Abstract
To develop a high-titer surrogate virus for human T-cell leukemia virus type 1 (HTLV-1), we generated recombinant vesicular stomatitis viruses (VSVs) in which the gene encoding the single transmembrane glycoprotein (G) was deleted. Genes encoding HTLV-1 envelope glycoproteins (HTEnv) or HTEnvG hybrid proteins were then inserted into either of two different sites in the VSV genome. The viruses also encoded a green fluorescent protein. With this surrogate virus, we found that a soluble protein, osteoprotegerin (OPG), or an OPG/Fc chimeric protein inhibited the infection of various cell lines. Our experiments indicate that this inhibition resulted from binding of heparan sulfate by OPG.
Human T-cell leukemia virus type 1 (HTLV-1) is a human retrovirus that causes adult T-cell leukemia (ATL) (16). ATL is a highly aggressive malignancy of CD4+ T lymphocytes and is frequently accompanied by hypercalcemia (20). High levels of Ca2+ are frequently observed in the serum of patients with ATL during the clinical course of the disease, and these levels are higher than in those with other hematological malignancies. It was recently reported that the hypercalcemia in ATL is caused by the receptor activator of nuclear factor κB (RANK)-RANK ligand (RANKL) interaction, which can be inhibited by osteoprotegerin (OPG), a decoy receptor for RANKL (28).
The HTLV-1 envelope glycoproteins mediate the viral entry process and also induce the formation of giant multinucleated cells called syncytia (32, 33). The envelope glycoproteins are composed of a 46-kDa surface glycoprotein (gp46, SU) and a 21-kDa transmembrane glycoprotein (gp21, TM) (32, 37), which are responsible for specific binding to an unidentified receptor and catalyze membrane fusion, respectively (9). Cell-cell HTLV-1 transmission appears to be more efficient than cell-free transmission, because cell-free HTLV-1 particles are poorly infectious (11). The mechanism of HTLV-1 infection remains poorly understood because of the poor infectivity of the cell-free virus. The lack of assay systems with high-titer infectious HTLV-1 has greatly limited studies on viral infection and the development of an HTLV-1 vaccine.
Recombinant vesicular stomatitis viruses (rVSVs) can be recovered from DNA copies, and foreign genes can be expressed at high levels from multiple sites in the genome (14, 24). Our laboratory has shown that rVSVs can be used to express foreign viral envelope glycoproteins at high levels and that these are normally incorporated into viral particles (22, 36). rVSVs lacking the VSV G protein and expressing foreign envelope proteins, such as human immunodeficiency virus type 1 (HIV-1) envelope proteins, can show new targeting specificity that is dependent on the proteins expressed on the surface of viral particles (4). Here we used the same approach to develop a VSV-based surrogate virus for HTLV-1.
HTLV-1 primarily infects and immortalizes human CD4+ T cells (34), but in vitro, it infects many cell types derived from various species (11, 30). This indicates that a primary receptor for HTLV-1 is a molecule ubiquitously expressed. Although cell fusion assays, including syncytium formation assays and viral pseudotype assays, have identified multiple cell surface components, including proteins such as adhesion molecules and lipids (7, 15, 29, 40), that are involved in HTLV-1 envelope-mediated cell-cell fusion and cell-free transmission, the primary HTLV-1 receptor remains to be elucidated.
To facilitate investigation of HTLV-1 infection, we developed novel surrogate HTLV-1 (sHTLV-1) strains by using rVSV. Furthermore, we have shown here that a soluble secreted protein, OPG, inhibited sHTLV-1 infection of cells via binding to heparan sulfate (HS), a new mechanism for inhibition of HTLV-1 infection.
Construction of rVSVs expressing the HTLV-1 envelope glycoprotein or a hybrid protein with the cytoplasmic tail from the VSV G protein.
To examine the mechanism of HTLV-1 infection of host cells and identify molecules involved in the infection, we developed rVSVs expressing HTLV-1 envelope glycoproteins. We constructed four recombinant viruses by inserting either of two different HTLV-1 envelope gene constructs into either of two different sites of the VSV genome within a plasmid DNA from which infectious VSV can be recovered (24) as follows.
The HTLV-1 envelope (HTEnv) gene was amplified from HTLV-I K30 DNA (47) by PCR with Vent polymerase (New England Biolabs). The forward primer was 5′-GCGGCCGCGGACGCGTCACCATGGGTAAGTTTCTCGCCACTTTG-3′. This primer contained an MluI site (bold) for further cloning. The reverse primer was 5′-GATCGATCGACTGACGCTAGCTTACAGGGATGACTCAGGGTTTATAAG-3′. This primer contained an NheI site (bold) for further cloning. This product was excised with MluI and NheI and ligated into the MluI and NheI sites of a modified pBluescript vector and of pVSVΔG/GFP in which the VSV G gene had been replaced with the green fluorescent protein (GFP) gene. The final plasmids were called pBSSK-HTLV-I env and pVSVHTEnv4, respectively.
The HTEnvG gene, encoding the HTLV-1 envelope glycoprotein with the cytoplasmic domain of VSV G replacing its native cytoplasmic domain, was amplified by a two-step PCR procedure. First, a hybrid gene segment encoding part of the transmembrane region of gp21 and the cytoplasmic domain of VSV G was amplified from a clone containing the VSV G gene. The forward primer was 5′-CCTTGCAGGACCATGCATCCTCCGAGTTGGTATCCATCTTTGCATTAAATTAAAG-3′. This primer contained the sequences encoding the transmembrane region of gp21 (bold) and the cytoplasmic domain of VSV G (underlined). The reverse primer was 5′-CGTACGTACGTGCTAGCGAGTTACTTTCCAAGTCGGTTCATC-3′. This primer contained an NheI site (bold) for further cloning and a sequence complementary to the G cytoplasmic domain coding sequence. Next, this PCR product was used to amplify the complete HTEnvG gene from HTLV-I K30 DNA along with the forward primer (5′-GCGGCCGCGGACGCGTCACCATGGGTAAGTTTCTCGCCACTTTG-3′) and the reverse primer described above. This product was excised with MluI and NheI and ligated into pBluescript and pVSVΔG/GFP after digestion with MluI and NheI. The resulting plasmids were designated pBS-HTEnvG and pVSVHTEnvG4, respectively.
