Abstract
Objective: To determine whether subjects with functional ankle instability suffered kinesthetic deficits in the injured ankle compared with the healthy ankle and to examine the effect of prophylactic ankle bracing on kinesthesia in uninjured and functionally unstable ankles.
Design and Setting: We tested subjects over 4 consecutive days in a climate-controlled athletic training/sports medicine laboratory setting. A single-group time-series design enabled all subjects to serve as their own controls. A different bracing condition was tested on each of those occasions.
Subjects: Sixteen subjects (8 men, 8 women; age = 21.6 ± 1.7 years; mass = 73.5 ± 15.0 kg; height = 172.9 ± 8.8 cm) with unilateral functional ankle instability participated in this study.
Measurements: Kinesthetic threshold-to-detection of passive motion (TTDPM) measurements were obtained during passive inversion and eversion movements (0.5°·s−1) under 4 different bracing or taping conditions (unbraced, Swede-O Ankle Lok, Aircast Air-Stirrup, and tape).
Results: We analyzed the data using a 3-factor analysis of variance with repeated measures on the ankle and motion factors. Threshold-to-detection of passive motion scores in the unbraced condition were significantly better than the TTDPM scores in any of the other 3 test conditions. No significant differences were seen in TTDPM scores between the 2 ankles under any of the 4 conditions.
Conclusions: Threshold-to-detection of passive motion scores did not differ in uninjured ankles and those with functional instability; however, bracing with either the Ankle Lok or Air-Stirrup decreased the ability to detect passive motion when compared with the no-tape (unbraced) condition. Further research is needed to determine the exact contributions of taping and bracing on ankle joint kinesthesia.
Keywords: proprioception, threshold to detection of passive motion, lateral ankle sprain, functional ankle dysfunction
Acute injury to the ankle-foot complex is of primary concern to the rehabilitation professional. Ankle sprains are among the most common injuries incurred by participants in running and jumping activities.1 Approximately 85% of these ankle sprains are due to an inversion injury involving lateral ligament damage.2 To help prevent possible recurrence, rehabilitation programs are designed to increase muscle strength (primarily peroneal muscle strength) and improve ankle joint proprioception. Despite meticulous rehabilitation programs and diligence on the parts of the patient and athletic trainer, functional ankle instability may persist.3
The term functionally unstable ankle was first introduced by Freeman et al4 and has been refined to mean joint motion beyond voluntary control but not necessarily exceeding physiologic (anatomical) range of motion.5 Functional ankle instability (FAI) is characterized by a feeling of “giving way” of a mechanically stable ankle under normal activity.6,7 Although many theories exist about the causes of FAI, 3 of the most common are anatomic instability (ligamentous laxity),8–11 peroneal muscle weakness,8,10,12 and proprioceptive deficits.10,13 It may be that all 3 contribute; however, the contributions of the first 2 have been questioned within the literature.7,13
In many cases of FAI, anatomic instability cannot be documented by either clinical or radiographic evaluation; thus, there appears to be little or no association between FAI and mechanical instability.8–11 The role of peroneal muscle weakness in FAI has not been firmly established. Kaminski et al13 reported that evertor muscle weakness was not present in subjects with unilateral FAI when compared with a control group with uninjured ankles. Other researchers have also reported no deficits in eversion strength in subjects with FAI.8,10,12 Perhaps the role of proprioception as a cause of FAI has been scrutinized the most in the literature.3,4,12 Proprioception has been defined as the ability to detect sensory stimuli such as touch, pain, pressure, and movements.14 Assessment of joint proprioception is divided into 2 components: kinesthesia and joint position sense (JPS).14,15 Kinesthesia is assessed by measuring the threshold-to-detection of passive motion (TTDPM), while JPS is assessed by measuring the reproduction of both passive and active positioning.14,15
Some authors16,17 have examined proprioception via JPS, but only a few12,18 have examined TTDPM. Glencross and Thornton16 studied JPS and reported significantly greater errors in the functionally unstable ankle compared with the uninvolved ankle. Detection of passive movement was also stated to be significantly impaired in the functionally unstable ankle.16 However, Gross17 reported no differences in JPS in subjects suffering from recurrent ankle sprains. More recently, Refshauge et al18 examined TTDPM in a group of subjects with recurrent ankle sprains and reported no differences between the injured and uninjured limbs. With such disparity in results, further research is needed to assess ankle joint proprioception via kinesthesia.18
When assessing kinesthesia in those with FAI, it would seem plausible to explore the effects of ankle bracing, given the fact that bracing is often used when athletes with FAI are returned to activity. Numerous researchers 19–21 have examined ankle bracing's effect on range of motion and proprioception in healthy ankles, but a void exists in contemporary research on the potential effects of bracing on FAI. For example, JPS has been reported to be improved significantly in both taped and braced uninjured ankles.22 The question remains whether the kinesthetic component of proprioception is affected by the use of prophylactic ankle bracing and taping. If wearing prophylactic ankle braces improves kinesthesia in subjects with FAI, lateral ankle sprains could be reduced.
