Abstract
Objective: To present a comprehensive review of the influence of altered kinesthesia and joint position sense on chronic ankle instability and to present a model connecting deficits in ankle position sense with the increased risk of sustaining lateral ankle sprains.
Data Sources: I searched MEDLINE for the years 1966–2001 using the key words ankle and kinesthesia or position sense and books on proprioception.
Data Synthesis: Study findings suggest a risk for unprovoked lateral ankle sprains when the lateral border of the foot accidentally catches the ground surface during the late swing phase of normal locomotion. In normal situations, the lateral border of the foot clears the ground by only 5 mm, and a small increase in ankle-position error may substantially increase the risk of a collision. Findings of affected kinesthesia and joint position sense in subjects with chronically unstable ankles dominate over studies showing nonsignificant results, but the answer is far from clear.
Conclusions/Recommendations: Changes in joint position sense and kinesthesia of a magnitude found in subjects with chronically unstable ankles can lead to an increased risk of sustaining lateral ankle sprains. Results from a small number of studies suggest that balance and coordination training can restore the increased uncertainty of joint positioning to normal levels.
Keywords: ankle injuries, kinesthesia, proprioception, position sense, sprains
Why measure kinesthesia and position sense in connection with chronic ankle instability? Several reasons explain why these rather cumbersome methods of assessing sensorimotor function have been applied to chronic ankle instability (CAI). First of all, in neurophysiology, proprioceptive functions have traditionally been tested by measuring kinesthesia and joint position sense,1,2 and these methods were readily adopted by researchers in sports traumatology.
Furthermore, it was theorized that proprioceptive information from the lateral part of the ankle joint was primarily elicited by mechanoreceptors in the lateral ligaments. If the ligaments were disrupted by trauma and then healed in an elongated state, ligament tension for a given angle of ankle inversion would be reduced and, subsequently, the mechanoreceptors would misinterpret the degree of inversion angle.
Finally, the subjective feeling reported by many injured athletes after a lateral ankle sprain is often a “loss of contact” with their ankles: the feeling of not being absolutely sure of the inversion or eversion position of the ankle during locomotion. Tests of kinesthesia and position sense were thought to be most likely to give an objective measurement to this subjective feeling.
To these primarily theoretic considerations, I would like to add our pathogenetic model, which tries to connect a deficit in position sense to an increased risk of stumbling during locomotion and, thus, sustaining a lateral ankle sprain.
TESTING FOR KINESTHESIA AND JOINT POSITION SENSE
Kinesthesia (joint motion detection) and joint position sense are both very precise sensorimotor functions, and measuring deficits in these functions requires accurate and sensitive equipment. Threshold levels of joint movement are typically less than 2°. A number of external input possibilities to the neuromuscular system (for example, the pressure of the strapping system on cutaneous receptors or the sound of motors producing the movement) must be excluded in order to receive a clear signal. The proprioceptive input is thought to be elicited close to the ankle-joint area but need not necessarily be restricted to the lateral ankle ligaments; injecting local anesthetics into these ligaments does not result in any change in kinesthesia and joint position sense.
The ability to detect a threshold level can be tested in a variety of ways, but the basic idea is always to move the ankle slowly within the normal range of ankle movement to test whether or not the subject can detect the discrete movements. As an example, Garn and Newton3 measured kinesthesia by moving the foot 5° in a plantar direction at a speed of 0.3°·s−1 in a percentage of situations of a total trial and then asked subjects whether or not they felt their foot had moved. The sensitivity for the “yes” and “no” signals was calculated as a measure of kinesthesia. In contrast, Lentell et al4 used the degree of inversion before conscious detection of movement as the kinesthetic measurement.
Measuring joint position sense requires the subject to match a set of index angles set by the investigator. Here the differences also are small (<2°), and precise measurements also require a precise method with accurate registration of limb motion and the elimination of input from other sources. The subject is always required to match an index angle in which the foot has been placed. There are, however, a variety of ways in which the index angle can be matched: using a visual analog scale,5 replicating the index angle with the contralateral foot,6 and copying the index angle with the ipsilateral foot, either actively7–10 or passively.8,10 The number of angles matched, the magnitudes of the angles, and the directions of the matching angles vary from study to study, as does the investigational equipment. The results are typically expressed in terms of a mean absolute error value of joint-position assessment, but the real errors with corresponding standard deviations about the mean have also been used.11
None of these methods is superior to the others. However, they might not all measure the same ability. In a study by Konradsen et al,10 an anesthetic ankle block resulted in a greatly increased ankle-position error when the ankle was moved passively to the index angle. If the subjects were allowed to reach the index angles by actively inverting their ankles, the anesthetic block did not influence position sense. Both methods have been used as a measure of position sense. In the passive trials, the proprioceptive ability of the ankle receptors was assessed. In the active testing situation, subjects seemed to rely on proprioceptors in the nonanesthetized muscle-tendon system.
