Abstract
Equine arteritis virus (EAV) is an enveloped plus-strand RNA virus of the family Arteriviridae (order Nidovirales) that causes respiratory and reproductive disease in equids. Protective, virus-neutralizing antibodies (VNAb) elicited by infection are directed predominantly against an immunodominant region in the membrane-proximal domain of the viral envelope glycoprotein GL, allowing recently the establishment of a sensitive peptide enzyme-linked immunosorbent assay (ELISA) based on this particular domain (J. Nugent et al., J. Virol. Methods 90:167-183, 2000). By using an infectious cDNA we have now generated, in the controlled background of a nonvirulent virus, a mutant EAV from which this immunodominant domain was deleted. This virus, EAV-GLΔ, replicated to normal titers in culture cells, although at a slower rate than wild-type EAV, and caused an asymptomatic infection in ponies. The antibodies induced neutralized the mutant virus efficiently in vitro but reacted poorly to wild-type EAV strains. Nevertheless, when inoculated subsequently with virulent EAV, the immunized animals, in contrast to nonvaccinated controls, were fully protected against disease; replication of the challenge virus occurred briefly at low though detectable levels. The levels of protection achieved suggest that an immune effector mechanism other than VNAb plays an important role in protection against infection. As expected, infection with EAV-GLΔ did not induce a measurable response in our GL-peptide ELISA while the challenge infection of the animals clearly did. EAV-GLΔ or similar mutants are therefore attractive marker vaccine candidates, enabling serological discrimination between vaccinated and wild-type virus-infected animals.
Equine arteritis virus (EAV), a plus-strand RNA virus of the family Arteriviridae (order Nidovirales), is a worldwide pathogen for horses and donkeys. The virus was first isolated from lung tissue of fetuses aborted during an outbreak in Ohio in 1953 (25, 27) and became the prototype arterivirus; it was joined later by the lactate dehydrogenase-elevating virus of mice, simian hemorrhagic fever virus, and porcine reproductive and respiratory syndrome virus. Though the virus infects cells from quite a variety of origins in vitro, its host range in nature is narrowly restricted to equids (17, 19, 36, 52, 54).
In the horse clinical signs of infection vary widely and appear to depend on the particular strain and dose of the virus, the age and physical condition of the animal, and possibly also the route of infection (58, 60). While epidemiological studies indicate that natural infections often occur asymptomatically (16, 46, 61), affected animals may develop moderate-to-severe symptoms as well. Lethal infections of horses with EAV have been reported only under experimental conditions (12, 29).
While infected horses usually recover after cessation of viremia, foal death as a result of rapidly progressive bronchointerstitial pneumonia and intestinal necrosis can occur in young and adolescent pregnant mares. In mares EAV infection does not seem to affect fertility. Stallions may, however, temporarily exhibit fertility problems due to a reduced production of morphologically normal sperm cells during the first months after infection (48).
Transmission of EAV occurs via the respiratory route through direct contact with infectious aerosolized nasopharyngeal secretions from acutely infected horses or other secretions such as urine; feces and vaginal fluids; and fetal, placental, and amniotic materials aborted by mares as a result of EAV infection (60). In addition, infected stallions play an important role in the epidemiology of the infection as the virus can be transmitted very efficiently by the venereal route. Acutely infected stallions usually secrete virus with their semen. Moreover, a proportion of infected stallions ranging from 30 to 50%, depending on horse breed, become persistently infected, excreting the virus in their semen for months or years.
EAV is an enveloped virus. The 12.7-kb RNA genome is packaged by the nucleocapsid protein (N) into an isometric nucleocapsid (38, 74) that is in turn surrounded by a lipid membrane. This envelope contains six proteins. The predominant ones are the GL and M proteins (21), two apparently triple spanning membrane proteins, the former one of which is N glycosylated. These proteins occur as disulfide-linked dimers (23). The remaining four are a small unglycosylated (E) protein (55) and three minor glycoproteins (GP2b, GP3, and GP4) (21, 71), which occur in a heterotrimeric complex (70).
Infection of horses by EAV induces antibodies mainly against the three major viral structural proteins (N, M, and GL). This humoral immune response is presently considered to be the most important factor mediating the recovery of animals from EAV infection as well as providing the long-lasting immunity that protects the animals from future EAV-related disease, though rarely from reinfection. Indeed, virus-neutralizing antibodies (VNAb) start to appear 1 to 2 weeks after primary infection, and their appearance usually coincides with the clearance of virus from the circulation (30, 42). Accordingly, passive transfer of colostrum antibodies from immune mares to foals was found to moderate or prevent EAV disease (45). Inactivated virus preparations, even when administered in nonadjuvanted form, have been demonstrated to elicit high levels of VNAb after repeated application and to provide protection against disease upon experimental EAV infection (13, 31-34).
The VNAb mapped so far are all directed against the GL protein (7-9, 15, 18, 35, 67, 68) or, more specifically, against the ectodomain thereof (7, 8, 18, 35). Although four different neutralization sites within this approximately 115-residue domain (including the signal peptide) have been distinguished, the vast majority of neutralizing monoclonal antibodies (MAbs) map to the membrane-proximal region (residues 67 to 106, which includes two of the neutralization sites), and this is clearly the immunodominant part of the protein (7, 8, 11, 35, 56, 57, 73). Consistently, peptides representing the entire GL ectodomain or parts of its immunodominant region induced VNAb (7, 14, 15), while a recombinant protein containing the complete ectodomain (residues 18 to 122) conferred protection in ponies against experimental infection (14). Surprisingly, expression of the GL protein by using an alphavirus vector induced antibodies against the protein in mice (6) and horses (5), but these were not virus neutralizing or protective against EAV infection. Only when the M protein was additionally coexpressed were these antiviral effects observed.
The present study describes the generation of a EAV deletion mutant, denoted EAV-GLΔ, which lacks amino acids (aa) 66 to 112 of the putative ectodomain of the EAV GL protein. The virus's replication features in vitro and its biological properties in vivo, including its immunogenicity, were studied to explore the potential for this approach to generate a marker vaccine against EAV infection. The modification introduced was based on the fact that this region is immunodominant, and deletion of the corresponding region was found in a neutralization escape mutant which retained its capacity to infect RK-13 cells (8). It is also known that the entire GL ectodomain of EAV may be replaced by the corresponding domains from other arteriviruses and still retain viability (24). Furthermore, the peptide antigen GL-OVA (aa 81 to 106), which forms the basis of an already-developed diagnostic enzyme-linked immunosorbent assay (ELISA) (49), is contained within the deleted sequence, theoretically permitting the serological discrimination between vaccinated and infected animals. We further wished to test whether removal of the immunodominant region of GL would affect the capacity of the deletion mutant virus to induce VNAb and, if so, whether the resulting immune response would protect against challenge EAV infection.
MATERIALS AND METHODS
Cells and viruses.
Baby hamster kidney cells (BHK-21 C13; American Type Culture Collection) were cultured in Glasgow minimal essential medium (GMEM; GIBCO BRL Life Technologies) supplemented with 10% heat-inactivated fetal bovine serum (FBS), 100 IU of penicillin per ml, and 100 μg of streptomycin per ml (GMEM-10% FBS). Primary equine embryonic lung cells (EELs; fibroblastoid) were obtained from an established in-house cell line prepared from an aborted fetus. This cell line was tested and found to be free of mycoplasma or equine viruses. The cells were maintained in Eagle minimum essential medium with Earle's salts (EMEM) (Sigma; M2279) supplemented with 100 IU of penicillin per ml, 10 μg of streptomycin per ml, nonessential amino acids, l-glutamine to a final concentration of 2 mM, and 10% heat-inactivated FBS (EMEM-10% FBS). For the in vitro studies, concentrated stocks of the Utrecht derivative of the Bucyrus strain of EAV were prepared as described earlier (21), except that the virus was finally suspended in GMEM-10% FBS. The EAV LP3A+ virus stock, a single-passage derivative in EEL cells of LP3A (14), was used for challenge infection of ponies as well as for serological testing together with the CVL Bucyrus EAV strain (28). These two viruses differ at some positions in their open reading frame 5 (ORF5) genes but show a high degree of antigenic cross-reactivity (14).
Antibodies.
To generate an antiserum directed against the carboxy terminus of the EAV GL protein (αGLC), the protein endodomain was synthesized in Escherichia coli as a fusion protein containing the glutathione S-transferase protein of Schistosoma japonicum at the amino terminus. To this end, the relevant part of EAV ORF5 (20) was amplified from cDNA clone PB106 by PCR using the primers 750 and 439 (Table 1). Both primers contain a 5′ extension introducing a BamHI restriction enzyme recognition site. The PCR product was digested with BamHI and ligated into a BamHI-digested pGEX-3X vector (Amersham Pharmacia Biotech), yielding pAVFP55. The fusion protein was then expressed in PC2495 cells (Phabagen) by standard procedures. The bacteria were subsequently pelleted by centrifugation for 15 min at 5,500 rpm and 4°C in a JA10 rotor (Beckman). The cell pellet was resuspended in 50 ml of ice-cold 50 mM Tris-HCl (pH 8.0)-2 mM EDTA-100 μg of lysozyme per ml, followed by an incubation for 20 min at 30°C. The suspension was then sonicated three times for 10 s with the pulse control set at 10 at 4°C with a Sonifier B-10 cell disruptor (Branson Sonic Power Company). After centrifugation for 15 min at 10,000 rpm and 4°C in a JA20 rotor (Beckman), the pellet was washed with demineralized water, with 50 mM Tris-HCl (pH 8.0)-5 mM EDTA-1 M urea, and then with 50 mM Tris-HCl (pH 8.0)-5 mM EDTA-2 M urea. After a final wash with demineralized water and another round of centrifugation, the pellet was resuspended in 5 ml of Laemmli sample buffer (40) containing 50 mM dithiothreitol. Subsequently, the sample was loaded on a preparative sodium dodecyl sulfate (SDS)-12.5% polyacrylamide gel. After electrophoresis, the gel was stained by incubation with 0.2 M imidazole-0.1% SDS and then with 0.2 M ZnSO4 (37). The part of the gel containing the fusion protein was excised and cut up. Next, the protein present in these gel fragments was eluted either passively by incubation overnight in phosphate-buffered saline at room temperature or by electroelution with a homemade device. The protein eluates were pooled and used to immunize a New Zealand White rabbit essentially as described previously (71).
