Abstract
Objective: To examine if patients with chronic ankle instability or a history of ankle sprains without chronic instability have worse proprioception or less invertor and evertor muscle strength.
Design and Setting: We assessed proprioception and muscle strength on the Biodex isokinetic dynamometer in the laboratory of the Department of Sports Medicine, University Hospital Ghent.
Subjects: Subjects included 87 physical education students (44 men, 43 women, age = 18.33 ± 1.25 years, mass = 66.09 ± 8.11 kg, height = 174.11 ± 8.57 cm) at the University of Ghent in Belgium. Their ankles were divided into 4 groups: a symptom-free control group, subjects with chronic ankle instability, subjects who had sustained an ankle sprain in the last 2 years without instability, and subjects who sustained an ankle sprain 3 to 5 years earlier without instability.
Measurements: Active and passive joint-position sense was assessed at the ankle, and isokinetic peak torque was determined for concentric and eccentric eversion and inversion movements at the ankle.
Results: Statistical analysis indicated significantly less accurate active position sense for the instability group compared with the control group at a position close to maximal inversion. The instability group also showed a significantly lower relative eversion muscle strength (% body weight). No significant differences were observed between the control group and the groups with past sprains without instability.
Conclusions: We suggest that the possible cause of chronic ankle instability is a combination of diminished proprioception and evertor muscle weakness. Therefore, we emphasize proprioception and strength training in the rehabilitation program for ankle instability.
Keywords: joint position sense, isokinetic strength, ankle injury, rehabilitation
Lateral ankle sprain is an extremely common athletic injury. Despite extensive clinical and basic science research, the recurrence rate remains high and the reasons why sprains tend to recur are unclear; thus, successful rehabilitation is difficult.1 In a review of the potential causes of functional ankle instability, Hertel2 cited joint position-sense deficits, muscle-strength deficits, delayed peroneal muscle-reaction time, balance deficits, altered common peroneal nerve function, and decreased dorsiflexion range of motion. However, it remains important to search for the contributory factors of chronic ankle instability (CAI), which is hypothesized to predispose individuals to reinjury after lateral ankle sprains.
Freeman et al3 proposed that ankle injury may disrupt joint afferents located in the supporting ligaments. After injury to the nervous and musculotendinous tissue, proprioceptive deficits are likely to occur and may manifest as reduced joint position sense. The ability to detect motion in the foot and to make postural adjustments in response to these detected motions is thought to be crucial in the prevention of ankle injury. Similarly, the ability of an individual to detect the position of the foot before foot contact is important. Several authors4–8 have suggested that inversion ankle sprains may occur due to improper positioning of the foot just before and at foot contact. Improper positioning may be due to the loss of proprioceptive input from mechanoreceptors.
Joint position sense is a component of proprioception and is often measured to assess proprioception. Studies of joint position sense in the chronically unstable ankle have demonstrated varying results.9–11 Glencross and Thornton9 reported a decrease in active joint-position sense of the chronically unstable ankle over that of the uninjured ankle. Gross10 and Holmes et al,11 however, failed to reveal any significant differences between injured and uninjured ankles in either active or passive joint-position sense.
The evertor muscles are often suggested to play an important role in preventing ligamentous injuries. The strength of the peroneus longus and brevis muscles is supposed to provide support to the lateral ligaments.4 Bosien et al12 and Staples13 were the first to measure peroneal muscle strength, but they used manual methods to detect peroneal muscle weakness and found long-term evertor muscle weakness after inversion sprains. Tropp14 was the first to measure muscle torque at the ankle with an isokinetic dynamometer. His results confirmed an earlier theory that peroneal muscle weakness is a component of CAI. He suggested that the muscular impairment is due to inadequate rehabilitation and secondary muscle atrophy. Baumhauer et al15 even found in a prospective study that individuals with muscle-strength imbalance exhibited a higher incidence of inversion ankle sprains. Conversely, Lentell et al16 found no significant differences in muscle strength, either isometrically or isokinetically, between the chronically unstable ankles and the uninvolved ankles, suggesting that muscular weakness is not a major contributing factor to the chronically unstable ankle.
We are not aware of any previous investigators who have examined muscle strength and joint position sense in subjects who sustained a sprain in which instability was not a factor. The most common risk factor for ankle sprains in sports is a history of a previous sprain17; therefore, we think it is important to search for proprioception or muscle-strength deficits in subjects with a history of previous sprains who do not report CAI to learn if these subjects are still at risk for sustaining sprains. Also, we would like to know if the risk for sustaining a sprain is higher for subjects who suffered sprains 1 or 2 years ago compared with subjects who had a sprain more than 2 years ago.