Our purpose was twofold: to determine whether subjects with unilateral FAI had kinesthetic deficits compared with the healthy ankle and to examine the effect of prophylactic ankle bracing on proprioception in uninjured and functionally unstable ankles. We hypothesized that a kinesthetic deficit would exist between the functionally unstable ankle and the uninjured ankle. Additionally, we also believed that prophylactic ankle bracing and taping would significantly improve kinesthesia in both ankles.
METHODS
A 2 × 2 × 4 factorial with repeated measures on 2 factors (ankle and motion) guided the study. The independent variables were condition (unbraced, prophylactic ankle tape, Swede-O Ankle Lok [Swede-O Inc, North Branch, MN], and Aircast Air-Stirrup [Aircast Inc, Summit, NJ]), ankle (FAI and uninjured), and motion (inversion and eversion). The dependent variable was TTDPM score measured in degrees.
Subjects
Sixteen subjects (8 men, 8 women; age = 21.6 ± 1.7 years; mass = 73.5 ± 15.0 kg; height = 172.9 ± 8.8 cm) with unilateral FAI from the College of Health and Human Performance at the University of Florida were recruited to participate. Any positive findings on an anterior drawer or talar tilt test were grounds for exclusion. A positive finding was laxity on either test when compared with the uninjured ankle. The University of Florida Institutional Review Board approved the study, and informed consent was obtained from each subject.
Instrumentation
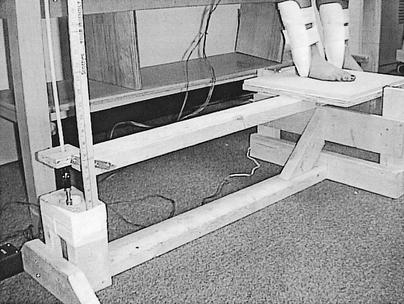
Threshold-to-detection of passive motion was achieved using a specially built device (Figure 1) that measured passive inversion and eversion ankle movements in degrees while maintaining a constant speed of 0.5°·s−1. It was imperative that the TTDPM device move at this slow angular velocity to minimize the contribution of the musculotendinous mechanoreceptors (muscle spindles and Golgi tendon organs) in providing feedback to the central nervous system regarding limb position.14,15 The design of this instrument was closely related to the instrument previously described and validated by Lentell et al.12 The device is equipped with a reversible motor that allowed the researchers to start and then return the footplate to the original starting position (zero degrees of talocrural joint flexion). The movable footplate rotates on a single axis. With the foot resting on the footplate, movement into ankle inversion and eversion from a starting position of zero degrees can occur.
Figure 1.
Threshold-to-detection of passive motion (TTDPM) measuring device.