TABLE 1.
Oligonucleotides
| Name (polarity) | Sequence (5′-3′)b | Positiona | Use |
|---|---|---|---|
| A2 (−) | TAAGCGTAGCATAGGGTAG | 11557-11575 | RT-PCR |
| A3 (−) | CCGCTGTAAATGCCATAG | 11610-11627 | RT-PCR |
| 439 (−) | CGGGATCCACCTAAAAATCCCGTCACCAC | 11923-11943 | Production of αGLC |
| 480 (−) | CGGGATCCAACACAACTATGCCG | 11493-11511 | Sequencing |
| 750 (+) | CGGGATCCTCCGCCAATTACTGTGGTT | 11684-11705 | Production of αGLC |
| JV1 (−) | TTACGACTGGTACGTTGGG | 11120-11138 | RT-PCR |
| JV2 (−) | GATACTCACCTAAAATCCCG | 11930-11949 | RT-PCR |
| 983 (−) | GAGAATTCACGGCCATACCAACAGGTTTTACTGGCGGAAC | 11315-11340 + 11482-11493 | Generation of EAV-GLΔ |
| 984 (+) | CTTGCGTGCAAGTGGTTG | 10628-10637 | Generation of EAV-GLΔ and RT-PCR |
Nucleotide sequence of the Utrecht variant of the EAV CVL Bucyrus strain.
The 5′ extensions used to introduce BamHI enzyme recognition sites are in boldface.
The production and characterization of the rabbit antipeptide sera αSP25, raised against aa 75 through 95 of the EAV GL protein, and αSP06, directed against the carboxy terminus of the EAV M protein, have been documented elsewhere (21, 23). The EAV GL-specific murine MAbs 74D(B) and 93B were generated by Glaser et al. (35).
Construction of EAV-GLΔ.
DNA techniques were performed essentially as described by Sambrook et al. (53). To construct pEANGLΔ, a PCR product was synthesized with the oligonucleotides 983 and 984 and pEAN515 as the DNA template. The plasmid pEAN515 is a derivative of EAV infectious cDNA clone pEAV030-BglII KO (22, 63) in which the cryptic transcription termination signal at position 8941 to 8956 was removed by site-directed mutagenesis and an MscI site was simultaneously created (mutations: A8941C, T8945A, C8946G, T8947C, T8950C, and G8956C). The resulting PCR fragment (724 nucleotides) was treated with BglII and EcoRI, and the 638-bp digestion product was cloned into BglII- and EcoRI-digested pEAN515 and sequenced. EAV RNA was transcribed in vitro from pEANGLΔ and from pEAN515, and parallel cultures of BHK-21 C13 cells were transfected with the synthetic RNAs by electroporation essentially as described by de Vries et al. (22). Infections and mock infections of BHK-21 cells with wild-type or mutant EAV at a high multiplicity of infection (MOI) have also been previously reported (71).
Reverse transcription-PCR (RT-PCR) and sequencing.
Viral RNA was purified from supernatants of infected cells and reverse transcribed and PCRs were performed all by using standard procedures. The primers used in these experiments are listed in Table 1.
Preparation of radiolabeled virions.
Subconfluent monolayers of BHK-21 C13 cells were infected with EAV at an MOI of >10. At 6 h postinfection (p.i.) the medium was removed, and the cells were washed with prewarmed starvation medium and incubated in 800 μl of the same medium. When indicated (see Fig. 4B) 1 mM 1-deoxymannojirimycin (DMJ; Boehringer Mannheim) was added to the starvation mixture. After a 30-min incubation at 39°C, 80 μCi of Redivue Pro-mix cell labeling mixture (Amersham Pharmacia Biotech.) was added and the cells were further incubated at 39°C. At 12 h p.i. the medium was harvested and cleared by centrifugation for 10 min at 4,000 rpm in an Eppendorf centrifuge. The supernatant was then mixed with 1/4 volume of 5× lysis buffer (100 mM Tris-HCl [pH 7.6]-150 mM NaCl-5% Nonidet P-40-2.5% sodium deoxycholate-0.5% SDS containing 5 μg each of aprotinin, leupeptin, and pepstatin A per ml) supplemented with 100 mM N-ethylmaleimide (NEM). The lysate was cleared and supplemented with EDTA (final concentration, 5 mM).
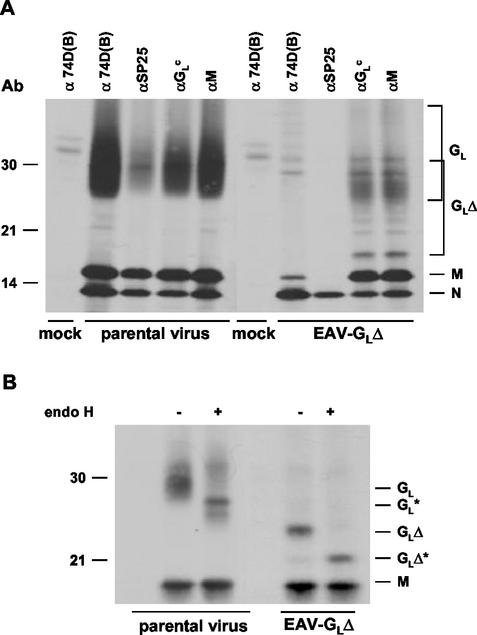
FIG. 4.
Immunoprecipitation analysis of EAV-GLΔ. EAV-GLΔ-infected, parental-virus-infected, and mock-infected BHK-21 C13 cells were labeled with [35S]methionine from 6.5 to 12 h p.i. in the absence (A) or presence (B) of DMJ. After removal of cell debris by low-speed centrifugation, the labeled virus present in the cell culture medium was dissociated in lysis buffer containing 20 mM NEM and subjected to immunoprecipitation. (A) Samples were immunoprecipitated either with the MAb 74D(B) or the antipeptide sera αGLC and αSP25 (all against GL) or with the antipeptide serum αM (directed against peptide SP06 derived from the M protein). (B) Samples were immunoprecipitated with αGLC. The immunoprecipitates were treated (+) or mock treated (−) with endo H as indicated. Samples were finally dissolved in Laemmli sample buffer containing 50 mM dithiothreitol and analyzed by SDS-15% polyacrylamide gel electrophoresis. Numbers on the left refer to positions of the molecular mass markers (in kilodaltons). Asterisks, positions of the deglycosylated GL polypeptides.
Characterization of EAV-GLΔ by neutralization test.
Portions of EAV stock (100 tissue culture infective doses [TCID50]) diluted in GMEM were mixed in parallel in 96-well microtiter plates with 6.25 μl of different horse sera or a similar volume of culture supernatant of hybridoma cells producing MAb 93B or 74D(B) or a similar volume of the rabbit serum αSP25. The plates were then incubated for 1 h at room temperature, after which 6.1 μl of guinea pig complement (Sigma) was added (final concentration, 10%). After another 1-h incubation at 37°C approximately 105 BHK-21 C13 cells in 250 μl were added. Individual wells were scored for cytopathic effect (CPE) following a 48- to 120-h incubation at 37°C. Each individual virus neutralization test was performed in triplicate.
In addition a titration experiment was performed as described earlier (14) using a number of sera from horses that had been inoculated with EAV strain LP3A or its derivative LP3A+. VNAb titers against the EAV strain CVL Bucyrus and against EAV-GLΔ were determined in parallel.
Immunoprecipitation and gel electrophoresis.
Proteins were immunoprecipitated from cell lysates or solubilized virions and analyzed in SDS-15% polyacrylamide gels essentially as described previously (71). The samples were incubated for 15 min at room temperature before being applied to the gel. After electrophoresis the gels were processed for fluorography and exposed at −80°C to Kodak X-ray films as previously reported (71).
Endoglycosidase treatment.
Washed immunoprecipitates were treated with endoglycosidase H (endo H) essentially as described previously (70).
Vaccination and challenge infections of ponies.
The EAV-GLΔ inoculum was prepared by infection of EELs at an MOI of approximately 0.002 with BHK-21 C13-derived virus and incubation for 72 h at 37°C. The tissue culture fluid was then harvested and freeze-thawed, cell debris was removed by centrifugation, and aliquots of the supernatant were stored at −70°C. Procedures for EAV inoculation of ponies have been described previously (14). Two-year-old castrated male Welsh Mountain Ponies (5062, 697b, 7b69, and 07d41), seronegative for EAV, were used in this study. Ponies 7b69 and 07d41 were stabled in a contained environment facility and inoculated with 106 TCID50 of EAV-GLΔ by the intranasopharyngeal route and monitored closely for 28 days. Nasopharyngeal swabs, heparinized blood, and serum samples were collected at regular intervals and analyzed for virus and antibodies as described below. After infectious virus could no longer be detected, the ponies were released from containment to an isolated barn. Forty-six days after the immunization ponies 7b69 and 07d41 and EAV-seronegative ponies 5062 and 697b were inoculated with 106.1 TCID50 of EAV strain LP3A+. All four ponies were clinically inspected twice a day, and serum, heparinized blood, and nasopharyngeal swabs were collected at regular intervals until the end of the study. The ponies were released to a third isolated barn when they were regarded as noninfectious; they were transferred 2 weeks later to an isolated paddock for 4 weeks before they were allowed to have contact with any other equines.
