Abstract
Objective: To present appropriate tools to assist in the assessment and evaluation of ankle injuries in athletes.
Data Sources: A MEDLINE search was performed for the years 1980–2001 using the terms ankle injuries and ankle sprains.
Data Synthesis: Ankle sprains are the most common injuries sustained by athletes. In order to render appropriate treatment, a proper evaluation must be made. Assessment of ankle injuries includes obtaining a good history of the mechanism of injury, a thorough physical examination, and judicious use of radiographic evaluation and special tests. I will outline techniques for diagnosing the most common ankle injuries among athletes.
Conclusions/Recommendations: In order to provide appropriate treatment, the examiner must differentiate among injuries to the lateral ankle-ligament complex, subtalar joint, deltoid ligament, and syndesmosis. It is important to realize that injury can occur to any or all of these structures simultaneously.
Keywords: ankle sprain, syndesmosis, deltoid ligament, subtalar joint
It is estimated that one ankle sprain occurs per 10 000 persons per day.1–3 Ankle sprains are the most common sports injury,4,5 accounting for 10% to 15% of sport-related injuries,6 and are responsible for 7% to 10% of all emergency room visits.7 Most of these injuries occur in persons under 35 years of age.8 Findings from a recent study9 suggested that women are more at risk for minor ankle sprains than men. Injuries to the lateral-ligament complex caused by ankle inversion are the most common ankle sprains.6
Isolated lateral ankle sprains must be differentiated from other sprains. Subtalar-joint sprains often occur with lateral ankle-ligament sprains but can occur as isolated injuries. Isolated subtalar sprains are difficult to diagnose but usually respond well to nonoperative treatment.
Isolated medial ankle sprains are relatively uncommon, with most deltoid injuries occurring in combination with lateral malleolus fractures or syndesmosis injuries.10 However, isolated injury to the deltoid ligament can occur during an eversion injury in which the body rolls over an everted foot. The anterior fibers of the deltoid are most commonly injured.10
Isolated syndesmosis injuries, often referred to as “high” ankle sprains, are also relatively uncommon, although they are probably underreported in the literature.11 More often, syndesmosis injuries are associated with an injury to the anterior part of the deltoid ligament or fractures of the medial or lateral malleoli (or both).12 The mechanism of injury is combined forced external rotation, dorsiflexion, and axial loading of the ankle.13 The anterior tibiofibular ligament is the usual site of injury in isolated sprains.14 Isolated partial tears can be treated nonoperatively,13 but complete syndesmosis ruptures carry a high risk for chronic pain, arthrosis, or ankle instability and are best treated surgically.14
LATERAL ANKLE-LIGAMENT SPRAINS AND INSTABILITY
The main lateral soft tissue stabilizers of the ankle are the ligaments of the lateral ligamentous complex: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). In the neutral position, especially when coupled with compressive loads during weight bearing, the bony architecture of the ankle joint greatly assists with stability.15 As the foot goes into plantar flexion, thereby dissociating the bony talar contribution to talocrural stability, the ligamentous structures assume a greater role in providing stability and are more susceptible to injury.
The ATFL is a small thickening of the tibiotalar capsule. When the foot is in plantar flexion, the ligament courses parallel to the axis of the leg.16,17 Because most sprains occur when the foot is in plantar flexion, this ligament is most frequently injured in inversion sprains. The CFL and PTFL are less commonly injured.18,19 Rupture of these ligaments typically occurs in more severe injuries, as the inversion force continues posteriorly around the ankle after the ATFL is sprained. Isolated injuries of the CFL can occur when the ligament is under maximum strain with the foot in dorsiflexion but are infrequent. Isolated injuries of the PTFL are extremely rare. Most injuries to the PTFL occur with very severe ankle sprains in which both the ATFL and CFL have been torn, and the forces continue around the lateral aspect of the ankle. Broström18 found that isolated, complete rupture of the ATFL was present in 65% of all ankle sprains. A combined injury involving the ATFL and the CFL occurred in 20% of his patients.
The extent of tissue damage that occurs during an injury depends on the direction and magnitude of the forces and the position of the foot and ankle during the trauma. Ankle sprains occur significantly more often in athletes who have had previous ankle sprains.20 Pes cavus, rearfoot varus, tibial varus, and previous trauma are factors that may contribute to ankle-inversion injury, although none of these have been scientifically verified as contributing factors.