To generate a vector for expression of foreign genes between the N and P genes (position 2) of the VSV genome, a double-stranded DNA linker was constructed from the oligonucleotides 5′-TATGAAAAAAACT AACAGATATCACGCTCGAGAGCGATCCCGGGATCGGTGCTAGCCT-3′ and 5′-TAAGGCTAGCACCGATCCCGGGATCGCTCTCGAGCGTGATATCTGTTAGTTTTTTTCA-3′. These oligonucleotides contained the minimally conserved VSV transcription stop and start sequences (underlined), as well as XhoI, SmaI, and NheI sites (bold) for use in further cloning. The oligonucleotides were annealed and then ligated into pBS-NP, which had been digested with NdeI. The fragment containing the linker was excised with BstZ17I and XbaI and cloned into pVSV, which had been digested with BstZ17I and XbaI. The resulting plasmid was called pVSV XSN.
The HTEnv gene was amplified from pBSSK-HTLV-I env by PCR. The forward primer was 5′-TCCCCCCGGGAACATGGGTAAGTTTCTCGCCACTTTG-3′. This primer contained an XmaI site (bold) for further cloning. The reverse primer was 5′-ACCCTCACTAAAGGGAACAA-3′. The PCR product was digested with XmaI and NheI and ligated into pVSV XSN, which had been digested with XmaI and NheI. Next, the fragment containing the HTEnv gene was excised with BstZ17I and XbaI and cloned into pVSVΔG/GFP, which had been digested with BstZ17I and XbaI. The final plasmid was called pVSVHTEnv2.
The HTEnvG gene was amplified from pBS-HTEnvG by PCR. The forward primer was the same as that used to amplify the HTEnv gene in pVSVHTEnv2. The reverse primer was 5′-CGGGCCCATCTAGAGCTAGCTTACTTTCCAAGTCGGTTCATCTC-3′. This primer contained an NheI site (bold) for further cloning. The product was digested with XmaI and NheI and ligated into pVSV XSN, which had been digested with XmaI and NheI. Next, the plasmid was digested with BstZ17I and XbaI, and the fragment containing the HTEnvG gene was cloned into pVSVΔG/GFP, which had been digested with BstZ17I and XbaI. The resulting plasmid was designated pVSVHTEnvG2.
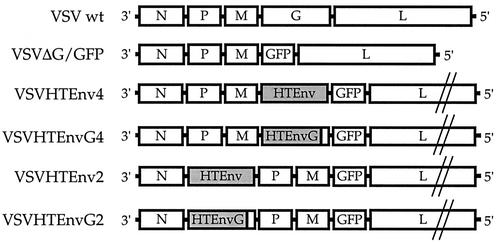
Figure 1 summarizes the diagrams of the gene order for the rVSV/HTLV-1 constructs, with numbers indicating the positions of the HTLV-1 envelope gene within the VSV genome. The gene encoding the HTLV-1 envelope protein precursor (HTEnv) or an Env protein with the VSV G cytoplasmic domain (HTEnvG) was cloned into expression sites at position 4 or 2 as indicated in Fig. 1. All constructs had the gene for GFP in position 5. The HTEnvG hybrid, in which the VSV G cytoplasmic domain replaces the HTLV-1 gp21 cytoplasmic domain, was generated in an attempt to increase incorporation of HTEnv proteins into VSV particles (19, 31). Because VSV transcription occurs sequentially and is attenuated, we anticipated higher envelope expression from position 2.
FIG. 1.
Constructs of rVSVs expressing HTLV-1 envelope glycoproteins. The gene order in four rVSV constructs encoding HTLV-1 envelope glycoproteins (HTEnv or HTEnvG hybrid) is illustrated. The numbers (e.g., Env2 and Env4) indicate the positions of the Env and EnvG genes relative to the 3′ end of the genome. The VSV wild-type (wt) and VSVΔG/GFP constructs are diagrammed also. The constructs were used for recovery of rVSV/HTLV-1.
rVSV/HTLV-1 constructs (VSVHTEnv and VSVHTEnvG) were recovered from pVSVHTEnv and pVSVHTEnvG by established methods (24). These stocks were then harvested and the supernatant was stored at −80°C.
For the preparation of ΔG viral stocks not complemented with VSV G, G-complemented stocks were inoculated into ∼107 BHK-21 cells. After adsorption at 37°C for 1 h, the cells were washed intensively with fetal bovine serum (FBS)-free Dulbecco’s modified Eagle’s medium (DMEM) to remove the G-complemented input viruses. The cells were then incubated in fresh 10% FBS-DMEM at 37°C overnight. The media containing the ΔG viruses (rVSV/HTLV-1 constructs) were stored at −80°C until use.
Expression of HTLV-1 envelope glycoproteins in infected cells.
