Abstract
Objective:
To describe the prevalence and characteristics of spit (smokeless)-tobacco (ST) use in rookie baseball players as they enter the professional ranks and to identify factors associated with use before entering professional baseball.
Design and Setting:
This cross-sectional study was an anonymous questionnaire survey administered during the 1999 baseball season by professional baseball athletic trainers at 30 professional baseball clubs.
Subjects:
The target group was all rookie professional baseball players entering professional baseball. Of 862 eligible players in the summer of 1999, 616 participated in the survey.
Measurements:
The questionnaire assessed tobacco use, demographic variables relevant to rookie professional baseball players, and factors hypothesized to be associated with current ST use (ie, other forms of tobacco use, social norms, environmental cues, and risky behavior intentions). Univariate associations with ST use were described by relative risks with 95% confidence intervals. For continuous variables, mean values of ST users and nonusers were compared.
Results:
Overall, 67% of the players had tried ST and 31% were current users. Significant risk factors for ST use were being a current cigarette or cigar smoker, having a family member who used ST, and perceiving ST use by peers and role models.
Conclusions:
Almost one third of rookie baseball players in the 1999 season were regular ST users on entering professional baseball. Interventions for prevention and cessation of the use of ST targeting young baseball players are needed.
Keywords: chewing tobacco, oral snuff
Athletes, particularly baseball players, are known to be heavy users of spit (smokeless) tobacco (ST). Investigators have reported that 33% to 40% of professional baseball players1–3 and 45% to 55% of college baseball players4,5 (National Collegiate Athletic Association, unpublished data, 2001) use ST regularly.
The 2 main types of ST are oral snuff and chewing tobacco. Oral snuff is a finely ground or shredded form of tobacco commonly sold in a round tin can. Users put a “dip” (pinch) of snuff between their lower lip or cheek and gum (the labial and buccal areas, respectively, of the oral cavity), where it stays in place until removed. Chewing tobacco is more coarsely cut than snuff and is packaged in loose or plug form, most commonly in pouches. Users put a “chew” or “wad” of tobacco in the buccal area of the oral cavity and chew it until they remove it. In 1993, the US Surgeon General advocated using the term “spit tobacco” rather than “smokeless tobacco” (a term coined by the tobacco industry) to prevent the erroneous suggestion that smokeless means harmless.6
The negative health effects of ST include oral cancer,7,8 oral leukoplakia9,10 (a premalignant lesion),11 gingival recession,12 dental caries,13 hypertension,14,15 and nicotine addiction.16 The risk of oral cancer is 4 times greater in ST users than in nonusers.7 Nitrosamines, potent carcinogens known to cause cancer in more than 30 species of animals, have been measured in ST products at levels 100-fold greater than the legal limits for nitrosamines in foodstuffs.16,17 In addition, chronic exposure to nicotine delays wound healing and is associated with cardiovascular disease, stomach ulcers, and sexual impotence.18
In 1991, because of the high risk of adverse health effects associated with ST use, Major League Baseball instituted a ban on tobacco use by Minor League players during practices, games, and team travel.19,20 Subsequently, the National College Athletic Association (NCAA) instituted a similar ban on the use of tobacco by college athletes.21 Because no data have been reported on ST use among rookie players entering professional baseball, we conducted a cross-sectional study of these players to assess, through a questionnaire, the prevalence of ST use and factors that influence use in this population. We hypothesized that current ST use would be associated with a player's perception of certain social norms and environmental factors identified in the questionnaire. These data are important to determine the need for tobacco-control interventions targeting this population and to identify factors helpful in planning such programs.
METHODS
Recruitment of Study Sample
To be eligible for participation, a player had to be a US citizen and signed with a professional baseball club either during the June 1999 amateur draft or as a free agent in June or July 1999. Head athletic trainers at all 30 professional baseball clubs were contacted in May 1999 by letter to explain the study and to gain permission for eligible rookie members of their baseball teams to participate in the study.
Survey Administration
During the 1999 Rookie League season (June through August), the athletic trainer at each club obtained informed consent and administered the anonymous, written survey in accordance with written, standardized instructions received from study investigators. Eligible players who agreed to participate in the study completed the questionnaire either on an individual basis or at a team meeting.
Conceptual Framework of the Survey
The Theory of Reasoned Action22 and the Health Belief Model23 provided the conceptual framework for questionnaire development. The Theory of Reasoned Action postulates that one's perception of general social norms regarding a particular behavior is an important determinant of intention to perform that behavior. In addition, the Health Belief Model maintains that before one adopts a new behavior, there needs to be a “cue to action” that triggers the new behavior. In applying these theories, we focused on identifying athletes' perceptions of social norms related to ST use and of “cues” in their environment that supported the adoption of this behavior.
