Abstract
Objective: To establish a time profile to determine how athletic training students use their time in clinical placements and to determine the effects of academic standing, sex, sport type, and risk of injury associated with a sport during athletic training students' clinical placements on instructional, clinical, unengaged, managerial, and active learning time.
Design and Setting: Subjects were enrolled in clinical placements within National Collegiate Athletic Association Division I athletics, intramural sports, and a local high school. Students were individually videotaped for approximately 4 hours.
Subjects: A total of 20 undergraduate athletic training students (17 women, 3 men) from a Committee on Accreditation of Allied Health Education Programs (CAAHEP)-accredited athletic training education program.
Measurements: We created a conceptual behavioral time framework to examine athletic training students' use of clinical-placement time with the performance domains associated with the 1999 National Athletic Trainers' Association Board of Certification Role Delineation Study. Students' use of time was analyzed with the Behavior Evaluation Strategies and Taxonomies software.
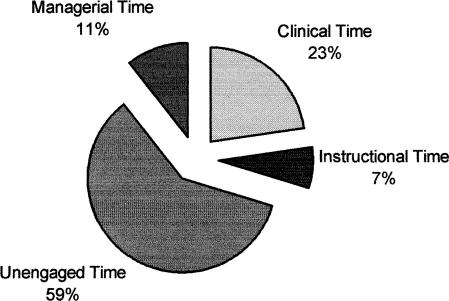
Results: Students spent 7% of their overall clinical-placement time in instructional activities, 23% in clinical activities, 10% in managerial activities, and 59% in unengaged activities. Using multiple 3 × 3 factorial analyses of variance, we found that advanced students were engaged in significantly more active learning and clinical time compared with novice and intermediate students. Students assigned to sports in which injuries predominately occur in the upper extremities (upper extremity sports) spent significantly more clinical-placement time unengaged compared with students assigned to sports in which injuries predominantly occur in the lower extremities (lower extremity sports) or in both upper and lower extremities (mixed extremity sports).
Conclusions: In this exploratory study, we examined only the clinical-placement component of 1 athletic training program; therefore, it may not be accurate to generalize the results for all CAAHEP-accredited programs. However, these results can be used by athletic training educators to examine the amount of time students are actually engaged in specific domains of athletic training, to determine the domains in which skills are most commonly being performed, to identify the relationships between the students and clinical instructors or supervisors, and to develop clinical placements in which students learn and practice clinical and educational competencies.
Keywords: engaged time, clinical behaviors, active learning time
Athletic training students spend many hours in the clinical setting working with a variety of patient populations in an attempt to learn the skills necessary to become competent certified athletic trainers. Competence, however, does not occur overnight; rather, “competence is attained only after a series of learning experiences that may take months or years to complete before a learner has developed a satisfactory degree of attainment in the field.”1 Competence, whether it occurs in the classroom or in the clinical placement, requires that students be provided with adequate time to learn and that this time be used constructively.1
Over the last 50 years, numerous authors have examined the effects of time on learning in a variety of educational settings. The foci of these studies vary, with most of the research dealing with the relationship of length of education time to student achievement,2 the effects of class size and availability of equipment on time engagement in motor-appropriate skills,3 allocation and utilization of the school day,4,5 and time engaged in on-task behaviors and academic learning.2,4,6,7 For example, in physical education, researchers found students spent approximately 20% to 30% of their time waiting for active classroom engagement and 15% to 20% of their time engaged in management activities.6,8 In elementary education, researchers found that of the approximately 6 hours allocated to classroom instruction, students spent only 32% to 38% of this time engaged in active learning.9,10 Although the methodologic approaches varied among these studies, one common denominator is the suggestion that a relationship exists between engaged time and achievement and between academic learning time and achievement.2
