Abstract
Objective: To review the surgical indications, techniques, biomechanical testing, and clinical results reported for the most common surgical techniques used to treat ankle instability.
Data Sources: We searched MEDLINE from 1960–2001 using the terms ankle instability, functional ankle instability, mechanical ankle instability, ankle ligament surgery, Broström, Chrisman-Snook, and Evans.
Data Synthesis: Although 80% to 85% of acute ankle sprains are successfully treated with a functional ankle-rehabilitation program, the remaining 15% to 20% have recurrent ankle instability and reinjury, necessitating surgical intervention. The fundamentals of the surgical approach to lateral ankle instability are based on the anatomy of the lateral ankle ligaments, the anterior talofibular ligament, and the calcaneofibular ligament. Ankle-instability surgery has been broadly divided into an anatomic repair consisting of an imbrication of the lateral ligamentous complex and an ankle-ligament reconstruction. An ankle-ligament reconstruction weaves a harvested tendon graft, most commonly the peroneus brevis, to augment the lateral ligaments of the ankle. Goals of surgery are to reestablish ankle stability and function without compromising motion and without complications. Anatomic repair and imbrication of the lateral ligament complex with the Gould modification has an 85% to 95% success rate, and the risk of associated nerve injuries is low. This approach provides increased stability by reinforcing local host tissue, preserving subtalar and talocrural motion, eliminating the comorbidity associated with tendon-graft harvest, and offering a quicker functional recovery. One concern in using the anatomic approach is the resultant strength of the repair, although the literature does not support this concern. Ankle-reconstruction procedures that sacrifice tendons are thought to provide a stronger construct, and hence, more stability. This increased stability results in loss of talocrural and subtalar range of motion, prolonging recovery and decreasing sport performance. Adjacent nerve injury is more common with ankle-ligament reconstruction.
Conclusions/Recommendations: Based on the literature, we believe that a modified Broström lateral-ligament repair should be considered the first choice for persistent ankle instability refractory to a functional ankle-rehabilitation protocol. Ankle reconstruction with tendon augmentation should be reserved for patients with generalized ligamentous laxity or long-standing ligamentous insufficiency or as a salvage procedure in a patient with a failed modified Broström lateral-ligament repair.
Keywords: Broström procedure, Chrisman-Snook procedure, Evans procedure
The primary static restraints to an inversion injury mechanism are the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL). These ligaments make up a portion of the lateral ligamentous complex and help to prevent inversion of the talus during plantar flexion and dorsiflexion of the ankle.1
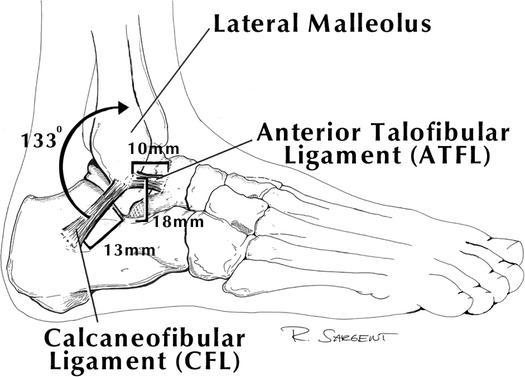
Burks and Morgan2 have described the anatomy of the ATFL and CFL, which demonstrate considerable anatomic variation. This anatomic variation in ligament position has been hypothesized as one factor predisposing individuals to chronic ankle instability.2,3 Burks and Morgan2 found that the ATFL originates 1 cm proximal to the tip of the lateral malleolus. The ligament averages 7.2 mm in width and inserts into the talus just distal to the articular surface, 18 mm proximal to the subtalar joint. The ATFL is contiguous with the joint capsule and not easily defined in patients who have sustained repetitive inversion sprains. The CFL originates adjacent to the ATFL, approximately 8 mm proximal to the tip of the fibula, and courses posterior and distal to the calcaneus. The angle at which the ligament lies in relation to the fibula is somewhat variable, averaging 133° (range, 113° to 150°) in a neutral ankle position. The CFL inserts onto the calcaneus 13 mm distal to the subtalar joint. The CFL ligament is an extracapsular ligament and makes up the floor of the peroneal sheath (Figure 1).