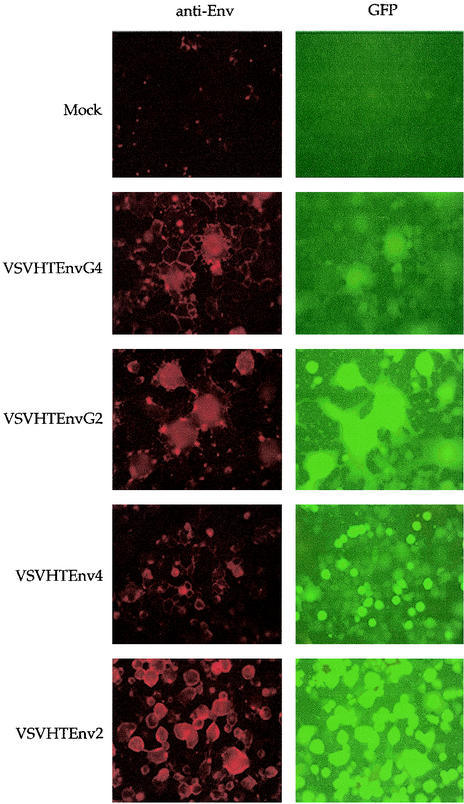
To evaluate whether the rVSVs expressed the correct HTLV-1 envelope glycoproteins in infected cells, we initially examined protein expression on the cell surface by immunofluorescence microscopy and simultaneously examined GFP expression. Figure 2 shows cell surface expression of HTLV-1 envelope glycoproteins and GFP expressed in BHK cells infected with the rVSVs. The viruses with HTEnv or HTEnvG in position 2 appeared to express more protein on the cell surface than those with HTEnv or HTEnvG in position 4. Given the sequential attenuation of VSV transcription, this result was expected. We also noted that the HTEnvG viruses generated larger syncytia than the HTEnv constructs, especially when expression from the same position was compared, suggesting greater membrane fusion activity of the EnvG protein. This greater membrane fusion could be caused by structural changes that also might make the protein less stable or less capable of mediating virus entry after incorporation into virus particles.
FIG. 2.
Expression of HTLV-1 envelope glycoproteins on the cell surface and internal expression of GFP. BHK cells were plated to approximately 60% confluency on coverslips and infected at a multiplicity of infection of 1 with G-complemented rVSV/HTLV-1 constructs. After overnight incubation at 37°C, the cells on coverslips were fixed in 3% paraformaldehyde. Coverslips were then washed in phosphate-buffered saline containing 10 mM glycine, and the cells were incubated in 5% normal donkey serum at 37°C for 10 min. The cells were next incubated in a 1:100 dilution of anti-HTLV-1 serum (NIH AIDS Research and Reference Reagent Program) at 37°C for 10 min and then with a 1:50 dilution of a rhodamine-conjugated donkey anti-goat antibody (Jackson Research) at 37°C for 10 min. The coverslips were then mounted on glass slides, and the expression of HTLV-1 envelope glycoproteins and GFP was observed in the same field of infected BHK cells and photographed with a Nikon Microphot-FX microscope with a 25× objective.
To examine the sizes of the proteins encoded by the rVSVs, we infected BHK cells with each virus, labeled with [35S]methionine and [35S]cysteine, and immunoprecipitated cell lysates with anti-gp46 antibody. Cells infected with rVSV/HTLV-1 constructs expressed a protein of the mobility expected for the HTLV-1 envelope precursor protein (∼61 kDa), while VSV-GFP (4)-infected cells showed no band at this position (data not shown).
Titration of rVSVs expressing HTLV-1 envelope glycoproteins.
We determined the titers of G-complemented and noncomplemented viruses with HTEnv or HTEnvG in position 2 or 4 on BHK and 293T cells (Table 1). Cells were plated to approximately 80% confluency. G-complemented and noncomplemented stocks of VSVHTEnv and VSVHTEnvG were diluted serially in FBS-free DMEM and used to infect these cells. Only the noncomplemented viruses included the I1 and I14 monoclonal antibodies (MAbs) (4) at a 1:200 dilution each to inhibit infection due to traces of VSV G protein. After 1 h of adsorption, the inocula were replaced with medium containing 1% methylcellulose. At about 15 h postinoculation, the number of GFP-expressing cells was determined by fluorescence microscopy and viral titers were calculated. G-complemented viruses showed high titers of 1 × 107 to 2 × 108 infectious units (IU)/ml. The titers of noncomplemented viruses were reduced by more than 3 logs. 293T cells were much more susceptible than BHK cells, and VSVHTEnv2 showed the highest titers (more than 106 IU/ml). The viruses with HTEnv or HTEnvG in position 2 showed higher titers than those with HTEnv or HTEnvG in position 4, respectively, suggesting that the expression level of HTLV-1 envelope proteins from position 2 was higher than that of HTLV-1 envelope proteins from position 4. Furthermore, the HTEnv-expressing viruses grew to higher titers than the HTEnvG-expressing viruses, although the HTEnvG-expressing viruses induced larger syncytia in the infected cells, as shown in Fig. 2. The greater syncytium formation by the EnvG proteins may have been inhibitory to virus production.
TABLE 1.
Titration of rVSVs bearing an HTLV-1 envelope gene in position 2 or 4 with or without G complementation
| Virus | Infectious titer (IU/ml)a on:
|
|
|---|---|---|
| BHK cells | 293T cells | |
| G complemented | ||
| VSVHTEnv2 | 1.1 × 108 | NDb |
| VSVHTEnv4 | 1.7 × 107 | ND |
| VSVHTEnvG2 | 8.7 × 107 | ND |
| VSVHTEnvG4 | 1.0 × 108 | ND |
| Noncomplemented | ||
| VSVHTEnv2 | 1.0 × 104 | 1.3 × 106 |
| VSVHTEnv4 | 3.9 × 103 | 8.0 × 104 |
| VSVHTEnvG2 | 6.0 × 102 | 1.2 × 104 |
| VSVHTEnvG4 | 2.3 × 102 | 1.9 × 103 |
Infectious titers were determined by counting GFP-expressing cells with a fluorescence microscope.
ND, not determined.
We also verified that infection by these noncomplemented viruses was completely inhibited with anti-HTLV-1 serum, indicating that it was mediated by the HTLV-1 Env proteins in the surrogate virus particles.
Effects of OPG on HTLV-1 infection of host cells.
It was shown that OPG/Fc (OPG fused to the C-terminal Fc region of human immunoglobulin G1 [IgG1]) suppressed osteoclastogenesis induced by cells from patients with ATL (28). Also, from a preliminary screen of genes encoding candidate HTLV-1 receptors, we identified OPG (K. Okuma, unpublished data). OPG has been shown to regulate the RANK-RANKL system, which is involved both in osteoclastogenesis, leading to hypercalcemia, and in T-cell immunity (1, 17, 21). OPG is a secreted, heparin- or HS-binding glycoprotein that belongs to the tumor necrosis factor receptor family (5, 41, 44). OPG is expressed in a variety of mouse and human tissues (39, 45) and inhibits the RANK-RANKL system by binding to RANKL (23). Furthermore, OPG is also a receptor for tumor necrosis factor-related apoptosis-inducing ligand (10).