If a relationship between engaged time and achievement exists, as suggested by Aronson et al,2 then the more time (hours) allocated to athletic training students in clinical placements, the more they should learn. Some allied health care educators challenge this notion that simply increasing the overall amount time spent in clinical placements increases a student's competence level.11,12 Simply lengthening the time spent in clinical placements to provide more opportunity for learning is not the answer.13,14 Students participating in clinical placements and even in the classroom must be provided with a foundation that allows them to be focused and engaged in skills and behaviors relevant to their academic level and cognitive or psychomotor ability.6 Clinical placements that provide clear cognitive and psychomotor objectives (identified in a clinical placement or practicum syllabus), adequate clinical supervision and instruction, and the opportunity for students to practice skills and behaviors relevant to their ability are more effective for learning and may be accomplished in a shorter period of time.13,14 However, if inadequate time allocation was the major cause of lower student achievement in the first place, then increasing opportunity or allocated time may enhance learning after all.4
Unlike traditional educational settings and other allied health care professions that have made a conscious effort to study the relationship between time and learning (eg, physical therapy and nursing), research examining the use of clinical-placement time by athletic training students is not well represented in the literature. It is imperative that athletic training educators begin to take the initial steps to disaggregate clinical-placement time to determine whether students are engaging in activities related to learning, academic achievement, and the development of professional competence. Therefore, our purpose was twofold: first, to establish a time profile to determine how athletic training students used their time in performing specific skills, tasks, and behaviors related to athletic training; and second, to determine the effects of student academic standing, sex, sport type, and risk of injury with respect to the use of clinical-placement time according to the dependent variables of instructional time, clinical time, unengaged time, managerial time, and active learning time.
METHODS
Subjects
Twenty subjects (17 women, 3 men) enrolled in a Commission on Accreditation of Allied Health Education Programs (CAAHEP)-accredited undergraduate athletic training education program located in the midwestern United States volunteered to participate in the study. The subjects were divided into 3 groups according to their academic level: sophomore (novice), junior (intermediate), and senior (advanced). Subjects were orally informed of the study's procedures and guidelines and signed an institutionally approved consent form before the videotaping. The institutional review board approved the study.
Videographers
Two student employees were hired by the investigators to videotape the subjects while they were engaged in their clinical placement. The videographers were provided with a Sony CCD-TRV57 8-mm video camcorder (New York, NY) and Memorex MP 120 8-mm videotapes (Santa Fe Springs, CA). Two training sessions were held to acclimate the videographers to the video equipment and videotaping procedures. After the second training session, each videographer participated in a mock videotaping trial session at one of the approved clinical-affiliation sites used in the study with a student volunteer who was excluded from the study sample. To control for Hawthorne effects, the viodegrapher was instructed to remain 6 to 8 feet (1.83 to 2.44 m) away from the students at all times and to not interfere with the clinical placement.
Procedures
Before the videotaping, we obtained permission from the site coordinator or administrator at each participating clinical affiliation. The subjects, investigators, and videographers then met to establish dates, times, and locations for videotaping each subject. The average length of a regular clinical-placement day was 4 hours. Therefore, to accurately capture the subjects' clinical-placement experience (eg, football, volleyball, field hockey, swimming, ice hockey, wrestling, etc), subjects were scheduled for 4 hours of videotaping 1 month into the fall academic quarter.
All observations were conducted during regular athletic practice sessions. Game-day preparation and postgame-day practices were not videotaped. Once the videotaping was completed, the videos were labeled with the subject's code number, clinical-placement location, date, and time. All tapes were locked in an investigator's office until all of the data were ready for analysis.
Behavioral Analysis Framework
Using Murphy's15 model for examining or profiling time in schools and information from the American Association of School Administrators,16 we created a conceptual behavioral time framework to examine athletic training students' use of clinical-placement time. A review of literature on academic learning time identified the remaining components necessary for completing the time-profiling framework. The National Athletic Trainers' Association Board of Certification (NATABOC) 1999 role delineation of performance domains and essential tasks was included in the time framework to construct a model representing the use of time during clinical placements.17 This time-profiling framework included the following time categories: instructional time, clinical time, unengaged time, and managerial time.