Figure 1.
Anatomy of the anterior talofibular and calcaneofibular ligaments of the ankle.
The ATFL is the primary restraint to inversion of the ankle throughout its arc of motion. Strain of the ATFL increases progressively as the ankle moves into plantar flexion and inversion. As a result, the ATFL is usually torn in inversion, plantar flexion, and internal rotation. The CFL stabilizes both the ankle joint and the subtalar joint. Strain in the CFL is greatest when the ankle is inverted and dorsiflexed. The CFL tears primarily in inversion and ankle dorsiflexion.1 Surgical repairs to correct lateral ankle instability should include repair and augmentation of the CFL if subtalar instability is suspected.4
The posterior talofibular ligament (PTFL) and the lateral talocalcaneal ligament (LTCL) are of less clinical significance in lateral ankle instability. The PTFL originates on the posteromedial aspect of the distal fibula and is directed posteromedially to the posterior process of the talus. The PTFL is rarely injured as the result of inversion and does not require reconstruction. The LTCL may or may not be present; when present, it limits subtalar motion.3
The pattern of ligamentous injury with an inversion mechanism has been well described.5,6 The most common mechanism of ankle sprains involves inversion and stress to the anterolateral capsule. The ATFL and CFL are then consecutively injured, depending on the energy and severity of the injury. Rasmussen,6 in a cadaveric study, noted that the ATFL was always torn when the CFL was torn. Similarly, Broström5 found no isolated tears of the CFL in 60 patients examined surgically.
The task of repairing or reconstructing unstable lateral ankle ligaments is challenging. The surgical approach requires restoration of the anatomic alignment and static functions of the ATFL and CFL. The repair should be durable and stable and allow for functional range of motion of the ankle and hindfoot. The repair should also avoid nerve injury and minimize damage to adjacent host tissue.
INDICATIONS
The initial management of patients with an acute inversion ankle sprain is nonoperative. After the early injury phase, functional rehabilitation begins and includes range of motion for the ankle and hindfoot, concentric and eccentric muscle strengthening, endurance training with particular attention to the peroneal musculature, and proprioceptive training. Proprioceptive exercises improve dynamic stability and are an essential part of the rehabilitation program.7 Functional bracing or taping may be useful to help prevent recurrent injury during “at-risk” activities. Most athletes can be treated successfully with rehabilitation and protective bracing.3
Surgery should be considered only if symptoms persist after a functional rehabilitation program for the ankle. These symptoms may include a feeling of “giving way,” defined as functional instability, or true mechanical instability demonstrated by provocative tests such as the anterior drawer or talar tilt, either clinically or with stress radiography. Similar surgical procedures have been described for both. Particular attention is needed to diagnose and correct subtle subtalar instability in individuals with functional instability.
SURGICAL CONSIDERATIONS
Various surgical approaches have been taken to lateral ankle instability. Understanding the differences in techniques is important to individualizing each patient's treatment and rehabilitation. Preoperative assessment of ankle instability includes an evaluation of extremity alignment. Secondary anatomic findings, such as hindfoot varus or generalized ligamentous laxity, are associated with a higher prevalence of chronic ankle sprains. Manual muscle-strength testing of the peroneal and anterior tibial muscles is performed and compared with the contralateral limb (if uninjured). No isolated ligament-stabilizing procedure will be successful in the presence of hindfoot varus malalignment or a primary motor weakness, such as occurs with common peroneal nerve injury. The modified criteria of Beighton et al8 allow for generalized ligamentous laxity testing. With generalized ligamentous laxity, tenodesis procedures are favored. A thorough history reviewing any previous surgery of the ankle and the duration of the instability problem should be obtained.3 Poorer results have been found in ligament repairs with increased duration of symptoms, prior surgery, and connective tissue disorders (eg, ligamentous laxity).
