Abstract
Objective: To outline rehabilitation concepts that are applicable to acute and chronic injury of the ankle, to provide evidence for current techniques used in the rehabilitation of the ankle, and to describe a functional rehabilitation program that progresses from basic to advanced, while taking into consideration empirical data from the literature and clinical practice.
Background: Important considerations in the rehabilitation of ankle injuries include controlling the acute inflammatory process, regaining full ankle range of motion, increasing muscle strength and power, and improving proprioceptive abilities. These goals can be achieved through various modalities, flexibility exercises, and progressive strength- and balance-training exercises. In this article, we discuss the deleterious effects of ankle injury on ankle-joint proprioception and muscular strength and how these variables can be quantifiably measured to follow progress through a rehabilitation program. Evidence to support the effectiveness of applying orthotics and ankle braces during the acute and subacute phases of ankle rehabilitation is provided, along with recommendations for functional rehabilitation of ankle injuries, including a structured progression of exercises.
Recommendations: Early functional rehabilitation of the ankle should include range-of-motion exercises and isometric and isotonic strength-training exercises. In the intermediate stage of rehabilitation, a progression of proprioception-training exercises should be incorporated. Advanced rehabilitation should focus on sport-specific activities to prepare the athlete for return to competition. Although it is important to individualize each rehabilitation program, this well-structured template for ankle rehabilitation can be adapted as needed.
Keywords: ankle sprain, neuromuscular rehabilitation, proprioception, functional ankle instability
Rehabilitation of athletic injuries requires the prescription of sport-specific exercise and activities that challenge the recovering tendons, ligaments, bones, and muscle fibers without overstressing them. The goal of rehabilitation is to return an athlete to the same or higher level of competition as before the injury. Rehabilitation must take into consideration normal tissue size, flexibility, muscular strength, power, and endurance. Control of swelling and effusion must be accomplished with frequent application of external pressure, modalities such as cryotherapy, and active range of motion (ROM).
The effectiveness of the rehabilitation program after injury (Figure 1) or surgery often determines the success of future function and athletic performance.1 An understanding of the body's response to injury is paramount to designing a rehabilitation approach. Ligamentous and soft tissue injury results in biochemical changes similar to those seen after an injury.2 Injury results in bleeding and damage to tissue, which produces pain. After the initial insult, the inflammatory response is initiated, followed by the proliferative phase and the maturation phase3 (Figure 2).
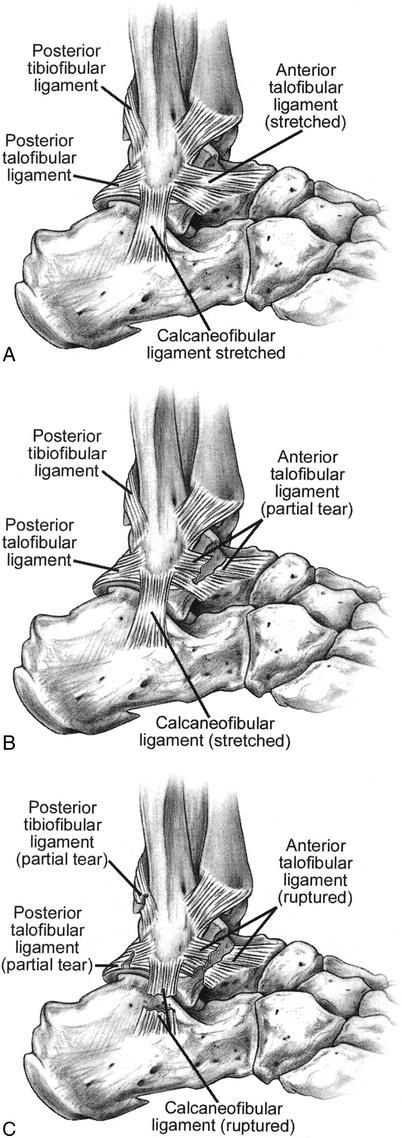
Figure 1.
Three grades of an ankle injury. A, The grade I sprain is characterized by stretching of the anterior talofibular and calcaneofibular ligaments. B, In the grade II sprain, the anterior talofibular ligament tears partially, and the calcaneofibular ligament stretches. C, The grade III sprain is characterized by rupture of the anterior talofibular and calcaneofibular ligaments, with partial tearing of the posterior talofibular and tibiofibular ligaments.
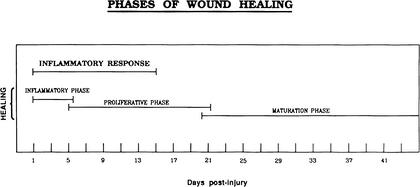
Figure 2.
Phases of wound healing. Reprinted with permission.3
Stress to collagen fibers results in fiber orientation along these specific lines of stress. Specifically, rehabilitation during days 1 through 5 should focus on protection of the injured tissue, then supervised and protected stress may be applied from days 6 to 42. The goal of athletic rehabilitation is to return the athlete to participation as quickly as possible, while allowing the injured tissue to heal without compromising it by further injury.
The following goals are important for any rehabilitation program: decreased swelling, pain, and initial inflammatory response and protection of the joint so that a secondary inflammatory response does not develop from overly aggressive rehabilitation. Similarly, ROM, muscular strength, power, and endurance must be returned to preinjury levels so that full, asymptomatic functional activities may be performed to the preinjury level and beyond.1
The application of specific functional exercises is important to stress the healing tissue. The specific adaptation to imposed demand (SAID) principle is helpful when designing functional progression.4 The activities and stresses placed on the tissue must be specific to those of the activities at hand. Nonetheless, development of the higher levels of the rehabilitation spectrum must incorporate a working knowledge of the specific activity. If the athletic trainer's knowledge of the specific activity is vague, incorporating the aid of a member of the coaching staff often results in a welcome collaboration and improved therapy.
Chronic instability (CAI) is thought to be the result of neural (proprioception, reflexes, muscular reaction time), muscular (strength, power, and endurance), and mechanical mechanisms (ligamentous laxity).5 Therefore, we will address each of these areas in this manuscript.
The multifaceted musculoskeletal system offers various ways that proprioception can be affected. Deficits in proprioception have been demonstrated after injury6 and with articular disease7 and increasing age.8,9 As a joint moves, impulses must arise from muscular, fascial, tendon, and articular receptors. Injury to any or all of these receptors can result in a sensory deficit.