Instructional time is defined as the amount of time subjects perform behaviors associated with didactic, practical, or observational learning with either a clinical instructor or supervisor (CIS) or peer. Clinical time is the total amount of time subjects perform clinical skills and behaviors associated with athletic training defined by the NATABOC's 1999 role delineation.17 Combining instructional time and clinical time yields the variable of active learning time, which represents the overall amount of time subjects are engaged in learning athletic training skills and behaviors. Unengaged time is the amount of time subjects spend performing behaviors seemingly unrelated to athletic training that appear to offer no apparent educational or clinical value, such as waiting, bathroom breaks, and social behaviors (eg, discussing events outside of athletic training, performing tasks unrelated to athletic training). Managerial time is the time subjects spend engaged in activities related to the day-to-day operational organization and administration (eg, record keeping, restocking taping tables) of their clinical placement.
We analyzed the videotapes using the Behavior Evaluation Strategies and Taxonomies (BEST) software package (version 3.0 Sage Publications Inc, Thousands Oaks, CA), which facilitates the real-time collection and analysis of observational category data. BEST consists of 2 parts: 1 for data collection and 1 for data analysis. The software program allows for the recording of start and stop times of mutually exclusive or overlapping events in real time using predefined keys on a laptop keyboard.
The videotapes were viewed, and all the observed clinical skills and behaviors for each subject were entered into the software application. All skills and behaviors were recorded in seconds and later converted to minutes for analysis. Before analyzing the data, intrarater reliability of the data was calculated. The project director, who had experience with observational recordings and interpretation of clinical and educational data, analyzed the videotapes to ensure that the coding of the skills or behaviors of the students was consistent. The principal investigator (M.G.M.) observed 3 separate 10-minute video segments of the videographers' mock training session and calculated the frequency and duration of times of the clinical skills and behaviors. He then reviewed the segments again and compared the results until a 90% agreement between trials was recorded.
Statistical Analysis
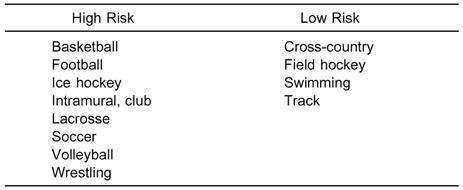
We calculated means and standard deviations for each of the framework's behavioral time categories and subcategories. Five 3 × 3 factorial analyses of variance (ANOVAs) were computed to compare the independent variables of academic standing (novice, intermediate, and advanced) and clinical placement (Table 1) with respect to the dependent variables of instructional time, clinical time, unengaged time, managerial time, and active learning time. A post hoc test with a Bonferroni critical-value procedure was used to determine significant differences within the independent variables. Independent t tests were also performed to compare the mean differences between sex and sport risk (Table 2) with respect to the dependent variables. All statistical testing was 2 tailed, and the level of statistical significance was set at P < .05. We used the Statistical Package for Social Sciences (version 10.0, SPSS Inc, Chicago, IL) to calculate the statistics.
Table 1. Clinical Placements
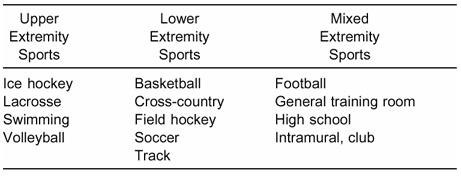
Table 2. Classification of Risk of Sport
RESULTS
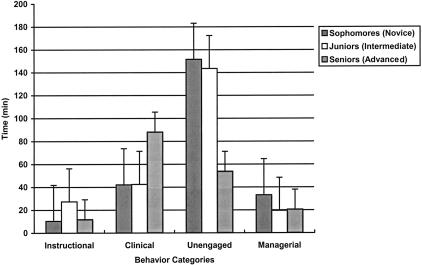
Factorial ANOVAs revealed significant differences among the levels of academic standing with respect to active learning time (F2,17 = 7.07, P < .05) and clinical time (F2,17 = 4.88, P < .05) (Tables 3 and 4, Figures 1 and 2). Using the Bonferroni critical-value procedure, we determined that advanced students spent significantly more time engaged in active learning compared with novice students (100.00 ± 28.48 minutes versus 52.60 ± 15.73 minutes) and that advanced students also spent significantly more time engaged in clinical time (88.15 ± 34.16 minutes) than intermediate (42.50 ± 24.12 minutes) and novice students (41.18 ± 12.15 minutes).