Test Procedures
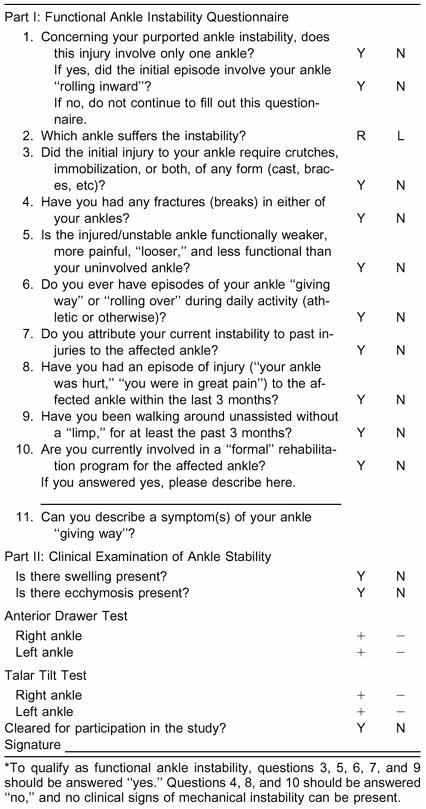
Subjects who self-reported functional ankle disability were convened at a general informational meeting before the study began. The potential subjects filled out the Functional Ankle Instability Questionnaire (Table 1), which contained the criteria for FAI. Subjects had no prior knowledge of these criteria. We then carefully scrutinized the completed questionnaires. Each qualified subject was then examined by an orthopaedic surgeon to rule out mechanical instability via an anterior drawer and talar tilt test. Of the 50 subjects who satisfied the criteria, only 16 were mechanically stable and invited to participate in the study. The subject's opposite, uninjured ankle served as the control. A third party collected all information so that the tester (T.J.H.) was blinded to which ankle was impaired.
Table 1. Criteria for Functional Ankle Instability*
A pilot study was conducted in order for the tester to become familiar with the use of the device. Testing was conducted over 4 consecutive days. A different bracing condition was tested on each day. Subjects were instructed not to reveal which ankle was affected, so the tester remained blinded throughout data collection. We used a Latin square to determine the bracing order for each subject. The 4 bracing conditions were unbraced, prophylactic ankle tape, Swede-O Ankle Lok, and Aircast Air-Stirrup. In all conditions, the subject was barefoot. For the taped condition, we used a closed basketweave ankle-taping technique23 with 3.81-cm (1.5-in) adhesive tape. The tester collected data and performed all taping procedures, in addition to fitting and securing all ankle braces. All braces were fitted according to the manufacturer's specifications. We flipped a coin to randomize the order of testing for ankle (FAI versus uninjured) and motion (inversion versus eversion). In 7 subjects, the injured ankle was tested first, while in the remaining 9 subjects, the uninjured ankle was tested first.
Each subject was instructed in the operation of the TTDPM measuring device and positioned on the device as previously described. The on-off switch was given to the subject, and he or she was instructed to turn it to the off position when any movement was first felt. To prevent the subject from trying to learn the time before the motor was started, the examiner instituted a delay from 0 to 10 seconds before turning on the device. The tester randomly selected a card that designated the delay (0 to 10 seconds) before each trial.
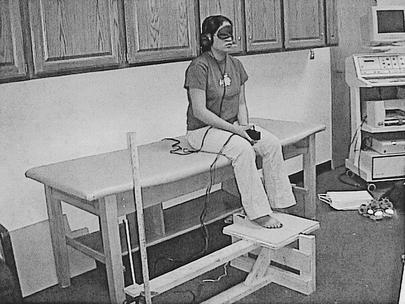
To eliminate auditory feedback, the subjects were blindfolded and listening to classical music through headphones while TTDPM measurements were taken (Figure 2). The subjects sat on a table with the knee and hip flexed to 90°. The foot to be tested rested on the footplate to promote a subtalar joint axis of rotation by aligning the midpoint of the heel with the interval between the first and second toe.12,24 As the device moved the tested ankle into either inversion or eversion, the subject stopped the device when movement was first felt by using the handheld on-off switch. The degrees of motion were determined based on the distance the footplate moved from the start position, using the law of sines.25 The law of sines states that the ratio between the length of any side of a triangle and the angle opposite that side is equal to the ratio between the length of any other side of the triangle and the angle opposite that side.25 We performed 3 trials on each ankle and motion, with the average TTDPM score from the 3 trials used for later analysis.
