Abstract
Objective: To determine if there were differences in concentric peak torque/body-weight (PT/BW) ratios and concentric time to peak torque (TPT) of the dorsiflexors and evertors in uninjured and functionally unstable ankles using a stretch-shortening cycle (SSC) protocol on an isokinetic dynamometer.
Design and Setting: We employed a case-control study design to examine the test subjects in a climate-controlled athletic training/sports medicine research laboratory.
Subjects: Thirty subjects volunteered to participate in this study, 15 with unilateral functional ankle instability and 15 matched controls.
Measurements: Participants were assessed isokinetically using an SSC protocol for the dorsiflexors and evertors at 120 and 240°·s−1, bilaterally. Strength was assessed using PT values normalized for body mass. Concentric TPT measurements were also compared between the groups.
Results: No differences in concentric PT/BW ratios or concentric TPT were evident between the groups (P > .05). Additionally, there were no differences in these measurements between the ankles for the same motion and speed between the ankles in the subjects with functional instability.
Conclusions: Using the SSC protocol as a measure of ankle function and the stretch-reflex phenomenon, we found no evidence to support the notion that differences in strength and TPT in the active, conscious state exist between those with functional ankle instability and a group of healthy control subjects.
Keywords: stretch reflex, peak torque, time to peak torque, isokinetics, plyometrics, chronic ankle dysfunction
Interest in ankle instability research has grown in the past few years. Previous researchers have examined several factors purported to be involved in this entity.1–5 Most recently, neuromuscular factors related to ankle instability have been evaluated.6–10 The biomechanics of the ankle function to transfer forces accepted during locomotion and produce a propulsive impetus to maintain movement. In response to these continual demands placed on the ankle during activity, ankle overload may occur, causing injury. Once an athlete experiences an initial traumatic event, he or she may continue to describe feelings of “giving way” or instability long after pain and inflammation have disappeared. This syndrome of continued dysfunction is termed functional ankle instability (FAI).2,11–14 Ankle joint stability is provided by both static and dynamic mechanisms. Dynamic joint stability relies heavily on a properly functioning neuromuscular communication network. Disruption in the pathway may predispose the ankle to further injury and future instability.
Freeman et al11 suggested that a loss of neuromuscular control was responsible for the giving way associated with FAI. Kaikkonen et al5 indicated that ankle proprioception is often disrupted after an ankle-ligament injury, resulting in impaired peripheral sensation. Having adequate peripheral feedback is important for the maintenance of static and dynamic postural stability of the body. Meanwhile, partial deafferentation of joint afferent receptors is believed to alter the muscles' ability to provide joint stability via antagonist cocontraction and synergistic muscle activation.15 Baumhauer et al4 prospectively investigated risk factors associated with susceptibility to lateral ankle sprain. Generalized joint laxity, anatomical measurements of the foot and ankle, anatomical alignment, and ankle-ligament stability were not found to be significant risk factors leading to ankle injury. However, evertor-to-invertor and plantar flexor-to-dorsiflexor strength ratios were elevated in the experimental group, indicating that altered antagonist strength relationships may be responsible for the long-term disability. Thus, neuromuscular control and force production are important to maintaining adequate joint stabilization. A number of studies have been conducted to examine strength and its relationship to FAI. No significant differences were noted in concentric, eccentric, or isometric ankle strength between subjects with FAI and those with healthy ankles.8 Bernier et al9 found no differences in eversion or inversion eccentric strength between participants with FAI and the uninjured group. However, they did show a strong inverse relationship between the degree of mechanical instability and invertor eccentric peak torque (r = .71).9 There is a belief that disrupted muscle-reaction time and amplitude to high-speed inversion may be more closely related to factors other than strength.
With growing evidence that differences in concentric, eccentric, and isometric strength, measured independently, may not be predisposing risk factors for those with unstable ankles, the problem may lie in a delayed reaction of the peroneal muscles to imposed stretch forces. Several groups have demonstrated the detrimental effect of either acute or chronic joint injury on reflex joint stabilization.6,15,16 These studies recreated the mechanism of the inversion ankle sprain using a trap-door stimulus. Latencies to ankle muscle response were measured via electromyographic analysis. The researchers6,15,16 concluded that stretch reflexes were slower to respond during sudden, unexpected passive inversion in subjects with FAI as compared with their uninjured counterparts.