Evaluation
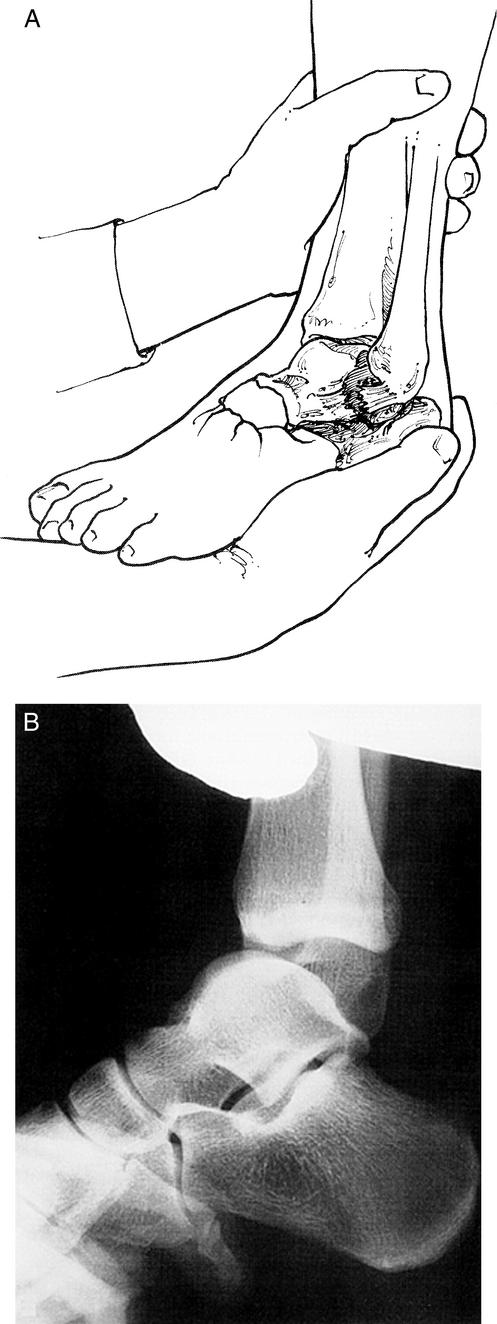
The most common mechanism of injury is an athlete who “rolled” over the outside of his or her ankle (Figure 1). This usually occurs as either a noncontact injury or when the athlete lands from a step or jumps onto an opponent's foot with an inverted foot. The foot is usually plantar flexed at the time of the injury. Many patients state that they have heard something “snap” during the trauma; however, feeling a tearing sensation or hearing a snap does not appear to correlate with the severity of the injury.8 The main site of pain and swelling is usually localized to the lateral side of the ankle over the ATFL. Several hours after the injury, generalized swelling and pain can make the evaluation more difficult and less reliable. Most patients have pain and discomfort when trying to ambulate on the injured extremity. Ecchymosis can occur 24 to 48 hours after the injury. The discoloration is usually worst along the lateral side but can also occur in the retrocalcaneal bursal area and along the heel because of the potential space available for swelling and the pooling effect of gravity. It is important that the entire leg, ankle, and foot be examined to ensure that no other injuries have occurred. With tenderness over the midshaft of the fibula or medial-side tenderness and swelling, the examiner should be suspicious of fracture or more significant injury.
Figure 1.
Typical ankle-inversion injury. Note the plantar-flexed ankle.
Clinical stability tests for ligamentous disruption are best performed between 4 and 7 days after the injury, when the acute pain and swelling are diminished and the patient is able to relax during the examination.21 The anterior drawer test is more specific for assessing the integrity of the ATFL, and the talar tilt test is more specific for detecting injury to the CFL. These findings are best recorded as differences between the ankles (assuming the opposite ankle is uninjured), but the tests can still be difficult to interpret, and the results often vary greatly among examiners.22,23 Caution must be exercised in interpreting these tests, but a positive test can help to confirm the diagnosis in a patient with a suspicious history.18,24,25
The anterior drawer test evaluates ATFL integrity by the amount of anterior-talar displacement that can be produced in the sagittal plane. To perform this test, the patient should be sitting with the knee flexed to relax the calf muscles and prevent the patient from actively guarding against the examiner. The examiner grasps the heel firmly in one hand and pulls forward while holding the anterior aspect of the distal tibia stable with the other hand (Figure 2). The sensitivity of the test can be improved by placing the ankle in 10° of plantar flexion.26 Increased anterior translation of the talus with respect to the tibia is a positive sign and indicates a tear of the ATFL, particularly if the translation is significantly different from the opposite side. However, how much translation is physiologically normal is the subject of disagreement: it has been reported to be anywhere from 2 mm to 9 mm.27,28 Therefore, it is better to compare the amount of pathologic anterior laxity with the normal side. This analysis by the examiner is subjective, and agreement among observers varies.
Figure 2.
Anterior drawer test. The ankle is held between neutral and 10° of plantar flexion, and the calcaneus is pulled anteriorly while the tibia is held stable.
The talar tilt test is defined as the angle produced by the tibial plafond and the dome of the talus in response to forceful inversion of the hindfoot. The talar tilt test is performed with the ankle in the neutral position. The examiner holds the heel stable while trying to invert the heel with respect to the tibia (Figure 3). It is important to try to grasp the talus and calcaneus as a unit to limit subtalar motion during the test. As in the anterior drawer examination, the results from the talar tilt test are difficult to interpret, with reports indicating normal values between 5° and 23°,29,30 but as a general rule, more than 10° difference from the normal side is considered abnormal.31
Figure 3.

