Abstract
Objective: To provide clinicians and researchers with an expanded perspective on the association between functional ankle instability and postural control.
Data Sources: I searched MEDLINE and SPORT Discus for the years 1966–2001 using the key words ankle, instability, and balance. Additional information was obtained from cross-referencing pertinent articles.
Data Synthesis: Conflicting reports have been published about whether postural control is disrupted in people with chronic ankle instability. The variety of testing methods and operational definitions used by various investigators make drawing a consensus difficult. In contrast, the results of investigations considering postural-control strategy disruptions in persons with chronic ankle instability have been compatible. Depending upon the effectiveness of an altered strategy, postural-control deficiencies may fail to be revealed in the absence of challenging tasks and environmental conditions.
Conclusions/Recommendations: If we accept the idea that postural control is disrupted after orthopaedic injury, the next step becomes identifying the causative factors within the postural-control system. Experimental evidence surrounding the role of lateral ankle-ligament mechanoreceptors in posture suggests that they cannot be the sole source of the alterations revealed. Consideration should be directed to other potential areas within the postural-control system, as outlined in the text, during ankle evaluations and rehabilitation.
Keywords: balance, equilibrium, rehabilitation
Since the work of Freeman et al1–5 describing postural-stability alterations in patients with chronic ankle instability (CAI), a large focus of the sports medicine community has been on using postural-control tasks to prevent, assess, and rehabilitate patients with CAI. Freeman et al1–5 suggested that alterations in postural control could be attributed to deficits in the afferent input arising from mechanoreceptors residing in the ankle ligaments and capsule (articular deafferentation). In addition to providing a basis for explaining the source of CAI, articular deafferentation has also been expanded to explain the source of chronic instability existing at other joints.6,7 Specific to the ankle, in addition to postural-control applications, the theory has been used to explain characteristics exhibited by people with CAI, such as deficiencies in the conscious perception of proprioceptive sensations (kinesthesia and joint position sense).8–11 Despite the popularity of the theory developed by Freeman et al,1–5 direct evidence supporting the importance of articular afferent information to the postural-control system in healthy individuals is largely debated.12 Aside from mechanoreceptor disruptions, other components of the postural-control system (PCS), such as strength, mechanical stability, and range of motion, often become altered in patients with CAI. The importance of these factors within the PCS would, therefore, suggest additional potential reasons postural control may become disrupted after injury.
The purpose of this article is to examine the link between postural control and CAI with the goal of expanding future research and clinical practice directions. To accomplish this goal, I present basic principles surrounding the physiology and assessment of postural control, review the literature considering postural instability in CAI patients, and examine the research investigating the role of ankle-ligament receptors in postural control. I will conclude with a synthesis of the material supporting potential topics for future research and clinical direction.
MAINTAINING POSTURAL EQUILIBRIUM
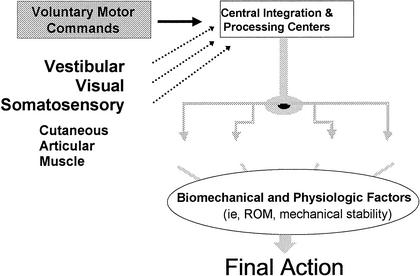
The mission of the PCS is to continuously maintain postural equilibrium during all motor activities of the body (Figure). For the convenience of discussion, the process of maintaining postural equilibrium can be considered in 3 parts. First, the body's position relative to the support surface and gravity and the positions of each segment relative to one another must be determined from afferent information. With respect to postural control, pertinent afferent information arises from vestibular, visual, and somatosensory sources. Next, the afferent information gathered from these 3 sources must be integrated and processed to determine the necessary motor commands. The motor commands are then executed by muscles along the entire kinetic chain. The exact spatial and temporal organization of commands must meet the demands of the functional task and environmental conditions.13 The last part of postural control involves the actual execution of motor commands by the neuromuscular tissues. Aside from the functional status of the skeletal muscle (ie, strength, endurance), the final outcome of a motor command depends upon many peripheral physiologic and biomechanical factors (ie, strength, mechanical stability, and available range of motion) about each of the joints in the kinetic chain.13–15 Superimposed onto this entire construct are postural requirements for conscious motor control and voluntary task initiation.
Fig. 1.
Information-processing perspective of the postural-control system. ROM indicates range of motion.
Inherent to the PCS on both the afferent and efferent sides are varying degrees of redundancy. For example, healthy individuals can close their eyes and remain in an upright bilateral-stance position with little or no increase in postural sway. In this circumstance, sufficient information is provided to the PCS by the remaining sensory inputs (vestibular, somatosensory) for equilibrium to be maintained. Similarly, on the efferent side, many possible motor combinations can be used to achieve the same end result.16 Despite the sensory and motor redundancy, it appears that the PCS uses only a limited set of distinct patterns.16–18 The selection of particular strategies appears to be dictated by previous experience, expectations, environment, task, individual characteristics, and the efficiency of the movement.17–20
Control over posture occurs in both feedback (reactive) and feedforward (preparatory) manners.21 For example, a feedback situation involves the response of the PCS to reestablish control of equilibrium when an athlete stumbles over an unseen obstacle. The response incorporates both reflexive and automatic muscle-activation sequences before any consciously initiated actions. In contrast to the feedback situation, feedforward involves the preparatory muscle activity that occurs upon the identification of the beginning and the effects of an impending event or stimulus.21,22 For example, feedforward encompasses the crouched position a wrestler assumes in response to a perceived offensive attack by his opponent or the muscle activity accompanying a voluntary motor command (ie, kicking a soccer ball).