The stretch-shortening cycle (SSC) has been studied extensively using muscles of the calf and thigh regions. Helgeson and Gajdosik17 suggested that measuring the SSC with an isokinetic dynamometer in isolated muscle groups could provide a better indication of how each muscle group performs during functional activities. Functional activities such as walking, running, and jumping are examples of the SSC, in which a continuous series of eccentric and concentric muscle actions occur.
The phases of the SSC include eccentric, amortization, and concentric intervals. The amortization phase is the transition between eccentric and concentric actions, during which time the muscle must switch from overcoming work to acceleration in the opposite direction.18 The amortization phase may be affected by the electromechanical delay, which is defined as the interval between initiation of sudden joint displacement and the generation of sufficient muscle tension to effectively resist the displacement moment.18 In individuals prone to ankle sprain, the SSC of the ankle dorsiflexors and evertor muscle groups is of primary importance. The electromechanical delay between mechanoreceptor activation and generation of adequate resistive muscle tension probably plays an important role in susceptibility to lateral ankle sprain. Perhaps the more quickly the individual can switch from yielding eccentric work to overcoming concentric work, the more powerful the response to the inversion and plantar-flexion motions will be.18 This is especially important given the fact that most lateral ankle sprains occur via this mechanism. It has been previously reported that the concentric contraction within the SSC may be 100% more powerful than an isolated concentric contraction in uninjured individuals when tested isokinetically.19 The researchers' reasons for this improvement in power, although there may be additional explanations, are the elastic recoil of the eccentrically stretched muscles and the stretch reflex.19 However, there is logical and strong debate concerning the significance of the contribution of the elastic recoil in the SSC.20 The stretch reflex recruits additional motor units, creating a more powerful concentric contraction. When the amortization phase is long, the elastic energy is lost as heat, and the stretch reflex fails to activate.21 In effect, the concentric contraction is less powerful. Whether or not the same holds true in an injured population, especially those with FAI, remains to be seen.
Therefore, our purpose was to determine if there were differences in dorsiflexor and evertor concentric force in subjects with uninjured and functionally unstable ankles executing an isokinetic SSC protocol. Concentric peak torque/body weight (PT/BW) and concentric time to peak torque (TPT) were employed as indicators of power. We hypothesized that concentric PT/BW would be less and concentric TPT would be slower in those with unilateral FAI when compared with uninjured controls. A secondary purpose of this study was to compare those same values in the involved and uninvolved ankles in subjects with FAI.
METHODS
Subjects
Fifteen subjects (age = 22.1 ± 3.7 years, height = 170.3 ± 8.5 cm, mass = 73.6 ± 12.0 kg) experienced unilateral FAI with no evidence of mechanical instability. Mechanical instability was assessed via anterior drawer and talar tilt tests performed by a certified athletic trainer. The FAI subjects satisfied the criteria previously established by Hubbard and Kaminski.22 Fifteen control (CON) subjects (age = 21.7 ± 3.1 years, height = 169.5 ± 7.6 cm, mass = 72.4 ± 11.8 kg) were paired with the FAI subjects. The control group's ankles had no history of injury, no functional or mechanical instability (as assessed via anterior drawer and talar tilt tests), and no other conditions affecting the ankle. Satisfaction of the inclusionary and exclusionary requirements was determined by questionnaire and initial assessment by the principal investigator (G.K.P.). Subjects were matched by height, weight, sex, activity level, and skill foot. Each group consisted of 6 men and 9 women. The skill foot was determined by asking the subjects which foot they would use to kick a ball. All 30 subjects were found to have a right skill foot. Informed consent was provided by all subjects. The study was approved by the University of Florida Institutional Review Board.
Instrumentation
The Kinetic Communicator (Kin Com) 125 AP (Chattanooga Group, Chattanooga, TN) isokinetic dynamometer, integrated with a computer and appropriate software, was used to assess both TPT and PT. The reliability of this device in the testing of ankle strength has been previously established.23 An SSC (eccentric action preceding a concentric contraction without delay) protocol was developed for the ankle dorsiflexors and evertors. The Kin Com footplate was programmed to move continuously with medium acceleration and deceleration, and the dynamometer was set to gather data in a continuous mode. We calibrated the dynamometer before each testing session.