Evaluating balance or postural stability is one method of assessing sensory deficits after injury. Postural stability is commonly measured as postural sway, the degree or amplitude that a person sways away from his or her center of balance. After injury, a patient must be able to maintain posture against gravity before progressing to more complicated functional activities. Therefore, it is essential that evaluation and rehabilitation for deficits in postural sway be used more frequently after musculoskeletal injuries.
Freeman et al10 were the first to report that exercises on a wobble board could reduce the incidence of instability after ankle sprain as measured with a modified Romberg test. Since then, various methods have been used to assess the function of postural stability before and after ankle injury. Tropp et al11 compared 127 soccer players with CAI with 30 normally active individuals. Players showing abnormal stabilometric values were at higher risk for sustaining an ankle injury during the next season. Specifically, they found that the overall incidence of ankle injury was 18% whether the player had suffered a previous injury or not. Twenty-three players sustained an ankle joint injury; 12 of 29 (42%) of those had a pathologic stabilometry value, while 11 of 98 (11%) of those players who had normal values suffered an ankle-joint injury. Therefore, the risk of sustaining an ankle injury was significantly lower if stabilometric recordings were within normal limits.11
Specifically, deficits in postural stability have been reported in the unstable ankle12,13 and after an acute ankle sprain.14 However, when subjects with chronically unstable and uninvolved ankles15 were compared with subjects with chronically unstable ankles and controls,16 no statistical difference was reported.
Injury to the ankle and CAI may result in deficits in postural stability. Assessment of postural stability using relatively inexpensive balance devices and equipment that is more sophisticated should be a standard part of the ankle-rehabilitation program. Documentation of progress and accurate assessment throughout the process makes setting goals for the athlete easier to document while providing quantitative data for the supporting athletic staff and insurance companies.
One goal of rehabilitation is to develop strength and neuromuscular control so that the ankle and foot are better controlled and protected during stance and impact. Injury to the ankle may result in neuromuscular compromise.17,18 Nitz et al17 demonstrated electromyographic abnormalities of the peripheral nerves in the legs of patients with acute grade II and III ankle sprains 2 weeks after injury. The possible causes of nerve injury after ankle sprain include compartment syndrome, epineural hematoma, and nerve traction.17
Peroneal nerve-conduction velocities may be reduced 4 to 22 days after inversion trauma. Kleinrensink et al18 showed that superficial and deep peroneal motor nerve-conduction velocity was reduced for 4 to 8 days after inversion trauma. Careful attention must be given to protecting the ankle while progressing the patient through ROM, proprioceptive neuromuscular facilitation, and functional exercise during the acute phase of injury. Atrophy and compromised performance resulting from nerve injury should be considered.
Adequate strength is necessary for normal movement patterns. The importance of developing correct motor patterns while subjects perform flexibility and strength exercises cannot be overemphasized. The ability or inability to perform multiple tasks depends on our conscious awareness unless the tasks are automated.19 Regaining strength bilaterally is accepted clinical practice and is thought to be important for the prevention of ligamentous injuries at the ankle20; however, agreement on which strength factors are most important is still lacking. While some authors reported peroneal weakness as a factor in ankle sprains,21,22 others have noted no measurable difference13,23–25
Wilkerson et al26 and Baumhauer et al27 have shown that eversion-to-inversion strength ratios are often different in subjects with ankle instability when compared with normal subjects. An eversion-inversion strength ratio of >1.0 is considered an important indicator of ankle-sprain susceptibility.26,27 Kaminski et al24 examined ankle eversion concentric, eccentric, and isometric strength and found no difference between subjects with CAI and matched-paired controls. Further study has led to the investigation of reciprocal muscle-group ratios. Specifically, concentric eversion-to-eccentric inversion and eccentric eversion-to-concentric inversion muscle-group ratios have recently been examined in subjects with CAI and, while no differences were found between the involved and uninvolved ankles,28 eversion-to-inversion ratios were improved after a 6-week strength and proprioception training protocol.29
If the rehabilitation process is effective and the athlete regains preinjury ROM, strength, proprioceptive function, and motor control, then one would assume the risk of injury is reduced. If the rehabilitation process is not complete or a major component was not incorporated, then the athlete may be at an increased risk of reinjury.
PROPHYLACTIC ANKLE BRACING AND ORTHOTIC INTERVENTION
A prophylactic ankle brace is used to provide mechanical stability. Advantages include ease of use, no need for professional assistance with application, and cost effectiveness when compared with tape over an extended period of time.30 Ankle braces can be classified as lace-up, stirrup, or elastic type of configuration.30 In addition to providing mechanical stabilization, an ankle brace offers proprioceptive stimulation.30–32 Jerosch et al30 found improvement in single-leg stance, single-leg jumping, and angle reproduction when stirrup and lace-up brace conditions were compared with a no-tape condition. Interestingly, angle-reproduction error was better in the uninjured ankle than the injured ankle for the no-brace condition but better in the injured ankle when braced with a stirrup, lace-up, or tape than no brace. This implies that the application of the brace improved proprioceptive and sensory feedback such that accuracy was better in the injured ankle than the uninjured ankle with no external application.30
Friden et al14 examined 14 patients with unilateral injury to the lateral ligaments of the ankle and compared them with a group of 55 healthy individuals.14 Subjects were tested in single-leg stance for 25.6 seconds. They recorded movement in the frontal plane with the following variables: mean value of the distance between the center of pressure and the reference line, its standard deviation, average speed in frontal-sway movements, mean sway amplitude, and number of movements exceeding defined amplitude levels of 5 mm and 10 mm. The standard deviation was significantly higher in the injured group measured without braces when compared with the reference group, the injured group with brace, and the uninjured side. A significant difference was also noted between the uninjured side in the braced group and the reference group. Friden et al14 made a significant contribution by demonstrating that postural-sway values were sensitive enough to distinguish differences between subjects with the injured leg and a reference group. They found that when the injured legs were tested without a brace, they were significantly different than the reference group for the following variables: number of sway movements exceeding 5 mm and 10 mm, mean sway amplitude, and standard deviation of center of pressure.
Baier and Hopf31 evaluated the effect of a rigid or flexible ankle orthosis on postural sway in subjects with CAI. They tested 22 subjects with CAI and 22 normal subjects. CAI was defined as more than 5 ankle sprains per year and feelings of giving way. In athletes with CAI, both rigid and flexible ankle orthoses significantly reduced mediolateral sway velocity, an effect that was not apparent for the control group. While not significant, there was a trend toward decreased mediolateral sway in the control group when wearing the rigid orthosis versus no orthosis. Subjects were tested in single-leg stance for 25 seconds. Baier and Hopf31 speculated that the differences in the ankle-brace group were due not just to mechanical instability but also to a proprioceptive effect.
