Abstract
Advances in antiviral therapy have dramatically shifted the demographics of pediatric human immunodeficiency virus type 1 (HIV-1) infection in the developed world, and a growing proportion of perinatally HIV-1-infected children are now entering their second or even third decade of life. Although cellular immune responses to HIV are known to be weak in early infancy, the magnitude, breadth, and specificity of responses later in childhood have not been characterized in detail. We performed a comprehensive characterization of HIV-1-specific CD8 responses in 18 perinatally infected children (age range, 6 to 17 years), most of whom were on antiviral therapy, using both previously defined HIV-1 epitopes and overlapping peptides spanning all HIV-1 proteins. Multispecific responses were detected in all subjects and accounted for a median of 0.25 to 0.3% of all peripheral blood mononuclear cells that was similar to the magnitude seen in HIV-infected adults. CD8 responses were broadly directed at an average of 11 epitopes (range, 2 to 27 epitopes) and targeted nearly all HIV-1 proteins, with the highest proportion in Gag. Responses were readily detected even in those children with suppressed viremia on highly active antiretroviral therapy, although the breadth (P = 0.037) and the magnitude (P = 0.021) were significantly lower in these subjects. Each child recognized only a small minority of the HIV-1 optimal epitopes defined for his or her class I HLA alleles. Together, these data indicate that perinatally infected children who survive infancy mount a robust HIV-1-specific CD8 response that is much stronger than previously thought and is comparable in magnitude and breadth to that of adults. Moreover, this response has the potential to be broadened to target more epitopes, making these children attractive candidates for immunotherapeutic interventions.
Mounting evidence supports a central role for the cytotoxic-T-lymphocyte (CTL) response in restricting human immunodeficiency virus type 1 (HIV-1) replication in infected adults (8, 23, 37). Early studies of the HIV-1-specific CTL response among perinatally infected children indicated that these responses emerge later and are generally weaker and narrower than in their adult counterparts (9, 11, 25, 26, 30, 38, 40). However, these studies relied on techniques that are less sensitive than those currently available and that provide no information about the epitopes targeted or the overall breadth of response.
Viral dynamics after perinatal HIV-1 infection are quite distinct from those observed in horizontally infected adults. Acute HIV-1 infection in adults is characterized by a high peak viral load that rapidly declines during the months after infection to reach a relatively stable setpoint (3, 29, 32, 36). This decline in viremia temporally coincides with the emergence of the HIV-1-specific CTL response (7, 23). In contrast, vertically infected infants resolve their primary viremia much more slowly. The geometric mean viral load remains >100,000 RNA copies/ml throughout the first 3 years of life and only gradually declines to reach levels seen in horizontally infected adults at ca. 4 to 6 years of age (31, 33). HIV-1-specific CTL responses are quite rare among infected infants during the first 6 months of life and are thought to be weak and narrowly directed throughout the early childhood years (25, 26, 28, 38, 40).
The reasons for the relatively late emergence, low magnitude, and narrow breadth of the HIV-1-specific CTL response during infancy are not clear. The cellular immune response of infants differs from that of adults in ways that remain poorly understood. This maturational delay in the development of cell-mediated immunity may lead to a propensity for tolerization or skewing toward ineffective Th2-type responses (14, 44). It has also been demonstrated that transmission of maternal escape mutants may limit the epitopes available for targeting by the haploidentical child (19).
Little is known about the magnitude and breadth of pediatric CTL responses beyond infancy and early childhood. If tolerization, Th2 skewing, or elimination of potential epitopes from the infecting viral inoculum were to blame for the weak HIV-1-specific CTL activity seen in infants, these factors might be expected to permanently alter the child's virus-specific immune response and limit its effectiveness. An increasingly large proportion of HIV-1-infected children are now entering the second or third decade of life, due to the changing demographics of pediatric HIV-1 in the developed world (16, 43). Few data exist regarding the HIV-1-specific immune responses present in these perinatally infected children whose immune systems have matured in the presence of HIV-1.
Recently developed screening approaches now allow a comprehensive assessment of the magnitude and breadth of the HIV-1-specific CD8 response, using small numbers of cells which can be easily obtained from children (1). In order to better define the full magnitude, breadth, and epitope specificity of CTL activity in perinatally HIV-1-infected children, we conducted a comprehensive assessment of CD8 responses in 18 pediatric subjects by using two parallel approaches: genome-wide screening with a panel of overlapping peptides and screening for recognition of class I-restricted optimal epitopes previously defined in adults. These data offer the first comprehensive assessment of the total breadth of the CTL response at the epitope level in perinatally HIV-1-infected children.
MATERIALS AND METHODS
Study subjects.
Eighteen perinatally HIV-1-infected subjects were recruited through the outpatient HIV clinic at Children's Hospital in Boston (Table 1). Twelve children were receiving highly active antiretroviral therapy (HAART), four were receiving single or dual nucleoside analogues only, and two were receiving no antiviral therapy. The mean age of the cohort was 10.8 ± 2.9 years (range, 6 to 17 years). All subjects and/or legal guardians signed written informed consent prior to participation.
TABLE 1.
Characteristics of the study cohorta
| Subject | Age (yr) | Sex | Race | CD4 count | CD4 percent (%) | HIV RNA (copies/ml of plasma) | ARV therapy | Duration (mo)b |
|---|---|---|---|---|---|---|---|---|
| TCH-015 | 11 | F | Latino | 1,166 | 39 | 30 | HAART | 13 |
| TCH-027 | 11 | M | Cauc | 1,325 | 36 | <50 | HAART | 17 |
| TCH-060 | 11 | F | AA | 496 | 28 | <50 | HAART | 3 |
| TCH-061 | 17 | F | Cauc | 1,078 | 44 | <50 | HAART | 8 |
| TCH-063 | 9 | F | Latino | 992 | 41 | <50 | HAART | 54 |
| TCH-064 | 14 | M | Cauc | 780 | 23 | <50 | HAART | 13 |
| TCH-066 | 9 | F | Cauc/AA | 1,079 | 31 | <50 | DDI | 8 |
| TCH-067 | 10 | F | AA | 1,049 | 38 | <50 | HAART | 35 |
| TCH-073 | 10 | F | Cauc | 1,110 | 32 | <50 | HAART | 43 |
| TCH-080 | 10 | F | Cauc | 1,252 | 28 | <50 | HAART | 21 |
| TCH-014 | 14 | F | Cauc/AA | 828 | 36 | 70 | HAART | 8 |
| TCH-017 | 12 | F | AA | 563 | 28 | 830 | None | NA |
| TCH-043 | 9 | M | AA | 1,181 | 32 | 200 | AZT/DDI | 89 |
| TCH-045 | 8 | F | Haitian | 1,406 | 33 | 42,000 | None | NA |
| TCH-065 | 10 | F | AA | 961 | 46 | 120 | HAART | 56 |
| TCH-068 | 6 | F | Cauc | 874 | 23 | 79 | AZT/DDI | 21 |
| TCH-069 | 7 | F | AA | 2,272 | 26 | 3400 | AZT/3TC | NA |
| TCH-077 | 16 | M | Cauc | 432 | 24 | 13,000 | HAART | NA |
Age, sex, race, HIV RNA measurement, CD4 data, and treatment status are displayed for the 18 perinatally infected children comprising the study cohort. For subjects with undetectable viremia, the duration of viral suppression is expressed as the number of months since the viral load fell below 400 copies/ml, since many subjects did not have measurements obtained by using ultrasensitive assays. HAART regimens varied by subject, but all consisted of at least three drugs, including a protease inhibitor and/or a nonnucleoside reverse transcriptase inhibitor. F, female; M, male; Cauc, Caucasian; AA, African-American; ARV, antiretroviral; DDI, didauosine; AZT, zidovudine; 3TC, lamivudine; NA, not applicable.