Talar tilt test. The calcaneus and talus are grasped as a unit and tilted into inversion. The tibia is held stable with the ankle in neutral dorsiflexion.
A new testing device developed by Kirk et al32 applies standardized loads for both the anterior drawer and talar tilt tests. At an anterior force of 111 N (25 lbs) and a torque of 16 Nm, the mean anterior-drawer translation was 5.9 mm, and the mean talar-tilt translation was 51°. The device has not yet been adopted into widespread use.
Radiographic Analysis
Clinical guidelines for determining the necessity of radiographs have been developed to limit the number of radiographs. These guidelines carry tremendous potential for cost savings. The Ottawa Ankle Rules (OAR) are the commonly used criteria for predicting which patients require radiographic images.33 Radiographs are only required for those patients with (1) tenderness at the posterior edge or tip of the medial or lateral malleolus; (2) inability to bear weight (4 steps) either immediately after the injury or in the emergency room; or (3) pain at the base of the fifth metatarsal. Following these rules provided nearly 100% sensitivity for detecting fractures while significantly reducing the number of unnecessary radiographs.33 Standard radiographs, if necessary, should include anteroposterior (AP), lateral, and mortise views. The mortise view is an AP view with the tibia internally rotated by 15° to 20°. This position allows evaluation of the syndesmosis and assessment of mortise disruption. In the mortise view, the talus should be equidistant from both malleoli.
Stress radiography for acute injuries will not change the treatment protocol and is generally not indicated. These techniques are more often used for research purposes or to differentiate between mechanical instability and functional instability in patients with chronic ankle problems. Specialized instruments have been developed to apply standardized loads during the stress radiographs. The anterior-drawer stress radiograph is more sensitive for ATFL insufficiency, and the talar-tilt stress radiograph is more sensitive for CFL integrity. However, the amount of displacement that represents a pathologic condition is variable. The most commonly used criteria for the anterior-drawer stress test are those of Karlsson,31 who defined abnormal laxity as an absolute anterior displacement of 10 mm or a side-to-side difference of more than 3 mm (Figure 4). Abnormal talar tilt is even more controversial due to the large variation in “normal” talar tilt, which is reported to be from 0° to 27°.19,31,34,35 A talar tilt of 15° more than the normal side correlated with a complete double-ligament rupture (ATFL and CFL).19 As a general rule, a finding of more than 10° greater than the normal side is considered abnormal (Figure 5).28
Figure 4.
Anterior-drawer stress test. A, schematic drawing, and B, radiograph. (Copyright 2002 by the Hughston Sports Medicine Foundation, Inc).
Figure 5.

Talar-tilt stress radiograph. (Copyright 2002 by the Hughston Sports Medicine Foundation, Inc).
If the results of the 2 stress-radiographic images are combined, the sensitivity of the tests increases to 68%, but the specificity falls to 71%21; therefore, it is difficult to recommend routine use of stress radiography.
Ankle-joint arthrography is a sensitive and specific diagnostic test for ligament ruptures,36,37 as shown by Lahde et al,22 who studied 7000 ankle arthrographies performed over a 15-year period. But they also found limitations of arthrography: it is reliable only within the first 24 to 48 hours, cannot quantify the severity of ligament damage, and is an invasive procedure. Proper interpretation of arthrographic images requires a full understanding of the variant and natural leakage of contrast. Arthrography is a valuable research tool, but it is rarely indicated for clinical use because it does not change the treatment protocol.
Similarly, magnetic resonance imaging (MRI) and computed tomography (CT) scanning are rarely necessary for typical acute ankle sprains because the results do not affect the treatment protocol. Gaebler et al19 compared intraoperative findings with MRI results in 25 patients who had a talar tilt greater than 15° and found that MRI was reliable in diagnosing lateral-ligament injuries. Magnetic resonance imaging and CT scanning have been useful for identifying osteochondral injuries that may mimic, or occur in conjunction with, chronic lateral ankle instability.38
Grading Lateral Ankle-Ligament Sprains
Several lateral ankle-ligament grading systems have been used. This makes comparison in the literature difficult, as many authors did not state which grading system they used. The traditional grading system for ligament injuries focuses on a single ligament, with a grade I injury representing a microscopic injury without stretching of the ligament on a macroscopic level. A grade II injury has macroscopic stretching, but the ligament remains intact. A grade III injury is a complete rupture of the ligament.31 Applying this grading system to lateral ankle-ligament sprains addresses only the status of the ATFL and ignores injury to either the CFL or PTFL. Some authors have thus resorted to grading lateral ankle-ligament sprains by the number of ligaments injured.18,19,24 The major drawback to this system is that, unless the injury is treated surgically, objective evidence of injury to each ligament is lacking. Finally, because of the problems of these grading systems, a classification based on clinical severity has been used. This system has 3 clinical grades: grade I (mild), grade II (moderate), and grade III (severe).16,17 A grade I injury involves little swelling and tenderness, minimal or no functional loss, and no mechanical joint instability. A grade II injury has moderate pain, swelling, and tenderness over the involved structures; some joint motion is lost, and joint instability is mild to moderate. A grade III injury is a complete ligament rupture with marked swelling, hemorrhage, and tenderness; function is lost, and joint motion and instability are markedly abnormal. Grading of ankle sprains remains a largely subjective interpretation, and agreement among independent observers varies.
