Background and epidemiology: Between May 15 and June 11, 2003, 50 people in Wisconsin, Illinois, Indiana and New Jersey were found to have human monkeypox.1 All of the individuals, ranging in age from 4 to 48 years, had contact with ill prairie dogs purchased as pets from exotic pet stores. Investigations are underway to determine whether the animals had come from the same supplier.
Human monkeypox, like smallpox, is a member of the genus Orthopoxvirus. Its manifestations are similar to those of smallpox but tend to be less severe. Until the recent outbreak in the United States, monkeypox has been limited mainly to sporadic cases in remote villages in western and central Africa, where it is thought to result from close contact between humans and animals living in the rain forests. Animals that harbour the virus include nonhuman primates, lagomorphs (rabbits) and some rodents. Person-to-person spread has historically been infrequent, usually ending after 1 or 2 generations of transmission, but the epidemiologic features of an outbreak in the Democratic Republic of the Congo suggests higher rates of infection.
Human monkeypox appears to be prevented by smallpox (vaccinia) vaccination (vaccine efficacy in preventing monkeypox is about 85%). In an outbreak of human monkeypox in the Democratic Republic of the Congo in 1996/97, a total of 338 cases were identified (of which 67% were confirmed by viral culture).2 The case-fatality rate among individuals not vaccinated with vaccinia was 9.8%. Case-fatality rates in Africa have ranged from 1% to 10%; there have been no deaths in the US outbreak so far. Since vaccinia vaccination has been stopped in children born after 1980, an increase in the frequency of human monkeypox is likely the result of decreased herd immunity. The US Centers for Disease Control and Prevention (CDC) is expected to make vaccines available to health care workers who care for patients with monkeypox.
Clinical management: The cases reported in the United States were typical of human monkeypox (see Box for case definition). After an incubation period of about 12 days, the illness begins with a nonspecific prodrome that lasts 1–10 days and consists of fever, headache, myalgia, chills and drenching sweats. About one third of the patients in the US outbreak had a nonproductive cough. The rash that typically follows this phase is initially papular and progresses through stages of vesiculation, pustulation, umbilication (a depression at the apex of a lesion) and crusting. In some patients the early lesions become ulcerated. The rash often begins on the face and is distributed on the head, trunk and extremities. Many patients have initial and satellite lesions on their palms, soles and extremities (see Figure). (For additional photographs go to http://research.marshfieldclinic.org/crc/monkeypox.asp). Unlike smallpox, which tends to have lesions at similar stages of evolution, rashes caused by monkeypox tend to occur in crops.3 Also, lymphadenopathy is more common with monkeypox.