PROCEDURES
Familiarization Session
A 5-minute warm-up consisting of moderate-intensity stationary bicycling at 90 revolutions per minute preceded the isokinetic activity. Subjects were also allowed to perform a series of lower extremity flexibility exercises. After warm-up and stretching, the participants were acquainted with the testing protocol. All subjects practiced the movements of the isokinetic test protocol at a submaximal effort at least 5 days before their scheduled test date. Because of the complexity and uniqueness of the testing protocol, subjects were able to practice until they felt comfortable with the SSC movements and the isokinetic dynamometer.
Testing
An experienced researcher (T.W.K.), who was blinded to the ankle status of the test subjects, performed all isokinetic tests. All testing occurred in the quiet, climate-controlled environment of the Athletic Training/Sports Medicine Research Laboratory. A warm-up and stretch identical to that used during the familiarization session was completed before all testing.
Ankle eversion and dorsiflexion strength were tested with subjects seated on the chair of the dynamometer. A knee-flexion angle of 45° was maintained during the dorsiflexion testing, while a plantar-flexion angle of 10° was sustained during the eversion tests. Participants were stabilized in the chair according to the manufacturer's guidelines, with straps securing the chest and the waist. The isokinetic dynamometer was moved to the appropriate position for strength testing using the automatic-positioning function. A universal stabilizer was used to position and hold the lower leg to prevent unwanted muscle substitutions. The foot was securely fastened into the footplate attachment using hook-and-loop closures. With the foot securely fastened into the footplate, the subject's available range of motion (ROM) was determined using the built-in electrogoniometer. A position of subtalar joint neutral determined with Donatelli's24 procedure was the midpoint (zero degrees) of ROM for both ankle movements tested. Eighty percent of the subject's available inversion-eversion and plantar-flexion-dorsiflexion ROM was employed during testing of these muscle groups. For the inversion-eversion motions, we used the 80% midrange of the entire eversion-to-inversion range, while 80% from full plantar flexion was used when setting the ROM stops for the plantar flexion-dorsiflexion motion. The start and stop angles were then set at the ends of this 80% ROM. During pilot testing, we found that a setting of 100% of the subject's available ROM would not allow the smooth eccentric-to-concentric transition that was necessary for this study. In this position at the end of the physiologic range, the muscle is stretched and rendered weak and unable to generate enough force to move the dynamometer arm in the opposite direction. Furthermore, by incorporating this test range, we attempted to mimic a range that the subjects experienced during activities of daily living. Once the subject reached the start and stop angles, the force required to initiate the eccentric and concentric movements was set at 20 Newtons. This adjustment was also necessary to maintain a quick, smooth eccentric-to-concentric transition during the SSC maneuver.
The gravity-correction procedure described in the Kin Com manual was performed for dorsiflexion testing to ensure accurate data collection. The eversion SSC protocol did not require gravity correction. We chose isokinetic velocities of 120°·s−1 and 240°·s−1 for testing both the ankle evertors and dorsiflexors, and we examined both eccentric and concentric muscle actions. Similar SSC testing procedures have revealed increased force or power output in comparison with only concentric contraction protocols.17,19
Each subject performed 3 to 5 submaximal warm-up repetitions before each test condition. A 1-minute rest followed the warm-up period. The order of extremity (right versus left), muscle group (evertors versus dorsiflexors), and velocity (120°·s−1 versus 240°·s−1) was randomized by a coin toss. Each subject in the matched-pair control group performed the test sequence in the same order as his or her FAI counterpart. Five maximal test repetitions were completed without interruption for both muscle groups at each test velocity. In order to accomplish this goal, each subject was allowed to look at the computer screen for visual feedback and received constant verbal encouragement (“pull, pull, pull, etc . . .”) to perform better on each test repetition. A 1-minute rest was provided between velocity presentations.
Data-Extraction Procedure
The data were extracted manually from the Kin Com computer by moving the cursor marker along the torque curves. Placing the marker on the last eccentric point along the curve denoted the start of concentric motion for each repetition. The start time of each concentric action was noted, and then the cursor was moved along the curve to the point of concentric PT and the subsequent time recorded. The time of concentric PT was then subtracted from the concentric starting time, producing concentric TPT. The highest concentric PT and associated concentric TPT were extracted from each 5-repetition test. All PT data were normalized for body mass (kg).
