Abstract
Objective: The objective is to provide insight to understanding public health officials' needs and promote access to data repositories and communication tools.
Methods: Survey questions were identified by a focus group with members drawn from the fields of librarianship, public health, and informatics. The resulting comprehensive information needs survey, organized in five distinct broad categories, was distributed to 775 Tennessee public health workers from ninety-five counties in 1999 as part of the National Library of Medicine–funded Partners in Information Access contract.
Results: The assessment pooled responses from 571 public health workers (73% return rate) representing seventy-two of ninety-five counties (53.4% urban and 46.6% rural) about their information-seeking behaviors, frequency of resources used, computer skills, and level of Internet access. Sixty-four percent of urban and 43% of rural respondents had email access at work and more than 50% of both urban and rural respondents had email at home (N = 289). Approximately 70% of urban and 78% of rural public health officials never or seldom used or needed the Centers for Disease Control (CDC) Website. Frequency data pooled from eleven job categories representing a subgroup of 232 health care professionals showed 72% never or seldom used or needed MEDLINE. Electronic resources used daily or weekly were email, Internet search engines, internal databases and mailing lists, and the Tennessee Department of Health Website.
Conclusions: While, due to the small sample size, data cannot be generalized to the larger population, a clear trend of significant barriers to computer and Internet access can be identified across the public health community. This contributes to an overall limited use of existing electronic resources that inhibits evidence-based practice.
INTRODUCTION
Public health informatics is defined by Yasnoff and O'Carroll [1] as the “systematic application of information and computer science and technology to public health practice, research, and learning that integrates public health and information technology.” Public health informatics as an emerging discipline has achieved increased visibility in the medical information community over the past several years. In 1988, the Institute of Medicine's The Future of Public Health reported that the nation's public health system was in “trouble” and “disarray.” The report further charged that the public health system was incapable of “applying fully current scientific knowledge” and “generating new knowledge, methods, and programs” [2].
Over fourteen years later, public health is still plagued by an underuse of information and technology, and the literature regarding public health information needs and information-seeking behavior is in its infancy. Even though a National Health Information Infrastructure (NHII) was proposed in 1995 [3], the interim report published in June 2000 admitted that the NHII did not exist in any “comprehensive” way [4]. The NHII is the set of technologies, standards, applications, systems, values, and laws that support all facets of individual health, health care, and public health. The vision of NHII is to deliver information to individuals—professionals as well as consumers and patients—when and where they need it, so they can use this information to make informed decisions. The American Medical Informatics Association (AMIA) Congress in 2001 advocated the rapid development of informatics in the public health community to face the new challenges of “bioterrorism, emerging infections and antibiotic-resistant organisms” [5]. A 2002 report from the Institute of Medicine, The Future of the Public's Health in the 21st Century, contended that underfunding, lack of political support, and unprepared workers contributed to this inadequate system, and, in fact, the executive summary stated that a “majority of government public health workers have little or no training in public health” [6]. Public health agencies adopted technology early but created separate, narrow applications that could not be integrated into other systems [7]. The telecommunication infrastructure necessary to deliver an information system to support small rural communities across the United States was missing in 1999.
AMIA recommends federally funded, dedicated, high-speed Internet access for all public and private health care facilities and related organizations [8]. To improve the nation's health outcomes, public health officials need to employ data systems containing individual and community information across jurisdictions and exchange these data to implement effective policies to avert acute events as well as address chronic diseases. Despite the strong calls for greater access to technology and training for public health workers, few formal studies of information needs and information-seeking behaviors in the community have been reported. To benchmark current public health information use and to develop training options for the information problems besetting public health, agencies including the National Library of Medicine have formed a coalition, the Partners in Information Access for Public Health Professionals, and have initiated a series of contracts to promote information use and Internet connectivity in the public health community. The Eskind Biomedical Library (EBL) at Vanderbilt University Medical Center (VUMC) was awarded an eighteen-month contract in 1999. This paper introduces the project's goals and presents findings from the EBL's assessment of the Tennessee public health community's information-seeking behaviors and needs.
BACKGROUND
Perhaps more than any other group of health professionals, public health workers embody the concept of diversity. The field of public health draws workers from the disciplines of nursing, health education, epidemiology, toxicology, environmental health, social work, nutrition, inspection, administration, and clinical medicine [9]. Among and within these subgroups, there are differing levels of education, different cultural practices, and a wide array of information-use styles [10]. Reflecting this heterogeneity, public health professionals' information needs do not fall into one domain. Rather, they include such diverse subject matters as air and water quality, violence prevention, day care and boarding home oversight, hospital regulation, smoking prevention, migrant health, food safety, sewage disposal, animal control, hazardous waste management, and many others [11]. The quality of information available on these subjects varies widely, as do the abilities of individual public health professionals to retrieve and judge information quality. Moreover, existing technologies for accessing important information resources have limitations, not only in terms of use and retrieval but also in terms of availability in rural and remote areas. As a result of all these factors, public health professionals need improved training, access, connectivity, and awareness of information resources and quality.
Despite their diversity, public health professionals share common training needs, including how to search effectively, how to evaluate the quality and authority of online information, where to search for different kinds of data, how to implement best practice information, and how to use information technologies for effective communication [12]. Although attention is being paid to public health training needs and information access through collaborations like the Partners in Information Access for Public Health Professionals [13–15] information awareness projects and national conferences such as the AMIA Spring 2001 Congress [16] to develop a national public health informatics agenda, few studies report the methods, the sources, or the frequency of information used by public health professionals. As Humphreys remarks, “few would argue that those seeking health policy or public health information are as well served as those seeking information relevant to clinical care or basic biomedical research” [17]. There is a dearth of formal studies of information needs and information-seeking behavior in health policy and public health, but available evidence suggests that many factors inhibit access [18].
The available studies generally surveyed connectivity or education needs. For instance, Hollander and Martin assessed equipment availability, Internet access, staff use of the Internet, and training opportunities among 348 Midwestern local health departments (LHD) in 1997 [19]. One summary questionnaire was sent to 713 LHDs in ten states, and the respondent in each LHD answered for the entire staff. These authors noted that 85% of LHD respondents had access to at least one Internet-capable computer. The National Association of County and City Health Officials (NACCHO) 1999 survey of health departments levels of access to the Internet found that, while larger health departments often had access to the Internet, connections were rarely high speed or available to all staff. Significantly, the survey reported that 25% of health departments serving smaller jurisdictions lacked Internet access altogether [20]. This survey did not report individuals' methods or levels of access.
