Abstract
Objective: To determine the helpfulness of clinical-education–setting standards in the professional preparation of entry-level certified athletic trainers.
Design and Setting: We developed a 22-item questionnaire based on the 12 standards presented by Weidner and Laurent. Subjects used a Likert scale (0 = no help, 5 = very helpful) to indicate their perceptions of the helpfulness of each standard in preparing them for their roles and responsibilities as certified athletic trainers.
Subjects: We surveyed employed, entry-level certified athletic trainers who recently completed Commission on Accreditation of Allied Health Education Programs-accredited athletic training education programs.
Measurements: Percentage means were computed for the helpfulness ratings of each standard. A percentage mean was computed for the overall contribution of clinical education to professional development. Chi-square analyses were used to assess the differences in helpfulness ratings among respondents.
Results: The overall mean score across all standards was 4.17. No significant differences in the helpfulness ratings of any of the respondents were noted regardless of sex, ethnicity, number of clinical-education hours, total semesters of clinical education, settings in which students gained clinical experience, or current employment (P ≤ .05).
Conclusions: The standards for athletic training clinical-education settings are helpful and should be applied to all settings. Varying standards do not need to be imposed on our different athletic training clinical-education settings.
Keywords: clinical instructors, learning environment, clinical environment
In recent years, athletic training education reform has been emphasized. The National Athletic Trainers' Association (NATA), through the work of the Education Council, has revised the Athletic Training Educational Competencies,1 and the Commission on Accreditation of Allied Health Education Programs (CAAHEP) has revised its Standards and Guidelines.2 Also, the NATA Board of Certification (NATABOC) has eliminated both the internship route to certification (beginning January 1, 2004) and the clock-hour requirement (beginning fall 2002 for those completing accredited programs) to sit for the examination.3 These changes have resulted from a shift away from quantity education markers (ie, hours) and toward quality education markers (ie, proficiencies). Clinical education, involving clinicians, students, and patients in a real-life environment, provides a realistic component to a student's education and has, therefore, remained a significant component of health care professional preparation.4–14 Because improvement in professional health care services depends, to a great degree, on maintaining high-quality clinical education,15–18 clinical education appears to also be important to maintaining high-quality athletic training services. Following this lead, the NATA Education Council has positioned clinical education as a priority through the development of the Clinical Instructor Educator and Approved Clinical Instructor credentials.19 All of these reforms are intended to improve the quality of the athletic training profession through enhanced entry-level athletic training professional preparation.
Consistent with the spirit of these reforms, Weidner and Laurent20 developed 12 standards and related measurement criteria for the selection and evaluation of athletic training clinical-education settings. These standards and criteria address the essential personnel, administrative, and environmental factors involved in high-quality clinical-education settings that meet the learning needs of students. As a result, selection and evaluation of clinical-education settings can be based on objective criteria rather than on convenience or availability of “slots.” The limitation of this research was that it did not include a student's perspective of the helpfulness of these 12 standards. Input was only received from athletic training education program directors and clinical instructors.
For the current study, clinical education was defined as the hands-on experience involving clinicians, students, and patients in a real-life environment. This experience provides a realistic component to a student's education. The purpose of clinical education is “to provide the student with sufficient opportunity to develop specific competencies pertaining to the health care of the athlete and those involved in physical activity.”2 Because the Weidner and Laurent standards20 were judged to be relevant, practical, and indicative of a high-quality clinical-education setting, we interpreted that they would be helpful in facilitating professional development of the student. The purpose of our present study was to determine the potential helpfulness of the Weidner and Laurent clinical-education–setting standards in the professional preparation of employed, entry-level certified athletic trainers (ATCs). A secondary purpose was to identify the contribution clinical education made to respondents' overall professional development.
METHODS
Subjects
Employed, entry-level ATCs who recently completed CAAHEP-accredited athletic training education programs were surveyed to determine the potential helpfulness of the Weidner and Laurent20 clinical-education–setting standards in preparing them for their professional roles and responsibilities as ATCs. This target group was chosen because they had some work experience as ATCs, but their education was recent enough to enable them to reflect on the potential helpfulness of the clinical-education–setting standards on their professional development. In 1999, a complete list (n = 2150) of names and addresses of those individuals certified in 1997 was obtained from the NATABOC. This group of athletic trainers had all been certified within 24 months of participating in this study. A random sample of 500 entry-level ATCs was selected from this listing. Unemployed ATCs and ATCs who were students at the time of the survey were excluded because we wanted to know how the standards helped prepare them for entry-level athletic training roles and responsibilities. Those not assuming the roles and responsibilities of an ATC may have a different perspective on the athletic training clinical-education–setting standards.