ASSESSMENT OF POSTURAL CONTROL
Investigators studying CAI and postural control have employed a wide variety of assessment techniques. Thus, a prerequisite to gaining an understanding of the link between postural control and CAI is to be aware of several fundamental principles governing postural-control assessment. Not only are the following principles important to postural-control assessments, they are also applicable to the design of rehabilitation exercise activities.
The first decision in assessing postural control is identifying the type of task employed. Generally, tasks can be grouped into 3 categories: maintaining equilibrium during quiet stance, perturbation, or performance of voluntary movement. Analyzing periods of quiet stance allows assessment of the potential open-loop control schemes and the steady-state behavior of the PCS.23 The unexpected displacements of the body and surrounding environment that often occur during activities of daily living provide the rationale behind using perturbations.24 During activities of daily living that involve voluntary movements, conscious attention is often not required for maintaining postural control.13,25 Typically, once a conscious motor command is initiated (eg, running) the specific details of the movement (ie, sequence of muscle activation) are programmed by supraspinal areas (cerebellum, motor cortex) and spinal neural networks, while the conscious shifts its focus to another thought. Thus, it naturally follows that a comprehensive postural-control assessment should include circumstances that attempt to duplicate similar scenarios. The challenge arises in finding the balance between attaining reliable measurements and maintaining a “natural” situation.
The second major aspect in the design of a postural-control assessment deals with the particular conditions that will be manipulated in conjunction with the task. In an attempt to better focus on particular aspects of the PCS, sensory information, base of support (BOS), and support-surface characteristics are often manipulated. Altering the BOS or support-surface characteristics alone can also change sensory information. A sensory alteration pertinent to examining the link between CAI and postural control is eliminating or altering visual inputs. Changing the BOS size or shape directly influences postural control.26–29 The BOS can be defined as the area contained within the parts of the body making physical contact with the external environment. In sports medicine testing and rehabilitation, single-leg stance is the most frequently used BOS. Standing on one limb requires the PCS to reorganize itself over a narrow and short BOS and allows bilateral comparisons. Lastly, support-surface characteristics, such as dimensions and stability, can be altered to change the demands imposed by a particular task. The most commonly used support surface is a fixed, firm, level surface. Unstable surfaces, such as uniaxial and multiaxial platforms, require faster stabilization mechanisms that originate from proprioception.30,31 Whether they better differentiate postural-control deficits in CAI patients remains unknown.
The last major decision that surrounds postural-control assessment is the actual variables to be measured. Both instrumented and noninstrumented measures have been developed and used in sports medicine populations. Noninstrumented measures include variables such as length of time in equilibrium32,33 and error scoring systems.29,34,35 The advantage of noninstrumented measures is the lack of sophisticated or expensive equipment required to conduct an assessment. The largest disadvantage of noninstrumented measures resides in reduced sensitivity. Instrumented measures can be derived from force-platform, kinematics, or electromyographic data. Center-of-pressure (COP) excursion characteristics are most frequently calculated during postural-control assessments in sports medicine settings. Center-of-pressure-based variables should not be confused with movement of the body's center of mass. Rather, they represent the location and movement of the net ground-reaction-force vector in response to the corrective action being taken to maintain equilibrium.36
It is important to recognize that the reliability, validity, and sensitivity in detecting deficiencies of the tasks and variables used to assess postural control are largely unknown. Because of the potent influence these measurement-related factors have on research results and, therefore, on clinical inference, it is strongly recommended that this be a priority area for future research. Furthermore, because postural control has been described as a task-specific process,13 one must question the relationship between performance of a traditional single-leg-stance task and a functional movement pattern. A preliminary examination of this issue failed to reveal any significant relationships between 2 voluntary movement tasks (single-leg-hop stabilization test and Star Excursion Balance Tests) and traditional stabilization tasks (quiet, single-leg stance on fixed and multiaxial surfaces).37 This issue is also very applicable to the tasks used in rehabilitation programs. In other words, the efficacy of unstable-platform stance exercises in restoring functional activity proficiency is unknown and represents an area for future research.
EFFECTS OF CHRONIC ANKLE INSTABILITY ON POSTURAL CONTROL
Is Postural Control Disrupted in Patients With Chronic Ankle Instability?
At first glance, answering this question seems to be straightforward. Unfortunately, an in-depth analysis of the literature quickly leaves one buried in confusion. As discussed in several works within this special issue, the first source of discrepancy among investigations resides in the lack of universally accepted operational definitions of functional, mechanical, and chronic instability. Further complicating the topic are the various assessment approaches used by researchers. In addition to task, condition, and instrumentation variety, the reference group has consisted of the contralateral uninjured limb (intraindividual differences) and a healthy reference group (interindividual differences). This section will focus on a review of those investigations considering postural-control disruptions in CAI patients.
Again, Freeman et al2 first introduced the premise that ankle injury causes a disruption in postural control. It is important to recognize that this frequently cited investigation used simple observation and patients' self-description of their performance to compare single-leg stance between the involved and uninvolved extremities. Comparison of the results before and after a training program prompted the investigators to conclude that a regimen of coordination exercises reduced both observed postural deficits and subjective symptoms.
Advancement of the idea of Freeman et al3 concerning the link between postural stability and ankle injury by more objective instrumented approaches occurred with a series of investigations performed by Tropp et al.38–40 Specifically, these researchers employed a force platform to record COP movement during single-leg stance with eyes open. Soccer players with functional instability had significantly higher COP excursions independent of mechanical stability.40 In a subsequent investigation, Tropp41 reported no significant bilateral differences (injured versus uninjured) in soccer players with functional instability. However, a comparison of both limbs in the patients with chronically unstable ankles with a healthy reference group revealed significantly higher COP excursions.41 This result immediately offers 2 interpretations: (1) The patients with functionally unstable ankles may have a predisposition to functional instability, as evidenced by the poorer performance in the contralateral healthy limb; and (2) Functional ankle instability affects the PCS at a level that is high enough to influence stability during stance on either extremity. Support for the former interpretation can be gathered from previous work by Tropp et al38 and a more recent report42 that will be discussed in the subsequent section.