Differential Diagnosis
Other problems can mimic, or be coupled with, lateral ankle-ligament sprains. Fractures of the ankle are often associated with ankle-ligament injuries.12 In particular, the examination should focus on potential fractures of the lateral, medial, and posterior malleolus; proximal fibula; lateral or posterior process of the talus; anterior process of the calcaneus; fifth metatarsal; navicular or other midtarsal bones; and children's epiphyseal separations.
Patients with stress fractures about the ankle joint may present with a different type of history but similar symptoms. In particular, a transverse, proximal diaphyseal fracture of the fifth metatarsal bone (Jones fracture) can mimic an acute lateral ankle sprain.33 This is particularly true when an acute fracture occurs through an area of previous stress reaction that may have had minimal or no symptoms. The distal fibula, medial malleolus, calcaneus, navicular, and metatarsals are also prone to stress fracture.
Osteochondral fractures or osteochondritis dissecans of the talar dome or the tibial plafond can occur with lateral ankle-ligament sprains.38 These fractures can become chronic problems, with continued pain and recurrent instability episodes. If plain radiographs are negative despite continued pain, a bone scan, CT scan, or MRI may be helpful to evaluate for this lesion.38 Arthroscopy is the definitive test for the diagnosis and treatment of these fractures.
Athletes with sprains of the subtalar joint or midfoot ligaments can present with a similar history.39 In particular, the dorsal calcaneocuboid ligament, bifurcate ligament, cervical ligament, and interosseous talocalcaneal ligament are prone to injury.
Subluxation or dislocation of the peroneal tendons can mimic an ankle sprain.40 However, these injuries typically occur by a violent dorsiflexion and pronation moment of the ankle instead of the typical inversion injury of lateral-ligament injuries.40
SUBTALAR-JOINT SPRAINS AND INSTABILITY
The incidence of subtalar sprains is unknown, mainly due to the difficulty of assessing these injuries and the common association with lateral ankle-ligament sprains. They are probably more common than appreciated. Meyer et al39 studied subtalar arthrograms in 40 patients with acute ankle sprains and found that 17 (43%) had subtalar-ligament injury. Fortunately, the incidence of chronic ankle problems is low, with subtalar instability present in only about 10% of patients who present with chronic lateral ankle-ligament instability.41 Patients with acute subtalar sprains seem to do well with nonoperative treatment similar to that used for acute lateral ankle-ligament sprains. However, since the definition and diagnosis of subtalar sprains are not agreed upon in the literature, this is difficult to prove.
Acute symptoms of subtalar sprains are similar to, and can occur with or be masked by, lateral ankle-ligament sprains. Tenderness over the subtalar joint is characteristic but can be difficult to differentiate from the tibiotalar joint because of the close proximity and the swelling that obscures the anatomy.
Clinical evaluation of subtalar instability is very difficult and unreliable. An evaluation of the change in angle between the heel and the tibia with passive inversion and eversion of the heel can be made by comparing this angle with that on the uninjured side,41 but the sensitivity and specificity of this test is unknown.
Radiographs should be obtained as per the Ottawa ankle rules.33 Subtalar stress radiographs,42 subtalar arthrography,39 or stress tomography41 can show increased motion and differentiate between subtalar and talocrural motion; however, most of these injuries can be effectively treated by rehabilitation, so specialized studies are usually unnecessary. If surgery is considered, stress radiographs may be helpful in planning the surgery.
Classification of Subtalar-Joint Sprains
Subtalar-joint sprains are classified by the injury mechanism and the degree of ligamentous damage.39 The injury can occur in either plantar flexion or dorsiflexion. Forceful supination with the foot in plantar flexion tears the ATFL (and possibly the cervical ligament), followed by either disruption of the CFL and lateral capsule (type 1) or tearing of the interosseous talocalcaneal ligament (type 2). When the ankle is in dorsiflexion, the ATFL is not under tension and remains uninjured. This type of injury tears the CFL, the cervical ligament, and the interosseous talocalcaneal ligament (type 3). A type 4 subtalar sprain is a rupture of all lateral and medial capsuloligamentous components of the posterior tarsus. This injury occurs as the foot moves from dorsiflexion to plantar flexion while forceful hindfoot supination occurs.39
DELTOID LIGAMENT TEARS
In Broström's18 series of 281 acute ankle sprains, medial-side ankle sprains constituted only 3%. Nearly all of the medial-side injuries were partial ligament tears. Complete deltoid ligament ruptures most often occur in combination with ankle fractures. In Harper's10 review of 42 patients with complete deltoid ligament ruptures, all had other injuries. In the ankle-fracture classification described by Lauge-Hansen,12 a deltoid ligament tear or medial malleolar fracture occurs as the injury pattern continues around the ankle in a circular fashion. The 3 most characteristic mechanisms of injury of the deltoid ligament are pronation-abduction, pronation-external rotation, and supination-external rotation of the foot.12,43,44 The first component describes the position of a planted foot, and the second term indicates the relative motion of the foot as the leg rotates about the planted foot. So, in the pronation-abduction injury, the foot is planted in pronation as the upper body falls to the lateral side of the foot, placing a large abduction force onto the ankle and deltoid ligament. Because the forces required to injure the strong deltoid ligament are so great, the injury usually continues through the syndesmosis by the strong lever action of the lateral malleolus on the lateral aspect of the talus.12
Evaluation
Deltoid ligament injuries cause pain, tenderness, and swelling on the medial side of the ankle. A defect may be palpable below the medial malleolus in complete ruptures. If a deltoid ligament injury is present, it is extremely important to evaluate the ankle for a syndesmosis sprain or fracture. The entire fibula, including the proximal third and proximal tibiofibular joint, must also be palpated to rule out complete syndesmosis disruption.