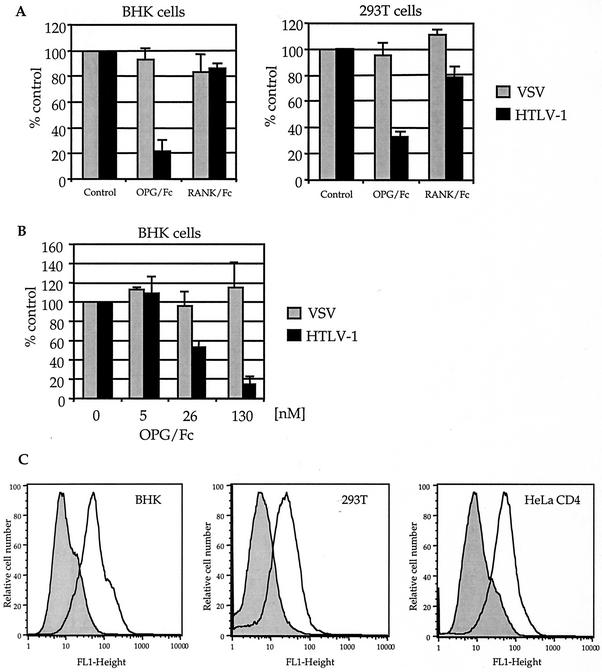
Although OPG is a soluble secreted protein, such a protein could act as a cellular receptor similar to the coreceptor for feline leukemia virus (2). Therefore, to investigate a possible additional role for OPG and RANK in HTLV-1 infection, we determined if human OPG/Fc (R & D Systems) and human RANK/Fc (the extracellular domain of RANK fused to the C-terminal Fc region of human IgG1; R&D Systems) could inhibit the infection of BHK or 293T cells by VSVHTEnv2 (sHTLV-1) (Fig. 3A and B). OPG/Fc significantly inhibited sHTLV-1 infection, but RANK/Fc showed only a marginal effect. Infection by VSV-GFP was not inhibited significantly by either protein (Fig. 3A). OPG/Fc also efficiently inhibited sHTLV-1 infection of BHK cells in a dose-dependent fashion but did not affect VSV-GFP (Fig. 3B).
FIG. 3.
Inhibitory effect of OPG/Fc on sHTLV-1 infection of cells and binding of OPG/Fc to cells. (A) The effects of OPG/Fc (10 μg/ml) and RANK/Fc (10 μg/ml) on the infection of cells by sHTLV-1 and VSV-GFP were evaluated. The viruses were diluted in FBS-free DMEM before inoculation, and the I1 and I14 anti-VSV G MAbs were also included in the inocula (except for VSV-GFP) at a dilution of 1:200 each to neutralize infection due to traces of G in the viral stock. Approximately 80% confluent cells were prepared on plates. After the media were removed, the cells were incubated with the mixture of the virus and the reagent(s) at 37°C for 1 h. The mixture was then withdrawn, and 5% FCS-DMEM containing 1% methylcellulose was added to the cells. To allow cells to express detectable levels of GFP, infections were allowed to continue at 37°C for 12 to 15 h. GFP-positive cells were then visualized, and the number of GFP-expressing cells was determined by fluorescence microscopy with an Olympus CK40 microscope with a 10× objective. The data shown are percentages of the control (means plus standard deviations) calculated from the numbers of GFP-positive cells among the treated and mock-treated cells (control) in repeated experiments. (B) The inhibitory effect of OPG/Fc on infection was examined at the indicated concentrations of OPG/Fc in BHK cells. After incubation of cells with sHTLV-1 or VSV-GFP and serially diluted OPG/Fc as described above, the number of GFP-expressing cells was determined after 12 to 15 h. The data shown are percentages of the control (means plus standard deviations) determined as described above. (C) Flow cytometry was used to examine OPG/Fc binding to the BHK, 293T, and HeLa CD4 cell surface. Live cells were incubated with or without OPG/Fc at 4°C for 30 min and then with an FITC-conjugated anti-human IgG Fc antibody at 4°C for 30 min. The stained cells were immediately analyzed by flow cytometry.
Binding of OPG to various cell lines.
Because OPG/Fc efficiently inhibited sHTLV-1 infection of the above cells, we determined by flow cytometry if OPG/Fc bound to the cells directly. Cells were collected by pipetting in phosphate-buffered saline containing 50 mM EDTA. Live cells were then incubated with or without 60 nM human OPG/Fc at 4°C for 30 min and then incubated with a 1:50 dilution of a fluorescein isothiocyanate (FITC)-conjugated goat anti-human IgG Fc antibody (Jackson Research) at 4°C for 30 min. Stained cells were analyzed immediately by flow cytometry for binding of OPG/Fc to the cells. Flow cytometry analysis showed that OPG/Fc bound to all of the cells we tested, including BHK (baby hamster kidney), 293T (human kidney), HeLa CD4 (human uterine cervix), L (murine fibroblast), and CHO-K1 (Chinese hamster ovary) cells (Fig. 3C and 4A). This result suggested that OPG might inhibit sHTLV-1 infection through binding to the surface of the target cell.