Using a similar assessment task (single-leg stance, eyes open) as Tropp et al,38–46 Konradsen and Ravn43 reported significantly altered postural stability (as measured by average distance away from the mean COP position) in patients with functional ankle instability. Similarly, Perrin et al44 compared 15 professional basketball players with a “long history” of ankle trauma (10–15 episodes) with a control group consisting of 50 healthy people (nonathletes). Their static test battery consisted of double-leg stances under eyes-open or eyes-closed conditions on a force platform. The dependent variables (excursion velocity and area) were also based on COP data. Significant differences between the 2 groups were noted for area (eyes open and closed) but not velocity. Further statistical analysis of Romberg quotients (eyes-closed results divided by eyes-open results) failed to reveal significant differences between the groups. The basketball group consisted of taller participants who also had a higher activity level than the control group. Both of these factors complicate the ability to confidently attribute the significant differences to a history of ankle sprains alone.45
Investigations using noninstrument measures with fixed, firm-surface stances have also revealed significant alterations in patients with functional ankle instability. Lentell et al,46 using an examiner to evaluate stability, compared eyes-open and eyes-closed single-leg stance between limbs (injured versus uninjured) in patients with unilateral functional ankle instability. Although 45% of the patients demonstrated symmetric performance, 55% exhibited deficits during stance on the involved extremity. In a similar manner, Forkin et al9 reported that 63% of gymnasts (9 women, 2 men) with functional ankle instability exhibited deficits during eyes-closed single-leg stance.
In contrast to the investigations that found significant postural deficits during stance on fixed, firm-support surfaces, several studies failed to detect differences. Baier and Hopf47 did not find significant differences between 22 patients with functional ankle instability and 22 healthy controls during eyes-open single-leg stance. Participants with positive anterior drawer and talar tilt tests were excluded. Dependent variables consisted of a battery of 6 COP-based measures: confidence ellipse, anteroposterior velocity, mediolateral velocity, total horizontal velocity, angular movement, and linear movement. The 2 latter variables were developed by the authors to characterize how frequently and how much the COP changes direction during a trial.
Isakov and Mizrahi48 also failed to demonstrate bilateral differences in 8 gymnasts with a history of repeated unilateral ankle sprains. In contrast to using COP-based variables, these authors used the average amplitude of the anterior-posterior and medial-lateral ground-reaction-force signals. The testing was completed under both eyes-open and eyes-closed conditions. Lastly, Bernier et al49 examined single- and double-leg stance stability in 9 patients with unilateral functional ankle instability compared with 9 healthy controls and failed to show any significant differences between the groups.
As previously mentioned, unstable support surfaces are theorized to stimulate a higher reliance on proprioception. Using this idea, Rozzi et al50 compared single-leg stance performance on a multiaxial surface in 13 healthy individuals and 13 with functional ankle instability. The participants were asked to keep the support surface as level and motionless as possible during 20-second trials. Unlike force-platform-derived measures that depend on the location and magnitude of ground-reaction forces, the instrumentation used in this investigation was purely related to the platform orientation with respect to the horizontal. Participants were assessed before and after a 4-week, 3-days-per-week multiaxial-surface training program. Initially, performance was significantly poorer in the patients with ankle instability than in the control participants during trials with decreased platform stability (lower resistance to tilt). Interestingly, after the training program, the deficits in the group with instability resolved, and both groups demonstrated significant performance improvement compared with the pretest scores.
In addition to the fixed, firm-surface condition, Bernier et al49 incorporated 2 moving support-surface conditions into their investigation. The first involved a 4° medial-lateral tilt (0.5°·s−1), while the second was a 1.91-cm medial-lateral horizontal displacement (0.31 cm·s−1). Theoretically, these conditions would require continuous reorganization of the body's center of mass over the moving BOS. The ankle joint would have been the likely location for the adaptations necessary to remain in equilibrium. Assuming varying degrees of static (mechanical) or dynamic (neuromuscular) ankle instability in their sample of participants with instability, compensatory adaptations would have become necessary at a proximal location. Although nonsignificant results were reported, it is plausible that differences may have gone undetected due to uncontrolled proximal-joint or upper extremity (or both) motions. Proximal- joint compensations will be further considered in the subsequent section.
Are Postural-Control Strategies Disrupted in Patients With Chronic Ankle Instability?
Numerous sensory and motor redundancy avenues exist in the PCS. Under normal conditions, healthy individuals may consider the redundancies to be an unnecessary luxury. In contrast, in a person with an abnormal PCS, the ability to use multiple compensatory sensory and motor pathways may mean the difference in maintaining equilibrium. This may be especially true under varying environmental conditions. As an extreme example, consider an individual with total peripheral neuropathy who walks across an unstable (movable) support surface. Without vision to provide compensatory information regarding lower extremity joint positions, the person may not be able to complete the task. Afferent information concerning joint position is important for determining body position and configuration and the temporal, spatial, and magnitude characteristics of the efferent commands (ie, joint position influencing muscle length-tension relationships). Although this represents an extreme example, it is a reasonable assumption that similar subtle situations exist after orthopaedic injury. Thus, it appears important that future orthopaedic postural-control assessments be designed and conducted with the goal of answering 2 questions: (1) Is postural control disrupted? (2) Are the strategies used to maintain postural control disrupted?
