Abstract
Objective: To describe the clinical picture, pathophysiology, and treatment of concomitant lesions of the peroneus brevis tendon and lateral ligament injuries to the ankle.
Background: In some cases, chronic lateral ankle instability is associated with a longitudinal partial tear in the peroneus brevis tendon. Patients who suffer from this lesion usually have atypical posterolateral ankle pain combined with signs of recurrent ligament instability (“giving way”). The tendon injury is often overlooked because it is combined with the ligament injury, and the injury mechanisms are similar.
Description: Tears or laxity in the superior peroneal retinaculum allow the anterior part of the injured peroneus brevis tendon to ride over the sharp posterior edge of the fibula, leading to a longitudinal tear in the tendon. This combined injury should be suspected in patients with recurrent giving way of the ankle joint and retromalleolar pain. The diagnosis can be established using either ultrasonography or magnetic resonance imaging.
Differential Diagnosis: Ligament injury, tenosynovitis, peroneus longus tendon lesion, os peroneum fracture, distal peroneus brevis tendon tear, or anomalous peroneus tertius tendon.
Treatment: The tendon injury and the ligament insufficiency should be repaired at the same time.
Conclusions: We recommend reconstruction of the superior peroneal retinaculum, combined with repair of the tendon, using side-to-side sutures and anatomical reconstruction of the lateral ankle ligaments.
Keywords: ankle ligament instability, ankle reconstruction
Longitudinal tear or attrition of the peroneus brevis tendon (PBT; the peroneus longus tendon is very seldom involved) has recently been mentioned as a cause of lateral ankle pain.1–9 The combination of PBT and chronic ankle instability has also received attention.1,2,9–12
The PBT is located in the retrofibular groove, behind the lateral malleolus. Longitudinal tear of the tendon was first mentioned by Meyers in 1924.13 More recently, both clinical and cadaveric studies have shown that the lesion is probably more common than previously believed.3–5,10 Some researchers2,3 have reported that this lesion is found in as many as 37% of cadaveric specimens. The clinical relevance of the autopsy lesion is, however, not entirely known. The pathophysiologic changes are repeated overload of the tendon in the retrofibular groove, compromising the vascularity of the tendon. The superior peroneal retinaculum (SPR) is partially torn from the posterior aspect of the fibula, making the PBT somewhat unstable.4,9 This may result in inhibition of the tissue-repair response, leading to subsequent tendon degeneration and tear.2,5
PERONEUS BREVIS TENDON TEAR AND LIGAMENT INJURY
Several researchers4–6,9 have proposed a correlation between a longitudinal tear in the PBT and chronic lateral ankle-ligament instability. An inversion injury to the ankle may thus not only produce ligament damage to the anterior talofibular and calcaneofibular ligaments but also injury to the SPR and the peroneal tendons (Figure 1). Almost always, the central portion of the tendon is damaged.7 The peroneus longus pulls on the PBT in the retrofibular groove, over the sharp posterior edge of the fibula, during eversion of the foot in the swing phase.2,8,14 This leads to the dislocation of the most anterior part of the damaged tendon6,14,15 and almost invariably to pain at the posterior aspect of the fibula.5,9
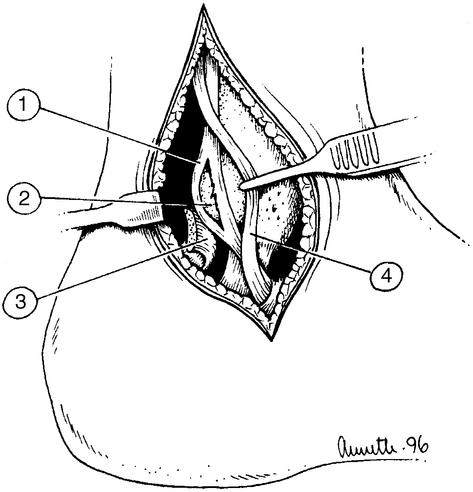
Figure 1.
Relationship among the longitudinal tear in the peroneus brevis tendon, the sharp posterior edge of the fibula, and the superior peroneal retinaculum. 1, Torn peroneus brevis tendon. 2, The sharp posterior edge of the fibula. 3, Superior peroneal retinaculum. 4, Normal peroneus longus tendon (retracted).