Figure 2.
Patient positioned on the threshold-to-detection of passive motion (TTDPM) measuring device in control of the on-off switch.
Statistical Analysis
Data were analyzed using a 2 × 2 × 4 analysis of variance with repeated measures on the ankle and motion. Statistical Package for the Social Sciences (SPSS) for Macintosh (version 6.1.1, SPSS Inc, Chicago, IL) assisted in the statistical analysis. The within-subject factors included condition (unbraced, Swede-O Ankle Lok, Aircast Air-Stirrup, and tape), ankle (FAI, uninjured), and motion (inversion, eversion). Threshold-to-detection of passive motion scores (degrees) served as the dependent measure. The Tukey Honestly Significant Difference (HSD) post hoc test was used to further examine significant differences of interest either as interactions or main effects. Level of significance was set a priori at P < .05 for all comparisons. An a priori power analysis was conducted to determine the power of the statistical design to detect significant differences of >1° error. Using our proposed sample size of 16 and an effect size of 1, the analysis resulted in a power of 0.87.
RESULTS
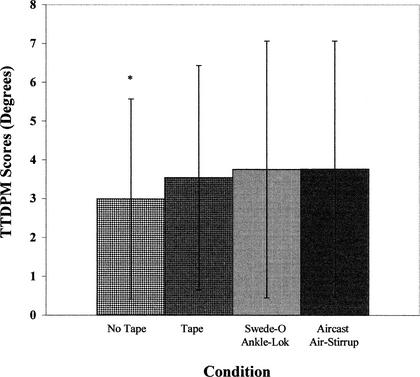
No significant interactions were noted among any of the variables (Table 2). This is best illustrated when the effect sizes for the differences between the functionally unstable ankle and the uninvolved ankle are compared across both condition and motion. These values ranged from .01 to .43, with 6 of the 8 comparisons being less than 0.2. These represent very small effect sizes and small magnitudes of differences between the 2 ankles. A statistically significant main effect for condition (unbraced, Swede-O Ankle Lok, Aircast Air-Stirrup, and tape) was found (F3,45= 3.90, P = .015), which resulted when TTDPM scores for both inversion and eversion and functionally unstable and uninjured ankles were pooled. Passive movement was detected by the unbraced ankle much sooner (with fewer degrees of motion) than under the Ankle Lok or Air-Stirrup ankle bracing conditions (Figure 3). The unbraced ankle was able to detect motion sooner than the taped condition, but the difference was not statistically significant. Effect sizes for the differences in TTDPM scores between the unbraced condition and the other 3 conditions (tape, Swede-O, Aircast) ranged from .21 to .30. These values represent small effect sizes, indicating small magnitudes of difference among the bracing conditions. There were no significant differences in TTDPM scores between the 2 ankles (F1,15 = 4.09, P = .061) or between the 2 motions tested (F1,15 = .13, P = .720). Interestingly, when the effect sizes for motion were compared between the ankles, the eversion TTDPM scores had effect sizes ranging from .26 to .52 (moderate levels), while the inversion scores ranged from .01 to .30 (low levels). Thus, it appears that taping and bracing had a greater effect during eversion compared with inversion, regardless of ankle status.
Table 2. Eversion and Inversion Threshold-to-Detection of Passive Motion Scores for the Functionally Unstable and Uninjured Ankles Under Each of the Test Conditions*
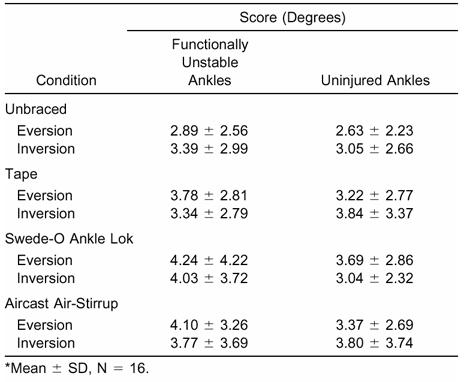
Figure 3.