In addition, few researchers have examined eccentric muscle strength. Most researchers have measured isometric or concentric muscle strength in subjects with CAI, although the evertor muscle must contract eccentrically to resist an ankle inversion sprain. Therefore, our purpose was to search for deficits in ankle proprioception and invertor and evertor concentric and eccentric muscle strength in subjects with CAI and a history of ankle sprains.
METHODS
Subjects
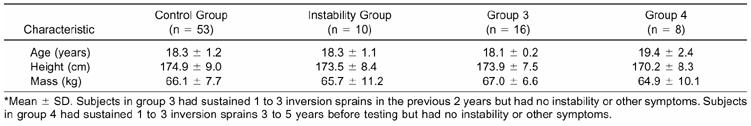
Subjects included 87 physical education students (44 men, 43 women; age range, 17–26 years; mean age, 18.33 ± 1.25 years) who were freshmen in 2000–2001 at the University of Ghent, Belgium (Table 1). Before testing, all students visited the same sports medicine physician for a comprehensive injury history. Based on these histories, we divided the ankles into 4 groups. Of the 174 ankles (both ankles of 87 subjects), 106 served as a control group (group 1). The 53 subjects (29 men, 24 women) in this control group had no prior history of injury to either ankle. The instability group (group 2) consisted of 14 chronically unstable ankles of 10 subjects (4 men, 6 women) who had a history of more than 3 inversion sprains of the same ankle, frequent giving-way episodes, and some complaints of pain during heavy and intense loading. Four subjects in this instability group complained of bilateral CAI. No subjects in the instability group had suffered severe injury to the unstable ankle for at least 3 months before testing. Group 3 consisted of 20 ankles of 16 subjects (8 men, 8 women) who had sustained 1 to 3 inversion sprains in the previous 2 years but did not complain of instability or other symptoms. Four persons in this group had inversion sprains of both ankles in the same period. Group 4 consisted of 8 ankles in 8 subjects (3 men, 5 women) who had sustained 1 to 3 inversion sprains 3 to 5 years before testing and did not complain of instability or other symptoms. Mechanical instability of the subjects' ankles was not measured. Each volunteer signed an informed consent. The study was approved by the Ethical Committee of Ghent University Hospital.
Table 1. Subject Characteristics*
INSTRUMENTATION AND PROTOCOL
Proprioception
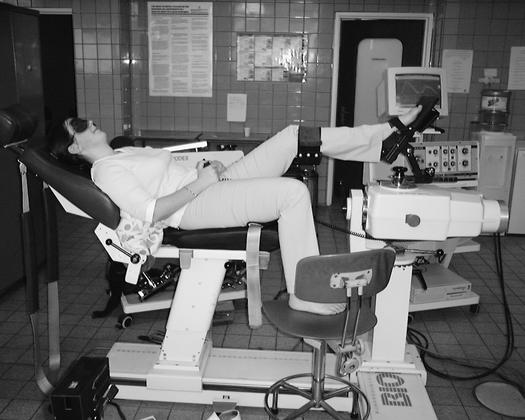
Active and passive joint position sense was assessed using the Biodex 2 isokinetic dynamometer (Biodex Medical Systems Inc, Shirley, NY) (Figure 1). Each subject was positioned supine on the associated chair, with the calf of the tested leg resting on a 40-cm-high platform. The bare foot of the subject was aligned with the axis of the dynamometer and attached to the footplate by a very small wrap to reduce cutaneous receptor input. The talocrural joint was in 15° of plantar flexion. The lower leg was secured to the platform by hook-and-loop straps. Two positions were tested: 15° of inversion and maximal active inversion minus 5°. Subjects were blindfolded throughout the examination.
Figure 1.
Positioning of the subject for testing active and passive joint-position sense on the Biodex 2 isokinetic dynamometer.