Ankle-instability surgeries fall into 2 broad categories: anatomic repair of the lateral-ligament complex and nonanatomic repair consisting of an ankle reconstruction using tendon-weave procedures.
SURGICAL TECHNIQUES
Anatomic Repair
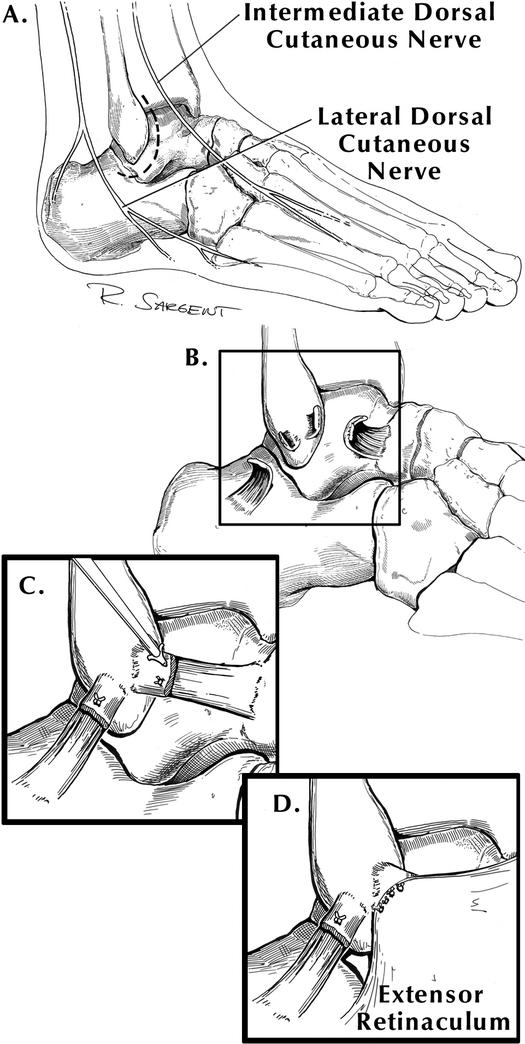
Anatomic repairs attempt to reconstruct the normal anatomy by imbricating the existing joint capsule and lateral ligaments. In 1966, Broström5 reported on direct late repair of the lateral ankle ligaments in 60 patients with chronic ankle instability. The torn ends of the ATFL were shortened and repaired directly by midsubstance suturing; in 30% of patients, the CFL was also repaired. He reported a success rate of 80% with this technique.5 This technique is the foundation of the anatomic repair (Figure 2). Variations of this procedure include imbrication of the midsubstance of the lateral ligaments and modifications in the suturing of the ligaments through drill holes in the fibula, with or without reinforcement with fibular periosteum. The functional outcomes have been excellent, reported as high as 87% to 95% success rates.5,9–13 Outcome variables have included range of motion, strength, return to preinjury activity level, need for reoperation, and complications.
Figure 2.
(A) Anatomy of the superficial peroneal nerve branches (intermediate and lateral dorsal cutaneous nerves) in relationship to the Broström anatomic repair incision (dotted lines). (B) Midsubstance tear of the anterior talofibular and calcaneofibular ligaments. (C) The Broström ligament repair of the anterior talofibular and calcaneofibular ligaments. (D) The Gould modification of the Broström ligament repair, mobilizing the proximal aspect of the inferior extensor retinaculum.
Gould et al10 reported on a subsequent modification to the Broström procedure (Figure 2D) involving the mobilization and reattachment of the lateral portion of the extensor retinaculum to the fibula after imbrication of the ATFL and CFL ligaments. This provided additional talocrural and, secondarily, subtalar joint stability and was to be performed in any patient requiring a Broström ligament repair. Hamilton et al14 noted excellent results in professional ballet dancers and recreational athletes with the Gould modification of the Broström procedure. This finding extended the indications for this procedure into a high-level athletic patient population.