Threshold-to-detection of passive motion scores (degrees) for both inversion and eversion and functionally unstable and uninjured ankles for each of the test conditions. Error bars represent standard deviations. *Significantly different from the 2 bracing conditions.
DISCUSSION
Proprioceptive deficits have been suggested as a cause of functional ankle dysfunction.8,10,13,18,26,27 As a result, restoring proprioception has become an important rehabilitative consideration to the clinician. Our results suggest that kinesthesia as measured by TTDPM did not differ significantly in subjects with unilateral FAI when compared with the opposite, unaffected ankle. Several studies17,18 support our results, whereas other authors12,16 have reported different results. Refshauge et al18 noted similar findings in a study using TTDPM scores for passive plantar-flexion and dorsiflexion motions in both functionally unstable and uninjured ankles.18 Refshauge et al18,28 and Hall and McCloskey29 contended that muscle afferents surrounding the major joints in the body provide the most important proprioceptive information to the central nervous system. Therefore, joint mechanoreceptors may duplicate information provided by these other sources (muscle afferents), so a decrease in the joint mechanoreceptor discharge would not result in a noticeable proprioceptive deficit.18,28,29 Gross17 reported that JPS scores in subjects with unilateral FAI and a control group with uninjured ankles were no different. He also tested both inversion and eversion motions. However, Lentell et al12 reported that TTDPM scores were significantly different between the ankles of 39 subjects suffering from unilateral FAI and the nonimpaired ankles were able to detect the passive movement sooner than the opposite, affected ankles.
When the means for the untaped condition in our study are compared with the untaped condition in the Lentell et al12 study, they are quite similar. In addition, Lentell et al12 had high TTDPM averages (4.3° ± 3.1°) for the FAI side, similar to our reported data. Interestingly, we used a similar set of criteria for determining FAI, along with a comparable TTDPM measuring device, yet we report different results. We are also quick to note that we had far fewer subjects (16) than Lentell et al12 (39). In contrast to our study, they only tested TTDPM into inversion and did not rule out mechanical instability.12 In fact, the additional eversion TTDPM scores may have confounded our results and contributed to the lack of significant findings between conditions in the FAI and uninjured groups.
To what extent, if any, learning influenced our results is unknown. We randomly tested both inversion and eversion motions, whereas some authors have examined just one motion (ie, inversion or plantar flexion)12,16,30 and reported differences between the FAI and uninjured groups. In contrast, Gross17 and Refshauge et al18 conducted studies similar to ours and failed to find differences between the groups. It is yet to be determined whether these differences can be attributed to the learning curve. The threat of this effect (learning curve) on the study outcomes must be addressed in future studies that involve the testing of more than 1 motion over several different conditions. We would suggest a 1- to 2-week familiarization period in which subjects have an opportunity to be tested repeatedly on the TTDPM device to alleviate the initial learning curve.
We were surprised that ankle bracing (Swede-O Ankle Lok or Aircast Air-Stirrup) decreased the subject's ability to detect passive motion. The taped condition was not significantly different from the unbraced condition when TTDPM scores were compared. This suggests that ankle taping did not significantly influence one's ability to detect the passive movement and had the same effect on TTDPM scores as the unbraced or untaped condition. Several sets of researchers20,22,31,32 have indicated that proprioception can be enhanced or improved by ankle taping or bracing. These studies used JPS as the measure of proprioception and several involved healthy, uninjured subjects. In a study similar to ours, Refshauge et al18 reported no enhancement in TTDPM scores with athletic tape applied to the ankle. It may be that the enhanced proprioceptive benefits of ankle taping or bracing are evident only when JPS is tested.
One of the potential limitations of our study is that we cannot be sure if our TTDPM device measured platform motion more than ankle motion. This discrepancy may explain the results of bracing decreasing kinesthesia. If the brace restricts motion at the foot, then the platform may have to move further before actual foot movement is detected. Thus, the finding may be better explained by mechanics than by sensory changes. It may have been appropriate to use a goniometer in addition to the law of sines to determine the amount of movement at the ankle. Future researchers should emphasize different measurement techniques so there is no discrepancy between the platform and ankle motion.