For passive testing, the subject's foot was first passively moved by the investigator to maximal eversion. The investigator then moved the foot to 1 of the 2 test positions, randomly determined. The test position was maintained for 10 seconds, with each subject instructed to concentrate on the position of the foot. The foot was then passively brought to maximal eversion and moved passively back toward inversion with a speed of 5°·s−1. The subject was instructed to push on a stop button when he or she thought the test position had been reached. The subject was tested twice at each of the 2 test positions. The active test was performed in the same manner, except after having the foot passively placed in the test position and moved to maximal eversion, the subject was asked to move the foot actively back to the test position. The subject was again asked to push on the stop button when he or she thought the test position was reached. The testing order, test positions, and side of body tested were randomly chosen. The amount of error in degrees was noted for further analysis.
We examined 3 types of errors in the subjects' ability to match the reference angles: the absolute, exact, and variable error. Average scores of the 2 trials were used for analysis. The absolute error is the difference in absolute value in degrees between the position chosen by the subject and the test-position angle. The exact error, calculated as the difference between the chosen position and the test-position angle, provides an indication of whether the subjects tended to, on average, systematically overshoot (positive exact error) or undershoot (negative exact error) the test-position angle. The variable error, which was calculated as the standard deviation of the exact error, provides an indication of the random error in matching the test-position angle.
Muscle Strength
We used a Biodex System 3 Dynamometer and Biodex Advantage Software Package (Biodex Medical Systems Inc, Shirley, NY) to determine isokinetic peak torque and peak torque/body-weight values for reciprocal concentric and eccentric eversion-inversion movements of the ankle (Figure 2). Subjects were tested in a semirecumbent position with 30° of seatback tilt. The ankle was in 10° of plantar flexion. The knee of the tested ankle was in extension to minimize substitution from the hamstrings and other tibial rotators. Dynamometer and chair adjustments were made to align the midline of the foot with the midline of the patella. Two straps were wrapped around the extremity proximal to the patella and the pelvis to minimize movements of the hip and knee during testing. Subjects wore their own athletic shoes during testing; each shoe was tightly secured with 2 straps to the dynamometer footplate to minimize movement between the shoe sole and the footplate surface. The tested range of motion was maximal active inversion and eversion minus 5° for both directions. The first test consisted of 3 maximal repetitions of concentric-eccentric eversion at 30°·s−1 to assess the strength of the evertor muscles. The second test for the same ankle consisted of 5 repetitions of concentric-eccentric eversion at 120°·s−1. The same 2 tests (concentric-eccentric at 30°·s−1 and 120°·s−1) were performed for inversion to assess the strength of the inversion muscles. The same 4 tests were then performed with the contralateral limb. The first tested ankle was randomly chosen. Before data collection, each subject was given an opportunity to become familiar with the testing procedure and to perform 3 warm-up repetitions. Consistent verbal encouragement for maximal effort was given to each subject throughout the testing procedure. None of the subjects felt any discomfort while testing.
Figure 2.
Positioning of the subject for testing isokinetic ankle inversion/eversion on the Biodex 3 isokinetic dynamometer.
Peak torque and peak torque/body-weight values were obtained for each ankle motion (concentric and eccentric) of each limb at the 2 speeds. Eversion-to-inversion strength ratios and eccentric-to-concentric strength ratios were calculated.
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) for Windows (version 10.0, SPSS Inc, Chicago, IL) was used for statistical analysis. The exact, absolute, and variable data from the proprioception test were examined with a nonparametric Kruskal-Wallis test to determine significant differences among the 4 groups. Peak torque, peak torque/body-weight values, and eversion-to-inversion and eccentric-to-concentric strength ratios were also analyzed for between-group differences. Post hoc comparisons of means were accomplished with Mann-Whitney U tests and corrected with the Bonferroni correction. Additionally, a Pearson correlation analysis was performed between peak torque and body weight. A significance level of P<.05 was used throughout the data analysis.
RESULTS
Proprioception
For the absolute error, we found no significant differences among the 4 groups for either active or passive joint-position sense (Table 2). For the exact error, a significant difference was noted for the active joint-position sense in the test position of maximal inversion minus 5° (P = .012) (Table 3). The instability group showed a significantly lower value for active joint-position sense at maximal inversion minus 5° compared with the control group (P = .042), group 3 (P = .012), and group 4 (P = .036). No significant differences were observed for the variable error among the 4 groups.