Gale [21] surveyed Washington state public health professionals regarding their training needs; one of the highest-rated needs was for training in electronic communication, which the authors did not define but noted could range from email communication to using the Internet for research. Similarly, O'Carroll [22] used a focus group of twenty-three health policy makers from across the country to investigate needs, and Rambo [23] surveyed seventy public health officials to identify information needs and information-seeking behaviors in the Washington state public health workforce. Chambers [24] queried members of a segment of the Canadian public health workforce about their use of various information resources.
Forsetlund and Bjorndal [25] conducted focus groups with fifty-two Norwegian public health practitioners (M.D.s) and an observational study of six of these public health physicians. Using the focus groups, the researchers identified cases in which searching for research-based information was appropriate and noted if these practitioners perceived and identified the same cases. The practitioners felt that many cases called simply for professional judgment, as opposed to evidence-based knowledge, and their general consensus was that they rarely had occasion to deal with questions requiring research-based information. These authors established that the practitioners were not opposed to using research for environmental issues, for example, but thought that evidence-based public health did not really apply to “management and organization.” Forsetlund and Bjorndal were able to identify at least six clear cases of problems that qualified for research-based information that the practitioners did not recognize in the focus group observation. During the six practitioner observation periods, Forsetlund and Bjorndal identified twenty-two more cases of questions where research could be used to support decision making, while the Norwegian public health practitioners did not identify any questions where research was necessary. These investigators concluded that generating research questions was not a common approach in public health practice [26]. This study provided evidence that framing objectives to measure public health outcomes could help provide incentives to use evidence-based research.
Other authors have also proposed methods to integrate electronic information resources into public health practice [27–29]. This paper will add to this small but growing body of knowledge of information-seeking behavior among a diverse group of public health officials through discussing the EBL's partners–funded effort to benchmark the awareness of vital information resources in the Tennessee public health community.
TRAINING PARTNERS FOR TENNESSEE PUBLIC HEALTH
The broad goals of the EBL's project are to increase the quality and quantity of awareness and usage of online information resources among Tennessee public health professionals, increase communication in the public health professional community, and increase what is known about how public health professionals use online information sources. In support of these broad goals, the project's specific objectives are to (1) develop and expand partnerships between EBL and public health organizations in the target region; (2) provide instruction, training, and support in the use of online resources and services such as PubMed and LoansomeDoc to targeted members of the public health community; (3) increase public health professionals' awareness of National Library of Medicine grant opportunities and other methods of bringing online connectivity to their home organizations; and (4) provide an online forum for public health professionals to access relevant resources and communicate with each other.
To achieve these aims, the EBL initiated several parallel strategies including developing the Training Partners for Tennessee Public Health (TPTPH) partnership [30], a broad-based coalition of the EBL, state and metropolitan health departments, a university-centered public health policy group, and the Area Health Education Center (AHEC) program of Tennessee. Other strategies included implementing a comprehensive information-needs assessment, a statewide video teleconference to broadcast information about training and grant writing opportunities, multiple training sessions, a Website, and a mailing list to foster communication in the public health community.
This paper addresses the results of the initial information-needs assessment conducted in October 1999 in preparation for developing the training session curriculum and the TPTPH Website. Over the course of the project, the EBL trained approximately 180 Tennessee public health workers in: (1) basic Internet searching, (2) use of PubMed MEDLINE, (3) use of the Centers for Disease Control and Prevention (CDC) Wonder and other statistical repositories, (4) use of Health Information Tennessee and the National Center for Health Statistics, (5) location and assessment of model program Websites, and (6) electronic document delivery via LoansomeDoc. The key to developing this comprehensive training program was the EBL's benchmark information-needs and information-seeking behavior assessment.
METHODS
The authors developed the needs assessment using an iterative method of individual and focus group review (Appendix). After developing a straw-man assessment, we convened a group of leaders from the Tennessee state health department, the Davidson County Metropolitan Health Department, and Tennessee environmental agencies as well as academic preventive medicine to review and comment on the usefulness and relevance of the questions. To obtain a representative opinion on the survey, we also asked public health experts from both rural and metropolitan regions to review the revised assessment and then tested the newly modified survey with several individuals from the state and local health departments.
The assessment tool was divided into questions covering professional and demographic information including job category based on employment grades used by the state health department, race or ethnicity, education, number of years in the profession, and information use and information-seeking behaviors including the frequency of use and type of resource used to locate information. We modified Rambo's [31] useful dissection of the categories of information generally employed in public heath (e.g., directory information, legislative information, health and environmental data, etc.) and asked respondents about their frequency of use of each category as well as frequency and type of nonelectronic (colleagues, news media, etc.) and electronic (CDC Wonder, Health Information Tennessee, etc.) resources used. We deliberately included a number of resources we felt were not likely to be heavily used, so that we could raise the community's awareness of these resources.
The survey queried respondents about their computer and information technology use, including questions about access to a computer and Internet connection, hours of computer use, and self-rated proficiency in various types of software. Respondents were asked to rate their preferred methods for learning (one-on-one, group sessions, etc.) and were queried about their grant-writing activities and interest in learning more about the grants process. Respondents were not “proctored” as they completed the survey, and, because the survey instrument was on paper, no “required fields” could be enforced, as they could be with an online survey. Because responses to many questions were dependent upon earlier questions, the number of responses varied substantially per question. Finally, the assessment concluded with space for respondent comments and open-ended questions about what resources or tools would enable respondents to work more efficiently.
Seven hundred seventy-five needs assessment questionnaires were distributed to individual public health workers at their workplaces, and 571 completed surveys from public health workers in seventy-two of ninety-five counties were returned for a response rate of 73%. Leaders from the Metropolitan Davidson County Health Department and Tennessee Health Department Bureau of Health Services guided the distribution of the sample to promote broad survey representation among public health professionals throughout the state.
The high survey return rate is a testament to the importance of collaborative partnerships in the EBL project. Not only did the partner contacts in the state and local health departments distribute the needs assessment, they encouraged their staff to complete the survey and collected completed surveys. The authors coded each survey with a distribution code and unique number to indicate in which of the thirteen health statistics regions the respondent worked; surveys were anonymous, but the codes allowed us to determine where response rates were lower and differentiate between urban and rural respondents. The questionnaire included 174 variables that we analyzed using SPSS™ version 10.0 to provide frequency data.