Virus isolation and serology.
Virus isolation from blood and nasopharyngeal samples and VNAb assays were conducted as previously described (14). The virus neutralization test was performed with three different EAV strains: LP3A+, CVL Bucyrus, and EAV-GLΔ. Antibody responses to two GL-derived antigens were analyzed by ELISA in accordance with the procedures described by Nugent et al. (49) with minor modifications. The antigens chosen were an ovalbumin-conjugated synthetic peptide representing aa 81 to 106 of GL (GL-OVA), a region deleted in EAV-GLΔ, and a six-histidine-tagged recombinant protein expressing the complete GL ectodomain (residues 18 to 122; GL-6His), both described earlier (49).
RESULTS
Construction of the EAV deletion mutant EAV-GLΔ.
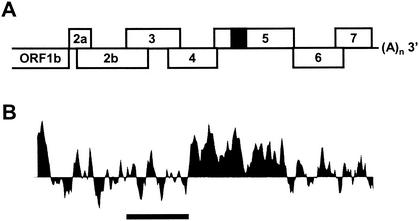
To delete the immunodominant domain of GL and thereby obtain a potential marker vaccine virus, an EAV infectious cDNA mutant clone with a deletion of the gene segment specifying residues 66 to 112 of the GL protein was constructed (Fig. 1). For this purpose we used the primers 984 (positive polarity) and 983 (negative polarity), and infectious cDNA clone pEAN515 served as the template. Primer 984 hybridizes upstream of a unique BglII site. Primer 983 hybridizes just upstream of the proposed deletion and contains an extension corresponding to the oligonucleotide sequence just downstream of the deletion, ending after a unique EcoRI site. The resulting 724-nucleotide PCR fragment was treated with BglII and EcoRI, and the 638-bp digestion product was cloned into BglII- and EcoRI-digested pEAN515, yielding pEANGLΔ. The nucleotide sequence of the insert was verified by sequencing. In addition, the restriction patterns of pEANGLΔ and its parent plasmid, pEAN515, obtained after digestion with BglII and EcoRI were compared, which confirmed the expected size reduction of the released fragment.
FIG. 1.
(A) Representation of the 3′ part of the EAV genome. Black box in ORF5, region deleted in the EAV-GLΔ mutant. (B) Hydropathy profile of the EAV GL protein as determined by the method of Kyte and Doolittle (39) with a seven-residue moving window. Peaks extending upward indicate hydrophobic domains, and those pointing downward correspond to hydrophilic regions. Black bar, region deleted in the EAV-GLΔ mutant.
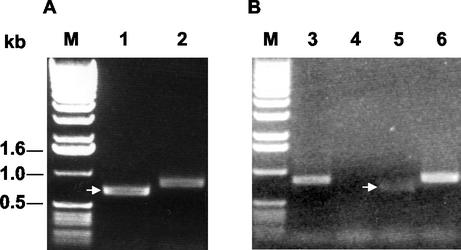
Subsequently, BHK-21 C13 cells were transfected in parallel with in vitro RNA transcripts derived from pEANGLΔ or from the parental construct. After electroporation, clear CPE developed in the cells for both constructs, indicating that EAV-GLΔ was viable. To investigate the presence and stability of the mutation, the virus in the culture medium of the electroporated cells was passaged four times in BHK-21 C13 cells, after which viral RNA was purified from the culture supernatants of the infected cells and the relevant genome segment was amplified by RT-PCR using primers 984 and A2. The resulting PCR product was cloned into the pGEM-T Easy vector and sequenced. As shown in Fig. 2 the deletion was still present; no other mutation could be observed in the PCR product, although point mutations elsewhere in the viral genome can obviously not be excluded.
FIG. 2.
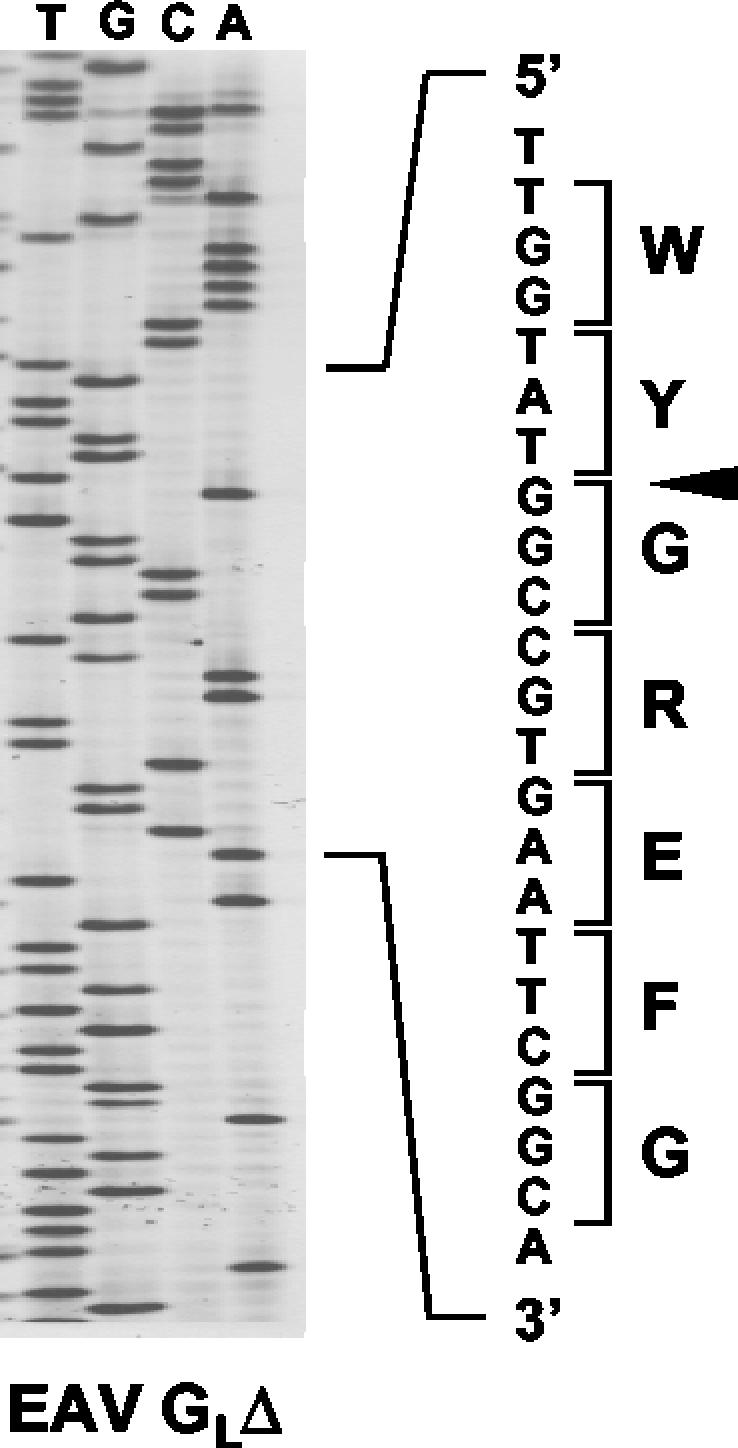
RT-PCR analysis of the EAV-GLΔ virus. Viral RNA was purified from supernatants of EAV-GLΔ-infected cells. cDNA synthesis was primed with primer (polarities are in parentheses) A3 (−); for PCR amplification primers 984 (+) and A2 (−) were used. The RT-PCR product was cloned into the pGEM-T Easy vector and sequenced. The nucleotide sequence of the relevant part of ORF5 and the deduced amino acid sequence are shown. Arrowhead, site of deletion.
Growth properties of the EAV-GLΔ mutant.
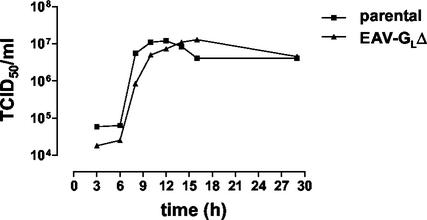
To investigate possible effects of the deletion in the GL protein on virus growth, BHK-21 C13 cells were infected in parallel at similar high (>10) MOIs with the EAV-GLΔ mutant or the parental virus. Subsequently, aliquots were taken from the culture supernatants at different times, and their infectious titers were determined. As Fig. 3 shows, the one-step growth curves of the viruses are very similar. The EAV-GLΔ mutant reproducibly exhibited a slightly slower onset of extracellular virus production, reaching its maximal titer a few hours later than its parent virus. The maximal titers reached by both viruses were, however, quite comparable. Consistently, the times of development of CPE during the infections were also very similar, that of the mutant again seeming slightly delayed. Similarly, in multistep growth curves, the mutant virus replicated with slightly slower kinetics than, but reached titers similar to, those for the wild-type virus LP3A+, used for the challenge infections (data not shown).
FIG. 3.