Table 3. Subject Characteristics and Clinical-Placement Hours

Table 4. Clinical-Placement–Behavior Time Categories*
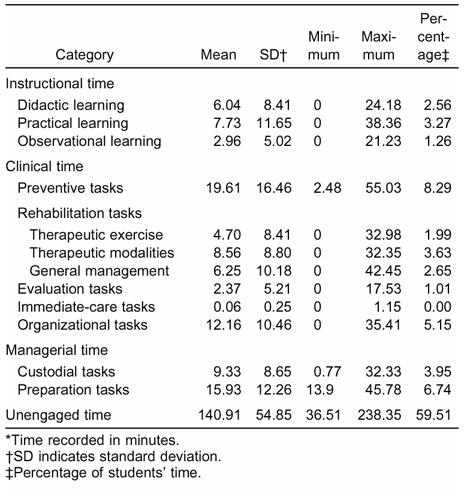
Figure 1.
Overall percentages of time spent by students in the 4 time (behavioral) categories.
Figure 2.
Time spent in each behavior category by academic level. The lower the student's academic standing, the more time spent in unengaged and managerial categories.
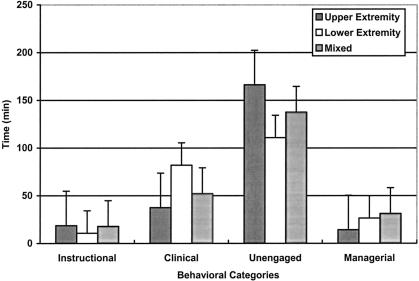
A factorial ANOVA revealed significant differences among the clinical placements with respect to unengaged time (F2,17 = 6.61, P < .05) (Figure 3). With the Bonferroni critical-value procedure, we found that students assigned to clinical placements in upper extremity sports spent significantly more time unengaged (166.33 ± 8.95 minutes) compared with students assigned to lower extremity sports (110.90 ± 28.76 minutes) and mixed extremity sports (137.68 ± 22.13 minutes). Independent t tests revealed no significant difference between sex and sport risk with respect to the dependent variables.
Figure 3.
Time spent in each category by clinical assignment. Students in upper extremity clinical placements spent more time in unengaged activities compared with students in lower extremity or mixed clinical placements.
DISCUSSION
Athletic training educators generally agree that exposing students to quality clinical placements is as important as providing them with appropriate classroom instruction. The challenge for contemporary educators is to optimize the productivity of the clinical placement to ensure the learning and comprehension of educational and clinical competencies rather than the mere application of skills and behaviors.18,19 However, most of the research examining clinical placements in other allied health care professions has been conducted qualitatively, providing narrative themes of how students viewed their clinical-placement experiences rather than providing quantitative data that identify how students actually used their time during clinical placements. Our study is the first known attempt to establish a time-profiling technique to examine students' use of clinical-placement time and to analyze the behaviors quantitatively.
Clinical Behaviors
Allied health care educators have used quantitative variables to predict examination-performance success. These quantitative variables are usually the accumulation of hours instead of the analysis of clinical skills and behaviors. In one such study,20 the passing rate was higher for athletic training students earning approximately 400 clinical-placement hours above the required 800 hours compared with those meeting the minimal requirements and those surpassing 1200 clinical-placement hours. Battersby and Hemmings12 found that nursing students who accumulated a high number of clinical-placement hours did not differ significantly in competency or clinical-performance levels compared with students accumulating a low number of clinical-placement hours. Thus, accumulating more or fewer hours than required does not necessarily improve examination performance, and the types of skills and behaviors performed by students during clinical placements should be the main emphasis of educational programs instead of hour accumulation.