Instrumentation
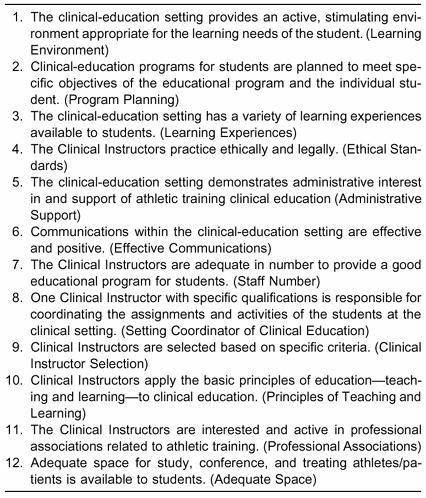
We developed a 22-item questionnaire based on the 12 standards presented by Weidner and Laurent20 (Table 1). Sex, ethnicity, number of clock hours completed, number of clinical-education semesters completed, clinical-experience settings, and current employment setting were recorded to allow for a comparison of these variables to the perception of helpfulness of the standards. Using a Likert scale of 0 (of no help) to 5 (very helpful), without qualifying markers for ratings 1 through 4, respondents indicated their perceptions regarding the potential helpfulness of each standard in preparing them for the requirements of working as ATCs. In an open-ended question, respondents provided their impression of the percentage contribution that clinical education made to their overall professional development compared with the contribution of didactic education to their overall professional development. In a second open-ended question, respondents indicated the aspect of clinical education that best prepared them for their entry-level positions. The instrument went through content and format review by a professional with athletic training expertise and a professional with survey-instrument expertise but no athletic training expertise. The instrument was pilot tested with 49 entry-level ATCs to ensure that the directions and content were clear. Final adjustments to the instrument were made with this input. The internal consistency of the instrument was good (α = .74) as assessed with the Cronbach alpha.
Table 1. Clinical-Education–Setting Standards20
Procedures
We received Ball State University Internal Review Board approval for this project. Respondents were informed that participation was voluntary and that they were free to withdraw at any time without prejudice from the researchers. The questionnaire, cover letter, and a postage-paid return envelope were sent to each respondent. Return envelopes were coded to allow a follow-up mailing to nonrespondents. A 3-week period was given for return of the questionnaires. In order to research a more homogenous group, those respondents who were not employed as athletic trainers or did not complete CAAHEP-accredited athletic training education programs were eliminated from data analysis. Demographic data (eg, sex, ethnicity, etc) for the sample were compared with the NATA membership to ensure a representative sample of the NATA certified membership.21
Statistical Analysis
Frequency counts and percentages were computed for the following questionnaire items:
Perceptions of whether a clinical-education–setting standard was addressed during clinical experiences;
Respondent sex;
Respondent ethnicity;
Total number of clock-hours spent in clinical education;
Total number of semesters spent in clinical education;
Settings in which students gained clinical experience (eg, college, high school, industry, community-based health care facility);
Current employment setting.
Percentage means were computed for the helpfulness ratings of each standard. The percentage mean was also computed for the perception of the overall contribution of clinical education to professional development as gathered through the open-ended question. Responses identifying the aspect of clinical education that best prepared participants for their responsibilities and roles as entry-level ATCs were grouped according to common themes. Chi-square analyses (χ2) were used to assess differences in the helpfulness ratings among respondents. The following categories and cells were used in the analysis: sex (male or female); ethnicity (white or nonwhite); clinical-education hours (<1800 or >1800); total semesters of clinical-education (3–4, 5–6, or 7–10); settings in which students gained clinical experience (college or no college; high school or no high school; industry or no industry; clinic or no clinic); and current employment (clinic or high school, college, or other). These categories were used for analysis because of their logical groupings and to ensure adequate responses in each cell for analysis. Helpfulness was divided into 2 cells. The first helpfulness cell combined ratings 0–3 and was labeled as “little/no help.” The second cell combined ratings 4–5 and was labeled “very helpful.” This more stringent grouping (4–5 rather than 3–5) was used because the standards were presented as “indicative of a high-quality clinical-education setting.”20 For this reason, we determined that a middle response of 3 was not strong enough to warrant consideration as “very helpful.” Only those respondents who indicated that a particular standard seemed to have been addressed in their clinical setting(s) were included in these analyses. This stipulation was included to ensure that a respondent actually had some experience upon which to base the perception of the helpfulness of the standards. The alpha level was set a priori at ≤ .05 for all analyses.