The unbraced ankle detected motion less than 1° before the braced ankle. This difference is statistically significant, but it may not be clinically significant. Konradsen et al33 discussed the significance of detecting 1° of motion. During the late swing phase of gait, the lateral edge of the foot passes close to the ground with a clearance of only 5 mm.33 Impact between the lateral edge of the foot and the supporting surface causes the ankle to invert, plantar flex, and internally rotate, potentially resulting in a stumble. The degree of inversion error necessary to cause an impact is approximately 8°.33 Further study is needed to examine exactly which TTDPM score differences are considered clinically significant and which are not.
The criteria used to define FAI vary greatly in the literature, which makes it difficult to compare studies. A consistent set of criteria for describing FAI is needed. The criteria used in the study by Lentell et al10 offer an excellent starting point. We built upon those criteria set forth by Lentell et al10 by incorporating additional responses. Furthermore, we solicited the expertise of an orthopaedic surgeon to rule out the possibility of mechanical instability. One of the potential flaws of the criteria is that they rely heavily on subjective responses. The subjective method by which FAI has been determined is questioned in reports because of the possibility of the subjects providing inaccurate information.11,13,34,35 We feel that clarification is needed as to whether recurrent ankle sprains or instances of the ankle giving way should be used as part of the criteria. The ambiguity between these criteria can potentially confound the dependent measure, because there are no data proving which of these factors contribute to FAI. We also suggest that mechanical instability be ruled out before subjects are classified as having FAI. This is important to ensure that subjects who have mechanical deficits, which may confound the functional instability, do not contaminate the subject pool. We recommend that a standard set of criteria be used in the determination of FAI status and made available for future research. This precaution should enable a more accurate assessment of FAI, more consistency across studies, and easier comparison of data pools, while lessening the variability in study designs.
CONCLUSIONS
The contribution of kinesthetic deficits to FAI remains unknown. A number of causes have been suggested, but the precise cause of FAI remains elusive. The use of prophylactic ankle bracing and taping in those with FAI may not enhance kinesthesia, as measured in this study. While other measures of ankle-joint proprioception may be improved with prophylactic ankle bracing and taping, the measures of TTDPM appear to be decreased when compared with the unbraced or untaped condition. Clinicians who have previously used ankle bracing and taping to enhance ankle-joint kinesthesia may want to reexamine whether the kinesthetic benefits are worthwhile.
REFERENCES
- Balduini F C, Tetzlaff J. Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med. 1982;1:3–12. [PubMed] [Google Scholar]
- Ekstrand J, Tropp H. The incidence of ankle sprains in soccer. Foot Ankle. 1990;11:41–44. doi: 10.1177/107110079001100108. [DOI] [PubMed] [Google Scholar]
- Freeman M A, Wyke B. Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal ankle-joint mechanoreceptors upon reflex activity in the leg muscles. Br J Surg. 1967;54:990–1001. doi: 10.1002/bjs.1800541204. [DOI] [PubMed] [Google Scholar]
- Freeman M A, Dean M R, Hanham I W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- Hals T M, Sitler M R, Mattacola C G. Effect of a semi-rigid ankle stabilizer on performance in persons with functional ankle instability. J Orthop Sports Phys Ther. 2000;30:552–556. doi: 10.2519/jospt.2000.30.9.552. [DOI] [PubMed] [Google Scholar]
- Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H, Rijke A M. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- Evans G A, Hardcastle P, Frenyo A D. Acute rupture of the lateral ligaments of the ankle: to suture or not to suture? J Bone Joint Surg Br. 1984;66:209–212. doi: 10.1302/0301-620X.66B2.6368563. [DOI] [PubMed] [Google Scholar]
