Previous articles in this series have discussed the relation of overweight and obesity with coronary heart disease (CHD) and individual cardiovascular disease risk factors—such as diabetes, raised blood pressure, and dyslipidaemia. This article examines the wider impact of obesity on vascular disease: the effect on cardiovascular disease of obesity as primary cause of the metabolic syndrome and of obesity as a risk factor for heart failure, stroke, other vascular conditions, and cognitive decline.
Metabolic syndrome
Definitions of insulin resistance
Broad definition
Insulin resistance is a clinical state in which a normal or raised insulin level produces an impaired biological response. As insulin has a number of physiological actions—including a central role in acute metabolic actions and growth and development—insulin resistance could mean impairment in any of these actions
Specific definition in relation to metabolic syndrome
Insulin resistance, when used to identify those at risk of type 2 diabetes and as a component of the metabolic syndrome, usually refers to resistance to insulin's ability to stimulate glucose uptake in insulin sensitive peripheral tissues and its ability to suppress hepatic glucose production, promote glucose storage, inhibit ketogenesis, and suppress lipolysis
The metabolic syndrome refers to the clustering within individuals of several CHD risk factors—including glucose intolerance, dyslipidaemia, and raised blood pressure—believed to be linked by a common pathophysiological process. Individuals may develop these factors in different orders, with different severities, and at different ages, but they are unified by the fact that adult weight gain is a risk factor in their development. Reaven suggested in 1988 that insulin resistance was important in causing these risk factors, but others have concluded that obesity, particularly intra-abdominal fat accumulation, is probably a common primary cause.
Environmental exposures throughout life (such as high fat, energy dense diets; low levels of physical activity in childhood and adulthood; and factors related to poor intrauterine growth) also contribute to development of the metabolic syndrome. The (unknown) genetic predisposition is probably present in about 20-30% of all people.
Summary definitions of metabolic syndrome
World Health Organization*
Insulin resistance plus at least two of the following: raised blood pressure, dyslipidaemia, obesity, microalbuminuria
American Treatment Panel III†
At least three of the following:
High fasting glucose
Raised blood pressure
Raised plasma triglycerides
Low HDL (high density lipoprotein) cholesterol
Obesity (large waist circumference)
International Diabetes Federation‡
Obesity (large waist) plus at least two of the following: raised triglycerides, reduced HDL cholesterol, raised blood pressure, raised fasting plasma glucose
*Alberti K, Zimmet P. Definition, diagnosis and classification of diabetes mellitus and its complications. Part I: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998;15:539-53.
†Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.
‡International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. 2005. www.idf.org/webdata/docs/Metac_syndrome_def.pdf (accessed 19 Sep 2006)
Three definitions of the metabolic syndrome have been developed. A review in 2005 by Kahn et al (see Further Reading box) questions the clinical value of the syndrome.
There are several problems with using a “diagnosis” of the metabolic syndrome (on the basis of the three definitions) as a screening test to identify people who would benefit from an intervention to improve cardiovascular health (such as weight management). The definitions use arbitrary thresholds for risk factors that are mostly linearly associated with cardiovascular disease. Despite the widespread practice of using thresholds of continuous risk factors to make “diagnoses” so that treatment can be started (for example, diagnosing hypertension on the basis of a blood pressure >140/90 mm Hg), it is now technically possible to be more accurate in predicting disease risk.
Potential weaknesses of current criteria for metabolic syndrome for predicting risk
The current criteria have not yet been shown definitively to add to risk prediction for cardiovascular disease beyond current charts
Arbitrary thresholds for risk factors and differing combinations of risk factors in the different definitions may lead to loss of important information about an individual's risk of cardiovascular disease
The criteria fail to include important risk factors such as age, low density lipoprotein cholesterol, and smoking—a weakness if metabolic syndrome is used as the sole means of defining cardiovascular disease risk
Prediction models that include additional risk factors (not just components of the metabolic syndrome) are a better means of identifying those at greatest risk
The requirement for specific combinations of risk factors means that some individuals who are at risk of cardiovascular disease will not be diagnosed with the syndrome. The extent to which different risk factors matter will vary by sex, age, and ethnic group, and therefore the definitions will perform differently in different populations.