RESULTS
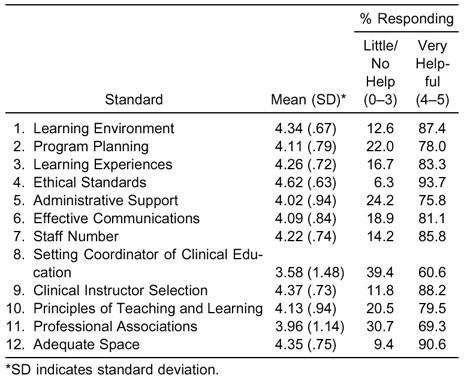
With follow-up to nonrespondents and after exclusion of the 125 questionnaires that were undeliverable due to incorrect mailing addresses, 244 completed surveys (of 500 mailed) were returned, for a response rate of 65.1%. Respondents who were not employed or who had not completed an accredited athletic training education program were eliminated from the data pool. All remaining respondents indicated that all clinical-education–setting standards seemed to have been met. Thus, a total of 129 respondents were included in the data analysis. Table 2 provides the respondents' demographics and clinical-education experience. The employment distribution of the respondents was similar to that of the NATA certified membership. Table 3 presents summary data on the helpfulness of each standard. The overall mean score across all standards was 4.17. Only 2 setting standards had a mean helpfulness rating below 4.0 (Setting Coordinator of Clinical Education [mean = 3.58 ± 1.48] and Professional Associations [mean = 3.96 ± 1.14]). No significant difference was noted in the helpfulness ratings among any of the groups of respondents, regardless of sex, ethnicity, number of clinical-education hours, total semesters of clinical education, clinical-education–setting experiences, or current employment (P ≤ .05). Respondents indicated that 53.0% of their entry-level professional development came from clinical education. Considering the aspects of this clinical education that best prepared them for their entry-level roles and responsibilities, participants commonly cited the importance of opportunities to improve athletic training skills (eg, rehabilitation and injury evaluation) through hands-on practice in a variety of situations and settings. They also indicated that clinical education allowed them to develop their decision-making and communication skills through their responsibilities in athlete and patient care.
Table 2. Demographic Data of Subjects (N = 129) in Comparison with the National Athletic Trainers' Association (NATA) Certified Membership*
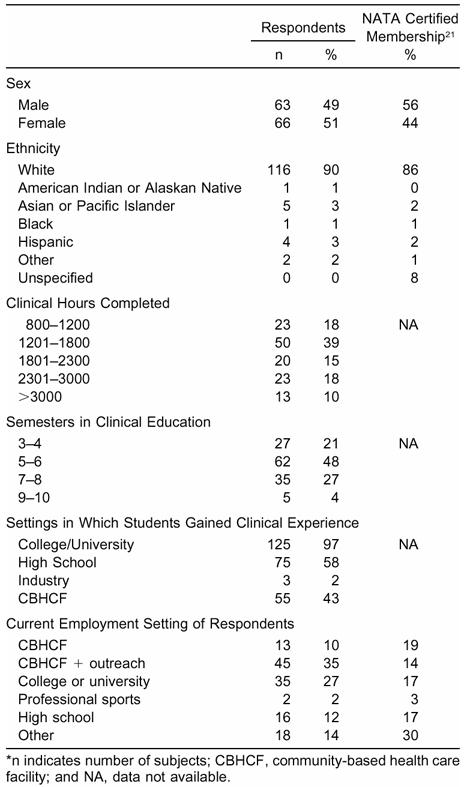
Table 3. Perceived Helpfulness of Standards for Clinical-Education Settings
DISCUSSION
The Weidner and Laurent20 clinical-setting standards are considered by employed, entry-level ATCs to be helpful to very helpful for professional preparation. Ten of these setting standards were judged as very helpful (mean ≥ 4.02). According to the respondents, slightly more than half (53.0%) of athletic training professional development was perceived to come from clinical education. Thus, not only should clinical education remain a large part of the athletic training education program, but clinical-education settings should be structured and evaluated to ensure that optimal education is taking place. Failure to objectively select and evaluate the setting in which students are receiving this clinical education may result in chance learning. Such learning is contrary to the purpose and requirements of accreditation, especially regarding the quality of athletic training clinical education.
These data complement research22,23 that quality rather than quantity of clinical education is more important in the professional preparation of ATCs. Appropriately, quantitative measures are being replaced with qualitative measures in preparing entry-level ATCs.2,3
Certainly it is logical to question the connection between perceived helpfulness of a set of standards and the actual knowledge and skills gained from a setting. Was the setting really more helpful in learning, or did the students just enjoy the setting more? When student evaluations of clinical experience were compared with their clinical skill gain on an objective posttest, the Objective Structured Clinical Examination (OSCE), students in the clinical setting with the most favorable student ratings ultimately scored the highest on the OSCE.18 This research gives some credibility to the respondents' perception of helpfulness ratings obtained in this study.