That is, once the viral load fell below 400 copies/ml.
Isolation of PBMC.
Peripheral blood mononuclear cells (PBMC) were isolated from fresh whole blood by Ficoll-Hypaque (Sigma, St. Louis, Mo.) density gradient centrifugation. For confirmation of the CD8 dependence of responses, RosetteSep CD4 depletion cocktail was used according to the manufacturer's instructions (StemCell Technologies, Vancouver, British Columbia, Canada).
HLA typing.
HLA typing of class I loci was performed by using DNA PCR with sequence-specific primers at the Massachusetts General Hospital (MGH) Tissue Typing Laboratory.
Peptides tested.
A panel of 410 overlapping peptides (18mers with a 10-amino-acid overlap) spanning the clade B HIV-1 consensus sequence were synthesized for use in screening assays on an automated peptide synthesizer by using Fmoc (9-fluorenylmethoxy carbonyl) chemistry at the Peptide Core Facility at MGH. Previously described HIV-1 optimal epitopes (Los Alamos HIV Sequence Database [hiv-web.lanl.gov]) were synthesized by identical methods.
IFN-γ ELISPOT assay.
Fresh PBMC were plated in 100 μl of R10 medium at 50,000 or 100,000 cells/well in 96-well polyvinylidene difluoride-backed plates (Millipore, Bedford, Mass.), which had been precoated overnight with 0.5 μg of anti-IFN-γ MAb (Mabtech, Stockholm, Sweden)/ml. Peptides were added at a final concentration of 10 μg/ml, and plates were incubated overnight at 37°C and 5% CO2 and then processed by standard methods (17). Three negative control wells contained cells and media alone, and a positive control well contained phytohemagglutinin. Individual gamma interferon (IFN-γ)-secreting cells were counted by using the AID enzyme-linked immunospot assay (ELISPOT) reader system (Cell Technology, Inc.). Results were calculated as the number of spot-forming cells per million input cells (SFC/million) after subtraction of the background response (mean SFC of all no-antigen wells; in all cases, ≤20 SFC/million). A response was considered positive if it was both ≥50 SFC/million PBMC and >3 standard deviations above the average of the negative control wells.
Matrix screening and confirmation strategy.
To minimize the cell number required for comprehensive screening, we used a matrix approach that has been previously validated in adult cohorts studied in our laboratory (1). The 410 overlapping HIV-1 18mer peptides were pooled into five two-dimensional matrices such that each peptide was present in two different pools, and each pool contained between 7 and 11 peptides (Gag, 7 to 9 peptides; RT, 8 to 9 peptides; Nef/protease/integrase, 9 to 10 peptides; Vif/Vpr/Vpu/Rev/Tat, 8 to 9 peptides; Env, 10 to 11 peptides). The resulting 92 pools were plated at a final concentration of 10 μg/ml per peptide with 50,000 or 100,000 PBMC/well on a single 96-well plate; thus, only 5 to 10 × 106 cells were required to comprehensively screen all translated HIV proteins. Each peptide within the “positive” pools was then tested individually in a separate ELISPOT assay the following day by using cells that had been incubated overnight at 106 PBMC/ml of R10 (methods above). In a few cases where cell numbers were insufficient, the confirmatory assay was deferred until a subsequent blood draw and then performed with fresh PBMC. Thus, each positive response was confirmed twice, by means of the internal control afforded by the matrix, and then individually in a confirmatory assay. In three subjects, the CD8 dependence of positive responses was established by an additional reconfirmation assay using CD4-depleted PBMC.
Autologous viral sequencing.
The method of proviral DNA ampification and sequencing used has been described previously (19). Briefly, proviral DNA was extracted from PBMC by using the Puregene DNA isolation kit (Gentra). Seven external primer pairs were used to amplify the whole HIV-1 genome. PCR conditions were as follows: 5 min at 94°C; 40 cycles of 15 s at 94°C, 30 s at the indicated annealing temperature (range, 52 to 61°C), and 1 min at 72°C; and a final extension at 72°C for 7 min. Internal primer pairs were used in nested PCRs to yield clonable fragments. PCR primers for the different regions of HIV are as follows: Gag external (forward, 5′-AAATCTCTAGCAGTGGCGCC-3′; reverse, 5′-TGTTGGCTCTGGTCTGCTCT-3′; annealing temperature, 61°C), Gag internal (forward, 5′-ACTAGCGGAGGCTAGAA-3′; reverse, 5′-GCCACAATTGAAACACTT-3′; annealing temperature, 61°C), Gag-Pol external (forward, 5′-ATGATGACAGCATGTCAGGG-3′; reverse 5′-CCACTCAGGAATCCAGGTGG-3′; annealing temperature, 54°C), Gag-Pol internal (forward, 5′-GGAGGACCCGGACATAAAGCAAG-3′; reverse, 5′-TCCACCATGCTTCCCATGTTTC-3′; annealing temperature, 57°C), Pol external (forward, 5′-CTGAAAACAGGAAAATATGCAAG-3′; reverse, 5′-TACTTGCCACACAATCATCACC-3′; annealing temperature, 52°C), Pol internal (forward, 5′-GAGGGGTGCCCACACTAATGA-3′; reverse, 5′-CTTTTCTTCTTGGCACTACTTTTA-3′; annealing temperature, 53°C), Vpr external (forward, 5′-TTTGGAAAGGACCAGCAAAGC-3′; reverse, 5′-GCATGTGTGGCCCAAACATTAT-3′; annealing temperature, 52°C), Vpr internal (forward, 5′-TAAAAGTAGTGCCAAGAAGAAAAG-3′; reverse, 5′-GGTACCCCATAATAGATTGTGAC-3′; annealing temperature, 52°C), Vpu-Env external (forward, 5′-AGTGGCAATGAGAGTGAAGG-3′; reverse, 5′-TAGTAGCAGCCCTGTAATATTTGA-3′; annealing temperature, 52°C), Vpu-Env internal (forward, 5′-CTCCTTGGGATGTTGATGAT-3′; reverse, 5′-TGGGAGGGGCATACATTG-3′; annealing temperature, 50°C), Env external (forward, 5′-GGAGATATAAGACAAGCACATTG-3′; reverse, 5′-CCAATCTGGGAAGAAGCCTTG-3′; annealing temperature, 53°C), Env internal (forward, 5′-GTGGAGGGGAATTTTTCTACTG-3′; reverse, 5′-GGGAGTGAACTAGCCCTTCCA-3′; annealing temperature, 54°C), Nef external (forward, 5′-TTCCAGTCAGACCTCAGGTAC-3′; reverse, 5′-TCTAGTTACCAGAGTCACACAA-3′; annealing temperature, 53°C), and Nef internal (forward, 5′-CTTTTTAAAAGAAAAGGGGGGAC-3′; reverse, 5′-TCAGATCTGGTCTAACCAGAG-3′; annealing temperature, 52°C). PCR fragments were then gel purified and cloned by TopoTA (Invitrogen). Plasmid DNA was isolated by using the QiaPrep Turbo Miniprep system (Qiagen) and sequenced by using the ABI 3700 DNA analyzer from Applied Biosystems. A minimum of four clones from each region were sequenced. Sequencher (Gene Codes Corp.) was used to edit and align sequences.