Frequently, athletic training students count hours that address no apparent athletic training educational skill or behavior. Students are often scheduled to arrive 1 hour before athletic practice and remain 1 hour after the completion of practice. Additionally, athletic training students are engaged in tasks, such as cleaning and restocking, that are not necessarily geared toward any specific competency achievement. These unengaged and managerial tasks of clinical placements might produce students who lack the cognitive and psychomotor skills necessary for the development of a competent professional. Because unengaged or managerial tasks are part of the clinical placement, students may be accumulating experiences that are not necessarily geared for the successful development of educational or clinical-skill acquisition.
We found that approximately 59% of the athletic training students' clinical-placement time was spent in unengaged activities, such as socialization (discussions or activities not related to athletic training clinical skills or behaviors), waiting, and moving between practice facilities. If this trend continued over the course of the student's clinical placement, less than 50% of his or her time would actually be engaged in activities related to athletic training skills and behaviors. Therefore, only a fraction of the time provided to students is used to cultivate and refine their cognitive, psychomotor, and affective competencies. Simply requiring students to meet a minimum number of clinical-placement hours does not ensure clinical competence and learning over time, especially if these earned hours are spent in unengaged activities. For this reason, the NATABOC is eliminating the hour requirement in favor of more emphasis on the quality and completion of clinical proficiencies during clinical placements and embracing the National Athletic Trainers' Association Education Committee's concept of learning over time.
As a result, athletic training educators need to determine if the remaining 37% of the earned clinical-placement hours (59% unengaged time + 3.9% managerial time [custodial domain specifically] = 62.9%) are adequate for professional and academic success. If not, how does the profession encourage quality clinical-placement experiences? Future research should investigate educational and clinical practices and interventions that facilitate an increase in the amount of time students are engaged in clinical skills and activities conducive for successful academic and clinical learning and achievement.
Clinical Placements
Research examining other allied health care professions has shown that the time offered to students during clinical placements is often used ineffectively.21,22 This poor use of time is most likely reflected by several factors, such as the increase in faculty workload both in the classroom and in the clinical setting,23 time spent writing formal assessments rather than directly interacting with students,22 lack of available or adequate equipment and facilities,18,24 overcrowding in the clinical setting,18,25 and decreased availability of quality CISs.11,22–24 These factors tend to expose students to clinical placements devoid of critical feedback, active learning, and patient and injury variety and to provide inadequate clinical supervision and instruction. Differences in clinical placements may occur among National Collegiate Athletic Association athletic levels and traditional versus nontraditional settings; however, due to our small sample size, this point is beyond the scope of this study.
Foster and Leslie26 found that athletic training clinical supervisors spent less than half of their time teaching students in the clinical setting. We found that only 7% of our subjects' clinical-placement time was spent in instructional activities with the CIS or peers. This limited time spent in instructional activities may be the result of CISs who are not professionally prepared to teach clinically or are unsure of the proper means to mentor students. In some instances when instruction does occur in the clinical setting, it is influenced by the strengths and weaknesses of the CIS.11 Additionally, demands placed upon the CIS to care for athletes and patients may limit time interactions with his or her students, ultimately affecting the amount of time available to instruct, monitor, test, correct, and retest students' competency levels. This problem not only plagues athletic training but also other allied health care professions. Polifroni et al22 found that 75% of nursing students' clinical-placement time was unsupervised, reflecting the need for more clinical supervision and instructional opportunities between the supervisor and the student.
The fact that students in our study spent so little time with their CIS was astonishing. Students, particularly those at the lower levels, require more guidance and encouragement to gain confidences in their skills. They also need constructive feedback to ensure that they are “on task” and properly performing athletic training clinical competencies within their ability level. An experienced CIS who is willing to recognize individual learning styles and who possesses good clinical skills sets aside time to work with the students and knows that reflecting on the students' experiences may help to facilitate a better learning environment. Harris and Naylor23 found that when clinical supervisors provided direct feedback, instructional activities, and appropriate daily structure, the quality of the clinical placement increased and led to independent student learning and autonomy.
