Abstract
Denaturing high-performance liquid chromatography (DHPLC) has been used extensively to detect genetic variation. We used this method to detect and identify Yersinia pestis KIM5 ciprofloxacin-resistant isolates by analyzing the quinolone resistance-determining region (QRDR) of the gyrase A gene. Sequencing of the Y. pestis KIM5 strain gyrA QRDR from 55 ciprofloxacin-resistant isolates revealed five mutation types. We analyzed the gyrA QRDR by DHPLC to assess its ability to detect point mutations and to determine whether DHPLC peak profile analysis could be used as a molecular fingerprint. In addition to the five mutation types found in our ciprofloxacin-resistant isolates, several mutations in the QRDR were generated by site-directed mutagenesis and analyzed to further evaluate this method for the ability to detect QRDR mutations. Furthermore, a blind panel of 42 samples was analyzed by screening for two mutant types to evaluate the potential diagnostic value of this method. Our results showed that DHPLC is an efficient method for detecting mutations in genes that confer antibiotic resistance.
Yersinia pestis is a gram-negative bacillus belonging to the Enterobacteriaceae family. This organism can cause several different forms of disease, including bubonic, pneumonic, and septicemic plague, depending on the route of exposure (26). Bubonic plague usually infects one group of lymph nodes, and infection can travel to the lungs. Pneumonic plague is transmitted by airborne droplets. Infection takes place within hours and causes bronchopneumonia. Plague pneumonia can be treated if it is recognized early. Delay of therapy results in high mortality rates (30), making the organism an effective biological warfare agent.
Ciprofloxacin is an antibiotic that has been used to treat many bacterial diseases, including Enterobacteriaceae infections (6, 7, 14, 19-21, 27, 32). Ciprofloxacin belongs to the fluoroquinolone class of antibiotics that inhibit bacterial DNA replication by inhibiting the activity of DNA gyrase. The major weakness of this class of compounds is that a single mutation in the DNA gyrase gene may make the bacteria resistant to antibiotic activity. In the event of a biological attack involving this agent, rapid detection of antibiotic-resistant bacteria would have critical importance.
In bacteria, DNA contains a little less than one helical turn for each 10.4 bp. This leaves the bacterial genome slightly unwound, and negative supertwists are unfavorable energetically. Topoisomerases are enzymes that alter the number of times a DNA strand wraps around itself. In prokaryotes, type II topoisomerase is a DNA gyrase which cleaves the double strand and introduces negative supercoils (9). DNA gyrase consists of two 100-kDa A subunits encoded by the gyrA gene and two 90-kDa B subunits encoded by the gyrB gene (35). Mutations in either or both of these genes may make an organism resistant to ciprofloxacin.
Denaturing high-performance liquid chromatography (DHPLC) is a quick and sensitive method for detecting genetic mutations and has been used extensively to analyze genes for mutations (1, 3-5, 11, 12, 17, 18, 23, 24, 31, 38). The method consists of four steps: amplification of driver and experimental DNA by PCR, quantification of the amplified PCR product, hybridization of amplified driver and experimental DNA, and analysis of the hybridized product. After PCR, heteroduplexes between driver and experimental amplicons are formed during hybridization. Mismatches between driver and experimental DNA sequences disrupt the heteroduplex, and DHPLC resolves these differences.
We amplified the quinolone resistance-determining region (QRDR) (39) and the 3′- and 5′-flanking regions from 55 ciprofloxacin-resistant isolates to determine whether DHPLC could be used to detect and identify ciprofloxacin-resistant strains of Y. pestis KIM5. In addition, we tested the capability of DHPLC to identify other types of mutations by creating four other mutations in the QRDR by site-directed mutagenesis. We also tested the potential of DHPLC to identify mutations in a blind panel. Two mutation types were used as controls and tested against a panel of 42 samples to demonstrate how this method may be used for identification purposes.
MATERIALS AND METHODS
Ciprofloxacin-resistant KIM5 mutants and antibiotic sensitivity.
The organism KIM5, an avirulent, pigmentation-negative (pgm-negative) mutant of Y. pestis, was used as wild type in the present study. KIM5 was the parental organism from which ciprofloxacin-resistant isolates were selected. The organism was grown on brain heart infusion (BHI) agar (Difco Laboratories, Detroit, Mich.) plates for 48 h at 30°C or overnight in BHI broth at 30°C with aeration. After incubation, the bacteria were twice washed with phosphate-buffered saline (150 mM NaCl, 1.7 mM KH2PO4, 5 mM Na2PO4 [pH 7.4]) and then suspended to a concentration of 1011 CFU/ml. A 100-μl portion of washed bacteria was plated on BHI agar plates containing 1 to 10 μg of ciprofloxacin (Bayer, Leverkusen, Germany)/ml. Ciprofloxacin-resistant mutants appeared after 48 to 72 h of incubation at 30°C. Isolated colonies were purified by streaking on fresh BHI agar plates containing the appropriate concentration of ciprofloxacin. The MIC for ciprofloxacin was determined by using E-Test (AB Biodisk, Piscataway, N.J.). Biosafety level 2 and level 3 procedures were followed when we worked with KIM5 and ciprofloxacin-resistant organisms.
