Abstract
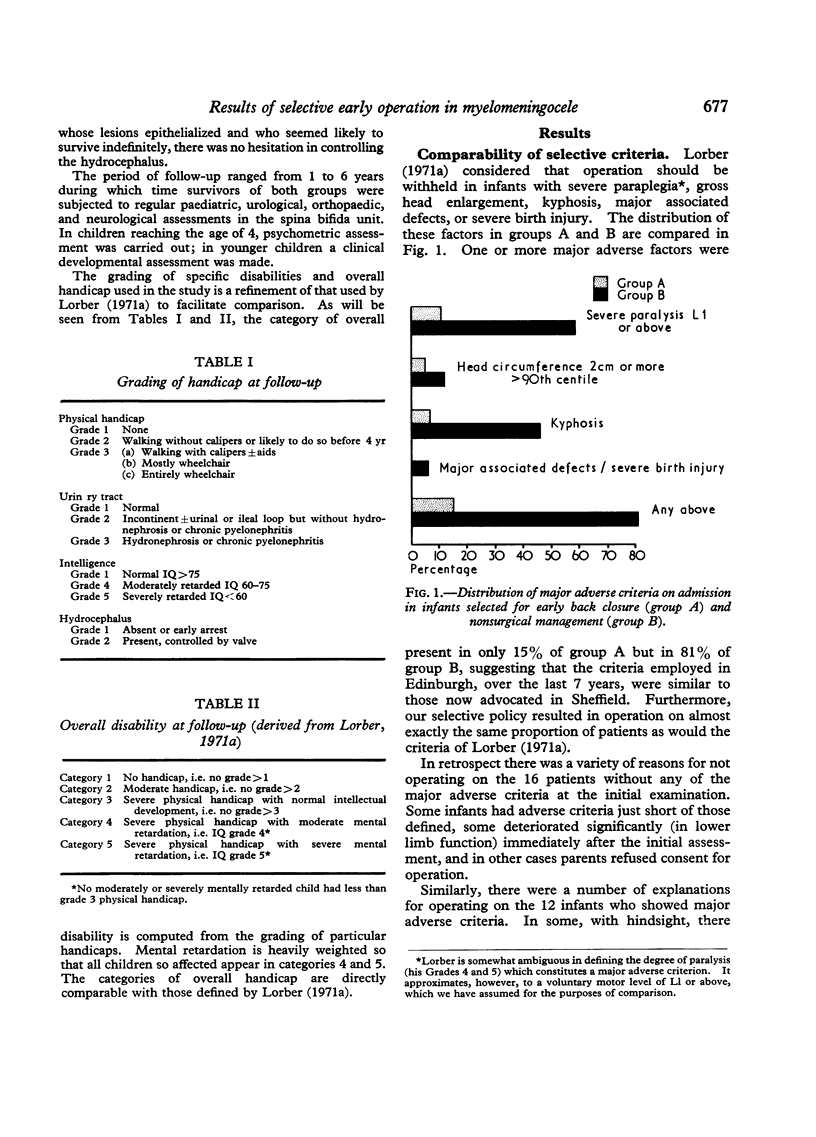
In a 6-year period 163 unselected newborn infants with open myelomeningocele were assessed. 48%, considered to have the most favourable prognosis, were selected for early back closure and vigorous subsequent treatment. The more severely affected remainder were given only symptomatic treatment unless long-term survival seemed likely. The major adverse criteria were severe paralysis, gross head enlargement, and spinal deformity such as kyphosis. More than 70% of selected infants were alive at 6 years, whereas more than 80% of untreated infants were dead at 3 months.