Without proper clinical-placement guidance and structure, students may enter the workforce ill prepared to perform adequately. To increase clinical-placement effectiveness, CISs should schedule time with their students to perform clinical proficiencies and allow more opportunities for students to interact with athletes and patients to practice these proficiencies. Decreasing the number of students assigned to an individual, decreasing some of the job responsibilities of the CIS, and increasing the number of CISs are other suggestions to increase student-CIS interaction time. However, with the introduction of the approved clinical instructor (ACI), students should have more opportunity to interact with their CIS to assess clinical and educational proficiencies and increase their contact time. Follow-up studies should be conducted to determine whether this is actually occurring.
Academic Standing
Students' academic standing or their initial exposure to the clinical placement may influence how they react or perform during their clinical placement.27,28 We found that advanced students spent 41% of their time engaged in active learning compared with intermediate (32%) and novice students (22%). Additionally, advanced students spent 36% of their time engaged in clinical tasks compared with intermediate (18%) and novice students (17%). Novice athletic training students, similar to the novice nursing students studied by Neill et al,27 are sometimes unsure of the roles they are expected to play and withdraw from active participation to become passive observers. This withdrawal may be a result of differences between expected and actual roles, or it may be part of the normal cognitive development.27 As students begin to develop a certain level of autonomy and confidence and become familiar with their roles, they can move from passive observers to active participants during clinical placements.27 This transition enables novice students to effectively engage in learning activities and promotes professional development.
Type of Sport
When examining the types of sports associated with clinical placements, we found that students assigned to upper extremity sports spent significantly more time unengaged compared with students assigned to lower extremity sports or in mixed extremity sports. Students assigned to upper extremity sports spent 70% of their time in unengaged activities and only 23% in active learning. In comparison, students assigned to lower extremity sports spent 48% and 40% of their time in unengaged activities and active learning, respectively, while students assigned to mixed extremity sports spent 57% of their time unengaged and 29% in active learning. These differences may be based on the CIS' clinical emphasis or a student's comfort level with the anatomical structures of the lower extremity versus the upper extremity. Other possible reasons include (1) increased exposure to lower extremity injuries, (2) season in which different sports are played (more lower extremity sports were in season), (3) classification of sports as upper, lower, or mixed extremity sport, (4) time of year when the observations were made, and (5) the clinical-engagement opportunities of students provided by the CIS.
These differences in the amount of time students are engaged in active learning support the idea that variations in students' clinical placements are necessary to ensure adequate clinical learning and competency achievement. Assigning students to a variety of clinical-placement settings allows them to interact and practice techniques learned in class with a diverse population and with a different CIS. The challenge for the CIS is to understand how each student learns by identifying his or her learning style and attempting to make a conscious effort to develop and implement teaching and clinical strategies and evaluate students based on their learning preference.29 Therefore, rotating students through different clinical-placement settings and clinical supervisors may be more effective in increasing the amount of time students spend engaged in active learning and decreasing the overall amount of unengaged time. In addition, these rotations might expose students to sports in which more injuries or certain types of injuries occur, thereby increasing active learning.
Limitations/Recommendations
Limitations of the present study include a relatively small sample size, sex biases, and a limited number of direct observation hours of the athletic training students. We also want to stress that the study is exploratory in nature and relevant only to the particular institution in question. In addition, the dynamics of this particular athletic training program may make it difficult to generalize to other accredited athletic training programs. However, unless substantial training is conducted to ensure consistency and reliability in the measurement of student clinical-placement time, direct determination of significant meaning using the quantitative measures used in this study is not readily feasible. Our findings and recommendations are intended to highlight aspects of student clinical placements and the need for athletic training educators to assess their students' use of clinical time relative to the activities occurring during clinical placements.