Measurements
Items included in the survey assessed ST use, factors presumed to be associated with ST use (eg, other tobacco use, social-norm factors, environmental cues, and intention to engage in risky behavior), and demographic factors. Except for the survey item on risky behaviors, all items were obtained from questionnaires used in previous studies of baseball athletes1,3,4 or from national surveys of same-aged males in the general population.24–26 The following more specifically explains the categories and specific variables assessed on the survey.
Use of Spit Tobacco
Current ST use was defined as use within the past 30 days. We also assessed type and brand of ST used, age of initiation of use (defined as age of first experimentation), and age of first purchase of ST products.
Factors Associated with Spit-Tobacco Use
As measures of other tobacco use, we assessed current cigarette smoking and current cigar smoking. Current use was defined for both products as use within the past 30 days.
Social-norm factors relating to perceived ST use by peers and role models were assessed by asking each player if any of the following referents used ST: high school and college peers, a family member, and his Little League coach. In addition, we asked each player if his mother or father were aware of his tobacco use. For all of these items, the response was either “yes” or “no.” We also asked each player to estimate his age of first awareness that professional baseball players used ST, the percentage of Major Leaguers who used ST, and the percentage of Major Leaguers who smoked cigarettes.
To identify environmental factors that might influence ST use, we presented a list of possible media (eg, magazines, billboards, television) and sports events (eg, baseball, football, hockey, NASCAR, rodeo) and asked players to indicate the ones that made them most aware of ST advertising. Other environmental factors assessed that might influence ST use related to awareness of the Minor League ban on ST use, history of a dental examination within the previous 2 years, and whether he was asked to show identification at the time of purchase if he had purchased ST before 18 years of age. History of a dental examination was included because previous authors27,28 have reported that an oral examination with feedback about ST-associated lesions in a player's mouth, advice to quit ST use, and brief counseling by dental professionals have been effective in promoting cessation of ST use.
As a general measure of risky behavior intention, we asked each player if he would use a legal supplement regardless of health risk if the supplement would ensure his reaching the Major Leagues. The 4 response options were “he would definitely not use it,” “he would consider using it,” “he would probably use it,” and “he would definitely use it.” Although not validated before our study, this hypothetical question was included in an attempt to quantify an attitude in which short-term success in athletics is perceived as being more important than long-term health consequences.
Demographic factors assessed included age, current position played, and history of playing Little League Baseball.
Data Analysis
Prevalence of tobacco use in the past 30 days was calculated for ST, cigarettes, and cigars. For generalization to a larger population, an exact binomial 95% confidence interval (CI) was calculated for each prevalence. The Epi Info software package (version 6, Centers for Disease Control, Atlanta, GA) was used for data management and analysis.29
Variables hypothesized to be associated with current ST use were analyzed individually. The association between each dichotomous variable and ST use was described by a relative risk (RR), and the statistical significance was assessed by the 95% CI. If the lower boundary of the CI exceeded 1, then the RR was statistically significant. Significance for continuous variables (ie, age, perception of percentage of tobacco use in Major League Baseball) was assessed with a t test. For descriptive purposes, the mean values for ST users and nonusers were compared. The risk-taking behavior variable had 4 categories, and the chi-square test was calculated for statistical significance.
RESULTS
Study Sample
In all, 30 professional baseball clubs were contacted and agreed to participate in the study. Of the 862 athletes who were eligible to participate, 246 either refused or were absent on the day the questionnaire was administered, yielding a response rate of 71% (n = 616). Because this was an anonymous survey, we were unable to follow up with the nonresponders.
Among the 616 subjects, the mean age was 21 years (range, 17 to 24 years). Among the responders, 51% (315) were pitchers, and 98% (587) had played Little League Baseball. Sixty-seven percent (408) had tried ST; 96% (561) were aware of the ban on the use of tobacco products in the Minor Leagues; and 89% (501) reported they had had a dental examination in the last 2 years. (Not all subjects answered each item.)
Prevalence of Spit-Tobacco Use
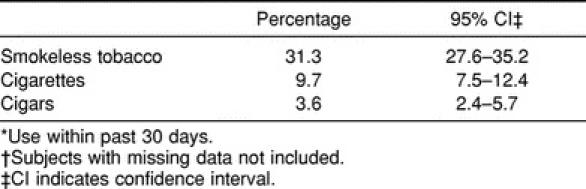
The overall prevalence of ST use within the past 30 days was 31% (n = 190), much higher than that reported for cigarette or cigar smoking (Table 1). Of these, 82% (133) reported using a snuff product and 18% (29), a chewing tobacco product. The reported snuff brands were Copenhagen (US Smokeless Tobacco Co, Greenwich, CT), 42% (56); Skoal (US Smokeless Tobacco Co), 41% (55); Kodiak (Conwood Corp, Memphis, TN), 12% (16); and other, 5% (6). The majority of responding chewing tobacco users, 71% (21), reported using Red Man (Pinkerton Tobacco Co, Owensboro, KY), and the remaining 29% (8) used Levi Garett (Conwood Corp). The mean age for initiation of ST use was 16 years, and the mean age of first purchase of ST was 17 years.
