Abstract
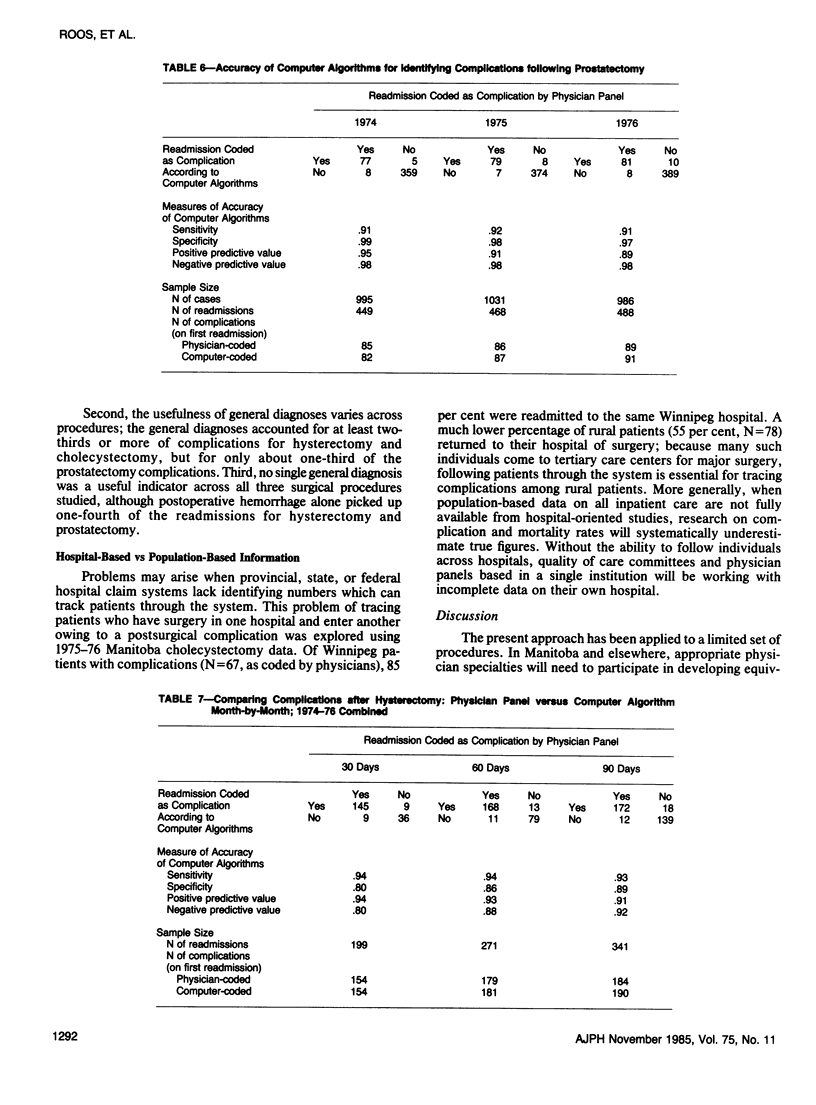
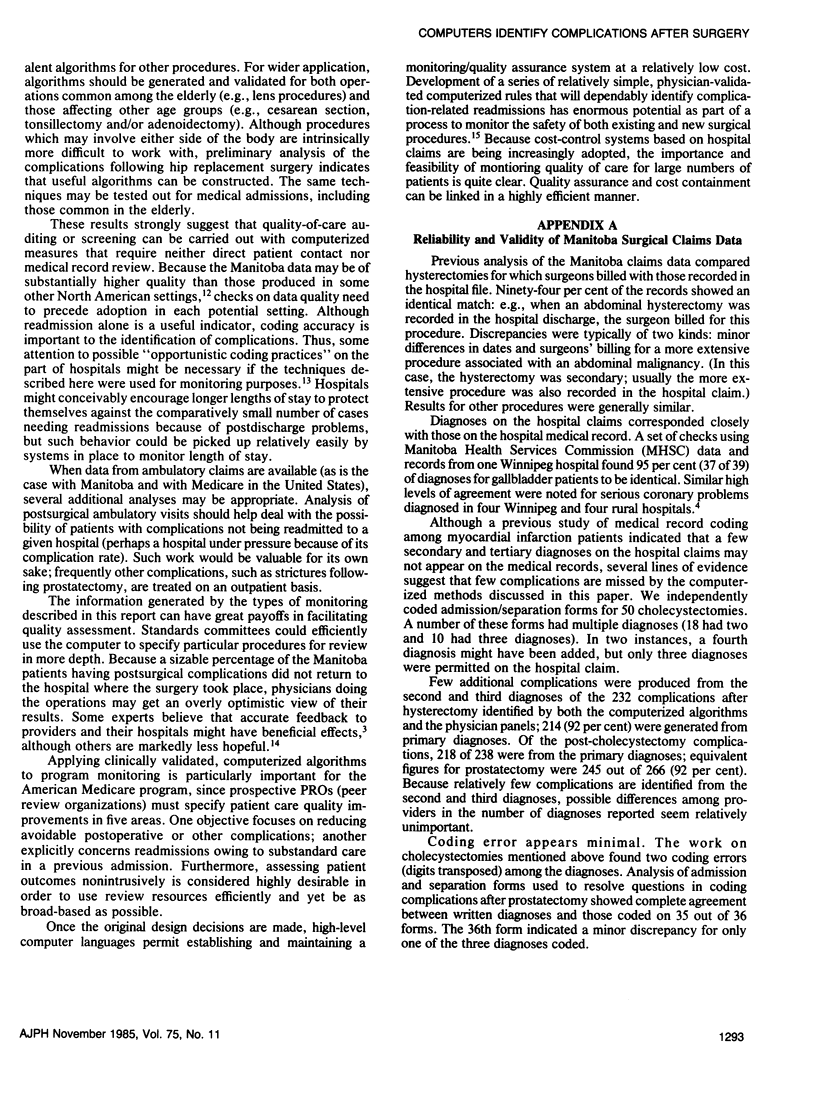
We used the Health Services Commission data from Manitoba, Canada to identify complications resulting from hysterectomy, cholecystectomy, and prostatectomy which led to hospital readmissions. For each procedure, two specialists independently judged whether the readmissions were for surgery-related complications on the basis of liberally interpreted literature guidelines. Then, each pair of physicians met to resolve differences; only complications agreed upon by physicians were retained in our computer-based analysis. The analysis was done in three steps: algorithms were developed using guidelines from the literature, physician input, and 1974 hospital claims; these were then modified using 1975 data; finally, the algorithms were tested with 1976 data. The computerized algorithms developed were compared with the clinical decisions of physician panels. The results showed high specificity, sensitivity, and predictive value. Given the increasing availability of routinely collected data bases, the possibilities for inexpensively monitoring the outcomes of different providers and institutions are appealing. More extensive validation and application of the methodology to a greater number of procedures are necessary to implement such a program.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chilton C. P., Morgan R. J., England H. R., Paris A. M., Blandy J. P. A critical evaluation of the results of transurethral resection of the prostate. Br J Urol. 1978 Dec;50(7):542–546. doi: 10.1111/j.1464-410x.1978.tb06208.x. [DOI] [PubMed] [Google Scholar]
- Demlo L. K., Campbell P. M. Improving hospital discharge data: lessons from the National Hospital Discharge Survey. Med Care. 1981 Oct;19(10):1030–1040. doi: 10.1097/00005650-198110000-00005. [DOI] [PubMed] [Google Scholar]