Site-directed mutagenesis to create additional QRDR mutations.
In vitro-generated Y. pestis gyrA templates were generated by performing splice overhang extension (SOE) PCR (13) to generate a 891-bp fragment encoding all of the GyrA QRDR. Nucleotide changes were chosen such that simple single-base-pair substitutions would change codons 67, 84, 87, and 106 (Escherichia coli numbering; GenBank accession no. P09097) to the most common amino acids found in ciprofloxacin-resistant mutants (29). The outside primers for these reactions were gyrAupper (AAAAGAATTCCTGGAGGATAGCGGGTGAG) and gyrAlower (CCCCGAATTCGCACGTGCGCGGATATAGAC). Underlined nucleotides indicate EcoRI sites added to facilitate cloning of the final PCR products into pUC19. The gyrAupper primer was combined with the reverse base substitution primers to generate the 5′ end of the Y. pestis gyrA sequence. The reverse base substitution primers were as follows: SOE67R, CACGGGACGATTTTTTGTATGG; SOE84R, CGGGCTGTCACCATGCGGG; SOE87R, CGATAGTGTTGTAGACCGC; and SOE106R, GAAGTTACCATGCCCATCCAC. The gyrAlower primer was combined with the forward base substitution primer to generate the 3′ end of the Y. pestis gyrA sequence. The forward base substitution primers were as follows: SOE67F, CCATACAAAAAATCGTCCCGTG; SOE84F, CCCGCATGGTGACAGCCCG; SOE87F, GCGGTCTACAACACTATCG; and SOE106F, GTGGATGGGCATGGTAACTTC. The underlined nucleotides in the base substitution primers represent the position of nucleotide changes relative to the wild-type Y. pestis KIM5 gyrA sequence. After SOE PCR, the products were purified (Qiagen, Valencia, Calif.), digested with EcoRI, and cloned into pUC19. All in vitro-generated mutants were sequenced on an Applied Biosystems 377XL apparatus by using BigDye (Applied Biosystems) cycle sequencing to confirm the presence of the expected nucleotide changes and that no other changes had occurred during PCR.
Amplification of the QRDRs of the gyrase A gene.
The primer set YPCPR1U (5′-TAC CGC AAT ACC CGA CGA A-3′; sense)-YPCPR1L (5′-ATT ATG CGA TGT CCG TTA TTG TC-3′; antisense) yielded a 419-bp product that spanned the QRDR in the DNA gyrase gyrA gene, as well as the 5′- and 3′-flanking regions. Each mutant and wild type was amplified in 100-μl reaction mixtures containing 1.0 μM concentrations of each primer, 40 μM concentrations of each deoxynucleoside triphosphate, 10 μl of 10× PCR buffer II, 5.0 U of AmpliTaq Gold (Applied Biosystems), and 8.0 μl of 25 mM MgCl2 in molecular-biology-grade water. Cycling conditions were a 10-min preincubation at 95°C to activate the AmpliTaq Gold, followed by 30 cycles of 1 min at 95°C, 1 min at 60°C, and 1 min at 72°C, and a 10-min final extension at 72°C. All PCRs were performed on an MJ Research PTC-100 thermocycler.
Quantification of PCR product.
PCR yields were quantitatively determined by reversed-phase high-performance liquid chromatography with Transgenomic WAVE software and a Transgenomic DNA fragment analysis system. The area under each peak was measured in millivolts; these units were used for quantification. The mobile phase was composed of buffer A (0.1 M triethylammonium acetate [pH 7.0], 0.025% acetonitrile) and buffer B (0.1 M triethylammonium acetate [pH 7.0], 25% acetonitrile). The analytical gradient used for quantification was 0.0 min in 45.0% buffer A-55.0% buffer B, 0.5 min in 40.0% buffer A -60.0% buffer B, 5.0 min in 31.0% buffer A-69.0% buffer B, 5.1 min in 0.0% buffer A-100.0% buffer B, 5.7 min in 45.0% buffer A-55.0% buffer B, and 6.6 min in 45.0% buffer A-55.0% buffer B at 0.9 ml/min at 50°C. The columns used for analysis were 50-by-4.4-mm ID DNASep cartridges packed with nonporous polystyrene divinylbenzene copolymer particles 2.1 ± 0.12 μm in diameter. A total of 15 μl of crude PCR product from each sample was injected onto the column.
Formation of heteroduplexes.
