Abstract
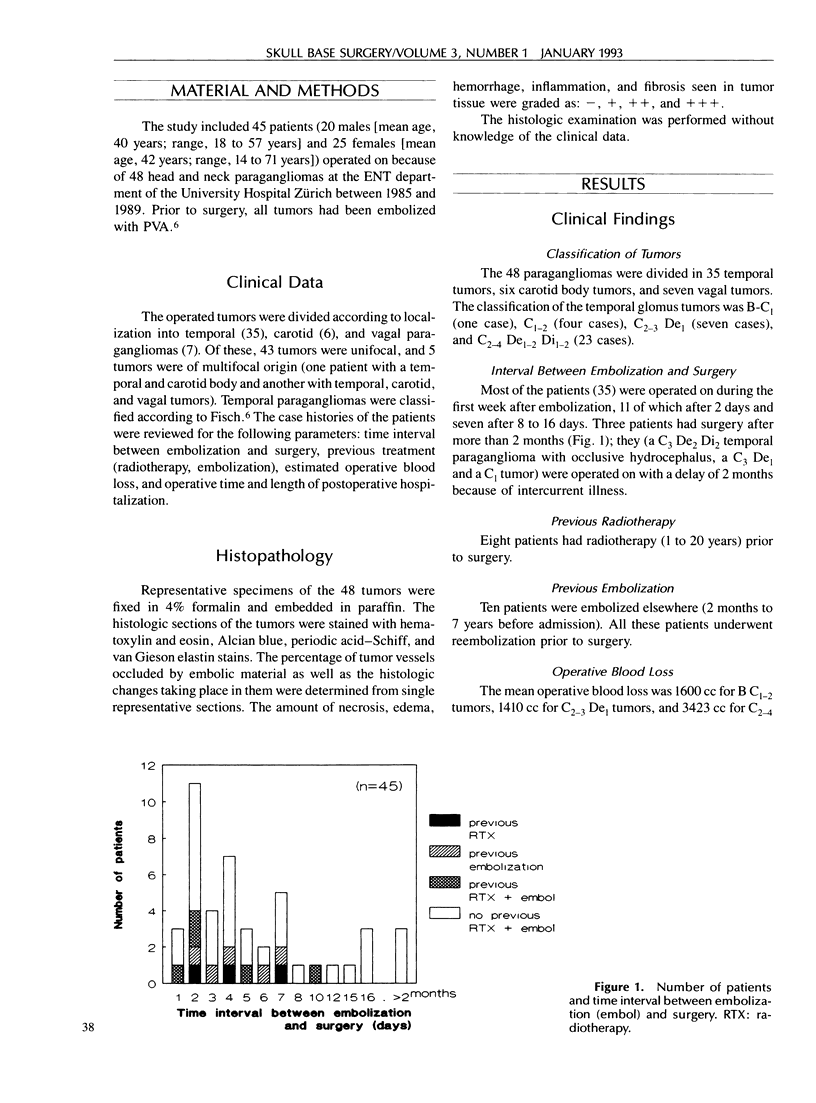
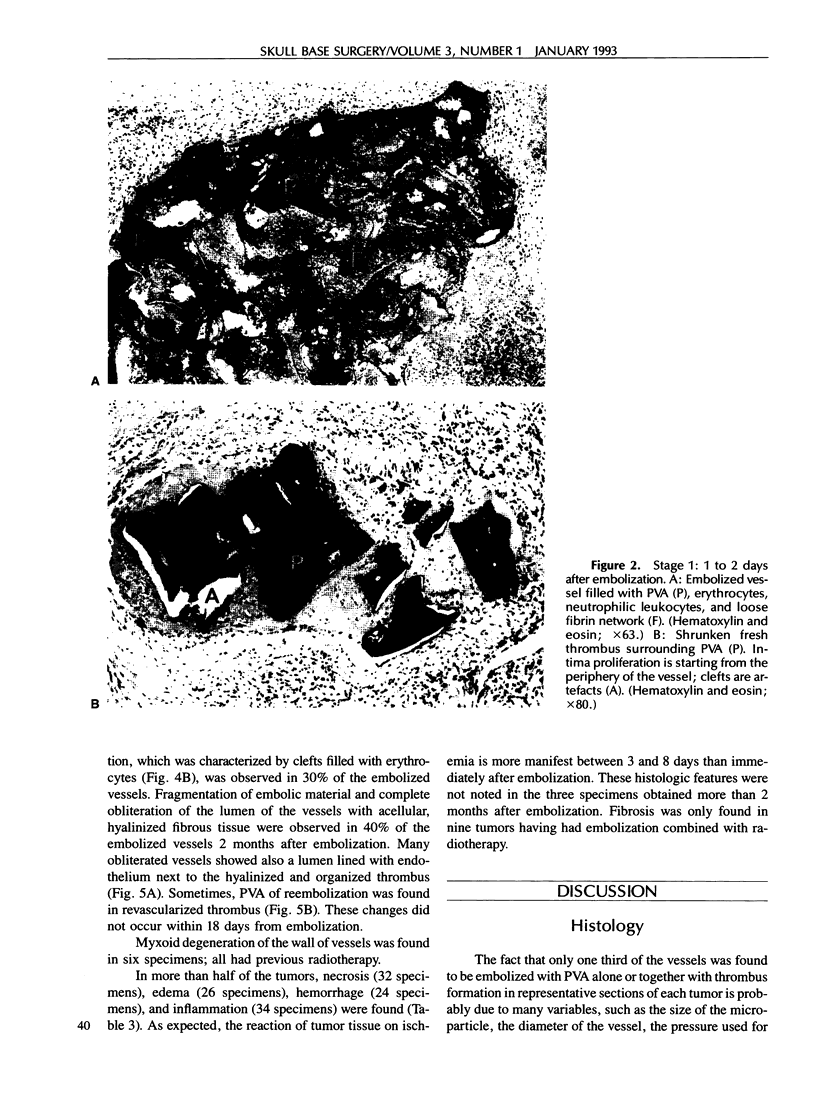
Forty-eight surgical specimens were examined histologically and the case histories reviewed to determine the histopathologic features of embolized paragangliomas (glomus tumors) in relation to the time interval between embolization and surgery. Different degrees of thrombus formation and of multinucleated foreign body giant cells occurred during the first 7 days after embolization; thereafter, glant cells with active phagocytosis, fragmentation of embolic material, and partial revascularization were observed. Only one third of the tumor vessels were embolized. Complete obliteration of 40% of embolized vessels occurred more than 2 months postembolization. The histologic changes induced by embolization in paragangliomas of the head and neck may be classified in four stages. Histologically, the best time for surgery is within 8 days from embolization; surgery performed more than 8 days following embolization, however, is not compromised by revascularization.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- DuBois J., Kelly W., McMenamin P., Macbeth G. A. Bilateral carotid body tumors managed with preoperative embolization: a case report and review. J Vasc Surg. 1987 Apr;5(4):648–650. [PubMed] [Google Scholar]
- Hawthorne M. R., Makek M. S., Harris J. P., Fisch U. The histopathological and clinical features of irradiated and nonirradiated temporal paragangliomas. Laryngoscope. 1988 Mar;98(3):325–331. doi: 10.1288/00005537-198803000-00018. [DOI] [PubMed] [Google Scholar]
- Murphy T. P., Brackmann D. E. Effects of preoperative embolization on glomus jugulare tumors. Laryngoscope. 1989 Dec;99(12):1244–1247. doi: 10.1288/00005537-198912000-00007. [DOI] [PubMed] [Google Scholar]