Statistical analysis.
Data analysis was performed by using Stata Statistical Software (StataCorp, release 7.0; College Station, Tex.). The breadth of response was defined as the number of overlapping peptides recognized. This value followed a normal distribution and was compared between groups by using the Student t test for equal variances. The total magnitude of the response, obtained by summing all individual peptide responses, showed an abnormal distribution and was compared by using the Wilcoxon rank sum test. Correlations were performed by using linear regression for normally distributed variables and Spearman correlation for nonnormal continuous variables. All tests were two tailed, with a P of <0.05 considered significant.
RESULTS
Perinatally infected children mount a strong multispecific CD8 response that is comparable in breadth and magnitude to that of adults.
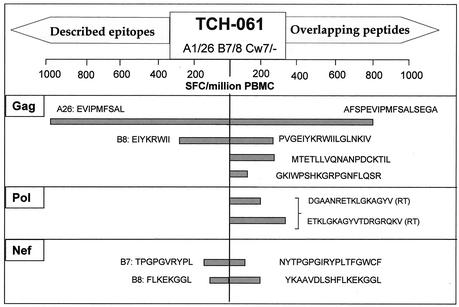
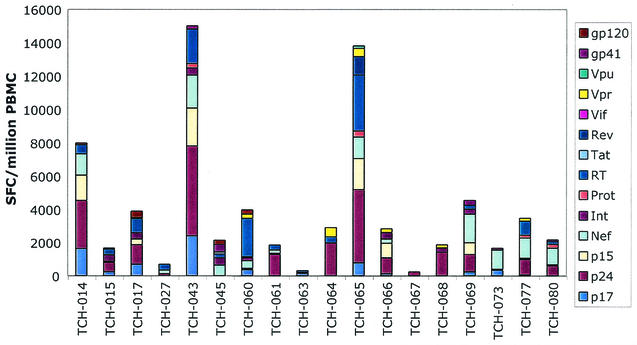
Prior studies of HIV-1-specific CTL activity in children largely relied on measurement of responses to vaccinia constructs expressing whole HIV-1 structural genes (10, 25-27, 35, 38, 40). Few studies have addressed pediatric CTL responses at the epitope level, and these were limited to assessment of only a few epitopes (27, 39, 41). We screened 18 perinatally infected children for T-cell responses to a panel of overlapping 18mer peptides spanning all translated regions of HIV-1. Each subject demonstrated measurable responses to multiple peptides. (An example of initial screening with overlapping peptides, as well as optimal epitopes known to be presented by the expressed class I alleles is shown in Fig. 1.) On average, subjects recognized 13 peptides (range, 2 to 37 peptides) of the 411 peptides tested. The total magnitude of the HIV-1-specific response, obtained by the addition of all positive peptide responses, varied greatly among the subjects, ranging from 230 to 16,580 SFC/million PBMC (Fig. 2). The median total magnitude was 3,000 SFC/million PBMC, indicating that 0.3% of the total PBMC population in these chronically HIV-infected children were specific for HIV-1. Expressed in terms of CD8+ input cells, the median total magnitude was 7,800 SFC/million CD8+ cells, or 0.78% of the total CD8+ population. These estimates of the magnitude and breadth are very similar to those obtained in chronically HIV-1-infected adults by using nearly identical methods in our laboratory (1). There was no correlation between age and the breadth (R2 = 0.0006; P = 0.93) or total magnitude (R2 = 0.004; P = 0.80) of the CTL response within this cohort. The CD8 dependence of positive responses was confirmed in three subjects by using CD4-depleted PBMC. All responses detected in these three individuals persisted after CD4 depletion, suggesting that the majority of responses detected by our screening approach are CD8 mediated.
FIG. 1.
Comprehensive CTL screening and testing of optimal epitopes. Data for one representative subject (TCH-061) are shown, with responses to previously described optimal epitopes shown on the left and responses to the corresponding overlapping 18mer on the right. Brackets indicate adjacent peptides that overlap. In this subject, only four responses were detected by using previously defined optimal epitopes, whereas each of these plus an additional four responses were detected by comprehensive screening with overlapping peptides.
FIG. 2.
Magnitude of total CTL response by protein. The total magnitude of the CTL response detected by comprehensive screening with overlapping peptides is shown for each subject as the number of SFC/million PBMC obtained by summing all positive 18mer responses. (Where adjacent peptides are recognized, the lower magnitude response is excluded). The stacked bars indicate the breakdown of the response among the 14 HIV-1 protein subunits.
The use of overlapping peptides as a screening tool could potentially underestimate the true number of targeted epitopes, as a single 18mer peptide may contain more than one epitope. Conversely, a single viral epitope may yield two positive peptide responses if it lies in the area of overlap between two adjacent peptides, resulting in an overestimation of the true number of targeted epitopes. To correct for this potential overestimation of breadth, a separate analysis was performed in which the lower magnitude response of adjacent positive peptides was discarded, yielding a minimal estimate of the number of recognized epitopes. In this adjusted analysis, subjects targeted an average of 11 regions (range, 2 to 27), with a median total magnitude of 2,500 SFC/million PBMC (range, 230 to 15,020). Therefore, a minimal estimate of the median total HIV-specific CTL response is 0.25% of PBMC (or 0.67% of CD8+ T cells).
CTL activity is broadly directed at nearly all HIV-1 proteins and protein subunits.
Our comprehensive screening strategy allowed us to assess for the first time the distribution of immune pressure throughout the viral genome in children. The wide distribution of CD8 responses among the 14 expressed HIV-1 gene products is shown in Fig. 3. With the exception of Vif, each protein or protein subunit was targeted by at least one subject. The median number of protein subunits recognized by an individual subject was six. The subject with the narrowest response (TCH-067) recognized only two peptides, both within p24 Gag, whereas the subject with the broadest response (TCH-065) recognized 9 of the 14 HIV-1 protein subunits.
