Abstract
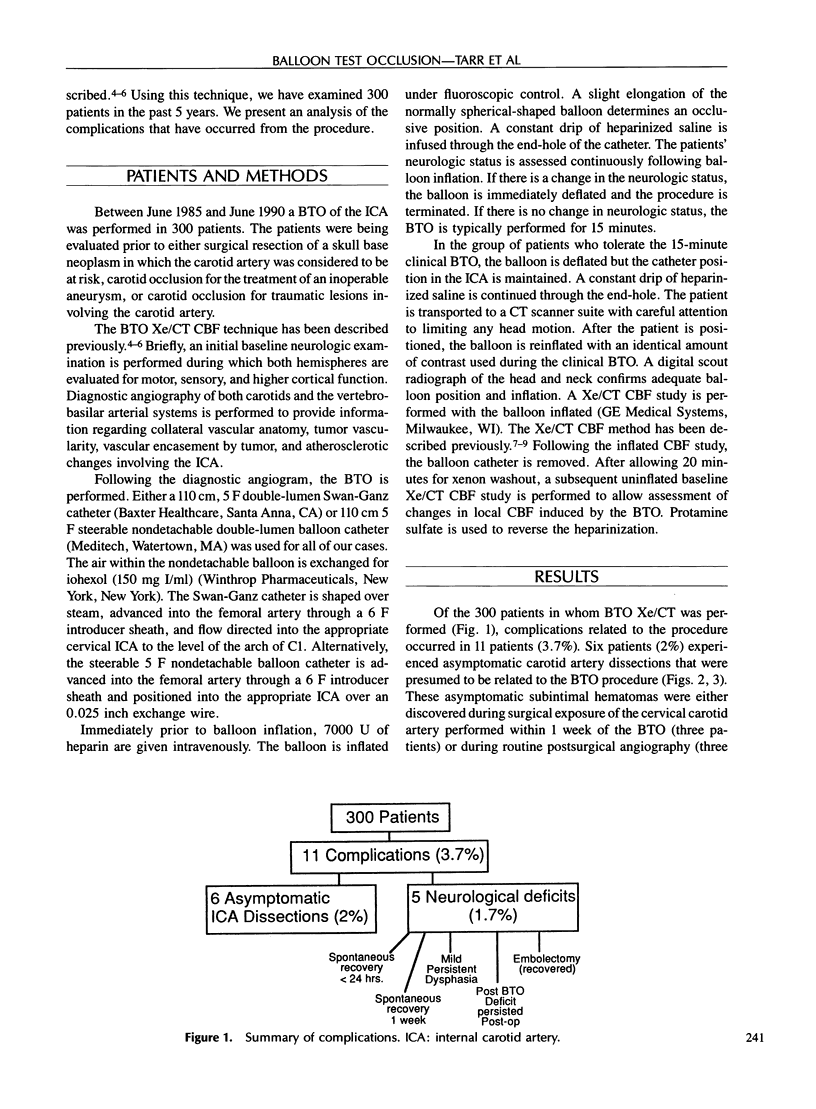
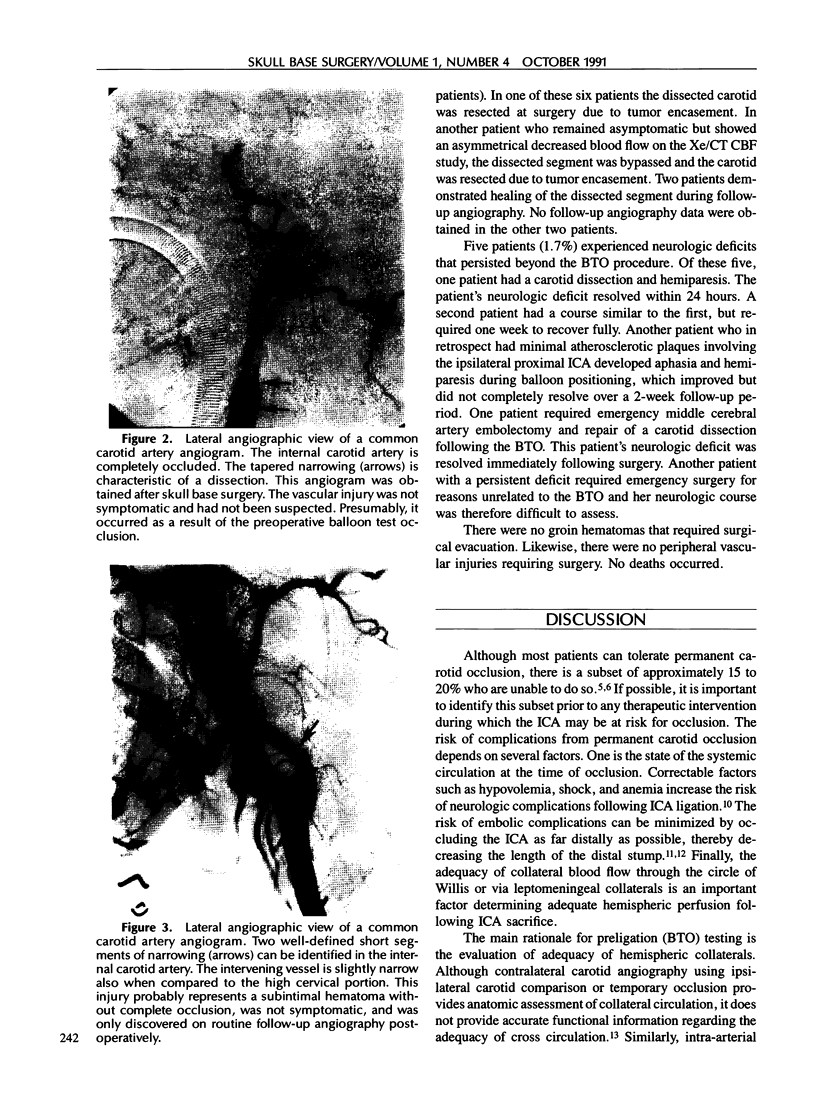
Treatment of some tumors and aneurysms of the skull base may require internal carotid artery (ICA) sacrifice. Preoperatively to determine the dependence of the cerebral blood flow on a particular vessel, we perform a balloon test occlusion (BTO) by temporarily occluding the vessel in an awake patient. During occlusion, clinical evaluations and cerebral blood flow measurements are assessed. We have performed 300 BTOs. Eleven patients (3.7%) have had complications. Six (2%) were asymptomatic dissections. Five (1.7%) had neurologic deficits that persisted beyond the test period. Of these five, one was back to baseline in less than 24 hours, one recovered completely in a week, and one (0.33%) had a minimal but persistent dysphasia. These latter three cases are unexplained but might have resulted from unrecognized dissections or embolic events. Finally, one patient with a persistent deficit required energency surgery for reasons unrelated to the BTO and was therefore difficult to assess, and one required emergency middle cerebral artery embolectomy and repair of the dissection. The preoperative knowledge of carotid dependence in cases in which the ICA is at risk is essential, since vascular grafts or alternative surgical approaches are necessary in patients unable to tolerate carotid sacrifice. Since approximately 15 to 20% of the population falls into this category, a preoperative BTO appears justified.