Hybridization reaction mixtures were 200 μl and contained 10 mM EDTA and equimolar amounts of driver (Y. pestis KIM5 PCR product) and experimental Y. pestis PCR product, KIM5, or mutant in molecular-biology-grade water. The quantity of crude PCR product was standardized to 200,000 U as determined by using Transgenomic 4.1 WAVE software. The hybridization conditions were a 4-min 95°C preincubation followed by cooling at −1.5°C/min to 25°C over 45 min.
DHPLC analysis of Y. pestis KIM5 strain ciprofloxacin-resistant isolates.
The QRDR, as well as the 5′- and 3′-flanking regions in the DNA gyrase gyrA gene of 86 Y. pestis KIM5 strain ciprofloxacin-resistant samples, was analyzed to determine whether DHPLC was a suitable method of detecting ciprofloxacin-resistant organisms. A 15-μl portion of hybridized PCR product was run with the following analytical gradient: 0.0 min in 47% buffer A-53% buffer B, 0.5 min in 42% buffer A-58% buffer B, 5.0 min in 33% buffer A-67% buffer B, 5.1 min in 0% buffer A-100% buffer B, 5.7 min in 47% buffer A-53% buffer B, and 6.6 min in 47% buffer A-53% buffer B at 0.9 ml/min.
Several columns were used in the course of the study. Past work in this laboratory showed that each column will produce slightly different results (15). To determine the optimal temperature for identifying mutations, the homoduplex was run at 61, 62, 63, 64, and 65°C. After the temperature at which the homoduplex eluted from the column had been found, a temperature gradient was run starting at the last temperature at which homoduplex did not run off the column and increasing it by 0.3, 0.5, and 0.7°C. The warmest temperature at which the homoduplex did not run off the column was used to identify mutations.
Sequencing of PCR amplicons.
The PCR product was purified by using a Montage PCR cleanup kit (Millipore). Sequencing reaction mixtures were 20 μl containing 2.5 μM primer, 45 ng of PCR product, 8 μl of BigDye, and molecular-biology-grade water. The sequence cycling conditions were a 30-s preincubation at 85°C followed by 25 cycles of 10 s at 96°C, 5 s at 50°C, and 4 min at 60°C, with a 10-min final extension at 60°C. The sequencing reaction products were purified with 96-well EX DYE plates (Qiagen). Sequencing was performed on an ABI Prism 3100 genetic analyzer (Applied Biosystems) according to the manufacturer's instructions. The newly identified Y. pestis KIM5 gyrA mutant had Ser-to-Arg change at position 83 and was designated M5 (Table 1).
TABLE 1.
Nucleotide sequences of the Y. pestis KIM5 mutations found in the samples examined in the present studya
| Mutation | Sequence | Amino acid substitutionb |
|---|---|---|
| KIM5 (wild type) | AC CAC CCG CAT GGT GAC AGC GCG GTC TAC GAC | None |
| M1 | AC CAC CCG CAT GAT GAC AGC GCG GTC TAC GAC | Gly to Asp at position 81 |
| M2 | AC CAC CCG CAT TGT GAC AGC GCG GTC TAC GAC | Gly to Cys at position 81 |
| M3 | AC CAC CCG CAT GGT GAC ATC GCG GTC TAC GAC | Ser to Ile at position 83 |
| M4 | AC CAC CCG CAT GGT GAC AGA GCG GTC TAC GAC | Ser to Arg at position 83 |
| M5 | AC CAC CCG CAT GGT GAC AGG GCG GTC TAC GAC | Ser to Arg at position 83 |
| M6 | AC CAC CCG CAT GGT GAC AGC CCG GTC TAC GAC | Ala to Pro at position 84 |
| M8 | AC CAC CCG CAT GGT GAC AGC GCG GTC TAC AAC | Asp to Asn at position 87 |
The mutation types are in boldface and underlined. Mutations M1 to M4 were previously described (22). Mutation M5 has not been previously reported in Y. pestis. Mutations M6 and M8 were generated by site-directed mutagenesis. In addition, two other mutations were generated by site-directed mutagenesis; M7 was an Ala-to-Ser change at position 67, and M9 was a Gln-to-His change at position 106 (data not shown).
Position refers to the amino acid residue encoded by E. coli gyrA.
Blind panel analysis.
To access the ability of DHPLC to identify particular KIM5 samples, a blind panel of 42 QRDR mutations, with 39 representing seven different QRDR mutations and 3 representing wild-type KIM5 (Table 2), was analyzed by using the previously described PCR conditions and analytical gradients. Blind panel samples were analyzed with a new column that was calibrated to determine optimal temperature for mutation detection by using the method described above. M1 and M8 heteroduplexes with Y. pestis KIM5 as driver were used to generate reference DHPLC peak profiles.
TABLE 2.