Regardless of the method, it is necessary to have strict control of the equipment, the tests, and the testing situations when measuring kinesthesia and ankle-position sense. For that reason, frequent testing (as can be done with postural sway throughout a course of rehabilitation) is not feasible for kinesthetic and position-sense tests in clinical practice, and they are almost exclusively applied in research.
KINESTHESIA AND POSITION SENSE IN CHRONIC ANKLE INSTABILITY
Kinesthesia, or movement threshold, has not been studied as extensively in the unstable ankle as in the knee. As previously mentioned, researchers have used very different methods of kinesthetic measurement. Garn and Newton3 found a significantly increased frequency of error (P < .01) when 20 subjects with CAI had to indicate whether or not their ankles had been moved from 0° to 5° of plantar flexion at a rate of 0.3°·s−1. Similar results with a similar test were found for 11 gymnasts with unilateral unstable ankles by Forkin et al.12 Lentell et al4 noted that the amount of motion necessary to register movement was increased by 1° (P = .044) when comparing inversion threshold in the injured and uninjured ankles of 42 subjects. In contrast, Refshauge et al13 found no difference between 25 subjects with CAI and 18 healthy controls when detecting thresholds of passive plantar-flexion and dorsiflexion movements.
For ankle position sense, Jerosch and Bischof9 showed an increased absolute error when replicating 3 inversion angles (5°, 15°, and 20°) in 16 subjects with unilateral CAI when comparing the stable and unstable sides. The difference between sides was approximately 0.9°. When the inversion angles 10°, 15°, and 20° were replicated 10 times each, 23 subjects with functionally and mechanically unstable ankles demonstrated a significant difference of 0.9° over 40 control subjects with stable ankles.14 Boyle and Negus15 also found a greater error in joint position sense for the plantar-flexed and inverted foot of a group with functionally unstable ankles when testing both actively and passively. In contrast, Gross8 noted no difference between 14 subjects with stable ankles and 14 CAI subjects in both passive and active angle replications. The angles (10° eversion, 10° inversion, and 20° inversion) were replicated twice.
Why some researchers detected a difference between subjects with CAI and those without, whereas others did not, has been ascribed to differences in the definition of CAI and to differences in the testing protocols. However, no investigators have shown that using different measuring techniques on the same population of subjects with CAI can provide different results. Most studies published on CAI and ankle kinesthesia and position sense have shown a deficiency in those proprioceptive functions, but results are not difinitive.
ACUTE INVERSION INJURY AND POSITION SENSE
Is the deficit in kinesthesia or position sense seen in CAI caused by a predisposition, the result of repeated ankle inversion injuries, or the result of a single inversion injury that was never rehabilitated? Tropp16 found that it was possible to predict which subjects had the greatest risk of sustaining ankle-inversion injuries during a soccer season based on their preseason postural-balancing ability. A similar study has not been undertaken for kinesthesia and position sense, and I am not aware of any longitudinal studies of subjects sustaining repeated injuries.
Some studies are concerned with the effect of an acute lateral sprain on ankle position sense. Konradsen et al17 found the passive ankle-position replication error was increased by approximately 100% one week after an acute ankle injury in 46 subjects with previously stable ankles. The subjects received no organized rehabilitation, and after 12 weeks, a 33% increase in errors was still present. In contrast, Holme et al18 noted no difference in position sense between sides 6 weeks after an acute injury but noted differences in both postural sway and peroneal muscle strength. After the same time span, Leanderson et al19 found no difference between sides in a population of 73 patients. However, Glencross and Thornton7 found increased errors in passive replication of plantar-flexion angles in 24 subjects months after the initial ankle sprain. Severe sprains seemed to result in greater degrees of replication error than mild sprains, and the replication error was greatest with the ankle plantar flexed.
These results seem to suggest that a single sprain can cause a substantial deficit in ankle-position assessment and that returning to normal function is a slow process and may be incomplete if organized rehabilitation is not instituted.