RESULTS
Demographics.
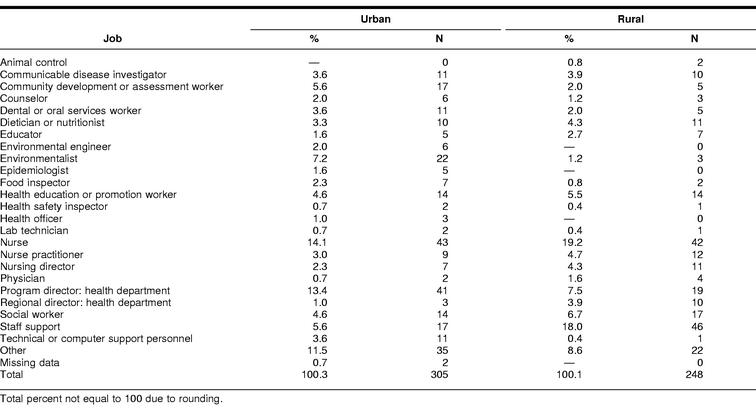
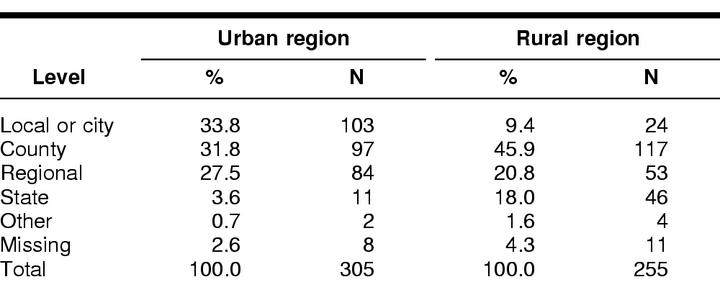
The Tennessee Health Department Bureau of Health Services divides the state into thirteen statistical regions, six urban and seven rural. The six urban regions or counties are Davidson (Nashville), Shelby (Memphis), Hamilton (Chattanooga), Knox (Knoxville), Madison (Jackson), and Sullivan (Johnson City). Tennessee has a county-level health officer in each of the ninety-five counties in addition to a local county director and a board of health. These health regions are shown in Figure 1. Respondents were asked to select from twenty-five categories to describe their specific job functions, as shown in Table 1 (N = 553). The total number of six physician respondents listed in Table 1 is misleading, because physicians are represented in other categories such as epidemiologists, communicable disease investigators, dentists, and regional health directors. Nurses are represented in categories for nurse practitioner, nursing director, educators, and health education or health promotion worker. Table 2 (N = 560) shows the distribution between urban and rural regions of survey respondents and the level or jurisdiction where they worked. Fifty-four percent were from urban regions and 46% from rural regions. The majority of respondents worked at the city or county level. In urban regions, 65.5% work on the city or local or county level, while 55.3% of the rural sample worked on the city or local or county level. The slight difference in urban versus rural percentages varies between Table 1 and Table 2, because the response rate for job category (N = 553) is lower than the response rate for jurisdiction level (N = 560).
Figure 1.
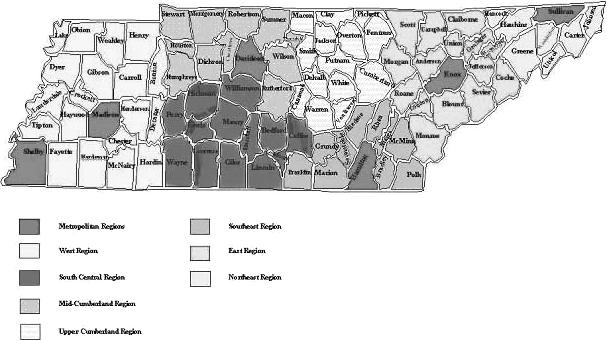
Tennessee health regions
Table 1 Distribution of public health officials by job function (N = 553)
Table 2 Urban versus rural health professionals: level of jurisdiction (N = 560)
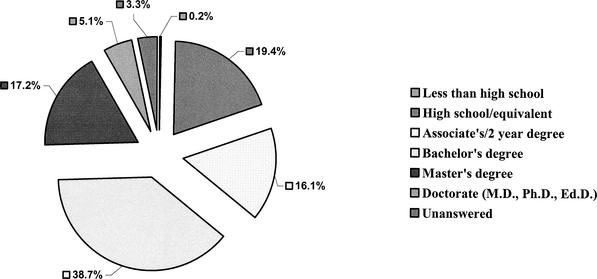
The education distribution shown in Figure 2 reveals 22% had either master's or doctorate degrees, while 38% had bachelor's degrees (N = 571). Seventy-seven percent of respondents were female and 23% male (N = 541). Twelve percent of respondents were African-American, while 86% listed themselves as white; very small percentages of respondents classed themselves as American Indian, Hispanic, Asian, or other (N = 565). Ninety-seven percent of respondents used English language exclusively, while 3% used other languages such as Spanish, Sign, Thai, and Arabic in the workplace (N = 540).
Figure 2.
Educational distribution of respondents (N = 571)
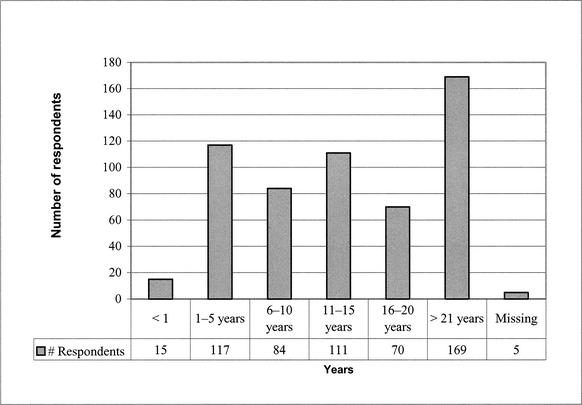
Respondents were fairly evenly distributed in the number of years they have been employed in public health; a high number of respondents, almost 30%, indicated they had greater than twenty years of experience in the field. Twelve percent indicated they had sixteen to twenty years of experience, 19% had eleven to fifteen years, 14.71% had six to ten years, 20.49% had one to five years, and 3% had less than one year of experience (N = 571). Figure 3 outlines respondents' years of experience.