Several investigations considering CAI have already sought to consider these questions. Tropp and Odenrick51 examined the ankle and hip kinematics of single-leg stance (eyes open) in 15 patients with functional ankle instability and 15 healthy people. Specifically, these authors measured the horizontal positions of the shank, anterior superior iliac spine, and sternum-manubrium in the frontal plane. From the positional data, the root mean square of the ankle angle (angle between the shank and the sagittal plane) and the hip angle (the angle between the trunk and the supporting limb) across each trial was calculated. Center-of-pressure excursion was significantly increased, and subjects with instability displayed a higher reliance on the hip joint for postural corrections than healthy participants.
Further supporting the results of the above investigation was a similar, subsequent project by the same researchers considering the efficacy of ankle-disk exercises in patients with functional ankle instability.52 Using identical kinematic variables, they revealed significant decreases in postural sway as evidenced by the COP excursion, amplitude of sternum and ankle displacements, and root mean square of the hip angle. Although only the symptomatic limb was exercised, a statistical reduction in COP excursion was also revealed in the contralateral (healthy) limb of 8 participants with unilateral instability. Additionally, when the results of the ankle-disk training in the group with functional instability were compared with the healthy subjects in the previous study, similar statistical differences were revealed.
Using randomly timed small and medium medial-lateral support-surface perturbations, Pintsaar et al53 also demonstrated postural-control strategy changes in people with ankle instability. Three groups of female soccer players were included in the study: (1) 12 healthy players, (2) 13 players with functional ankle instability who underwent an 8-week ankle-disk training program, (3) 11 players with mechanical instability (confirmed with positive anterior drawer tests) without functional instability. Dependent variables included latency of force production (measured by the forceplate in the support surface) and strategy scores (based on the magnitude of horizontal shear forces). No significant group differences with respect to the latencies were seen. A significantly increased hip strategy was revealed in the functionally unstable group compared with the healthy group before training. After training, the strategy differences were resolved, as no significant between-group differences were noted.
THE LINK BETWEEN CHRONIC ANKLE INSTABILITY AND POSTURAL CONTROL
The previous section demonstrated that while it remains controversial whether postural control is disrupted (ie, increased postural instability evidenced by COP excursions), more consistent evidence suggested that the manner in which postural control was maintained appeared to be altered in patients with chronic instability (ie, increased reliance on corrective actions at the hip joint). Assuming the strategies used to maintain postural control are altered in CAI patients, with or without presentation of gross instability, the next step is to establish the underlying physiologic basis. In other words, “What is physiologically altered in CAI patients that could account for the demonstrated postural alterations?” In attempting to answer this question, I will examine the role of ankle articular mechanoreceptors in postural control and present other potential factors linking postural-control deficits to CAI.
THE ROLE OF ANKLE MECHANORECEPTORS IN POSTURAL CONTROL
Again, it was Freeman et al1,2 who originally proposed that joint deafferentation, or a loss of sensory input from the lateral ankle-ligament mechanoreceptors, accounted for their observations of impaired single-limb postural control in patients with CAI. Unfortunately, little direct evidence exists documenting the function of ankle articular inputs in postural control. Most of the research into the sensory aspects of postural control has focused on the roles of each broad source (vestibular, visual, and somatosensory) as a whole.18,54–66 Specifically, under the umbrella of somasensory inputs (cutaneous, muscle, articular), more inquiries have been conducted concerning the roles of the muscle and cutaneous receptors than the articular receptors.
One of the reasons for the limited number of studies may be the difficulty in experimentally isolating articular mechanoreceptor function in vivo. Additionally, the numerous interactions and compensatory pathways existing among mechanoreceptors located in cutaneous, muscle, and articular tissues make attributing results to one particular population of receptors difficult.67 The complexity of muscle-spindle function provides a good example. Muscle spindles, in addition to containing specialized afferent nerve endings for conveying muscle length and rate of changes in length to the central nervous system, also contain peripheral contractile elements. The contractile regions are innervated by gamma motor neurons (γ-MNs) and provide for the sensitivity of the muscle spindle to be adjusted. The level of γ-MN activation is under both descending (supraspinal) and peripheral influence (ie, final common-input hypothesis.68)
To date, only 2 studies69,70 have been published that used methods allowing the contribution of articular inputs in postural control to be determined. Hertel et al69 determined the effect of isolated joint-afferent reduction on postural control by anesthetizing the anterior talofibular ligament and lateral joint capsule. Single-leg postural-control assessments were conducted under eyes-open and eyes-closed conditions using a fixed support surface and a slowly rotating support surface (plantar flexion-dorsiflexion and inversion-eversion). Postural control was measured by the net location of COP with respect to the foot and the amount of movement around the mean COP location. Alterations were seen in the mean COP location during both the fixed and moving support-surface conditions: a lateral adjustment during the fixed-surface condition and a medial adjustment during the rotating-surface condition after anesthesia. Movement around the mean COP location was not significant under either of the conditions. The authors suggested that an adaptive mechanism occurred after anesthesia to compensate for the loss of afferent inputs from the lateral ankle.
Using a more dynamic approach, the effect of anterior talofibular ligament anesthesia on multiaxial-platform stability was considered by DeCarlo and Talbot.70 The study consisted of a pretest, anesthetic injection, and posttest. Stability was significantly increased after anesthesia. The authors attributed the increased stability to a learning effect based on the repeated exposures. It is important to note that the methods used to measure platform stability were not sensitive, as they were based solely on whether the platform fell completely out of balance and contacted the underlying support bracket.