A PATHOGENETIC MODEL OF UNPROVOKED ANKLE SPRAIN
As mentioned earlier, a number of tests are used to assess different aspects of proprioception and sensorimotor control around the ankle. Kinesthesia and ankle position sense are particularly time consuming and difficult to test. A problem with the easier tests, such as single-limb balance tests and agility tests, is that although these tests may be excellent indicators of the general proprioceptive state of the ankle, the direct connection between impaired balancing ability and the multiple ankle sprains is not obvious. I believe that we can make this pathogenetic connection between a defect in ankle position sense and the increased risk of sustaining ankle-inversion injuries with the help of the following biomechanical model.
In CAI, subjects sustain many of their repeated ankle-inversion injuries in situations that would not put subjects with stable ankles at risk. It has been said, “these are the people who trip over the flowers in a rug.” When I interviewed subjects with CAI, they uniformly stated that their disability seemed to be a 2-phase occurrence: they tripped, and then the ankle twisted. Thus, it seemed appropriate to concentrate on the movements and control of the lower leg during the swing phase of locomotion.
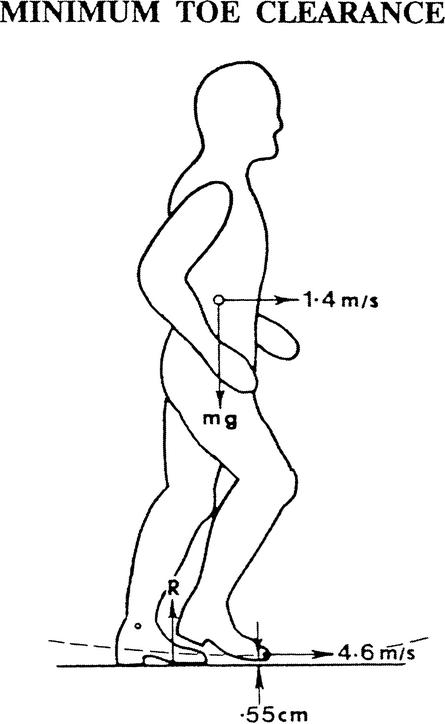
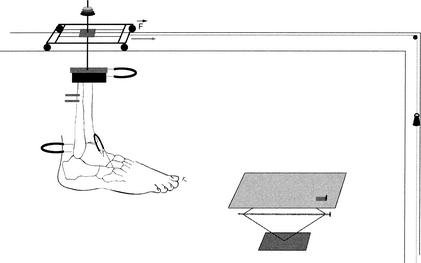
In the normal stride during level-surface walking, the latter part of the swing phase seems to require very accurate sensorimotor control. In this part of the stride, the lateral border of the foot passes just 5 mm above the ground surface (Figure 1).20 In a cadaver study, when the swing phase of the lower limb was simulated (Figure 2), Konradsen and Voigt21 found that if impact occurs between the lateral border of a foot inverted 10° and the ground surface, the foot rotates into 40° of inversion, 40° of plantar flexion, and 30° of internal tibial rotation (the limit of our set-up). The foot-ankle complex had lost its bony restrictions in this position. When the complex was loaded with the body weight at the anticipated time of heel contact, an inversion torque would be produced. This inversion torque would cause further forced inversion of the ankle, rendering it susceptible to injury.
Figure 1.
Close proximity between the lateral border of the foot and the ground during the late swing phase of the gait cycle. (Reprinted with permission.20)
Figure 2.
The experimental set-up imitates a collision between the lateral border of the foot and the ground surface during simulated swing phase. The lower leg specimen is accelerated toward the platform, where the lateral part of the foot is arrested by the lateral stop of the platform. The jig allows free movement of the specimen in all directions except posteriorly and inferiorly.