Figure 3.
Public health workers: years of experience
Computer and Internet access.
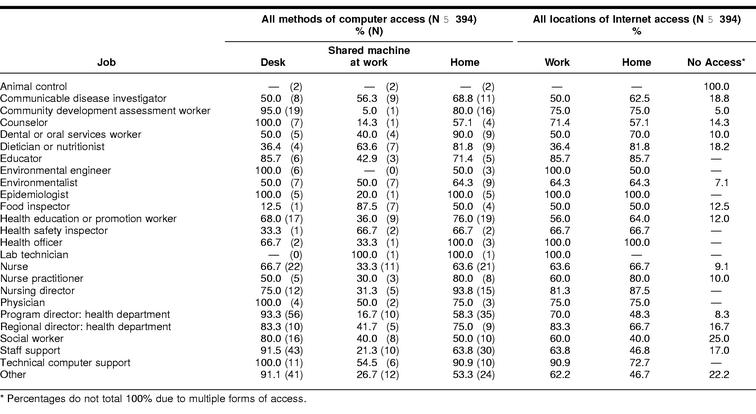
We asked users to indicate all methods of computer access: machine at desk at work, shared machine at work, or machine at home. All local health departments in Tennessee had at least one Internet-capable office computer in 1999. However, no state email system was available for all health department employees at the time of the survey. The survey results showed that the number of individuals sharing computers was much higher than we expected. We defined a high frequency of sharing desktop computers as one-third of respondents in any job category. Frequencies in Table 3 do not add up to 100% because respondents could have checked all three methods if they had a computer on their desks but had to share it with others, in addition to having computer access at home. Table 3 shows respondents by job category who had access to the Internet at work or at home and the percent who had no access. Data shown in Table 3 are derived from only 394 respondents who answered a series of questions about both computer and Internet access.
Table 3 Computer and Internet access by job function
Though a total of 553 respondents categorized their job function in Table 1, not all of these professionals answered the computer-related questions. The two animal control workers whose jobs were primarily in the field and who responded to this question had no access to a computer or the Internet either at work or home. Thus, a value of 100 in the “No Access” column of Table 3 is interpreted as no person in that job category had Internet access at any location. Seventy-five percent of nursing director respondents had desktop computer access compared to 50% of nurse practitioners. The nursing directors also showed a higher percentage of Internet access at work (81.3%), compared to nurse practitioners, of whom only 60% had Internet access at work. Only in the job categories of epidemiologists and environmental engineers did 100% of respondents indicate having a desktop computer and Internet access at work.
However, unlike the desktop computer–access questions, the Internet access data do not show if the individuals' Internet access was on their desktop or from a shared computer in the same office. The key partners who reviewed the survey questions advised us that Internet access was not widespread throughout the regional offices and local health departments; therefore, we did not structure the survey to ascertain the number of individuals sharing Internet access in an office. Although two job categories had 100% of respondents with desktop computers and Internet access, we cannot conclude the Internet access was from the respondents' desktop computer.
Physicians, counselors, and computer support staff respondents had 100% access to desktop computers but did not all have Internet access from these machines. Several other job groups who had limited Internet access at work indicated having access at home: health officers, 100%; dieticians, 81.8%; health safety inspectors, 66.7%; dental or oral services workers, 90%; educators, 74.1%; and communicable disease investigators, 68.8%. Many respondents had multiple methods of computer access. It is important to note that though many had access through a shared computer at work, this computer could be the primary desktop of another worker, rather than an open-access machine found in a library. Access to the Internet at work did not necessarily mean exclusive use of the computer. Those who had desktop computers—such as nurses, 66.7%; nurse practitioners, 50%; and nursing directors, 75%—also indicated a high percentage of computer sharing. Another job category revealing a high frequency of computer sharing was social worker; while 80% had desktop access, 40% had to share and 25% had no access to the Internet at work or home. Values and frequencies shown in Table 3 reveal the small sample size in these job categories; however, the trend toward limited computer and Internet access is clear across most job groups. Of the twenty-five job categories in Table 3, fifteen, or almost two-thirds, showed a sharing frequency above 33%. The survey did not determine the number of individuals sharing a single computer. It is important to remember that in 1999 Internet service in many small communities in Tennessee did not exist, so the absence of home access was not necessarily by choice.
Many of these professionals were involved with direct patient care daily, so the survey queried respondents about hours of work-related computer use per week (other than patient system/data entry). The median number of hours of weekly computer use by epidemiologists was 40 hours; nursing directors, 5 hours; nurse practitioners, 2 hours; nurses, 5 hours; community assessment workers, 20 hours; environmental engineers, 15 hours; health educators, 10 hours; physicians, 5.5 hours; counselors, 20 hours; and communicable disease investigators, 5 hours. Though many workers shared computers, these data showed that, for most job categories, tasks requiring a computer were not their primary work activities.
Computer proficiency and email access.
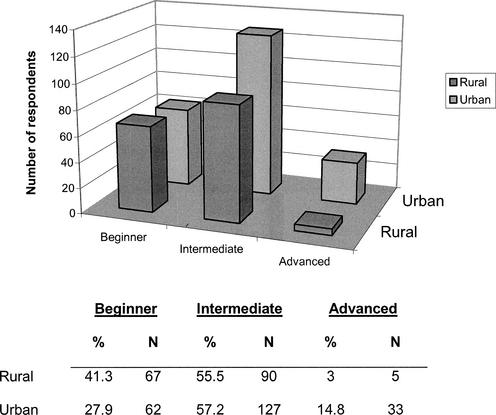
The survey also asked respondents to rate their computer expertise as beginner, intermediate, or advanced. Figure 4 indicates the urban versus rural respondents' self-ranking of their expertise (N = 384). Self-reported “intermediate users” in both urban and rural regions were similar, ninety and 127, respectively, but sixty-seven of the rural respondents rated themselves as beginners, while only sixty-two of the urban respondents rated themselves beginners. In marked contrast, only five of rural respondents considered themselves advanced users, while thirty-three of urban respondents self-reported as advanced users.
Figure 4.
Self-ranking of computer expertise (N = 384)
Sixty-four percent of the urban and 43% of the rural respondents had email access at work, and more than 50% of both urban and rural respondents had email at home (N = 289). Of those who did not have email in 1999, 94% of urban and 92% of rural respondents indicated they did want to use email (N = 143).