The study of braces to prevent injuries has been undertaken by Garrick and Requa,33 Sitler et al,34 and Surve et al.35 Sitler et al34 demonstrated a 3-fold decrease in ankle injuries among braced cadets when compared with nonbraced controls, and Surve et al35 reported a 5-fold reduction in ankle sprains when braced athletes were compared with nonbraced athletes who had previous ankle injuries. Therefore, the use of ankle taping and bracing has proprioceptive, mechanical, and injury-protection benefits and causes minimal to no performance decrements.36–38
Because the application of an ankle brace has been shown to increase joint position sense, it may be suggested that after an acute ankle sprain, initial exercises and ROM should be performed with some prophylactic support in an attempt to improve sensory and proprioceptive feedback. While this is common when preparing an athlete to return home or before competition, we recommend using a prophylactic stabilizer (neoprene, softshell, or hardshell) intermittently during functional rehabilitation to provide feedback, compression, and support (Figure 3). The presumed efficacy of this technique is based on clinical interpretation of the literature, and justification of rehabilitation outcomes needs further investigation.
Figure 3.
Use of external ankle support to provide stability and sensorimotor feedback during exercise (DJ Orthopaedics, Vista, CA).
The use of orthotics shows promise in the treatment of ankle instability, particularly in response to improving balance after injury39 or fatigue,40 when rearfoot motion is altered,41 and in normal subjects.42 In the clinical setting, orthotics are commonly prescribed for many reasons: to alter the rearfoot motion in the gait cycle, assist in shock absorption, and provide proprioceptive benefits. Recently, some authors have suggested that orthotics can be used clinically as an aid to postural stability. Guskiewicz and Perrin39 evaluated the use of orthotics after an acute ankle sprain. Orthotics significantly reduced postural sway between the orthotic and nonorthotic conditions during anteroposterior and mediolateral sway. Orteza et al43 assessed the effects of molded and unmolded orthotics on balance and pain after an inversion ankle sprain. Subjects reported significantly less pain during jogging while wearing molded orthotics compared with unmolded orthotics and no orthotics. Similarly, Ochsendorf et al40 reported a significant reduction in postural sway after orthotic intervention. The authors fatigued the plantar-flexor and dorsiflexor muscle groups and noted that postural-stability values for the orthotic conditions (prefatigue and postfatigue) were less (better) than for the nonorthotic conditions (prefatigue and postfatigue). Miller et al41 studied control subjects and subjects with malaligned rearfoot motion (>5° of rearfoot motion) for changes in postural sway during a 6-week period. Postural sway in the malaligned group with orthotics was initially worse than in the control group with orthotics. However, the use of orthotics improved bilateral (eyes-closed) postural sway in the malaligned group when values from baseline were compared with weeks 2, 4, and 6 (P < .05).
Therefore, we recommend the use of orthotics during the acute and subacute phases for subjects after an ankle sprain. The use of orthotics provides somatosensory benefits because cutaneous afferents contribute to human balance control44,45 and may provide neutral alignment for proper muscle activation and reduce unnecessary strain on already stressed soft tissue.45 If the athlete has abnormal rearfoot or forefoot alignment, the use of orthotics is justified for all activities. There is a paucity of information describing the use of orthotics for CAI and limited information describing long-term effectiveness in normal individuals and individuals with malalignment. This area needs further study to document functional outcome after an intervention.
FUNCTIONAL REHABILITATION
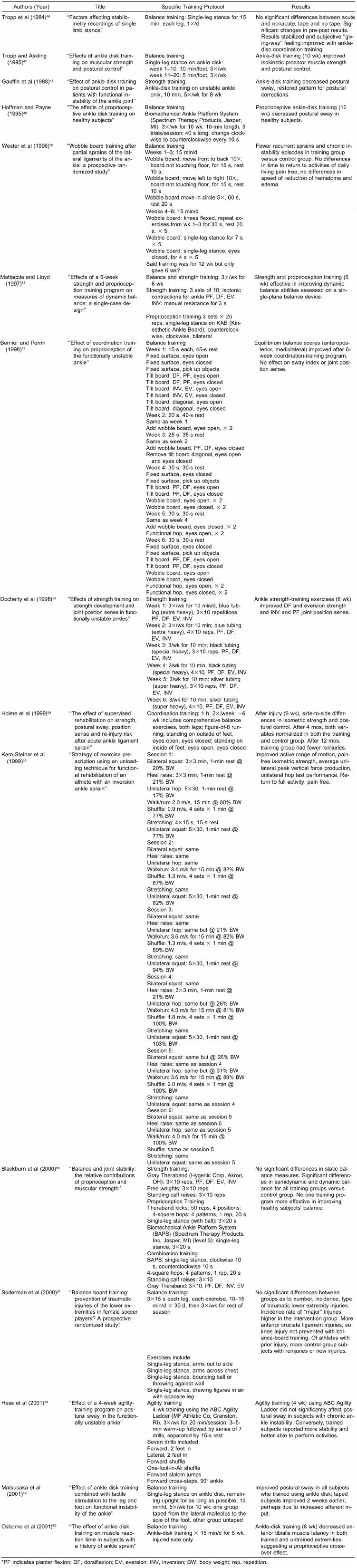
Many researchers have examined the effects of various training regimens on the characteristics of CAI and the symptoms of acute ankle sprains (Appendix). The available research regarding rehabilitation of ankle injuries and CAI ankle instability focuses on a wide variety of exercises and programs. Many experts have succeeded using a type of balance board to improve strength and balance measures in subjects with acute injury and CAI.46–50,57,59,60 Others have found that incorporating a variety of coordination-training exercises produces significant improvements in measures of strength and proprioception.52,54,56 And still others have found that strength training can be helpful in increasing not only ankle strength53,55 but also ankle-joint proprioception.53,56 While various investigators have shown that strength and balance training can be effective, a definitive series of outcome studies that document the number of treatments, the combination, and the volume of exercise necessary to return athletes to full function is lacking. The implications of such research are paramount as evidence for the effectiveness of management.