Statistical Analysis
In this case-control study, comparisons were made between FAI and matched-pair control subjects. The involved ankle from the FAI group was compared with the same ankle in the control match. For example, if the FAI subject had chronic disability in the left ankle, then it was compared with the left side in the control match. Similarly, the uninvolved ankle was compared with the same ankle in the control. In addition, the FAI group's involved ankle was compared with the opposite uninvolved ankle.
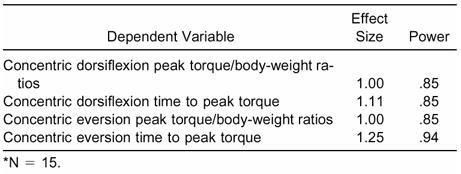
We performed four 2 × 2 × 2, three-way, mixed-model analyses of variance to investigate the group-by-ankle-by-speed interaction. The between-subjects factor was group status (FAI versus CON) with repeated measures on the 2 ankles (involved versus uninvolved) and 2 isokinetic speeds (120°·s−1 versus 240°·s−1). The dependent variables were concentric PT/BW for dorsiflexion, concentric PT/BW for eversion, concentric TPT for dorsiflexion, and concentric TPT for eversion. Significant interactions were examined with a Tukey Honestly Significant Difference post hoc analysis. An a priori alpha level of significance was set at P < .05 for all comparisons. We used the Statistical Package for the Social Sciences for Windows (version 10.0.0, SPSS Inc, Chicago, IL) to assist with the statistical analyses. Post hoc effect sizes were also determined for each of the 4 dependent variables studied using a method described by Cohen.25 Effect sizes for the 4 dependent measures ranged from 1.00 to 1.25 (Table 1).
Table 1. Effect Sizes of All Dependent Variables*
RESULTS
Concentric Dorsiflexion
The PT/BW ratios for concentric dorsiflexion ranged from 0.68 to 1.30 in the FAI group and from 0.69 to 1.57 in the CON group. Concentric PT/BW means for each group are found in Table 2. We found no significant differences among any of the factors (ankle, speed, and group) involving the PT/BW ratios (F1,28 = .054, P = .817). Of particular interest, there was no difference in PT/BW ratio measures between the involved and uninvolved ankles in the FAI subjects and no differences between the groups.
Table 2. Dorsiflexion Concentric Peak Torque/Body-Weight Ratios*

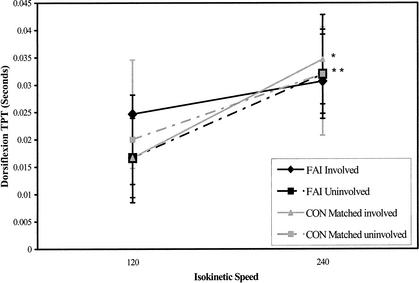
The TPT values ranged from 0.00 to 0.05 seconds in both the FAI and CON groups. Concentric TPT means for each group are found in Table 3. We found a significant 3-way (ankle-by-speed-by-group) interaction (F1,28 = 6.131, P = .020) for the concentric TPT variable (Figure). The Tukey post hoc analysis demonstrated that differences of ≥ .010 seconds were needed for significance. The concentric TPT measurements taken at 240°·s−1 were significantly higher than the concentric TPT measurements at 120°·s−1 for the CON involved, CON uninvolved, and FAI uninvolved ankles. There was no statistical difference in concentric TPT between these 2 speeds in the FAI involved ankles. Furthermore, no significant differences were noted in concentric TPT between the FAI and CON groups when the involved and uninvolved ankles were compared. As expected, the speed main effect was significant (F1,28 = 47.815, P < .001). The TPT values at 240°·s−1 (.032 ± .009 seconds) were significantly greater than the TPT values at 120°·s−1 (.020 ± .009 seconds).
Table 3. Dorsiflexion Concentric Time to Peak Torque Values*
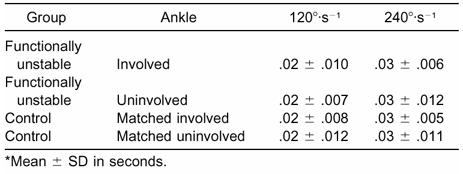
Fig. 1.