Karlsson et al11 reported on a modified Broström repair in which some patients received isolated ATFL imbrication and some received CFL and ATFL combined repairs. Excellent or good results were obtained in 80% of the patients, with improved mechanical stability as evidenced on stress radiographs. Most of the unsatisfactory results were in patients with generalized ligamentous laxity, long-standing ligamentous insufficiency, or a previous operation. Better functional results were obtained with repair of both ligaments than with an isolated repair of the ATFL. Karlsson et al11 recommended routine combined repair of both ligaments.
The benefits of an anatomic repair include the simple surgical approach, the utilization of local host anatomy while preserving talocrural and subtalar motion, and fewer complications. The most severe complication, although quite rare, is injury to the superficial peroneal or sural nerve.
Reconstructive Tenodesis
Nonanatomic reconstructions use tendon or other types of grafts to tighten the lateral ankle. Despite attempts by the surgeon, these grafts have not been found to follow the orientation of the normal ligaments. The most common graft procedures involve a weave of the peroneus brevis tendon. The Chrisman-Snook procedure most closely approximates the ATFL and CFL anatomically. The Evans procedure has been used to augment the modified Broström in special cases. The greatest limitation of these procedures is the decrease in subtalar and, to a lesser extent, talocrural motion and the increased risk of adjacent cutaneous nerve injury. These procedures sacrifice all or a portion of the peroneus brevis, which is important in dynamic stability of the ankle.
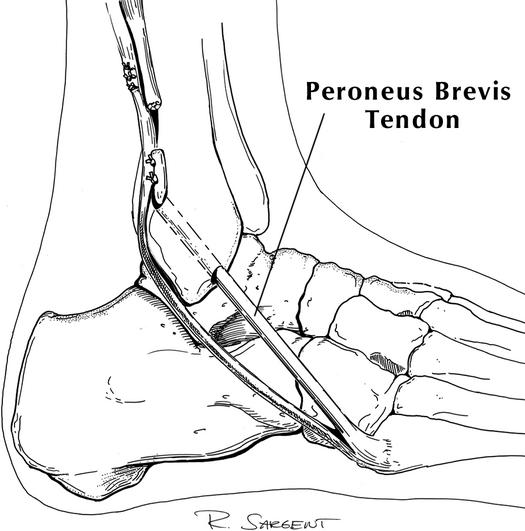
The Evans procedure involves harvesting either half or the entire peroneus brevis tendon proximally and leaving it attached to the fifth metatarsal base distally. The free arm is then passed anterior to posterior through a drill hole in the distal fibula or placed over the anterior fibula and sutured to the periosteum, as originally described by Evans, then anchored to itself (Figure 3). The position of the foot and the amount of tension applied during the suturing influence the degree of stability and the degree of restriction of subtalar motion. Anatomically, the position of this tendon weave does not recreate the ATFL or CFL but lies somewhere in between. While ankle dorsiflexion and plantar flexion are minimally altered with this procedure, anterior translation of the talus is not well controlled and subtalar motion is decreased.3
Figure 3.
An Evans reconstructive lateral ankle tenodesis. One half of the proximal peroneus brevis tendon is harvested, leaving it attached distally to the fifth metatarsal base. The proximal end is weaved anterior to posterior through a drill hole in the fibula and sutured to itself.
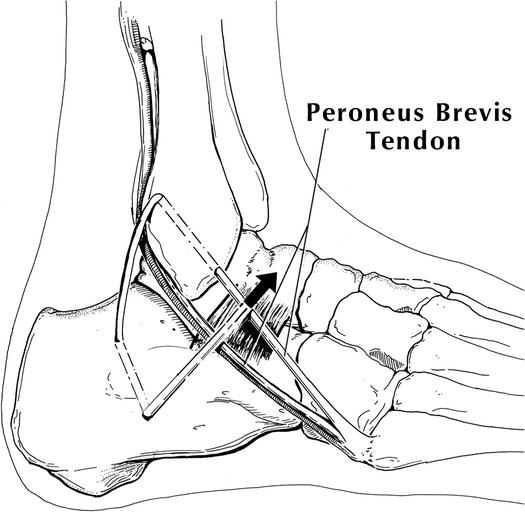
The procedure described by Chrisman and Snook uses a split peroneus brevis tendon detached proximally, thus preserving dynamic function of the muscle. The graft is brought through the fibula anterior to posterior, then placed through a drill hole in the calcaneus and sutured to itself (Figure 4). If performed as originally described, the procedure limits subtalar motion.