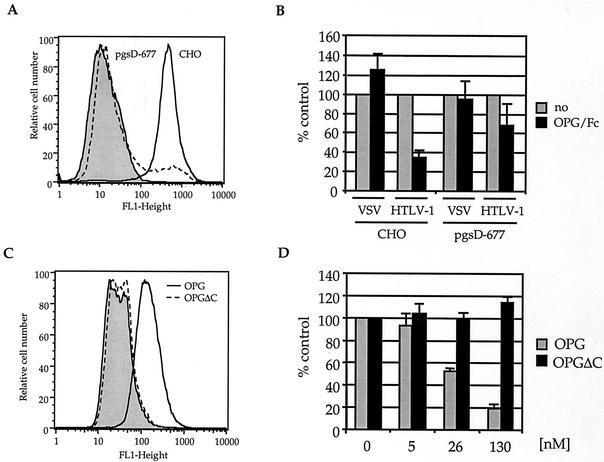
FIG. 4.
Analysis of binding and inhibitory effect of OPG. (A) The ability of OPG/Fc to bind mutant CHO cells (pgsD-677 cells) was determined by flow cytometry after staining. Live cells were incubated with or without 60 nM human OPG/Fc at 4°C for 30 min and then with a 1:50 dilution of an FITC-conjugated goat anti-human IgG Fc antibody at 4°C for 30 min. Stained cells were analyzed immediately by flow cytometry. (B) The effect of OPG/Fc on sHTLV-1 infection was examined in HS-deficient pgsD-677 cells. After the cells were incubated with sHTLV-1 or VSV-GFP and OPG/Fc (130 nM) at 37°C for 1 h, the mixtures were aspirated and the media containing 1% methylcellulose were added to the cells. GFP expression was observed under a fluorescence microscope after about 15 h. The data shown are percentages of the control (means plus standard deviations) from four independent experiments, as in Fig. 3. (C) Binding of OPGΔC lacking the HS-binding domain to CHO cells was analyzed by flow cytometry. The cells were incubated with or without OPG or OPGΔC at 4°C for 30 min, with polyclonal anti-human OPG at 4°C for 30 min, and then with FITC-conjugated anti-goat IgG at 4°C for 30 min. The stained cells were immediately examined by flow cytometry. (D) Inhibition of sHTLV-1 infection by OPG lacking the HS-binding domain was determined on CHO cells. The cells were incubated with sHTLV-1 and OPG or OPGΔC at 37°C for 1 h, and the number of GFP-expressing cells was determined after an additional 12 to 15 h. The results are percentages of the control (means plus standard deviations) from four repeated experiments, as described above.
Effects of OPG and SDF-1α on infection mediated by HTLV-1 and HIV-1 envelope proteins.
Because OPG/Fc bound to a variety of cell lines, it was possible that OPG, which contains a heparin-binding domain (44), interacted through binding to HS ubiquitously expressed on the cell surface. The inhibition of sHTLV-1 infection of cells might occur by competition of OPG for HS-binding sites.
To determine the specificity of the OPG effect, we determined if OPG/Fc inhibited the infection of a surrogate HIV-1 based on a VSVΔG-HIVEnv-GFP recombinant (4), because HIV-1 envelope proteins are known to interact to some degree with HS (42). HeLa CD4 cells (26) were incubated with a mixture of the virus and the reagent at 37°C for 1 h, and the number of GFP-positive cells was determined by fluorescence microscopy after 12 to 15 h. The effect was specific to the HTLV-1 Env-mediated infection (data not shown). Furthermore, because stromal cell-derived factor 1α (SDF-1α) interacts with HS (43), we tested whether SDF-1α (R&D Systems) inhibits sHTLV-1 infection. HeLa CD4 cells were incubated with the mixture of the virus and SDF-1α at 37°C for 1 h, and the number of GFP-positive cells was determined as described above. SDF-1α showed only a small inhibitory effect on sHTLV-1 infection but efficiently inhibited infection by the surrogate HIV-1, as expected (data not shown). These results suggest that the effect of OPG was specific to HTLV-1 infection. However, it is possible that the SDF-1α molecule has a lower affinity for HS or has less of an effect than OPG because it is a smaller molecule and has a reduced capacity to interfere with sHTLV-1 binding through steric hindrance of binding to a primary receptor.
Significant role of HS in HTLV-1 infection.
To define the importance of HS in HTLV-1 infection of host cells, we evaluated the susceptibility of HS-deficient cells to sHTLV-1. Appropriately diluted VSV-GFP or sHTLV-1 (including the I1 and I14 MAbs) was inoculated into the same number of cells prepared on a 96-well plate. The infection was allowed to proceed for about 15 h, and then the numbers of GFP-positive parental and mutant cells were compared. GAG (including HS)-deficient sog9 (3) and HS-deficient pgsD-677 (25) cells (American Type Culture Collection) showed much lower susceptibility (about 60 to 70% lower infection) to sHTLV-1 than did parental L and CHO cells, respectively, while these HS-deficient cells exhibited somewhat greater susceptibility to VSV-GFP than did the parental cells. The sog9 EXT1 cells, sog9 cells transfected with the EXT1 gene encoding HS copolymerase (27), express HS and showed greater susceptibility to sHTLV-1 than did sog9 cells lacking HS (data not shown). These data indicate that HTLV-1 envelope glycoproteins might interact with HS and that HS plays a significant role in HTLV-1 infection of host cells.
Involvement of HS in OPG inhibition of sHTLV-1 infection.
To confirm the ability of OPG to bind HS, we determined if OPG/Fc bound to HS-deficient CHO cells (pgsD-677 cells) by flow cytometry (Fig. 4A). OPG/Fc bound to parental CHO cells but to only a small fraction of HS-deficient pgsD-677 cells. This result confirms a role for HS in OPG binding to cells. Next, we examined the OPG inhibitory effect by using pgsD-677 cells. OPG/Fc strongly inhibited sHTLV-1 infection of CHO cells but had a smaller effect on pgsD-677 cells lacking HS (Fig. 4B). This result indicates that OPG elicited the inhibitory effect in the HTLV-1 infection through binding to HS.