Table 1.
Prevalence of Current Tobacco Use* (n = 607)†
Variables Associated With Spit-Tobacco Use
Other Tobacco Use and Demographics
The prevalence of ST use was significantly higher among smokers than among nonsmokers. Table 2 shows an RR of 2.4, with a significant CI of 1.9 to 3.0, indicating that the risk of ST use was more than double for current smokers as compared with nonsmokers (65% versus 28%). ST use, however, was not significantly associated with age group or position played (see Table 2).
Table 2.
Prevalence of Current Spit (Smokeless)-Tobacco (ST) Use by Other Characteristics (n = 607)*
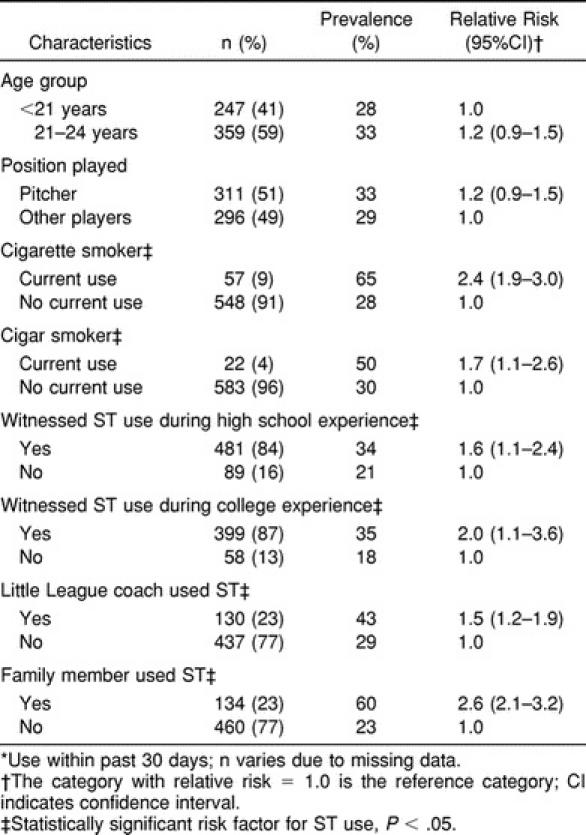
Social-Norm Factors
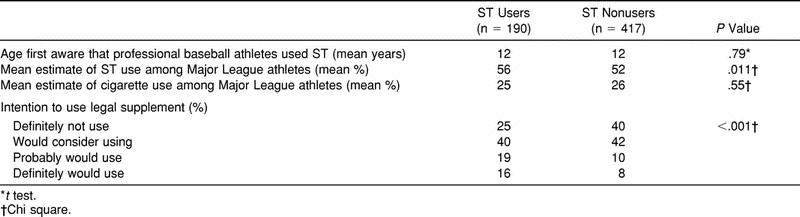
The use of ST was significantly associated with use by family members (RR = 2.6, 95% CI = 2.1 to 3.2), Little League coaches (RR = 1.5, 95% CI = 1.2 to 1.9), and peers (high school: RR = 1.6, 95% CI = 1.1 to 2.4; college: RR = 2.0, 95% CI = 1.1 to 3.6) (see Table 2). In addition, 80% of ST users (152) reported that at least one of their parents was aware of their tobacco use, as compared with only 40% of cigarette smokers. Both ST users and nonusers estimated that ST was used by more than half of the Major League Baseball players. ST users, however, estimated that a greater proportion of Major League Baseball players used ST than nonusers estimated (56% versus 52%); although this difference was small, it was statistically significant (t1 = 2.56, P = .011). There was no difference between ST users and nonusers with regard to the age at which they first became aware that professional baseball players used ST or their perception of cigarette smoking among Major League athletes (Table 3).
Table 3.
Perceptions Related to Spit (Smokeless)-Tobacco (ST) Use Among Users and Nonusers
Environmental Factors
The environmental factors we measured were not significantly associated with ST use. Overall, however, when asked about where they perceived advertisements most enhanced their awareness of ST products, 62% of players indicated magazines; 53%, rodeos; and 49%, baseball and car-racing sporting events. (The groups were not mutually exclusive.) For those players who first purchased ST when they were less than 18 years of age, more than three fourths reported that they were not asked to show proof of age.