For medial-side injuries, radiographs are necessary to evaluate the bony structures and syndesmosis. The minimum radiographic series includes AP, lateral, and mortise views. If there is any suspicion for a proximal fibular fracture, AP and lateral radiographs of the entire tibia and fibula should be taken. If the deltoid ligament and syndesmosis are both completely disrupted, the medial clear space between the medial talus and the lateral border of the medial malleolus will be widened to 4 mm or more (Figure 6).45,46 However, isolated deltoid ruptures do not cause widening of the medial clear space because the lateral malleolus holds the talus in position. Similarly, syndesmosis injuries without deltoid tears do not have medial joint-space widening. In this case, the inferior tibiofibular joint must be carefully evaluated for syndesmosis injury. Eversion-stress radiographs, arthrography, or MRI may be helpful in difficult cases, but the diagnosis can most often be made with clinical examination and plain radiographs.
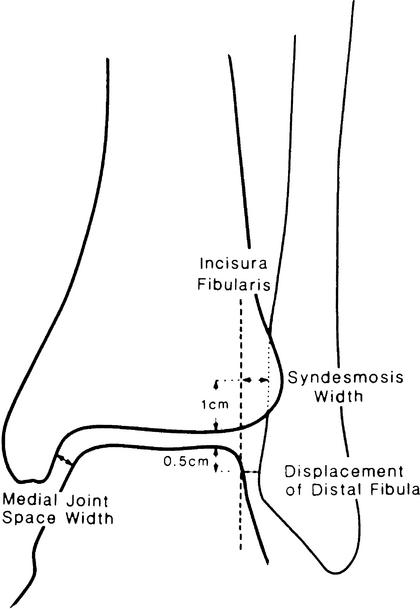
Figure 6.
Radiographic measurements of deltoid and syndesmosis injuries. (Adapted with permission from Harper MC. The deltoid ligament: an evaluation of need for surgical repair. Clin Orthop. 1988;226:156–158; Lippincott Williams & Wilkins.10).
TIBIOFIBULAR SYNDESMOSIS TEARS: “HIGH” ANKLE SPRAINS
Partial or complete rupture of the syndesmosis ligament complex can cause diastasis of the inferior tibiofibular joint.47 Isolated complete syndesmosis injuries are rare, and relatively little information exists in the literature about ankle diastasis in the absence of fracture. Fritschy48 reported only 12 cases of complete isolated syndesmosis ruptures in a series of more than 400 ankle-ligament ruptures. All 12 injuries were caused by a sudden external rotation of the ankle that caused the talus to pry the fibula laterally, thus opening the distal tibiofibular articulation.