Consistent with the literature,22 no differences were seen between the respondents' demographic characteristics and clinical experiences and the perceived helpfulness of the standards. Any differences among the helpfulness ratings would have indicated that the clinical-education standards should vary for students. However, the uniform helpfulness ratings obtained in this study indicate that a standard is helpful for all students in all clinical situations. What follows is a discussion of each of the Weidner and Laurent20 clinical-setting standards. The results of this study and the literature amply support their potential helpfulness in clinical education.
Learning Environment
Good management, high staff morale, harmonious working relationships, and sound interdisciplinary patient-management procedures characterize the desirable learning environment.20 Further, a desirable learning experience requires that health care personnel be receptive to students, have a variety of expertise, be interested in new techniques, and be involved with professions outside athletic training. Respondents in this study reported that an active learning environment was very helpful (mean = 4.34 ± 0.67) in their professional development. Respondents also commented that hands-on experiences were valuable and important as part of an active learning environment. Clinical experience is designed to involve students in the actual practice of a profession, allowing them an opportunity to apply theoretic knowledge to real-life situations.10,15–18,24–26 Whether through trial and error or guided by clinical instructors, learning by doing fosters skill acquisition.27 An active learning environment provides ample learning opportunities.28
Program Planning
Specific objectives should be assigned to clinical-education experiences.2 The use of learning objectives is a commonly accepted practice in pedagogy and should be central to planning educational experiences.29 Some athletic training education programs are already using learning objectives to guide students' clinical experiences.30 Certainly objectives improve the uniformity of the educational experience31 and enable program administrators to provide for the educational needs of the individual student. Objectives create the framework to provide students with opportunities to expand their professional knowledge, skills, and attitudes. Both the taxonomy of Bloom et al32 and the CAAHEP Standards and Guidelines2 requirement of learning over time provide for a progression of student learning from introduction to mastery of professional knowledge, skills, and attitudes around which a clinical education program should be organized. Specific planning of level-appropriate learning objectives should occur for each clinical-education rotation and be adapted to the needs of the individual athletic training student.
Learning Experiences
Variety in clinical experiences has been reported by many clinical educators as valuable to students' education.6,12,14,27,33–38 Variety in learning experiences is important not only because it provides more opportunities for students to learn, but also because it provides athletic training students with a wider array of treatment options for their future professional use.38 These treatment options are often referred to as “tools in the toolbox.” Because not every patient responds the same way to every treatment, professionals need to possess the knowledge and skill to address similar problems in a variety of ways.
This specific standard not only addresses variety within a single clinical-education setting but within the total clinical-education program. Because learning styles vary, athletic training students need to be exposed to the multiple teaching methods inherent in a variety of clinical learning experiences.39 Therefore, program directors and clinical-education coordinators should focus both on a variety of learning experiences within a clinical-education setting and on variety throughout the entire clinical-education program.
Ethical Standards
Ethics can be defined as a set of standards that guide the actions and judgments of a profession.40 The goal of the NATA Code of Ethics is to provide high-quality health care delivery through members who conduct themselves with high practice standards at all times.41 Respondents believed that practicing ethically and legally would be the most helpful standard (mean = 4.62 ± 0.63, with 93.7% of the respondents rating this as very helpful). This finding concurs with the literature that identified role modeling as the most helpful clinical-instructor characteristic.42 Clinical settings in which clinical instructors practice unethically may certainly detract from quality clinical education.43
Administrative Support
Considering the variety of the roles and responsibilities of ATCs,44–47 it is not surprising that they may not have time to adequately serve as clinical instructors. Administrative support for clinical instruction may take the form of a reduced workload that allows time for an ATC to prepare and teach clinical skills. Accreditation standards and guidelines require that appropriate resources be available to operate the educational program,2 including adequate clerical and other support staff. This standard would seem to impose a similar requirement on clinical-education settings.
Effective Communications
Communication between the clinical instructor and the student is vitally important to the education process.36,48 The more people involved in communication, however, the greater the chance for misunderstanding.49,50 Course objectives and frequent interactions among program directors, clinical-education coordinators, clinical instructors, and students should help to keep communication clear.