Significant ankle-by-speed-by-group interaction for dorsiflexion concentric time-to-peak-torque values. FAI indicates functionally unstable group; CON, control group.
Concentric Eversion
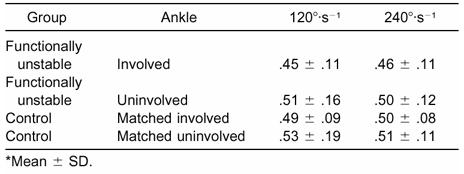
The PT/BW ratios for concentric eversion ranged from 0.29 to 0.96 in the FAI group and from 0.29 to 1.09 in the CON group. Concentric PT/BW means for each group are found in Table 4. The main effect for ankle was significant (F1,28 = 4.918, P = .035). The ratios in the involved ankles (0.47 ± 0.10) were significantly lower than the ratios in the uninvolved ankles (0.51 ± 0.14). What is important to remember, however, is that the main effect combines the ratios across both speeds and groups. Interestingly, there were no differences in eversion PT/BW ratios between the ankles of the FAI group alone or between the groups.
Table 4. Eversion Concentric Peak Torque/Body-Weight Ratios*
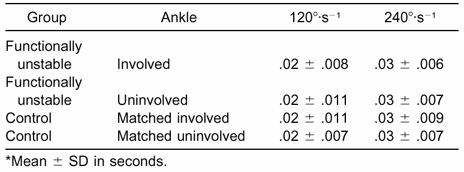
The TPT values ranged from 0.00 to 0.04 seconds in the FAI group, while the values in the CON group ranged from 0.00 to 0.05 seconds. Concentric TPT means for each group are found in Table 5. As expected, the main effect for speed was significant (F1,28 = 70.313, P < .001). The TPT values at 240°·s−1 (.030 ± .007 seconds) were significantly slower than those TPT values at 120°·s−1 (.018 ± .009 seconds). No significant interactions or other main effects were demonstrated in this analysis.
Table 5. Eversion Concentric Time to Peak Torque Values*
DISCUSSION
We hypothesized that the involved and uninvolved ankles from the group experiencing FAI would have significantly smaller concentric PT/BW ratios than those ankles in the CON group for both eversion and dorsiflexion motions. Therefore, we were surprised to find that this was not the case. When comparing the matched ankles of the FAI and CON groups, the PT/BW ratios were not significantly different. Others8,9 provide limited support, reporting no differences in strength of the evertors when comparing FAI ankles with controls. The clear distinction between those authors' findings and ours is that they used isolated concentric, eccentric, and isometric muscle actions to compare strength differences and not an SSC protocol. Perhaps strength is not an issue in the FAI group regardless of the strength-testing protocol administered.
Our study was designed to identify differences in concentric PT/BW ratios and concentric TPT of the dorsiflexors and evertors in uninjured and functionally unstable ankles using an SSC protocol with an isokinetic dynamometer. After an exhaustive literature review, we determined that our study was the only one known to investigate the SSC in individuals with FAI. Other researchers have investigated isolated eccentric, concentric, and isometric muscle actions of the ankle.1,8,9,26 Although these studies were necessary and historically important in determining raw strength differences in unstable ankles, our study takes a functional perspective on strength testing for those with FAI. Concentric contractions are commonly preceded by eccentric actions in sports and activities of daily living. Isolated muscle actions are unnatural in sports, and it is unusual to begin a movement from a static position; typically, an initial countermovement in the opposite direction is required. For example, when a basketball player attempts to rebound a ball, he or she normally squats immediately before jumping up for the ball. Everyday activities such as walking, running, and jumping meet the SSC criteria, in which an eccentric preload is immediately followed by a concentric contraction. Walking, running, and jumping consist of many SSC sequences in which the eccentric and concentric actions are coupled. This coupling creates a stronger concentric contraction than an isolated concentric contraction.17,19,21,27–32 Using a Kin Com dynamometer, Svantesson et al19 demonstrated that a concentric contraction preceded by an eccentric action (ie, SSC) generated approximate average torque values 100% larger than a concentric contraction alone. They examined the SSC phenomenon in the ankle plantar flexors at both 120°·s−1 and 240°·s−1. Helgeson and Gajdosik17 reported similar results when testing the SSC with the quadriceps femoris muscle group on a Biodex isokinetic dynamometer (Biodex Medical Systems Inc, Shirley, NY).