FIG. 3.
Breadth of CD8 T-cell responses to HIV-1 proteins and protein subunits. (A) Percentage of subjects recognizing at least one peptide within each of the 14 HIV-1 proteins or protein subunits; (B) frequency of recognition adjusted for protein length (percentage of subjects recognizing each protein divided by its length in amino acids); (C) relative contribution of each protein (or subunit) to the total number of responses detected by comprehensive screening.
The most frequently recognized protein subunits were p24 Gag and RT (each targeted by 78% of subjects), followed by Nef (72%) (Fig. 3A). However, the highest density of responses (assessed by dividing the frequency of recognition of a protein by its length) was in p17 Gag, followed closely by p15 Gag and Vpr (Fig. 3B). With the exception of Vpr, recognized by 39% of subjects, the regulatory and accessory proteins were infrequently targeted. In particular, the early expressed proteins Tat and Rev were each recognized by only one of the 18 subjects (5.6%). The p24 subunit of Gag was the most heavily targeted region in terms of both the total number of responses and the total magnitude of responses, followed by Nef and RT (Fig. 3c).
CTL breadth and magnitude are greater in children with detectable viremia.
It has been demonstrated in adults that viral suppression mediated by antiviral therapy results in a decrease in the magnitude of CTL responses (4, 36). Reflecting the high prevalence of HAART in current clinical practice in Boston, 10 of our study subjects (56%) had HIV RNA levels of <50 copies/ml. Consistent with published data from adult cohorts (4, 36), the responses in the viremic group were both broader (mean, 18.1 versus 9.5 peptides recognized; P = 0.037) and of greater total magnitude (median, 5,600 versus 2,200 SFC/million; P = 0.021) than in children with undetectable viremia (Fig. 4). Among the eight subjects with measurable viremia, there was no statistical correlation between viral load and total CTL magnitude or breadth. Interestingly, the two subjects with the broadest and strongest responses (TCH-043 and TCH-065) had both maintained undetectable viremia for many years (7.5 and 4.7 years) before experiencing a small viral blip (200 and 120 RNA copies/ml, respectively) at the time point under study. When analyzed by current treatment status (HAART, nucleosides only, or no therapy), there was no significant difference in the magnitude (P = 0.44) or breadth (P = 0.21) of response among the three groups (Kruskal-Wallis test), suggesting that the impact of therapy on CTL responses is predominantly mediated through reduction in viral load.
FIG. 4.
Magnitude and breadth of response are higher in subjects with detectable viremia. The breadth (A) and total magnitude (B) of response are compared between subjects with detectable viremia (>50 RNA copies/ml; n = 8) and nondetectable viremia (<50 RNA copies/ml; n = 10).
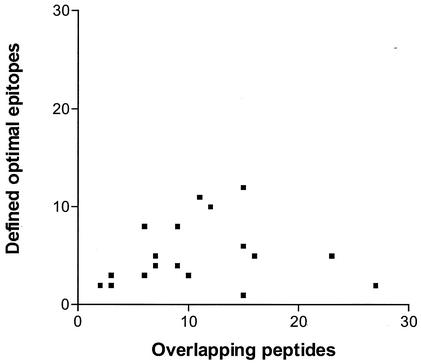
Testing of previously defined class I HLA optimal epitopes underestimates the total CD8 response.
Many HLA class I-restricted HIV-1 optimal epitopes have been defined in adults with HIV infection (http://hiv-web.lanl.gov). Each subject in our cohort was screened for recognition of all previously described optimal epitopes known to be presented by his or her class I HLA molecules (median of 25 optimal epitopes tested; range, 5 to 37). The median number of optimal peptides recognized by each subject was 5, and the median summed magnitude of all optimal peptide responses was 1,385 SFC/million PBMC. In all subjects except for one, comprehensive screening detected responses that would have been missed by screening for optimal epitopes alone (Fig. 5). In the most striking instance, subject TCH-065 recognized only two previously described optimal epitopes for a total response of 220 SFC/million PBMC, whereas comprehensive screening revealed 27 distinct responses (with responses to adjacent peptides counted only once) for a total magnitude of 13,820 SFC/million PBMC. Thus, assessment limited to optimal epitopes alone would have underestimated the breadth of this subject's response by at least 93% and the magnitude by at least 98%. This bias toward underestimation of the CTL response using optimal epitopes is likely to be greater among individuals with rarer HLA alleles that have not been well studied, including many alleles common in racial minority groups.
FIG. 5.
Comprehensive screening detects many responses that would be missed if screening for optimals only. Scatter plot display of the relationship between the entire breadth of response to all HIV-1 proteins detected by comprehensive screening (x axis) and the number of responses that would have been detected by screening for the recognition of previously defined optimal epitopes only (y axis).
Autologous sequence variation does not explain the failure to target all potential epitopes.
No subject mounted a detectable IFN-γ response to all of the optimal HIV-1 epitopes described for his or her HLA class I alleles. On average, subjects recognized 20% of the optimal peptides tested (range, 7 to 39%). This suggests that CTL responses in these subjects could theoretically be broadened. One potential reason for the failure to target optimal epitopes of appropriate class I HLA restriction is that the autologous viral isolate may differ in sequence from that of the synthetic peptide tested. Viral sequencing performed in two subjects revealed that sequence variation does not on its own explain such “failures” (Table 2). In subjects TCH-017 and TCH-066, viral sequencing of 20 unrecognized epitopes (i.e., those that failed to elicit a response despite being of the appropriate HLA class I restriction) revealed that in 14 cases the autologous virus was identical in sequence to the described optimal epitope used in the assay. It therefore appears that failure to recognize an appropriate class I-restricted optimal epitope cannot be explained by variations in the autologous sequence alone.
TABLE 2.