Typically, the patient gives a history of lateral ankle-inversion injury. In most cases, the tendon damage is overlooked, and the diagnosis may be delayed or even missed. Because of the damage to the SPR, the instability of the PBT, and the tendon tissue degeneration, these cases are often refractory to nonsurgical treatment, and the tendon tear progresses.1,5,6,9,16,17
During the last decade, several investigations of the microvascular anatomy and descriptions of the pathophysiology and the biomechanics of the PBT8,11,14,15,18,19 and several investigations of the treatment of concomitant ankle instability and partial longitudinal tears in the PBT1,5,6,8,9,12,14 have been published. The cause of the tendon injury is inversion ankle injury, with secondary insufficiency of the lateral ligaments and rupture (or possibly elongation) of the SPR. The damaged retinaculum cannot restrain the PBT behind the sharp posterior edge of the fibula, an injury mechanism well described by Sobel et al4,6 and subsequently verified by other researchers.5,9,17 Some other possible mechanisms have been mentioned; they include the distally located muscle belly of the peroneus brevis or the presence of an anomalous peroneus tertius tendon.16,20 However, the importance of these structures in the degenerative process of the PBT has been questioned.
The most likely cause of a combined lesion is recurrent ankle instability, followed by SPR insufficiency, leading to a secondary PBT subluxation and attrition of the tendon. This evolves to become a degenerative longitudinal tear in the PBT. The main predisposing factor is probably the tear in the SPR, but the exact pathophysiologic mechanism is not known.4,5,10 Intraoperative findings in several studies have been consistent with this hypothesis.5,6,9,17 A longitudinal tear in the PBT has also been described more distally, along the lateral wall of the calcaneus or in the cuboid tunnel.21 However, another somewhat uncommon injury is chronic lateral ankle pain associated with a fracture of the os peroneum, which, in some cases, should be considered in the differential diagnosis.22,23
CLINICAL PRESENTATION
The typical patient describes recurrent lateral instability of the ankle joint as the primary problem. In addition, retromalleolar pain combined with recurrent giving way is typical. The pain is almost always localized posterior to the lateral malleolus. This is in contrast to patients with chronic lateral ankle instability alone, who usually mention giving way as the main complaint and anterior ankle pain as a secondary problem, most frequently caused by anterior tibial or talar osteophytes or loose intra-articular bodies (bone or cartilage). A thorough physical examination includes an assessment of ligament integrity (ie, positive anterior drawer test or increased supination of the foot suggests injury). An assessment of range of motion is mandatory. Palpable swelling around and behind the lateral malleolus can raise the suspicion of a tendon tear.
RADIOGRAPHIC EVALUATION
There is a substantial risk of delayed or missed diagnosis with PBT tear. Either magnetic resonance imaging (Figure 2) or ultrasound imaging is recommended to increase the diagnostic accuracy in these patients.
Figure 2.

Sagittal oblique spin-echo proton density-weighted magnetic resonance image showing high signal intensity within the peroneus brevis tendon at the lateral malleolar level (black arrow). The peroneus longus tendon (white arrow) is normal.
TREATMENT
One constant finding at surgery is the subluxation of the anterior half of the PBT over the sharp posterior edge of the fibula. Moreover, the SPR is partially torn away from the posterior ridge of the fibula. Some authors5 have mentioned that this lesion resembles a Bankart lesion in recurrent anterior dislocation of the shoulder. Recurrent dislocation of the peroneal tendons is, however, not a primary problem.24 If concomitant lateral ankle instability is present, the consensus in the literature is that the tendon injury should be repaired at the same time as the ligament stabilization. Only a few reports on surgical treatment have been published, and we found no large series. Sobel and Geppert14 recommended a modification of the Broström-Gould procedure25 for the treatment of concomitant lateral ankle instability and PBT tear using a posterolateral approach.
A modified Chrisman-Snook procedure has been suggested by some researchers.8,24 The largest series is described by Bonnin et al,17 who operated on 18 patients with split lesions of the PBT associated with chronic ankle instability. During a 3-year period, 18 of 77 patients (23%) with chronic ankle-ligament laxity who underwent surgical repair had a concomitant PBT tear. The modfied Chrisman-Snook procedure was used in 13 of 18 patients studied. Regrettably, the clinical results were not described in detail in this report, making it impossible to draw any conclusions in terms of the choice of treatment. One potential problem when using this procedure is fraying of the tendon, making repair technically impossible.
In several reports,5,26 the anatomical reconstruction of the lateral ankle ligaments has been described as simple and safe, producing stable ankles with a low risk of complications in most patients. This procedure can be combined with the reconstruction of the SPR (Figures 3,4,5). The operation begins with a curvilinear 7- to 8-cm long incision along the posterior ridge of the fibula, exposing the peroneal tendons and the anterior talofibular and calcaneofibular ligaments. The ligaments are tested for laxity, and the SPR is exposed. The peroneal tendon sheath is incised approximately 5 mm posterior to the attachment to the fibula. Then the PBT is carefully examined. The degenerative tissue is carefully excised, and the tendon is repaired with side-to-side sutures. In some cases, the ruptured anterior part of the tendon may have to be excised; however, this is infrequent, and complete rupture of the PBT is extremely uncommon. A reconstruction of the SPR is performed, using three 2.0-mm drill holes in the posterior aspect of the fibular edge. Because insufficiency of the lateral ligaments is usually present, anatomical reconstruction of both the anterior talofibular and calcaneofibular ligaments is performed.