Risky Behavior Intentions
The use of ST was associated with the desire to be successful in baseball regardless of health risks (χ23 = 23.62, P < .001, see Table 3). Twice as many ST users as nonusers said they would definitely use a legal supplement despite health risks if it would assure membership on a Major League team (16% [30] versus 8% [15]).
DISCUSSION
We found that the prevalence of ST use among entering rookie professional baseball players (31%) was similar to the 33% reported in 1999 for Minor League professional baseball players in general.1 This finding suggests that most ST users in professional baseball start using ST before they join the professional ranks. Although the prevalence of ST use was much higher than the 11% reported nationally for 18- to 25-year-old men,26 it was lower than that reported in 2001 for NCAA male baseball, wrestling, ice hockey, and lacrosse athletes (41%, 39%, 35%, and 32%, respectively) and higher than that reported in 2001 for other NCAA male sports (eg, football, 29%; golf, 27%; water polo, 25%; soccer, 21%; track and field, 13%; basketball, 12%) (National Collegiate Athletic Association, unpublished data, 2001).
In contrast, the prevalence of current cigarette smoking in our sample of athletes (9%) was much lower than the national prevalence rate for 18- to 25-year-old men (45%) but slightly higher than the 7% previously reported for Minor League professional baseball players.30
Consistent with previous research,31 the association between the use of ST and cigarette smoking in our study sample was strong. Smokers were twice as likely to use ST as nonsmokers. This finding suggests an addictive pattern of behavior and the need for treatment to address the addictive process.
Because we found an association between the use of ST and the desire to be successful in baseball regardless of health risks, ST use–prevention programs provided for rookie and student baseball players should reinforce previously reported findings that ST use does not improve athletic performance.32
Correcting misconceptions is consistent with the Social Influence Model,33 which postulates that social and psychological processes influence health attitudes, values, beliefs, and behaviors in important ways. Edwards' framework for applying the Social Influence Model34 identifies 9 types of social influence that can enhance health: education, persuasion, imitation, induced counterattitudinal action (a process that uses subtle coaxing or role playing to influence others to engage in actions contrary to their attitudes or habitual behaviors), conformity, compliance, conditioning, leadership, and obedience. Although it is beyond the scope of this article to describe in detail these social-influence processes (readers are referred to other resources34–37), the process of conformity will be explained to illustrate one application of the model that athletic trainers can use as an ST use–prevention strategy.
Conformity is a process through which the majority in a group express judgments to other group members to gain agreement by using the mechanisms of social comparison and the need for acceptance. Youth in general are very susceptible to this process and want to behave in conformity with peer-group norms. Rookie baseball players in this study perceived the prevalence of ST use among Major League Baseball players to be higher than it actually is. Specifically, ST users and nonusers in this study estimated, respectively, that 56% and 52% of Major League players used ST, when actually the most recent documented prevalence of ST use among Major Leaguers was 36%.1 Because many rookie baseball players tend to overestimate the amount of ST use among professional baseball athletes, communicating to them that ST users are actually in the minority among professional baseball athletes may help them realize that they are already in conformity with the norm of their peers and, thus, prevent ST-use initiation. Such an approach is also consistent with the Theory of Reasoned Action,22 which maintains that perception of social norms is an important determinant of behavior.
We also found that ST use was associated with perceived use by family members and Little League coaches. These findings suggest that the involvement of significant others in ST-intervention programs could allow important role models to reinforce nonuse. Consistent with our findings and with the Theory of Reasoned Action, Gottlieb et al38 reported that athletes who did not intend to use ST perceived significantly less acceptance of ST use by important figures in their lives than athletes who intended to use ST.
Effective in-service programs for baseball coaches and athletic trainers at all levels are needed to gain their support for policy-level interventions targeting athletes and to promote positive role modeling. Levenson-Gingiss39 described a program that incorporates strategies to influence teachers' perceptions of their work roles, capabilities to implement an innovative health program, and commitment to the new program. Research is needed to examine the effect of such staff-development programs on coaches and athletic trainers and on subsequent use of ST by student-athletes.