As extensions to the 2 investigations above, investigators at the Neuromuscular Research Laboratory (University of Pittsburgh, Pittsburgh, PA) recently concluded a series of investigations to identify the role of the lateral ankle-ligament mechanoreceptors in postural control during static, reflexive, and functional tasks. In addition to incorporating a wide variety of tasks, postural control was considered from a multivariate perspective by using electromyographic, kinematic, and forceplate measurements. Preliminary results of these studies are briefly presented below.
The first investigation was focused on the contribution of lateral ankle-ligament inputs to single-leg postural control.71 Postural control was measured during stance on fixed- and multiaxial-support surfaces (eyes open and closed), and a single-leg landing task. Fourteen healthy subjects underwent 2 treatment conditions (control, lateral ankle-ligament anesthesia) in a counterbalanced order (48-hour intertest interval). During the treatment condition, an anesthetic solution was injected directly into the anterior talofibular and calcaneofibular ligaments. Initial statistical analyses were focused on the means and variances of the electromyographic, kinematic, and forceplate data collected during each task. Analyses across all variables failed to demonstrate significant alterations in postural control between the 2 conditions.
The subsequent investigation involved 13 healthy subjects (7 men, 6 women) attending 2 testing sessions.72 At each testing session, subjects were injected bilaterally with either an anesthetic solution or a placebo solution into the anterior talofibular or calcaneofibular ligament. Before and after the injections, anterior tibialis, peroneus longus, peroneus brevis, and gluteus medius muscle electromyographic activity was collected following a high-speed standing inversion perturbation, treadmill walking, and jogging. Significantly decreased muscle function occurred after both the anesthetic and placebo conditions; however, there was no significant difference between the 2 solutions.
Based on these investigations, it would appear that isolated losses of articular mechanoreceptor input alone do not explain the postural alterations in CAI patients reported in the literature. Yet this should not be interpreted as a definitive declaration that lateral ankle-ligament mechanoreceptors do not have a role in postural control. Animal studies documenting the effects of mechanoreceptor stimulation on γ-MNs and the findings of suppressed activity of the dynamic ankle restraints after ligamentous distention suggest that articular receptors contribute to the process of maintaining postural control. It may be that their isolated role is very subtle (ie, influencing muscle-spindle sensitivity via γ-MNs) and goes undetected by currently available measurement tools and techniques. Further research is needed in this area. Again, the pertinent concept is that isolated articular deafferentation accompanying repetitive ankle trauma does not appear to be the cause of the postural alterations reported in patients with CAI.
OTHER POTENTIAL FACTORS LINKING POSTURAL-CONTROL DEFICITS TO CHRONIC ANKLE INSTABILITY
Accepting the idea that reduced mechanoreceptor input does not account for the postural alterations in patients with CAI naturally leads one to ponder the question: What is the cause of the postural-control alterations demonstrated in CAI patients? In answering this question, one has to revert to the composition and mechanisms involved in maintaining postural control. In other words, to understand the relationship between postural alterations and CAI, athletic trainers must broaden their traditional perspective and consider the effects of injury upon each of the PCS components.
During an ankle-joint sprain, disruptions to the mechanoreceptors are believed to accompany the ligamentous and joint capsule tearing. Also, potentially occurring at the time of injury are tensile or compressive (or both) loading of the afferent fibers and nerves conveying the mechanoreceptive information to the central nervous system. Both of these events can lead to an immediate reduction in afferent input arising from the joint (ie, deafferentation). To date, experimental research has only considered the effect of isolated mechanoreceptor reduction on postural control. It may be that infliction of external loads by repetitive inversion injury on the afferent fibers adversely affects the conveyed inputs arising from populations of mechanoreceptors located in adjacent tissues. An additional explanation might be that damage to the muscle mechanoreceptors or their associated afferent fibers also occurs. Furthermore, sensory and tissue damage can affect the joints distal (ie, subtalar) or proximal (ie, knee) to the talocrural joint.
After acute injury, patients often present with voluntary guarding and inhibition, which may be attributed to pain or fear of reinjury. Over repeated injury episodes, such as in patients with CAI, the voluntary avoidance strategies may become more permanent and automatic elements of their motor programs. This may explain the bilateral deficits demonstrated in patients with unilateral ankle instability by Tropp41 and the bilateral training responses reported by Gauffin et al.52 In addition, reorganization of the central afferent pathways may occur after anterior cruciate ligament rupture.73 Although the clinical significance of this finding and whether a similar change occurs after ankle-ligament injuries has yet to be determined, it could potentially explain postural alterations in CAI patients.
Analogous to the inversion-injury mechanism's effect on the sensory nerve fibers, a similar situation appears to occur with motor neurons. Several investigators74–76 have demonstrated decreased nerve-conduction velocities and nerve injury after inversion injury. Although the results of the studies can only be directly applied to subjects with acute injuries, one could reasonably speculate that repeated trauma to the motor nerves might lead to permanent neural disruptions and, therefore, an inhibited ability to control the temporal and spatial characteristics of muscle activation. Moreover, although no direct supportive evidence exists, it is a sensible conjecture that this idea in isolation could explain the shift toward increased hip strategies demonstrated by CAI patients.
Although deficits in muscle strength and endurance as contributory factors in CAI remain a controversial topic, it is important to recognize that these deficits affect the ability of the PCS to execute motor commands involving the ankle musculature. Finally, several of the biomechanical and physiologic characteristics appear to be altered in CAI. Many people with CAI (but not all) appear to have deficits in the mechanical stability of the ankle joint as revealed by excessive joint laxity during clinical stress tests and stress radiography.8 The effect of decreased mechanical ankle-joint stability might require higher levels of ankle-muscle coactivation to maintain the joint in optimal alignment, thereby increasing reliance on corrective action at the hip joint. Additionally, many patients present with altered ankle range of motion, which also could influence the execution of motor strategies concerned with maintaining equilibrium.