Grant-writing information.
Twenty percent of respondents indicated they wrote grants; 0.05% noted that grant writing “could be” a job duty. The needs assessment also asked participants what grant-related training they desired. Of the 221 respondents who answered this question, 95% (N = 210) indicated they needed basic instruction in locating grant sources and the mechanics of writing a proposal. Other respondents noted they wanted instruction in administering a grant after its award, and a few listed specific kinds of grants they were seeking—health department construction funding, funding for housing facilities for alcoholics or substance abusers, and funding for health maintenance and education programs. One respondent desired instruction in writing outcome-based goals and objectives and in designing evaluation strategies.
Information-seeking behaviors and resources used.
We modified the public health information categories described by Rambo [32] to ask respondents to indicate how often they used various categories of information. This paper presents a subset of the voluminous frequency data for each of these resources. Frequency data from selected questions give us insight into the information-seeking habits of the respondents. We asked respondents whether they used any of the following methods to locate information (respondents could select as many methods as applied): looking for information themselves, asking an assistant to locate information, asking a colleague to locate information, or asking a librarian to locate information. Not surprisingly, 95% of respondents (N = 542) indicated they looked for information themselves. Just 24% asked assistants to locate information, and, as is often seen in the biomedical community, overall 65% of respondents noted they asked colleagues for information.
The survey briefly defined each resource category and left room for respondents to add categories if they desired. The most frequently consulted categories of information included directory information (telephone numbers/addresses, schedules for official meetings, events, etc.), used daily by 51% of respondents, and internal communications (telephone calls, memos, etc.), used daily by 62% of respondents (N = 553). Many respondents, 24%, also used internal documents such as unpublished reports, manuals, and policies daily, and 24% of respondents indicated they used information about their computers daily.
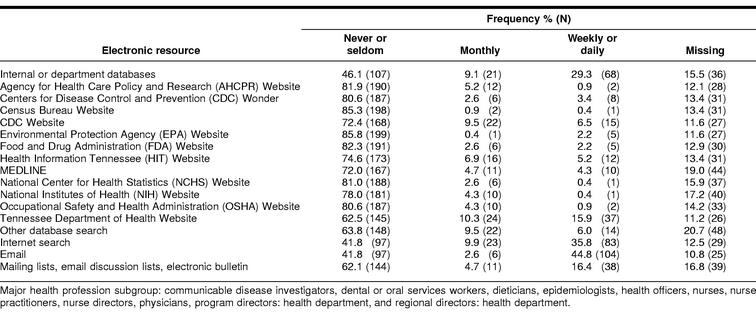
Health professional subgroup usage of electronic resources.
Pooled responses from fourteen job functions encompassing individuals in clinical medicine, nursing, epidemiology, and public health services management were targeted for a subgroup analysis to focus on their information-seeking habits as opposed to the broader diverse population. Jobs selected for this analysis were: communicable disease investigator, community development assessment, counselor, dental or oral services worked, dietician, educator, health education or promotion worker, nurse, nurse practitioner, nursing director, physician, program director, regional director, and social worker. Data in Table 4 show this subgroup analysis of responses from the major health profession categories, revealing usage and frequency of major resources critical to the public health mission. The survey form divided frequency into five categories: never, seldom, monthly, weekly, and daily, but the subgroup analysis collapsed frequency into three groupings, “Never or Seldom,” “Monthly,” and “Weekly or Daily.” Results revealed that the top five electronic resources used weekly or daily were: email, 44.8%; Internet search, 35.8%; internal databases, 29.3%; mailing lists and email discussion lists, 16.4%; and Tennessee Department of Health Website 15.9%. The CDC was ranked sixth, with 6.5% using the site daily or weekly. The five sites most frequently identified as never or seldom used are: (1) Environmental Protection Agency (EPA) Website, 85.8%; (2) Census Bureau, 85.3%; (3) Food and Drug Administration (FDA) Website, 82.3%; (4) Agency for Health Care Policy and Research (AHCPR), 81.9%; and (5) National Center for Health Statistics (NCHS), 81%. CDC Wonder was never or seldom used by 80.6% and Health Information Tennessee (HIT) by 74.6%. Table 4 also reports frequency of missing values or no response for the resource, because, in some cases, these numbers are large.
Table 4 Frequency of use of electronic resources by subgroup of major health professions (N = 232)
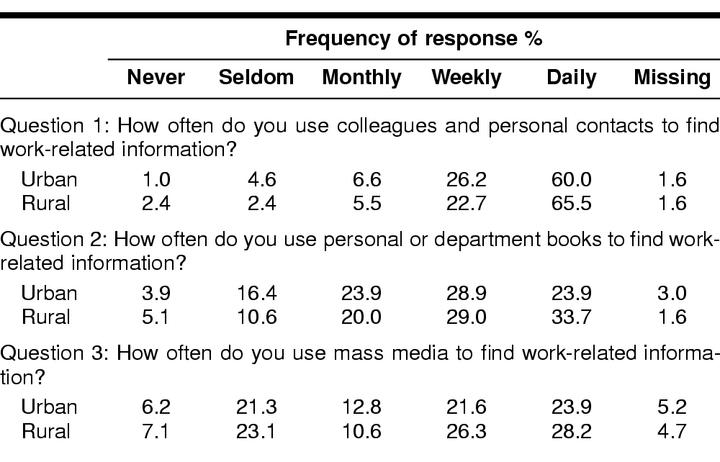
Nonelectronic resources: urban versus rural.
The survey asked respondents to indicate how frequently they consulted various nonelectronic resources for information. Table 5 shows the summary results subdivided by urban or rural respondents. Colleagues were among the most frequently used resources for information, with 60% of urban respondents and 65% of rural respondents consulting colleagues daily, shown in question 1 of Table 5. Personal or departmental books were highly used resources as well, with 52.8% of urban respondents consulting books daily or weekly and 62.7% rural consulting personal collections either daily or weekly (Table 5, question 2). Dependence upon mass media (including newspapers, radio, and television), shown in Table 5, question 3, was not surprising, because public health services work is frequently “complaint-driven” and reported in mass media. The distribution between urban and rural areas did not vary substantially.
