Abstract
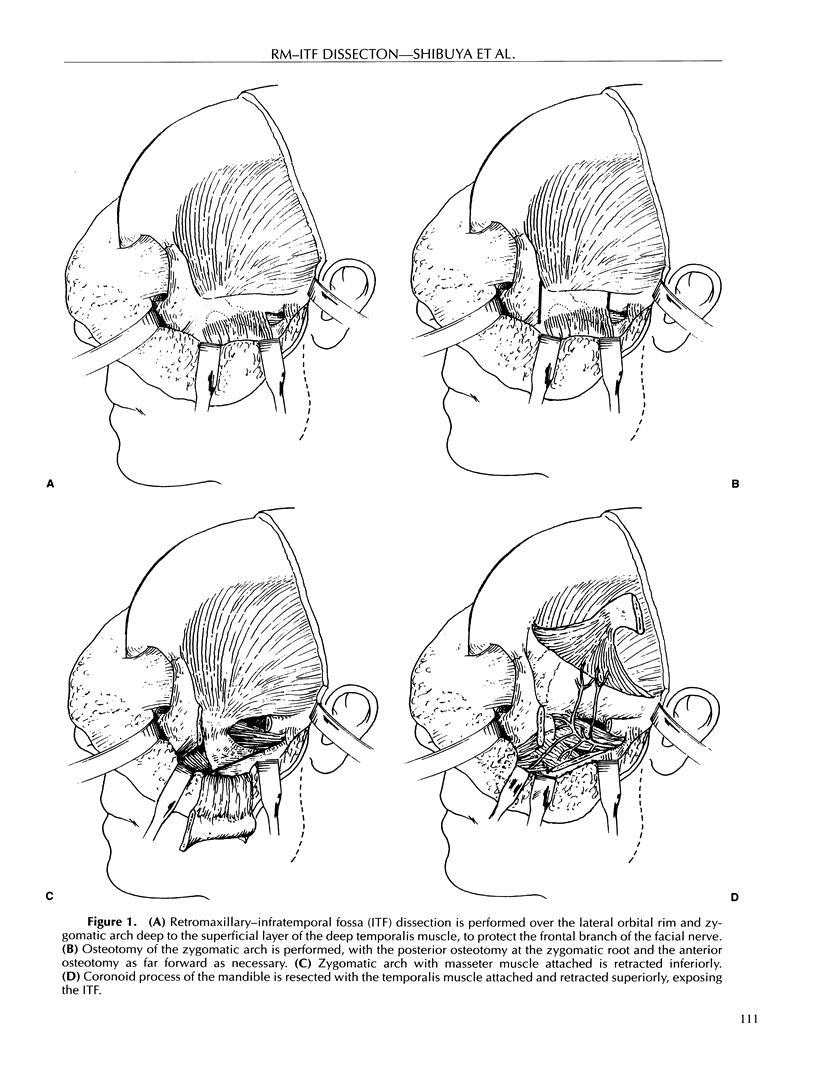
The retromaxillary-infratemporal fossa (RM-ITF) dissection, using a preauricular incision, was initially popularized for the treatment of temporomandibular joint disorders, facial fractures, and orbital tumors. This approach has been expanded for the treatment of advanced head and neck and skull base tumors extending into the infratemporal fossa. We studied prospectively eight consecutive patients requiring a RM-ITF dissection. Pre- and postoperative functional outcomes measured were mastication, speech, swallowing, cranial nerve function, pain, and cosmesis. A significant reduction in pain was noted postoperatively in all patients studied. Limited changes were identified in mastication, speech, swallowing, vision, hearing, or cosmesis postoperatively. The RM-ITF dissection should be considered when resecting advanced head and neck/skull base lesions that extend into this region. We have found minimal morbidity associated with this dissection. This procedure may have a useful place in palliation of patients with incurable pain caused by tumor invasion into the infratemporal fossa.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CONLEY J. J. The surgical approach to the pterygoid area. Ann Surg. 1956 Jul;144(1):39–43. doi: 10.1097/00000658-195607000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CROCKETT D. J. SURGICAL APPROACH TO THE BACK OF THE MAXILLA. Br J Surg. 1963 Sep;50:819–821. doi: 10.1002/bjs.18005022613. [DOI] [PubMed] [Google Scholar]
- Fagan J. J., Snyderman C. H., Carrau R. L., Janecka I. P. Nasopharyngeal angiofibromas: selecting a surgical approach. Head Neck. 1997 Aug;19(5):391–399. doi: 10.1002/(sici)1097-0347(199708)19:5<391::aid-hed5>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Fisch U., Fagan P., Valavanis A. The infratemporal fossa approach for the lateral skull base. Otolaryngol Clin North Am. 1984 Aug;17(3):513–552. [PubMed] [Google Scholar]
- Fisch U. The infratemporal fossa approach for nasopharyngeal tumors. Laryngoscope. 1983 Jan;93(1):36–44. doi: 10.1288/00005537-198301000-00007. [DOI] [PubMed] [Google Scholar]
- House J. W., Brackmann D. E. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985 Apr;93(2):146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- Irish J. C., Gullane P. J., Gentili F., Freeman J., Boyd J. B., Brown D., Rutka J. Tumors of the skull base: outcome and survival analysis of 77 cases. Head Neck. 1994 Jan-Feb;16(1):3–10. doi: 10.1002/hed.2880160103. [DOI] [PubMed] [Google Scholar]