Blind panel testing for ciprofloxacin-resistant mutations M1 and M8
| Mutation | No. of tested samples | No. of samples positive by:
|
|
|---|---|---|---|
| M1 DHPLC | M8 DHPLC | ||
| M1 | 15 | 15 | 0 |
| M2 | 3 | 0 | 0 |
| M3 | 11 | 0 | 0 |
| M4 | 6 | 0 | 0 |
| M5 | 2 | 0 | 0 |
| M8 | 1 | 0 | 1 |
| M9 | 1 | 0 | 0 |
| Ciprofloxacin-sensitive KIM5 | 3 | 0 | 0 |
Nucleotide sequence accession number.
The nucleotide sequence of the M5 gyrA mutant has been deposited in GenBank under accession no. AF487466.
RESULTS
Analysis by DHPLC to detect mutations associated with resistance to ciprofloxacin.
To determine whether DHPLC can be used as a method of detecting ciprofloxacin-resistant Y. pestis, we formed homoduplexes and heteroduplexes among amplified DNAs representing the QRDR of gyrA and then analyzed DHPLC adsorbance profiles from these duplexes. To form a heteroduplex, we hybridized driver amplicons from ciprofloxacin-sensitive strain KIM5 with a sample of experimental DNA. Experimental DNA was amplified from 55 ciprofloxacin-resistant isolates and from four products of site-directed mutagenisis. We analyzed a total of 86 samples in two lots (Table 3) and with two different DHPLC columns. Two different DHPLC columns were used because a previous DHPLC study showed that each column will give slightly different results (15). We obtained nine peak profile types from the 31 samples [Fig. 1 and Fig. 2]. Each of the mutations M1, M2, M3, M4, and M5 had a unique peak profile type that was distinct from that of the KIM5 wild type (Fig. 1). The four mutations generated by site-directed mutagenesis (M6, M7, M8, and M9) were also analyzed in this group (Fig. 2). These in vitro-derived templates showed that the M6 mutation had a peak profile identical to M4, whereas the M7 mutation produced a unique chromatogram. Mutation types M8 and M9 had peak profiles similar to that of the KIM5 wild type but could be differentiated from each other based on maximum absorbance (Fig. 2).
TABLE 3.
Summary of mutations in the Y. pestis KIM5 ciprofloxacin-resistant isolates used for the initial proof of concept
| Mutation | MICb (μg/ml) | No. of samplesa in:
|
Total no. of samples | |
|---|---|---|---|---|
| Lot 1 | Lot 2 | |||
| M1 | 4.10 | 13 | 27 | 40 |
| M2 | 1.33 | 4 | 4 | 8 |
| M3 | 1.31 | 9 | 21 | 30 |
| M4 | 4.35 | 4 | 3 | 7 |
| M5 | 1.12 | 1 | 0 | 1 |
| Total | 31 | 55 | 86 | |
Fifty-five isolates (isolated bacterial colonies) were selected for the 86 samples in lots 1 and 2. Some isolates are represented more than once within a lot: lot 1 contained 31 samples from 23 isolates, and lot 2 contained 55 samples from 32 isolates.
The average MICs for the Y. pestis KIM5 mutants were determined by duplicate E-Tests in five independent experiments.
FIG. 1.
DHPLC peak profiles obtained from Y. pestis strain KIM5 and ciprofloxacin-resistant mutants of KIM5. All peak profiles depicted are from the first lot of samples and were generated from the same column, which was the column used to generate the peak profiles depicted in Fig. 2. (A) KIM5 homoduplex; (B) KIM5-mutation type M1 heteroduplex; (C) KIM5-mutation type M2 heteroduplex; (D) KIM5-mutation type M3 heteroduplex; (E) KIM5-mutation type M4 heteroduplex; (F) KIM5-mutation type M5 heteroduplex.
FIG. 2.
DHPLC peak profiles of QRDR mutations generated by site-directed mutagenesis. All peak profiles depicted are from the first lot of samples and were generated from the same column, which was the column used to generate the peak profiles depicted in Fig. 1. (A) KIM5-mutation type M6 heteroduplex; (B) overlay of KIM5-M4 mutation type heteroduplex (tan) and KIM5-M6 mutation type heteroduplex (red); (C) KIM5-M7 mutation type heteroduplex; (D) KIM5 homoduplex (right), KIM5-M8 mutation type heteroduplex (left) and KIM5-M9 mutation type heteroduplex (middle).
A different column was used to analyze the second lot of samples that contained 55 samples from 32 isolates. We ran the KIM5 homoduplex to determine the optimal temperature for mutation detection and found it to be 0.2°C cooler than that of the first column. This column produced chromatograms similar to those of the previous column. We were able to identify all four mutation types (M1, M2, M3, and M4) in this lot.
Sequencing of Y. pestis KIM5, ciprofloxacin-resistant isolates, and site-directed mutations.
In order to determine the nucleotide sequence of all KIM5 mutants, we sequenced the amplicons from the PCR product of 55 ciprofloxacin-resistant isolates by using the previously described YPCPR primer set. The sequencing data revealed that there were five different types of mutations present in these 55 ciprofloxacin-resistant isolates, confirming the DHPLC results. In addition to four previously reported mutations (22), one new mutation was found. Sequencing of the mutations created by site-directed mutagenesis revealed four additional mutation types (Table 1).