Mechanisms for the increase in the concentric contraction within the SSC have been proposed. One plausible explanation is that the time to develop force is longer when an eccentric action precedes a concentric contraction, allowing the muscle to become fully activated before beginning concentric contraction.33 Because the positive work is measured as area under the curve, an increase in muscle force due to greater muscle activation at the beginning of a concentric contraction would enhance the amount of work that can be done.33 An additional explanation is force potentiation, which suggests that muscle-force production is enhanced due to the preceding stretch stimulus.33 Reasons most often suggested for this stronger concentric contraction include the myotactic stretch reflex17,19,21,30,32 and the reaction of the muscle's elastic properties to the eccentric prestretch.17,19,21,27–32 Testing isolated actions may not account for these responses. Therefore, an SSC protocol may be more functional than a protocol using isolated eccentric, concentric, and isometric actions. Training with the SSC, the basis of plyometric exercise, is quite functional and would be advocated if our hypotheses were correct. Training using an SSC protocol has been suggested to improve the stretch reflex via an increase in muscle-spindle sensitivity and Golgi tendon organ inhibition, enriching the muscles' elasticity, decreasing amortization time, and promoting neuromuscular coordination, all of which in concert enhance force output and dynamic stability.21,32,34 Therefore, we felt that an investigation of the SSC in subjects with FAI was warranted.
We further hypothesized that the FAI group's involved and uninvolved ankles would have significantly slower concentric TPTs than the CON group ankles across both eversion and dorsiflexion movements. The ankle-by-speed-by-group interaction involving the dorsiflexion concentric TPT measures was significant; however, differences were evident only between the 2 isokinetic speeds within the ankles. We found it quite surprising that no difference in TPT existed between the FAI and CON group ankles. Without other studies for comparison, it is difficult for us to offer explanations. Yet it must be noted that TPT measurements taken from the Kin Com dynamometer were measured to 0.01 second. Perhaps if the TPT measurements had been derived using a more precise timing instrument (one that can read in milliseconds), differences in TPT between the groups might have been evident. We believe that this was a limitation of our method for assessing this variable.
No previous studies accounted for TPT in a functionally unstable ankle. Our hypothesis was based on passive ankle-perturbation studies that indicated slower reaction times in subjects with functionally unstable ankles when compared with uninjured subjects.6,15,16 In these passive perturbation studies, subjects stood on a trapdoor that dropped downward in a motion imitating the classic inversion ankle sprain. Motor latencies were measured by electromyography for the lower leg muscle's reaction to perturbation. These studies demonstrated that that the myotactic stretch reflex was slower in people with functional ankle instability during passive perturbations.
In our study, we thought that a slower reactive stretch reflex could influence concentric TPT in the FAI group in an active SSC state; however, this idea was not supported by the evidence. Some possible explanations are the open chain testing method, the relatively small arc of inversion, and the relatively slow velocities permitted by the instrument. Ricard et al35 reported maximum inversion velocity during closed chain testing at 740°·s−1. Unfortunately, the Kin Com dynamometer we used has a maximum velocity setting of 240°·s−1, making it impossible for us to measure at such high speeds. Another possible reason for not finding differences between groups in our study may be that the testing protocol did not facilitate a stretch response in the subjects. Perhaps the stretch reflex in a conscious, active state does not affect muscle activity in the FAI subjects to the same degree that it does during passive ankle perturbation. Subjects in our study consciously and actively moved the footplate of the isokinetic dynamometer, whereas during an ankle perturbation, a passive strategy is employed. During passive states, the stretch reflex serves as a monosynaptic negative-feedback model devoted to postural controls; however, in the active states, the reflexes may be modified by polysynaptic central controls.36 In active states, the muscle-spindle activity may be mentally biased by the alpha motor neuron for optimal extrafusal muscle contraction.21 Therefore, processing differences exist in the stretch reflex between the active and passive states. By chance, functionally unstable ankles may be more likely to be sprained while the subjects are in an unconscious, passive, perturbed state compared with an active, conscious state.