Table 5 Frequency of use of non-electronic resources (N = 571)
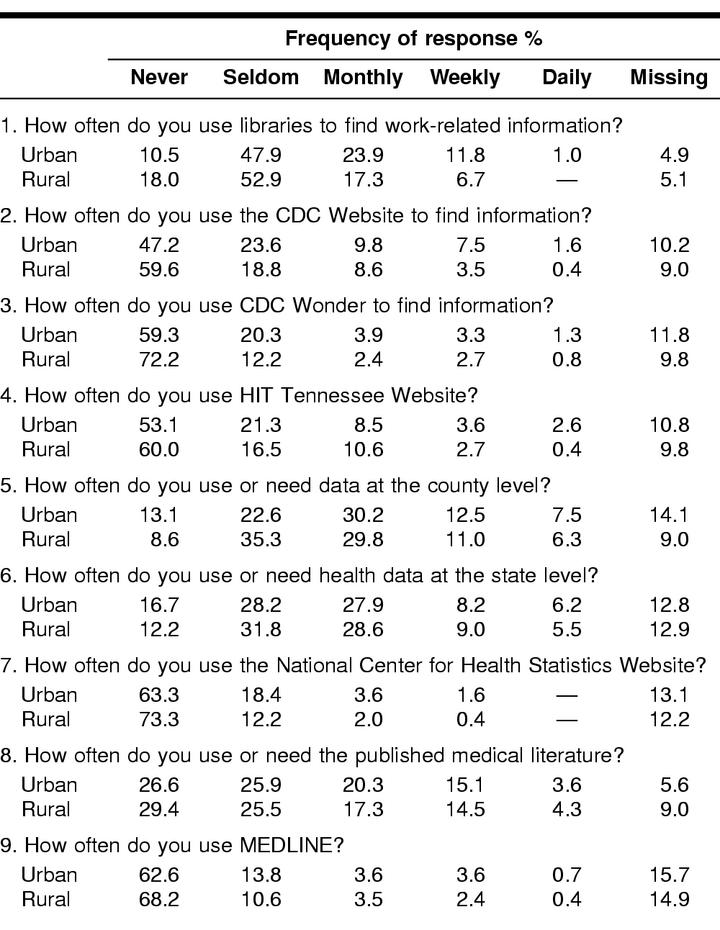
Libraries and electronic resources use: urban versus rural distribution.
Table 6 reports frequency categories: never, seldom, monthly, weekly, or daily and the urban versus rural distribution of all respondents (N = 571) for nine resources recognized as important for public health officials. Question 1 in Table 6 documents the low use of libraries. More than 58% (58.4%) of urban and 70.9% of rural respondents never or seldom use libraries to find information. Currently, academic medical library collections are located in Memphis, Nashville, Knoxville, and Johnson City. Public health officials in the counties surrounding Nashville can purchase an access card for the EBL. The Davidson County Metropolitan Health Department is the only health department in the state with its own library collection and full-time professional librarian.
Table 6 Frequency data for libraries and electronic resources: urban versus rural distribution (N = 571)
Table 6 shows the responses from questions asking if the respondents either use or need the electronic resource or a specific type of health information. We wanted to determine if respondents use the appropriate electronic resource to meet an identified information need. Table 6, question 2, reveals that only about 9% of urban and 4% of rural respondents use the CDC Website either daily or weekly for information. Approximately 71% of urban public health officials never or seldom use the CDC Website, while 78% of rural respondents do not use this site. Still, the subgroup analysis of 232 health professionals reported in Table 4 showed 6.5% used the CDC site weekly or daily.
Health statistics data and Health Information Tennessee.
In 1997, the Tennessee Health Department and University of Tennessee Knoxville, Community Health Research Group (UTK CHRG) [33], launched a new Website, Health Information Tennessee (HIT), containing health status reports from all thirteen regional health councils and ninety-five counties. A component of the HIT system, Statistical Profile of Tennessee (SPOT), has been designed so users may enter a query to retrieve vital statistics, staff numbers, facilities, and other health surveys by county accompanied by maps, plots, charts, or tables. Question 4 in Table 6 shows that only 14.7% of urban and 13.7% of rural users use the HIT site at least monthly, but question 5 shows that 50.2% of urban and 47.1% of rural respondents needed or used county-level data at least monthly. Clearly, the respondents recognize the need for health statistics data to support outcomes-based community planning; however, users apparently either do not recognize a relevant specific primary source or encounter obstacles in its use. Obviously, those who do indeed use county-level health data did not access the HIT site. The HIT resource has been specifically created to fulfill the need for county data. In fact, the HIT/SPOT Website has been available since early 1997 with death and survey data sets, followed by birth data. The HIT component MapMaker, online since 1999, allows users to construct thematic maps showing data distributions on county-level maps. Question 6 in Table 6 indicates that state health statistics data are used or needed at least monthly by 42.3% of urban and 43.1% of rural respondents. Tennessee summary data are available on the HIT site, but respondents are unable to correlate their expressed need with the most relevant resource.
Published medical literature.
Question 8 in Table 6 regarding the published literature shows only 18.7% of urban and 19% of rural respondents needing or using medical information either daily or weekly (N = 571). Monthly use by 20% of urban and 17% of rural respondents is low considering the broad scope of the question (N = 571).
Question 9 in Table 6 (N = 571) shows the frequency of daily or weekly use for MEDLINE. Only 4.3% of urban and less than 3% of rural region respondents reported daily or weekly use. Over 60% of urban and rural respondents never use or need MEDLINE.
Other tools.
The survey also included open-ended questions, including one asking which tools or resources would enable respondents to work better. Respondents often indicated multiple items (N = 285). One hundred twenty-two (43%) noted they would be best served by computer or Internet access, a finding which echoes recommendations from the AMIA 2001 Spring Congress that “computers and information technology are part of public health practice, [and] computers should be on all desks” [34]. Sixty-eight respondents (23.8%) indicated they needed training in basic computer use or concepts, and thirty-four (11.9%) desired access to specific software or training in specific software. Twenty-five respondents (8%) to the question noted they needed general Internet training, and lesser percentages indicated a need for more time, assistance, books or journals, data sources, or technical support.