- Jenkins V. R., 2nd Unnecessary-elective-indicated? Audit criteria of the American College of Obstetricians and Gynecologists to assess abdominal hysterectomy for uterine leiomyoma. QRB Qual Rev Bull. 1977 May;3(5):7-12,21. [PubMed] [Google Scholar]
- Johnson A. N., Appel G. L. DRGs and hospital case records: implications for Medicare case mix accuracy. Inquiry. 1984 Summer;21(2):128–134. [PubMed] [Google Scholar]
- Lohr K. N., Brook R. H., Kaufman M. A. Quality of care in the New Mexico Medicaid program (1971-1975): the effect of the New Mexico Experimental Medical Care Review Organization on the use of antibiotics for common infectious diseases. Med Care. 1980 Jan;18(1 Suppl):i-vi, 1-129. [PubMed] [Google Scholar]
- Roos L. L., Jr, Roos N. P., Cageorge S. M., Nicol J. P. How good are the data? Reliability of one health care data bank. Med Care. 1982 Mar;20(3):266–276. doi: 10.1097/00005650-198203000-00003. [DOI] [PubMed] [Google Scholar]
- Roos N. P. Hysterectomies in one Canadian Province: a new look at risks and benefits. Am J Public Health. 1984 Jan;74(1):39–46. doi: 10.2105/ajph.74.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simborg D. W. DRG creep: a new hospital-acquired disease. N Engl J Med. 1981 Jun 25;304(26):1602–1604. doi: 10.1056/NEJM198106253042611. [DOI] [PubMed] [Google Scholar]
- Smits H. L., Watson R. E. DRGs and the future of surgical practice. N Engl J Med. 1984 Dec 20;311(25):1612–1615. doi: 10.1056/NEJM198412203112505. [DOI] [PubMed] [Google Scholar]
- Stern R. S., Epstein A. M. Institutional responses to prospective payment based on diagnosis-related groups. Implications for cost, quality, and access. N Engl J Med. 1985 Mar 7;312(10):621–627. doi: 10.1056/NEJM198503073121005. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E. Dealing with medical practice variations: a proposal for action. Health Aff (Millwood) 1984 Summer;3(2):6–32. doi: 10.1377/hlthaff.3.2.6. [DOI] [PubMed] [Google Scholar]