DHPLC analysis to identify two particular mutant types.
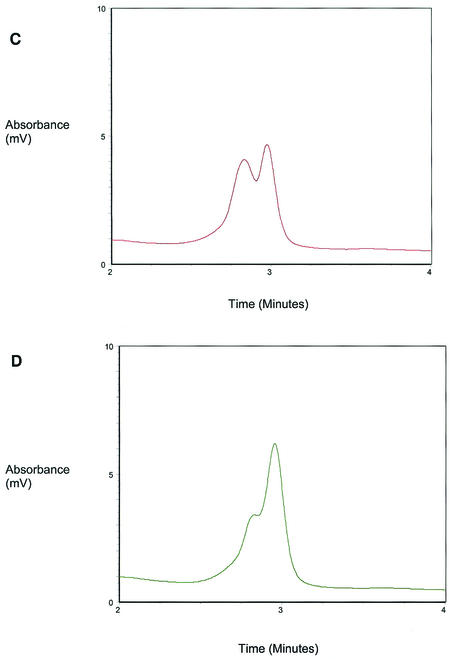
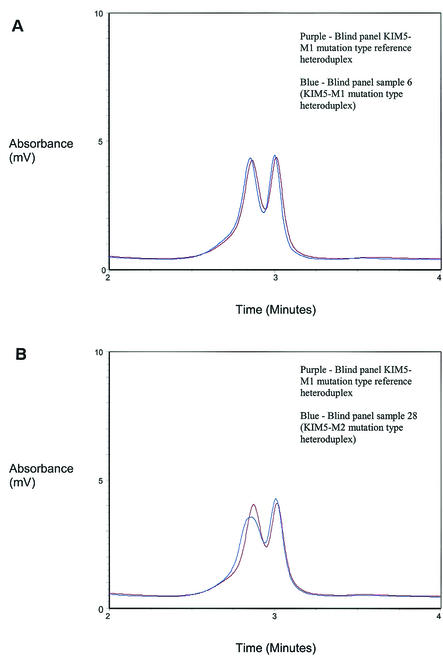
To evaluate DHPLC as a method of identifying two Y. pestis KIM5 mutants, we used overlays of chromatograms to look for DHPLC patterns matching those acquired from Y. pestis KIM5-M1 and -M8 heteroduplexes from a blinded panel of 42 randomly picked samples (Fig. 3). To ensure that the analysis was blind, a new DHPLC column was used. Of the 15 M1 mutants on the panel, all were identified correctly. The one M8 mutant on the panel was also identified correctly (Table 2). None of the remaining 26 panel samples were incorrectly identified as M1 or M8.
FIG. 3.
Blind panel DHPLC peak profiles. All peak profiles depicted are from the first lot and second lot of samples and were generated from a column different from the column used for Fig. 1 and 2. (A) Overlay of blind panel KIM5-M1 mutation type reference heteroduplex (purple) and blind panel sample 6 (KIM5-M1 mutation type heteroduplex) (blue); (B) overlay of blind panel KIM5-M1 mutation type reference heteroduplex (purple) and blind panel sample 28 (KIM5-M2 mutation type heteroduplex) (blue); (C) overlay of blind panel KIM5-M8 mutation type reference heteroduplex (green) and blind panel sample 7 (KIM5-M9 mutation type heteroduplex) (gray); (D) overlay of KIM5-M8 mutation type reference heteroduplex (green) and blind panel sample 9 (KIM5-M4 mutation type heteroduplex) (black).
DISCUSSION
We analyzed a portion of the gyrA gene that contained the QRDR in Y. pestis KIM5 by DHPLC to determine whether the technique can be used as a method of detecting and identifying ciprofloxacin-resistant organisms. We successfully detected every mutation in our sample set. In addition, we were able to obtain unique peak profiles for seven of the nine types of mutations. Two mutations, M4 and M6, had similar peak profiles at all temperatures tested. However, M6 is an in vitro-generated mutation and we do not know if this point mutation can occur naturally. None of the ciprofloxacin-derived mutation types (M1 to M5) had peak profiles similar to each other.
Our sequencing data revealed five distinct mutations in the gyrA QRDR from 55 ciprofloxacin-resistant isolates of Y. pestis KIM5. Four of the mutations in the Y. pestis gyrA QRDR leading to amino acid substitutions at 81 and 83 were previously described by Lindler et al. (22). One mutation was unique and has not been previously reported: Ser→Arg at position 83. In addition, four mutations corresponding to amino acids 67, 84, 87, and 106 of the E. coli gyrA gene were generated by site-directed mutagenesis to further evaluate this method of detection and identification. These mutations are well characterized and have been reported to occur in other organisms with quinolone resistance (39, 40).