DISCUSSION
The data document the overarching theme of reports of the information crisis in public health: significant diversity in education, job functions, computer access, and technology skills. Also, health department staff work in diverse areas, and many (possibly a majority) do not have exclusive access to a computer with Internet access on their desktop. Of the twenty-five job categories in Table 3, fifteen show a sharing frequency above 33%. We do not know if the sharing of one computer is between two professionals or some larger number. The public health workforce is large, and most individuals are unaffiliated with institutions with a professional materials collection, either print or electronic [35]. This limited access to equipment, the Internet, information, training services, and medical literature is an overwhelming obstacle to information seeking. As mentioned previously, Tennessee has only one public health library in a health department setting and no document delivery service to health policy makers in the state health department. This lack of affiliation decreases the awareness of the wealth of electronic and print materials and isolates health professionals responsible for improving health outcomes in large populations.
In addition, because many public health professionals work in the field, in the lab, or in direct contact with patients for many hours per week, they have less opportunity for exploring the Internet. Indeed, the results indicate that the high rate of computer sharing is an obstacle and that limited time at an office desktop further complicates public health professionals' ability to conduct Internet research. Low usage of electronic resources is consistent with factors such as limited equipment, shared equipment with Internet connections, limited time during the work day for self-exploration, lack of awareness, limited access to libraries, and, perhaps most importantly, the perception that public health professionals' needs are not applicable to existing evidence-based electronic resources. One flaw in the survey is that we did not document the travel component of these professionals' job responsibilities. Travel time creates another obstacle limiting the time available for staff to learn computer skills, because the continuity of the learning process is broken into discontinuous segments.
Few resources or categories of information exceeded 50% of respondents' frequency of use or need; those that are rated most highly in terms of daily use included colleagues and internal communications such as telephone calls, memoranda, and personal conversations, all generally a part of the largely unrecorded, tacit body of knowledge that helps to comprise a professional culture.
These results bolster Lynch's assertion that “the base of information needed [in public health] goes far beyond traditional published literature and encompasses a wide range of fugitive information and information created as a by-product of organizational and institutional operations” [36]. Clearly, these respondents do not rely on a particular commercial resource or database to meet their information needs but use resources that are close at hand. Given these preliminary data, the public health community would be equally well served by altering their workflow to incorporate knowledge management principles to organize information for reuse, as well as increase use of electronic resources.
Results are derived from self-reported data, and the limitation of this approach is well recognized. The sample size is broad and is not representative in some job categories with a small number of respondents such as animal control workers, lab technicians, or health safety inspectors. However, these needs assessment data help us to understand the composition and information needs of a sampling of the Tennessee public health community. The assessment and the training sessions have laid a foundation of awareness of many information resources available to the public health community and engendered an idea of what types of resources and information behaviors would benefit public health in the library and information science community. Humphreys posits that the ability to use information services effectively depends on access to appropriate computer equipment and the Internet, awareness of available services that contain useful information, a core level of competence in the use of information technology and relevant information services, and help from experts (e.g., librarians or other information specialists) when it is needed [37]. Once an infrastructure of mutual awareness is in place, we can move toward building this “core level of competence.” Forsetlund's work with Norwegian public health physicians, however, shows the hesitation of these professionals to perceive and relate a question to published research for planning and management of public health issues. Failure to frame a question related to need will not be overcome by simply providing high-speed Internet desktop computers and raising awareness of existing electronic resources but by documenting direct applications of evidence-based knowledge to identified needs in this community.
Finally, we should not lose sight of the significance of the large budget and array of patient services managed by these professionals. According to the Tennessee budget, health department expenditures totaled $81 million in fiscal year 2001. The job responsibilities of some of the professionals who responded to this survey include management of: (1) patient care services for more than 820,000 Tennesseans in eighty-nine rural county health departments and six metro health departments, (2) multiple vendor contracts in the range of $100,000 to $500,000 each, and (3) program effectiveness. Yet, these management professionals share desktop computers and Internet access with an unknown number of coworkers. What other private company, nonprofit organization, or academic medical center would entrust such responsibilities to employees without the infrastructure to support communication and decision making?
FUTURE RESEARCH
While the results presented in this initial paper are frequency data, we are in the process of analyzing levels of self-reported knowledge of electronic resources indicated in pretest, posttest, and six-months after the survey evaluations for statistical significance to determine the value of group training. Most importantly, the EBL continues to collaborate with the Tennessee public health workforce. This initial project focuses mainly on raising awareness and documenting use through a broad needs assessment that both provides data for developing the training component of the project and has introduced, however passively, survey recipients to a variety of resources. Details of the training program and the use of resources afterward will be reported in subsequent papers. A single training session cannot instill knowledge of resources, and class participants quickly forget how to use resources unless they employ them frequently. To articulate a model to overcome this problem of knowledge fade as well as a model for building core competence atop an infrastructure of awareness, the EBL has embarked on a contract extension to experiment with developing inhouse information expertise, as opposed to broad awareness, in the public health community.
Note: Since the initial survey was conducted in 1999, changes have significantly improved Tennessee public health workers' accessibility to information resources. Every county health department has the capacity to support at least five computers with Internet access. Virtually all public health workers have email accounts. Satellite dishes have been installed at every regional health office and at the central office to facilitate satellite training.
Acknowledgments
We gratefully acknowledge The National Library of Medicine, National Network of Libraries of Medicine Southeastern/Atlantic Region for support and the Training Partners for Tennessee Public Health collaborators, especially Bart Perkey, Becky Hawks, Wendy Long, Fredia Wadley, and Judy Dias for their advice and assistance. We also acknowledge considerable support from Annette Williams, Taneya Koonce, and Rebecca Jerome in the preparation of this manuscript.
APPENDIX
Needs assessment questionnaire
Footnotes
* National Library of Medicine contract number N01-LM-6-3522 administered by the University of Maryland, Baltimore.
Contributor Information
Patricia Lee, Email: patricia.lee@vanderbilt.edu.
Nunzia B. Giuse, Email: nunzia.giuse@vanderbilt.edu.
Nila A. Sathe, Email: nila.a.sathe@vanderbilt.edu.