Staff Number
The respondents indicated that a low student-to-clinical instructor ratio would be very helpful in clinical education. The ratio of students to clinical instructors in medical and allied health clinical education is reported as 1:1 to 8:1.18,31,51,52 In general, CAAHEP Standards and Guidelines2 recommend a maximum of 8 students to 1 clinical instructor for appropriate overall clinical supervision, but in specific instances, the Standards and Guidelines require a direct supervision ratio of 1 student to 1 clinical instructor. Direct supervision requires that a clinical instructor be close enough to intervene on behalf of the patient and to instruct and evaluate the clinical proficiencies of a student. A low ratio may be more important with less-experienced students, who benefit from more teacher interaction.39 In contrast, experienced students need more autonomy, and they may benefit more from a larger student to clinical-instructor ratio (eg, 8:1). Certainly even the more-experienced student needs supervision. The ratio should never be so large as to interfere with communication between student and clinical instructor, result in minimal supervision, or cause the clinical instructor to more frequently use a lecture-based format in order to disseminate information.
Setting Coordinator of Clinical Education
Recommendations for medicine18 and physical therapy53 programs suggest using a coordinator at each clinical-education setting. The coordinator keeps the channels of communication open among the students, other clinical instructors at the setting, and program administrators. In this way, the chance for miscommunications and confusion should be less. Although this is a logical approach to coordinating clinical education for the student at the setting, respondents did not perceive this standard to be quite as helpful (mean = 3.58 ± 1.48) as other standards. This may indicate that setting coordination of clinical education is important to the clinical instructors and program administrators but beyond the awareness of the students. As athletic training clinical-education programs incorporate additional settings, a single coordinator of clinical experience likely becomes more important. The more complex the clinical-education structure, the lower the students will rate the educational experiences.28 A single setting coordinator should be able to minimize the confusion that may occur when multiple students are involved with many clinical instructors.
Clinical-Instructor Selection
This standard addresses the need to select clinical instructors based on attributes that make them more effective teachers.20 Expert teachers communicate well, are enthusiastic and organized, get students involved, and use a variety of teaching strategies.6,36 The way a clinical instructor interacts with a student can either help or hinder the learning process.26,54 The CAAHEP Standards and Guidelines2 suggest the importance of clinical instructors by requiring that they have at least one year of athletic training work experience. Physical therapy education programs use this same requirement for their clinical instructors.28,53 Also, CAAHEP Standards and Guidelines2 state, “A clinical instructor should have appropriate experience … and a sincere interest in the professional preparation of athletic training students.” The importance of a good clinical instructor to the overall benefit of the clinical education experience should not be underestimated. Clinical instructors are the most important factor in student satisfaction with clinical-education experience.28 It is therefore important to select clinical instructors who not only have clinical expertise but who understand students as learners and can facilitate the learning process through sound teaching skills.51
Principles of Teaching and Learning
This standard addresses the need for clinical instructors to apply basic principles of teaching and learning in clinical education. Clinical instructors should know how to implement objectives and evaluate student performance.20 Clinical instructors must also have access to materials and workshops that enhance their knowledge and skills as educators; content expertise is not enough to ensure student learning or student satisfaction.31 A pedagogy background helps clinical instructors determine the best instructional approach to use with a particular group of students. Role modeling has been identified as the most important teaching characteristic in athletic training clinical instructors.42 As students learn by applying and practicing skills during clinical education,55 they also need guidance.
Professional Associations
Respondents did not perceive that clinical instructors who are interested and active in professional associations related to athletic training would be quite as helpful (mean = 3.96 ± 1.14) in their professional preparation compared with other standards. Certainly continuing education is required of ATCs in order to maintain their certification.3 The CAAHEP guidelines encourage additional professional involvement of program administrators, faculty, and clinical instructors.2 Clearly the logic is that professionals and professional educators, in particular, need to stay knowledgeable in order to convey current information to students. However, professional involvement does not appear to translate as well to helping students as other standards.
Adequate Space
The CAAHEP Standards and Guidelines require that there be adequate space for clinical education.2 Because the athletic training room is the primary clinical-education factility, space is needed for studying, instructor-student conferences, and treating athletes and patients. While total space is not the complete determinant of the educational value of a facility, the physical environment directly contributes to student learning.56–58 Students acquire and use information by doing, by interacting, and by assigning meaning to information.59 Adequate space allows students to practice skills and interact with patients and instructors and ultimately gives meaning to what they are learning. The physical environment can also stimulate or stifle collaborative learning58,60 as well as assist or inhibit direct supervision of athletic training students. As clinical sites are chosen, educators and clinical instructors need to be aware of the influence of physical facilities on learning.