Isolated partial syndesmosis injuries occur with some frequency, and their incidence is probably underreported in the literature. It is important to recognize that syndesmosis involvement generally increases recovery time 2- or 3-fold over that for a lateral ankle-ligament sprain. Early diagnosis of the syndesmosis sprain can help to give the athlete and coaches realistic expectations of return to play. Nussbaum et al13 suggested that the expanse of the syndesmosis tenderness was predictive of recovery time, with more syndesmosis tenderness correlating with more playing days missed. However, it is much more common for the injury to be associated with a fracture or deltoid ligament injury (or both).12 With ankle fractures, the frequency of syndesmosis ruptures is related to the type and level of associated fibular fractures.12 Syndesmosis injuries are more common as the level of the fibular fracture rises above the level of the ankle joint, as predicted by the Lauge-Hansen12 injury-mechanism classification of ankle fractures. In this classification scheme, ligamentous injuries or fractures occur as the rotatory forces continue around the ankle in a circular fashion.12
Evaluation
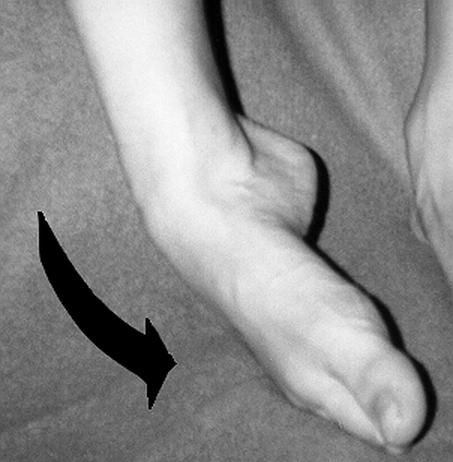
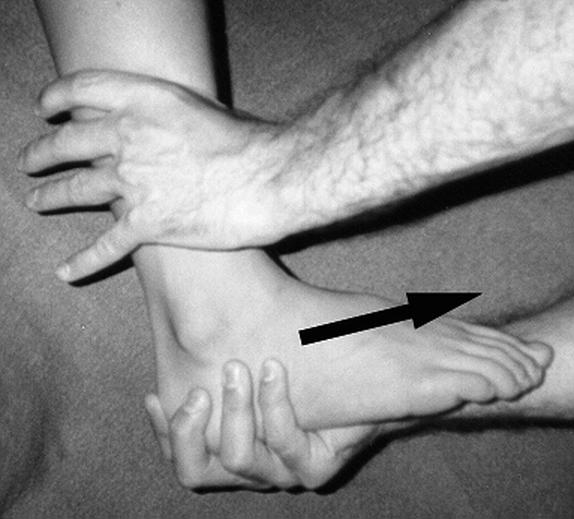
Pain and tenderness are located primarily on the anterior aspect of the syndesmosis and interosseous membrane. Active and passive external rotation of the foot is painful. The external-rotation test is performed by externally rotating the foot with the ankle in dorsiflexion (Figure 7), which stresses the syndesmosis by levering the talus against the lateral malleolus. Patients with a syndesmosis injury have pain over the anterior inferior tibiofibular ligament and joint. The squeeze test is performed by compressing the midshaft of the tibia and fibula together. If a syndesmosis injury is present, the patient has pain at the inferior tibiofibular joint. Biomechanical studies have confirmed distal tibiofibular motion during the squeeze test.49
Figure 7.
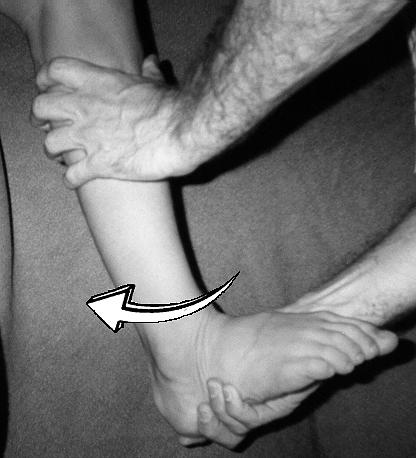
Dorsiflexion and external-rotation stress test for syndesmosis injury. The tibia is held stable while the foot is dorsiflexed and externally rotated.
Radiographs should be taken according to the Ottawa ankle rules as outlined in the previous sections.33 Anteroposterior, lateral, and mortise views may be needed to exclude fractures and osseous avulsions and to evaluate syndesmosis widening. In athletes with possible syndesmosis widening or proximal fibular tenderness, AP and lateral films of the entire tibia and fibula are necessary to rule out a Maisonneuve fracture. Acceptable radiographic guidelines that indicate syndesmosis diastasis are controversial, and measurements can be affected greatly by the amount of tibial rotation. The most commonly used guidelines are a joint-space widening of greater than 5 mm or a tibiofibular overlap of less than 10 mm, both as measured on the AP view. Other authors prefer to use the ratio of measurements to the fibular width.50 Ninety percent predictive intervals for a normal relationship were a tibiofibular overlap-to-fibular width ratio greater than 24% and a tibiofibular clear space-to-fibular width ratio of less than 44%, both as measured on the AP radiograph.50 Stress radiographs with the foot in external rotation in both dorsiflexion and plantar flexion may demonstrate the diastasis.48 Magnetic resonance imaging has now become the test of choice for evaluating the syndesmosis in difficult cases.51
CONCLUSIONS
In order to provide appropriate treatment after an athlete sprains an ankle, a thorough evaluation is necessary. This should include the mechanism of injury, physical examination, and appropriate radiographic studies and special tests. The injury can affect the lateral ankle-ligament complex, the subtalar joint, the deltoid ligament, or the syndesmosis or any combination of these structures simultaneously. Defining the extent of injury allows the clinician to institute the proper treatment regimen in preparation for the athlete's safe return to sport.
