle sprain and postural sway in basketball players. Knee Surg Sports Traumatol Arthrosc. 1993;1:203–205. doi: 10.1007/BF01560207. [DOI] [PubMed] [Google Scholar]
- Wiesler E R, Hunter D M, Martin D F, Curl W W, Hoen H. Ankle flexibility and injury patterns in dancers. Am J Sports Med. 1996;24:754–757. doi: 10.1177/036354659602400609. [DOI] [PubMed] [Google Scholar]
- Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81:984–994. [PubMed] [Google Scholar]
- Denegar C R, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32:166–173. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- DiGiovanni B F, Fraga C J, Cohen B E, Shereff M J. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809–815. doi: 10.1177/107110070002101003. [DOI] [PubMed] [Google Scholar]
- Taillard W, Meyer J M, Garcia J, Blanc Y. The sinus tarsi syndrome. Int Orthop. 1981;5:117–130. doi: 10.1007/BF00267842. [DOI] [PubMed] [Google Scholar]
- Sugimoto K, Samoto N, Takakura Y, Tamai S. Varus tilt of the tibial plafond as a factor in chronic ligament instability of the ankle. Foot Ankle Int. 1997;18:402–405. doi: 10.1177/107110079701800705. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Pincivero D M, Rozzi S L. Proprioception of the ankle and knee. Sports Med. 1998;25:149–155. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Forkin D M, Koczur C, Battle R, Newton R A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Docherty C L, Moore J H, Arnold B L. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33:310–314. [PMC free article] [PubMed] [Google Scholar]
- Konradsen L, Magnusson P. Increased inversion angle replication error in functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2000;8:246–251. doi: 10.1007/s001670000124. [DOI] [PubMed] [Google Scholar]
- Gross M T. Effects of recurrent lateral ankle sprains on active and passive judgements of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Ashton-Miller J A, Wojtys E M, Huston L J, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- Stoff M D, Greene A F. Common peroneal nerve palsy following inversion ankle injury: a report of two cases. Phys Ther. 1982;62:1463–1464. doi: 10.1093/ptj/62.10.1463. [DOI] [PubMed] [Google Scholar]
- Nitz A J, Dobner J J, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med. 1985;13:177–182. doi: 10.1177/036354658501300306. [DOI] [PubMed] [Google Scholar]
- Bullock-Saxton J E. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74:17–28. doi: 10.1093/ptj/74.1.17. [DOI] [PubMed] [Google Scholar]
- Bullock-Saxton J E. Sensory changes associated with severe ankle sprain. Scand J Rehabil Med. 1995;27:161–167. [PubMed] [Google Scholar]
- Kleinrensink G J, Stoeckart R, Meulstee J, et al. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med Sci Sports Exerc. 1994;26:877–883. [PubMed] [Google Scholar]
- Karlsson J, Andréasson G O. The effect of external ankle support in chronic lateral ankle joint instability: an electromyographic study. Am J Sports Med. 1992;20:257–261. doi: 10.1177/036354659202000304. [DOI] [PubMed] [Google Scholar]
- Brunt D, Anderson J C, Huntsman B, Reinhert L B, Thorell A C, Sterling J C. Postural responses to lateral perturbation in healthy subjects and ankle sprain patients. Med Sci Sports Exerc. 1992;24:171–176. [PubMed] [Google Scholar]
- Konradsen L, Ravn J B. Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand. 1990;61:388–390. doi: 10.3109/17453679008993546. [DOI] [PubMed] [Google Scholar]
- Lynch S A, Eklund U, Gottlieb D, Renström P A, Beynnon B. Electromyographic latency changes in the ankle musculature during inversion moments. Am J Sports Med. 1996;24:362–369. doi: 10.1177/036354659602400319. [DOI] [PubMed] [Google Scholar]
- Lofvenberg R, Karrholm J, Sundelin G, Ahlgren O. Prolonged reaction time in patients with chronic lateral instability of the ankle. Am J Sports Med. 1995;23:414–417. doi: 10.1177/036354659502300407. [DOI] [PubMed] [Google Scholar]
- Bullock-Saxton J E, Janda V, Bullock M I. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med. 1994;15:330–334. doi: 10.1055/s-2007-1021069. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Olesen S, Hansen H M. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26:72–77. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- Nawoczenski D A, Cook T M, Saltzman C L. The effect of foot orthotics on three-dimensional kinematics of the leg and rearfoot during running. J Orthop Sports Phys Ther. 1995;21:317–327. doi: 10.2519/jospt.1995.21.6.317. [DOI] [PubMed] [Google Scholar]
- Johnson M B, Johnson C L. Electromyographic response of peroneal muscles in surgical and nonsurgical injured ankles during sudden inversion. J Orthop Sports Phys Ther. 1993;18:497–501. doi: 10.2519/jospt.1993.18.3.497. [DOI] [PubMed] [Google Scholar]
- Ebig M, Lephart S M, Burdett R G, Miller M C, Pincivero D M. The effect of sudden inversion stress on EMG activity of the peroneal and tibialis anterior muscles in the chronically unstable ankle. J Orthop Sports Phys Ther. 1997;26:73–77. doi: 10.2519/jospt.1997.26.2.73. [DOI] [PubMed] [Google Scholar]