Furthermore, to evaluate the importance of the HS-binding domain of OPG in the inhibitory effect on sHTLV-1 infection, we examined the cell-binding activity of OPG lacking its C-terminal domain (including the HS-binding domain) (PeproTech, referred to as OPGΔC herein). CHO cells were incubated in 5% normal donkey serum at 4°C for 30 min and incubated without or with 0.1 μM human OPGΔC or OPG (R&D Systems) at 4°C for 30 min. They were then incubated at 4°C for 30 min with 2 μg of polyclonal goat anti-human OPG neutralizing antibody (R&D Systems) per ml. Finally, they were incubated with a 1:50 dilution of an FITC-conjugated donkey anti-goat antibody (Jackson Research) at 4°C for 30 min and then analyzed by flow cytometry. Flow cytometry analysis showed that OPG bound to CHO cells but OPGΔC did not (Fig. 4C). Next, we determined if OPGΔC inhibited sHTLV-1 infection of cells. Although OPG inhibited sHTLV-1 infection of CHO cells, OPGΔC did not (Fig. 4D). These data reveal that OPG bound to HS on the cell surface via the HS-binding domain and blocked HTLV-1 infection through the interaction with HS.
There could be several explanations for the inhibitory effects of OPG on sHTLV-1 infection. (i) OPG could compete with HTLV-1 envelope glycoproteins for binding to cell surface HS and thus limit binding to an HTLV-1-specific receptor. (ii) OPG could induce the internalization of HS proteoglycan into the cytoplasm through cross-linking of HS proteoglycan by OPG (13, 41) and reduce the binding of HTLV-1 to a specific receptor. (iii) If HS is present on the surface of sHTLV-1 virions, OPG might also interact with HS on virions, resulting in the steric hindrance of virus binding to HS or to a primary receptor on the cell surface. This third mechanism could explain why OPG/Fc still shows some inhibition of sHTLV-1 infection on HS-deficient pgsD-677 cells (Fig. 4B). (iv) If an HS-binding protein, such as cyclophilin A as an attachment mediator on HIV (35), is incorporated on the surface of sHTLV-1 particles, OPG may block the interaction of such an HS-binding protein, but not HTLV-1 Env, with cell surface HS.
Several other viruses, such as HIV-1, are known to use HS as a receptor (6, 8, 12, 38, 42), although this role of HS in HIV-1 infection appears to be dependent on the envelope (18, 46). From these studies, a general model has emerged in which HS is a primary virus attachment molecule used by many viruses and in which initial binding to HS facilitates subsequent binding to a primary receptor. This general model appears to fit HTLV-1 well also. Although HS is not essential for sHTLV-1 infection, it greatly facilitates the process.
We have shown here that an rVSV expressing high levels of HTLV-1 envelope glycoproteins is a useful tool with which to explore molecules involved in HTLV-1 infection and to analyze the mechanism of the inhibitory effect of the OPG molecule. We have also confirmed and extended information on the requirement for cell surface HS in efficient infection by HTLV-1. Our findings suggest that HTLV-1 spread in vivo may also be subject to inhibition by HS-binding proteins such as OPG in serum.
Acknowledgments
We thank Frank Tufaro and Amy Jackson-Fisher for generously providing mutant L cells and 293T cells, respectively. We are grateful to Yusuke Yanagi and Minoru Nakamura for comments and helpful suggestions about HTLV-1. We also thank Geraldine L. Shu and Edward A. Clark for helpful suggestions concerning OPG.
This work was supported by grants from the National Institutes of Health.
REFERENCES
- 1.Anderson, D. M., E. Maraskovsky, W. L. Billingsley, W. C. Dougall, M. E. Tometsko, E. R. Roux, M. C. Teepe, R. F. DuBose, D. Cosman, and L. Galibert. 1997. A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature 390:175-179. [DOI] [PubMed] [Google Scholar]
- 2.Anderson, M. M., A. S. Lauring, C. C. Burns, and J. Overbaugh. 2000. Identification of a cellular cofactor required for infection by feline leukemia virus. Science 287:1828-1830. [DOI] [PubMed] [Google Scholar]
- 3.Banfield, B. W., Y. Leduc, L. Esford, K. Schubert, and F. Tufaro. 1995. Sequential isolation of proteoglycan synthesis mutants by using herpes simplex virus as a selective agent: evidence for a proteoglycan-independent virus entry pathway. J. Virol. 69:3290-3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boritz, E., J. Gerlach, J. E. Johnson, and J. K. Rose. 1999. Replication-competent rhabdoviruses with human immunodeficiency virus type 1 coats and green fluorescent protein: entry by a pH-independent pathway. J. Virol. 73:6937-6945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borset, M., O. Hjertner, S. Yaccoby, J. Epstein, and R. D. Sanderson. 2000. Syndecan-1 is targeted to the uropods of polarized myeloma cells where it promotes adhesion and sequesters heparin-binding proteins. Blood 96:2528-2536. [PubMed] [Google Scholar]
- 6.Byrnes, A. P., and D. E. Griffin. 1998. Binding of Sindbis virus to cell surface heparan sulfate. J. Virol. 72:7349-7356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daenke, S., S. A. McCracken, and S. Booth. 1999. Human T-cell leukaemia/lymphoma virus type 1 syncytium formation is regulated in a cell-specific manner by ICAM-1, ICAM-3 and VCAM-1 and can be inhibited by antibodies to integrin beta2 or beta7. J. Gen. Virol. 80(Pt. 6):1429-1436. [DOI] [PubMed] [Google Scholar]