Unrecognized epitopes are predominantly consensus sequencea
| Protein | Epitope | Autologous sequence (no. of clones/total) | Predominant sequence type |
|---|---|---|---|
| Gag | SLYNTVATL | --F------(17/17) | Variant |
| ELRSLYNTV | --K------ (17/17) | Variant | |
| SPRTLNAWV | --------- (16/16) | Consensus | |
| TPQDLNTML | ---------(17/17) | Consensus | |
| GPGHKARVL | ---------(16/17) | Consensus | |
| GPGHKARVL | ----I---- (1/17) | ||
| HPVHAGPIA | ---------(17/17) | Consensus | |
| DCKTILKAL | ---------(17/17) | Consensus | |
| RFAVNPGLL | --------- (8/8) | Consensus | |
| RDYVDRFYKTL | --------- (8/8) | Consensus | |
| DYVDRFYKTL | --------- (8/8) | Consensus | |
| QASQEVKNW | ----D---- (7/7) | Variant | |
| FLGKIWPSYK | --------H- (5/6) | Variant | |
| FLGKIWPSYK | -----R--H- (1/6) | ||
| Nef | PLTFGWCYKL | -------F-- (4/5) | Variant |
| PLTFGWCYKL | ---------- (1/5) | ||
| VLEWRFDSRL | --V-K---M- (2/5) | Variant | |
| VLEWRFDSRL | --V-K---K- (2/5) | ||
| VLEWRFDSRL | ---------- (1/5) | ||
| Pol | ALVEICTEM | --------- (3/5) | Consensus |
| ALVEICTEM | ---G----- (1/5) | ||
| ALVEICTEM | --------L (1/5) | ||
| VIYQYMDDL | --------- (5/5) | Consensus | |
| ILKEPVHGV | --------- (5/5) | Consensus | |
| ITLWQRPLV | --------- (5/5) | Consensus | |
| DTVLEEMNL | --------- (3/5) | Consensus | |
| DTVLEEMNL | -----D--- (2/5) | ||
| Vpr | AIIRILQQL | -LV-----M (2/4) | Variant |
| AIIRILQQL | --L------ (1/4) |
In subjects TCH-017 and TCH-066, 20 previously described optimal HIV-1 epitopes were unrecognized despite having the appropriate HLA class I restriction. The viral sequencing of isolates from these subjects is shown. The predominant viral sequence within 14 of these 20 unrecognized epitopes was identical to that of the described optimal epitope used in the assay.
DISCUSSION
Virus-specific CTL responses appear to play a critical role in the containment of HIV-1 in adults (7, 23) and simian immunodeficiency virus in primates (5, 21, 37), but a detailed characterization of this response has not been performed in perinatally HIV-infected children. Using a comprehensive set of overlapping HIV peptides in an IFN-γ ELISPOT assay, we found that most children mount a broad and vigorous CTL response targeting epitopes in multiple viral proteins, even when viremia is fully suppressed by HAART. These findings contrast with prior studies of the HIV-1-specific immune response in young perinatally infected children; in those earlier studies the responses were weak and narrowly directed. Our data indicate that HIV-1-specific CD8 responses in late childhood are similar in both magnitude and breadth to those of adults.
Previous studies of pediatric CTL responses have been constrained by the limited sample volumes that can be obtained from children and by assays that required large cell numbers. Because of such limitations, earlier assessments of HIV-1-specific CTL activity in children largely relied upon the measurement of responses to vaccinia constructs expressing whole HIV-1 genes (10, 25-27, 35, 38, 40). This approach enabled investigators to determine which of the major structural proteins were recognized but could not give an accurate picture of the breadth of the response or identify the epitopes targeted. The few studies that measured epitope-specific responses assessed only a few epitopes (27, 39, 41). Our comprehensive screening strategy represents a significant methodological advance in the study of pediatric T-cell-mediated immune responses and should prove useful for the study of other viruses as well. Using a highly sensitive assay that is able to detect peptide-specific cells at frequencies as low as 0.005% of PBMC, we were able to perform a comprehensive screen of all translated viral proteins, with relatively small numbers of PBMC. Because responses were found to be distributed throughout the viral genome, prior assessments that were limited to select HIV-1 proteins almost certainly underestimated the total virus-specific response. Importantly, our approach also overcomes the bias inherent in screening for recognition of previously defined optimal peptides. The ability to comprehensively assess responses throughout the genome in a manner that is not dependent on prior definition of class I optimal epitopes is particularly valuable in children, since the pediatric epidemic is dominated by racial minorities for whom fewer HLA-restricted epitopes have been defined.
Most prior studies of perinatally infected children found HIV-specific CTL responses to be weak and narrowly directed (25-28, 38, 40, 41). These earlier studies, which focused largely on infants and young children, indicated that CTL responses are infrequent among infants younger than 6 months of age (25, 26) and remain weak and narrowly directed throughout the early childhood years (26, 40, 41). The most comprehensive assessment to date that has included older children found the average total HIV-1-specific IFN-γ response (sum of responses to vaccinia constructs expressing Env, Gag, Pol, and Nef) to be only 522 SFC/million PBMC among a cohort with a mean age of 8.1 years (41). In contrast, we measured a much higher median HIV-1-specific response of 2,500 SFC/million PBMC, despite the fact that most subjects were on antiviral therapy with low viral loads. This estimate is remarkably similar to the recently reported median value of 2,568 SFC/million PBMC obtained by similar methods among chronically HIV-1-infected adults on therapy (1). The discrepancy between our findings and earlier reports of deficient HIV-1-specific CTL in children may to some extent reflect the greater sensitivity of our assay and the comprehensive nature of our screening approach. Alternatively, it may reflect the different age composition of the cohorts and indicate a true biological difference between CTL responses in early and late childhood. If CTL responses are indeed late to emerge, this delay may help to explain the prolonged primary viremia of infants relative to adults, in whom the CTL response is brisk. Longitudinal data are needed to clarify timing of CTL emergence in relation to both age and viral load decline, as well as the progressive maturation and broadening of the CTL response over time. It will also be important to understand what additional factors, such as virus-specific T-helper responses (2, 22), might serve as prerequisites for development of a fully mature adult-like CTL response. As vaccine development efforts move forward, it will be critical to elucidate the barriers to development of mature T-cell responses in order to achieve immunogenicity in infants.
Differences in technical approach may explain some of the discrepancy between the high prevalence of strong responses detected in our cohort and the relatively weak responses reported in prior studies. The ELISPOT assay used in the present study is highly sensitive for the detection of IFN-γ secretion but does not measure the cytolytic function of CD8 cells, whereas prior studies have measured pediatric CTL responses by using limiting-dilution assays (LDAs) and direct cytotoxicity assays (10, 24, 26, 28, 35, 41). It is possible that a proportion of the IFN-γ-secreting cells measured in our assay lack cytolytic function, although prior studies comparing tetramer-staining, IFN-γ secretion, and LDAs in HIV-infected children and adults have found excellent correlation between all three modalities; the majority of IFN-γ-positive cells can be demonstrated to possess cytolytic function, although the sensitivity of the LDA is significantly lower (20). Our assay system also differed from earlier pediatric studies in that we used peptide-pulsed cells as targets, which may bypass the requirement for intracellular processing prior to presentation, unlike ELISPOT assays which employ vaccinia vector targets (41, 42; Z. A. Scott, E. G. Chadwick, M. D. Catalina, M. McManus, R. Yogev, P. Palumbo, P. Britto, J. L. Sullivan, and K. Luzuriaga, unpublished data). Finally, our use of unfractionated PBMC in the IFN-γ ELISPOT may theoretically lead to the detection of some CD4-mediated responses as well as CD8-mediated responses, although in the three subjects for whom depletion assays were performed, no such responses were detected.