LIMITATIONS AND SUGGESTIONS FOR FURTHER RESEARCH
Clinical education involves the clinical setting, the student, and the clinical instructor. This research focused on employed, entry-level ATCs' percepetions of the helpfulness of clinical-education–setting standards in preparing them to assume their professional roles and responsibilities. In this way, it serves as a means of assessing the quality of a clinical-education setting. The strength of this research was that it made the connection between clinical-education settings and their contribution in preparing athletic training students for professional roles and responsibilites. A limitation of this research was that it relied on the recall of participants. It is possible that the participants' perceptions of their clinical-education experiences were not completely reliable. It is also possible that participants had difficulty separating those skills and knowledge gained in clinical versus didactic education. Although we asked about clinical education as an isolated part of professional preparation, it is likely that there is an important interaction between didactic and clinical education. This potential interaction should be explored. Also, outcome studies that focus on knowledge and skill gained in clinical education may help to determine which aspects of clinical-education are most helpful.
CONCLUSIONS
The 12 Weidner and Laurent20 standards for clinical-education settings in athletic training are considered practical, relevant, and suggestive of high-quality clinical-education settings by educators, clinical instructors, students, and employed, entry-level certified athletic trainers. The assumption about these standards before this research was that the standards were helpful in preparing students for their roles and responsibilities as entry-level certified athletic trainers. Our current findings and other research support this assumption.
The standards are applicable to all athletic training students in all clinical-education settings. Regardless of where students received their experience or where they worked as certified athletic trainers after entry-level education, the setting standards were helpful. Varying standards need not be imposed on our different athletic training clinical-education settings.
Athletic training program administrators may want to consider giving less weight to Setting Coordinator of Clinical Education and Professional Associations when using the Weidner and Laurent clinical-education–setting standards to select and evaluate clinical-education settings. Program administrators should be aware that this group of entry-level athletic trainers was less confident of the helpfulness of these 2 standards.
Clinical education makes a substantial contribution to the professional preparation of athletic training students.
Acknowledgments
ACKNOWLEDGMENTS
This research was supported through a grant from the Great Lakes Athletic Trainers' Association Research Assistance Fund (Tim Laurent).
REFERENCES
- National Athletic Trainers' Association, Inc . Athletic Training Educational Competencies. 3rd ed National Athletic Trainers' Association, Inc.; Dallas, TX: 1999. [Google Scholar]
- Commission on Accreditation of Allied Health Education Programs Standards and Guidelines. Available at: http://www.CAAHEP.org. Accessed October 7, 2001.
- National Athletic Trainers' Association Board of Certification Certification requirements. Available at: http://www.nataboc.org/fut_ATC/certexam/reqs/. Accessed September 27, 2001.
- Andersen M B, Larson G A, Luebe J J. Student and supervisor perceptions of the quality of supervision in athletic training education. J Athl Train. 1997;32:328–332. [PMC free article] [PubMed] [Google Scholar]
- Weidner T G, August J. The athletic therapist as clinical instructor. Athl Ther Today. 1997;2:49–52. [Google Scholar]
- Irby D M. What clinical teachers in medicine need to know. Acad Med. 1994;69:333–342. doi: 10.1097/00001888-199405000-00003. [DOI] [PubMed] [Google Scholar]
- Gwyer J, Barr J S, Talmor Z. Selection of clinical education centers in physical therapy. J Allied Health. 1992;11:272–281. [PubMed] [Google Scholar]
- Foord L, DeMont M. Teaching students in the clinical setting: managing the problem situation. J Phys Ther Educ. 1990;4:61–66. [Google Scholar]
- Schweitzer K L, Cohen P A. Teaching dental materials using the personalized system of instruction. J Dent Educ. 1987;51:589–593. [PubMed] [Google Scholar]