Table 2. Absolute Error on the Proprioception Test*
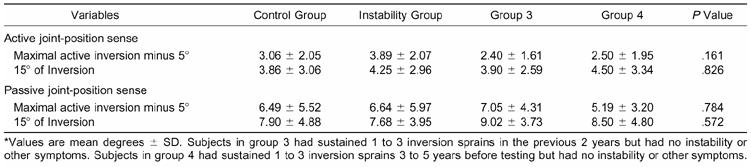
Table 3. Exact Error on the Proprioception Test*
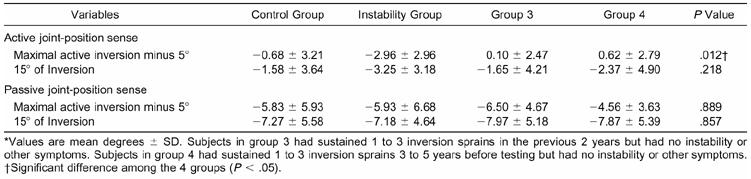
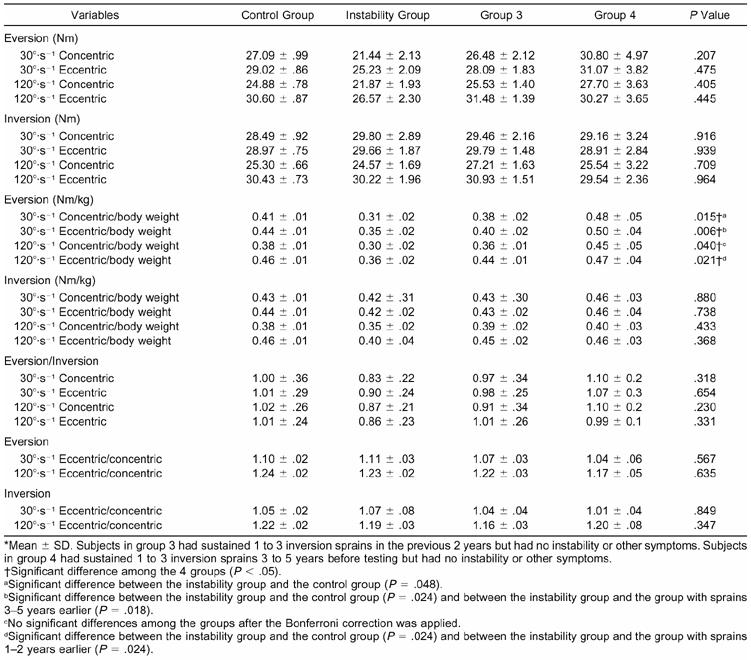
Muscle Strength
We found significant differences in the strength of the eversion muscles compared with body weight at both speeds (30°·s−1 and 120°·s−1) for concentric and eccentric test conditions (Table 4). The instability group had a significantly lower value compared with the control group for eversion strength/body weight at 30°·s−1 for both concentric (P = .048) and eccentric (P = .024) test conditions and at 120°·s−1 for the eccentric condition (P = .024). The instability group also had a significantly lower value compared with group 3 for eversion strength/body weight at 120°·s−1 (P = .024) and with group 4 for eversion strength/body weight at 30°·s−1 (P = .018), both for the eccentric condition. There were no significant differences for strength/body weight between the control group and the other 2 groups that sustained ankle sprains in the past without instability as complaint. No significant differences were observed among the 4 groups for peak torque, inversion-to-eversion strength ratio, or eccentric-to-concentric strength ratio (P > .05). We noted a significant association between inversion and eversion peak torque and body weight (P < .001, .47 < r > .60) for the concentric and eccentric conditions and for both speeds.
Table 4. Muscle Strength
DISCUSSION
Proprioception
It is widely believed that the tendency for ankle sprains to recur is due to a proprioceptive deficit caused by deafferentation during the original trauma.1 Many methods have been devised to assess ankle proprioception, such as quantification of postural sway in standing using instant single-leg stance,18 stance on a wobble board,19 and standing with eyes open or closed.20 These techniques do not isolate variations in performance to the ankle region and may involve other factors such as visual and vestibular cues, neuromuscular control, and the influence of other joints21; however, these techniques have the advantage of testing in the weight-bearing position.21 Although visual and vestibular inputs contribute to proprioception, the peripheral mechanoreceptors are most important from a clinical orthopaedic perspective. These peripheral mechanoreceptors include cutaneous, muscle, and joint types. The neural input provided by these mechanoreceptors and the visual and vestibular receptors are all integrated by the central nervous system to generate a motor response. These motor responses generally may be categorized within 3 levels of motor control: spinal reflexes, brain stem activity, and cognitive programming. Quantifying the reproduction of joint position (either active or passive) and the detection of changes in joint position is processed at the highest level of organization: the somatosensory cortex. These methods can objectively isolate the measurement of joint position at the ankle, although in a non-weight-bearing position. Our study involved a protocol simulating positions associated with the most common mechanism of injury for the ankle joint: inversion and plantar flexion.