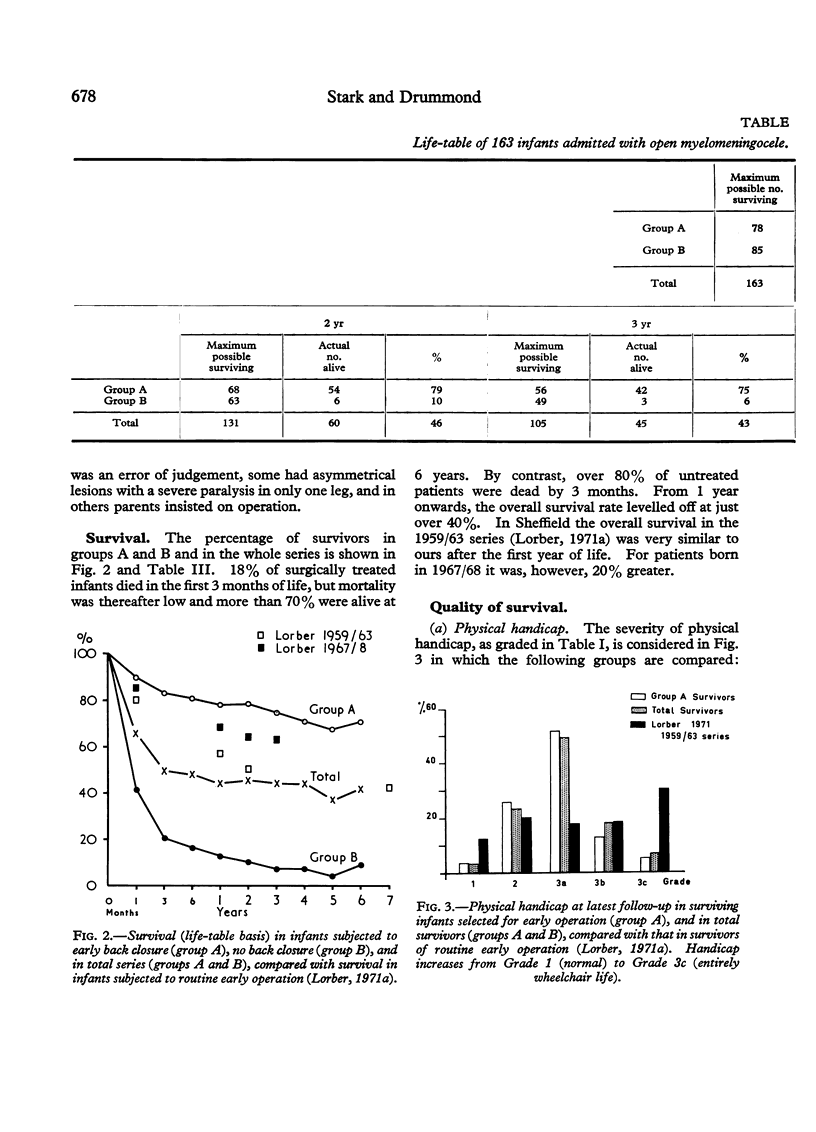
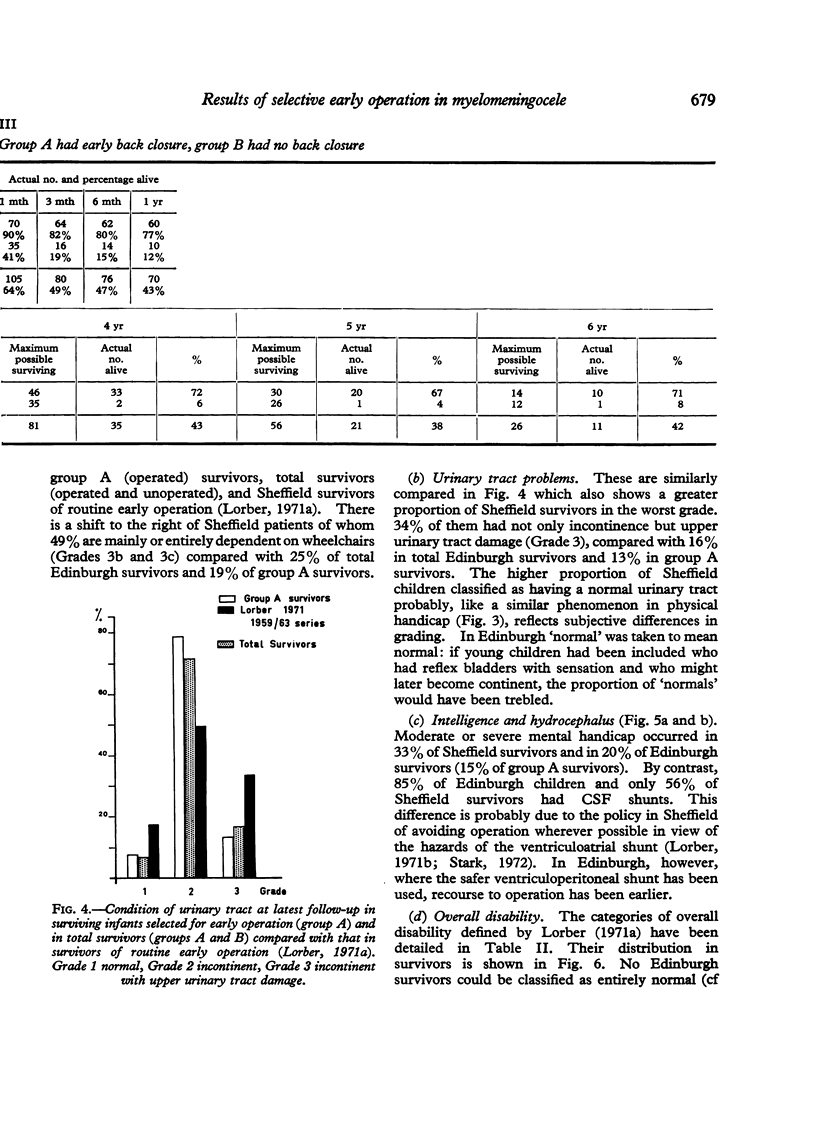
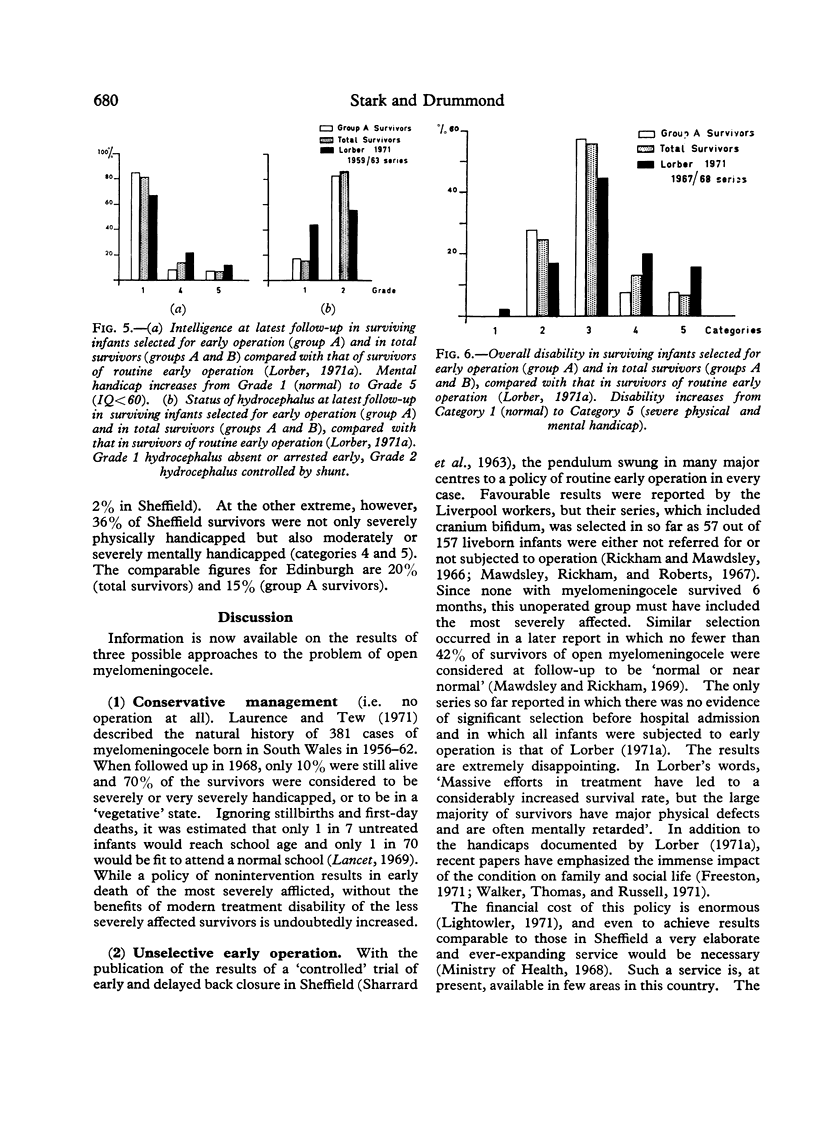
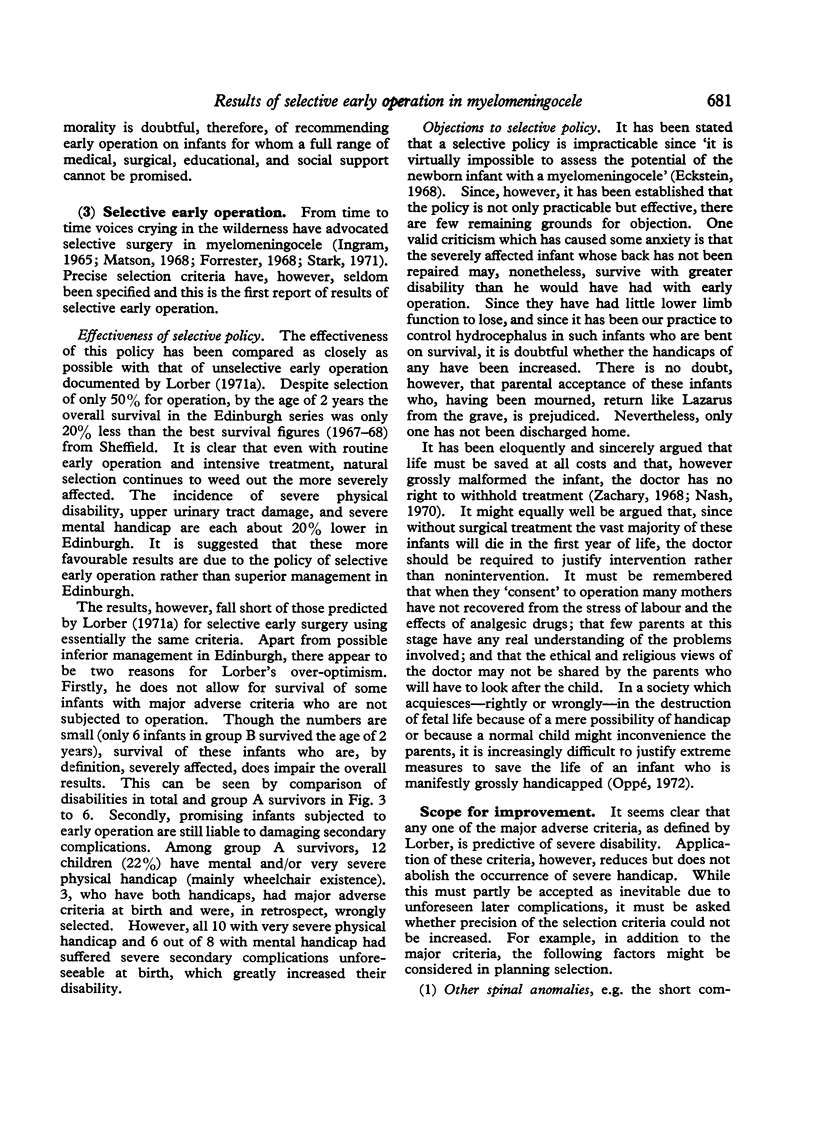
The follow-up results are compared with those of routine early operation (Lorber, 1971a). After 1 year, the overall survival levelled out at 40% (cf 60%). The survivors were, however, less severely handicapped. Only 25% were mainly or entirely in wheelchairs (cf 49%). Only 16% had upper urinary tract damage in addition to incontinence (cf 34%). A combination of mental and severe physical handicap occurred in only 20% (cf 36%). Severe disability was encountered mainly in children who had suffered from complications, e.g. ventriculitis, unforeseeable at birth.
It is concluded that the overall results of selective early operation compare favourably with those of purely conservative management on the one hand, and with routine early operation on the other. It is suggested that this policy offers the best prospects of independence for the less severely affected child, and the least distress and suffering for the grossly afflicted.