Full text
PDF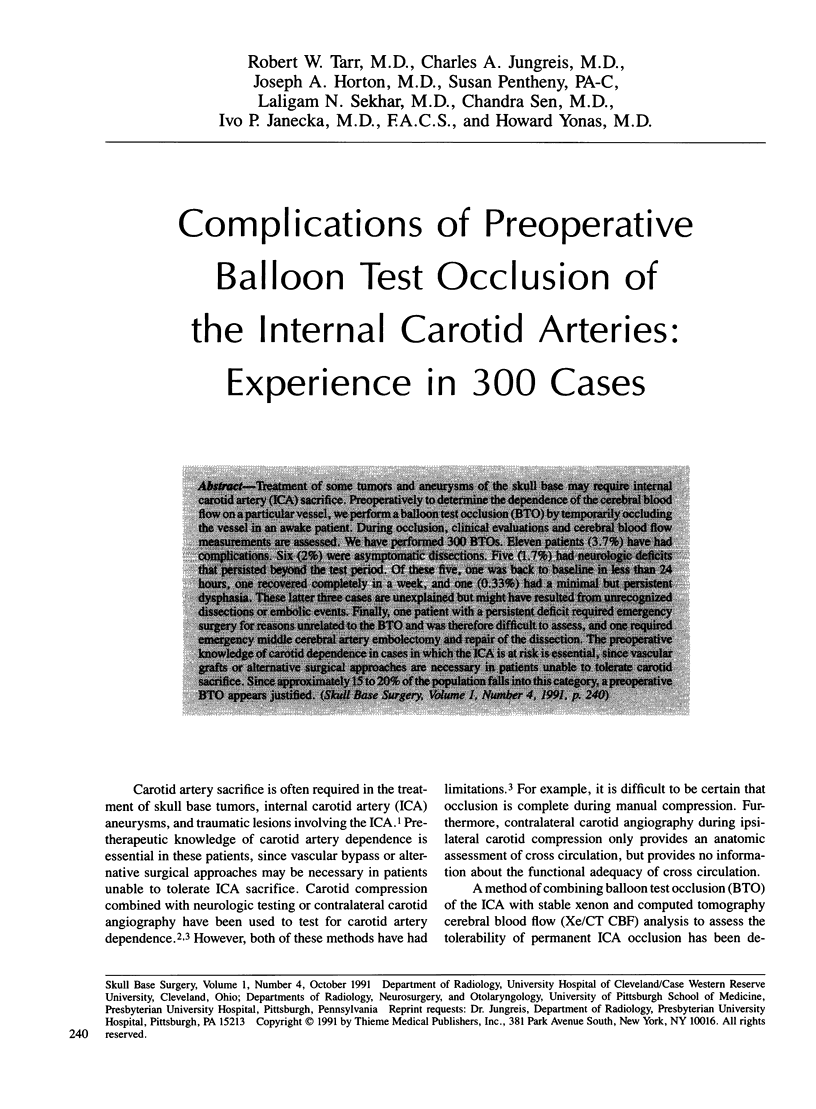

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dion J. E., Gates P. C., Fox A. J., Barnett H. J., Blom R. J. Clinical events following neuroangiography: a prospective study. Stroke. 1987 Nov-Dec;18(6):997–1004. doi: 10.1161/01.str.18.6.997. [DOI] [PubMed] [Google Scholar]
- Eisenberg R. L., Bank W. O., Hedgcock M. W. Neurologic complications of angiography for cerebrovascular disease. Neurology. 1980 Aug;30(8):895–897. doi: 10.1212/wnl.30.8.895. [DOI] [PubMed] [Google Scholar]
- Erba S. M., Horton J. A., Latchaw R. E., Yonas H., Sekhar L., Schramm V., Pentheny S. Balloon test occlusion of the internal carotid artery with stable xenon/CT cerebral blood flow imaging. AJNR Am J Neuroradiol. 1988 May-Jun;9(3):533–538. [PMC free article] [PubMed] [Google Scholar]
- Faught E., Trader S. D., Hanna G. R. Cerebral complications of angiography for transient ischemia and stroke: prediction of risk. Neurology. 1979 Jan;29(1):4–15. doi: 10.1212/wnl.29.1.4. [DOI] [PubMed] [Google Scholar]
- Gonzalez C. F., Moret J. Balloon occlusion of the carotid artery prior to surgery for neck tumors. AJNR Am J Neuroradiol. 1990 Jul-Aug;11(4):649–652. [PMC free article] [PubMed] [Google Scholar]
- Gur D., Good W. F., Wolfson S. K., Jr, Yonas H., Shabason L. In vivo mapping of local cerebral blood flow by xenon-enhanced computed tomography. Science. 1982 Mar 5;215(4537):1267–1268. doi: 10.1126/science.7058347. [DOI] [PubMed] [Google Scholar]
- Gur D., Wolfson S. K., Jr, Yonas H., Good W. F., Shabason L., Latchaw R. E., Miller D. M., Cook E. E. Progress in cerebrovascular disease: local cerebral blood flow by xenon enhanced CT. Stroke. 1982 Nov-Dec;13(6):750–758. doi: 10.1161/01.str.13.6.750. [DOI] [PubMed] [Google Scholar]
- HARRIS P., UDVARHELYI G. B. Aneurysms arising at the internal carotid-posterior communicating artery junction. J Neurosurg. 1957 Mar;14(2):180–191. doi: 10.3171/jns.1957.14.2.0180. [DOI] [PubMed] [Google Scholar]
- Kelly J. J., Callow A. D., O'Donnell T. F., McBride K., Ehrenberg B., Korwin S., Welch H., Gembarowicz R. M. Failure of carotid stump pressures. Its incidence as a predictor for a temporary shunt during carotid endarterectomy. Arch Surg. 1979 Dec;114(12):1361–1366. doi: 10.1001/archsurg.1979.01370360015002. [DOI] [PubMed] [Google Scholar]