- Fernandes N, Allison G T, Hopper D. Peroneal latency in normal and injured ankles at varying angles of perturbation. Clin Orthop. 2000;375:193–201. doi: 10.1097/00003086-200006000-00023. [DOI] [PubMed] [Google Scholar]
- Friden T, Zatterstrom R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- Hertel J, Buckley W E, Denegar C R. Serial testing of postural control after acute lateral ankle sprain. J Athl Train. 2001;35:363–368. [PMC free article] [PubMed] [Google Scholar]
- Hertel J, Denegar C R, Buckley W E, Sharkey N A, Stokes W L. Effect of rearfoot orthotics on postural sway after lateral ankle sprain. Arch Phys Med Rehabil. 2001;82:1000–1003. doi: 10.1053/apmr.2001.22349. [DOI] [PubMed] [Google Scholar]
- Cornwall M W, Murrell P M. Postural sway following inversion sprain of the ankle. J Am Podiatr Med Assoc. 1991;81:243–247. doi: 10.7547/87507315-81-5-243. [DOI] [PubMed] [Google Scholar]
- Golomer E, Dupui P, Bessou P. Spectral frequency analysis of dynamic balance in healthy and injured athletes. Arch Int Physiol Biomech Biophys. 1994;102:225–229. doi: 10.3109/13813459409007543. [DOI] [PubMed] [Google Scholar]
- Goldie P A, Evans O M, Bach T M. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75:969–975. [PubMed] [Google Scholar]
- Guskiewicz K M, Perrin D H. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23:326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- Leanderson J, Eriksson E, Nilsson C. Proprioception in classical ballet dancers: a prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med. 1996;24:370–374. doi: 10.1177/036354659602400320. [DOI] [PubMed] [Google Scholar]
- Mattacola C G, Lloyd J W. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32:127–135. [PMC free article] [PubMed] [Google Scholar]
- Holme E, Magnusson S P, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- Forkin D M, Koczur C, Battle R, Newton R A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- Perrin P P, Bene M C, Perrin C A, Durupt D. Ankle trauma significantly impairs postural control—a study in basketball players and controls. Int J Sports Med. 1997;18:387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- Rozzi S L, Lephart S M, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- Lentell G L, Katzmann L L, Walters M R. The relationship between muscle function and ankle instability. J Orthop Sports Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle? Br J Sports Med. 1997;31:65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- Tropp H, Eckstrand J, Gillquist J. Factors affecting stabiliometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- Rose A, Lee R J, Williams R M, Thomson L C, Forsyth A. Functional instability in non-contact ankle ligament injuries. Br J Sports Med. 2000;34:352–358. doi: 10.1136/bjsm.34.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardized perturbations of single leg stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996;30:151–155. doi: 10.1136/bjsm.30.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leanderson J, Bergqvist M, Rolf C, Westblad P, Wigelius-Roovers S, Wredmark T. Early influence of an ankle sprain on objective measures of ankle joint function: a prospective randomised study of ankle brace treatment. Knee Surg Sports Traumatol Arthrosc. 1999;7:51–58. doi: 10.1007/s001670050120. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- Ryan L. Mechanical stability, muscle strength, and proprioception in the functionally unstable ankle. Aust J Physiother. 1994;40:41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- Bush K W. Predicting ankle sprain. J Manual Manip Ther. 1996;4:54–58. [Google Scholar]
- Hartsell H D, Spaulding S J. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med. 1999;33:255–258. doi: 10.1136/bjsm.33.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H, Gansneder B M. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34:239–245. [PMC free article] [PubMed] [Google Scholar]
- Olmsted L C, Carcia C R, Hertel J, Shultz S J. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37:501–506. [PMC free article] [PubMed] [Google Scholar]
- Verhagen E A, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med. 2000;10:291–296. doi: 10.1097/00042752-200010000-00012. [DOI] [PubMed] [Google Scholar]
- Wester J U, Jespersen S M, Nielsen K D, Neumann L. Wobble board training after partial sprains of the lateral ligament of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- Surve I, Schwellnus M P, Noakes T, Lombard C. A fivefold reduction in the incidence of recurrent ankle sprains in soccer players using the Sport-Stirrup orthosis. Am J Sports Med. 1994;22:601–606. doi: 10.1177/036354659402200506. [DOI] [PubMed] [Google Scholar]
- Sharpe S R, Knapik J, Jones B. Ankle braces effectively reduce recurrence of ankle sprains in female soccer players. J Athl Train. 1997;32:21–24. [PMC free article] [PubMed] [Google Scholar]