Figure 4.
The Chrisman-Snook reconstructive lateral ankle tenodesis. One half of the proximal aspect of the peroneus brevis tendon is harvested, leaving it attached distally to the fifth metatarsal base. The proximal tendon is weaved anterior to posterior through a drill hole in the fibula and posterior to anterior in a calcaneal bone tunnel and sutured to itself in the region of the anterior talofibular ligament.
In 1985, Snook et al15 reported a modification of their procedure in which extensive tightening of the graft is avoided to allow more subtalar motion. In addition, they recommended that the graft insertion into the calcaneus be moved posteriorly to more closely approximate the course of the CFL and avoid overconstraint of talocrural and subtalar motion. They presented a 10-year follow-up with excellent results in 38 of 48 ankles. All patients with fair or poor results had a severe reinjury. Leach et al16 described a further modification of this reconstruction incorporating the anterior limb of the graft into the ATFL to more nearly replicate the orientation of the ligament. Colville and Grondel17 performed the Chrisman-Snook procedure on cadaveric ankles, which were then dissected to see how closely the reconstruction paralleled the normal courses of the ATFL and CFL. Due to the broad variation in the positioning of these ligaments, the reconstructions deviated significantly from anatomic alignment in a large number of limbs.
The benefits of an extra-anatomic reconstruction include increased strength of the reconstruction in patients in whom the ligaments are attenuated. In most cases, reconstruction tenodesis is reserved for patients with ligamentous laxity in whom the host tissues are severely attenuated. Another relative indication is the obese patient requiring additional stability due to large size.
CLINICAL OUTCOME STUDIES
Karlsson et al18 presented long-term follow-up of patients with lateral ankle instability treated by the Evans procedure. Fifty percent of patients had satisfactory long-term results. Twelve patients with early satisfactory results had deteriorated at 3 to 6 years. Kaikkonen et al19 similarly found poor results with the Evans procedure. Surgical treatment of chronic ankle instability with the Evans procedure restored the mechanical stability of the joint, but too frequently, the function of the ankle did not return to the preinjury level, with only 35% of their patients achieving an excellent or good result in performance testing. This finding was primarily due to decreased range of motion, swelling of the ankle, and atrophy of the calf.19 Both the Evans and Chrisman-Snook procedures result in weakness in the surgical limb compared with the contralateral control limb.20
Colville et al21 reported on reconstruction of the lateral ligaments in 15 cadaver ankles. The Evans and Chrisman-Snook procedures were tested for stability, motion, and isometry of graft placement. The Evans procedure allowed for increased anterior displacement, internal rotation, and tilt of the talus compared with the control ankles. Subtalar motion was restricted in all reconstructions. The Chrisman-Snook reconstructive procedure allowed increased internal rotation and anterior displacement. This procedure was effective in limiting talar tilt but restricted subtalar joint motion.
Many clinical comparisons have been performed between anatomic repairs and reconstructive tenodeses. Karlsson et al11 found that the tenodeses did not restore normal anatomy of the lateral ankle ligaments, unlike the anatomic repairs in their 2- to 10-year follow-up in a multicenter trial. The absence of normal anatomy resulted in restricted range of motion, reduced long-term stability, and an increased risk of medial degenerative joint disease of the ankle. They found a larger number of reoperations and less satisfactory overall results. Hennrikus et al22 demonstrated that both the Chrisman-Snook and modified Broström procedures provided good or excellent stability in more than 80% of patients; however, the modified Broström procedure resulted in higher patient satisfaction. In addition, a greater proportion of complications occurred with the Chrisman-Snook procedure.