Our results show 2 ways to interpret proprioceptive data: the absolute and exact error. Most previous investigators of joint position sense have examined only absolute errors.9–11,21 These studies lack a distinct measure of whether subjects were systematically biased to overestimate or underestimate the reference angle. In our study, the exact error was usually negative; thus, our subjects were mostly biased to undershoot the test-position angle. These data do not support the findings of Feuerbach et al,22 who found that exact error was not significantly different from zero for subjects without injuries. Measuring proprioception in different planes could cause these conflicting results. In this study, proprioception was measured in 1 plane (inversion-eversion). Subjects studied by Feuerbach et al22 were required to match test positions in 3 planes.
We demonstrated significant differences among the 4 groups for the absolute error; however, we found a difference between the instability group and the other groups for the exact error. Subjects with unstable ankles did not differ from the others in matching the reference position; none were able to perfectly match the reference angle, but the subjects with unstable ankles systematically underestimated the reference angle whereas the other subjects sometimes underestimated and sometimes overestimated the reference angle. Gross,10 who examined active and passive joint-position sense in the inversion-eversion plane, did not find significant differences between controls and subjects with recurrent ankle sprains. Holme et al11 also noted no difference in active joint-position sense in the inversion-eversion plane between the injured and uninjured ankles of subjects with a unilateral ankle sprain. These studies only investigated the absolute error and therefore lack distinction in direction. Our observed differences between the unstable and stable ankles in this study in the exact error agree with previous investigations.9,21,23 Some studies have reported less accurate joint-position sense in chronically unstable ankles. Glencross and Thornton9 reported postinjury deficits in judgment of active joint-position sense in the plantar flexion-dorsiflexion plane. Boyle and Negus21 found significantly less accurate judgment of active and passive joint-position sense in subjects with recurrent ankle sprains compared with uninjured subjects. Hartsell24 also showed those with chronically unstable ankles to have poorer active joint-position sense awareness than did those with healthy ankles at a test position of 15° inversion.
Our results for the exact error indicated that subjects with instability had a significantly less accurate active joint-position sense at maximal inversion minus 5°. Correct positioning of the foot is very important in gait and sports. Hitting the ground in an overly inverted position could result in spraining the ankle. Our findings suggest that subjects with CAI may have inappropriate foot positioning. Because of the altered afferent input, these subjects may be more susceptible to ankle reinjury.
Interestingly, we found no significant differences between the control group and the 2 groups of subjects who had sustained ankle sprains in the past. We demonstrated significant differences between the ankles that had previously sustained an inversion sprain not associated with instability and the chronically unstable ankles. Therefore, past ankle sprains without resultant instability did not affect an individual's ability to judge ankle position.
Because subjects with past sprains without instability had normal proprioception, the proprioceptive deficit may be the reason ankle sprains recur in patients with CAI. One of the main goals in the treatment of lateral ankle injuries should be the prevention of CAI.
Joint position sense is affected in subjects with CAI, and taping or bracing may counterbalance this deficit. Previous studies have already shown that taping and bracing reduce the error in joint position sense.22,24 Feuerbach et al22 suggested that application of an orthosis may increase the afferent feedback from cutaneous receptors, which may lead to improved ankle joint-position sense. This increased stimulation could result in a more appropriate positioning of the unstable ankle and may protect it from reinjury.
Muscle Strength
Many investigators have found a relationship between peroneal muscle weakness and chronically unstable ankles.12–14,23 Others have found significant invertor weakness in the chronically unstable ankles.19,23 Ryan19 suggested that the invertor weakness could be the result of interruption of the muscles' nerve supply or the result of selective inhibition of the invertors' ability to start moving in the direction of initial injury. However, we found no relationship between invertor muscle strength and ankle sprains, although we did find a significant difference for evertor muscle strength (peak torque/body weight) between subjects with CAI and the control group. Subjects with CAI seemed to have less concentric and eccentric evertor muscle strength than normal subjects.