In this study, 75% of ST users reported that their parents were aware of their ST use, whereas only 35% of smokers reported that their parents were aware of their smoking. This finding suggests that ST use may be more acceptable to parents and the public in general than smoking, possibly because of the misconception that ST is harmless. Public education programs on the dangers of ST use are needed to counter aggressive manufacturers' promotions of ST. Clearly, ST products are not safe. For example, data from one study7 indicated that ST users have a 4 times greater risk of developing oral cancer than nonusers, and the risk was as high as 50 times greater for cancer of the gum and cheek (where the tobacco was held), depending on the frequency and duration of use. In another study of US veterans,8 the use of chewing tobacco or snuff was significantly associated with death from cancers of the cheek (buccal mucosa) and throat. Frequent users were 3 times more likely to acquire cancer of the buccal area of the oral cavity than less frequent users and 4 times more likely to have throat cancer. Those who started using ST before the age of 14 years were 20 times more likely to develop throat cancer. Considering the scientific evidence, the US Surgeon General and the Congress have determined that ST products are a cause of serious disease and should carry warning labels and be treated accordingly.40 With the alarmingly high use of ST among young males, especially athletes, widespread knowledge of information about the hazardous effects is important. The public should not be fooled into thinking that a tobacco product called “smokeless” is harmless.
Findings from our study also suggest that several environmental and social factors support ST use among baseball players before they enter the professional ranks. For example, 75% of players who purchased ST before they were 18 years old reported that they were not asked to show proof of age. Players in this study also reported that advertisements and promotions in magazines and at rodeo, baseball, and car-racing sports events enhanced their awareness of ST products. These latter findings are consistent with the Federal Trade Commission's report that ST manufacturers spent a record $150.4 million promoting their products in 1997, and much of this spending was on billboards, free hat offers, and sponsorship of sporting events.41 To counteract these influences, promotion of ST and candy look-a-like products at youth sports events should be prohibited and penalties for transgression enforced to protect youths who attend these events.
Most ST users in this study regularly used snuff products, suggesting a greater potential for nicotine addiction. Blood-nicotine levels in snuff users were higher than in chewing-tobacco users, as indicated by cotinine level.42 Cotinine, a metabolite of nicotine, has a longer half-life than nicotine in blood and saliva and, consequently, is used as a biochemical marker of tobacco use and level of nicotine addiction. The greater addiction potential for snuff as compared with chewing tobacco has been attributed to the fact that snuff is a more finely ground tobacco leaf and, thus, presents more surface area for nicotine to diffuse from the tobacco and into the bloodstream.42
Moreover, specific snuff products themselves have different nicotine-dosing characteristics.43 The amount of nicotine available for the body to use is a function not only of the quantity of nicotine in the product but also of its speed of delivery. Because nicotine is absorbed across the oral mucosa most rapidly in an alkaline environment, ST manufacturers control the rate of delivery of nicotine in their products (the bioavailability) through the addition of alkaline buffering agents.43 In our study, 42% of current snuff users named Copenhagen as their usual brand. Because of its high alkaline pH (8.0), Copenhagen has a higher level of bioavailable nicotine than most other brands of snuff and chewing tobacco, even though the latter products may contain the same or higher concentrations of nicotine.43
Athletes in the Minor Leagues or in colleges who use snuff, especially Copenhagen, may find it difficult to comply with the ban on ST use in their athletic environment without additional help to manage their nicotine-withdrawal symptoms (ie, craving, irritability, anger, restlessness, inability to concentrate, anxiety, insomnia, increased appetite, and depressed mood). It is important that those ST users who indicate they want to stop ST use altogether are assisted to obtain the knowledge and skills needed to prepare to quit, to cope with cravings and triggers to use, and to use pharmacologic agents to reduce nicotine-withdrawal symptoms if necessary.
Nicotine-patch use in combination with behavioral counseling has been found to improve short-term quitting success in ST users and to reduce ST cravings and other withdrawal symptoms.44 However, 2 mg of nicotine gum with and without counseling has not been found to be an effective treatment.45 Further research assessing higher doses of nicotine gum is needed. Although Zyban (GlaxoSmithKline, Triangle Park, NC), a nonnicotine antidepressant, has been found to promote smoking cessation, its efficacy in ST users is unknown.46 Zyban appears to target the neurochemistry of addiction by increasing dopamine levels in the brain to enhance feelings of well-being. Histories of head injury or seizure disorders are contraindications for use of Zyban.47
The fact that use of snuff was much more common in this group of athletes than use of chewing tobacco also is of concern because the strongest data associating the use of ST with oral lesions,9,10 gingival recession,12 and oral cancer7 were obtained in snuff users. Although the more serious adverse health effects of ST use may be delayed for many years, the early onset of ST use among young athletes provides time to build nicotine addiction and time for long-term exposure to the high concentration of carcinogens in ST products.