One-step growth curve for EAV-GLΔ. BHK-21 C13 cell cultures were infected in parallel at high MOI with the EAV-GLΔ mutant and the parental virus. Samples were taken from the culture supernatants at different times p.i., and their infectivity titers were determined.
Analysis of the GL protein of EAV-GLΔ.
We also studied the size and the antigenic properties of the GL protein of the deletion mutant virus. BHK-21 C13 cells were mock infected or infected with EAV-GLΔ or the parental virus and labeled with [35S]methionine. Labeled EAV particles present in the culture supernatants were dissociated by detergents in the presence of 20 mM NEM and subjected to immunoprecipitation with different antibodies directed against the EAV GL protein and with an antiserum directed against the M protein and analyzed by SDS-polyacrylamide gel electrophoresis. As Fig. 4A reveals, the parental GL protein was precipitated when each of these antibodies was used. It migrated as the well-known collection of heterogeneously glycosylated proteins of about 30 to 38 kDa (21). Also the GLΔ protein behaved heterogeneously: after immunoprecipitation with the αGLC serum, which is directed against the protein's carboxy terminus, it was seen as a smear of about 28 to 34 kDa, i.e., running slightly faster than the wild-type protein. In addition, a protein of 19 kDa was immunoprecipitated; this protein, as discussed below, probably represents the unglycosylated GLΔ protein. As expected, the GLΔ protein was not immunoprecipitated by MAbs 74D(B) and αSP25, since these antibodies recognize the deleted region. Furthermore, like the wild-type GL and M proteins, the GLΔ protein appears to be disulfide linked to M because the two proteins were coprecipitated both by the GLC antiserum and by the anti-M serum. The apparently lower ratios of GLΔ levels to M levels in the EAV-GLΔ particles than in wild-type EAV (Fig. 4A) probably relate to differences in glycosylation as these differences are not obvious when the viruses are grown in the presence of DMJ (Fig. 4B). The identity of the approximately 17-kDa protein which was immunoprecipitated from the EAV-GLΔ material by MAb 74D(B) and which comigrated with the M protein is not clear. The protein is probably precipitated nonspecifically by MAb 74D(B), since a protein of similar size is also seen in immunoprecipitates with different preimmune sera (70, 71). A protein of 13 kDa represents the EAV nucleocapsid protein, which is known to be immunoprecipitated nonspecifically (62).
Because their heterogeneous glycosylation precluded a careful size comparison of wild-type and mutant GL proteins, we repeated the labeling in the presence and absence of DMJ, an inhibitor of N-linked oligosaccharide processing. Viral particles in the culture supernatant were solubilized, and proteins were subjected to immunoprecipitation with the GLC serum or its corresponding preserum, after which the precipitates were treated or mock treated with endo H, which cleaves unprocessed oligosaccharides. The electrophoretic analysis (Fig. 4B) shows that the inhibitor indeed prevented the extensive glycosylation, thereby clearly revealing the size difference between the wild-type and the mutant GL proteins. In addition, the deglycosylation by endo H reduced the apparent sizes of both proteins similarly, indicating that they carried the same number (i.e., one) of sugar side chains. Finally, the mobility difference between the deglycosylated proteins is consistent with the predicted approximately 5-kDa molecular mass difference resulting from the 47-residue deletion.
Neutralization of EAV-GLΔ by antibodies.
To study the effect of the deletion on virus neutralization in vitro, a virus neutralization assay was performed using the MAbs 93B and 74D(B), the rabbit antipeptide serum αSP25, three horse sera positive for EAV antibodies, and two seronegative horse sera (Table 2). The MAbs 93B and 74D(B) and αSP25 recognize epitopes in the region deleted from the GL protein ectodomain. It turned out that the EAV antibody-positive horse sera were able to neutralize both EAV-GLΔ and the parental virus. In contrast, while the two MAbs and αSP25 efficiently blocked infection by the parental virus, they were unable to affect the infectivity of the EAV-GLΔ mutant virus. The two seronegative horse sera were unreactive to either virus.
TABLE 2.
Sensitivity of mutant and parental virus to neutralization by different antibodies
| Serum or MAba | Ability to neutralize:b
|
|
|---|---|---|
| EAV-GLΔ | Parental virus | |
| MAb 74D(B) | − | + |
| MAb 93B | − | + |
| αSP25 | − | + |
| Gar (EAV pos.) | + | + |
| Cyr (EAV pos.) | + | + |
| Jip (EAV pos.) | + | + |
| Gie (EAV neg.) | − | − |
| Ig (EAV neg.) | − | − |
The presence (pos.) or absence (neg.) of antibodies against EAV is indicated in parentheses.
+, neutralization positive; −, neutralization negative.
In another experiment we comparatively analyzed the VNAb titers of a panel of sera collected from horses experimentally infected with the virulent EAV strain LP3A or its single-passage derivative LP3A+. These sera were titrated in parallel against EAV-GLΔ and against EAV strain CVL Bucyrus, which has a wild-type GL protein. As Table 3 shows, all sera neutralized the wild-type virus much more efficiently than the deletion virus EAV-GLΔ, which was neutralized relatively poorly.
TABLE 3.
Virus neutralization assay results
| Pony | Virus | Sampling day after inoculation | Log10 VNAb titer for:
|
|
|---|---|---|---|---|
| CVL Bucyrus | EAV-GLΔ | |||
| 6d2C | LP3A | 28 | 2.40 | 0.75 |
| 3566 | LP3A | 28 | 2.30 | 0.75 |
| 297e | LP3A | 14 | 1.95 | <0.60 |
| chnt | LP3A | 14 | 2.25 | 1.05 |
| 7378 | LP3A+ | 30 | 2.85 | 0.75 |
| 5d66 | LP3A+ | 30 | 3.40 | 1.40 |
| 027a | LP3A+ | 30 | 2.85 | 1.05 |
Immunization of ponies with EAV-GLΔ.
A stock of the mutant virus was prepared in EEL cells. An additional check for the presence of the deletion by RT-PCR as described in Materials and Methods showed the reduced size of the ORF5-derived fragment relative to that of the fragment from the wild-type CVL Bucyrus strain (Fig. 5A). Seronegative ponies 7b69 and 07d41 were inoculated with 106 TCID50 of the mutant virus by the intranasopharyngeal route. The animals were monitored daily for their general clinical features, while nasopharyngeal swabs and blood were collected at regular intervals. Neither of the two ponies exhibited any apparent signs of clinical disease. Accordingly, rectal temperatures remained normal (Table 4). However, cell-associated viremia and nasopharyngeal virus excretion were observed in both ponies, demonstrating that infections had been established. Viremia was first detected on day 4 for pony 7b69 and on day 6 for pony 07d41 and lasted until day 14 in both animals. Thereafter (days 16, 19, and 21; data not shown), virus was no longer detected in the blood. Virus excretion from the upper respiratory tract occurred essentially between days 1 and 12; the infectivity was below 101.5 TCID50/ml except for the sample collected on day 5 from pony 07d41 (101.5 TCID50/ml). RT-PCR analysis of viral RNA extracted from the virus isolated from a blood sample collected from pony 7b69 on day 4 postinoculation confirmed that the recovered virus carried the expected internal deletion in ORF5 (Fig. 5B). As will be described in more detail below, both ponies developed significant levels of serum neutralizing antibodies against the immunizing virus, but development of antibodies against EAV strains LP3A+ and CVL Bucyrus, which carry wild-type GL proteins, was weak.
FIG. 5.
RT-PCR analysis of ORF5 from EAV-GLΔ inoculated into (A) and retrieved from (B) ponies. RT-PCR amplification of ORF5 was carried out on tissue culture fluid with primers JV1 and JV2. The presence of the deletion in ORF5 both for the input virus and the virus present in the blood of one of the ponies (7b69) was checked at day 4 after inoculation with EAV-GLΔ. Lane 1, EAV-GLΔ inoculum virus prepared in EEL cells; lanes 2 and 3, wild-type EAV strain CVL Bucyrus grown in RK13 cells; lane 4, uninfected RK13 tissue culture fluid; lane 5, virus recovered in RK13 cells from an EAV-GLΔ-infected pony (7b69); lane 6, challenge virus (LP3A+) prepared in EEL cells. On the left the positions and sizes of marker DNA fragments are indicated.
TABLE 4.
Monitoring of pyrexia, viremia, and nasal virus excretion after intranasal inoculation of ponies with EAV-GLΔ
| Day | Pony 07d41
|
Pony 7b69
|
||||
|---|---|---|---|---|---|---|
| Virus isolationa from:
|
Temp (°C) | Virus isolation from:
|
Temp (°C) | |||
| Swab | Blood | Swab | Blood | |||
| 0 | 37.8 | 37.6 | ||||
| 1 | + | 37.9 | 37.9 | |||
| 2 | + | − | 37.4 | + | − | 37.4 |
| 3 | + | 37.8 | + | 37.8 | ||
| 4 | − | 37.7 | + | + | 37.9 | |
| 5 | + | 38.1 | + | 38.1 | ||
| 6 | + | + | 37.8 | + | + | 38.0 |
| 7 | + | 37.9 | + | 38.1 | ||
| 8 | + | 38.0 | + | 37.7 | ||
| 9 | ||||||
| 10 | − | + | 38.0 | − | − | 38.1 |
| 11 | ||||||
| 12 | − | + | 37.8 | + | + | 38.1 |
| 13 | ||||||
| 14 | − | + | − | + | ||
+, virus isolation positive; −, virus isolation negative.
Challenge infection of immunized ponies with virulent EAV.