Appendix. Rehabilitation Articles on Acute and Chronic Ankle Instability
A secondary purpose of this manuscript was to present a functional-rehabilitation program drawing on concepts from the available literature. A rehabilitation program must be individualized to meet the needs of each athlete.1 While the importance of creating an individualized rehabilitation program cannot be overstressed, it is our opinion that an individualized rehabilitation program cannot be instituted without prior experience with a structured and well-designed rehabilitation program. Although the educational aims of many undergraduate and graduate programs are to develop clinicians who can be critical thinkers and decision makers, a health care professional can only design an individualized program for a particular patient after gaining substantial experience with a variety of well-structured, progressive rehabilitation programs. Therefore, we provide a structured rehabilitation program that is based on previous experience and empirical evidence. In addition, we supply some alternative concepts that are based on a review of the neuromuscular literature dealing with ankle rehabilitation, bracing, and postural control.
The significance of proper rehabilitation after an ankle sprain cannot be overemphasized, especially when considering the debilitating consequences of decreased ankle ROM, persistent pain, swelling, and CAI. Neglecting appropriate therapy may also precipitate the loss of work hours. In one study, a lack of rehabilitation resulted in several months' delay in return to military duty.61 A regimen of Achilles tendon stretching, progressive muscle strengthening, and proprioceptive training after acute treatment plays a pivotal role in hastening return to activity and preventing CAI.
Prolonged immobilization of ankle sprains is a common treatment error.62–64 Kerkhoffs et al62 recently examined the variation of practice with respect to the treatment of the acutely sprained ankle. They performed a formal, systematic review of the literature to scrutinize evidence-based management strategies for the treatment of the acute ankle sprain. Inclusion of the potential studies was independently assessed by 2 reviewers and, when appropriate, results of comparable studies were pooled. They found that immobilization alone should not be used to manage acute lateral ankle-ligament injuries. Kerkoffs et al62 reported statistically significant differences for the following outcomes when treatment with immobilization was compared with a functional treatment (based on the available literature): higher percentage of patients returned to work, the length of time elapsed before returning to work was shorter, fewer patients suffered from persistent swelling, fewer patients suffered from objective instability at follow-up, ROM was limited in fewer patients, and subjective satisfaction was higher.
Functional stress stimulates the incorporation of stronger replacement collagen.63 Functional rehabilitation begins on the day of injury and continues until pain-free gait and activities are attained. Functional rehabilitation has 4 aspects: ROM, strengthening, proprioception, and activity-specific training. Ankle-joint stability is a prerequisite to the institution of functional rehabilitation. Since grade I and grade II injuries are considered stable, functional rehabilitation should begin immediately.
RANGE-OF-MOTION AND STRENGTHENING EXERCISES
Range of motion must be regained before functional rehabilitation is initiated (Table 1). Achilles tendon stretching should be instituted within 48 to 72 hours of injury, regardless of weight-bearing capacity, in light of the tissue's tendency to contract after trauma (Figure 4). Once ROM is achieved and swelling and pain are controlled, the patient is ready to progress to the strengthening phase of rehabilitation. Strengthening of weakened muscles is essential to rapid recovery and is a preventive measure against reinjury.65 Exercises should focus on the conditioning of the peroneal muscles because insufficient strength in this group has been associated with CAI and recurrent injury.66 However, all muscles of the ankle should be targeted and all exercises performed bilaterally. If the training is performed bilaterally, we would expect substantial strength gains in both extremities, while the cross-over effect of training only 1 limb may equal only 1.5% to 3.5%.67 Strengthening begins with isometric exercises performed against an immovable object in 4 directions of ankle movement and progresses to dynamic resistive exercises using ankle weights, surgical tubing, or resistance bands.
Table 1. Recommended Guidelines for Early Functional Rehabilitation*
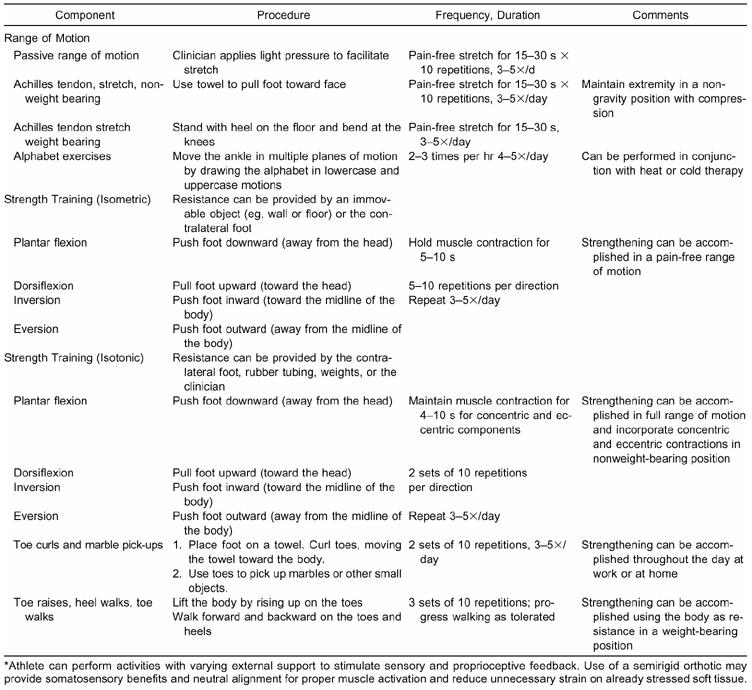
Figure 4.
Achilles stretching, A, weight bearing, and B, nonweight bearing.
Our opinion is that the strength components of many exercise programs would be more effective if performed with clinician-assisted manual resistance. It is common to see athletes perform hundreds of repetitions with various grades of exercise tubing, yet the targeted musculature is hardly fatigued (Figure 5). We recommend that manual resistance be applied for 3 to 5 seconds for 10 to 12 repetitions in each cardinal plane. While controlling the time that a maximal contraction is maintained, the clinician can be assured that the targeted musculature is being maximally loaded in a pain-free arc. Advanced exercises include asking the athlete to maximally resist randomly applied perturbations (Figure 6).