It is possible that the high prevalence of strong CTL responses detected in the present study may be due in part to a “survivor bias” within this cohort of older children, which might occur if strong HIV-1-specific immune responses are disproportionately frequent among those who survive early childhood. However, the average age of the study cohort (10.8 years) is very similar to the average age of the entire clinic population from which the subjects were recruited (11.6 years, n = 140). Therefore, it appears that the older age of our cohort reflects the current epidemiology of pediatric HIV infection. Also, the majority of the subjects in the present study began antiretroviral therapy during early childhood (at a median age of 18 months), so the survival of many of these children is likely attributable in part to drug therapy. Because most children in our cohort had a relatively high CD4 count and low viral load, our findings may not be extendable to children with declining CD4 counts and advanced disease.
Studies of HIV-1-infected adults suggest that the interplay between CTL magnitude and the level of HIV viremia is complex. While some studies have detected an inverse correlation between viral load and epitope-specific responses (34), subsequent studies have found no statistical relationship between viral load and CTL magnitude (1, 6), and one recent pediatric study found a positive correlation between viral load and certain A2-restricted responses (12). In agreement with two published adult studies that analyzed responses throughout the HIV-1 genome, we found no statistical correlation between viral load and the total magnitude or breadth of the HIV-1-specific response (1, 6). Our data also support the observation made in adults that HAART-mediated viral suppression is associated with a lower magnitude of CTL response (1, 4, 18), though in our cohort these responses remained readily detectable even in those with full viral suppression. Among viremic subjects we found no statistical correlation between CTL and viral load although, interestingly, the strongest responses were seen in two subjects experiencing viral “blips” after many years of suppression.
Despite the vigorous CTL activity detected in the majority of the children studied, each child recognized only a minority of the epitopes defined for his or her HLA alleles. In the majority of cases, this could not be explained by transmission of escape mutations from the mother or by prior escape in the child, as autologous viral sequencing revealed that most of these unrecognized potential epitopes lacked mutations. This failure to recognize all potential HLA-restricted epitopes suggests that the CTL response could theoretically be broadened in these subjects through therapeutic vaccination or other immunomodulatory strategies. Children may be particularly attractive candidates for such interventions due to their relatively preserved thymopoiesis (13) and greater proportion of naive CD45RA+ cells after the initiation of HAART (15).
Antiretroviral interventions to reduce mother-to-child transmission and HAART therapy have dramatically shifted the epidemiology of pediatric HIV in the United States. As more perinatally HIV-infected children survive into the second and third decades of life, new approaches that are complementary to HAART, such as therapeutic vaccination, may provide the best hope for long-term management of HIV-1 infection. It is encouraging that perinatally infected children are capable of mounting a broad and vigorous HIV-specific immune response.
Acknowledgments
We thank all study participants, their families, and the dedicated clinical research staff at Children's Hospital in Boston, including Rosemary Galvin, Nancy Karthas, Catherine Kneut, Lynne Lewis, and Ken Gilmartin.
This study was supported by the National Institutes of Health (AI52078, AI28568, AI46995) (P.J.R.G., M.E.F., and B.D.W.), the Elizabeth Glaser Pediatric AIDS Foundation (M.E.F. and P.J.R.G.), the Scholars in Clinical Science Program at Harvard Medical School (K30 HL04095), The Wellcome Trust (P.J.R.G.), the Howard Hughes Medical Institute (B.D.W.), and the Partners/Fenway/Shattuck Center for AIDS Research. P.J.R.G. is an Elizabeth Glaser Scientist of the Elizabeth Glaser Pediatric AIDS Foundation. B.D.W. is the recipient of a Doris Duke Distinguished Clinical Scientist Award.
REFERENCES
- 1.Addo, M. M., X. G. Yu, A. Rathod, D. Cohen, R. L. Eldridge, D. Strick, M. N. Johnston, C. Corcoran, A. G. Wurcel, C. A. Fitzpatrick, M. E. Feeney, W. R. Rodriguez, N. Basgoz, R. Draenert, D. R. Stone, C. Brander, P. J. R. Goulder, E. S. Rosenberg, M. Altfeld, and B. D. Walker. 2003. Comprehensive epitope analysis of HIV-1-specific T-cell responses directed against the entire expressed HIV-1 genome demonstrate broadly directed responses, but no correlation to viral load. J. Virol. 77:2081-2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altfeld, M., and E. S. Rosenberg. 2000. The role of CD4+ T helper cells in the cytotoxic T lymphocyte response to HIV-1. Curr. Opin. Immunol. 12:375-380. [DOI] [PubMed] [Google Scholar]
- 3.Altfeld, M., E. S. Rosenberg, R. Shankarappa, J. S. Mukherjee, F. M. Hecht, R. L. Eldridge, M. M. Addo, S. H. Poon, M. N. Phillips, G. K. Robbins, P. E. Sax, S. Boswell, J. O. Kahn, C. Brander, P. J. Goulder, J. A. Levy, J. I. Mullins, and B. D. Walker. 2001. Cellular immune responses and viral diversity in individuals treated during acute and early HIV-1 infection. J. Exp. Med. 193:169-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altfeld, M., J. van Lunzen, N. Frahm, X. G. Yu, C. Schneider, R. L. Eldridge, M. E. Feeney, D. Meyer-Olson, H. J. Stellbrink, and B. D. Walker. 2002. Expansion of pre-existing, lymph node-localized CD8+ T cells during supervised treatment interruptions in chronic HIV-1 infection. J. Clin. Investig. 109:837-843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barouch, D. H., J. Kunstman, M. J. Kuroda, J. E. Schmitz, S. Santra, F. W. Peyerl, G. R. Krivulka, K. Beaudry, M. A. Lifton, D. A. Gorgone, D. C. Montefiori, M. G. Lewis, S. M. Wolinsky, and N. L. Letvin. 2002. Eventual AIDS vaccine failure in a rhesus monkey by viral escape from cytotoxic T lymphocytes. Nature 415:335-339. [DOI] [PubMed] [Google Scholar]