Full text
PDF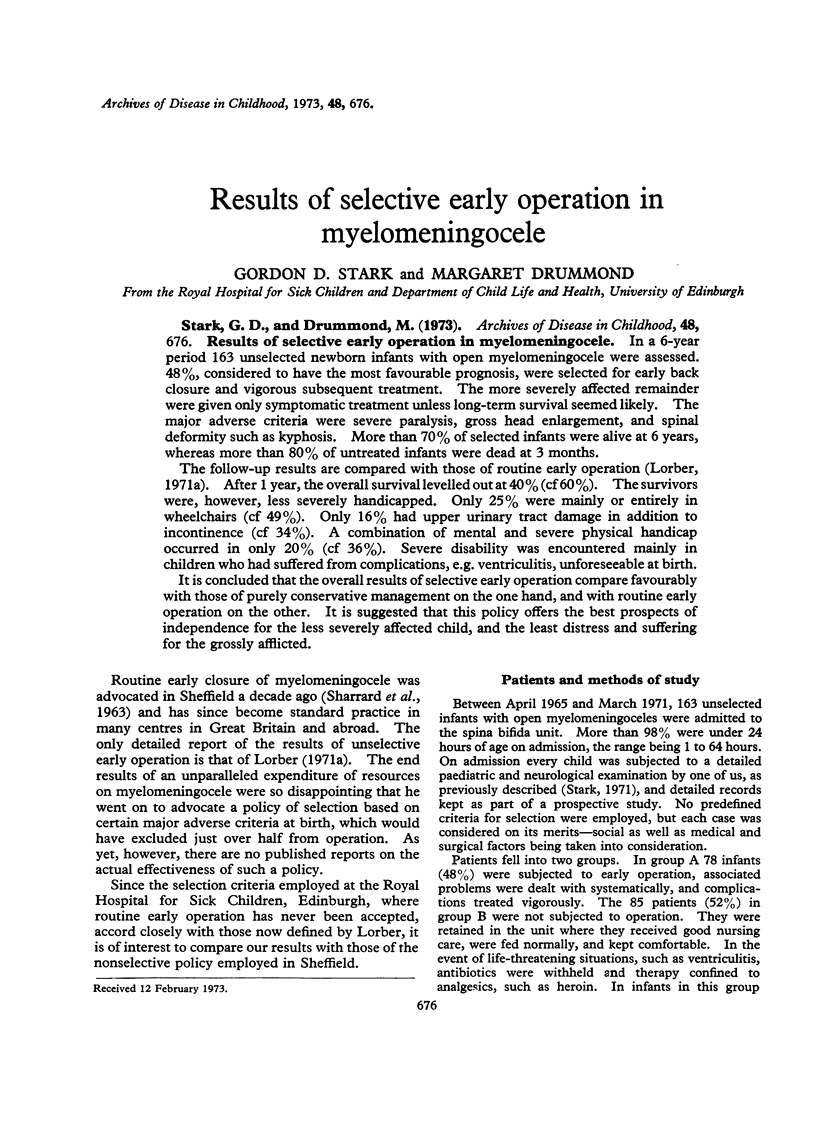

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Forrester R. M. Ethical and social aspects of treatment of spina bifida. Lancet. 1968 Nov 9;2(7576):1033–1033. doi: 10.1016/s0140-6736(68)91325-1. [DOI] [PubMed] [Google Scholar]
- Freeston B. M. An enquiry into the effect of a spina bifida child upon family life. Dev Med Child Neurol. 1971 Aug;13(4):456–461. doi: 10.1111/j.1469-8749.1971.tb03052.x. [DOI] [PubMed] [Google Scholar]
- Laurence K. M., Tew B. J. Natural history of spina bifida cystica and cranium bifidum cysticum. Major central nervous system malformations in South Wales. IV. Arch Dis Child. 1971 Apr;46(246):127–138. doi: 10.1136/adc.46.246.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightowler C. D. Meningomyelocele: the price of treatment. Br Med J. 1971 May 15;2(5758):385–387. doi: 10.1136/bmj.2.5758.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber J. Medical and surgical aspects in the treatment of congenital hydrocephalus. Neuropadiatrie. 1971 Feb;2(3):239–246. doi: 10.1055/s-0028-1091785. [DOI] [PubMed] [Google Scholar]
- Lorber J. Results of treatment of myelomeningocele. An analysis of 524 unselected cases, with special reference to possible selection for treatment. Dev Med Child Neurol. 1971 Jun;13(3):279–303. [PubMed] [Google Scholar]
- Matson D. D. Surgical treatment of myelomeningocele. Pediatrics. 1968 Aug;42(2):225–227. [PubMed] [Google Scholar]
- Mawdsley T., Rickham P. P., Roberts J. R. Long-term results of early operation of open myelomeningoceles and encephaloceles. Br Med J. 1967 Mar 18;1(5541):663–666. doi: 10.1136/bmj.1.5541.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark G. D. Neonatal assessment of the child with a myelomeningocele. Arch Dis Child. 1971 Aug;46(248):539–548. doi: 10.1136/adc.46.248.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark G. Conservative treatment of hydrocephalus. Dev Med Child Neurol. 1972 Dec;14(6):804–805. doi: 10.1111/j.1469-8749.1972.tb03324.x. [DOI] [PubMed] [Google Scholar]
- Walker J. H., Thomas M., Russell I. T. Spina bifida--and the parents. Dev Med Child Neurol. 1971 Aug;13(4):462–476. doi: 10.1111/j.1469-8749.1971.tb03053.x. [DOI] [PubMed] [Google Scholar]
- Zachary R. B. Ethical and social aspects of treatment of spina bifida. Lancet. 1968 Aug 3;2(7562):274–276. doi: 10.1016/s0140-6736(68)92369-6. [DOI] [PubMed] [Google Scholar]