- Lentell G L, Katzman L, Walters M. The relationship between muscle function and ankle stability. J Orthop Sport Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Staples O S. Result study of rupture of lateral ligaments of the ankle. Clin Orthop. 1972;85:50–58. doi: 10.1097/00003086-197206000-00011. [DOI] [PubMed] [Google Scholar]
- Lentell G B, Bass B, Lopez D, McGuire L, Sarrel M, Synder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H, Gansneder B M. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34:239–249. [PMC free article] [PubMed] [Google Scholar]
- Lephart S M, Pincivero D M, Rozzi S L. Proprioception of the ankle and knee. Sports Med. 1998;25:149–155. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]
- Lephart S, Henry T. The physiologic basis for open and closed kinetic chain rehabilitation for the upper extremity. J Sport Rehabil. 1996;5:71–87. [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Gross M T. Effects of recurrent lateral ankle sprains on active and passive judgments of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Refshauge K M, Kilbreath S L, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med Sci Sports Exerc. 2000;32:10–15. doi: 10.1097/00005768-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Alves J W, Alday R V, Ketcham D L, Lentell G L. A comparison of the passive support provided by various ankle braces. J Orthop Sports Phys Ther. 1992;1:10–18. doi: 10.2519/jospt.1992.15.1.10. [DOI] [PubMed] [Google Scholar]
- Feuerbach J W, Grabiner M D, Koh T J, Weiker G G. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am J Sports Med. 1994;22:223–229. doi: 10.1177/036354659402200212. [DOI] [PubMed] [Google Scholar]
- Paris D L, Vardaxis V G, Kokkaliaris J. Ankle ranges of motion during extended activity periods while taped and braced. J Athl Train. 1995;30:223–228. [PMC free article] [PubMed] [Google Scholar]
- Heit E, Lephart S, Rozzi S. The effect of ankle bracing and taping on joint position in the stable ankle. J Sport Rehabil. 1996;5:206–213. [Google Scholar]
- Arnheim D D, Prentice W E. 10th ed McGraw-Hill; St Louis, MO: 2000. Principles of Athletic Training. [Google Scholar]
- Mantor J. Movements of the subtalar and transverse tarsal joint. Anat Rec. 1941;80:387–410. [Google Scholar]
- Hall S. 2nd ed Mosby-Year Book; Louis St: 1995. Basic Biomechanics. [Google Scholar]
- Ebig M, Lephart S M, Burdett R G, Miller M C, Pincivero D M. The effect of sudden inversion stress on EMG activity of the peroneal and tibialis anterior muscles in the functionally unstable ankle. J Orthop Sports Phys Ther. 1997;26:73–77. doi: 10.2519/jospt.1997.26.2.73. [DOI] [PubMed] [Google Scholar]
- Freeman M A. Instability of the foot after injury to the lateral ligaments of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- Refshauge K M, Fitzpatrick R C. Perception of movement at the human ankle: effects of leg position. J Physiol. 1995;488:243–248. doi: 10.1113/jphysiol.1995.sp020962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall L A, McCloskey D I. Detections of movements imposed on finger, elbow and shoulder joints. J Physiol. 1983;35:519–533. doi: 10.1113/jphysiol.1983.sp014548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1998;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Bennell K L, Goldie P A. The differential effects on external ankle support on postural control. J Orthop Sports Phys Ther. 1994;20:287–295. doi: 10.2519/jospt.1994.20.6.287. [DOI] [PubMed] [Google Scholar]
- Robbins S, Waked E, Rappel R. Ankle taping improves proprioception before and after exercise in young men. Br J Sports Med. 1995;29:242–247. doi: 10.1136/bjsm.29.4.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konradsen L, Beynnon B D, Renström P A. Proprioception and sensorimotor control in the functionally unstable ankle. In: Lephart S M, Fu F H, editors. Proprioception and Neuromuscular Control in Joint Stability. Human Kinetics; Champaign, IL: 2000. pp. 237–246. [Google Scholar]
- Bosien W R, Staples O S, Russell S W. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37:1237–1243. [PubMed] [Google Scholar]
- Staples O S. Ruptures of the fibular collateral ligaments of the ankle: result study of immediate surgical treatment. J Bone Joint Surg Am. 1975;57:101–107. [PubMed] [Google Scholar]