Requirements of future research
Identify the best prediction models for cardiovascular disease and diabetes in different population groups (by pooling data from large number of individual prospective data sets in different populations)
Evaluate the long term effect on disease risk of using these prediction models in clinical practice
Determine the long term effect of weight maintenance and reduction programmes on cardiovascular disease risk using appropriately resourced and powered prospective trials
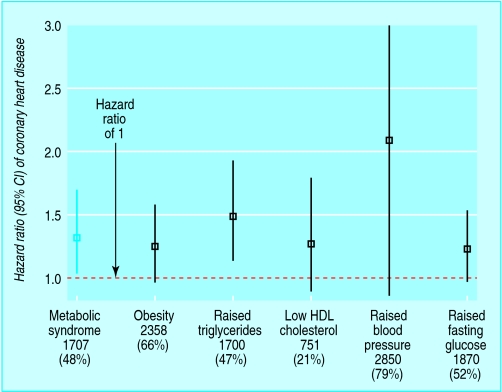
Age adjusted hazard ratio of coronary heart disease associated with International Diabetes Federation's definition of metabolic syndrome and each component of this definition among 3589 British women aged 60-79 years. Data from Lawlor et al (Diabetologia 2006 doi: 10.1007/s00125-005-0040-3)
These issues are illustrated with an example from a study of British women aged 60-79 years. In this study there were similar weak associations of all three definitions of metabolic syndrome with incident CHD but greater association from hypertension. As hypertension is common in this age group, its absolute effect on CHD is high, whereas that of the metabolic syndrome (by any of the three definitions) is not. Obesity, however, was not an important predictor in this study.
Practical strategy for managing raised waist circumference in relation to cardiovascular disease risk
| Waist /score for cardiovascular risk | Treatment |
|---|---|
| Circumference <80 cm in women, <94 cm in men (low risk) | Requires no intervention (avoid weight gain and stay below these levels) |
| Circumference ≥80 cm in women, ≥94 cm men, and <10% risk of cardiovascular disease* over next 10 years (raised risk) | Requires health promotion and public health measures for self directed treatment to prevent further weight gain |
| Circumference 80-88 cm in women and 94-102 cm men, and >10% risk of cardiovascular disease* over next 10 years (high risk) | Requires effective treatment to lose 5-10% body weight and to prevent further weight gain |
| Circumference >88 cm in women and >102 cm in men irrespective of 10 year risk of cardiovascular disease* (high risk for other medical problems associated with obesity or intra-abdominal fat accumulation) | Requires effective treatment to lose 5-10% body weight and to prevent further weight gain |
*Risk based on Joint British Society's guidelines (or equivalent); cardiovascular risk score of >20% requires management in line with the society's guidelines
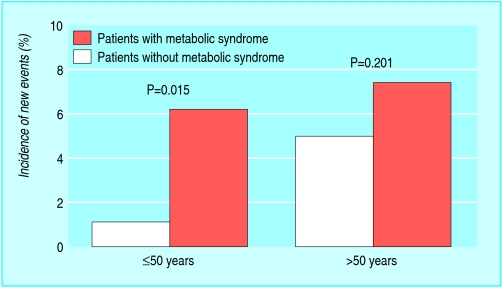
Other studies have found that body mass index (weight in kilograms divided by height in metres squared) does not predict CHD in older individuals, probably reflecting a proportionately greater loss of lean muscle than fat with increased age. Thus, to reduce CHD in older women, assessing and appropriately treating raised blood pressure may be more important than diagnosing and treating the metabolic syndrome. Metabolic syndrome may, however, be a more potent predictor in younger subjects (say, <50 years) with premature CHD, as suggested by recent studies. This important point requires greater study, given the rising prevalence of obesity and its potentially greater impact on vascular risk in younger subjects.
Age stratified incidence of new cardiovascular events (myocardial infarction, revascularisation, cardiac death) in patients with or without metabolic syndrome (according to modified criteria of American Treatment Panel III). Adapted from Reinhard et al (Am J Cardiol 2006;97:964-7)
For clinical practice we therefore need to develop more sophisticated risk prediction scores. Many primary care staff already have computer based, user friendly systems for estimating Framingham risk scores. An easy to use computer package could be developed that combines information on metabolic syndrome components and all other risk factors of an individual to give the best information about an individual's risk. In the meantime, to target obesity, a practical alternative strategy needs to recognise the importance of weight management in conjunction with cardiovascular disease risk.
Although obesity (in particular intra-abdominal fat accumulation), insulin resistance, diabetes risk, and cardiovascular disease risk are all associated with each other, models to predict cardiovascular disease are likely to differ from those used to predict type 2 diabetes. This is because some risk factors are specific to one but not the other. For example, raised concentration of low density lipoprotein (LDL) cholesterol is a specific cardiovascular disease risk factor, and the metabolic syndrome is a stronger predictor of type 2 diabetes than it is of cardiovascular disease (see Sattar, Further Reading box.) However, studies using a variety of methods have found that people with metabolic syndrome (any definition) show a wide range of insulin sensitisation.