To evaluate the immunity conferred by EAV-GLΔ, the two immunized ponies together with two EAV-naive controls (697b and 5062) were inoculated on day 46 after immunization with 106.1 TCID50 of the virulent EAV strain LP3A+ by the intranasopharyngeal route. All animals were again monitored clinically as well as for their virological and serological responses.
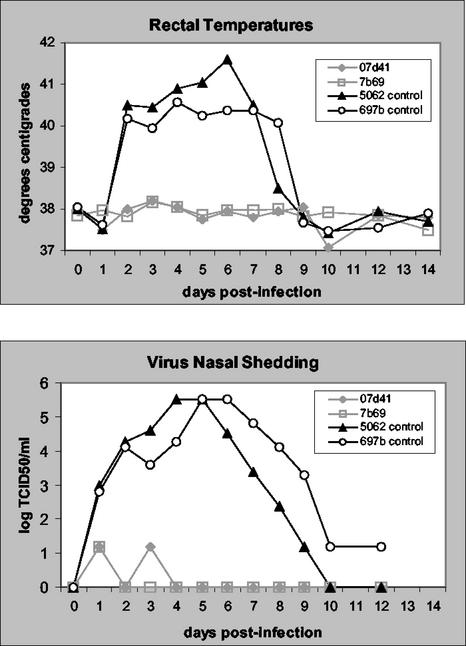
Both control ponies developed obvious clinical signs. Their symptoms included pyrexia, depression, anorexia, conjunctivitis, nasal discharge, and ataxia, the well-known sequelae of an evident EAV infection. In contrast, the preimmunized ponies 07d41 and 7b69 remained asymptomatic during the entire study period. The rectal temperatures measured during the first 2 weeks were fully consistent with these observations. As diagrammed in Fig. 6 high fever developed in the control ponies during the second day p.i. and remained for almost a week, while no obvious elevation in body temperature was observed in the vaccinated animals. Viremia was obvious in the control ponies from day 2 until day 21 p.i., whereas virus was detected only on day 8 in blood from both vaccinated ponies (data not shown). Virus was excreted from the upper respiratory tracts of the control animals during the first 10 to 12 days, peaking around day 5 p.i.; viral infectivities in the nasal swab extracts were very high (>103 TCID50/ml) between days 2 and 9 (697b) and 2 and 7 (5062), reaching maximum levels exceeding 105 TCID50/ml. In contrast, for the immunized ponies, 7b69 and 07d41, virus was isolated on only one and two occasions, respectively, and the infectivity remained below 101.5 TCID50/ml.
FIG. 6.
Pyrexia (top) and nasal virus excretion (bottom) determined over a 14-day period for prevaccinated (7b69 and 07d41) and control ponies (5062 and 697b) following intranasopharyngeal challenge with EAV strain LP3A+.
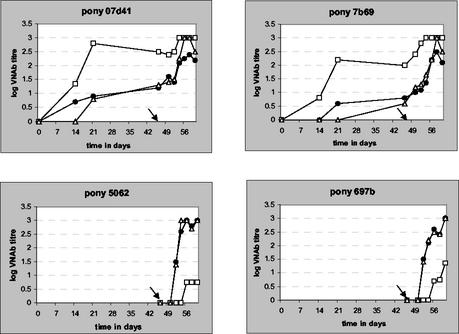
Neutralizing-antibody responses to vaccination and challenge infection.
The sera collected throughout the experiment were used to determine the development of virus-neutralizing activity in each individual animal. To evaluate the effect of the lack of the immunodominant region of GL in the vaccine virus, we analyzed the VNAb titers not only against EAV-GLΔ but also against EAV strains LP3A+ and CVL Bucyrus, which carry wild-type GL proteins. The results of the assays are compiled in Fig. 7. Following immunization, ponies 7b69 and 07d41 developed a weak VNAb response against the CVL Bucyrus and LP3A+ strains. By day 14 p.i., neutralizing antibodies against only the LP3A+ strain for a single pony were detectable. The VNAb titers increased slightly until the day of the challenge on day 46, when low log titers (less than 1.0) for both EAV wild-type strains were detectable in both ponies. In contrast, the response against EAV-GLΔ was much stronger, reaching log titers of 1.35 and 0.8 already by day 14 p.i. and 2.2 and 2.8 on day 21 for ponies 7b69 and 07d41, respectively. At the time of challenge, VNAb titers for both immunized ponies against EAV-GLΔ were at least 10 times higher than those against the wild-type strains.
FIG. 7.
Virus-neutralizing antibody responses in serum of ponies 7b69, 07d41, 5062, and 697b against EAV-GLΔ (□), LP3A+ (•), and CVL Bucyrus (▵) after intranasopharyngeal vaccination (ponies 7b69 and 07d41) with EAV-GLΔ (day 0) and intranasopharyngeal challenge infection with EAV LP3A+ (day 46; arrows).
After the challenge both immunized ponies responded with a further increase in neutralizing antibodies against all three viruses, with titers against EAV-GLΔ being generally higher. The control ponies showed a typical VNAb response after EAV infection against both wild-type viruses, with titers detectable by day 6 and increasing rapidly to reach high log values of around 3 by day 14. In contrast the titers against the EAV-GLΔ virus were very low.
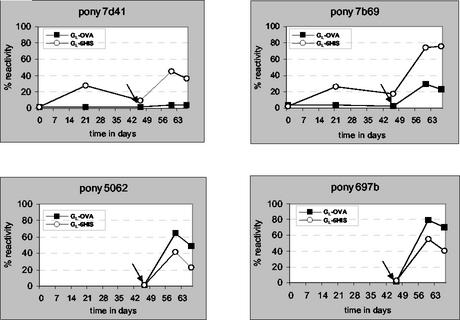
Evaluation of GL-specific antibody responses.
The availability of GL-based ELISAs that Nugent et al. established recently (49) allowed us to analyze the antibody responses directed against the entire GL ectodomain (residues 18 to 122) and against a part (residues 81 to 106) of the domain deleted in EAV-GLΔ (residues 66 to 112). The former test uses as an antigen a His-tagged bacterial expression product (GL-6His), while in the latter assay an ovalbumin-coupled synthetic peptide (GL-OVA) is applied to the ELISA plates. Selected serum samples from the four ponies were analyzed in parallel with a positive-control serum taken from a pony that had been immunized twice with the GL-6His protein (pony p6, 2 weeks after vaccination with the GL-6His antigen [14]). The results, expressed as the percentages of the ELISA reactivities with respect to the control, are compiled in Fig. 8. As expected, the vaccination of ponies 7b69 and 07d4 with EAV-GLΔ did not induce a detectable antibody response against the deleted GL domain. Reactivity against GL-OVA became measurable only after the challenge infection with wild-type EAV, particularly in the nonvaccinated animals. However, induction of anti-GL-OVA responses was higher for control ponies (60 to 80% reactivity by day 60) than for EAV-GLΔ-vaccinated ponies (<10 to 30% reactivity by day 60). In contrast, both vaccinated ponies developed an antibody response against GL-6His, which was subsequently boosted after challenge, becoming at least threefold higher than that those against GL-OVA. In the two control ponies, however, the challenge infection induced antibody responses against the two antigens that, in contrast to those for the preimmunized ponies, were at similar levels for both antigens.
FIG. 8.
GL protein-specific antibody responses of ponies 7b69, 07d41, 5062, and 697b after intranasopharyngeal immunization (ponies 7b69 and 07d41) with EAV-GLΔ (day 0) and intranasopharyngeal challenge infection with EAV LP3A+ (day 46; arrows) measured by ELISA for antigens GL-6His (GL residues 18 to 122) and GL-OVA (GL residues 81 to 106). Reactivities of sera are expressed with respect to that for a positive-control serum sample obtained from pony p6 2 weeks after vaccination with GL-6His antigen (14).
DISCUSSION
It has been generally assumed that protection against EAV infection is mediated via high levels of virus-neutralizing antibody. In this study we prepared, in the controlled background of a nonvirulent virus, a mutant EAV lacking the domain against which the vast majority of virus-neutralizing antibodies are directed. The virus, which replicated with slightly delayed kinetics compared to the parent in tissue culture, caused an asymptomatic infection in ponies, during which it induced an antibody response which in vitro neutralized the mutant virus efficiently but neutralized wild-type EAV strains only poorly. Nevertheless, the immunity induced via mutant virus infection protected the animals effectively against subsequent challenge infection with virulent EAV. Protection in the absence of significant neutralizing antibodies against the challenge virus suggests that an alternative immune effector mechanism was responsible. Because the mutant virus, as expected, did not induce an antibody response against a peptide antigen derived from the deleted region—on the basis of which a sensitive EAV ELISA was recently established—our work provides a potential candidate EAV marker vaccine.
Arteriviruses do not carry the conspicuous spike structures that other nidoviruses exhibit on their surfaces. Rather, electron-microscopic studies of EAV showed only tiny, ringlike projections on the otherwise smooth envelopes of viral particles (38, 41). Analyses of the protein structure of virions led to the concept that these projections are formed by the disulfide-linked ectodomains of the main envelope proteins GL and M (23). Actually, as the M protein ectodomain contributes only some 15 to 18 exposed residues, the surface structures are supposedly composed mainly of the GL protein, including the huge oligosaccharide side chain attached to it (21). Because EAV-neutralizing antibodies are directed against the GL ectodomain, it was speculated that the surface projections determine viral tropism, via involvement in receptor recognition. It was therefore quite surprising that the virus appeared to tolerate dramatic changes in its GL protein without any noticeable changes in its in vitro cell tropism. Thus, MAb escape mutants lacking up to 47 aa of the 97-residue ectodomain were obtained (8), while replacement of even the complete ectodomain by that of the GL protein of lactate dehydrogenase-elevating virus or porcine reproductive and respiratory syndrome virus generated viruses that, though significantly attenuated in their growth, maintained their ability to infect BHK-21 and RK-13 cells (24). In our studies we observed that the deletion mutant created was still able to infect BHK cells in vitro and equine cells in vivo, although the virus seemed to have replicated at a slower rate than wild-type EAV. Altogether these data indicate that the GL protein is therefore unlikely to be critical for receptor targeting although it may still serve some other function in viral entry.