Biomechanically, the modified Broström procedure was associated with less anterior talar displacement and a decreased talar-tilt angle compared with the Chrisman-Snook procedure.23 The modified Broström procedure produced a greater mechanical restraint than either the Evans or Chrisman-Snook procedures.23
SPECIAL CONSIDERATIONS
Limitations of the modified Broström anatomic repair are rare and appear to be confined to specific patient populations, such as the overweight, the hypermobile, and high-demand, strenuous workers or athletes. Girard et al24 reported on a modified Broström lateral-ligament repair augmented with an Evans procedure in 21 patients who were considered higher-demand athletes. These patients showed a statistically significant loss of inversion and eversion motion in addition to loss of peroneal strength; however, they were able to return to sporting activities.
In patients with a fixed varus hindfoot, a calcaneal osteotomy should be considered to reestablish a plantigrade foot position. A calcaneal osteotomy can be performed concurrently with an ankle-repair or tendon-weave procedure.
Thermal shrinkage is now commonly performed adjunctively in the shoulder and knee to provide additional ligamentous support. Whether it offers any benefit as an adjunct to an anatomic or tenodesis reconstruction of the ankle is unknown. One study25 showed that thermal shrinkage of the anterolateral capsule reduced angular displacement to varus stress and reduced anterior-talar excursion with an anterior drawer test. The appropriateness of this technique awaits further study.
CONCLUSIONS
The fundamentals of the surgical approach to lateral ankle instability are based on the anatomy of the lateral ankle ligaments, the anterior talofibular ligament, and the calcaneofibular ligament. Anatomic repair of the lateral-ligament complex supplemented with the Gould modification has become the preferred method of surgical treatment, with an 85% to 95% success rate. This approach provides increased stability through the reinforcement of local host tissue; preserves subtalar and talocrural motion; has fewer associated nerve injuries and less morbidity associated with the harvest of tendon grafts; and provides a quicker functional recovery. Ankle-reconstruction procedures that sacrifice tendons to be used as donor tissues are thought to provide a theoretically stronger construct and, hence, more stability. This increased stability can result in loss of talocrural and subtalar range of motion and lead to prolonged recovery and decreased sports performance. Adjacent nerve injury is more common with reconstructive ankle-ligament surgery. An ankle-reconstruction procedure using tendon augmentation should be reserved for patients with generalized ligamentous laxity or long-standing ligamentous insufficiency or as a salvage procedure in an individual with a failed modified Broström lateral-ligament repair.
Acknowledgments
ACKNOWLEDGMENTS
We thank Benedict DiGiovanni, MD, for his assistance in the preparation of this manuscript. The copyright for Figures 1,2,3,4 is maintained by the Hughston Sports Medicine Foundation, Inc, Columbus, GA.
REFERENCES
- Colville M R, Marder R A, Boyle J J, Zarins B. Strain measurement in lateral ankle ligaments. Am J Sports Med. 1990;18:196–200. doi: 10.1177/036354659001800214. [DOI] [PubMed] [Google Scholar]
- Burks R T, Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22:72–77. doi: 10.1177/036354659402200113. [DOI] [PubMed] [Google Scholar]
- Colville M R. Surgical treatment of the unstable ankle. J Am Acad Orthop Surg. 1998;6:368–377. doi: 10.5435/00124635-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Heilman A E, Braly W G, Bishop J O, Noble P C, Tullos H S. An anatomic study of subtalar instability. Foot Ankle. 1990;10:224–228. doi: 10.1177/107110079001000407. [DOI] [PubMed] [Google Scholar]
- Broström L. Sprained ankles, VI: surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;243:551–565. [PubMed] [Google Scholar]