- 8.Dechecchi, M. C., P. Melotti, A. Bonizzato, M. Santacatterina, M. Chilosi, and G. Cabrini. 2001. Heparan sulfate glycosaminoglycans are receptors sufficient to mediate the initial binding of adenovirus types 2 and 5. J. Virol. 75:8772-8780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delamarre, L., A. R. Rosenberg, C. Pique, D. Pham, I. Callebaut, and M. C. Dokhelar. 1996. The HTLV-I envelope glycoproteins: structure and functions. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13:S85-S91. [DOI] [PubMed] [Google Scholar]
- 10.Emery, J. G., P. McDonnell, M. B. Burke, K. C. Deen, S. Lyn, C. Silverman, E. Dul, E. R. Appelbaum, C. Eichman, R. DiPrinzio, R. A. Dodds, I. E. James, M. Rosenberg, J. C. Lee, and P. R. Young. 1998. Osteoprotegerin is a receptor for the cytotoxic ligand TRAIL. J. Biol. Chem. 273:14363-14367. [DOI] [PubMed] [Google Scholar]
- 11.Fan, N., J. Gavalchin, B. Paul, K. H. Wells, M. J. Lane, and B. J. Poiesz. 1992. Infection of peripheral blood mononuclear cells and cell lines by cell-free human T-cell lymphoma/leukemia virus type I. J. Clin. Microbiol. 30:905-910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldman, S. A., S. Audet, and J. A. Beeler. 2000. The fusion glycoprotein of human respiratory syncytial virus facilitates virus attachment and infectivity via an interaction with cellular heparan sulfate. J. Virol. 74:6442-6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fuki, I. V., K. M. Kuhn, I. R. Lomazov, V. L. Rothman, G. P. Tuszynski, R. V. Iozzo, T. L. Swenson, E. A. Fisher, and K. J. Williams. 1997. The syndecan family of proteoglycans. Novel receptors mediating internalization of atherogenic lipoproteins in vitro. J. Clin. Investig. 100:1611-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haglund, K., I. Leiner, K. Kerksiek, L. Buonocore, E. Pamer, and J. K. Rose. 2002. High-level primary CD8+ T-cell response to human immunodeficiency virus type 1 Gag and Env generated by vaccination with recombinant vesicular stomatitis viruses. J. Virol. 76:2730-2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hildreth, J. E., A. Subramanium, and R. A. Hampton. 1997. Human T-cell lymphotropic virus type 1 (HTLV-1)-induced syncytium formation mediated by vascular cell adhesion molecule 1: evidence for involvement of cell adhesion molecules in HTLV-1 biology. J. Virol. 71:1173-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinuma, Y., K. Nagata, M. Hanaoka, M. Nakai, T. Matsumoto, K. I. Kinoshita, S. Shirakawa, and I. Miyoshi. 1981. Adult T-cell leukemia: antigen in an ATL cell line and detection of antibodies to the antigen in human sera. Proc. Natl. Acad. Sci. USA 78:6476-6480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsu, H., D. L. Lacey, C. R. Dunstan, I. Solovyev, A. Colombero, E. Timms, H. L. Tan, G. Elliott, M. J. Kelley, I. Sarosi, L. Wang, X. Z. Xia, R. Elliott, L. Chiu, T. Black, S. Scully, C. Capparelli, S. Morony, G. Shimamoto, M. B. Bass, and W. J. Boyle. 1999. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc. Natl. Acad. Sci. USA 96:3540-3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ibrahim, J., P. Griffin, D. R. Coombe, C. C. Rider, and W. James. 1999. Cell-surface heparan sulfate facilitates human immunodeficiency virus type 1 entry into some cell lines but not primary lymphocytes. Virus Res. 60:159-169. [DOI] [PubMed] [Google Scholar]
- 19.Johnson, J. E., M. J. Schnell, L. Buonocore, and J. K. Rose. 1997. Specific targeting to CD4+ cells of recombinant vesicular stomatitis viruses encoding human immunodeficiency virus envelope proteins. J. Virol. 71:5060-5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kiyokawa, T., K. Yamaguchi, M. Takeya, K. Takahashi, T. Watanabe, T. Matsumoto, S. Y. Lee, and K. Takatsuki. 1987. Hypercalcemia and osteoclast proliferation in adult T-cell leukemia. Cancer 59:1187-1191. [DOI] [PubMed] [Google Scholar]
- 21.Kong, Y. Y., W. J. Boyle, and J. M. Penninger. 2000. Osteoprotegerin ligand: a regulator of immune responses and bone physiology. Immunol. Today 21:495-502. [DOI] [PubMed] [Google Scholar]
- 22.Kretzschmar, E., L. Buonocore, M. J. Schnell, and J. K. Rose. 1997. High-efficiency incorporation of functional influenza virus glycoproteins into recombinant vesicular stomatitis viruses. J. Virol. 71:5982-5989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lacey, D. L., E. Timms, H. L. Tan, M. J. Kelley, C. R. Dunstan, T. Burgess, R. Elliott, A. Colombero, G. Elliott, S. Scully, H. Hsu, J. Sullivan, N. Hawkins, E. Davy, C. Capparelli, A. Eli, Y. X. Qian, S. Kaufman, I. Sarosi, V. Shalhoub, G. Senaldi, J. Guo, J. Delaney, and W. J. Boyle. 1998. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93:165-176. [DOI] [PubMed] [Google Scholar]
- 24.Lawson, N. D., E. A. Stillman, M. A. Whitt, and J. K. Rose. 1995. Recombinant vesicular stomatitis viruses from DNA. Proc. Natl. Acad. Sci. USA 92:4477-4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lidholt, K., J. L. Weinke, C. S. Kiser, F. N. Lugemwa, K. J. Bame, S. Cheifetz, J. Massague, U. Lindahl, and J. D. Esko. 1992. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a Chinese hamster ovary cell mutant defective in heparan sulfate biosynthesis. Proc. Natl. Acad. Sci. USA 89:2267-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maddon, P. J., A. G. Dalgleish, J. S. McDougal, P. R. Clapham, R. A. Weiss, and R. Axel. 1986. The T4 gene encodes the AIDS virus receptor and is expressed in the immune system and the brain. Cell 47:333-348. [DOI] [PubMed] [Google Scholar]