Box 1.
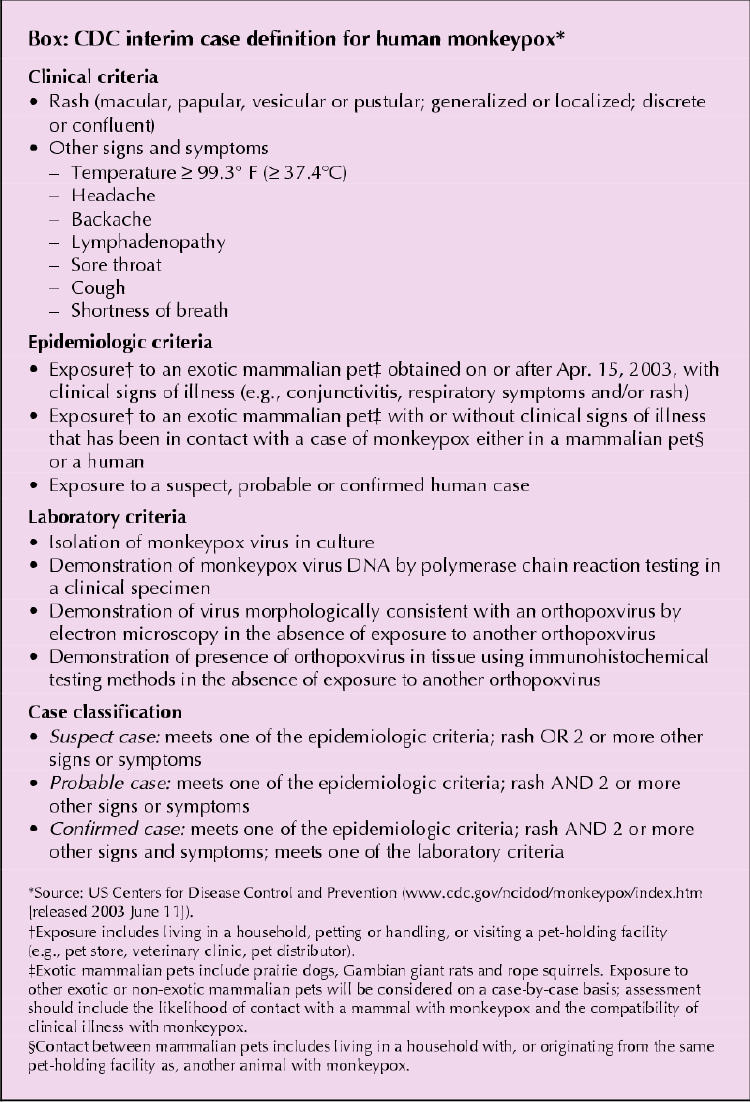

Figure 1. Lesions on the hand of a child with human monkeypox after being bitten by a pet prairie dog. Photo: Marshfield Clinic
The infected prairie dogs involved in the US outbreak reportedly had blepharoconjunctivitis, which progressed to nodular lesions in some cases. Some of the animals succumbed to the disease.
Laboratory studies can identify the virus through culture or DNA amplification of samples from skin lesions. In addition, antibody neutralization assays can detect antibodies against orthopoxovirus. IgM antibodies against varicella virus have also been detected in studies investigating outbreaks of monkeypox; this was either the result of a misclassification (both are eruptive diseases) or coinfection. There is no specific treatment, although the CDC is assessing the potential role of postexposure smallpox vaccination and of the antiviral drug cidofovir.
Patients presenting with the prodromal symptoms and rash as described above and who have had exposure to potentially infected small mammals should be managed with airborne and droplet precautions. Individuals suspected of having the disease should be isolated, and asymptomatic contacts should be placed under symptom surveillance. Further guidance is offered on the CDC Web site (www.cdc.gov/ncidod/monkeypox/infectioncontrol.htm).
Prevention: Until the epidemiologic features and distribution of this most recently arrived (in North America) pathogen has been elucidated, the CDC recommends that people avoid contact with any prairie dogs or Gambian giant rats that appear to be ill (e.g., are missing patches of fur, have a visible rash on the skin or have discharge from eyes or nose). In addition, the CDC advises hand washing after any contact with prairie dogs, Gambian giant rats or any ill animal.
James Maskalyk Editorial Fellow CMAJ
Footnotes
Published at www.cmaj.ca on June 13, 2003.
References
- 1.Preliminary report: multistate outbreak of monkeypox in persons exposed to pet prairie dogs. Atlanta: US Centers for Disease Control and Prevention; 2003 June 9. Available: www.cdc.gov/ncidod/monkeypox/report060903.htm (accessed 2003 June 9).
- 2.Hutin YJ, Williams RJ, Malfait P, Pebody R, Loparev VN, Ropp SL, et al. Outbreak of human monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerg Infect Dis 2001; 7(3):434-8. Available: www.cdc.gov/ncidod/eid/vol7no3/hutin.htm (accessed 2003 June 9). [DOI] [PMC free article] [PubMed]
- 3.Diven DG. An overview of poxviruses. J Am Acad Dermatol 2001;44(1):1-16. [DOI] [PubMed]