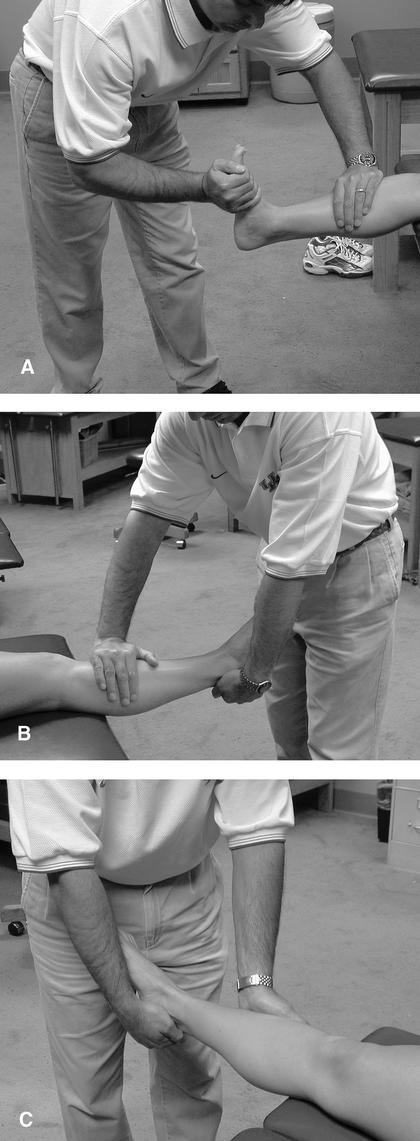
Figure 5.
Clinician-assisted manual resistance performed in pain-free range of motion. A, plantar flexion and dorsiflexion, B, eversion, and C, inversion.
Figure 6.
Manually applied perturbation into inversion and plantar flexion. Athlete is asked to quickly and forcefully resist the perturbation, and move the ankle into dorsiflexion and eversion.
If time is an issue and clinician-assisted manual resistance is not feasible, we recommend a progressive resistive program with weights rather than tubing. Table 2 provides a Daily Adjustable Progressive Resistance Exercise (DAPRE) strength progression for the ankle that was originally described by Knight68 and later modified by Perrin and Gieck.69 In this progression, the athlete performs 4 sets of 10 repetitions while increasing the applied weight for each set. The athlete can advance to the next level when he or she can lock out (complete with correct form) the 4th set 10 times. With a structured progression, the athlete can create continuous goals and more easily appreciate improvements. These exercises should be performed with an emphasis on the eccentric component.66 Patients should be instructed to pause 1 second between the concentric and eccentric phases of exercise and perform the eccentric component over a 4-second period. Concentric contraction refers to the active shortening of muscle with resultant lengthening of the resistance band, while eccentric contraction involves the passive lengthening of the muscle by the elastic pull of the band. Resistive exercises should be performed (2 to 3 sets of 10 to 12 repetitions) in all 4 directions twice a day. Toe raises, heel walks, and toe walks may also be attempted to regain strength and coordination (Figure 7). Continual monitoring of strength is important. Isokinetic strength testing is an accepted method of assessing ankle strength.24,70–72 Less expensive, yet often overlooked, is the use of hand-held dynamometry for consistent monitoring of strength performance.73
Table 2. Strength-Training Progression*
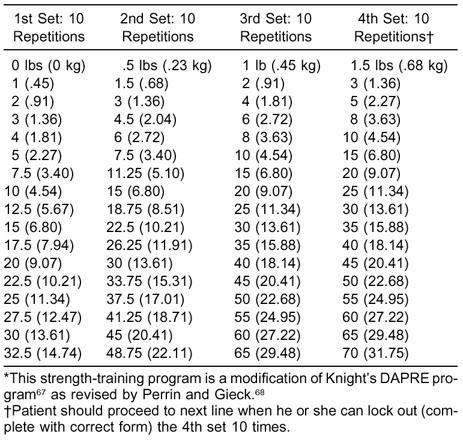
Figure 7.
Walking on the heel, A, and toes, B, for assessment of ability to bear weight and maintain balance. This can be used as a gross measure of functional status and as an intermediate rehabilitation exercise.
PROPRIOCEPTIVE AND BALANCE TRAINING
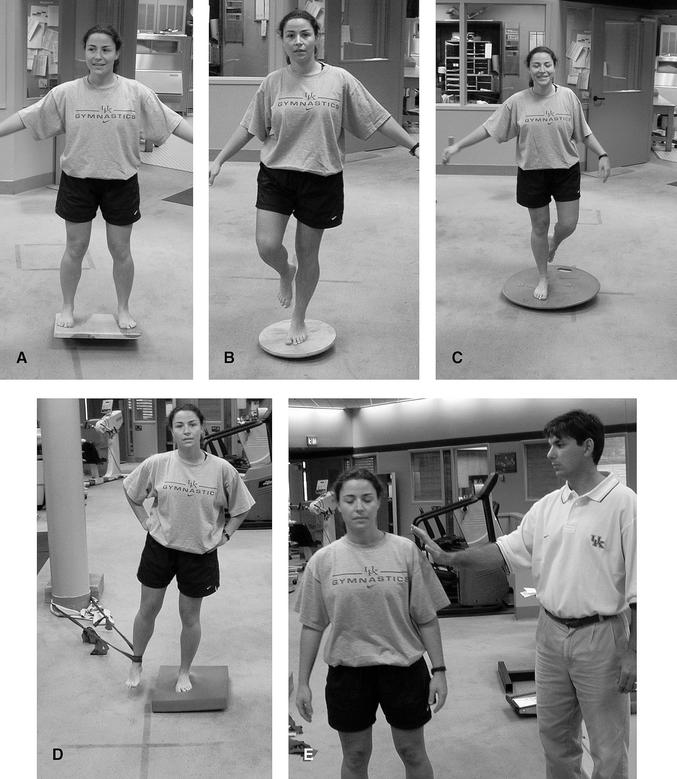
As the patient achieves full weight bearing without pain, proprioceptive training is initiated for the recovery of balance and postural control (Table 3). Various devices have been specifically designed for this phase of rehabilitation, and their use in concert with a series of progressive drills has effectively returned patients to a high functional level.51,74 The simplest device for proprioceptive training is the wobble board, a small discoid platform attached to a hemispheric base.75 The patient is instructed to stand on the wobble board on 1 foot and shift his or her weight, causing the disc's edge to scribe a continuous circular path (Figure 8). These exercises can be progressed by having the patient use different-sized hemispheres and by varying visual input. In addition, the athlete can be tested under various visual and support conditions (Figure 9). As somatosensory and visual feedback is altered, the athlete must develop consistent motor patterns despite inconsistent feedback. A common progression when performing balance exercise is to move from a position of nonweight bearing to weight bearing, bilateral stance to unilateral stance, eyes open to eyes closed, firm surface to soft surface, uneven or moving surface (Table 4). The variation of surfaces and conditions is vast, allowing the clinician ample opportunity to offer fresh challenges during the rehabilitation process. For example, the use of turbine-produced resistance in water offers an unstable yet forgiving environment (Figure 10). If time is available, the clinician can manually move the ankle and foot through various positions and then request that the athlete actively and passively replicate joint angles. While the body reacts to perturbations in various ways (feed-forward versus feedback response), sensory input is received from all parts of the body and sent to the central nervous system via afferent pathways. Therefore, conscious and unconscious appreciation is important to protect functional joint stability. Proprioception is useful for preventing injury in slow, moderately rapid, or even rapid tasks; however, it may not be adequate for forces that challenge the neuromuscular system at the highest levels.76 A common mistake when performing proprioception and balance exercises is the lack of variability in speed and intensity. There are various methods of assessing improvements in joint position sense, postural stability, and threshold to detection of motion.77,78
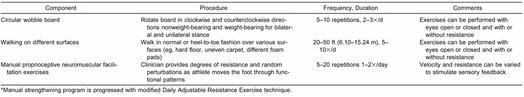
Table 3. Proprioceptive Training Components of Intermediate Functional Rehabilitation*
Figure 8.