- Repa I., Moradian G. P., Dehner L. P., Tadavarthy S. M., Hunter D. W., Castañeda-Zúiga W. R., Wright G. B., Katkov H., Johnson P., Chrenka B. Mortalities associated with use of a commercial suspension of polyvinyl alcohol. Radiology. 1989 Feb;170(2):395–399. doi: 10.1148/radiology.170.2.2911663. [DOI] [PubMed] [Google Scholar]
- Robison J. G., Shagets F. W., Beckett W. C., Jr, Spies J. B. A multidisciplinary approach to reducing morbidity and operative blood loss during resection of carotid body tumor. Surg Gynecol Obstet. 1989 Feb;168(2):166–170. [PubMed] [Google Scholar]
- Russell E. J. Functional angiography of the head and neck. AJNR Am J Neuroradiol. 1986 Sep-Oct;7(5):927–936. [PMC free article] [PubMed] [Google Scholar]
- Schick P. M., Hieshima G. B., White R. A., Fiaschetti F. L., Mehringer C. M., Grinnell V. S., Everhart F. R. Arterial catheter embolization followed by surgery for large chemodectoma. Surgery. 1980 Apr;87(4):459–464. [PubMed] [Google Scholar]
- Simpson G. T., 2nd, Konrad H. R., Takahashi M., House J. Immediate postembolization excision of glomus jugulare tumors: advantages of new combined techniques. Arch Otolaryngol. 1979 Nov;105(11):639–643. doi: 10.1001/archotol.1979.00790230009002. [DOI] [PubMed] [Google Scholar]
- Tadavarthy S. M., Moller J. H., Amplatz K. Polyvinyl alcohol (Ivalon)--a new embolic material. Am J Roentgenol Radium Ther Nucl Med. 1975 Nov;125(3):609–616. doi: 10.2214/ajr.125.3.609. [DOI] [PubMed] [Google Scholar]
- Ward P. H., Liu C., Vinuela F., Bentson J. R. Embolization: an adjunctive measure for removal of carotid body tumors. Laryngoscope. 1988 Dec;98(12):1287–1291. doi: 10.1288/00005537-198812000-00002. [DOI] [PubMed] [Google Scholar]
- Young N. M., Wiet R. J., Russell E. J., Monsell E. M. Superselective embolization of glomus jugulare tumors. Ann Otol Rhinol Laryngol. 1988 Nov-Dec;97(6 Pt 1):613–620. doi: 10.1177/000348948809700607. [DOI] [PubMed] [Google Scholar]