REFERENCES
- Brooks S C, Potter B T, Rainey J B. Treatment for partial tears of the lateral ligament of the ankle: a prospective trial. Br Med J (Clin Res Ed) 1981;282:606–607. doi: 10.1136/bmj.282.6264.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch P G, Holden P, Robson D J, Rowley D I, Norris S H. The value of mobilisation and non-steroidal anti-inflammatory analgesia in the management of inversion injuries of the ankle. Br J Clin Pract. 1985;2:69–72. [PubMed] [Google Scholar]
- Ruth C. The surgical treatment of injuries of the fibular collateral ligaments of the ankle. J Bone Joint Surg Am. 1961;43:229–239. [Google Scholar]
- Lassiter T E, Jr, Malone T R, Garrett W E., Jr Injury to the lateral ligaments of the ankle. Orthop Clin North Am. 1989;20:629–640. [PubMed] [Google Scholar]
- McConkey J P. Ankle sprains, consequences and mimics. Med Sport Sci. 1987;23:39–55. [Google Scholar]
- MacAuley D. Ankle injuries: same joint, different sports. Med Sci Sports Exerc. 1999;31(7 suppl):409–411. doi: 10.1097/00005768-199907001-00001. [DOI] [PubMed] [Google Scholar]
- Viljakka T, Rokkanen P. The treatment of ankle sprain by bandaging and antiphlogistic drugs. Ann Chir Gynaecol. 1983;72:66–70. [PubMed] [Google Scholar]
- Nilsson S. Sprains of the lateral ankle ligaments, part II: epidemiological and clinical study with special reference to different forms of conservative treatment. J Oslo City Hosp. 1983;33:13–36. [PubMed] [Google Scholar]
- Hosea T M, Carey C C, Harrer M F. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop. 2000;372:45–49. doi: 10.1097/00003086-200003000-00006. [DOI] [PubMed] [Google Scholar]
- Harper M C. The deltoid ligament: an evaluation of need for surgical repair. Clin Orthop. 1988;226:156–168. [PubMed] [Google Scholar]
- Boytim M J, Fischer D A, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–298. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- Lauge-Hansen N. Fractures of the ankle, II: combined experimental surgical and experimental roentgenologic investigation. Arch Surg. 1950;60:957–985. [PubMed] [Google Scholar]
- Nussbaum E D, Hosea T M, Sieler S D, Incremona B R, Kessler D E. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29:31–35. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- Ogilvie-Harris D J, Reed S C. Disruption of the ankle syndesmosis: diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10:561–568. doi: 10.1016/s0749-8063(05)80015-5. [DOI] [PubMed] [Google Scholar]
- Stormont D M, Morrey B F, An K N, Cass J R. Stability of the loaded ankle: relation between articular restraint and primary and secondary static restraints. Am J Sports Med. 1985;13:295–300. doi: 10.1177/036354658501300502. [DOI] [PubMed] [Google Scholar]
- Balduini F C, Tetzlaff J. Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med. 1982;1:3–12. [PubMed] [Google Scholar]
- Balduini F C, Vegso J J, Torg J S, Torg E. Management and rehabilitation of ligamentous injuries to the ankle. Sports Med. 1987;4:364–380. doi: 10.2165/00007256-198704050-00004. [DOI] [PubMed] [Google Scholar]
- Broström L. Sprained ankles, I: anatomic lesions in recent sprains. Acta Chir Scand. 1964;128:483–495. [PubMed] [Google Scholar]
- Gaebler C, Kukla C, Breitenseher M J, et al. Diagnosis of lateral ankle ligament injuries: comparison between talar tilt, MRI and operative findings in 112 athletes. Acta Orthop Scand. 1997;68:286–290. doi: 10.3109/17453679708996703. [DOI] [PubMed] [Google Scholar]
- Sitler M, Ryan J, Wheeler B, et al. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball: a randomized clinical study at West Point. Am J Sports Med. 1994;22:454–461. doi: 10.1177/036354659402200404. [DOI] [PubMed] [Google Scholar]
- Van Dijk C N. University of Amsterdam; Amsterdam, Netherlands: 1994. On Diagnostic Strategies in Patients with Severe Ankle Sprain [master's thesis] [Google Scholar]
- Lahde S, Putkonen M, Puranen J, Raatikainen T. Examination of the sprained ankle: anterior drawer test or arthrography? Eur J Radiol. 1988;8:255–257. [PubMed] [Google Scholar]
- Rasmussen O. Stability of the ankle joint: analysis of the function and traumatology of the ankle ligaments. Acta Orthop Scand Suppl. 1985;211:1–75. [PubMed] [Google Scholar]
- Chapman M W. Sprains of the ankle. Instr Course Lect. 1975;24:294–308. [Google Scholar]
- Ryan J B, Hopkinson W J, Wheeler J H, Arciero R A, Swain J H. Office management of the acute ankle sprain. Clin Sports Med. 1989;8:477–495. [PubMed] [Google Scholar]
- Renström P, Theis M. Biomechanics and function of ankle ligaments: experimental results and clinical application. Sportverletz Sportschaden. 1993;7:29–35. [Google Scholar]