Balance exercises can be performed on different surfaces, A and B, and with eyes open or closed, C, and can be progressed to active movements that invoke perturbations while maintaining balance, D, and perturbations invoked externally, E.
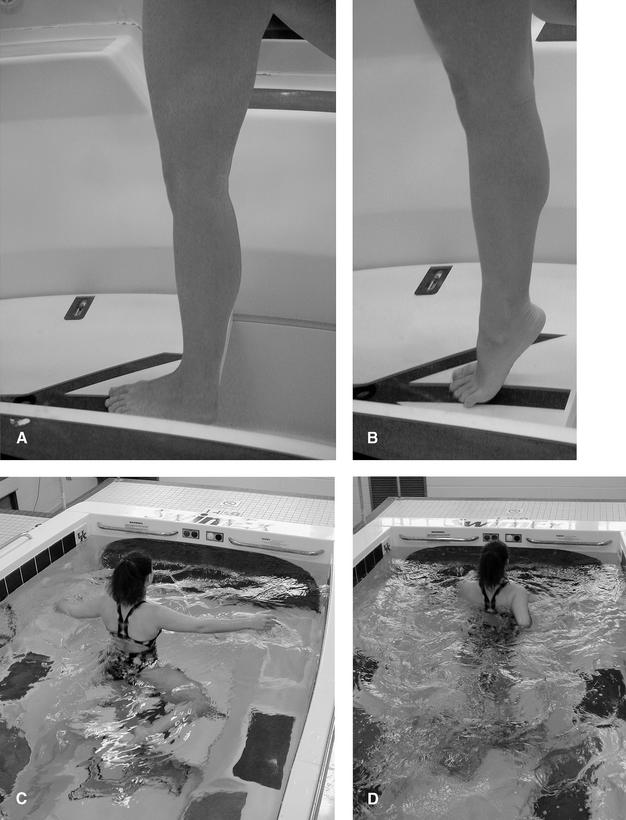
Figure 9.
A and B, Advanced balance and functional exercise with internal provoked perturbations while performing dynamic activities.
Table 4. Return to Activity Components of Advanced Functional Rehabilitation
Figure 10.
Exercise in water reduces compressive forces and supports injured tissue. A and B, Exercises can be initiated without resistance and then progressed, C, to resistance until D, functional exercises can be performed.
RETURN TO ACTIVITY-SPECIFIC TRAINING
When the distance walked by the patient is no longer limited by pain, he or she may progress to a regimen of 50% walking and 50% jogging (see Table 4). Using the same criteria, jogging eventually progresses to running, backward running, and pattern running. Circles and figures of 8 are commonly employed patterns. The final phase of the rehabilitation process is documentation that the athlete can perform sport-specific exercises pain free and at a level consistent with preinjury status. Although time consuming, these routines represent the final phase of ankle-joint rehabilitation, and completion of this program is essential for the recovery of ankle stability. In short, clinicians need to create exercises and movement patterns that will increasingly challenge the neuromuscular coordination of the injured athlete.
CONCLUSIONS
Rehabilitation of ankle injuries should be structured and individualized. In the acute phase, the focus should be on controlling inflammation, reestablishing full range of motion, and gaining strength. Once pain-free range of motion and weight bearing have been established, balance-training exercises should be incorporated to normalize neuromuscular control. Advanced-phase rehabilitation activities should focus on regaining normal function. This includes exercises specific to those that will be performed during sport. While having a basic template to follow for the rehabilitation of ankle injuries is important, clinicians must remember that individuals respond differently to exercises. Therefore, each program needs to be modified to fit the individual's needs.