Several methods exist for identifying antibiotic-resistant organisms. These include agar diffusion assay (2), single-stranded confirmation polymorphism (28), mismatch amplification mutation assay (16, 39, 41), 5′ nuclease assay (25), fluorescence resonance energy transfer (FRET) assay (22), and nucleic acid sequencing. Agar diffusion assays are time-consuming. This method requires an overnight incubation, followed by reading of the plates. Single-stranded confirmation polymorphism identifies individual mutations but requires gel electrophoresis. Mismatch amplification mutation assay also identifies particular mutations. However, to identify individual mutations in a gene, multiple primer sets are required, and gel electrophoresis is required. The 5′ nuclease assay and FRET probes are sensitive and fast but only allow the analysis of a limited number of mutations for each assay. DNA sequencing is time-consuming and expensive. The advantage of DHPLC over these other techniques is that it is fast and economical, and it allows the detection of all mutations in a given region of the genome. A single primer set can be used to detect mutations in an entire gene region.
Recently, a mutation outside the traditional GyrA QRDR was described (8). This mutation occurs at amino acid 51 in the Escherichia coli GyrA protein and confers a greater level of quinolone resistance than mutations found in amino acids 67, 84, 87, and 106. Additional mutations may lie outside the traditional QRDR, and DHPLC has the ability to detect these nontraditional mutations. In addition, each mutation (or mutations) is associated with different MIC (33, 34, 36, 37). Thus, it may be possible to use DHPLC as a method of screening for particularly troublesome organisms.
Denaturing HPLC is typically used to detect variations in DNA sequences by comparing wild-type chromatograms to experimental chromatograms. We expanded this method so that it can be used for identification purposes. A previous study conducted in this lab demonstrated the reproducibility of DHPLC by analyzing heteroduplexes generated from a segment of the 16S rRNA gene in a variety of microorganisms. Reproducibility was confirmed in that study by performing three consecutive injections on four different days (15). In the present study, we identified mutation types and, to demonstrate the effectiveness of the method, we screened a blind panel for two mutation types. To identify more mutation types, additional reference mutation types would have to be used. Overlaying a large number of reference chromatograms on top of a large number of experimental chromatograms would be cumbersome, and, with each additional overlay, the chance of technician error increases. An alternate approach would be to run the assay in two steps. The first step would be to use a reference ciprofloxacin-sensitive homoduplex and a reference heteroduplex representing a predominant mutation type. The second part of the assay would be a rerun of samples that did not match either the reference homoduplex or the predominant reference heteroduplex with reference heteroduplexes representing the other mutation types. However, the assay is no longer quick when multiple steps are used. It may be possible to develop pattern recognition software. With such software a computer would analyze reference and experimental chromatograms and determine which are matches. Computer analysis would speed up the analyzing time and reduce the number of technician errors.
In addition to the gyrA and gyrB genes in DNA gyrase, quinolone resistance has also been associated with mutations of another type II bacterial topoisomerase, topoisomerase IV. This enzyme has DNA decantation activity and is encoded by the parC and parE genes (11). Double gyrA-parC mutations have been associated with increased levels of quinolone resistance compared to single gyrA mutations (10). Several primer sets could be used to analyze the QRDRs of all genes involved in quinolone resistance.
In summary, we tested a total of 86 samples from 55 isolates to determine whether DHPLC could be used to detect mutations in the gyrA QRDR of Y. pestis KIM5. In addition, four samples were generated by site-directed mutagenesis. We detected every mutation in the sample set. Furthermore, a blind panel of 42 samples containing seven mutation types and several KIM5 wild-type samples was used to investigate DHPLC's ability to identify particular mutations. We were successful in identifying the two mutations tested.
Acknowledgments
This work was supported by an In-House Laboratory Independent Research Reports grant from the Medical, Chemical, Biological, and Defense Research Program of the U.S. Army Medical Research and Materiel Command, Fort Detrick, Md.