Lastly, we were interested in determining if differences in concentric TPT and PT/BW ratios existed between the involved and uninvolved ankles in the FAI group. We had anticipated no differences and, indeed, this was the case. Our PT/BW ratio results are supported by Lentell et al,1,26 who indicated no concentric strength differences, and by Bernier et al,9 who noted no eccentric strength differences in the FAI group when bilateral isokinetic comparisons were made. In contrast, our results are inconsistent with those reported by Tropp,14 who showed evertor concentric strength deficits in the involved ankle in the FAI group when isokinetic measurements were compared with the uninjured side. However, none of the these studies involved an SSC strength protocol. The lack of differences in concentric TPT between the ankles is supported by 2 studies that showed no differences in reaction time in subjects with functional ankle instability during passive ankle perturbation when compared bilaterally.6,10 If there were indications that the myotactic stretch reflex was similar bilaterally in the FAI group, then this could influence concentric TPT in the active SSC condition. However, eliciting the stretch reflex in the active and passive states may be processed differently across individuals. This may explain the differences between our study and those studies previously performed using passive perturbations.
CONCLUSIONS
We chose a stretch-shortening protocol for this study because this method of testing was purported to be a more functional isokinetic test than testing eccentric and concentric actions in isolation. Using this protocol, we were unable to delineate any muscle-performance deficiencies in subjects with chronic ankle instability. No differences were noted in concentric strength or time to peak torque under the conditions of the study. These variables were hypothesized to be deficient in the group with functionally unstable ankles due to indications that the stretch reflex in these subjects may be affected. Typically, the peak torque values of our subjects were within 2° or .05 seconds from the concentric start angle. However, we speculate that group differences might have been evident had a greater ankle range of motion been used during testing. Further research is needed to understand the neuromuscular aspects of the ankle with regard to the stretch reflex and other proprioceptive variables.
REFERENCES
- Lentell G B, Bass B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Hertel J, Denegar C R, Monroe M M, Stokes W L. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508. doi: 10.1097/00005768-199911000-00002. [DOI] [PubMed] [Google Scholar]
- Hintermann B. Biomechanics of the unstable ankle joint and clinical implications. Med Sci Sports Exerc. 1999;31(suppl):459–469. doi: 10.1097/00005768-199907001-00007. [DOI] [PubMed] [Google Scholar]
- Baumhauer J F, Alosa D M, Renstrom A F, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- Kaikkonen A, Kannus P, Jarvinen M. A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med. 1994;22:462–469. doi: 10.1177/036354659402200405. [DOI] [PubMed] [Google Scholar]
- Lofvenburg R, Karrholm J, Sundelin G, Ahlgren O. Prolonged reaction time in patients with chronic lateral instability of the ankle. Am J Sports Med. 1995;23:414–417. doi: 10.1177/036354659502300407. [DOI] [PubMed] [Google Scholar]
- Garn S N, Newton R A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1998;68:1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H, Gansneder B M. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34:239–245. [PMC free article] [PubMed] [Google Scholar]
- Bernier J N, Perrin D H, Rijke A M. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- Ebig M, Lephart S M, Burdett R G, Miller M C, Pincivero D M. The effect of sudden inversion stress on EMG activity of the peroneal and tibialis anterior muscles in the chronically unstable ankle. J Orthop Sports Phys Ther. 1997;26:73–77. doi: 10.2519/jospt.1997.26.2.73. [DOI] [PubMed] [Google Scholar]
- Freeman M AR, Dean M RE, Hanham I WF. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Ravn J B. Prolonged peroneal reaction time in ankle instability. Int J Sports Med. 1991;12:290–292. doi: 10.1055/s-2007-1024683. [DOI] [PubMed] [Google Scholar]