- Rasmussen O. Stability of the ankle joint: analysis of the function and traumatology of the ankle ligaments. Acta Orthop Scand Suppl. 1985;211:1–75. [PubMed] [Google Scholar]
- Mascaro T B, Swanson L E. Rehabilitation of the foot and ankle. Orthop Clin North Am. 1994;25:147–160. [PubMed] [Google Scholar]
- Beighton P, Solomon L, Soskolne C L. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlgren O, Larsson S. Reconstruction for lateral ligament injuries of the ankle. J Bone Joint Surg Br. 1989;71:300–303. doi: 10.1302/0301-620X.71B2.2647757. [DOI] [PubMed] [Google Scholar]
- Gould N, Seligson D, Gassman J. Early and late repair of the lateral ligaments of the ankle. Foot Ankle. 1980;1:84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988;70:581–588. [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Surgical treatment of chronic lateral instability of the ankle joint: a new procedure. Am J Sports Med. 1989;17:268–273. doi: 10.1177/036354658901700220. [DOI] [PubMed] [Google Scholar]
- Zwipp H, Tscherne H. Zur behandlung der chronischen antero-lateralen instabilitat des oberen sprunggelenkes: derekte bandrekonstruktion-periostlappenplastik-tenodese. Unfallheilkunde. 1984;87:405–415. [PubMed] [Google Scholar]
- Hamilton W G, Thompson F M, Snow S W. The modified Brostrom procedure for lateral ankle instability. Foot Ankle. 1993;14:1–7. doi: 10.1177/107110079301400101. [DOI] [PubMed] [Google Scholar]
- Snook G A, Chrisman O D, Wilson T C. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985;67:1–7. [PubMed] [Google Scholar]
- Leach R E, Namiki O, Paul G R, Stockel J. Secondary reconstruction of the lateral ligaments of the ankle. Clin Orthop. 1981;160:201–211. [PubMed] [Google Scholar]
- Colville M R, Grondel R J. Anatomic reconstruction of the lateral ankle ligaments using a split peroneus brevis tendon graft. Am J Sports Med. 1995;23:210–213. doi: 10.1177/036354659502300214. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Lateral ankle instability of the ankle treated by the Evans procedure: a long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988;70:476–480. doi: 10.1302/0301-620X.70B3.3372575. [DOI] [PubMed] [Google Scholar]
- Kaikkonen A, Lehtonen H, Kannus P, Jarvinen M. Long-term functional outcome after surgery of chronic ankle instability: a 5-year follow-up of the modified Evans procedure. Scand J Med Sci Sports. 1999;9:239–244. doi: 10.1111/j.1600-0838.1999.tb00240.x. [DOI] [PubMed] [Google Scholar]
- St Pierre R K, Andrews L, Allman F, Jr, Fleming L L. The Cybex II evaluation of lateral ankle ligamentous reconstructions. Am J Sports Med. 1984;12:52–56. doi: 10.1177/036354658401200108. [DOI] [PubMed] [Google Scholar]
- Colville M R, Marder R A, Zarins B. Reconstruction of the lateral ligaments: a biomechanical analysis. Am J Sports Med. 1992;20:594–600. doi: 10.1177/036354659202000518. [DOI] [PubMed] [Google Scholar]
- Hennrikus W L, Mapes R C, Lyons P M, Lapoint J M. Outcomes of the Chrisman-Snook and modified-Brostrom procedures for chronic lateral ankle instability: a prospective, randomized comparison. Am J Sports Med. 1996;24:400–404. doi: 10.1177/036354659602400402. [DOI] [PubMed] [Google Scholar]
- Liu S H, Baker C L. Comparison of lateral ankle ligamentous reconstruction procedures. Am J Sports Med. 1994;22:313–317. doi: 10.1177/036354659402200303. [DOI] [PubMed] [Google Scholar]
- Girard P, Anderson R B, Davis W H, Isear J A, Kiebzak G M. Clinical evaluation of the modified Brostrom-Evans procedure to restore ankle stability. Foot Ankle Int. 1999;20:246–252. doi: 10.1177/107110079902000407. [DOI] [PubMed] [Google Scholar]
- Oloff L M, Bocko A P, Fanton G. Arthroscopic monopolar radiofrequency thermal stabilization for chronic lateral ankle instability: a preliminary report on 10 cases. J Foot Ankle Surg. 2000;39:144–153. doi: 10.1016/s1067-2516(00)80015-0. [DOI] [PubMed] [Google Scholar]