An essential requirement for any live virus vaccine is that it be avirulent, inducing no or at most very mild disease manifestations. EAV-GLΔ was likely to fulfill this requirement because it was derived from a full-size infectious cDNA clone previously shown to produce nonvirulent virus (10). Intranasal inoculation of two stallions each with 2 × 106.25 TCID50 of this virus caused a transient infection without clinical symptoms apart from very mild pyrexia. However, the effect of deleting the immunodominant region of EAV could not a priori be predicted, since it might either have resulted in attenuation or have increased virulence, as a result of a reduced induction of neutralizing antibody responses.
The present study allowed us to evaluate the immunity against EAV infection provided by exposure to the deletion mutant virus. Both ponies inoculated with EAV-GLΔ mounted an immune response to EAV as evidenced by the detection of antibodies in serum against the whole GL ectodomain and by the demonstration of VNAb against wild-type EAV. We observed complete clinical protection against the virulent LP3A+ virus, accompanied by only occasional isolation of challenge virus from nasal swabs and blood in the vaccinated ponies. This level of protection was unexpected in the light of the relatively low log VNAb titers (1.2 and 0.8) against LP3A+ at the time of challenge. These VNAb were stimulated after EAV-GLΔ infection and boosted after challenge although the GL ectodomain was partially deleted from the immunizing virus. Consequently, these antibodies must either recognize epitopes in the modified GL polypeptide (antigenic sites A and B as identified by Balasuriya et al. [8] are still present in the deletion mutant virus) or be directed to yet-unidentified neutralizing epitopes lying outside the GL protein.
However, it seems unlikely that VNAb alone can have provided the levels of protection observed. Previous studies (14) showed that ponies vaccinated with a recombinant protein comprising the entire GL ectodomain and presenting log titers of around 1.0 at the time of challenge were only partially protected, although these ponies showed a significant anamnestic response after infection. More likely, the intranasal administration of a replicative immunogen stimulated a wide range of immune effector mechanisms, not dependent on the deleted region of the GL protein. Thus, strong VNAb responses directed against epitopes outside the GL (aa 66 to 112) region may have been elicited efficiently, particularly at the natural port of virus entry in the nasal mucosa. Alternatively, cell-mediated immunity may have contributed to the protection against challenge infection. Antibody-dependent cell-mediated cytotoxicity and cytotoxic T lymphocytes (CTL) in the horse have been described (1, 50). Recently, methods for the detection of EAV-specific cytotoxic responses have been developed and the induction of CD8+ CTL responses following wild-type EAV infection has been demonstrated (Castillo-Olivares et al., unpublished data). These and other methods should enable us to characterize the immune effector mechanisms that are stimulated after immunization with EAV-GLΔ and to evaluate the relative importance of antibody- versus cell-mediated mechanisms.
Both live-attenuated and killed-virus vaccines for EAV are presently commercially available. The live vaccine is a modified virus that has been attenuated for horses by multiple serial transfers in equine and rabbit cell cultures (42, 44, 59). It has been shown to be safe and protective for stallions and nonpregnant mares. Vaccination of foals under 6 weeks of age and of pregnant mares in the final 2 months of gestation is contraindicated. The killed-virus vaccine is an inactivated, adjuvanted product prepared from virus grown in equine cell culture that can be used in nonbreeding and breeding horses though its use in pregnant mares is not recommended (26, 42, 43). The efficacy of live vaccines is generally higher since they stimulate a wider range of immune effector responses and the immunity lasts longer than that produced by inactivated-virus vaccines. EAV-GLΔ is therefore a very attractive vaccine candidate for the future as it combines all the desired features of a live-attenuated virus with the additional ability to discriminate vaccinated from infected animals.
Marker vaccines are characterized by the absence of one or more proteins, or parts thereof, of the pathogen. Thus, antibodies against the deleted polypeptide(s) allow vaccinated animals to be differentiated from infected ones. These vaccines have become attractive or mandatory in programs aimed at controlling or eradicating virus infections in food as well as in companion animals (2-4, 65). Herpesvirus (glycoprotein gE-deleted pseudorabies virus and bovine herpesvirus) marker vaccines were among the first to be developed and used in the field (66), followed later by various genetically modified RNA viruses such as classical swine fever virus (64, 69) and Newcastle disease virus (47, 51). Marker vaccines can be based on live and inactivated viruses as well as on viral subunits, but they also include DNA and vector vaccines. The essential feature is the availability of a test that can identify infected animals irrespective of their vaccination status.
Despite the availability and efficacy of current live and inactivated EAV vaccines, their use suffers from the drawback of not permitting discrimination of vaccinated from naturally infected animals. Consequently their use is restricted in order to avoid confounding disease surveillance and prevention programs. Equine viral arteritis is a contagious disease that can be silently introduced by asymptomatic carrier stallions and easily spread in naive equine populations, as has been documented (72). Spread of the virus is additionally facilitated by specific features of the horse industry, which is characterized by active international trade and traffic. Moreover, horses are frequently used in various branches of equestrian sport, which necessitates close contacts between animals, often from all points of the compass, thereby increasing the risk of exposure. All these conditions call for a marker vaccine. This need is also realized by the legislative authorities, for which the discrimination between vaccination and infection is becoming a ruling issue. In view of its performance and of the availability of a sensitive discriminating ELISA, EAV-GLΔ has the potential to be a live-attenuated marker vaccine.
Immunization of ponies with EAV-GLΔ went without noticeable clinical symptoms. Subsequent inoculation with virulent EAV showed that the vaccination prevented disease while strongly reducing infection by the challenge virus: infectivity was briefly observed in nasal secretions and blood at low but detectable levels. Promising as these observations are, several features of the candidate vaccine yet need to be established. It will, for instance, be important to determine the duration of the immunity provided. Moreover, it will be of interest to know whether the vaccine virus can cause a persistent infection in stallions. Furthermore, it will be important to evaluate the performance of the virus in pregnant mares in order to find out whether it is sufficiently attenuated to not be abortigenic. The results of these and other studies will set the conditions under which the vaccine may eventually be deployed.
Acknowledgments
Roeland Wieringa and Javier Castillo-Olivares contributed equally to this work.
We are very grateful to Martin Raamsman for technical assistance for the preparation of the antiserum directed against the carboxy terminus of the EAV GL protein. We thank Eric Snijder for making available the full-length EAV cDNA clone pEAN515.
Part of this work was supported by the BBSRC (United Kingdom). Nick J. Davis-Poynter was supported by a Tetra Laval Senior Fellowship.