- Frisch N A, Coscarelli W. Systematic instructional strategies in clinical teaching: outcomes in student charting. Nurse Educ. 1986;11:29–32. doi: 10.1097/00006223-198611000-00008. [DOI] [PubMed] [Google Scholar]
- Peat M. Enid Graham memorial lecture: clinical education of health professionals. Physiother Can. 1985;37:301–307. [Google Scholar]
- Gjerde C L, Coble R J. Resident and faculty perceptions of effective clinical teaching in family practice. J Fam Pract. 1982;14:323–327. [PubMed] [Google Scholar]
- Barrett J E, Powell G L. Dental faculty training in clinical instruction. J Biocommun. 1980;7:11–15. [PubMed] [Google Scholar]
- Flom-Kegel P. Evaluating and improving clinical instruction. Am J Optom Physiol Opt. 1977;54:708–715. doi: 10.1097/00006324-197710000-00009. [DOI] [PubMed] [Google Scholar]
- Blue A V, Stratton T D, Plymale E M, DeGnore L T, Schwartz R W, Sloan D A. The effectiveness of the structured clinical instruction module. Am J Surg. 1998;176:67–70. doi: 10.1016/s0002-9610(98)00109-3. [DOI] [PubMed] [Google Scholar]
- Slotnick H B. How doctors learn: the role of clinical problems across the medical school-to-practice continuum. Acad Med. 1996;71:28–34. doi: 10.1097/00001888-199601000-00014. [DOI] [PubMed] [Google Scholar]
- Villafuerte A. Structured clinical preparation time for culturally diverse baccalaureate nursing students. Int J Nurs Stud. 1996;33:161–170. doi: 10.1016/0020-7489(95)00047-x. [DOI] [PubMed] [Google Scholar]
- Anderson D C, Harris I B, Allen S, et al. Comparing students' feedback about clinical instruction with their performances. Acad Med. 1991;66:29–34. doi: 10.1097/00001888-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Starkey C. Reforming athletic training education [editorial] J Athl Train. 1997;32:113–114. [PMC free article] [PubMed] [Google Scholar]
- Weidner T G, Laurent T G. Selection and evaluation guidelines for clinical education settings in athletic training. J Athl Train. 2001;36:62–67. [PMC free article] [PubMed] [Google Scholar]
- National Athletic Trainers' Association 2000 membership statistics Available at: www.nata.org/membership/graphs/bodgraphs2000.htm. Accessed July 20, 2001.
- Turocy P S, Comfort R E, Perrin D H, Gieck J H. Clinical experiences are not predictive of outcomes on the NATABOC examination. J Athl Train. 2000;35:70–75. [PMC free article] [PubMed] [Google Scholar]
- Weidner T G, Vincent W J. Evaluation of professional preparation in athletic training by employed, entry-level athletic trainers. J Athl Train. 1997;27:304–307. [PMC free article] [PubMed] [Google Scholar]
- Sloan D A, Donnelly M B, Plymale M A, et al. Improving residents' clinical skills with the structured clinical instruction module for breast cancer: results of a multiinstitutional study. Breast Cancer Education Working Group. Surgery. 1997;122:324–333. doi: 10.1016/s0039-6060(97)90024-6. [DOI] [PubMed] [Google Scholar]
- Ladyshewsky R K, Barrie S C, Drake V M. A comparison of productivity and learning outcomes in individual and cooperative physical therapy clinical education models. Phys Ther. 1998;78:1288–1298. doi: 10.1093/ptj/78.12.1288. [DOI] [PubMed] [Google Scholar]
- Jarski R W, Kulig K, Olson R E. Clinical teaching in physical therapy: student and teacher perceptions. Phys Ther. 1990;70:173–178. doi: 10.1093/ptj/70.3.173. [DOI] [PubMed] [Google Scholar]
- Singer R N, Gaines L. Effects of prompted and problem-solving approaches on learning and transfer of motor skills. Am Educ Res J. 1975;12:395–403. [Google Scholar]
- Stith J S, Butterfield W H, Strube M J, Deusinger S S, Gillespie D F. Personal, interpersonal, and organizational influences on student satisfaction with clinical education. Phys Ther. 1998;78:635–645. doi: 10.1093/ptj/78.6.635. [DOI] [PubMed] [Google Scholar]
- Davies I K. Objectives in Curriculum Design. McGraw-Hill; New York, NY: 1976. [Google Scholar]
- Fuller D. Critical thinking in undergraduate athletic training education. J Athl Train. 1997;32:242–247. [PMC free article] [PubMed] [Google Scholar]
- Davis W K, Oh M S, Anderson R M, Gruppen L, Nairn R. Influence of a highly focused case on the effect of small-group facilitators' content expertise on students' learning and satisfaction. Acad Med. 1994;69:663–669. doi: 10.1097/00001888-199408000-00016. [DOI] [PubMed] [Google Scholar]
- Bloom B S, Engelhart M D, Furst E J, Hill W H, Krathwohl D R. Taxonomy of Educational Objectives: Handbook 1. Longmans; New York, NY: 1959. [Google Scholar]
- Education Task Force Update. NATA News. Feb, 1997. pp. 16–24.