REFERENCES
- Yasnoff WA, O'Carroll PW, Koo D, Linkins RW, and Kilbourne EM. Public health informatics: improving and transforming public health in the Information Age. J Public Health Management Practice. 2000 Nov; 6(6):67–75. [DOI] [PubMed] [Google Scholar]
- Committee for the Study of the Future of Public Health, Division of Health Care Services, Institute of Medicine. The future of public health. Washington, DC: National Academy Press, 1988. [Google Scholar]
- Lasker RD, Humphreys BL, and Braithwaite WR. Making a powerful connection: the health of the public and the national information infrastructure. Washington, DC: Public Health Service, U.S. Department of Health and Human Services, 1995. [Google Scholar]
- Information for health: a strategy for building the national health information infrastructure. [Web document]. Washington, DC: The National Committee on Vital and Health Statistics, 15 Nov 2001. [cited 10 Feb 2003]. <http://ncvhs.hhs.gov/nhiilayo.pdf>. [Google Scholar]
- Yasnoff WA, Overhage JM, Humphreys BL, and LaVenture M. A national agenda for public health informatics: summarized recommendations from the 2001 AMIA Spring Congress. J Am Med Inform Assoc. 2001 Nov–Dec; 8(6):535–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Assuring the Health of the Public in the 21st Century, Institute of Medicine. The future of the public's health in the 21st century. [Web Document]. Washington, DC: The National Academies Press, 2002. [cited 10 Jan 2003]. <http://www.nap.edu/books/0309086221/html/>. [Google Scholar]
- Yasnoff . 2000. op. cit., 67. [Google Scholar]
- Tang PC. AMIA advocates national health information system in fight against national health threats. J Am Med Inform Assoc. 2002 Mar–Apr; 9(2):123–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullet M, Rawding N, Brown CK, Custer D, and Suen J. Descriptive epidemiology of local public health systems. Am J Prev Med. 1995 Nov–Dec; 11(6 Suppl):9–16. [PubMed] [Google Scholar]
- Rambo N, Dunham P. Information needs and uses of the public health workforce. Washington 1997–1998. Morb Mortal Wkly Rep. 2000 Feb 18; 49(6):118–120. [PubMed] [Google Scholar]
- Rambo N, Dunham P. Information needs and uses of the public health workforce. Washington 1997–1998. Morb Mortal Wkly Rep. 2000 Feb 18; 49(6):119. [PubMed] [Google Scholar]
- O'Carroll PW, Cahn MA, Auston L, and Selden CR. Information needs in public health and health policy: results of recent studies. J Urban Health. 1998 Dec; 75(4):785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenan J, Townsend W. Partners in Information Access for Public Health Professionals—the Nevada experience. Paper presented at: MLA 2000, 100th Medical Association Annual Meeting; Vancouver, BC; 2000. [Google Scholar]
- Zenan JS, Rambo N, Burroughs CM, Alpi KM, Cahn MA, and Rankin J. Public Health Outreach Forum: report. Bull Med Libr Assoc. 2001 Oct; 89(4):400–3. [PMC free article] [PubMed] [Google Scholar]
- Rambo N, Zenan JS, Alpi KM, Burroughs CM, Cahn MA, and Rankin J. Public Health Outreach Forum: lessons learned. Bull Med Libr Assoc. 2001 Oct; 89(4):403–6. [PMC free article] [PubMed] [Google Scholar]
- Yasnoff . 2001. op. cit., 538. [Google Scholar]
- Humphreys BL. Meeting information needs in health policy and public health: priorities for the National Library of Medicine and the National Network of Libraries of Medicine. J Urban Health. 1998 Dec; 75(4):878–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys BL. Meeting information needs in health policy and public health: priorities for the National Library of Medicine and the National Network of Libraries of Medicine. J Urban Health. 1998 Dec; 75(4):878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander SM, Martin ER. Public health professionals in the Midwest: a profile of connectivity and information technology skills. Bull Med Libr Assoc. 1999 Jul; 87(3):329–36. [PMC free article] [PubMed] [Google Scholar]
- National Association of City and County Health Officials. Information technology capacity and local public health agencies. Res Brief 1999;4:1–2. [Google Scholar]
- Gale J. A profile and training needs assessment of community/public health professionals in Washington State. Northwest Center for Public Health Practice: School of Public Health and Community Medicine, University of Washington, 1998:1–30. [Google Scholar]
- O'Carroll . op. cit., 788. [Google Scholar]
- Rambo . 2000. op. cit., 118. [Google Scholar]
- Chambers LW, Haynes RB, Pickering R, McKibbon A, Walker-Dilks CJ, Panton L, and Goldblatt E. New approaches to addressing information needs in local public health agencies. Can J Public Health. 1991 Mar–Apr; 82(2):109–14. [PubMed] [Google Scholar]
- Forsetlund L, Bjorndal A. The potential for research-based information in public health: identifying unrecognised information needs. [Web document]. BMC Public Health 2001;1:1. [cited 14 Apr 2002]. <http://www.biomedcentral.com/1471–2458/1/1/>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsetlund L, Bjorndal A. The potential for research-based information in public health: identifying unrecognised information needs. [Web document]. BMC Public Health 2001;1:1. [cited 14 Apr 2002]. <http://www.biomedcentral.com/1471–2458/1/1/>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton LJ, Hasson S, Ross FV, and Martin ER. Outreach to public health professionals: lessons learned from a collaborative Iowa public health project. Bull Med Libr Assoc. 2000 Apr; 88(2):165–71. [PMC free article] [PubMed] [Google Scholar]
- Curtis J, Bedard M, Hayes B, Rondon S, and Schell M. Information services in a natural disaster: customized public health information before, during, and after hurricane Floyd. Paper presented at: MLA 2000, 100th Medical Library Association Annual Meeting; Vancouver, BC; 2000. [Google Scholar]
- Zenan . 2000. op. cit. [Google Scholar]
- Lee P, Sathe NA, Lynch F, Martin S, and Giuse NG. The role of collaborative partnerships in a public health outreach program. Paper presented at: MLA 2000, 100th Medical Library Association Annual Meeting; Vancouver, BC; 2000. [Google Scholar]
- Rambo N. Information resources for public health practice. J Urban Health. 1998 Dec; 75(4):807–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rambo N. Information resources for public health practice. J Urban Health. 1998 Dec; 75(4):816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennessee Department of Health, University of Tennessee Community Health Research Group. HIT: health information Tennessee. [Web document]. Knoxville, TN: The Group. [cited 10 Apr 2001]. <http://hitspot.utk.edu>. [Google Scholar]
- Yasnoff . 2001. op. cit., 538. [Google Scholar]
- O'Carroll . op. cit. [Google Scholar]
- Lynch C. The retrieval problem for health policy and public health: knowledge bases and search engines. J Urban Health. 1998 Dec; 75(4):794–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys . op. cit., 882. [Google Scholar]