- 27.Mardberg, K., E. Trybala, F. Tufaro, and T. Bergstrom. 2002. Herpes simplex virus type 1 glycoprotein C is necessary for efficient infection of chondroitin sulfate-expressing gro2C cells. J. Gen. Virol. 83:291-300. [DOI] [PubMed] [Google Scholar]
- 28.Nosaka, K., T. Miyamoto, T. Sakai, H. Mitsuya, T. Suda, and M. Matsuoka. 2002. Mechanism of hypercalcemia in adult T-cell leukemia: overexpression of receptor activator of nuclear factor κB ligand on adult T-cell leukemia cells. Blood 99:634-640. [DOI] [PubMed] [Google Scholar]
- 29.Okuma, K., Y. Matsuura, H. Tatsuo, Y. Inagaki, M. Nakamura, N. Yamamoto, and Y. Yanagi. 2001. Analysis of the molecules involved in human T-cell leukaemia virus type 1 entry by a vesicular stomatitis virus pseudotype bearing its envelope glycoproteins. J. Gen. Virol. 82:821-830. [DOI] [PubMed] [Google Scholar]
- 30.Okuma, K., M. Nakamura, S. Nakano, Y. Niho, and Y. Matsuura. 1999. Host range of human T-cell leukemia virus type I analyzed by a cell fusion-dependent reporter gene activation assay. Virology 254:235-244. [DOI] [PubMed] [Google Scholar]
- 31.Owens, R. J., and J. K. Rose. 1993. Cytoplasmic domain requirement for incorporation of a foreign envelope protein into vesicular stomatitis virus. J. Virol. 67:360-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pique, C., D. Pham, T. Tursz, and M. C. Dokhelar. 1992. Human T-cell leukemia virus type I envelope protein maturation process: requirements for syncytium formation. J. Virol. 66:906-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pique, C., T. Tursz, and M. C. Dokhelar. 1990. Mutations introduced along the HTLV-I envelope gene result in a non-functional protein: a basis for envelope conservation? EMBO J. 9:4243-4248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poiesz, B. J., F. W. Ruscetti, A. F. Gazdar, P. A. Bunn, J. D. Minna, and R. C. Gallo. 1980. Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc. Natl. Acad. Sci. USA 77:7415-7419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saphire, A. C., M. D. Bobardt, and P. A. Gallay. 1999. Host cyclophilin A mediates HIV-1 attachment to target cells via heparans. EMBO J. 18:6771-6785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schnell, M. J., L. Buonocore, E. Kretzschmar, E. Johnson, and J. K. Rose. 1996. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc. Natl. Acad. Sci. USA 93:11359-11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seiki, M., S. Hattori, Y. Hirayama, and M. Yoshida. 1983. Human adult T-cell leukemia virus: complete nucleotide sequence of the provirus genome integrated in leukemia cell DNA. Proc. Natl. Acad. Sci. USA 80:3618-3622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shukla, D., J. Liu, P. Blaiklock, N. W. Shworak, X. Bai, J. D. Esko, G. H. Cohen, R. J. Eisenberg, R. D. Rosenberg, and P. G. Spear. 1999. A novel role for 3-O-sulfated heparan sulfate in herpes simplex virus 1 entry. Cell 99:13-22. [DOI] [PubMed] [Google Scholar]
- 39.Simonet, W. S., D. L. Lacey, C. R. Dunstan, M. Kelley, M. S. Chang, R. Luthy, H. Q. Nguyen, S. Wooden, L. Bennett, T. Boone, G. Shimamoto, M. DeRose, R. Elliott, A. Colombero, H. L. Tan, G. Trail, J. Sullivan, E. Davy, N. Bucay, L. Renshaw-Gegg, T. M. Hughes, D. Hill, W. Pattison, P. Campbell, W. J. Boyle, et al. 1997. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309-319. [DOI] [PubMed] [Google Scholar]
- 40.Sommerfelt, M. A. 1999. Retrovirus receptors. J. Gen. Virol. 80:3049-3064. [DOI] [PubMed] [Google Scholar]
- 41.Standal, T., C. Seidel, O. Hjertner, T. Plesner, R. D. Sanderson, A. Waage, M. Borset, and A. Sundan. 2002. Osteoprotegerin is bound, internalized, and degraded by multiple myeloma cells. Blood 100:3002-3007. [DOI] [PubMed] [Google Scholar]
- 42.Ugolini, S., I. Mondor, and Q. J. Sattentau. 1999. HIV-1 attachment: another look. Trends Microbiol. 7:144-149. [DOI] [PubMed] [Google Scholar]
- 43.Valenzuela-Fernandez, A., T. Palanche, A. Amara, A. Magerus, R. Altmeyer, T. Delaunay, J. L. Virelizier, F. Baleux, J. L. Galzi, and F. Arenzana-Seisdedos. 2001. Optimal inhibition of X4 HIV isolates by the CXC chemokine stromal cell-derived factor 1α requires interaction with cell surface heparan sulfate proteoglycans. J. Biol. Chem. 276:26550-26558. [DOI] [PubMed] [Google Scholar]
- 44.Yamaguchi, K., M. Kinosaki, M. Goto, F. Kobayashi, E. Tsuda, T. Morinaga, and K. Higashio. 1998. Characterization of structural domains of human osteoclastogenesis inhibitory factor. J. Biol. Chem. 273:5117-5123. [DOI] [PubMed] [Google Scholar]
- 45.Yun, T. J., P. M. Chaudhary, G. L. Shu, J. K. Frazer, M. K. Ewings, S. M. Schwartz, V. Pascual, L. E. Hood, and E. A. Clark. 1998. OPG/FDCR-1, a TNF receptor family member, is expressed in lymphoid cells and is up-regulated by ligating CD40. J. Immunol. 161:6113-6121. [PubMed] [Google Scholar]
- 46.Zhang, Y. J., T. Hatziioannou, T. Zang, D. Braaten, J. Luban, S. P. Goff, and P. D. Bieniasz. 2002. Envelope-dependent, cyclophilin-independent effects of glycosaminoglycans on human immunodeficiency virus type 1 attachment and infection. J. Virol. 76:6332-6343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao, T. M., M. A. Robinson, F. S. Bowers, and T. J. Kindt. 1995. Characterization of an infectious molecular clone of human T-cell leukemia virus type I. J. Virol. 69:2024-2030. [DOI] [PMC free article] [PubMed] [Google Scholar]