- Irby D M, Ramsey P G, Gillmore G M, Schaad D. Characteristics of effective clinical teachers of ambulatory care medicine. Acad Med. 1991;66:54–55. doi: 10.1097/00001888-199101000-00017. [DOI] [PubMed] [Google Scholar]
- Deusinger S S. Evaluating the effectiveness of clinical education. J Phys Ther Educ. 1990;4:66–70. [Google Scholar]
- Emery M J. Effectiveness of the clinical instructor: students' perspective. Phys Ther. 1984;64:1079–1083. doi: 10.1093/ptj/64.7.1079. [DOI] [PubMed] [Google Scholar]
- Irby D M. Clinical teacher effectiveness in medicine. J Med Educ. 1978;53:808–815. doi: 10.1097/00001888-197810000-00003. [DOI] [PubMed] [Google Scholar]
- Stritter F T, Hain J D, Grimes D A. Clinical teaching reexamined. J Med Educ. 1975;50:876–882. doi: 10.1097/00001888-197509000-00005. [DOI] [PubMed] [Google Scholar]
- Harrelson G L, Leaver-Dunn D, Wright K E. An assessment of learning styles among undergraduate athletic training students. J Athl Train. 1998;33:50–53. [PMC free article] [PubMed] [Google Scholar]
- Mangus B C, Ingersoll C D. Approaches to ethical decision making in athletic training. J Athl Train. 1990;25:340–343. [Google Scholar]
- National Athletic Trainers' Association Code of Ethics Available at: http://www.nata.org/publications/brochures/ethics.htm. Accessed October 7, 2001.
- Laurent T, Weidner T G. Clinical instructors' and student athletic trainers' perceptions of helpful clinical instructor characteristics. J Athl Train. 2001;36:58–61. [PMC free article] [PubMed] [Google Scholar]
- Haskins A R, Rose-St Prix C, Elbaum L. Covert bias in evaluation of physical therapist students' clinical performance. Phys Ther. 1997;77:155–163. doi: 10.1093/ptj/77.2.155. [DOI] [PubMed] [Google Scholar]
- Staurowsky E, Scriber K. An analysis of selected factors that affect the work lives of athletic trainers employed in accredited educational programs. J Athl Train. 1998;33:244–248. [PMC free article] [PubMed] [Google Scholar]
- Duncan K M, Wright K E. A national survey of athletic trainer roles and responsibilities in the allied clinical setting. J Athl Train. 1992;27:311–316. [PMC free article] [PubMed] [Google Scholar]
- Perrin D H, Lephart S M. Role of the NATA curriculum director as clinician and educator. J Athl Train. 1988;23:41–43. [Google Scholar]
- National Athletic Trainers' Association Board of Certification . Role Delineation Study: Athletic Training Profession. 4th ed Columbia Assessment Services; Morrisville, NC: 1999. [Google Scholar]
- Swann E, Walker S E. Interpersonal communications of the athletic training clinical instructor [abstract] J Athl Train. 2001;36(suppl):S-48. [Google Scholar]
- Hanson E M. Educational Administration and Organizational Behavior. 4th ed Allyn and Bacon; Boston, MA: 1996. [Google Scholar]
- Kowalski T J. The School Superintendent: Theory, Practice, and Cases. Merrill Prentice Hall; Columbus, OH: 1999. [Google Scholar]
- Triggs Nemshick M T, Shepard K F. Physical therapy clinical education in a 2:1 student-instructor education model. Phys Ther. 1996;76:968–981. doi: 10.1093/ptj/76.9.968. [DOI] [PubMed] [Google Scholar]
- Foster D T, Leslie D K. Clinical teaching roles of athletic trainers. J Athl Train. 1992;27:298–302. [PMC free article] [PubMed] [Google Scholar]
- American Physical Therapy Association PT/PTA educators and clinical educators–information. Available at: https://www.apta.org/Education/educatorinfo. Accessed October 4, 2001.
- Curtis N, Helion J G, Domsohn M. Student athletic trainer perceptions of clinical supervisor behaviors: a critical incident study. J Athl Train. 1998;33:249–253. [PMC free article] [PubMed] [Google Scholar]
- Draper D O. An evaluation model of the student athletic trainer's clinical experience. J Athl Train. 1987;22:111–114. [Google Scholar]
- Kennedy M. Making an impact. Am School Univ. 1999;72:16–26. [Google Scholar]
- Kennedy M. Creating ideal facilities: here are 10 ways a school can provide an effective learning environment. Am School Univ. 2002;74:30–33. [Google Scholar]
- Tinto V. Classrooms as communities: exploring the educational character of student persistence. J Higher Educ. 1997;68:599–624. [Google Scholar]
- Gardner H. Frames of Mind: The Theory of Multiple Intelligences. Basic Books; New York, NY: 1983. [Google Scholar]
- Metcalf M C. Changing the rules. College Plan Manage. 2000;3:52–54. [Google Scholar]