Another variable to consider is the likelihood that all the subjects were not performing their regular or normal daily activities while being videotaped. To control for Hawthorne effects,30 the subjects were made aware of the nature and importance of the study and encouraged to engage in their normal daily routines while being videotaped. In addition, the videographers attempted to remain at least 6 to 8 feet away from the subjects while videotaping, taking care not to interfere with the normal routine of the subject or the clinical-placement setting. Upon observation and recording of the data, the project director only noticed differences in behaviors during off-task time when several students made comments directly to the camera, and thus, these behaviors should not have affected the outcome. Therefore, to limit Hawthorne effects, we suggest videotaping students for several sessions so they become acclimated to the camera.
We recommend conducting a nationwide survey of a larger sample size to determine students' perception of time spent engaged in the clinical placements and then using this information to guide educators to enhance students' clinical placements. We also recommend conducting a study with students matched by sex and setting and videotaping students in various clinical-placement environments and athletic seasons to determine if these variables produce differences in clinical skills, activities, and behaviors. Additionally, athletic training educators should examine the amount of time CISs are actively engaged in clinical instruction with athletic training students during the clinical-field placements. Finally, we recommend that athletic training educators examine the relationship between the amount of time spent by students engaged in active learning during their clinical placement and success on the NATABOC certification exam.
CONCLUSIONS
The question athletic training educators and other professionals need to ask is, “How much time is enough time for students to develop adequate skills to become competent allied health care providers?” Although we only examined 79 hours of student clinical placements, the results clearly indicate that most of their time was spent in unengaged activities. As educators, identifying how students' time is managed is undoubtedly the first step in developing clinical placements that will maximize student learning and promote professional development. Examining the use of clinical-placement time may allow educators to address work-force issues, competency achievement, quality of clinical hours, and clinical instructors' and supervisors' management of students' use of time. In addition, videotapes of athletic training students in the clinical setting can become part of a portfolio assessment to provide students with constructive feedback of their clinical skills. The student and the clinical instructor can review the videotapes periodically to determine the level of skill acquisition and proficiency achievement.
Acknowledgments
ACKNOWLEDGMENTS
This research was supported by the College of Health and Human Services, Ohio University, Athens, Ohio, Scholarly Activity Grant.
REFERENCES
- Bloom B S. Time and learning. Am Psychol. 1974;29:682–688. [Google Scholar]
- Aronson J, Zimmerman J, Carlos L. Improving Student Achievement by Extending School: Is it Just a Matter of Time? Office of Educational Research and Improvement; San Francisco, CA: 1999. (ERIC no. 435 082; report no. EA 030 111) [Google Scholar]
- Hastie P A, Saunders J E. Effects of class size and equipment availability on student involvement in physical education. J Exp Educ. 1991;59:212–223. [Google Scholar]
- Karweit N. Time-on-task reconsidered: synthesis of research on time and learning. Educ Leadership. 1984;41:32–35. [Google Scholar]
- Lindsay P. The effect of high school size on student participation, satisfaction, and attendance. Educ Eval Policy Ann. 1976;4:422–434. [Google Scholar]
- Beauchamp L, Darst P W, Thompson L P. Academic learning time as an indication of quality of high school physical education. J Phys Educ Rec Dance. 1990;61:92–95. [Google Scholar]