REFERENCES
- 1.Allen, G., M. Yeargan, L. R. Costa, and R. Cross. 1995. Major histocompatibility complex class I-restricted cytotoxic T-lymphocyte responses in horses infected with equine herpesvirus 1. J. Virol. 69:606-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babiuk, L., J. Lewis, S. Suradhat, M. Baca-Estrada, M. Foldvari, and S. Babiuk. 1999. Polynucleotide vaccines: potential for inducing immunity in animals. J. Biotechnol. 73:131-140. [DOI] [PubMed] [Google Scholar]
- 3.Babiuk, L. A. 1999. Broadening the approaches to developing more effective vaccines. Vaccine 17:1587-1595. [DOI] [PubMed] [Google Scholar]
- 4.Babiuk, L. A., S. L. Babiuk, and M. E. Baca-Estrada. 2002. Novel vaccine strategies. Adv. Virus Res. 58:29-80. [DOI] [PubMed] [Google Scholar]
- 5.Balasuriya, U. B., H. W. Heidner, N. L. Davis, H. M. Wagner, P. J. Hullinger, J. F. Hedges, J. C. Williams, R. E. Johnston, W. W. David, I. K. Liu, and M. L. James. 2002. Alphavirus replicon particles expressing the two major envelope proteins of equine arteritis virus induce high level protection against challenge with virulent virus in vaccinated horses. Vaccine 20:1609-1617. [DOI] [PubMed] [Google Scholar]
- 6.Balasuriya, U. B., H. W. Heidner, J. F. Hedges, J. C. Williams, N. L. Davis, R. E. Johnston, and N. J. MacLachlan. 2000. Expression of the two major envelope proteins of equine arteritis virus as a heterodimer is necessary for induction of neutralizing antibodies in mice immunized with recombinant Venezuelan equine encephalitis virus replicon particles. J. Virol. 74:10623-10630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balasuriya, U. B., N. J. MacLachlan, A. A. F. de Vries, P. V. Rossitto, and P. J. M. Rottier. 1995. Identification of a neutralization site in the major envelope glycoprotein (GL) of equine arteritis virus. Virology 207:518-527. [DOI] [PubMed] [Google Scholar]
- 8.Balasuriya, U. B., J. F. Patton, P. V. Rossitto, P. J. Timoney, W. H. McCollum, and N. J. MacLachlan. 1997. Neutralization determinants of laboratory strains and field isolates of equine arteritis virus: identification of four neutralization sites in the amino-terminal ectodomain of the GL envelope glycoprotein. Virology 232:114-128. [DOI] [PubMed] [Google Scholar]
- 9.Balasuriya, U. B., P. V. Rossitto, C. D. DeMaula, and N. J. MacLachlan. 1993. A 29K envelope glycoprotein of equine arteritis virus expresses neutralization determinants recognized by murine monoclonal antibodies. J. Gen. Virol. 74:2525-2529. [DOI] [PubMed] [Google Scholar]
- 10.Balasuriya, U. B., E. J. Snijder, L. C. van Dinten, H. W. Heidner, W. D. Wilson, J. F. Hedges, P. J. Hullinger, and N. J. MacLachlan. 1999. Equine arteritis virus derived from an infectious cDNA clone is attenuated and genetically stable in infected stallions. Virology 260:201-208. [DOI] [PubMed] [Google Scholar]
- 11.Balasuriya, U. B., P. J. Timoney, W. H. McCollum, and N. J. MacLachlan. 1995. Phylogenetic analysis of open reading frame 5 of field isolates of equine arteritis virus and identification of conserved and nonconserved regions in the GL envelope glycoprotein. Virology 214:690-697. [DOI] [PubMed] [Google Scholar]
- 12.Bryans, J. T., E. R. Doll, M. E. W. Crowe, and W. H. McCollum. 1957. The blood picture and thermal reaction in experimental viral arteritis of horses. Cornell Vet. 47:42-52. [PubMed] [Google Scholar]
- 13.Bryans, J. T., E. R. Doll, J. C. Wilson, and W. H. McCollum. 1966. Immunization for equine influenza. J. Am. Vet. Med. Assoc. 148:413-417. [PubMed] [Google Scholar]
- 14.Castillo-Olivares, J., A. A. F. de Vries, M. J. B. Raamsman, P. J. M. Rottier, K. Lakhani, D. Westcott, J. P. Tearle, J. L. N. Wood, J. A. Mumford, D. Hannant, and N. J. Davis-Poynter. 2001. Evaluation of a prototype sub-unit vaccine against equine arteritis virus comprising the entire ectodomain of the virus large envelope glycoprotein (GL): induction of virus-neutralizing antibody and assessment of protection in ponies. J. Gen. Virol. 82:2425-2435. [DOI] [PubMed] [Google Scholar]
- 15.Chirnside, E. D., A. A. F. de Vries, J. A. Mumford, and P. J. M. Rottier. 1995. Equine arteritis virus-neutralizing antibody in the horse is induced by a determinant on the large envelope glycoprotein GL. J. Gen. Virol. 76:1989-1998. [DOI] [PubMed] [Google Scholar]
- 16.Collins, J. K., S. Kari, S. L. Ralston, D. G. Bennet, J. L. Traub Dargatz, and A. O. McKinnon. 1987. Equine viral arteritis in a veterinary teaching hospital. Prev. Vet. Med. 4:389-397. [Google Scholar]
- 17.Dea, S., C. A. Gagnon, H. Mardassi, B. Pirzadeh, and D. Rogan. 2000. Current knowledge on the structural proteins of porcine reproductive and respiratory syndrome (PRRS) virus: comparison of the North American and European isolates. Arch. Virol. 145:659-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deregt, D., A. A. F. de Vries, M. J. B. Raamsman, L. D. Elmgren, and P. J. M. Rottier. 1994. Monoclonal antibodies to equine arteritis virus proteins identify the GL protein as a target for virus neutralization. J. Gen. Virol. 75:2439-2444. [DOI] [PubMed] [Google Scholar]
- 19.de Vries, A. A. F. 1994. The molecular biology of equine arteritis virus. Ph.D. thesis. Utrecht University, Utrecht, The Netherlands.
- 20.de Vries, A. A. F., E. D. Chirnside, P. J. Bredenbeek, L. A. Gravestein, M. C. Horzinek, and W. J. M. Spaan. 1990. All subgenomic mRNAs of equine arteritis virus contain a common leader sequence. Nucleic Acids Res. 18:3241-3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Vries, A. A. F., E. D. Chirnside, M. C. Horzinek, and P. J. M. Rottier. 1992. Structural proteins of equine arteritis virus. J. Virol. 66:6294-6303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Vries, A. A. F., A. L. Glaser, M. J. B. Raamsman, C. A. M. de Haan, S. Sarnataro, G. J. Godeke, and P. J. M. Rottier. 2000. Genetic manipulation of equine arteritis virus using full-length cDNA clones: separation of overlapping genes and expression of a foreign epitope. Virology 270:84-97. [DOI] [PubMed] [Google Scholar]
- 23.de Vries, A. A. F., S. M. Post, M. J. B. Raamsman, M. C. Horzinek, and P. J. M. Rottier. 1995. The two major envelope proteins of equine arteritis virus associate into disulfide-linked heterodimers. J. Virol. 69:4668-4674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dobbe, J. C., Y. van der Meer, W. J. M. Spaan, and E. J. Snijder. 2001. Construction of chimeric arteriviruses reveals that the ectodomain of the major glycoprotein is not the main determinant of equine arteritis virus tropism in cell culture. Virology 288:283-294. [DOI] [PubMed] [Google Scholar]
- 25.Doll, E. R., J. T. Bryans, W. H. McCollum, and M. E. W. Crowe. 1957. Isolation of a filterable agent causing arteritis of horses and abortion by mares. Its differentiation from the equine abortion (influenza) virus. Cornell Vet. 47:3-41. [PubMed] [Google Scholar]
- 26.Doll, E. R., J. T. Bryans, J. C. Wilson, and W. H. McCollum. 1968. Immunization against equine viral arteritis using modified live virus propagated in cell cultures of rabbit kidney. Cornell Vet. 48:497-524. [PubMed] [Google Scholar]
- 27.Doll, E. R., R. E. Knappenberg, and J. T. Bryans. 1957. An outbreak of abortion caused by the equine arteritis virus. Cornell Vet. 47:69-75. [PubMed] [Google Scholar]
- 28.Edwards, S., J. Castillo-Olivares, A. Cullinane, J. Lable, J. Lenihan, J. A. Mumford, D. J. Paton, J. E. Pearson, R. Sinclair, D. G. F. Westcott, J. L. N. Wood, S. Zientara, and M. Nelly. 1998. International harmonization of laboratory diagnostic tests for equine viral arteritis, p. 359-362. In U. Wernery, J. F. Wade, J. A. Mumford, and O.-R. Kaaden (ed.), Proceedings of the 8th International Conference on Equine Infectious Diseases. R&W Publications, Newmarket, United Kingdom.
- 29.Estes, P. C., and N. F. Cheville. 1970. The ultrastructure of vascular lesions in equine viral arteritis. Am. J. Pathol. 58:235-253. [PMC free article] [PubMed] [Google Scholar]
- 30.Fukunaga, Y., H. Imagawa, E. Tabuchi, and Y. Akiyama. 1981. Clinical and virological findings on experimental equine viral arteritis in horses. Bull. Equine Res. Inst. 18:110-118. [Google Scholar]
- 31.Fukunaga, Y., T. Matsumura, T. Sugiura, R. Wada, H. Imagawa, T. Kanemaru, and M. Kamada. 1994. Use of the serum neutralisation test for equine viral arteritis with different virus strains. Vet. Rec. 134:574-576. [DOI] [PubMed] [Google Scholar]
- 32.Fukunaga, Y., R. Wada, H. Imagawa, and T. Kanemaru. 1997. Venereal infection of mares by equine arteritis virus and use of killed vaccine against the infection. J. Comp. Pathol. 117:201-208. [DOI] [PubMed] [Google Scholar]
- 33.Fukunaga, Y., R. Wada, T. Kanemaru, H. Imagawa, M. Kamada, and T. Samejima. 1996. Immune potency of lyophilized, killed vaccine for equine viral arteritis and its protection against abortion in pregnant mares. J. Equine Vet. Sci. 16:217-221. [Google Scholar]
- 34.Fukunaga, Y., R. Wada, T. Matsumura, T. Sugiura, and H. Imagawa. 1990. Induction of immune response and protection from equine viral arteritis (EVA) by formalin inactivated-virus vaccine for EVA in horses. Zentralbl. Vetmed. Reihe B 37:135-141. [DOI] [PubMed] [Google Scholar]
- 35.Glaser, A. L., A. A. F. de Vries, and E. J. Dubovi. 1995. Comparison of equine arteritis virus isolates using neutralizing monoclonal antibodies and identification of sequence changes in GL associated with neutralization resistance. J. Gen. Virol. 76:2223-2233. [DOI] [PubMed] [Google Scholar]
- 36.Glaser, A. L., A. A. F. de Vries, P. J. M. Rottier, M. C. Horzinek, and B. Colenbrander. 1996. Equine arteritis virus: a review of clinical features and management aspects. Vet. Q. 18:95-99. [DOI] [PubMed] [Google Scholar]
- 37.Hardy, E., H. Santana, A. Sosa, L. Hernandez, C. Fernandez-Patron, and L. Castellanos-Serra. 1996. Recovery of biologically active proteins detected with imidazole-sodium dodecyl sulfate-zinc (reverse stain) on sodium dodecyl sulfate gels. Anal. Biochem. 240:150-152. [DOI] [PubMed] [Google Scholar]
- 38.Hyllseth, B. 1973. Structural proteins of equine arteritis virus. Arch. Gesamte Virusforsch. 40:177-188. [DOI] [PubMed] [Google Scholar]
- 39.Kyte, J., and R. F. Doolittle. 1982. A simple method for displaying the hydropathic character of a protein. J. Mol. Biol. 157:105-132. [DOI] [PubMed] [Google Scholar]
- 40.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 41.Magnusson, P., B. Hyllseth, and H. Marusyk. 1970. Morphological studies on equine arteritis virus. Arch. Gesamte Virusforsch. 30:105-112. [DOI] [PubMed] [Google Scholar]
- 42.McCollum, W. H. 1969. Development of a modified virus strain and vaccine for equine viral arteritis. J. Am. Vet. Med. Assoc. 155:318-322. [PubMed] [Google Scholar]
- 43.McCollum, W. H. 1970. Vaccination for equine arteritis virus, p. 143-151. In J. T. Bryans and H. Gerber (ed.), Proceeding of the 2nd International Conference on Equine Infectious Diseases. S. Karger, Basel, Switzerland.