- Johannsen A. Radiological diagnosis of lateral ligament lesion of the ankle. Acta Orthop Scand. 1978;49:295–301. doi: 10.3109/17453677809005768. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Surgical treatment of chronic lateral instability of the ankle joint: a new procedure. Am J Sports Med. 1989;17:268–274. doi: 10.1177/036354658901700220. [DOI] [PubMed] [Google Scholar]
- Cox J S. Surgical and nonsurgical treatment of acute ankle sprains. Clin Orthop. 1985;198:118–126. [PubMed] [Google Scholar]
- Rubin G, Whitten M. The talar tilt angle and fibular collateral ligaments: a method for the determination of talar tilt. J Bone Joint Surg Am. 1960;42:311–326. [Google Scholar]
- Karlsson J. Göteborg University; Göteborg, Sweden: 1989. Chronic Lateral Instability of the Ankle [master's thesis] p. 158. [Google Scholar]
- Kirk T, Saha S, Bowman L S. A new ankle laxity tester and its use in the measurement of the effectiveness of taping. Med Eng Phys. 2000;22:723–731. doi: 10.1016/s1350-4533(01)00008-x. [DOI] [PubMed] [Google Scholar]
- Stiell I G, Greenberg G H, McKnight R D, Nair R C, McDowell I. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384–390. doi: 10.1016/s0196-0644(05)82656-3. [DOI] [PubMed] [Google Scholar]
- Perlman M, Leveille D, DeLeonibus J, et al. Inversion lateral ankle trauma: differential diagnosis, review of the literature, and prospective study. J Foot Surg. 1987;26:95–135. [PubMed] [Google Scholar]
- Cox J S, Hewes T F. “Normal” talar tilt angle. Clin Orthop. 1979;140:37–41. [PubMed] [Google Scholar]
- Broström L. Sprained ankles, 3: clinical observations in recent ligament ruptures. Acta Chir Scand. 1965;130:560–569. [PubMed] [Google Scholar]
- van Moppens Fl, van den Hoogenband C R. University of Maastricht; Maastricht, Netherlands: 1992. Diagnostic and Therapeutic Aspects of Inversion Trauma of the Ankle Joint [master's thesis] [Google Scholar]
- Lazarus M L. Imaging of the foot and ankle in the injured athlete. Med Sci Sport Exerc. 1999;31(7 suppl):412–420. doi: 10.1097/00005768-199907001-00002. [DOI] [PubMed] [Google Scholar]
- Meyer J M, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain: a roentgenographic study. Clin Orthop. 1988;226:169–173. [PubMed] [Google Scholar]
- Safran M R, O'Malley D, Jr, Fu F H. Peroneal tendon subluxation in athletes: new exam technique, case reports, and review. Med Sci Sports Exerc. 1999;31(7 suppl):487–492. doi: 10.1097/00005768-199907001-00009. [DOI] [PubMed] [Google Scholar]
- Brantigan J W, Pedegana L R, Lippert F G. Instability of the subtalar joint: diagnosis by stress tomography in three cases. J Bone Joint Surg Am. 1977;59:321–324. [PubMed] [Google Scholar]
- Laurin C A, Ouellet R, St-Jacques R. Talar and subtalar tilt: an experimental investigation. Can J Surg. 1968;11:270–279. [PubMed] [Google Scholar]
- Sclafani S J. Ligamentous injury of the lower tibiofibular syndesmosis: radiographic evidence. Radiology. 1985;156:21–27. doi: 10.1148/radiology.156.1.4001407. [DOI] [PubMed] [Google Scholar]
- Yde J. The Lauge-Hansen classification of malleolar fractures. Acta Orthop Scand. 1980;51:181–192. doi: 10.3109/17453678008990784. [DOI] [PubMed] [Google Scholar]
- Grath G B. Widening of the ankle mortise. Acta Chir Scand. 1960;263:1–7. [PubMed] [Google Scholar]
- Harper M C. An anatomic study of the short oblique fracture of the distal fibula and ankle stability. Foot Ankle. 1983;4:23–29. doi: 10.1177/107110078300400106. [DOI] [PubMed] [Google Scholar]
- Marymont J V, Lynch M A, Henning C E. Acute ligamentous diastasis of the ankle without fracture: evaluation by radionuclide imaging. Am J Sports Med. 1986;14:407–409. doi: 10.1177/036354658601400514. [DOI] [PubMed] [Google Scholar]
- Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17:282–286. doi: 10.1177/036354658901700223. [DOI] [PubMed] [Google Scholar]
- Teitz C C, Harrington R M. A biomechanical analysis of the squeeze test for sprains of the syndesmotic ligaments of the ankle. Foot Ankle Int. 1998;19:489–492. doi: 10.1177/107110079801900713. [DOI] [PubMed] [Google Scholar]
- Ostrum Rf, De Meo P, Subramanian R. A critical analysis of the anterior-posterior radiographic anatomy of the ankle syndesmosis. Foot Ankle Int. 1995;16:128–131. doi: 10.1177/107110079501600304. [DOI] [PubMed] [Google Scholar]
- Vogl T J, Hochmuth K, Diebold T, et al. Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol. 1997;32:401–409. doi: 10.1097/00004424-199707000-00006. [DOI] [PubMed] [Google Scholar]