REFERENCES
- Andrews J R, Harrelson G L, Wilk K E. 2nd ed WB Saunders; Philadelphia, PA: 1998. Physical Rehabilitation of the Injured Athlete. [Google Scholar]
- Andriacchi T, Sabiston P, DeHaven K, et al. Ligament: injury and repair. In: Woo S L, Buckwalter J A, editors. Injury and Repair of the Musculoskeletal Soft Tissues. American Academy of Orthopaedic Surgeons; Park Ridge, IL: 1987. pp. 103–128. [Google Scholar]
- Martinez-Hernandez A, Amenta P S. Basic concepts in wound healing: clinical and basic science concepts. In: Leadbetter W B, Buckwalter J A, Gordon S L, editors. Sports-Induced Inflammation. American Academy of Orthopaedic Surgeons; Park Ridge, IL: 1990. pp. 55–102. [Google Scholar]
- Kegerreis S. The construction and implementation of functional progression as a component of athletic rehabilitation. J Orthop Sports Phys Ther. 1983;5:14–19. doi: 10.2519/jospt.1983.5.1.14. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Olesen S, Hansen H M. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26:72–77. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Barrack R L, Skinner H B, Cook S D, Haddad R J. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol. 1983;50:684–687. doi: 10.1152/jn.1983.50.3.684. [DOI] [PubMed] [Google Scholar]
- Anacker S L, Di Fabio R P. Influence of sensory inputs on standing balance in community-dwelling elders with a recent history of falling. Phys Ther. 1992;72:575–584. doi: 10.1093/ptj/72.8.575. [DOI] [PubMed] [Google Scholar]
- Skinner H B, Barrack R L, Cook S D. Age-related decline in proprioception. Clin Orthop. 1984;184:208–211. [PubMed] [Google Scholar]
- Freeman M A, Dean M R, Hanham I W. The etiology and prevention of functional instabilities of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Ryan L. Mechanical instability, muscle strength, and proprioception in the functionally unstable ankle. Austral J Physiother. 1994;40:41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- Friden T, Zatterstrom R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle? Br J Sports Med. 1997;31:65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella S, Harrison D. A study to examine the balance of subjects with recurrent ankle sprains. Physiother Ireland. 1998;19:9–13. [Google Scholar]
- Nitz A J, Dobner J J, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med. 1985;13:177–182. doi: 10.1177/036354658501300306. [DOI] [PubMed] [Google Scholar]
- Kleinrensink G J, Stoeckart R, Meulstee J, et al. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med Sci Sports Exerc. 1994;26:877–883. [PubMed] [Google Scholar]
- Tononi G, Edelman G M. Consciousness and complexity. Science. 1998;282:1846–1851. doi: 10.1126/science.282.5395.1846. [DOI] [PubMed] [Google Scholar]
- Kaumeyer G, Malone T R. Ankle injuries: anatomical and biomechanical considerations necessary for the development of an injury prevention program. J Orthop Sports Phys Ther. 1980;1:171–177. doi: 10.2519/jospt.1980.1.3.171. [DOI] [PubMed] [Google Scholar]
- Balduini F C, Vegso J J, Torg J S, Torg E. Management and rehabilitation of ligamentous injuries to the ankle. Sports Med. 1987;4:364–380. doi: 10.2165/00007256-198704050-00004. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- Lentell G L, Katzman L L, Walters M R. The relationship between muscle function and ankle stability. J Orthop Sports Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H, Gansneder B M. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34:239–245. [PMC free article] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H, Rijke A M. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- Wilkerson G B, Pinerola J J, Caturano R W. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997;26:78–86. doi: 10.2519/jospt.1997.26.2.78. [DOI] [PubMed] [Google Scholar]
- Baumhauer J F, Alosa D M, Renström F H, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;223:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- Buckley B D, Kaminski T W, Powers M E, Ortiz C, Hubbard T J. Using reciprocal muscle group ratios to examine isokinetic strength in the ankle: a new concept [abstract] J Athl Train. 2001;36(suppl):S-93. [Google Scholar]
- Kaminski T W, Powers M E, Buckley B D, Hubbard T J, Ortiz C. The influence of strength and proprioception training on strength and postural stability in individuals with unilateral functional ankle instability [abstract] J Athl Train. 2001;36(suppl):S-93. [Google Scholar]
- Jerosch J, Hoffstetter I, Bork H, Bischof M. The influence of orthoses on the proprioception of the ankle joint. Knee Surg Sports Traumatol Arthrosc. 1995;3:39–46. doi: 10.1007/BF01553524. [DOI] [PubMed] [Google Scholar]
- Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Arch Phys Med Rehabil. 1998;79:939–944. doi: 10.1016/s0003-9993(98)90091-0. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Ravn J B, Sorensen A I. Proprioception at the ankle: the effect of anaesthetic blockade of ligament receptors. J Bone Joint Surg Br. 1993;75:433–436. doi: 10.1302/0301-620X.75B3.8496215. [DOI] [PubMed] [Google Scholar]
- Garrick J G, Requa R K. Role of external support in the prevention of ankle sprains. Med Sci Sports. 1973;5:200–203. [PubMed] [Google Scholar]
- Sitler M R, Ryan J, Wheeler B, et al. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball: a randomized clinical study at West Point. Am J Sports Med. 1994;22:454–461. doi: 10.1177/036354659402200404. [DOI] [PubMed] [Google Scholar]
- Surve I, Schwellnus M P, Noakes T, Lombard C. A fivefold reduction in the incidence of recurrent ankle sprains in soccer players using the Sport-Stirrup orthosis. Am J Sports Med. 1994;22:601–606. doi: 10.1177/036354659402200506. [DOI] [PubMed] [Google Scholar]
- Bocchinfuso C, Sitler M R, Kimura I F. Effects of two semirigid prophylactic ankle stabilizers on speed, agility, and vertical jump. J Sport Rehabil. 1994;3:125–134. [Google Scholar]
- Macpherson K, Sitler M R, Kimura I F, Horodyski M. Effects of a semirigid and softshell prophylactic ankle stabilizer on selected performance tests among high school football players. J Orthop Sports Phys Ther. 1995;21:147–152. doi: 10.2519/jospt.1995.21.3.147. [DOI] [PubMed] [Google Scholar]
- Pienkowski D, McMorrow M, Shapiro R, Caborn D N, Stayton J. The effect of ankle stabilizers on athletic performance: a randomized prospective study. Am J Sports Med. 1995;23:757–762. doi: 10.1177/036354659502300621. [DOI] [PubMed] [Google Scholar]
- Guskiewicz K M, Perrin D H. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23:326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- Ochsendorf D T, Mattacola C G, Arnold B L. Effect of orthotics on postural sway after fatigue of the plantar flexors and dorsiflexors. J Athl Train. 2000;35:26–30. [PMC free article] [PubMed] [Google Scholar]
- Miller A K, Mattacola C G, Uhl T L, McCrory J L, Malone T R. Effect of orthotics on postural stability over a six week acclimation period [abstract] J Athl Train. 2001;36(suppl):S-67. [Google Scholar]