Glucose, waist circumference, and triglyceride—three of the key components of the criteria for metabolic syndrome—are far stronger predictors of diabetes than of cardiovascular disease
The outlined conclusions on the associations of obesity with heart failure, stroke, and cognitive decline are based on the best available published evidence from prospective cohort studies that have used measures to minimise these sources of bias
Potential bias and confounding
Three potential sources of bias could lead to underestimation of the effect of obesity on the development of vascular disease.
Firstly, as individuals developing cardiac disease may start to lose weight before the disease is diagnosed, reverse causality can explain null or weak findings. This can be avoided if only healthy individuals (at baseline) are included and long term prospective cohort studies are conducted.
Secondly, smoking is linked with lower body mass index (though larger waist), and so the underweight and “normal” weight categories (based on body mass index) will be over-represented with individuals who smoke. As smoking raises the risk of cardiovascular disease it can mask the effect of overweight and obesity on cardiovascular disease outcomes.
Thirdly, patients who are at high risk of cardiovascular disease (for example, those with a family history) may intentionally lose weight, and if this is not taken into account in the study design or analysis it again will result in an underestimation of the true effect of obesity on disease risk.
Heart failure
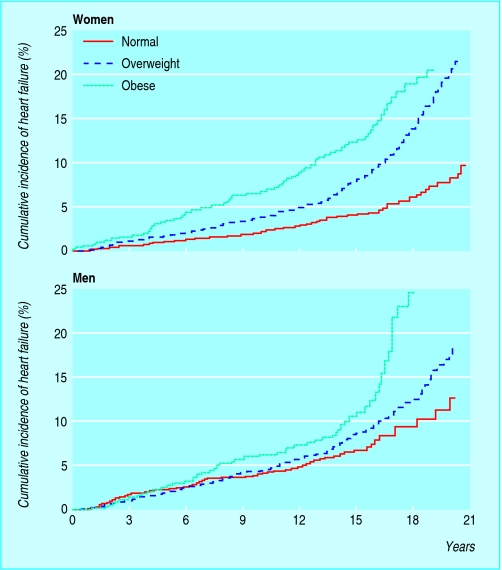
Overweight and obesity are associated with left ventricular hypertrophy and dilatation, which are known precursors of heart failure.
In the Framingham prospective cohort the incidence of heart failure gradually increased with greater body mass index, with the risk doubling in obese individuals. This increased risk was not fully explained by other risk factors, such as hypertension, raised cholesterol concentration, and diabetes, which had previously been thought to mediate the effect of obesity on heart failure. Obesity alone accounted for 11% of cases of heart failure in men and 14% of cases in women.
Survival in obese patients with heart failure
An apparent survival advantage associated with higher body mass index in patients with heart failure does not mean that obesity is protective. Rather, a combination of earlier presentation of heart failure in obese subjects (due to symptoms at less severe levels of heart failure) and possibly reverse causality (non-purposeful weight loss in patients with heart failure who have a lower BMI associated with worse prognosis) may partly explain this “obesity paradox”
Purposeful weight loss in heart failure patients with morbid obesity has been associated with improvements in systolic and diastolic function and in heart failure severity
However, sufficiently powered randomised trials are needed to establish the effectiveness of weight reduction programmes in obese heart failure patients in relation to event-free survival
Similarly, results from the recently reported Uppsala longitudinal study of adult men found that greater body mass index and waist circumference were each associated with an increased risk of congestive heart failure in models that adjusted for diabetes, prior myocardial infarction, left ventricular hypertrophy, smoking, and serum cholesterol concentration. The study found strong evidence that insulin resistance might mediate the effect of obesity on heart failure.
Stroke
Obesity is also associated with increased risk of atrial fibrillation, venous thromboembolism, and sudden death. Obesity is therefore associated with a broad range of fatal and non-fatal CV events
Several long term prospective cohort studies have found a strong association between greater body mass index or relative weight and risk of either total stroke or ischaemic stroke. The effect is attenuated by adjustment for risk factors such as hypertension, raised cholesterol concentration, and glucose intolerance. These risk factors are likely to be on the causal pathway between obesity and stroke, and therefore the attenuation of effect with their adjustment should not be interpreted as indicating that obesity is not causally related to stroke risk.