CLINICAL SIGNIFICANCE
The clinical significance of the information presented in this manuscript can be focused on 2 major points. First, it remains unknown if postural control is disrupted in patients with CAI. The number of investigators reporting alterations is matched with investigators failing to find significant differences. The wide disparity in subject-inclusion criteria, assessment tasks, and variables tested makes drawing a consensus difficult. In addition to different experimental methods, one possibility to potentially explain the varied results is the altered strategies demonstrated in subjects with CAI. Depending upon the effectiveness of a particular strategy, deficiencies in the PCS may not be revealed in the absence of challenging tasks and environmental conditions. In other words, based on the investigations that revealed increased hip strategies, it is possible that the altered strategies enable patients to demonstrate normal equilibrium as measured by forceplate variables (especially COP), leading investigators to conclude that no differences exist. Several researchers have noted the large influence of ankle function on forceplate measures of postural control.51,77,78 Future researchers should consider measuring postural control through multivariate measures, including electromyographic, kinematic, and forceplate variables under a variety of tasks and environmental conditions.
The second major clinically relevant detail is that reduced mechanoreceptor input in isolation does not appear to explain the postural alterations reported in the literature. Common to the investigations using isolated injections into the lateral ankle ligaments were no significant differences that could be attributed to mechanoreceptor anesthesia. Thus, other areas within the PCS must be explored as potential causes. It is very likely that the source of postural deficits in CAI patients is unique to each individual. In some patients, decreased mechanical stability may account for alterations, while in other patients, damaged afferent or efferent (or both) neural pathways might be responsible. Thus, clinicians need to evaluate patients individually to design customized rehabilitation strategies. Using the guidelines presented in the “Assessment of Postural Control” section, clinicians could design a progressive battery of tasks to target, challenge, and evaluate the various components of the PCS. During evaluations in the optimal setting, instrumented measures can be used to determine whether a postural-control deficiency exists and whether altered strategies are being used. Clinicians without access to sophisticated instrumentation may want to consider using the various noninstrumented measures available. It is important that the final stages of the evaluative and rehabilitation process involve functional tasks of increasing complexity to ensure synchronization of the individual PCS components to the overall motor system. Clinical activities need to be included that simulate the demands imposed by functional movements to determine the capability of the PCS to control posture in a “natural” context.
In conclusion, potentially more important than the issue of whether postural control becomes disrupted as a result of ankle injury is the effect on the selection of sensory and motor strategies. Given the documented and potentially related sensory, central nervous system, and motor alterations associated with CAI, it follows that the manner in which postural equilibrium is maintained or restored would naturally become altered. Several immediate questions naturally follow acceptance of this idea: (1) When a strategy is not available because of the effects of injury, how is postural equilibrium maintained when that strategy is most appropriate? (2) Does a reliance on different motor strategies cause a predisposition to other injuries? (3) In the case of athletes, do altered strategies adversely affect performance? Thus, while research in this area began more than 30 years ago, a plethora of avenues is available for future investigation.
REFERENCES
- Freeman M AR. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- Freeman M AR, Dean M R, Hanham I W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Freeman M AR, Wyke B. Articular contributions to limb muscle reflexes: the effects of partial neurectomy of the knee joint on postural reflexes. Br J Surg. 1966;53:61–68. doi: 10.1002/bjs.1800530116. [DOI] [PubMed] [Google Scholar]
- Freeman M AR, Wyke B. The innervation of the ankle joint: an anatomical and histological study in the cat. Acta Anat (Basel) 1967;68:321–333. doi: 10.1159/000143037. [DOI] [PubMed] [Google Scholar]
- Freeman M AR, Wyke B D. Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors upon reflex activity in the leg muscles. Br J Surg. 1967;54:990–1001. doi: 10.1002/bjs.1800541204. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Warner J P, Borsa P A, Fu F H. Proprioception of the shoulder joint in healthy, unstable and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380. doi: 10.1016/S1058-2746(09)80022-0. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Kocher M S, Fu F H. Proprioception following ACL reconstruction. J Sport Rehabil. 1992;1:186–196. [Google Scholar]
- Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Forkin D M, Koczur C, Battle R, Newton R A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- Gross M. Effects of recurrent lateral ankle sprains on active and passive judgments of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Riemann B L, Guskiewicz K M. Contribution of peripheral somatosensory system to balance and postural equilibrium. In: Lephart S, Fu F, editors. Proprioception and Neuromuscular Control in Joint Stability. Human Kinetics; Champaign, IL: 2000. pp. 37–51. [Google Scholar]