- 6.Betts, M. R., D. R. Ambrozak, D. C. Douek, S. Bonhoeffer, J. M. Brenchley, J. P. Casazza, R. A. Koup, and L. J. Picker. 2001. Analysis of total human immunodeficiency virus (HIV)-specific CD4+ and CD8+ T-cell responses: relationship to viral load in untreated HIV infection. J. Virol. 75:11983-11991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borrow, P., H. Lewicki, B. H. Hahn, G. M. Shaw, and M. B. Oldstone. 1994. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68:6103-6110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borrow, P., H. Lewicki, X. Wei, M. S. Horwitz, N. Peffer, H. Meyers, J. A. Nelson, J. E. Gairin, B. H. Hahn, M. B. Oldstone, and G. M. Shaw. 1997. Antiviral pressure exerted by HIV-1-specific cytotoxic T lymphocytes (CTLs) during primary infection demonstrated by rapid selection of CTL escape virus. Nat. Med. 3:205-211. [DOI] [PubMed] [Google Scholar]
- 9.Buseyne, F., S. Blanche, D. Schmitt, C. Griscelli, and Y. Riviere. 1993. Detection of HIV-specific cell-mediated cytotoxicity in the peripheral blood from infected children. J. Immunol. 150:3569-3581. [PubMed] [Google Scholar]
- 10.Buseyne, F., M. Burgard, J. P. Teglas, E. Bui, C. Rouzioux, M. J. Mayaux, S. Blanche, and Y. Riviere. 1998. Early HIV-specific cytotoxic T lymphocytes and disease progression in children born to HIV-infected mothers. AIDS Res. Hum. Retrovir. 14:1435-1444. [DOI] [PubMed] [Google Scholar]
- 11.Buseyne, F., M. L. Chaix, B. Fleury, O. Manigard, M. Burgard, S. Blanche, C. Rouzioux, and Y. Riviere. 1998. Cross-clade-specific cytotoxic T lymphocytes in HIV-1-infected children. Virology 250:316-324. [DOI] [PubMed] [Google Scholar]
- 12.Buseyne, F., D. Scott-Algara, F. Porrot, B. Corre, N. Bellal, M. Burgard, C. Rouzioux, S. Blanche, and Y. Riviere. 2002. Frequencies of ex vivo-activated human immunodeficiency virus type 1-specific gamma-interferon-producing CD8+ T cells in infected children correlate positively with plasma viral load. J. Virol. 76:12414-12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Douek, D. C., R. D. McFarland, P. H. Keiser, E. A. Gage, J. M. Massey, B. F. Haynes, M. A. Polis, A. T. Haase, M. B. Feinberg, J. L. Sullivan, B. D. Jamieson, J. A. Zack, L. J. Picker, and R. A. Koup. 1998. Changes in thymic function with age and during the treatment of HIV infection. Nature 396:690-695. [DOI] [PubMed] [Google Scholar]
- 14.Forsthuber, T., H. C. Yip, and P. V. Lehmann. 1996. Induction of Th1 and Th2 immunity in neonatal mice. Science 271:1728-1730. [DOI] [PubMed] [Google Scholar]
- 15.Gibb, D. M., A. Newberry, N. Klein, A. de Rossi, I. Grosch-Woerner, and A. Babiker. 2000. Immune repopulation after HAART in previously untreated HIV-1-infected children. Lancet 355:1331-1332. [DOI] [PubMed] [Google Scholar]
- 16.Gortmaker, S. L., M. Hughes, J. Cervia, M. Brady, G. M. Johnson, G. R. Seage III, L. Y. Song, W. M. Dankner, and J. M. Oleske. 2001. Effect of combination therapy including protease inhibitors on mortality among children and adolescents infected with HIV-1. N. Engl. J. Med. 345:1522-1528. [DOI] [PubMed] [Google Scholar]
- 17.Goulder, P. J., M. M. Addo, M. A. Altfeld, E. S. Rosenberg, Y. Tang, U. Govender, N. Mngqundaniso, K. Annamalai, T. U. Vogel, M. Hammond, M. Bunce, H. M. Coovadia, and B. D. Walker. 2001. Rapid definition of five novel HLA-A*3002-restricted human immunodeficiency virus-specific cytotoxic T-lymphocyte epitopes by elispot and intracellular cytokine staining assays. J. Virol. 75:1339-1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goulder, P. J., M. A. Altfeld, E. S. Rosenberg, T. Nguyen, Y. Tang, R. L. Eldridge, M. M. Addo, S. He, J. S. Mukherjee, M. N. Phillips, M. Bunce, S. A. Kalams, R. P. Sekaly, B. D. Walker, and C. Brander. 2001. Substantial differences in specificity of HIV-specific cytotoxic T cells in acute and chronic HIV infection. J. Exp. Med. 193:181-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goulder, P. J., C. Brander, Y. Tang, C. Tremblay, R. A. Colbert, M. M. Addo, E. S. Rosenberg, T. Nguyen, R. Allen, A. Trocha, M. Altfeld, S. He, M. Bunce, R. Funkhouser, S. I. Pelton, S. K. Burchett, K. McIntosh, B. T. Korber, and B. D. Walker. 2001. Evolution and transmission of stable CTL escape mutations in HIV infection. Nature 412:334-338. [DOI] [PubMed] [Google Scholar]
- 20.Goulder, P. J., Y. Tang, C. Brander, M. R. Betts, M. Altfeld, K. Annamalai, A. Trocha, S. He, E. S. Rosenberg, G. Ogg, C. A. O'Callaghan, S. A. Kalams, R. E. McKinney, Jr., K. Mayer, R. A. Koup, S. I. Pelton, S. K. Burchett, K. McIntosh, and B. D. Walker. 2000. Functionally inert HIV-specific cytotoxic T lymphocytes do not play a major role in chronically infected adults and children. J. Exp. Med. 192:1819-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jin, X., D. E. Bauer, S. E. Tuttleton, S. Lewin, A. Gettie, J. Blanchard, C. E. Irwin, J. T. Safrit, J. Mittler, L. Weinberger, L. G. Kostrikis, L. Zhang, A. S. Perelson, and D. D. Ho. 1999. Dramatic rise in plasma viremia after CD8+ T-cell depletion in simian immunodeficiency virus-infected macaques. J. Exp. Med. 189:991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalams, S. A., S. P. Buchbinder, E. S. Rosenberg, J. M. Billingsley, D. S. Colbert, N. G. Jones, A. K. Shea, A. K. Trocha, and B. D. Walker. 1999. Association between virus-specific cytotoxic T-lymphocyte and helper responses in human immunodeficiency virus type 1 infection. J. Virol. 73:6715-6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koup, R. A., J. T. Safrit, Y. Cao, C. A. Andrews, G. McLeod, W. Borkowsky, C. Farthing, and D. D. Ho. 1994. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68:4650-4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luzuriaga, K., Y. Bryson, P. Krogstad, J. Robinson, B. Stechenberg, M. Lamson, S. Cort, and J. L. Sullivan. 1997. Combination treatment with zidovudine, didanosine, and nevirapine in infants with human immunodeficiency virus type 1 infection. N. Engl. J. Med. 336:1343-1349. [DOI] [PubMed] [Google Scholar]