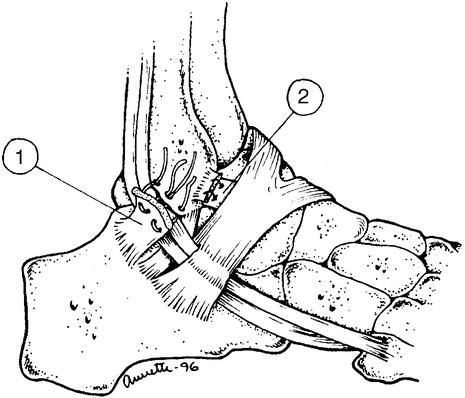
Figure 3.

Lateral view of the left ankle. A longitudinal tear is present in the peroneus brevis tendon. The peroneus longus tendon is normal.
Figure 4.
Reconstruction of the superior peroneal retinaculum is performed after the peroneus brevis tendon has been debrided and sutured (see Figure 5). The superior peroneal retinaculum is attached to the posterior fibular edge with nonabsorbable sutures through 2-mm drill holes. 1, Superior peroneal retinaculum. 2, Anterior talofibular ligament.
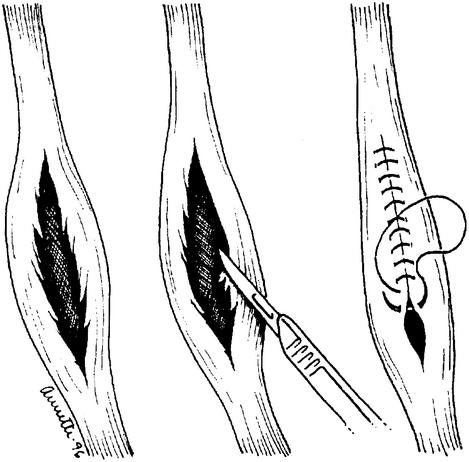
Figure 5.
A side-to-side suture (repair) of the partial longitudinal tear of the peroneus brevis tendon.
Postoperatively, a plaster cast is applied for 2 to 6 weeks, or, instead of prolonged postoperative immobilization, an Aircast brace (Aircast, Inc, Summit, NJ) can be used to facilitate range-of-motion training after the second postoperative week. Full weight bearing is allowed. After the sixth week, coordination training using tilt boards is initiated. Strength training with weight boots is initiated 6 to 8 weeks after the operation and increased until full functional strength has been regained. After approximately 12 weeks, the athlete is allowed to return to full sport activity provided that functional stability is normal and the ankle is not swollen. An external ankle support (ankle tape or Aircast brace) can thereafter be used as preferred by the athlete.
The results after anatomical reconstruction have been reported as satisfactory in most patients.5,9,14 Ligament stabilization should always be combined with repair of the tendon tear and reconstruction of the SPR.
CONCLUSIONS
Patients with a partial longitudinal tear in the peroneus brevis tendon most often present with atypical posterolateral (retromalleolar) pain. The tendon injury may be combined with injury to the lateral ankle ligaments. In order to produce the best clinical results, both the tendon injury and the ligament insufficiency should be repaired at the same time.