- Shumway-Cook A, Woollacott M H. Williams & Wilkins; Baltimore, MD: 1995. Motor Control: Theory And Practical Applications. [Google Scholar]
- Nashner L M. Practical biomechanics and physiology of balance. In: Jacobson G, Newman C, Kartush J, editors. Handbook of Balance Function and Testing. Mosby Year Book; St Louis, MO: 1993. pp. 261–279. [Google Scholar]
- Horak F B. Clinical measurement of postural control in adults. Phys Ther. 1987;67:1881–1885. doi: 10.1093/ptj/67.12.1881. [DOI] [PubMed] [Google Scholar]
- Pedotti A, Crenna P. Individual strategies of muscle recruitment in complex natural movements. In: Winters J, Woo S Y, editors. Biomechanics and Movement Organization. Springer-Verlag; New York, NY: 1990. pp. 542–549. [Google Scholar]
- Nashner L M, McCollum G. The organization of human postural movements: a formal basis and experimental synthesis. Behav Brain Sci. 1985;8:135–172. [Google Scholar]
- Horak F B, Nashner L M, Diener H C. Postural strategies associated with somatosensory and vestibular loss. Exp Brain Res. 1990;82:167–177. doi: 10.1007/BF00230848. [DOI] [PubMed] [Google Scholar]
- Horak F B, Nashner L M. Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol. 1986;55:1369–1381. doi: 10.1152/jn.1986.55.6.1369. [DOI] [PubMed] [Google Scholar]
- Horak F B, Diener H C, Nashner L M. Influence of central set on human postural responses. J Neurophysiol. 1989;62:841–853. doi: 10.1152/jn.1989.62.4.841. [DOI] [PubMed] [Google Scholar]
- Johansson R, Magnusson M. Human postural dynamics. Crit Rev Biomech Eng. 1991;18:413–437. [PubMed] [Google Scholar]
- Leonard C T. Mosby-Year Book; St Louis, MO: 1998. The Neuroscience of Human Movement. [Google Scholar]
- Collins J J, DeLuca C J. Open-loop and closed-loop control of posture: a random-walk analysis of center-of-pressure trajectories. Exp Brain Res. 1993;95:308–318. doi: 10.1007/BF00229788. [DOI] [PubMed] [Google Scholar]
- Maki B E, Holliday P J, Fernie G R. A posture control model and balance test for the prediction of relative postural stability. IEEE Trans Biomed Eng. 1987;10:797–810. doi: 10.1109/tbme.1987.325922. [DOI] [PubMed] [Google Scholar]
- Enoka R M. 2nd ed Human Kinetics; Champaign, IL: 1994. Neuromechanical Basis of Kinesiology. [Google Scholar]
- Kirby R L, Price N A, MacLeod D A. The influence of foot position on standing balance. J Biomech. 1987;20:423–427. doi: 10.1016/0021-9290(87)90049-2. [DOI] [PubMed] [Google Scholar]
- Day B L, Steiger M J, Thompson P D, Marsden C D. Effect of vision and stance width on human body motion when standing: implications for afferent control of lateral sway. J Physiol. 1993;469:479–499. doi: 10.1113/jphysiol.1993.sp019824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uimonen S, Laitakari K, Sorri M, Bloigu R, Palva A. Effect of positioning of the feet in posturography. J Vestib Res. 1992;2:349–356. [PubMed] [Google Scholar]
- Riemann B L, Guskiewicz K M, Shields E W. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8:71–82. [Google Scholar]
- Dietz V, Mauritz K H, Dichgans J. Body oscillations in balancing due to segmental stretch reflex activity. Exp Brain Res. 1980;40:89–95. doi: 10.1007/BF00236666. [DOI] [PubMed] [Google Scholar]
- Dietz V, Berger W. Spinal coordination of bilateral leg muscle activity during balancing. Exp Brain Res. 1982;47:172–176. doi: 10.1007/BF00239376. [DOI] [PubMed] [Google Scholar]
- Ekdahl C, Jarnlo G B, Andersson S I. Standing balance in healthy subjects: evaluation of a quantitative test battery on a force platform. Scan J Rehabil Med. 1989;21:187–195. [PubMed] [Google Scholar]
- Crotts D, Thompson B, Nahom M, Ryan S, Newton R A. Balance abilities of professional dancers on select balance tests. J Orthop Sports Phys Ther. 1996;23:12–17. doi: 10.2519/jospt.1996.23.1.12. [DOI] [PubMed] [Google Scholar]
- Riemann B L, Caggiano N A, Lephart S M. Examination of a clinical method of assessing postural control during a functional performance task. J Sport Rehabil. 1999;8:171–183. [Google Scholar]
- Riemann B L, Guskiewicz K M. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35:19–25. [PMC free article] [PubMed] [Google Scholar]
- Winter D A. 2nd ed John Wiley & Sons; New York, NY: 1990. Biomechanics and Motor Control of Human Movement. [Google Scholar]
- Riemann B L, Schmitz R J, Jackson S A. Relationship between static, dynamic and functional single leg postural control performance [abstract] J Athl Train. 2001;36(suppl):S-77. [Google Scholar]
- Tropp J, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- Tropp J, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- McGuine T A, Greene J J, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Ravn J B. Prolonged peroneal reaction time in ankle instability. Int J Sports Med. 1991;12:290–292. doi: 10.1055/s-2007-1024683. [DOI] [PubMed] [Google Scholar]
- Perrin P P, Bene M C, Perrin C A, Durupt D. Ankle trauma significantly impairs postural control: a study in basketball players and controls. Int J Sports Med. 1997;18:387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- Berger W, Trippel M, Discher M, Dietz V. Influence of subjects' height on the stabilization of posture. Acta Otolaryngol. 1992;112:22–30. doi: 10.3109/00016489209100778. [DOI] [PubMed] [Google Scholar]
- Lentell G L, Katzman L L, Walters M R. The relationship between muscle function and ankle stability. J Orthop Sports Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Arch Phys Med Rehabil. 1998;79:939–944. doi: 10.1016/s0003-9993(98)90091-0. [DOI] [PubMed] [Google Scholar]
- Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle? Br J Sports Med. 1997;31:65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- Rozzi S L, Lephart S M, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardized perturbations of single limb stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996;30:151–155. doi: 10.1136/bjsm.30.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allum J J, Honegger F, Acuna H. Differential control of leg and trunk muscle activity by vestibulo-spinal and proprioceptive signals during human balance corrections. Acta Otolaryngol. 1995;115:124–129. doi: 10.3109/00016489509139273. [DOI] [PubMed] [Google Scholar]
- Black F, Nashner L. Vestibulospinal control differs in patients with reduced versus distorted vestibular function. Acta Otolaryngol. 1984;406:110–114. doi: 10.3109/00016488309123015. [DOI] [PubMed] [Google Scholar]
- Diener H C, Dichgans B, Guschlbauer B, Mau H. The significance of proprioception on postural stabilization as assessed by ischemia. Brain Res. 1984;296:103–109. doi: 10.1016/0006-8993(84)90515-8. [DOI] [PubMed] [Google Scholar]
- Diener H C, Dichgans J, Guschlbauer B, Bacher M. Role of visual and static vestibular influences on dynamic posture control. Hum Neurobiol. 1986;5:105–113. [PubMed] [Google Scholar]
- Diener H C, Dichgans J. On the role of vestibular, visual and somatosensory information for dynamic postural control in humans. Prog Brain Res. 1988;76:253–262. doi: 10.1016/s0079-6123(08)64512-4. [DOI] [PubMed] [Google Scholar]
- Dietz V, Horstmann G A, Berger W. Significance of proprioceptive mechanisms in the regulation of stance. Prog Brain Res. 1989;80:419–423. doi: 10.1016/s0079-6123(08)62238-4. [DOI] [PubMed] [Google Scholar]
- Do M C, Bussel B, Breniere Y. Influence of plantar cutaneous afferent on early compensatory reactions to forward fall. Exp Brain Res. 1990;79:319–324. doi: 10.1007/BF00608241. [DOI] [PubMed] [Google Scholar]
- Dornan J, Fernie G R, Holliday P J. Visual input: its significance in the control of postural sway. Arch Phys Med Rehabil. 1978;59:586–591. [PubMed] [Google Scholar]
- Fitzpatrick R, Gorman R B, Burke D, Gandevia S C. Postural proprioceptive reflexes in standing human subjects: bandwidth of response and transmission characteristics. J Physiol. 1992;458:69–83. doi: 10.1113/jphysiol.1992.sp019406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick R, McCloskey D I. Proprioceptive, visual and vestibular thresholds for the perception of sway during standing in humans. J Physiol. 1994;478:173–186. doi: 10.1113/jphysiol.1994.sp020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglis J T, Horak F B, Shupert C L, Jones-Rycewicz C. The importance of somatosensory information in triggering and scaling automatic postural responses in humans. Exp Brain Res. 1994;101:159–164. doi: 10.1007/BF00243226. [DOI] [PubMed] [Google Scholar]
- Magnusson M, Enbom H, Johansson R, Pyykko I. Significance of pressor input from the human feet in anterior-posterior postural control: the effect of hypothermia on vibration-induced body sway. Acta Otolaryngol. 1990;110:182–188. doi: 10.3109/00016489009122535. [DOI] [PubMed] [Google Scholar]
- Wu G, Chiang J H. The significance of somatosensory stimulations to the human foot in the control of postural reflexes. Exp Brain Res. 1997;114:163–169. doi: 10.1007/pl00005616. [DOI] [PubMed] [Google Scholar]
- Riemann B L, Myers J B, Lephart S M. Sensorimotor system measurement techniques. J Athl Train. 2002;37:85–98. [PMC free article] [PubMed] [Google Scholar]
- Johansson J, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop. 1991;268:161–178. [PubMed] [Google Scholar]
- Hertel J, Guskiewicz K M, Kahler D M, Perrin D H. Effect of lateral ankle joint anesthesia on center of balance, postural sway and joint position sense. J Sport Rehabil. 1996;5:111–119. [Google Scholar]
- DeCarlo M S, Talbot R W. Evaluation of ankle proprioception following injection of the anterior talofibular ligament. J Orthop Sports Phys Ther. 1986;8:70–76. doi: 10.2519/jospt.1986.8.2.70. [DOI] [PubMed] [Google Scholar]
- Riemann B L. University of Pittsburgh; Pittsburgh, PA: 2000. Effect of Ankle Somatosensory Alterations on Single Leg Postural Control During Static, Dynamic and Functional Tasks [dissertation] [Google Scholar]
- Myers J B, Riemann B L, Hwang J H, Lephart S M, Fu F H. Effect of proprioceptive alteration of the lateral ankle ligaments on dynamic stability. Presented at: 2002 American Orthopaedic Society for Sports Medicine Specialty Day. June 30–July 3, 2002; Orlando, FL.
- Valeriani M, Restuccia D, Di Lazzaro V, Franceschi F, Fabbriciani C, Tonali P. Central nervous system modifications in patients with lesion of the anterior cruciate ligament of the knee. Brain. 1996;119:1751–1762. doi: 10.1093/brain/119.5.1751. [DOI] [PubMed] [Google Scholar]
- Meals R A. Peroneal nerve palsy complicating ankle sprain: a report of two cases and review of the literature. J Bone Joint Surg Am. 1977;59:966–968. [PubMed] [Google Scholar]
- Kleinrensink G J, Stoechart R, Meulstee J, et al. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med Sci Sports Exerc. 1993. pp. 877–883. [PubMed]
- Nitz A J, Dobner J J, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med. 1985;13:177–182. doi: 10.1177/036354658501300306. [DOI] [PubMed] [Google Scholar]
- Winter D A, Patla A E, Frank J S. Assessment of balance control in humans. Med Prog Technol. 1990;16:31–51. [PubMed] [Google Scholar]
- Koles Z J, Castelein R D. The relationship between body sway and foot pressure in normal man. J Med Eng Technol. 1980;4:279–285. doi: 10.3109/03091908009161703. [DOI] [PubMed] [Google Scholar]