- Leonetti J. P., al-Mefty O., Eisenbeis J. F., Carr W. C., Jr Orbitocranial exposure in the management of infratemporal fossa tumors. Otolaryngol Head Neck Surg. 1993 Oct;109(4):769–772. doi: 10.1177/019459989310900424. [DOI] [PubMed] [Google Scholar]
- Mann W. J., Gilsbach J., Seeger W., Flöel H. Use of a malar bone graft to augment skull-base access. Arch Otolaryngol. 1985 Jan;111(1):30–33. doi: 10.1001/archotol.1985.00800030064007. [DOI] [PubMed] [Google Scholar]
- McCaffrey T. V., Olsen K. D., Yohanan J. M., Lewis J. E., Ebersold M. J., Piepgras D. G. Factors affecting survival of patients with tumors of the anterior skull base. Laryngoscope. 1994 Aug;104(8 Pt 1):940–945. doi: 10.1288/00005537-199408000-00006. [DOI] [PubMed] [Google Scholar]
- Obwegeser H. L. Temporal approach to the TMJ, the orbit, and the retromaxillary-infracranial region. Head Neck Surg. 1985 Jan-Feb;7(3):185–199. doi: 10.1002/hed.2890070302. [DOI] [PubMed] [Google Scholar]
- Osguthorpe J. D. Sinus neoplasia. Arch Otolaryngol Head Neck Surg. 1994 Jan;120(1):19–25. doi: 10.1001/archotol.1994.01880250015001. [DOI] [PubMed] [Google Scholar]
- Palmieri C., Ellis E., 3rd, Throckmorton G. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg. 1999 Jul;57(7):764–776. doi: 10.1016/s0278-2391(99)90810-8. [DOI] [PubMed] [Google Scholar]
- Samy L. L., Girgis I. H. Transzygomatic approach for nasopharyngeal fibromata with extrapharyngeal extension. J Laryngol Otol. 1965 Sep;79(9):782–795. doi: 10.1017/s0022215100064379. [DOI] [PubMed] [Google Scholar]
- Throckmorton G. S., Talwar R. M., Ellis E., 3rd Changes in masticatory patterns after bilateral fracture of the mandibular condylar process. J Oral Maxillofac Surg. 1999 May;57(5):500–509. doi: 10.1016/s0278-2391(99)90061-7. [DOI] [PubMed] [Google Scholar]
- Wetmore S. J., Suen J. Y., Snyderman N. L. Preauricular approach to infratemporal fossa. Head Neck Surg. 1986 Nov-Dec;9(2):93–103. doi: 10.1002/hed.2890090205. [DOI] [PubMed] [Google Scholar]
- Zhang M., Garvis W., Linder T., Fisch U. Update on the infratemporal fossa approaches to nasopharyngeal angiofibroma. Laryngoscope. 1998 Nov;108(11 Pt 1):1717–1723. doi: 10.1097/00005537-199811000-00023. [DOI] [PubMed] [Google Scholar]