The effect of obesity on haemorrhagic stroke is less well established, but a large prospective cohort study of Korean men found a positive linear association between body mass index and ischaemic stroke and a J shaped association with haemorrhagic stroke. Thus, for both ischaemic and haemorrhagic stroke, individuals with a body mass index above the reference category of 22-23 were at increased risk.
Conclusion
Clear evidence exists that obesity has a wider impact on cardiovascular health beyond its effect on coronary heart disease
Individuals who are obese in mid-life are at increased risk of heart failure and stroke in later life, and emerging evidence shows that they may also be at increased risk of dementia. For all these associations, the link between obesity and disease outcome could result from the behaviours that cause adult weight gain—namely, inactivity and high fat diets
Further, the associations may in part be mediated by obesity related diabetes, hypertension, and dyslipidaemia, but the causal pathway still involves adult weight gain
This emphasises the importance of reversing the current obesity epidemic, not only because of its impact on premature mortality but because of the devastating effect it will have on quality of life in older age through its impact on these disease outcomes
Cognitive decline
A recent prospective study of over 10 000 individuals whose weight, height, and subscapular and triceps skinfold thickness were assessed between 1964 and 1973 found that those who were overweight or obese (defined by body mass index) were at increased risk of dementia (that is, as recorded in their medical notes between 1994 and 2003).
The study also found positive linear associations between both measures of skinfold thickness and dementia. These associations remained after adjustment for potential confounders (age, sex, ethnicity, marital status, alcohol, smoking, and education) and potential mediating factors (hypertension, diabetes, high cholesterol, stroke).
Further reading
Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2005;28:2289-304.
Sattar N. The metabolic syndrome: should current criteria influence clinical practice? Curr Opin Lipidol 2006;17:404-11.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med 2002;347:305-13.
Ingelsson E, Sundstrom J, Arnlov J, Zethelius B, Lind L. Insulin resistance and risk of congestive heart failure. JAMA 2005;294:334-41.
Lavie CJ, Mehra MR, Milani RV. Obesity and heart failure prognosis: paradox of reverse epidemiology? Eur Heart J 2005;26:5-7.
Song Y-M, Sung J, Davey Smith G, Ebrahim S. Body mass index and ischemic and hemorrhagic stroke. A prospective study in Korean men. Stroke 2004;35:831-6.
Murphy NF, MacIntyre K, Stewart S, Hart CL, Hole D, McMurray JJ. Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew-Paisley study). Eur Heart J 2006;27:96-106.
Whitmer RA, Gunderson EP, Barrett-Connor E, Quesenberry CP Jr, Yaffe K. Obesity in middle age and future risk of dementia: a 27 year longitudinal population based study. BMJ 2005;330:1360-5.
British Cardiac Society et al. Joint British societies' guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005;91(suppl 5):v1-52.
As dementia was obtained from medical records, “confounding by indication” may in part explain the association: individuals who are obese are more likely to visit their doctors and more likely to be assessed for the presence of a range of conditions. Thus, it would be useful to see this association repeated in a prospective study that assessed dementia by means of a clinical interview with all cohort members. The authors suggested that obesity might increase the risk of dementia through its effect on diabetes and heart disease and may also have a direct effect on neuronal degradation. Emerging evidence also supports a link between higher physical activity levels and reduced risk of cognitive decline.
Cumulative incidence of heart failure by weight category (based on body mass index) at baseline examination in Framingham study. Adapted from Kenchaiah et al (see Further Reading box)
Ethnic and sex specific definitions of obesity (based on waist circumference) used in the International Diabetes Federation's definition of metabolic syndrome
| Ethnic group | Waist circumference (women; men) |
|---|---|
| Europids | ≥80cm; ≥94cm |
| South Asians, Chinese, Japanese | ≥80cm; ≥90cm |
| Ethnic south and central Americans | Use data for South Asians pending more specific research data |
| Sub-Saharan Africans; eastern Mediterranean and middle eastern (Arab) populations | Use data for Europids pending more specific research data |
Debbie A Lawlor is professor of epidemiology in the department of social medicine at the University of Bristol.
The ABC of Obesity is edited by Naveed Sattar (nsattar@clinmed.gla.ac.uk), professor of metabolic medicine, and Mike Lean, professor of nutrition, University of Glasgow. The series will be published as a book by Blackwell Publishing in early 2007.
Competing interests: For series editors' competing interests, see the first article in this series.
The photograph is published with permission from Mauro Fermariello/SPL
This is the eighth article in the series