- 44.McCollum, W. H. 1986. Responses of horses vaccinated with avirulent modified-live equine arteritis virus propagated in the E. Derm (NBL-6) cell line to nasal inoculation with virulent virus. Am. J. Vet. Res. 47:1931-1934. [PubMed] [Google Scholar]
- 45.McCollum, W. H. 2002. Studies of passive immunity in foals to equine viral arteritis. Vet. Microbiol. 1:45-54. [Google Scholar]
- 46.McCollum, W. H., and J. T. Bryans. 1973. Serological identification of infection by equine arteritis virus in horses of several countries, p. 256-263. In J. T. Bryans and H. Gerber (ed.), Proceedings of the 3rd International Conference on Equine Infectious Diseases. S. Karger, Basel, Switzerland.
- 47.Mebatsion, T., M. J. Koolen, L. T. de Vaan, N. de Haas, M. Braber, A. Romer-Oberdorfer, P. van den Elzen, and P. van der Marel. 2002. Newcastle disease virus (NDV) marker vaccine: an immunodominant epitope on the nucleoprotein gene of NDV can be deleted or replaced by a foreign epitope. J. Virol. 76:10138-10146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neu, S. M., P. J. Timoney, and S. R. Lowry. 1992. Changes in semen quality following experimental equine arteritis virus infection in the stallion. Theriogenology 37:407-431. [Google Scholar]
- 49.Nugent, J., R. Sinclair, A. A. F. de Vries, R. Y. Eberhardt, J. Castillo-Olivares, N. J. Davis-Poynter, P. J. M. Rottier, and J. A. Mumford. 2000. Development and evaluation of ELISA procedures to detect antibodies against the major envelope protein (G(L)) of equine arteritis virus. J. Virol. Methods 90:167-183. [DOI] [PubMed] [Google Scholar]
- 50.O'Neill, T., J. H. Kydd, G. P. Allen, E. Wattrang, J. A. Mumford, and D. Hannant. 1999. Determination of equid herpesvirus 1-specific, CD8+, cytotoxic T lymphocyte precursor frequencies in ponies. Vet. Immunol. Immunopathol. 70:43-54. [DOI] [PubMed] [Google Scholar]
- 51.Peeters, B. P., O. S. de Leeuw, I. Verstegen, G. Koch, and A. L. Gielkens. 2001. Generation of a recombinant chimeric Newcastle disease virus vaccine that allows serological differentiation between vaccinated and infected animals. Vaccine 19:1616-1627. [DOI] [PubMed] [Google Scholar]
- 52.Plagemann, P. G. W., and V. Moennig. 1992. Lactate dehydrogenase-elevating virus, equine arteritis virus, and simian hemorrhagic fever virus: a new group of positive-strand RNA viruses. Adv. Virus Res. 41:99-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 54.Snijder, E. J., and J. J. M. Meulenberg. 1998. The molecular biology of arteriviruses. J. Gen. Virol. 79:961-979. [DOI] [PubMed] [Google Scholar]
- 55.Snijder, E. J., H. van Tol, K. W. Pedersen, M. J. B. Raamsman, and A. A. F. de Vries. 1999. Identification of a novel structural protein of arteriviruses. J. Virol. 73:6335-6345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stadejek, T., H. Bjorklund, C. R. Bascunana, I. M. Ciabatti, M. T. Scicluna, D. Amaddeo, W. H. McCollum, G. L. Autorino, P. J. Timoney, D. J. Paton, B. Klingeborn, and S. Belak. 1999. Genetic diversity of equine arteritis virus. J. Gen. Virol. 80:691-699. [DOI] [PubMed] [Google Scholar]
- 57.St. Laurent, G., N. Lepage, S. Carman, and D. Archambault. 1997. Genetic and amino acid analysis of the GL protein of Canadian, American and European equine arteritis virus isolates. Can. J. Vet. Res. 61:72-76. [PMC free article] [PubMed] [Google Scholar]
- 58.Timoney, P. J., and W. H. McCollum. 1987. Equine viral arteritis. Can. Vet. J. 28:693-695. [PMC free article] [PubMed] [Google Scholar]
- 59.Timoney, P. J., and W. H. McCollum. 1988. Equine viral arteritis: epidemiology and control. J. Equine Vet. Sci. 8:54-59. [Google Scholar]
- 60.Timoney, P. J., and W. H. McCollum. 1993. Equine viral arteritis. Vet. Clin. N. Am. Equine Pract. 9:295-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vaala, W. E., A. N. Hamir, E. J. Dubovi, P. J. Timoney, and B. Ruiz. 1992. Fatal, congenitally acquired infection with equine arteritis virus in a neonatal Thoroughbred. Equine Vet. J. 24:155-158. [DOI] [PubMed] [Google Scholar]
- 62.van Berlo, M. F., J. J. W. Zeegers, M. C. Horzinek, and B. A. M. van der Zeijst. 1983. Antigenic comparison of equine arteritis virus (EAV) and lactic dehydrogenase virus (LDV); binding of staphylococcal protein A to the nucleocapsid protein of EAV. Zentralbl. Vetmed. Reihe B 30:297-304. [DOI] [PubMed] [Google Scholar]
- 63.van Dinten, L. C., J. A. den Boon, A. L. M. Wassenaar, W. J. M. Spaan, and E. J. Snijder. 1997. An infectious arterivirus cDNA clone: identification of a replicase point mutation that abolishes discontinuous mRNA transcription. Proc. Natl. Acad. Sci. USA 94:991-996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.van Gennip, H. G., A. Bouma, P. A. van Rijn, M. N. Widjojoatmodjo, and R. J. Moormann. 2002. Experimental non-transmissible marker vaccines for classical swine fever (CSF) by trans-complementation of E(rns) or E2 of CSFV. Vaccine 20:1544-1556. [DOI] [PubMed] [Google Scholar]
- 65.van Oirschot, J. T. 2001. Present and future of veterinary viral vaccinology: a review. Vet. Q. 23:100-108. [DOI] [PubMed] [Google Scholar]
- 66.van Oirschot, J. T., M. J. Kaashoek, F. A. Rijsewijk, and J. A. Stegeman. 1996. The use of marker vaccines in eradication of herpesviruses. J. Biotechnol. 44:75-81. [DOI] [PubMed] [Google Scholar]
- 67.Weiland, E., S. Bolz, F. Weiland, W. Herbst, M. J. B. Raamsman, P. J. M. Rottier, and A. A. F. de Vries. 2000. Monoclonal antibodies directed against conserved epitopes on the nucleocapsid protein and the major envelope glycoprotein of equine arteritis virus. J. Clin. Microbiol. 38:2065-2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Westcott, D., M. H. Lucas, and D. J. Paton. 1995. Equine arteritis virus: antigenic analysis of strain variation, p. 479-483. In M. Schwyzer, M. Ackermann, G. Bertoni, R. Kocherhaus, K. McCullough, M. Engels, R. Wittek, and R. Zanoni (ed.), Immunobiology of viral infections. Proceedings of the 3rd Congress of the European Society for Veterinary Virology. Fondation Marcel Merieux, Lyon, France.
- 69.Widjojoatmodjo, M. N., H. G. van Gennip, A. Bouma, P. A. van Rijn, and R. J. Moormann. 2000. Classical swine fever virus E(rns) deletion mutants: trans-complementation and potential use as nontransmissible, modified, live-attenuated marker vaccines. J. Virol. 74:2973-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wieringa, R., A. A. F. de Vries, and P. J. M. Rottier. 2003. Formation of disulfide-linked complexes between the three minor envelope glycoproteins (GP2b, GP3, and GP4) of equine arteritis virus. J. Virol. 77:6216-6226. [DOI] [PMC free article] [PubMed]
- 71.Wieringa, R., A. A. F. de Vries, M. J. B. Raamsman, and P. J. M. Rottier. 2002. Characterization of two new structural glycoproteins, GP3 and GP4, of equine arteritis virus. J. Virol. 76:10829-10840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wood, J. L., E. D. Chirnside, J. A. Mumford, and A. J. Higgins. 1995. First recorded outbreak of equine viral arteritis in the United Kingdom. Vet. Rec. 136:381-385. [DOI] [PubMed] [Google Scholar]
- 73.Yamaguchi, S., T. Kanno, H. Akashi, and T. Kondo. 1997. Identification of two neutralization sites in GL protein of equine arteritis virus by means of monoclonal antibodies. J. Equine Sci. 8:7-11. [Google Scholar]
- 74.Zeegers, J. J. W., B. A. M. van der Zeijst, and M. C. Horzinek. 1976. The structural proteins of equine arteritis virus. Virology 73:200-205. [DOI] [PubMed] [Google Scholar]