REFERENCES
- 1.Arnold, N., E. Gross, U. Schwarz-Boeger, J. Pfisterer, W. Jonat, and M. Kiechle. 1999. A highly sensitive, fast, and economical technique for mutation analysis in hereditary breast and ovarian cancers. Hum. Mutat. 14:333-339. [DOI] [PubMed] [Google Scholar]
- 2.Bauer, A. W., W. M. Kirby, J. C. Sherris, and M. Turck. 1966. Antibiotic susceptibility testing by a standardized single disk method. Am. J. Clin. Pathol. 45:493-496. [PubMed] [Google Scholar]
- 3.Cargill, M., D. Altshuler, J. Ireland, P. Sklar, K. Ardlie, N. Patil, N. Shaw, C. R. Lane, E. P. Lim, N. Kalyanaraman, J. Nemesh, L. Ziaugra, L. Friedland, A. Rolfe, J. Warrington, R. Lipshutz, G. Q. Daley, and E. S. Lander. 1999. Characterization of single-nucleotide polymorphisms in coding regions of human genes. Nat. Genet. 22:231-238. [DOI] [PubMed] [Google Scholar]
- 4.Claes, L., J. Del-Favero, B. Ceulemans, L. Lagae, C. Van Broeckhoven, and P. De Jonghe. 2001. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. Am. J. Hum. Genet. 68:1327-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devaney, J. M., E. L. Pettit, S. G. Kaler, P. M. Vallone, J. M. Butler, and M. A. Marino. 2001. Genotyping of two mutations in the HFE gene using single-base extension and high-performance liquid chromatography. Anal. Chem. 73:620-624. [DOI] [PubMed] [Google Scholar]
- 6.DuPont, H. L. 1993. Quinolones in Salmonella typhi infection. Drugs 45(Suppl. 3):119-124. [DOI] [PubMed] [Google Scholar]
- 7.DuPont, H. L. 1991. Use of quinolones in the treatment of gastrointestinal infections. Eur. J. Clin. Microbiol. Infect. Dis. 10:325-329. [DOI] [PubMed] [Google Scholar]
- 8.Friedman, S. M., T. Lu, and K. Drlica. 2001. Mutation in the DNA gyrase A gene of Escherichia coli that expands the quinolone resistance-determining region. Antimicrob. Agents Chemother. 45:2378-2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gellert, M., K. Mizuuchi, M. H. O'Dea, and H. A. Nash. 1976. DNA gyrase: an enzyme that introduces superhelical turns into DNA. Proc. Natl. Acad. Sci. USA 73:3872-3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goni-Urriza, M., C. Arpin, M. Capdepuy, V. Dubois, P. Caumette, and C. Quentin. 2002. Type II topoisomerase quinolone resistance-determining regions of Aeromonas caviae, A. hydrophila, and A. sobria complexes and mutations associated with quinolone resistance. Antimicrob. Agents Chemother. 46:350-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall, A. G., P. Hamilton, L. Minto, and S. A. Coulthard. 2001. The use of denaturing high-pressure liquid chromatography for the detection of mutations in thiopurine methyltransferase. J. Biochem. Biophys. Methods 47:65-71. [DOI] [PubMed] [Google Scholar]
- 12.Hayward-Lester, A., P. J. Oefner, and P. A. Doris. 1996. Rapid quantification of gene expression by competitive RT-PCR and ion-pair reversed-phase HPLC. BioTechniques 20:250-257. [DOI] [PubMed] [Google Scholar]
- 13.Horton, R. M., H. D. Hunt, S. N. Ho, J. K. Pullen, and L. R. Pease. 1989. Engineering hybrid genes without the use of restriction enzymes: gene splicing by overlap extension. Gene 77:61-68. [DOI] [PubMed] [Google Scholar]
- 14.Huczko, E., B. Conetta, D. Bonner, L. Valera, T. Stickle, A. Macko, and J. Fung-Tomc. 2000. Susceptibility of bacterial isolates to gatifloxacin and ciprofloxacin from clinical trials 1997-1998. Int. J. Antimicrob. Agents 16:401-405. [DOI] [PubMed] [Google Scholar]
- 15.Hurtle, W., D. Shoemaker, E. Henchal, and D. Norwood. 2002. Denaturing HPLC for identifying bacteria. BioTechniques 33:386-391. [DOI] [PubMed] [Google Scholar]
- 16.Jinneman, K. C., and W. E. Hill. 2001. Listeria monocytogenes lineage group classification by MAMA-PCR of the listeriolysin gene. Curr. Microbiol. 43:129-133. [DOI] [PubMed] [Google Scholar]
- 17.Klein, B., G. Weirich, and H. Brauch. 2001. DHPLC-based germline mutation screening in the analysis of the VHL tumor suppressor gene: usefulness and limitations. Hum. Genet. 108:376-384. [DOI] [PubMed] [Google Scholar]
- 18.Kleymenova, E., and C. L. Walker. 2001. Determination of loss of heterozygosity in frozen and paraffin embedded tumors by denaturating high-performance liquid chromatography (DHPLC). J. Biochem. Biophys. Methods 47:83-90. [DOI] [PubMed] [Google Scholar]
- 19.Langemeyer, T. N., W. H. Ferwerda, J. A. Hoogkamp-Korstanje, E. J. de Leur, H. van Oort, J. J. Schipper, and T. van der Wal. 1987. Treatment of chronic bacterial prostatitis with ciprofloxacin. Pharm. Weekbl. Sci. 9(Suppl.):S78-S81. [DOI] [PubMed]