- Hertel J, Denegar C, Buckley W E, Sharkey N A, Stokes W L. Effect of rear-foot orthotics on postural control in healthy subjects. J Sport Rehabil. 2001;10:36–47. [Google Scholar]
- Orteza L C, Vogelbach W D, Denegar C R. The effect of molded and unmolded orthotics on balance and pain while jogging following inversion ankle sprain. J Athl Train. 1992;27:80–84. [PMC free article] [PubMed] [Google Scholar]
- Kavounoudias A, Roll R, Roll J P. The plantar sole is a ‘dynamometric map’ for human balance control. Neuroreport. 1998;9:3247–3252. doi: 10.1097/00001756-199810050-00021. [DOI] [PubMed] [Google Scholar]
- Nigg B M, Nurse M A, Stefanyshyn D J. Shoe inserts and orthotics for sport and physical activities. Med Sci Sport Exerc. 1999;31(suppl):421–428. doi: 10.1097/00005768-199907001-00003. [DOI] [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- Tropp H, Askling C. Effects of ankle disk training on muscular strength and postural control. Clin Biomech. 1988;3:88–91. doi: 10.1016/0268-0033(88)90050-2. [DOI] [PubMed] [Google Scholar]
- Gauffin H, Tropp H, Odendrick P. Effect of ankle disk training on postural control in patients with functional ankle instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- Hoffman M, Payne V G. The effects of proprioceptive ankle disk training on healthy subjects. J Orthop Sports Phys Ther. 1995;21:90–93. doi: 10.2519/jospt.1995.21.2.90. [DOI] [PubMed] [Google Scholar]
- Wester J U, Jespersen S M, Nielsen K D, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- Mattacola C G, Lloyd J W. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32:127–135. [PMC free article] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27:264–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]
- Docherty C, Moore J, Arnold B. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33:310–314. [PMC free article] [PubMed] [Google Scholar]
- Holme E, Magnusson S P, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- Kern-Steiner R, Washecheck H S, Kelsey D D. Strategy of exercise prescription using an unloading technique for functional rehabilitation of an athlete with an inversion ankle sprain. J Orthop Sports Phys Ther. 1999;29:282–287. doi: 10.2519/jospt.1999.29.5.282. [DOI] [PubMed] [Google Scholar]
- Blackburn J T, Guskiewicz K M, Petschauer M, Prentice W. Balance and joint stability: the relative contributions of proprioception and muscular strength. J Sport Rehabil. 2000;9:315–328. [Google Scholar]
- Soderman K, Werner S, Pietila T, Engstrom B, Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8:356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- Hess D, Joyce C, Arnold B, Gansneder B. Effect of a 4-week agility-training program on postural sway in the functionally unstable ankle. J Sport Rehabil. 2001;10:24–35. [Google Scholar]
- Matsusaka N, Yokoyama S, Tsurusaki T, Inokuchi S, Okita M. Effect of ankle disk training combined with tactile stimulation to the leg and foot on functional instability of the ankle. Am J Sports Med. 2001;29:25–30. doi: 10.1177/03635465010290010901. [DOI] [PubMed] [Google Scholar]
- Osborne M, Chou L S, Laskowski E R, Smith J, Kaufman K R. The effect of ankle disk training on muscle reaction time in subjects with a history of ankle sprain. Am J Sports Med. 2001;29:627–632. doi: 10.1177/03635465010290051601. [DOI] [PubMed] [Google Scholar]
- Weinstein M L. An ankle protocol for second-degree ankle sprains. Mil Med. 1993;158:771–774. [PubMed] [Google Scholar]
- Kerkhoffs G M, Rowe B H, Assendelft W J, Kelly K D, Struijs P A, van Dijk C N. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462–471. doi: 10.1007/s004020100283. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Lundin O, Lind K, Styf J. Early mobilization versus immobilization after ankle ligament stabilization. Scand J Med Sci Sports. 1999;9:299–303. doi: 10.1111/j.1600-0838.1999.tb00250.x. [DOI] [PubMed] [Google Scholar]
- Dettori J R, Pearson B D, Basmania C J, Lednar W M. Early ankle mobilization, part I: the immediate effect on acute, lateral ankle sprains (a randomized clinical trial) Mil Med. 1994;159:15–20. [PubMed] [Google Scholar]
- Thacker S B, Stroup D F, Branche C M, Gilchrist J, Goodman R A, Weitman E A. The prevention of ankle sprains in sports: a systematic review of the literature. Am J Sports Med. 1999;27:753–760. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- Hartsell H D, Spaulding S J. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med. 1999;33:255–258. doi: 10.1136/bjsm.33.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uh B S, Beynnon B D, Helie B V, Alosa D, Renström P A. The benefit of a single-leg strength training program for the muscles around the untrained ankle: a prospective, randomized, controlled study. Am J Sports Med. 2000;28:568–573. doi: 10.1177/03635465000280042101. [DOI] [PubMed] [Google Scholar]
- Knight K L. Knee rehabilitation by the daily adjustable progressive resistive exercise technique. Am J Sports Med. 1979;7:336–337. doi: 10.1177/036354657900700605. [DOI] [PubMed] [Google Scholar]
- Perrin D H, Gieck J H. Principles of therapeutic exercise. In: Perrin D H, editor. The Injured Athlete. 3rd ed. Lippincott-Raven; Philadelphia, PA: 1999. pp. 123–139. [Google Scholar]
- Perrin D H. Human Kinetics; Champaign, IL: 1993. Isokinetic Exercise and Assessment; p. 59. [Google Scholar]
- Kaminski T W, Perrin D H, Mattacola C G, Szczerba J E, Bernier J N. The reliability and validity of ankle inversion and eversion torque measurements from the Kin Com II isokinetic dynamometer. J Sport Rehabil. 1995;4:210–218. [Google Scholar]
- Wilkerson G B, Horn-Kingery H M. Treatment of the inversion ankle sprain: comparison of different modes of compression and cryotherapy. J Orthop Sports Phys Ther. 1993;17:240–246. doi: 10.2519/jospt.1993.17.5.240. [DOI] [PubMed] [Google Scholar]
- Kimura I F, Jefferson L M, Gulick D T, Coll R D. Intra- and intertester reliability of Chatillon and Microfet hand-held dynamometers in measuring force production. J Sport Rehabil. 1996;5:197–205. [Google Scholar]
- Bahr R, Lian O, Bahr I A. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7:172–177. doi: 10.1111/j.1600-0838.1997.tb00135.x. [DOI] [PubMed] [Google Scholar]
- Hintermann B. Biomechanics of the unstable ankle joint and clinical implications. Med Sci Sports Exerc. 1999;31(7 suppl):459–469. doi: 10.1097/00005768-199907001-00007. [DOI] [PubMed] [Google Scholar]
- Ashton-Miller J A, Wojtys E M, Huston L J, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- Riemann B L. Is there a link between chronic ankle instability and postural instability? J Athl Train. 2002;37:386–393. [PMC free article] [PubMed] [Google Scholar]
- Konradsen L. Factors contributing to chronic ankle instability: kinesthesia and joint position sense. J Athl Train. 2002;37:381–385. [PMC free article] [PubMed] [Google Scholar]