- 25.Luzuriaga, K., D. Holmes, A. Hereema, J. Wong, D. L. Panicali, and J. L. Sullivan. 1995. HIV-1-specific cytotoxic T lymphocyte responses in the first year of life. J. Immunology 154:433-443. [PubMed] [Google Scholar]
- 26.Luzuriaga, K., R. A. Koup, C. A. Pikora, D. B. Brettler, and J. L. Sullivan. 1991. Deficient human immunodeficiency virus type 1-specific cytotoxic T-cell responses in vertically infected children. J. Pediatr. 119:230-236. [DOI] [PubMed] [Google Scholar]
- 27.Luzuriaga, K., M. McManus, M. Catalina, S. Mayack, M. Sharkey, M. Stevenson, and J. L. Sullivan. 2000. Early therapy of vertical human immunodeficiency virus type 1 (HIV-1) infection: control of viral replication and absence of persistent HIV-1-specific immune responses. J. Virol. 74:6984-6991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luzuriaga, K., P. McQuilken, A. Alimenti, M. Somasundaran, R. Hesselton, and J. L. Sullivan. 1993. Early viremia and immune responses in vertical human immunodeficiency virus type 1 infection. J. Infect. Dis. 167:1008-1013. [DOI] [PubMed] [Google Scholar]
- 29.Lyles, R. H., A. Munoz, T. E. Yamashita, H. Bazmi, R. Detels, C. R. Rinaldo, J. B. Margolick, J. P. Phair, and J. W. Mellors. 2000. Natural history of human immunodeficiency virus type 1 viremia after seroconversion and proximal to AIDS in a large cohort of homosexual men. J. Infect. Dis. 181:872-880. [DOI] [PubMed] [Google Scholar]
- 30.McFarland, E. J., P. A. Harding, D. Luckey, B. Conway, R. K. Young, and D. R. Kuritzkes. 1994. High frequency of Gag- and envelope-specific cytotoxic T lymphocyte precursors in children with vertically acquired human immunodeficiency virus type 1 infection. J. Infect. Dis. 170:766-774. [DOI] [PubMed] [Google Scholar]
- 31.McIntosh, K., A. Shevitz, D. Zaknun, J. Kornegay, P. Chatis, N. Karthas, and S. K. Burchett. 1996. Age- and time-related changes in extracellular viral load in children vertically infected by human immunodeficiency virus. Pediatr. Infect. Dis. J. 15:1087-1091. [DOI] [PubMed] [Google Scholar]
- 32.Mellors, J. W., C. R. Rinaldo, Jr., P. Gupta, R. M. White, J. A. Todd, and L. A. Kingsley. 1996. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science 272:1167-1170. [DOI] [PubMed] [Google Scholar]
- 33.Mofenson, L. M., J. Korelitz, W. A. Meyer III, J. Bethel, K. Rich, S. Pahwa, J. Moye, Jr., R. Nugent, J. Read, et al. 1997. The relationship between serum human immunodeficiency virus type 1 (HIV-1) RNA level, CD4 lymphocyte percent, and long-term mortality risk in HIV-1-infected children. J. Infect. Dis. 175:1029-1038. [DOI] [PubMed] [Google Scholar]
- 34.Ogg, G. S., X. Jin, S. Bonhoeffer, P. R. Dunbar, M. A. Nowak, S. Monard, J. P. Segal, Y. Cao, S. L. Rowland-Jones, V. Cerundolo, A. Hurley, M. Markowitz, D. D. Ho, D. F. Nixon, and A. J. McMichael. 1998. Quantitation of HIV-1-specific cytotoxic T lymphocytes and plasma load of viral RNA. Science 279:2103-2106. [DOI] [PubMed] [Google Scholar]
- 35.Pikora, C. A., J. L. Sullivan, D. Panicali, and K. Luzuriaga. 1997. Early HIV-1 envelope-specific cytotoxic T lymphocyte responses in vertically infected infants. J. Exp. Med. 185:1153-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenberg, E. S., M. Altfeld, S. H. Poon, M. N. Phillips, B. M. Wilkes, R. L. Eldridge, G. K. Robbins, R. T. D'Aquila, P. J. Goulder, and B. D. Walker. 2000. Immune control of HIV-1 after early treatment of acute infection. Nature 407:523-526. [DOI] [PubMed] [Google Scholar]
- 37.Schmitz, J. E., M. J. Kuroda, S. Santra, V. G. Sasseville, M. A. Simon, M. A. Lifton, P. Racz, K. Tenner-Racz, M. Dalesandro, B. J. Scallon, J. Ghrayeb, M. A. Forman, D. C. Montefiori, E. P. Rieber, N. L. Letvin, and K. A. Reimann. 1999. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283:857-860. [DOI] [PubMed] [Google Scholar]
- 38.Scott, Z. A., E. G. Chadwick, L. L. Gibson, M. D. Catalina, M. M. McManus, R. Yogev, P. Palumbo, J. L. Sullivan, P. Britto, H. Gay, and K. Luzuriaga. 2001. Infrequent detection of HIV-1-specific, but not cytomegalovirus-specific, CD8+ T-cell responses in young HIV-1-infected infants. J. Immunol. 167:7134-7140. [DOI] [PubMed] [Google Scholar]
- 39.Scott-Algara, D., F. Buseyne, S. Blanche, C. Rouzioux, C. Jouanne, F. Romagne, and Y. Riviere. 2001. Frequency and phenotyping of human immunodeficiency virus (HIV)-specific CD8+ T cells in HIV-infected children, using major histocompatibility complex class I peptide tetramers. J. Infect. Dis. 183:1565-1573. [DOI] [PubMed] [Google Scholar]
- 40.Spiegel, H. M., R. Chandwani, M. E. Sheehy, J. Dobroszycki, G. Fennelly, A. Wiznia, J. Radding, M. Rigaud, H. Pollack, W. Borkowsky, M. Rosenberg, and D. F. Nixon. 2000. The impact of early initiation of highly active antiretroviral therapy on the human immunodeficiency virus type 1-specific CD8 T-cell response in children. J. Infect. Dis. 182:88-95. [DOI] [PubMed] [Google Scholar]
- 41.Spiegel, H. M., E. DeFalcon, G. S. Ogg, M. Larsson, T. J. Beadle, P. Tao, A. J. McMichael, N. Bhardwaj, C. O'Callaghan, W. I. Cox, K. Krasinski, H. Pollack, W. Borkowsky, and D. F. Nixon. 1999. Changes in frequency of HIV-1-specific cytotoxic T-cell precursors and circulating effectors after combination antiretroviral therapy in children. J. Infect. Dis. 180:359-368. [DOI] [PubMed] [Google Scholar]
- 42.Spiegel, H. M., G. S. Ogg, E. DeFalcon, M. E. Sheehy, S. Monard, P. A. Haslett, G. Gillespie, S. M. Donahoe, H. Pollack, W. Borkowsky, A. J. McMichael, and D. F. Nixon. 2000. Human immunodeficiency virus type 1- and cytomegalovirus-specific cytotoxic T lymphocytes can persist at high frequency for prolonged periods in the absence of circulating peripheral CD4+ T cells. J. Virol. 74:1018-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sullivan, J. L., and K. Luzuriaga. 2001. The changing face of pediatric HIV-1 infection. N. Engl. J. Med. 345:1568-1569. [DOI] [PubMed] [Google Scholar]
- 44.Wasik, T. J., P. P. Jagodzinski, E. M. Hyjek, J. Wustner, G. Trinchieri, H. W. Lischner, and D. Kozbor. 1997. Diminished HIV-specific CTL activity is associated with lower type 1 and enhanced type 2 responses to HIV-specific peptides during perinatal HIV infection. J. Immunol. 158:6029-6036. [PubMed] [Google Scholar]