Previous investigators have tested evertor and invertor muscle strength at different speeds. We chose to use 30°·s−1 and 120°·s−1 to measure muscle peak torque because slower speeds, identified in the literature as those between 30°·s−1 and 120°·s−1, define strength, while the faster speeds, identified in the literature as those between 120°·s−1 and 300°·s−1, define muscle power.25 Otherwise, high-velocity eccentric contractions are not without risk and are very hard to perform.
Most researchers report only mean peak-torque values rather than values normalized by body weight. We find the peak torque for both muscle groups at both speeds to be significantly related to body weight. Normalizing by body weight is, thus, an important consideration for better comparison among subjects of varied body types. Additionally, as inversion sprains most often occur in the closed kinetic chain, body weight also has an influence on the inversion moment generated at the ankle. Therefore, we consider peak torque/body weight a more relevant value compared with peak torque. In addition, the functional assessment of muscular stabilization must consider the fact that the evertor muscles contract eccentrically to resist an inversion trust.16 Nevertheless, isokinetic assessment of ankle muscles has traditionally been tested by concentric contractions only. Hartsell and Spaulding23 were the first to retrospectively test the strength of the invertor and evertor muscles eccentrically in subjects with healthy and chronically unstable ankles. Chronically unstable ankles were significantly weaker concentrically and eccentrically for both inversion and eversion. Although we did not find significant differences among the groups for inversion muscle strength, we did find the unstable ankles weaker concentrically and eccentrically for eversion strength/body weight at both speeds.
Hartsell and Spaulding23 calculated eccentric/concentric ratios at several velocities (60, 120, 180, and 240°·s−1). Their hypothesis was that the eccentric/concentric ratios would be significantly different for subjects with CAI because abnormalities in the ratio may imply abnormality or predispose to injury.26–28 Bennett and Stauber28 tested patients with knee problems who showed a deficiency in eccentric activity. They found a particularly low eccentric/concentric ratio and proposed that this was a potential cause of patellofemoral problems. The problem was proposed to be related to an error in the neuromotor control of the quadriceps muscle, although another feasible explanation may be selective inhibition of eccentric performance of the quadriceps as the result of pain. Although Hartsell and Spaulding23 tested subjects with healthy and chronically unstable ankles over a velocity continuum, they were not able to identify an eccentric/concentric ratio pattern suggestive of instability. Our results affirm these findings of no significant differences for the eccentric/concentric ratio between subjects with healthy ankles and those with unstable ankles or ankles with past inversion sprains. Perhaps the invertor and evertor muscles produce too little torque in relation to the quadriceps muscles to display differences in the eccentric/concentric ratios.
In a prospective study of ankle-injury risk factors, Baumhauer et al15 found that individuals with muscle-strength imbalance, as measured by an elevated eversion-to-inversion ratio, exhibited a higher incidence of inversion ankle sprains. We examined this factor retrospectively in uninjured subjects and subjects with instability or past sprains and noted no significant differences among the groups.
As in the proprioception test, none of the variables tested showed significant differences between the control group and the 2 groups of subjects who had previously sustained ankle sprains without instability. Interestingly, some eversion-strength factors showed significantly higher values for the groups with past sprains compared with the instability group. This could mean that a deficit in muscle strength is one cause of instability; however, it is difficult to say whether these findings are the cause or the effect of the instability. Probably the 2 tested components, proprioception and muscle strength, both play a role in ankle instability. We suggest that neuromuscular disorders such as proprioceptive deficits and muscle weakness may cause persistent instability of the ankle. We also think that subjects who sustain an inversion sprain without associated CAI are at less risk to resprain their ankles than subjects with CAI because they have greater muscle strength and more accurate joint position sense.
CONCLUSIONS
Chronic instability was significantly related to active joint-position sense in the ankle at angles near maximal inversion. Ankle instability and evertor muscle weakness coexist; however, we found no evidence for a lack of muscle strength or proprioception deficit in subjects who had sustained sprains in the past without instability as a complaint.
We suggest that a possible cause of recurrent sprains in the instability group is the combined action of diminished proprioception and evertor muscle weakness. If the ankle is inverted at the moment the foot touches the ground, due to the diminished proprioception, the result could be a varus thrust from an inversion lever through the subtalar axis. If the evertor muscles are not strong enough to counteract this motion, the tensile strength of the lateral ligaments may be exceeded, resulting in injury.
Our results affirm the importance of proprioception training and strength training of the peroneal muscles in the rehabilitation of ankle injuries. These exercises may effectively stabilize an unstable ankle and break the vicious cycle of recurrent sprains and subsequent loss of proprioception and muscle atrophy.