REFERENCES
- Larsen E. Longitudinal rupture of the peroneus brevis tendon. J Bone Joint Surg Br. 1987;69:340–341. doi: 10.1302/0301-620X.69B2.3818773. [DOI] [PubMed] [Google Scholar]
- Sobel M, DiCarlo E, Bohne W HO, Collins L. Longitudinal splitting of the peroneus brevis tendon: an anatomic and histologic study of cadaveric material. Foot Ankle. 1991;12:165–170. doi: 10.1177/107110079101200306. [DOI] [PubMed] [Google Scholar]
- Sobel M, Levy M E, Bohne W HO. Congenital variations of the peroneus quartus muscle: an anatomic study. Foot Ankle. 1990;11:81–89. doi: 10.1177/107110079001100204. [DOI] [PubMed] [Google Scholar]
- Sobel M, Bohne W HO, Markisz J A. Cadaver correlation of peroneal tendon changes with magnetic resonance imaging. Foot Ankle. 1991;11:384–388. doi: 10.1177/107110079101100608. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Brandsson S, Kälebo P, Eriksson B I. Surgical treatment of concomitant chronic ankle instability and longitudinal rupture of the peroneus brevis tendon. Scand J Med Sci Sports. 1998;8:42–49. doi: 10.1111/j.1600-0838.1998.tb00227.x. [DOI] [PubMed] [Google Scholar]
- Sobel M, Geppert M J, Warren R F. Chronic ankle instability as a cause of peroneal tendon injury. Clin Orthop. 1993;296:187–191. [PubMed] [Google Scholar]
- Sobel M, Bohne W HO, O'Brien S J. Peroneal tendon subluxation in a case of anomalous peroneus brevis muscle. Acta Orthop Scand. 1992;63:682–684. [PubMed] [Google Scholar]
- Sobel M, Warren R F, Brourman S. Lateral ankle instability associated with dislocation of the peroneal tendons treated by the Chrisman-Snook procedure: a case report and literature review. Am J Sports Med. 1990;18:539–543. doi: 10.1177/036354659001800518. [DOI] [PubMed] [Google Scholar]
- Minoyama O, Uahiyama E, Iwaso H, Hiranuma K, Takeda Y. Two cases of peroneus brevis tendon tear. Br J Sports Med. 2002;36:65–66. doi: 10.1136/bjsm.36.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sammarco G J, DiRaimondo C V. Chronic peroneus brevis tendon lesions. Foot Ankle. 1989;9:163–170. doi: 10.1177/107110078900900403. [DOI] [PubMed] [Google Scholar]
- DiRaimondo C V. Overuse conditions of the foot and ankle. In: Sammarco G J, editor. Foot and Ankle Manual. Lea & Febiger; Philadelphia, PA: 1991. pp. 266–268. [Google Scholar]
- Munk R L, Davis P H. Longitudinal rupture of the peroneus brevis tendon. J Trauma. 1976;10:803–806. doi: 10.1097/00005373-197610000-00009. [DOI] [PubMed] [Google Scholar]
- Meyers A W. Further evidence of attrition of the human body. Am J Anat. 1924;34:241–248. [Google Scholar]
- Sobel M, Geppert M J. Repair of concomitant lateral ankle ligament instability and peroneus brevis splits through a posteriorly modified Broström Gould. Foot Ankle. 1992;13:224–225. doi: 10.1177/107110079201300411. [DOI] [PubMed] [Google Scholar]
- Bassett F H, III, Speer K P. Longitudinal rupture of the peroneal tendons. Am J Sports Med. 1993;21:354–357. doi: 10.1177/036354659302100305. [DOI] [PubMed] [Google Scholar]
- Sobel M, Bohne W HO, Levy M E. Longitudinal attrition of the peroneus brevis tendon in the fibular groove: an anatomic study. Foot Ankle. 1990;11:124–128. doi: 10.1177/107110079001100302. [DOI] [PubMed] [Google Scholar]
- Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med. 1997;25:699–703. doi: 10.1177/036354659702500520. [DOI] [PubMed] [Google Scholar]
- Sobel M, Geppert M J, Hannafin J A, Bohne W HO, Arnoczky S P. Microvascular anatomy of the peroneal tendons. Foot Ankle. 1992;13:469–472. doi: 10.1177/107110079201300807. [DOI] [PubMed] [Google Scholar]
- Sobel M, Geppert M J, Olson E J, Bohne W HO, Arnoczky S P. The dynamics of peroneus brevis tendon splits: a proposed mechanism, technique of diagnosis, and classification of injury. Foot Ankle. 1992;13:413–422. doi: 10.1177/107110079201300710. [DOI] [PubMed] [Google Scholar]
- Sobel M, Mizel M. Injuries to the peroneal tendons. In: Pfeifer G B, Frey C C, editors. Current Practice in Foot and Ankle Surgery. VOL. McGraw Hill; New York, NY: 1993. pp. 30–36. [Google Scholar]
- Evans J D. Subcutaneous rupture of the tendon of peroneus longus: report of a case. J Bone Joint Surg Br. 1966;48:507–509. [PubMed] [Google Scholar]
- Patterson M J, Cox W K. Peroneus longus tendon rupture as a cause of chronic lateral ankle pain. Clin Orthop. 1999;365:163–166. doi: 10.1097/00003086-199908000-00021. [DOI] [PubMed] [Google Scholar]
- Wander D S, Ludden J W, Galli K, Mayer D P. Surgical management of a ruptured peroneus longus tendon with a fractured multipartite os peroneum. J Foot Ankle Surg. 1994;33:124–128. [PubMed] [Google Scholar]
- Arrowsmith S R, Fleming L L, Allman F L. Traumatic dislocations of the peroneal tendons. Am J Sports Med. 1983;11:142–146. doi: 10.1177/036354658301100306. [DOI] [PubMed] [Google Scholar]
- Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability of the ankle joint. J Bone Joint Surg Am. 1988;70:581–588. [PubMed] [Google Scholar]