In the normal stride, the foot is brought forward in approximately 10° of inversion, and this balance of passive inversion and eversion restraints creates stability. If the degree of inversion is perceived to be too great in the midswing phase, lateral muscle contractions can be instituted for correction. This regulatory mechanism has not been demonstrated directly, but indirect evidence exists for it.22 The frequency of midswing-phase peroneal muscle activity was measured during 100 gait cycles of vigorous walking. Application of an ankle support that held the ankle in neutral inversion-eversion significantly reduced the frequency of peroneal activity. It was proposed that the reduced need for eversion corrections was responsible for this reduction in the frequency of peroneal muscle activation.22
If we then return to measurements of position sense, we find that subjects with healthy ankles had inversion-angle replication errors of 1.7°.9,14 The subjects' chance of not incurring a rotational error of approximately 8° to 10° (which would make the lateral border of the foot drop 5 mm and engage the ground during late swing phase) is extremely small (less than once every 100 000 steps). After acute ankle-inversion injury, we found the ankle-position replication error increased by approximately 100% after 1 week.17 For these subjects, given their mean ankle-position-sense error with its standard deviation and postulating a normal distribution of the error, the risk of making a rotational mistake of 8° or more is approximately 0.1%. In other words, statistically, they trip once every 1000 steps. Not many subjects with CAI are, however, this disabled in their everyday life. This model is purely static and does not account for activation of the lower leg muscles, nor does every stumbling incident necessarily result in a complete ankle-inversion injury. The model does, however, provide a reasonable explanation for the frequent sprains of the population with CAI. It underlines the pathogenetic importance of the sense of joint positioning among the different sensorimotor functions that are discussed in this issue, and it illustrates that small differences in replication errors can have a substantial clinical impact.
KINESTHESIA AND ANKLE POSITION SENSE DURING PHYSICAL ACTIVITY
Very little is known about the effect of activity on kinesthesia and ankle position sense, and the available information is nearly exclusively based on subjects with healthy ankles. Konradsen and Magnusson14 found that a normal warm-up of 20 minutes enhanced ankle position sense in a group of experienced cross-country runners. With fatigue, greater absolute errors of movement detection were noted by Forestier et al23; included were 8 subjects who performed isometric lower leg muscle training to fatigue. Whether improved kinesthetic ability can be achieved by prophylactic taping is uncertain. There may24 or may not13 be enhancement of ankle kinesthesia with ankle taping.
THE EFFECT OF COORDINATION AND BALANCE TRAINING ON ANKLE POSITION SENSE IN SUBJECTS WITH CHRONIC ANKLE INSTABILITY
Coordination and balance training (often designated as proprioceptive training) has proven very effective in reducing the frequency of ankle sprains in subjects with CAI: 80% were functionally stable after completing a well-designed program.25 There is no doubt that rehabilitation programs concerned with balance, coordination, and strength reduce postural sway and increase peroneal muscle strength. Whether this kind of training also enhances kinesthesia and position sense is less well studied. In a study by Eils and Rosenbaum,26 a group of 20 subjects with CAI improved their angle-reproduction ability significantly after 6 weeks of balance training. The same was found for a group of 20 subjects with healthy ankles 6 weeks after instituting an ankle strength-training protocol. Bernier and Perrin,27 however, did not register a change in active or passive position sense after a similar period of coordination and balance training.
The specifics of the training programs applied in these studies were not described in detail. Researchers using balance tests as the proprioceptive assessment have gone further in studying the frequency of training, and their results are discussed in other articles. However, if rehabilitation of the kinesthetic and ankle position senses primarily serves to increase the sensitivity of the higher neural centers to the information received from the ankle area, the exact rehabilitation modality may be less important than a high degree of stimulation and activity provided to the ankle area.
SUMMARY
Although the evidence is somewhat ambiguous, there is a measurable deficit in ankle kinesthesia and ankle position sense in subjects with CAI. Whether these deficits were present before the subjects' ankle disability as a predisposition, the result of repeated inversion injuries, or the result of a single injury with insufficient rehabilitation is as yet unclear. After acute injuries, however, substantial deficits are apparent and without rehabilitation they seem to prevail.
Both kinesthesia and joint position sense are difficult proprioceptive abilities to measure. Measurements require a surplus of time and advanced equipment and laboratory set-ups. These measurements, therefore, are not the choice when frequent tests are warranted. Postural-balance tests and agility tests are superior. However, contrary to other ankle sensorimotor measurements, I believe it is possible to link a deficiency in ankle position sense with the actual clinical problem of repeated ankle-inversion injuries during locomotion using a biomechanical model.
Although little information is available, it seems possible to enhance ankle position sense by warming up, at least in experienced runners. Alternatively, fatigue seems to increase kinesthetic errors. Rehabilitation activities such as balance, coordination, or lower leg strength training seem to reduce kinesthetic and ankle-position errors, but studies to date are too few to draw a conclusion as to the best rehabilitation modality concerning kinesthesia and ankle position sense.