Acknowledgments
ACKNOWLEDGMENTS
We thank Guy Vanderstraeten, MD, PhD, for assistance in revising the manuscript.
REFERENCES
- Refshauge K M, Kilbreath S L, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med Sci Sports Exerc. 2000;32:10–15. doi: 10.1097/00005768-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- Freeman M A, Dean M R, Hanham I W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Glick J M, Gordon R B, Nishimoto D. The prevention and treatment of ankle injuries. Am J Sports Med. 1976;4:136–141. doi: 10.1177/036354657600400402. [DOI] [PubMed] [Google Scholar]
- Sammarco J. Biomechanics of the ankle, I: surface velocity and instant center of rotation in the sagittal plane. Am J Sports Med. 1977;5:231–234. doi: 10.1177/036354657700500603. [DOI] [PubMed] [Google Scholar]
- Stormont D M, Morrey B F, An K, Cass J R. Stability of the loaded ankle: relation between articular restraints and primary and secondary static restraints. Am J Sports Med. 1985;13:295–300. doi: 10.1177/036354658501300502. [DOI] [PubMed] [Google Scholar]
- Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- Wright I C, Neptune R R, van den Bogert A J, Nigg B M. The influence of foot positioning on ankle sprains. J Biomech. 2000;33:513–519. doi: 10.1016/s0021-9290(99)00218-3. [DOI] [PubMed] [Google Scholar]
- Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- Gross M T. Effects of recurrent lateral ankle sprains on active and passive judgments of joint position. Phys Ther. 1987;67:1505–1509. doi: 10.1093/ptj/67.10.1505. [DOI] [PubMed] [Google Scholar]
- Holme E, Magnusson S P, Becker K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- Bosien W R, Staples S, Russell S W. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37:1237–1243. [PubMed] [Google Scholar]
- Staples O S. Result study of ruptures of lateral ligaments of the ankle. Clin Orthop. 1972;85:50–58. doi: 10.1097/00003086-197206000-00011. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- Baumhauer J F, Alosa D M, Renström A F, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- Lentell G L, Katzman L L, Walters M R. The relationship between muscle function and ankle stability. J Orthop Sports Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Thacker S B, Stroup D F, Branche C M, Gilchrist J, Goodman R A, Weitman E A. The prevention of ankle sprains in sports: a systematic review of the literature. Am J Sports Med. 1999;27:753–760. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle? Br J Sports Med. 1997;31:65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan L. Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Austr J Physiother. 1994;40:41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- Perrin P P, Béné M C, Perrin C A, Durupt D. Ankle trauma significantly impairs posture control: a study in basketball players and controls. Int J Sports Med. 1997;18:387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- Boyle J, Negus V. Joint position sense in the recurrently sprained ankle. Austr J Physiother. 1998;44:159–163. doi: 10.1016/s0004-9514(14)60375-5. [DOI] [PubMed] [Google Scholar]
- Feuerbach J W, Grabiner M D, Koh T J, Weiker G G. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am J Sports Med. 1994;22:223–229. doi: 10.1177/036354659402200212. [DOI] [PubMed] [Google Scholar]
- Hartsell H D, Spaulding S J. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med. 1999;33:255–258. doi: 10.1136/bjsm.33.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartsell H D. The effects of external bracing on joint position sense awareness for the chronically unstable ankle. J Sport Rehabil. 2000;9:279–289. [Google Scholar]
- St Pierre R K, Andrews L, Allman F, Jr, Fleming L L. The Cybex II evaluation of lateral ankle ligamentous reconstructions. Am J Sports Med. 1984;12:52–56. doi: 10.1177/036354658401200108. [DOI] [PubMed] [Google Scholar]
- Trudelle-Jackson E, Meske N, Highenboten C. Eccentric/concentric torque deficits in the quadriceps muscle. J Orthop Sports Phys Ther. 1989;11:142–145. doi: 10.2519/jospt.1989.11.4.142. [DOI] [PubMed] [Google Scholar]
- Dvir Z. Churchill Livingstone; New York, NY: 1995. Isokinetics: Muscle Testing, Interpretation and Clinical Applications. [Google Scholar]
- Bennett J G, Stauber W T. Evaluation and treatment of anterior knee pain using eccentric exercise. Med Sci Sports Exerc. 1986;18:526–530. [PubMed] [Google Scholar]