- Brunt D, Andersen J C, Huntsman B, Reinhert L B, Thorell A C, Sterling J C. Postural responses to lateral perturbation in healthy subjects and ankle sprain patients. Med Sci Sports Exerc. 1992;28:171–176. [PubMed] [Google Scholar]
- Helgeson K, Gajdosik R L. The stretch-shortening cycle of the quadriceps femoris muscle group measured by isokinetic dynamometry. J Orthop Sports Phys Ther. 1993;17:17–23. doi: 10.2519/jospt.1993.17.1.17. [DOI] [PubMed] [Google Scholar]
- Voight M, Tippett S. Plyometric exercise in rehabilitation. In: Prentice W E, editor. Rehabilitation Techniques in Sports Medicine. 2nd ed. Mosby-Year Book; St Louis, MO: 1994. pp. 88–97. [Google Scholar]
- Svantesson U, Ernstoff B, Bergh P, Grimby G. Use of a Kin-Com dynamometer to study the stretch-shortening cycle during plantar flexion. Eur J Appl Physiol Occup Physiol. 1991;62:415–419. doi: 10.1007/BF00626613. [DOI] [PubMed] [Google Scholar]
- Zatsiorsky V M. The review is nice: I disagree with it. J Appl Biomech. 1997;13:479–483. [Google Scholar]
- Wilk K E, Voight M L, Keirns M A, Gambetta V, Andrews J R, Dillman C J. Stretch-shortening drills for the upper extremities: theory and clinical application. J Orthop Sports Phys Ther. 1993;17:225–239. doi: 10.2519/jospt.1993.17.5.225. [DOI] [PubMed] [Google Scholar]
- Hubbard T J, Kaminski T W. Kinesthesia is not affected by functional ankle instability status. J Athl Train. 2002;37:481–486. [PMC free article] [PubMed] [Google Scholar]
- Kaminski T W, Perrin D H, Mattacola C G, Szczerba J E, Bernier J N. The reliability and validity of ankle inversion and eversion torque measurements from the Kin Com II isokinetic dynamometer. J Sport Rehabil. 1995;4:210–218. [Google Scholar]
- Donatelli R. Normal biomechanics of the foot and ankle. J Orthop Sports Phys Ther. 1985;7:91–95. doi: 10.2519/jospt.1985.7.3.91. [DOI] [PubMed] [Google Scholar]
- Cohen J. 2nd ed. Erlbaum Associates; Hillsdale, NJ: 1988. Statistical Power Analysis for the Behavioral Sciences; pp. 20–40. [Google Scholar]
- Lentell G L, Katzman L, Walters M. The relationship between muscle function and ankle stability. J Orthop Sport Phys Ther. 1990;11:605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- Thys H, Faraggiana T, Margaria R. Utilization of muscle elasticity in exercise. J Appl Physiol. 1972;32:491–494. doi: 10.1152/jappl.1972.32.4.491. [DOI] [PubMed] [Google Scholar]
- Cavagna G A, Saibene F P, Margaria R. Effect of negative work on the amount of positive work performed by an isolated muscle. J Appl Physiol. 1965;20:157–158. doi: 10.1152/jappl.1965.20.1.157. [DOI] [PubMed] [Google Scholar]
- Cavagna G A, Dusman B, Margaria R. Positive work done by a previously stretched muscle. J Appl Physiol. 1968;24:21–32. doi: 10.1152/jappl.1968.24.1.21. [DOI] [PubMed] [Google Scholar]
- Radcliffe J C, Osternig L R. Effects on performance of variable eccentric loads during depth jumps. J Sport Rehabil. 1995;4:31–41. [Google Scholar]
- Belli A, Bosco C. Influence of stretch-shortening cycle on mechanical behaviour of triceps surae during hopping. Acta Physiol Scand. 1992;144:401–408. doi: 10.1111/j.1748-1716.1992.tb09313.x. [DOI] [PubMed] [Google Scholar]
- Duke S, BenEliyahu D. Plyometrics: optimizing athletic performance through the development of power as assessed by vertical leap ability: an observational study. Chir Sports Med. 1992;6:10–15. [Google Scholar]
- Enoka R M. 3rd ed. Human Kinetics; Champaign, IL: 2002. Neuromechanics of Human Movement; pp. 256–258. [Google Scholar]
- Swanik K A. University of Pittsburgh; Pittsburgh, PA: 1998. The Effects of Shoulder Plyometric Training On Proprioception and Muscle Performance Characteristics [dissertation] [DOI] [PubMed] [Google Scholar]
- Ricard M D, Sherwood S M, Schulthies S S, Knight K L. Effects of tape and exercise on dynamic ankle inversion. J Athl Train. 2000;35:31–37. [PMC free article] [PubMed] [Google Scholar]
- Clarac F, Cattaert D, Le Ray D. Central control components of a ‘simple’ stretch reflex. Trends Neurosci. 2000;23:199–208. doi: 10.1016/s0166-2236(99)01535-0. [DOI] [PubMed] [Google Scholar]