REFERENCES
- Browne K, Lee J, Ring P A. The sensation of passive movement at the metatarsophalangeal joint of the great toe in man. J Physiol. 1954;126:448–458. doi: 10.1113/jphysiol.1954.sp005221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin G M, McCloskey D I, Matthews P C. The persistence of appreciable kinesthesia after paralysing joint afferents but preserving muscle afferents. Brain Res. 1972;37:326–329. doi: 10.1016/0006-8993(72)90679-8. [DOI] [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Robbins S, Waked E, McClaran J. Proprioception and stability: foot position awareness as a function of age and footwear. Age Ageing. 1995;24:67–72. doi: 10.1093/ageing/24.1.67. [DOI] [PubMed] [Google Scholar]
- Berenberg R A, Shefner J M, Sabol J J., Jr Quantitative assessment of position sense at the ankle: a functional approach. Neurology. 1987;37:89–93. doi: 10.1212/wnl.37.1.89. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Gross M T. Effects of recurrent lateral ankle sprains on active and passive judgements of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Jerosch J, Bischof M. Proprioceptive capabilities of the ankle in stable and unstable joints. Sports Exerc Inj. 1996;2:167–171. [Google Scholar]
- Konradsen L, Ravn J B, Sørensen A I. Proprioception at the ankle: the effect of anaesthetic blockade of ligament receptors. J Bone Joint Surg Br. 1993;75:433–436. doi: 10.1302/0301-620X.75B3.8496215. [DOI] [PubMed] [Google Scholar]
- Feuerbach J W, Grabiner M D, Koh T J, Weiker G G. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am J Sports Med. 1994;22:223–229. doi: 10.1177/036354659402200212. [DOI] [PubMed] [Google Scholar]
- Forkin D M, Koczur C, Battle R, Newton R A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- Refshauge K M, Kilbreath S L, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med Sci Sports Exerc. 2000;32:10–15. doi: 10.1097/00005768-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Magnusson P. Increased inversion angle replication error in functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2000;8:246–251. doi: 10.1007/s001670000124. [DOI] [PubMed] [Google Scholar]
- Boyle J, Negus V. Joint position sense in the recurrently sprained ankle. Aust J Physiother. 1998;44:159–163. doi: 10.1016/s0004-9514(14)60375-5. [DOI] [PubMed] [Google Scholar]
- Tropp H. Linköping University; Linköping Sweden: 1985. Functional instability of the ankle joint [thesis] [Google Scholar]
- Konradsen L, Olesen S, Hansen H M. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26:72–77. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- Holme E, Magnusson S P, Becher K, Bieler T, Aagaard P, Kjær M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- Leanderson J, Bergqvist M, Rolf C, Westblad P, Wigelius-Roovers S, Wredmark T. Early influence of an ankle sprain on objective measures of ankle joint function: a prospective randomised study of ankle brace treatment. Knee Surg Sports Traumatol Arthrosc. 1999;7:51–58. doi: 10.1007/s001670050120. [DOI] [PubMed] [Google Scholar]
- Winter D A. 2nd ed University of Waterloo Press; Waterloo, Ontario, Canada: 1991. The Biomechanics and Motor Control of Human Gait: Normal, Elderly and Pathological. [Google Scholar]
- Konradsen L, Voigt M. Ankle complex behavior during simulated limb loading. Presented at: European Society of Sports Traumatology, Knee Surgery and Arthroscopy meeting; April 28–May 2, 1998; Nice, France.
- Konradsen L, Højsgaard C. Pre-heel-strike peroneal muscle activity during walking and running with and without an external ankle support. Scand J Med Sci Sports. 1993;3:99–103. [Google Scholar]
- Forestier N, Teasdale N, Nougier V. Alteration of the position sense at the ankle induced by muscular fatigue in humans. Med Sci Sports Exerc. 2002;34:117–122. doi: 10.1097/00005768-200201000-00018. [DOI] [PubMed] [Google Scholar]
- Robbins S, Waked E, Rappel R. Ankle taping improves proprioception before and after exercise in young men. Br J Sports Med. 1995;29:242–247. doi: 10.1136/bjsm.29.4.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson J, Lansinger O. [Lateral instability of the ankle joint (1). Non-surgical treatment is the first choice–20 per cent may need ligament surgery] Lakartidningen. 1991;88:1399–1402. [PubMed] [Google Scholar]
- Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33:1991–1998. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27:274–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]