Because athletic trainers address health issues with athletes daily, they are in an ideal position to advise ST users to stop their tobacco use and to assist those who wish help with the cessation process. For example, athletic trainers can provide self-help quitting guides, brief cessation counseling, instruction on pharmacologic agents, and ongoing support and motivation for the quitting process. A step-by-step, self-help quitting guide for ST users, tailored to baseball players and available from the National Cancer Institute,48 is a valuable adjunct for athletic trainers to use in counseling users about ST. For athletes who need more intensive supportive and problem-solving treatment, athletic trainers can institute a system for confidential referral to expert ST-cessation counselors in the community identified through the American Cancer Society.
Most importantly, however, athletic trainers can facilitate the inclusion of an oral-cancer screening examination by a dental professional as part of the mandated health screenings of athletes. To date, the only effective ST-cessation programs among college athletes27 and other adults28 have involved oral examinations with feedback about ST-associated oral lesions and brief cessation counseling by dental professionals. Such examinations provide a “teaching moment” to prevent initiation of tobacco use among nonusers and to motivate tobacco-use cessation among ST users. More than 60% of ST-using college baseball and football players in California said that seeing harmful changes in their mouth or receiving advice to quit from a dentist would motivate them to stop ST use.4 Working with college athletes in California and with professional baseball players during spring training, we found that the videotapes “The Tragic Choice: The Bob Leslie Story” (Oral Health America, Chicago, IL) and “The Dangerous Game” (National Cancer Institute, Bethesda, MD) effectively communicated the adverse health consequences of using ST, were positively received by athletic trainers and athletes, and motivated many ST users to try to quit.27 Others also have reported that discussion of the negative oral-health effects from ST use has a significant influence on ST users' desire to quit.45
Changing the social norms that sanction and support ST use in all levels of baseball is essential. Use of peer leaders to endorse behavioral innovation to alter social norms has been effective in other research49,50 and should be considered in the development of ST-use interventions for athletes as well. The big challenge is to discover effective strategies to convince young athletes of their personal vulnerability to health risks associated with ST use and, at the same time, override what they see as the positive aspects, including the approval of their male peers.
In summary, our findings indicate that considerable experimentation with ST products occurs among rookie baseball players, many of them use ST regularly, and many enter professional baseball already addicted to nicotine. This is an unfortunate circumstance because use of ST by professional baseball players, who are constantly in front of the public, may help to perpetuate the cycle of initiation of ST use by youth who tend to emulate them. Most professional baseball athletes, however, do not use ST, and preventive programs should highlight that fact. Because athletic trainers work on a day-to-day basis with athletes regarding health issues, their role as tobacco-cessation interventionists should be studied. Finally, our findings indicate that the sale of tobacco to minors, parental acceptance of ST use, ST use by family members, and perceptions of use by baseball-associated role models are factors that may support the use of ST among young baseball athletes. Interventions against the use of ST targeting this population should address these factors and the addiction process.
ACKNOWLEDGMENTS
We gratefully acknowledge Joe Garagiola, Sr, for his leadership in increasing awareness of the risk of oral cancer associated with ST use and for supporting this study. We also gratefully acknowledge the invaluable efforts of the athletic trainers and athletes of the 30 professional baseball clubs that participated in this study.
REFERENCES
- 1.Severson HH, Kaufman N, Williams CJ, Hatsukami D, Walsh M, Orleans CT. Tobacco use and spit tobacco cessation among professional baseball players. Paper presented at: Annual Meeting of the Society for Research on Nicotine and Tobacco; February 18, 2000; Arlington, VA. [Google Scholar]