- Walther M, Beare P. The effect of videotape feedback on the on-task behavior of a student with emotional/behavioral disorders. Educ Treat Child. 1991;14:53–60. [Google Scholar]
- Siedentop D. Developing Teaching Skills in Physical Education. 3rd ed Mayfield Publishing Co; Mountain View, CA: 1991. [Google Scholar]
- Rich H L, McNeils M J. A study of academic time-on-task in the elementary school. Educ Res Q. 1988;12:37–45. [Google Scholar]
- Karweit N. Should we lengthen the school term? Educ Researcher. 1985;14:9–15. [Google Scholar]
- Weidner T G, August J A. The athletic therapist as clinical instructor. Athl Ther Today. 1997;2:49–52. [Google Scholar]
- Battersby D, Hemmings L. Clinical performance of university nursing graduates. Aust J Adv Nurs. 1991;9:30–34. [PubMed] [Google Scholar]
- Redfern L. Check the quality not the length. Nurs Times. 1999;95:22. [PubMed] [Google Scholar]
- Strickland J W, Siemsen D W, Weber R C. Increasing the quantity of the clinical education experience. Optomet Educ. 1996;22:22–28. [Google Scholar]
- Murphy J. Instructional leadership: focus on time to learn. Natl Assoc Second School Principals Bull. 1992;76:19–26. [Google Scholar]
- American Association of School Administrators . Time on Task: Using Instructional Time More Effectively. American Association of School Administrators; Arlington, VA: 1982. [Google Scholar]
- Columbia Assessment Services . National Athletic Trainers' Association Board of Certification Role Delineation Study. 4th ed Columbia Assessment Services; Morrisville, MO: 1999. [Google Scholar]
- Nolan C A. Learning on clinical placement: the experience of six Australian student nurses. Nurse Educ Today. 1998;18:622–629. doi: 10.1016/s0260-6917(98)80059-2. [DOI] [PubMed] [Google Scholar]
- Taylor K L, Care W D. Nursing education as cognitive apprenticeship: a framework for clinical education. Nurse Educ. 1999;24:31–36. doi: 10.1097/00006223-199907000-00018. [DOI] [PubMed] [Google Scholar]
- Sammarone Turocy P, Comfort R E, Perrin D H, Gieck J H. Clinical experiences are not predictive of outcomes on the NATABOC examination. J Athl Train. 2000;35:70–75. [PMC free article] [PubMed] [Google Scholar]
- Ashworth P, Morrison P. Some ambiguities of the student's role in undergraduate nurse training. J Adv Nurs. 1989;14:1009–1015. doi: 10.1111/j.1365-2648.1989.tb01511.x. [DOI] [PubMed] [Google Scholar]
- Polifroni E C, Packard S A, Shah H S, MacAvoy S. Activities and interactions of baccalaureate nursing students in clinical practice. J Prof Nurs. 1995;11:161–169. doi: 10.1016/s8755-7223(95)80115-4. [DOI] [PubMed] [Google Scholar]
- Harris D, Naylor S. Case study: learner physiotherapists' perceptions of clinical education. Educ Training Tech Intl. 1992;29:124–131. [Google Scholar]
- Trevitt C. Clinical experience in undergraduate education: issues and challenges. Contemp Nurse. 1999;8:270. doi: 10.5172/conu.1999.8.1.270. [DOI] [PubMed] [Google Scholar]
- Dean-Baar S. Preparing the next generation of nurses. Rehabil Nurs. 1999;24:46. doi: 10.1002/j.2048-7940.1999.tb01834.x. [DOI] [PubMed] [Google Scholar]
- Foster D, Leslie D. Clinical teaching roles of athletic trainers. J Athl Train. 1992;27:298–302. [PMC free article] [PubMed] [Google Scholar]
- Neill K M, McCoy A K, Parry C B, Cohran J, Curtis J C, Ransom R B. The clinical experience of novice nursing students. Nurse Educ. 1998;23:16–21. doi: 10.1097/00006223-199807000-00008. [DOI] [PubMed] [Google Scholar]
- Wilkinson C, Peters L, Mitchell K, Irwin T, McCorrie K, MacLeod M. “Being there”: learning through active participation. Nurse Educ Today. 1998;18:226–230. doi: 10.1016/s0260-6917(98)80083-x. [DOI] [PubMed] [Google Scholar]
- National Athletic Trainers' Association . National Athletic Trainers' Association; Dallas, TX: 2001. Clinical Instructor Educator Seminar Handbook. [Google Scholar]
- Light R J, Singer J D, Willett J B. By Design: Planning Research in Higher Education. Harvard University Press; Cambridge, MA: 1990. p. 149. [Google Scholar]