- 20.Lew, D. P., and F. A. Waldvogel. 1999. Use of quinolones in osteomyelitis and infected orthopaedic prosthesis. Drugs 58(Suppl. 2):85-91. [DOI] [PubMed] [Google Scholar]
- 21.Limson, B. M. 1995. Short course quinolone therapy of typhoid fever in developing countries. Drugs 49(Suppl. 2):136-138. [DOI] [PubMed] [Google Scholar]
- 22.Lindler, L. E., W. Fan, and N. Jahan. 2001. Detection of ciprofloxacin-resistant Yersinia pestis by fluorogenic PCR using the LightCycler. J. Clin. Microbiol. 39:3649-3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lipkin, S. M., V. Wang, D. L. Stoler, G. R. Anderson, I. Kirsch, D. Hadley, H. T. Lynch, and F. S. Collins. 2001. Germline and somatic mutation analyses in the DNA mismatch repair gene MLH3: evidence for somatic mutation in colorectal cancers. Hum. Mutat. 17:389-396. [DOI] [PubMed] [Google Scholar]
- 24.Liu, W. O., P. J. Oefner, C. Qian, R. S. Odom, and U. Francke. 1997. Denaturing HPLC-identified novel FBN1 mutations, polymorphisms, and sequence variants in Marfan syndrome and related connective tissue disorders. Genet. Test 1:237-242. [DOI] [PubMed] [Google Scholar]
- 25.Livak, K. J. 1999. Allelic discrimination using fluorogenic probes and the 5′ nuclease assay. Genet. Anal. 14:143-149. [DOI] [PubMed] [Google Scholar]
- 26.McGovern, V. 2002. Taking a world view of asthma. Environ. Health Perspect. 110:A514-A515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Modai, J., et al. 1989. Treatment of serious infections with intravenous ciprofloxacin. Am. J. Med. 87:243S-247S. [DOI] [PubMed]
- 28.Orita, M., Y. Suzuki, T. Sekiya, and K. Hayashi. 1989. Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics 5:874-879. [DOI] [PubMed] [Google Scholar]
- 29.Piddock, L. J. 1999. Mechanisms of fluoroquinolone resistance: an update 1994-1998. Drugs 58(Suppl. 2):11-18. [DOI] [PubMed] [Google Scholar]
- 30.Salyers, A. A. 2002. An overview of the genetic basis of antibiotic resistance in bacteria and its implications for agriculture. Anim. Biotechnol. 13:1-5. [DOI] [PubMed] [Google Scholar]
- 31.Schriml, L. M., R. J. Peterson, B. Gerrard, and M. Dean. 2000. Use of denaturing HPLC to map human and murine genes and to validate single-nucleotide polymorphisms. BioTechniques 28:740-745. [DOI] [PubMed] [Google Scholar]
- 32.van Poppel, H., V. Chysky, R. Hullmann, and L. Baert. 1988. Clinical experience with ciprofloxacin in the treatment of urinary tract infections: a review. Infection 16:337-344. [DOI] [PubMed] [Google Scholar]
- 33.Vila, J., J. Ruiz, P. Goni, A. Marcos, and T. Jimenez de Anta. 1995. Mutation in the gyrA gene of quinolone-resistant clinical isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 39:1201-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vila, J., J. Ruiz, F. Marco, A. Barcelo, P. Goni, E. Giralt, and T. Jimenez de Anta. 1994. Association between double mutation in gyrA gene of ciprofloxacin-resistant clinical isolates of Escherichia coli and MICs. Antimicrob. Agents Chemother. 38:2477-2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang, J. C. 1985. DNA topoisomerases. Annu. Rev. Biochem. 54:665-697. [DOI] [PubMed] [Google Scholar]
- 36.Weigel, L. M., G. J. Anderson, R. R. Facklam, and F. C. Tenover. 2001. Genetic analyses of mutations contributing to fluoroquinolone resistance in clinical isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:3517-3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weigel, L. M., G. J. Anderson, and F. C. Tenover. 2002. DNA gyrase and topoisomerase IV mutations associated with fluoroquinolone resistance in Proteus mirabilis. Antimicrob. Agents Chemother. 46:2582-2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiao, W., and P. J. Oefner. 2001. Denaturing high-performance liquid chromatography: a review. Hum. Mutat. 17:439-474. [DOI] [PubMed] [Google Scholar]
- 39.Yoshida, H., M. Bogaki, M. Nakamura, and S. Nakamura. 1990. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob. Agents Chemother. 34:1271-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoshida, H., T. Kojima, J. Yamagishi, and S. Nakamura. 1988. Quinolone-resistant mutations of the gyrA gene of Escherichia coli. Mol. Gen. Genet. 211:1-7. [DOI] [PubMed] [Google Scholar]
- 41.Zirnstein, G., Y. Li, B. Swaminathan, and F. Angulo. 1999. Ciprofloxacin resistance in Campylobacter jejuni isolates: detection of gyrA resistance mutations by mismatch amplification mutation assay PCR and DNA sequence analysis. J. Clin. Microbiol. 37:3276-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]