- 2.Connolly GN, Orleans CT, Kogan M. Use of smokeless tobacco in major-league baseball. N Engl J Med. 1988;318:1281–1285. doi: 10.1056/NEJM198805123181918. [DOI] [PubMed] [Google Scholar]
- 3.Ernster VL, Grady DG, Greene JC, et al. Smokeless tobacco use and health effects among baseball players. JAMA. 1990;264:218–224. [PubMed] [Google Scholar]
- 4.Walsh MM, Hilton JF, Ernster VL, Masouredis CM, Grady DG. Prevalence, patterns, and correlates of smokeless tobacco use in a college athlete population. Addict Behav. 1994;19:411–427. doi: 10.1016/0306-4603(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 5.Levenson-Gingiss P, Morrow JR, Dratt LM. Patterns of smokeless tobacco use among university athletes. J Am Coll Health. 1989;38:87–90. doi: 10.1080/07448481.1989.9938421. [DOI] [PubMed] [Google Scholar]
- 6.Mooney D. PBATS enlists United States Surgeon General in war on ST. PBATS Newsletter. 1993;6(1):18. [Google Scholar]
- 7.Winn DM, Blot WJ, Shy CM, Pickle LW, Toledo A, Fraumeni JF., Jr Snuff dipping and oral cancer among women in the southern United States. N Engl J Med. 1981;304:745–749. doi: 10.1056/NEJM198103263041301. [DOI] [PubMed] [Google Scholar]
- 8.Zahm SH, Heineman EF, Vaught JB. Soft tissue sarcoma and tobacco use: data from a prospective cohort study of United States veterans. Cancer Causes Control. 1992;3:371–376. doi: 10.1007/BF00146891. [DOI] [PubMed] [Google Scholar]
- 9.Grady D, Greene J, Daniels TE, et al. Oral mucosal lesions found in smokeless tobacco users. J Am Dent Assoc. 1990;121:117–123. doi: 10.14219/jada.archive.1990.0139. [DOI] [PubMed] [Google Scholar]
- 10.Tomar SL, Winn DM, Swango PA, Giovino GA, Kleinman DV. Oral mucosal smokeless tobacco lesions among adolescents in the United States. J Dent Res. 1997;76:1227–1286. doi: 10.1177/00220345970760060701. [DOI] [PubMed] [Google Scholar]
- 11.Squier CA. Smokeless tobacco and oral cancer: a cause for concern? CA Cancer J Clin. 1984;34:242–247. doi: 10.3322/canjclin.34.5.242. [DOI] [PubMed] [Google Scholar]
- 12.Robertson PB, Walsh M, Greene J, Ernster V, Grady D, Hauck W. Periodontal effects associated with the use of smokeless tobacco. J Periodontol. 1990;61:438–443. doi: 10.1902/jop.1990.61.7.438. [DOI] [PubMed] [Google Scholar]
- 13.Tomar SL, Winn DM. Chewing tobacco use and dental caries among U.S. men. J Am Dent Assoc. 1999;130:1601–1610. doi: 10.14219/jada.archive.1999.0099. [DOI] [PubMed] [Google Scholar]
- 14.Bolinder G, Alfredsson L, Englund A, de Faire U. Smokeless tobacco use and increased cardiovascular mortality among Swedish construction workers. Am J Public Health. 1994;84:399–404. doi: 10.2105/ajph.84.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westman EC. Does smokeless tobacco cause hypertension? South Med J. 1995;88:716–720. doi: 10.1097/00007611-199507000-00004. [DOI] [PubMed] [Google Scholar]
- 16.The Health Consequences of Using Smokeless Tobacco: A Report of the Advisory Committee to the Surgeon General. Bethesda, MD: National Institutes of Health; 1986. NIH publication 86-2874. [Google Scholar]
- 17.Tomar SL, Henningfield JE. Additional evidence implicating moist snuff as a potent carcinogen. J Natl Cancer Inst. 1995;87:1822–1824. doi: 10.1093/jnci/87.24.1822. [DOI] [PubMed] [Google Scholar]
- 18.Shabsigh R, Fishman IJ, Schum C, Dunn JK. Cigarette smoking and other vascular risk factors in vasculogenic impotence. Urology. 1991;38:227–231. doi: 10.1016/s0090-4295(91)80350-g. [DOI] [PubMed] [Google Scholar]
- 19.“ST” banned in 4 minor leagues. PBATS Newsletter. 1991;4(2):6. [Google Scholar]
- 20.Ban on smokeless tobacco expanded to single “A” Ball. PBATS Newsletter. 1992;5(1):7. [Google Scholar]
- 21.National Collegiate Athletic Association. 2002–2003 NCAA Sports Medicine Handbook. Indianapolis, IN: National Collegiate Athletic Association; 2002. p. 85. [Google Scholar]
- 22.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 23.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 24.Youth Risk Behavior Surveillance: National College Health Risk Behavior Survey—United States, 1995. MMWR CDC Surveill Summ. 1997;46:1–56. [PubMed] [Google Scholar]
- 25.State-specific prevalence among adults of current smoking and smokeless tobacco use and per capita tax-paid sales of cigarettes—United States, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:922–926. [PubMed] [Google Scholar]
- 26.Kapstein A. Tobacco Use in America: Findings From the 1999 National Household Survey on Drug Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2001. Analytic Series: A-15, DHHS publication SMA 02-3622. [Google Scholar]