- Kerber C. W., Cromwell L. D., Drayer B. P., Bank W. O. Cerebral ischemia. I. Current angiographic techniques, complications, and safety. AJR Am J Roentgenol. 1978 Jun;130(6):1097–1103. doi: 10.2214/ajr.130.6.1097. [DOI] [PubMed] [Google Scholar]
- Mani R. L., Eisenberg R. L., McDonald E. J., Jr, Pollock J. A., Mani J. R. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. I. Criteria and incidence. AJR Am J Roentgenol. 1978 Nov;131(5):861–865. doi: 10.2214/ajr.131.5.861. [DOI] [PubMed] [Google Scholar]
- Matas R. I. Testing the Efficiency of the Collateral Circulation as a Preliminary to the Occlusion of the Great Surgical Arteries. Ann Surg. 1911 Jan;53(1):1–43. doi: 10.1097/00000658-191101000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakano S., Kinoshita K., Jinnouchi S., Hoshi H., Watanabe K. Comparative study of regional cerebral blood flow images by SPECT using xenon-133, iodine-123 IMP, and technetium-99m HM-PAO. J Nucl Med. 1989 Feb;30(2):157–164. [PubMed] [Google Scholar]
- Nishioka H. Results of the treatment of intracranial aneurysms by occlusion of the carotid artery in the neck. J Neurosurg. 1966 Dec;25(6):660–704. doi: 10.3171/jns.1966.25.6.0660. [DOI] [PubMed] [Google Scholar]
- POTTER J. M., TAYLOR F. M. Electroencephalography during carotid occlusion; confusing results in thirty-four cases. AMA Arch Neurol Psychiatry. 1955 Oct;74(4):414–423. doi: 10.1001/archneurpsyc.1955.02330160064009. [DOI] [PubMed] [Google Scholar]
- Podreka I., Suess E., Goldenberg G., Steiner M., Brücke T., Müller C., Lang W., Neirinckx R. D., Deecke L. Initial experience with technetium-99m HM-PAO brain SPECT. J Nucl Med. 1987 Nov;28(11):1657–1666. [PubMed] [Google Scholar]
- Sekhar L. N., Schramm V. L., Jr, Jones N. F., Yonas H., Horton J., Latchaw R. E., Curtin H. Operative exposure and management of the petrous and upper cervical internal carotid artery. Neurosurgery. 1986 Dec;19(6):967–982. doi: 10.1227/00006123-198612000-00012. [DOI] [PubMed] [Google Scholar]
- Yonas H., Good W. F., Gur D., Wolfson S. K., Jr, Latchaw R. E., Good B. C., Leanza R., Miller S. L. Mapping cerebral blood flow by xenon-enhanced computed tomography: clinical experience. Radiology. 1984 Aug;152(2):435–442. doi: 10.1148/radiology.152.2.6739811. [DOI] [PubMed] [Google Scholar]
- de Vries E. J., Sekhar L. N., Horton J. A., Eibling D. E., Janecka I. P., Schramm V. L., Jr, Yonas H. A new method to predict safe resection of the internal carotid artery. Laryngoscope. 1990 Jan;100(1):85–88. doi: 10.1288/00005537-199001000-00017. [DOI] [PubMed] [Google Scholar]