- 27.Walsh MM, Hilton JF, Masouredis CM, Gee L, Chesney MA, Ernster VL. Spit tobacco cessation intervention for college athletes: results after 1 year. Am J Public Health. 1999;89:228–234. doi: 10.2105/ajph.89.2.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevens VJ, Severson H, Lichtenstein E, Little SJ, Leben J. Making the most of a teachable moment: a smokeless-tobacco cessation intervention in the dental office. Am J Public Health. 1995;85:231–235. doi: 10.2105/ajph.85.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dean AG, Dean JA, Coulombier D, et al. Epi Info, Version 6: A Word-Processing, Database, and Statistics Program for Public Health on IBM-Compatible Microcomputers. Atlanta, GA: Centers for Disease Control and Prevention; 1995. [Google Scholar]
- 30.Severson H, Williams C, Kaufman N, Hatsukami D, Walsh M, Orleans C. Survey of spit tobacco cessation among professional baseball players. Paper presented at: Annual Meeting of the Society of Behavioral Medicine; April 5–8, 2000; Nashville, TN. [Google Scholar]
- 31.Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–3287. [PubMed] [Google Scholar]
- 32.Robertson PB, DeRouen TA, Ernster V, et al. Smokeless tobacco use: how it affects the performance of major league baseball players. J Am Dent Assoc. 1995;126:1115–1121. doi: 10.14219/jada.archive.1995.0328. [DOI] [PubMed] [Google Scholar]
- 33.Mittelmark MB. The psychology of social influence and healthy public policy. Prev Med. 1999;29(6 Pt 2):S24–S29. doi: 10.1006/pmed.1998.0468. [DOI] [PubMed] [Google Scholar]
- 34.Edwards J. Frameworks for applying social psychological processes to social issues. In: Edwards J, Tindale RS, Heath L, Posavac E, editors. Social Influence Processes and Prevention. New York, NY: Plenum; 1990. [Google Scholar]
- 35.Jones E. Major developments in social psychology during the past five decades. In: Lindzey G, Aronson E, editors. Handbook of Social Psychology. Vol I. New York, NY: Random House; 1985. pp. 47–107. [Google Scholar]
- 36.Eagly AH, Chaiken S. The Psychology of Attitudes. New York, NY: Harcourt Brace Jovanovich; 1993. [Google Scholar]
- 37.Tesser A, editor. Advanced Social Psychology. New York, NY: McGraw-Hill; 1995. [Google Scholar]
- 38.Gottlieb NH, Levenson-Gingiss P, Weinstein RP. Attitudes, subjective norms and models of use for smokeless tobacco among college athletes: implications for prevention and cessation programming. Health Educ Res. 1992;7:359–368. [Google Scholar]
- 39.Levenson-Gingiss PL. Peer coaching: building collegial support for using innovative health problems. J Sch Health. 1993;63:79–85. doi: 10.1111/j.1746-1561.1993.tb06085.x. [DOI] [PubMed] [Google Scholar]
- 40.Ernster VL. Advertising and promotion of smokeless tobacco products. In: Boyd GM, Darby CA, editors. Smokeless Tobacco Use in the United States. Bethesda, MD: National Cancer Institute; 1989. pp. 87–94. [PubMed] [Google Scholar]
- 41.Promotional spending for smokeless tobacco increased 21% in 1997. Wall Street Journal. 1999 Jan 13;:A13. [Google Scholar]
- 42.Siegel D, Benowitz N, Ernster VL, Grady DG, Hauck WW. Smokeless tobacco, cardiovascular risk factors, and nicotine and cotinine levels in professional baseball players. Am J Public Health. 1992;82:417–421. doi: 10.2105/ajph.82.3.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Henningfield JE, Radzius A, Cone EJ. Estimation of available nicotine content of six smokeless tobacco products. Tob Control. 1995;4:57–61. [Google Scholar]
- 44.Hatsukami DK, Severson HH. Oral spit tobacco: addiction, prevention and treatment. Nicotine Tob Res. 1999;1:21–41. doi: 10.1080/14622299050011131. [DOI] [PubMed] [Google Scholar]
- 45.Hatsukami DK, Boyle RG. Prevention and treatment of smokeless tobacco use. Adv Dent Res. 1997;11:342–349. doi: 10.1177/08959374970110030601. [DOI] [PubMed] [Google Scholar]
- 46.Jorneby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med. 1999;340:685–691. doi: 10.1056/NEJM199903043400903. [DOI] [PubMed] [Google Scholar]
- 47.Zyban prescribing information, RL-1066. GlaxoSmithKline. Available at: http://www.ghk.com/products/prescriptionmedications. Accessed November 19, 2002.
- 48.Orleans CT, Connolly GN, Workman S. Beat the Smokeless Habit. Bethesda, MD: National Cancer Institute, Major League Baseball, Fox Chase Center, National Institutes of Dental Research, Professional Baseball Athletic Trainers Society, National Collegiate Athletic Association; 1993. [Google Scholar]
- 49.Kelly JA, St. Lawrence JS, Diaz YE, et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perry CL, Kelder SH. Models for effective prevention. J Adolesc Health. 1992;13:355–363. doi: 10.1016/1054-139x(92)90028-a. [DOI] [PubMed] [Google Scholar]


